INTRODUCTION
Ectopic pancreas is a relatively rare submucosal tumor (SMT) of gastrointestinal (GI) tract, and it is histologically similar to normal pancreas. It may occur at a variety of sites in the GI tract with a propensity to affect the stomach and small intestine. Although it is usually a silent anomaly, an ectopic pancreas may become clinically evident when complicated by inflammation, bleeding, obstruction or malignant transformation.1,2 Although several cases of ectopic pancreas accompanied by bleeding have been reported,3,4 bleeding found by capsule endoscopy has not been reported except one in Taiwan.5
Here, we report a case of an ectopic pancreas in a 46-year-old woman, who visited our hospital with a sign of GI bleeding. The capsule endoscopy revealed that the bleeding was caused by the SMT in the small intestine, and it was surgically resected.
CASE REPORT
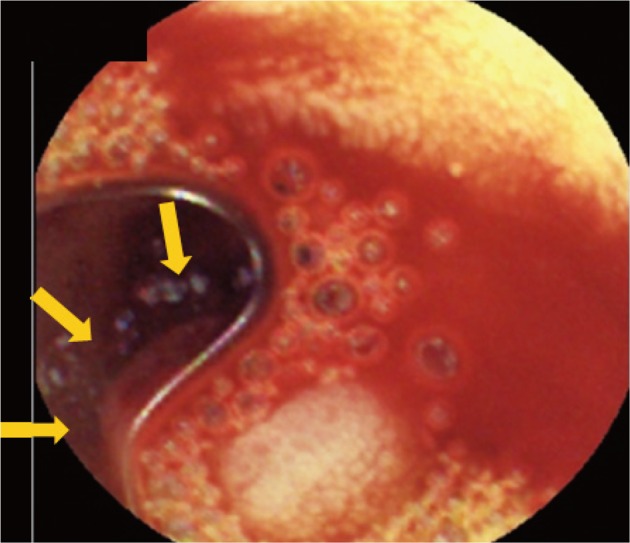
A 46-year-old female presented with episodes of melena and hematochezia accompanied by dizziness, which had been continuing for a week. The patient had been on antihypertensive medication including aspirin for 2 years at the moment. The vital signs showed that pulse rate was 90/min, blood pressure 100/60 mm Hg, and respiratory rate 20/min. She complained mild periumbilical discomfort, but no tenderness was observed. Her initial serum hemoglobin and hematocrit levels were 4.7 g/dL and 14.4%, respectively, and there were no abnormal findings in biochemical and blood coagulation tests. A nasogastric tube was inserted and irrigation with saline was performed. The irrigated saline was clear without blood. On rectal examination, dark red liquid stool was noted. Abdominal computed tomography scan showed no significant abnormalities. Upper GI endoscopy was performed, and there were no lesions to cause bleeding at the esophagus, stomach, or duodenum. On the 2nd hospital day, we performed colonoscopy, which also showed no specific bleeding lesion. Following colonoscopy, second-look upper GI endoscopy was performed, which did not reveal the bleeding focus. Then, a capsule endoscopy was performed subsequently to evaluate the obscure GI bleeding. It revealed active bleeding from a submucosal lesion slightly larger than 1 cm located in the jejunum (Fig. 1) without other erosions or erythemas in the small bowel except the lesion.
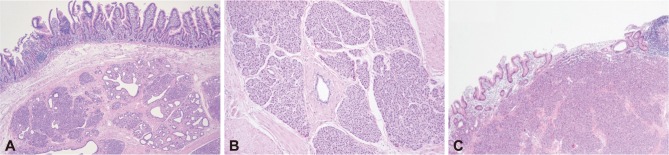
On the 3rd hospital day, barium small bowel examination was performed for exact localization of the tumor, but it could not clarify the SMT of the small bowel. Finally, the patient underwent surgery. The SMT was located in the distal jejunum. It was a round, well-demarcated solid mass (1.5Ć1.5 cm) with a yellow rubbery surface and umbilication (Fig. 2). Histological examination revealed submucosal ectopic pancreatic tissues with focal mucosal defect on the surface (Fig. 3). The patient recovered well after the surgery and has been followed up on an outpatient bases.
