Introduction
Periampullary diverticula (PAD) are present in 7.5%ŌłÆ20% of all endoscopic retrograde cholangiopancreatography (ERCP) cases [1,2] and are classified by the position of the major papilla as inside, marginal to, or near the duodenal diverticulum within a 2-cm radius [3]. Recent studies reported that the technical success or complication rates of ERCP did not increase in patients with PAD [4]. However, ERCP through an intradiverticular papilla, especially one with an invisible orifice, remains difficult, and success rates are lower with an invisible orifice [5]. Several techniques have been introduced to evert the papillary opening to facilitate cannulation [1,6-15]. Submucosal injection [6], endoscopic clipping [9], and two-devices-in-one-channel [10], have been introduced. The submucosal injection method involves lifting of the mucosa to enable eversion and fixing of a papilla in the diverticulum and allows selective cannulation of the biliary tree [6]. This may be a safe and convenient technique and is easily performed in ordinary ERCP settings.
We report a case of cholelithiasis with an intradiverticular papilla treated using the submucosal saline injection method, and also provide a literature review.
Case Report
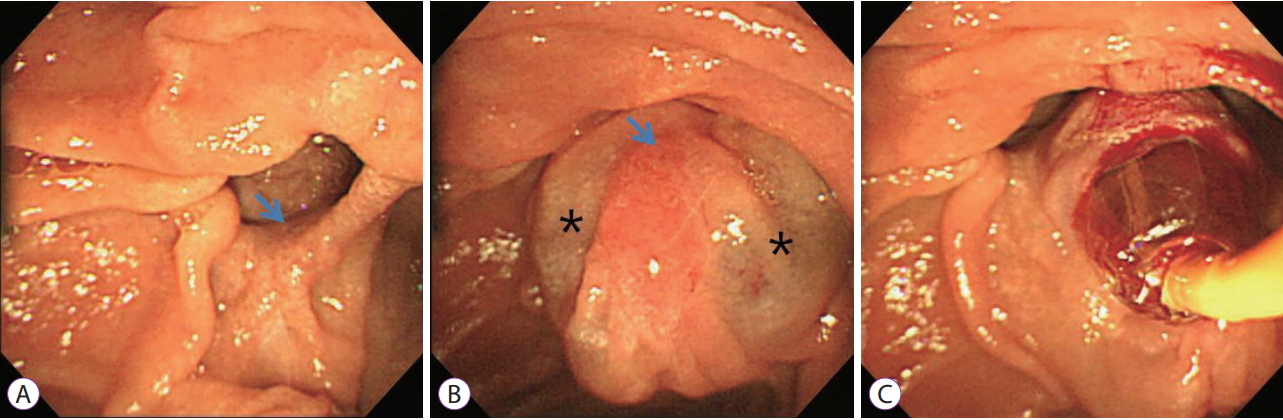
A-79-year-old-woman was admitted to our hospital with a 1-week history of epigastric pain but no fever or jaundice. Physical examination on admission revealed mild epigastric tenderness. Laboratory data showed a white blood cell count of 6,120/mm3, hemoglobin of 11.0 g/dL, hematocrit of 33.9%, platelet count of 189├Ś103/mm3, total protein of 6.8 g/dL, albumin of 4.3 g/dL, aspartate aminotransferase of 32 U/L, alanine aminotransferase of 33 U/L, alkaline phosphatase of 34 U/L, total bilirubin of 0.39 mg/dL, amylase of 25 U/L, and lipase of 27 U/L. Abdominal computed tomography revealed a round stone in the dilated common bile duct and presence of a periampullary diverticulum (Fig. 1). ERCP revealed that the papilla was at the inferior border of a large duodenal diverticulum (Fig. 2A), and the papilla could not be cannulated with a usual method because of inward rotation. We tried cannulation by entering the duodenal diverticulum [14], and a double-catheter method [15], but failed. We chose the submucosal saline injection method to enable eversion and fixation of the papilla in the diverticulum. The submucosal injection of 3 cc of saline at 3 and 9 oŌĆÖclock on the papilla enabled eversion and fixation in the diverticulum and the ability to performed selective cannulation of the biliary tree (Fig. 2B). After endoscopic papillary balloon dilation (EPBD, 10 mm for 60 s), the stones were extracted (Fig. 1C) and a Zimmon single pigtailed biliary stent (7 F, 5 cm) (Cook Medical, Bloomington, IN, USA) was placed. The patient had an uneventful post-procedural course and has been asymptomatic for 2 years.
