Endoscopic Submucosal Dissection for Recurrent or Residual Superficial Esophageal Cancer after Chemoradiotherapy: Two Cases
Article information
Abstract
We report two cases of endoscopic submucosal dissection (ESD) for recurrent or residual esophageal squamous cell carcinoma (ESCC) lesions after chemoradiotherapy for advanced esophageal cancer. Case 1 involved a 64-year-old man who had previously undergone chemoradiotherapy for advanced ESCC and achieved a complete response (CR) for 22 months, until metachronous recurrent superficial ESCC was detected on follow-up esophagogastroduodenoscopy (EGD). We performed ESD and found no evidence of recurrence for 24 months. Case 2 involved a 59-year-old man who had previously undergone chemoradiotherapy for advanced ESCC. He responded favorably to treatment, and most of the tumor had disappeared on follow-up EGD 4 months later. However, there were two residual superficial esophageal lugol-voiding lesions. We performed ESD, and he had a CR for 32 months thereafter. ESD can be considered a viable treatment option for recurrent or residual superficial ESCC after chemoradiotherapy for advanced esophageal cancer.
INTRODUCTION
Chemoradiotherapy (CRT) is the preferred primary treatment modality for esophageal squamous cell carcinoma (ESCC). However, about 13% of patients treated for ESCC with CRT have residual tumor or experience recurrence after treatment [1,2]. The optimal treatment method for local recurrence remains controversial. Surgery is suggested as a salvage therapy for such patients; however, the high mortality and morbidity rates associated with this approach are a cause for concern [2]. Recently, several authors have reported favorable outcomes with esophageal endoscopic submucosal dissection (ESD) for recurrent ESCC after CRT [3,4]. En bloc resection of mucosal lesions can be achieved with ESD. In addition, ESD is an effective and relatively safe treatment for ESCC [5,6]. Although ESCC is responsive to CRT, CRT monotherapy can sometimes result in local recurrence [7]. In the present study, we used ESD for recurrent and residual ESCC lesions after CRT for advanced esophageal cancer.
CASE REPORTS
Case 1
A 64-year-old man visited our department with a complaint of dysphagia and chest discomfort that had been present for 1 month. Esophagogastroduodenoscopy (EGD) revealed an esophageal ulcerofungating mass 24 cm from the incisors (Fig. 1A); the scope could not be passed beyond the lesion. The biopsy report revealed moderately differentiated invasive squamous cell carcinoma (SCC).
Initial esophagogastroduodenoscopy and positron emission tomography (PET) findings of case 1. (A) Esophageal mass lesion 24 cm from the incisors causing malignant stricture; the scope could not reach past the lesion. (B) PET image showing esophageal cancer at the mid to distal portion with paraesophageal invasion, including invasion of the subcarinal lymph node. (C) Image showing the radiation field.
Computed tomography (CT) and positron emission tomography (PET) showed subcarinal lymph node metastasis; however, there was no other lymph node involvement or distant metastasis (Fig. 1B). The tumor was staged as T3N1M0, and CRT was performed. The chemotherapy regimen included 12 courses of 750 mg/m2/day 5-fluorouracil (5-FU) plus 20 mg/m2/day cisplatin for 5 days. One cycle of chemotherapy lasted for 4 weeks. Cisplatin was discontinued because of neuropathy from the eighth chemotherapy cycle. Radiotherapy including 63-Gy doses in 35 fractions was concurrently delivered during the first and second chemotherapy cycles. He showed a complete response (CR) after CRT. We assessed him with EGD every 6 months, and each examination until the 16-month follow-up revealed only scar tissue at the mid-esophagus. The pathological examination of the esophageal scar tissue revealed only glycogenic acanthosis. However, the follow-up EGD at 22 months revealed metachronous recurrence, including an 11-mm superficial esophageal lugol-voiding lesion 33 cm from the incisors, which was involved in the previous radiation field (Fig. 1C). This lesion was pathologically identified as SCC. We then performed endoscopic ultrasonography, which showed that the lesion was confined to the mucosal layer with an intact submucosal layer. We performed ESD for metachronous recurrent ESCC. A submucosal cushion was established through the submucosal injection of a solution consisting of a mixture of sodium hyaluronate (LG Life Science Co., Seoul, Korea), 10% glycerol, and 5% fructose in normal saline solution (Cerol; JW Pharmaceutical Co., Seoul, Korea); a small amount of epinephrine; and indigo carmine. Mucosal cutting and submucosal dissection were performed with a dual knife (KD-650Q; Olympus, Tokyo, Japan). The fibrosis in the submucosal layer was very subtle; submucosal dissection was performed without complications; and en bloc resection was achieved within 25 minutes (Fig. 2). The final pathology results showed well-differentiated SCC with negative basal and lateral resection margins, and invasion to the depth of the lamina propria (Fig. 2C). We assessed him at regular follow-ups with EGD, chest CT, and PET after ESD. Each EGD result showed only scar tissue that was histologically negative for cancer cells. Until 24 months after ESD, follow-up CT and PET scans showed no evidence of local recurrence or distant metastasis.