DISCUSSION
Ectopic pancreas is a disease showing histological structures similar to normal pancreatic tissues without any anatomical relation or direct connections by blood vessel with the pancreas. It was first reported in 1727 by Schiltz, and its histological features were studied in 1859 by Klob et al.6 Most cases of ectopic pancreas are found by radiological screenings, endoscopic examinations or during surgeries or autopsies.6,7 Because ectopic pancreas is shown as a SMT by endoscopy, differential diagnosis is necessary to distinguish from other SMTs arising from GI tract. However, pathological diagnosis of ectopic pancreas by endoscopy-guided biopsy is often difficult because the tumor is located deeper than where the biopsy forceps can reach. Recently, endoscopic ultrasonographic biopsies are introduced for diagnosis of SMTs.8 Because aspirated biopsy specimen is often not enough for the diagnosis and the cost of the procedure is high, surgical resection is often considered and performed. Around 70% of ectopic pancreas cases are found in the stomach (24% to 38%), duodenum (9% to 36%), and jejunum (0.5% to 27%). Ectopic pancreas has been also reported in the colon, spleen, liver, Meckel's diverticulum, gallbladder, bile ducts, or fallopian tubes.9 Ectopic pancreas in the small intestine mostly occurs in the duodenum and jejunum. The second portion of the duodenum around the ampulla of Vater is considered as a frequent site of ectopic pancreas,10 which is rare in the ileum, though.11 Most cases of ectopic pancreas are known to be asymptomatic,3 but some cases might accompany symptoms.11 The most common symptoms include epigastric pain (77%), abdominal fullness (30%), and hematochezia (24%).6 Bleeding has been reported in 3 out of 73 symptomatic cases among 212 ectopic pancreas patients,4 and in 5 out of 15 symptomatic cases among 39 ectopic pancreas patients.3
The patient in this case report took aspirin, which made it difficult to identify the causes of bleeding in the ectopic pancreas. There were no other erosion by aspirin in the small bowel, and consequently we considered that the aspirin was not the major factor for bleeding. However, aspirin could have incidentally induced ulcer in the ectopic pancreas, which could be a trigger factor for bleeding in the ectopic pancreas of small bowel.
It is difficult to identify bleeding from ectopic pancreas in the small intestine and it is often considered as obscure GI bleeding. Obscure GI bleeding is known to occupy about 5% of all GI bleedings, and 75% of these are thought to be a bleeding from a lesion of the small bowel.13 For the evaluation of the small bowel, capsule endoscopy, push enteroscopy, double balloon enteroscopy, angiography, and barium small bowel examination are available.13,14 A retrospective study reported that 3 cases of ectopic pancreas causing bleeding in the small bowel among 76 cases of obscure GI bleeding were identified using angiography, barium small bowel examination, and enteroscopy.7 There were reports of an ectopic pancreas in the duodenum accompanying massive bleeding detected by side-viewing endoscope followed by surgical resection,15 and a jejunal ectopic pancreas with massive bleeding detected by red blood cell scan and angiography.16 Ectopic pancreas bleeding detected by double balloon endoscopy was also reported.17
Capsule endoscopy has high sensitivity and specificity in detecting cases of obscure GI bleeding.18 A retrospective multicenter study has reported that capsule endoscopy discovered the causes of obscure GI bleedings in 56.2% of 151 patients.19 It is a better result compared with barium small bowel examination, angiography, or push enteroscopy.20 Bleeding from SMT was also well identified in our case by capsule endoscopy-Capsule endoscopy can be considered as the first evaluation method for small bowel lesions, especially those with bleeding from SMT. Ectopic pancreas bleeding was detected by capsule endoscopy only in one case in Taiwan as far as we know,5 and there have been no reports of it in Korea. We reported here a case of bleeding from jejunal ectopic pancreas, which was revealed by capsule endoscopy and treated by surgical excision.