Discussion
ERCP in patients with PAD is not difficult when performed by experienced endoscopists using specialized techniques and devices [7,8]. Endoscopists must be aware of available cannulation techniques in specific conditions of the papilla. Several techniques have been introduced to facilitate cannulation in the setting of intradiverticular papilla (Table 1) [1,6,9-18]. To enable informed decisions and ensure the best outcomes, endoscopists should be aware of differences in technical feasibility and safety of each technique. The best method depends on the endoscopistŌĆÖs preference and patient conditions. The main goal of various techniques involves bringing the papilla into a better orientation by grasping, pushing, or lifting, or by performing pancreatic duct stenting [7]. Several different methods, such as submucosal injection [6], endoscopic clipping [9], two-devices-in-one-channel [10], reverse guidewire anchoring [11], double endoscopy [12], cap-assisted with forward viewing endoscopy [13], entering the duodenal diverticulum with the distal tip of the duodenoscope [14], and pre-cut biliary sphincterotomy after pancreatic duct stent placement1 have been introduced.
Endoscopic clips are used to evert and stabilize the papillary opening [9]. Deployment of endoscopic clips at the proper positions could be improved using rotatable devices. The twodevices-through-one-channel method exposes the papilla using different devices: grasping by biopsy forceps [10] or pushing by a catheter [15] or reverse guidewire [11]. The reverse guidewire method involves pushing the adjacent mucosa of the papilla toward the duodenal lumen and straightening the folds using the stiff reverse end of the guidewire [11]. Because the two devices work in the same direction, coordination of the two instruments is sometimes difficult. The double endoscope method involves grasping the tissue just beside the papilla with foreign body forceps through the attached clear gastroscope cap and insertion of the duodenoscope alongside the gastroscope for cannulation [12]. Direct visualization of the papillary orifice using cap-assisted forward viewing endoscopy [13] or entering the duodenal diverticulum with the distal tip of the duodenoscope [14] can be effective in some conditions. If the pancreatic duct is cannulated, stent placement aims to keep the papilla out of the diverticulum, and a pre-cut biliary sphincterotomy is performed, which can be helpful for selective biliary cannulation [1]. For patients with a narrow-necked diverticulum, balloon dilation inside the diverticulum allows papillary eversion [16].
When ERCP fails, alternative methods, such as percutaneous ultrasound-guided [17] or endoscopic ultrasound-guided [18] rendezvous technique can be attempted. After percutaneous ultrasound-guided transhepatic biliary puncture or endoscopic ultrasound-guided bile duct puncture, a guidewire is inserted into the bile duct and across the papilla under fluoroscopic guidance to enable deep bile duct cannulation.
Here we used the submucosal saline injection method to lift the papilla into the diverticulum. The submucosal injection of 2ŌĆō4 mL of normal saline at single or multiple points enables intradiverticular papillary eversion. The important step is selecting the best inflation point to preserve the bile duct opening and to maintain papillary eversion. To prolong the submucosal indwelling time, a hyperviscous fluid, such as sodium hyaluronate, can be used. Harada et al. used sodium hyaluronate as an injection fluid for lifting of an intradiverticular papilla and successfully performed ERCP in five cases [6]. They performed endoscopic sphincterotomy (EST) and pancreatic stent placement to prevent post-ERCP pancreatitis. We preferred normal saline as the lifting material because papillary cannulation can be performed within several minutes before normal saline absorption. The absorption of normal saline within several minutes may have an advantage of preventing pancreatitis. We did not perform any procedure to prevent pancreatitis. This method is safe as well as convenient as it requires neither endoscopy changes nor specialized equipment. The injection needle is easily available in ordinary ERCP rooms.
We performed EPBD because of an undefined upper margin due to the saline injection and retrieved bile duct stones. When a large EST is technically difficult in patients with a PAD, EPBD alone or EPBD combined with small EST are alternatives [19].
For patients with PAD, papillary identification is sometimes difficult. Papillae are usually located on the lower margin of or just inside the diverticulum, somewhere between the 4 and 8 oŌĆÖclock positions [7]. Cannulation is more difficult when a papilla is positioned at the 1 oŌĆÖclock position in the diverticulum [2]. In the present case, the papilla was located at the 5 oŌĆÖclock position, and so it could be easily detected. One study reported that an ultrathin gastroscope was used to locate a papilla hidden within a duodenal diverticulum [20].
In conclusion, the submucosal saline injection method may be a safe and convenient technique for biliary cannulation and may be recommended when selective cannulation is difficult in patients with an intradiverticular papilla.