The transmission risk from infected patients to healthcare workers and/or other patients is a concern during the coronavirus disease 2019 (COVID-19) pandemic.1 Especially when performing digestive endoscopy, it seems inevitable that healthcare workers will be exposed to either respiratory or gastrointestinal fluids from patients.2 Therefore, appropriate infection control during digestive endoscopy based on experience is recommended by the World Endoscopy Organization.3 We read with interest the papers reported by Higashimori et al.4 and Nadatani et al.5 In these studies, nasal insertion of a thin endoscope and covering of the patient's mouth with a surgical mask prevented the spread of aerosol droplets due to coughing during the procedure. We support the studiesт findings and suggest that this simple infection control measure be implemented for all screening endoscopy cases. Conversely, several reports on gas leakage or release of fluid droplets from biopsy valves of full-sized endoscopes during insertion and withdrawal of endoscopic instruments have been published.6,7 Gas leakage may be observed even in thin endoscopes. If so, transnasal endoscopy with a surgical mask may be inadequate as an infection control measure, especially when performing procedures requiring instrument traffic, such as biopsies. Therefore, we aimed to visualize the gas leakage from the biopsy valve of the thin endoscope and to prove that simply covering the mouth with a mask is insufficient to prevent COVID-19 infection during endoscopy.
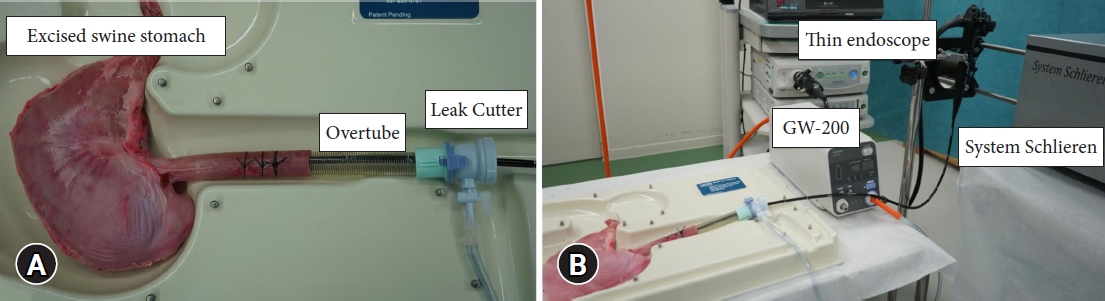
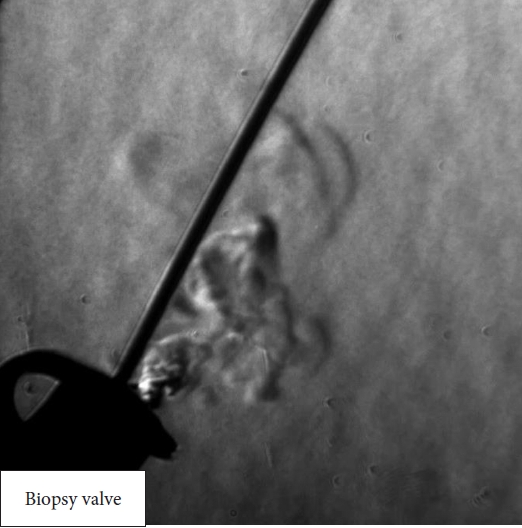
We used System Schlieren (SS100; Kato Koken Co., Ltd.) to visualize the gas leakage in this study. More information on this system can be found on the following website: https://kk-co.jp/products/schlierens.php. System Schlieren is a device that visualizes minute changes in airflow that are invisible to the naked eye by identifying differences in the refractive index of materials. This method is extremely useful for the visualization and evaluation of high-speed phenomena, mainly in the engineering field.8,9 The following experiments were conducted with the intra-gastric pressure of an excised swine stomach maintained at 8 mmHg using a carbon dioxide insufflation system (GW-200; Fujifilm). A thin endoscope (EG-6400N; Fujifilm) was advanced into the stomach, and gas leakage from the biopsy valve during insertion and withdrawal of the biopsy forceps was visualized (Fig. 1). In this experiment, the biopsy forceps for the thin endoscope with an outer diameter of 1.8 mm (Radial Jaw 4P; Boston Scientific) was inserted and withdrawn 3 cm every 3 seconds. This procedure was repeated five times.
Gas leakage from the biopsy valve of the thin endoscope was successfully visualized during forceps insertion and withdrawal (Fig. 2, Supplementary Video 1) in all five procedures, indicating that endoscopists and assistants may be exposed to potentially virus-infected aerosols. Even if the patientтs mouth is covered with a surgical mask, gas leakage cannot be prevented if the biopsy valve is airtight. Therefore, endoscopists and assistants must consider this and take further precautions against COVID-19. To optimize precaution, the development of a reinforced, improved, and leak-proof type biopsy valve is a pressing task.
The entire experimental protocol of this study was approved by the institutional animal care and ethical review board (IVTeC Co., Ltd., Animal Welfare Committee). This study was performed according to the Guide for the Care and Use of Laboratory Animals.