Esophagogastroduodenoscopy procedure and pathologic findings of case 1. (A, B) Salvage endoscopic submucosal dissection (ESD) for metachronous recurrent superficial esophageal squamous cell carcinoma. The lesion is 32 cm from the incisors and previously treated with radiation. (C) The pathologic finding of the ESD specimen showing a well-differentiated squamous cell carcinoma with lamina propria invasion. Ulceration with dilated vessels (white arrows), inflammatory infiltrates (black arrow), and mild fibrosis (arrowhead) in the lamina propria, so-called radiation change, are noted (H&E stain, ×200).
Case 2
A 59-year-old man visited our department with a complaint of dyspepsia and chest discomfort that had been present for 3 months. We performed EGD and found a large esophageal ulcerofungating mass 29 to 43 cm from the incisors (Fig. 3A). The biopsy results confirmed SCC with an uncertain level of invasiveness. CT and PET showed metastasis to the left supraclavicular lymph node and multiple lymph nodes at the mediastinum (Fig. 3B). The mass was staged as T4N3M1a, and CRT was performed. The chemotherapy regimen included 12 courses of 750 mg/m2/day 5-FU plus 20 mg/m2/day cisplatin for 5 days. One cycle of chemotherapy lasted for 4 weeks. Radiotherapy at 54 Gy was delivered in 30 fractions concurrently during the first and second chemotherapy cycles (Fig. 3C). He responded favorably, and most of the mass disappeared after CRT. EGD at 4 months after CRT showed fibrotic scars 29 to 43 cm from the incisors. However, there were still two small residual superficial esophageal lugol-voiding lesions 38 and 43 cm from the incisors, respectively, and biopsy results revealed moderate- to high-grade squamous dysplasia. EGD at 5 months after CRT still showed mostly fibrotic scars at the previous lesion location; however, two (23×17 and 18×12 mm) superficial lugol-voiding lesions remained 38 and 43 cm from the incisors, respectively, which were located within the initial advanced ESCC margins (14 cm long). We performed ESD for the two residual lesions. A submucosal cushion was established through the submucosal injection of a solution composed of a mixture of sodium hyaluronate (LG Life Science), 10% glycerol, and 5% fructose in normal saline solution (Cerol); a small amount of epinephrine; and indigo carmine. Mucosal cutting and submucosal dissection were performed with a dual knife (KD-650Q). Although ESD for these lesions showed mild submucosal fibrosis caused by the earlier CRT, we achieved en bloc resection for both lesions without any complications within 55 minutes (Fig. 4). The final pathology results revealed well-differentiated SCC confined within the lamina propria 38 cm from the incisors, and high-grade squamous dysplasia 43 cm from the incisors. The resection margins were all negative (Fig. 4C). We followed him regularly with EGD, chest CT, and PET after ESD. Each EGD result showed only scar tissue that was histologically negative for cancer cells. Until 32 months after ESD, follow-up CT and PET showed no evidence of local recurrence or distant metastasis.
