CME for
KSGE members
Lee and Kang: Differential Diagnosis for Chronic Diarrhea: Are Multiple Random Biopsies with Colonoscopy Mandatory?
Quiz
A 65-year-old woman visited our hospital complaining of watery diarrhea and intermittent low abdominal pain for the past 6 months. Her stool frequency was generally 5ŌĆō10 times a day. Her symptoms did not include fever, weight loss, rectal bleeding, or bowel movements at night. Colonoscopy 6 months ago were not remarkable. She takes aceclofenac for knee pain as needed.
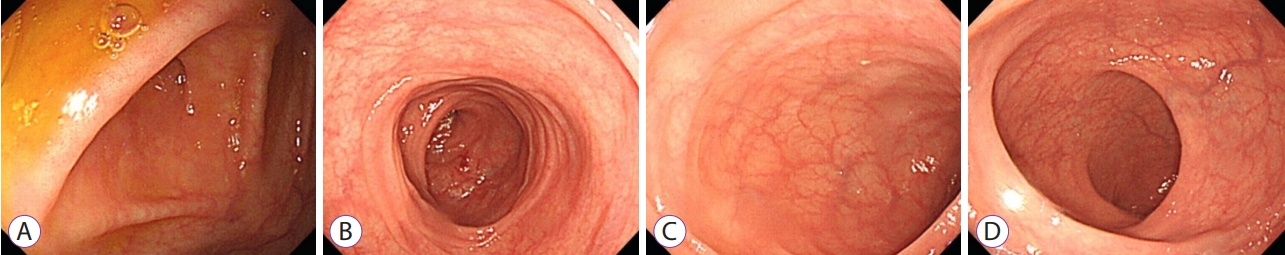
Her complete blood count, blood chemistry, and thyroid function analysis were normal. Results of stool examination, including toxin for Clostridium difficile, were negative, except for a slightly elevated fecal calprotectin level (110 ╬╝g/mg). Colonoscopy was performed to identify the cause of chronic diarrhea. The colonic mucosa was relatively normal, but the vascular pattern sporadically decreased ( Fig. 1). Multiple random biopsies were performed in the entire colon ( Fig. 2). What is the most likely diagnosis?
Answer 
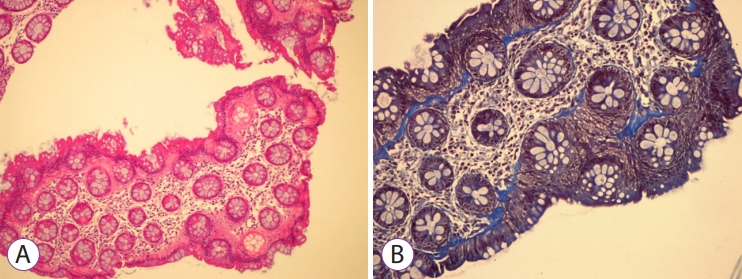
Based on the pathological findings, the diagnosis was collagenous colitis (CC), a subtype of microscopic colitis (MC). MC is a relatively common cause of chronic and intermittent, watery, non-bloody diarrhea, especially in women and elderly individuals [ 1]. Other symptoms may include abdominal pain, weight loss, urgency, fecal incontinence, fatigue, arthralgia, and myalgia. Diabetes, thyroid dysfunction, and psoriasis are more common in patients with MC. Studies have reported on the association of MC with several medications, such as non-steroidal anti-inflammatory drugs, proton pump inhibitors, aspirin, acarbose, selective serotonin reuptake inhibitors, and ticlopidine [ 2]. Colonoscopic findings are usually normal, even in cases of minor colonic mucosal changes such as erythema, edema, and abnormal vascular pattern. Occasionally, colonic mucosal tears (cat-scratch colon) may also be observed [ 3]. Multiple random biopsies are essential for differential diagnosis, considering that the majority of the presenting symptoms are non-specific and it is difficult to distinguish them from those of irritable bowel syndrome. The two most typical forms of MC are CC and lymphocytic colitis (LC). The characteristic histopathological finding of CC is a subepithelial collagen band Ōēź10 ╬╝m in thickness. The diagnosis of LC depends on the presence of an increased number of intraepithelial lymphocytes (IELs), for example, over 20 IELs per 100 epithelial cells. Fecal calprotectin is generally slightly elevated [ 4]. Antidiarrheal medications such as loperamide, diphenoxylate, mesalamine, budesonide, azathioprine, and tumor necrosis factor-alpha inhibitors can be effective in the treatment of patients with MC [ 5]. Therefore multiple random biopsies should be performed to evaluate the cause of chronic diarrhea.
Fig.┬Ā1.
Colonoscopic findings demonstrating a relatively normal colonic mucosa with some areas of decreased vascular pattern in the cecum (A), transverse colon (B), sigmoid colon (C), and rectum (D). 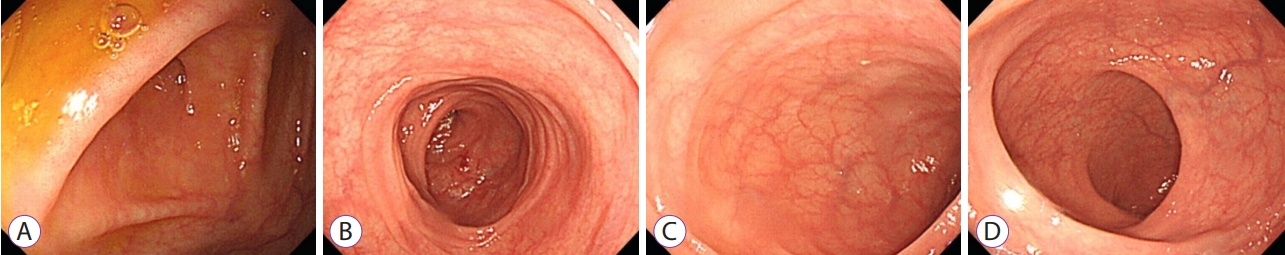
Fig.┬Ā2.
Microscopic findings showing a thickened subepithelial collagen band (12 ╬╝m) with (A) hematoxylin and eosin stain, ├Ś50 magnification, and (B) MassonŌĆÖs Trichrome stain, ├Ś100 magnification. 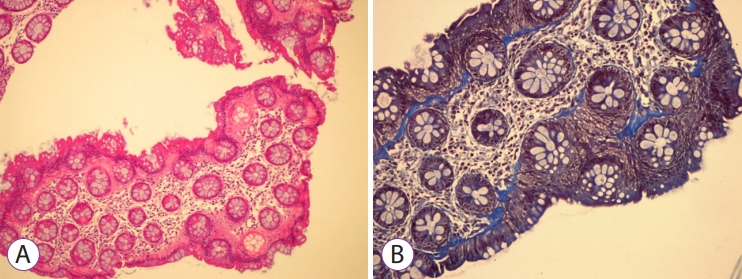
REFERENCES
1. Mellander MR, Ekbom A, Hultcrantz R, L├Čfberg R, ├¢st ├ģ, Bj├Črk J. Microscopic colitis: a descriptive clinical cohort study of 795 patients with collagenous and lymphocytic colitis. Scand J Gastroenterol 2016;51:556ŌĆō562.   4. Pardi DS. Diagnosis and management of microscopic colitis. Am J Gastroenterol 2017;112:78ŌĆō85.   5. Miehlke S, Verhaegh B, Tontini GE, Madisch A, Langner C, M├╝nch A. Microscopic colitis: pathophysiology and clinical management. Lancet Gastroenterol Hepatol 2019;4:305ŌĆō314.  
|
|