Initial esophagogastroduodenoscopy (EGD) and positron emission tomography (PET) findings of case 2. (A) EGD image showing an esophageal ulcerofungating mass. (B) PET scan showing a large esophageal lesion 29 to 43 cm from the incisors and metastasis to the left supraclavicular lymph node (white arrows). (C) Image showing the radiation field.
Esophagogastroduodenoscopy procedure and pathologic finding of case 2. (A, B) Endoscopic submucosal dissection (ESD) en bloc resection of the residual superficial lugol-voiding lesion 38 cm from the incisors. (C) The pathologic finding of the ESD specimen showing a well-differentiated squamous cell carcinoma with lamina propria invasion. Dilated vessels (white arrow), inflammatory infiltrates (black arrow), and mild fibrosis (arrowhead) in the lamina propria are shown (H&E stain, ×200).
DISCUSSION
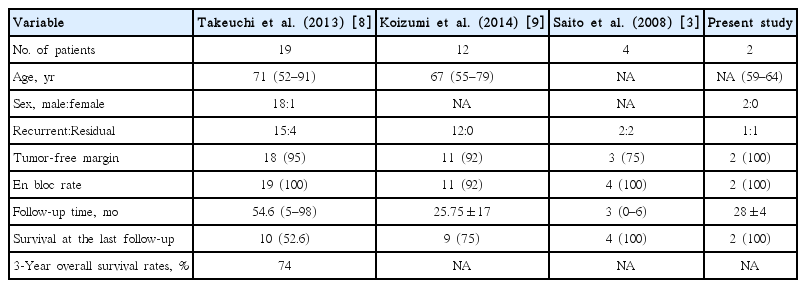
It is challenging to completely cure locally recurrent or residual ESCC after CRT [1,2]. The optimal treatment for these lesions is controversial; however, recent studies have shown that ESD could be an option [2-4]. Saito et al. [3] reported that ESD can be used for the en bloc resection of recurrent or residual superficial esophageal tumors after CRT, with a high rate of CR and without greater risk than for endoscopic mucosal resection. They used ESD to treat four patients with local recurrence of ESCC, and successfully achieved en bloc resection in all patients. Furthermore, Takeuchi et al. [8] reported that ESD represents an acceptable treatment option for recurrent or residual ESCC involving only the submucosal layer without metastasis after CRT because of its effect in improving local control. They successfully treated 19 lesions in 19 patients who underwent salvage ESD. At a median follow-up of 54.6 months, no local recurrence was noted at the treatment site in any patient. The 3-year overall survival rate after salvage ESD was 74% [8]. Koizumi et al. [9] also reported 12 cases of salvage ESD for esophageal SCC after a definitive CRT. The median survival duration after salvage ESD for all patients was 18 months (range, 8 to 70), and 9 of 12 patients have survived [9]. Table 1 shows a summary of the findings of the three previous reports along with the findings in our cases.
Esophageal ESD for ESCC is not an easy procedure. A high level of technical skill is necessary to achieve en bloc resection and to avoid complications such as perforation. Moreover, when there is fibrosis in the submucosal layer, esophageal ESD becomes more technically demanding. Because CRT induces some fibrosis in the esophageal wall, fibrosis at the treatment location can be predicted. This makes ESD procedures difficult, and frequently leads to complications. There are concerns about the technical difficulty of ESD and possible complications from ESD after CRT. Although data on the outcomes of esophageal ESD after CRT are limited, several Japanese authors have reported favorable outcomes for esophageal ESD after CRT [3,8-10]. In addition, our two patients showed favorable outcomes without complications. Safe management of mild fibrosis caused by CRT and acceptable outcomes can be achieved depending on technical skill of the ESD endoscopists.
In this report, we presented two cases of recurrent and residual ESCC treated successfully with ESD after CRT. No complications such as perforation or major bleeding were observed. With a longer follow-up duration, tumors may recur at the original site; however, there has been no recurrence for 26 months in case 1 and for 32 months in case 2. Although it requires patients to be assessed for a long period, salvage ESD can be considered an effective and safe treatment option that requires a certain level of technical expertise when locoregional failure is limited to the mucosal layer with no distant metastases.
Notes
Conflicts of Interest: The authors have no financial conflicts of interest.