AbstractBackground/AimsThe aim of the study was to evaluate the efficacy of i-scans for the diagnosis of gastroesophageal reflux disease, especially where only minimal change is involved.
MethodsThe esophageal mucosa was inspected using an i-scan following conventional white light endoscopy. The examination with iscan was performed under tone enhancement (TE) esophagus (e) mode. Patients with subtle distal esophageal mucosal changes without definite mucosal breaks, such as blurring of Z-line (B), mucosal coarseness (C), hyperemic or purplish discoloration (D), erythema (E), ectopic gastric mucosal islet (I) and mixed type were classified as minimal change.
ResultsA total of 156 patients were included. Using i-scan endoscopy, the number of minimal change was found to further increase from 94 (conventional endoscopy; 19B, 9C, 29D, 13E, 5I, 19 mixed type) to 109 (i-scan; 15B, 8C, 29D, 16E, 5I, 36 mixed type). And 14 patients who had single type by conventional endoscopy were converted to mixed type after i-scan. Therefore, 29 of 156 patients were upgraded after i-scan, they were account for 19% (p<0.0001; 95% confidence interval, 0.13 to 0.25).
INTRODUCTIONGastroesophageal reflux disease (GERD) is defined as abnormal reflux of gastric contents to the esophagus.1 Its prevalence is approximately 10-30% in U.S. population.2 Changes in dietary habits to more fat consumption, and decreased prevalence of Helicobacter pylori infection had led to an increase in the prevalence of GERD in Asian countries including Korea.3-5
Endoscopy is a widely used diagnostic tool for reflux esophagitis detection.6,7 However, more than half of patients with GERD reveal no visible abnormality on conventional endoscopy, and it is possible that subtle distal esophageal mucosal changes form acid refluxate are underestimated by conventional endoscopy. Recently, there are various studies being published on detection of minimal change of reflux esophagitis using narrow band imaging (NBI), autofluorescence imaging (AFI), Fujinon Intelligent Chromo Endoscopy (FICE) or i-scan.8-11 Especially, i-scan technology (Pentax Co., a subsidiary of Hoya Co., Tokyo, Japan) is a newly developed digital filter-based contrast enhancement technique, which is similar to the conventional endoscopy in structure but uses software-based real-time modification of sharpness, hue and contrast of high-resolution digital image. The aim of this study was to test the efficacy of i-scan endoscopy for the detection of minimal change in GERD, and to find whether i-scan is helpful to overcome limitations of the conventional endoscopy.
MATERIALS AND METHODSPatientsThe study was performed in patients who received esophagogastroscopy between September 2009 and October 2010 at Dong-A University Medical Center for medical checkup or regular follow up, or for symptoms of heartburn and acid regurgitation suggesting GERD. Patients with upper gastrointestinal structural disease such as peptic ulcer or tumor, or systemic disease affecting esophageal motility were excluded from the study. Subjects' information was analyzed retrospectively based on their medical records.
MethodsIn each study patient, the gastroesophageal junction was first inspected using standard white light endoscopy alone without i-scan. And then, the i-scan mode was activated by pressing the appropriate button at the endoscope control head and the gastroesophageal junction was re-inspected. The examination with i-scan was performed under tone enhancement (TE) esophagus (e) mode, which were able to characterize the details of the gastroesophageal junction. All endoscopic examination was performed by two expert endoscopists with more than 1,000 cases of experience, who were highly familiar with Pentax i-scan.
Patients with mucosal breaks identified by endoscopy were classified as erosive esophagitis based on the Los Angeles (LA) classification (grade A, one or more mucosal breaks no longer than 5 mm, not bridging the tops of mucosal folds; grade B, one or more mucosal breaks longer than 5 mm not bridging the tops of mucosal folds; grade C, one or more mucosal breaks bridging the tops of mucosal folds involving <75% of the circumference are; grade D, one or more mucosal breaks bridging the tops of mucosal folds involving >75% of the circumference).12 Patients with no visible mucosal break on endoscopy were classified as non-erosive reflux disease (NERD). Of NERD patients, patients with subtle distal esophageal mucosal changes, such as blurring of Z-line (B), mucosal coarseness (C), hyperemic or purplish discoloration (D), erythema (E), ectopic gastric mucosal islet (I), and mixed type were classified as minimal change.13,14
Statistical analysisAll data are given as meanТБstandard deviation. Weighted kappa value and Я2 test were performed in order to assess the influence of the use of the i-scan compared with conventional endoscopy on the number of detected lesion. According to statistical conventions, the confidence level for this test was chosen as alpha=5%. The interobserver agreements for the i-scan findings between investigators were determined using kappa statistics. The strength of interobserver agreement was categorized according to the following definitions: 0.0-0.20, slight; 0.21-0.40, fair; 0.41-0.60, moderate; 0.61-0.80, good; 0.81-1.00, almost perfect. A p-value was considered significant if it was <0.05. The statistical software program (SAS, version 9.1; SAS Institute Inc., Cary, NC, USA) was used for all data analysis.
RESULTSA total of 156 patients with mean age of 57.5ТБ13.4 years were included in the study. The male was 85 patients, the female was 71 patients. A total of 96 (62%) patients had typical gastroesophageal reflux symptoms. One hundred three were inpatients, 53 were outpatients. One hundred sixteen patients had underlying medical diseases and 53 patients had medication history (Table 1).
With conventional endoscopy, 41 patients demonstrated mucosal breaks consistent with erosive esophagitis. According to the LA classification, 36 patients had grade A, 4 patients had grade B, and 1 patient had grade C esophagitis. And 94 patients were diagnosed as GERD with minimal change, including B (n=19), C (n=9), D (n=29), E (n=13), I (n=5), B+C (n=1), B+D (n=5), B+E (n=3), B+I (n=1), C+D (n=5), C+E (n=1), and D+E (n=3). After applying i-scan endoscopy, there was no improvement in detection of erosive esophagitis comparing conventional endoscopy (LA grade A, n=36; grade B, n=4; grade C, n=1). But, the number of minimal change was found to further increase from 94 to 109, including B (n=15), C (n=8), D (n=29), E (n=16), I (n=5), B+C (n=3), B+D (n=5), B+E (n=7), B+I (n=3), C+D (n=6), C+E (n=3), D+E (n=6), and E+I (n=3) (ЮК=0.84, p<0.0001) (Tables 2, 3, Figs. 1, 2). By using i-scan endoscopy, 15 patients who were diagnosed as normal by conventional endoscopy were additionally diagnosed as minimal change, and 14 patients who had single types of minimal change by conventional endoscopy were converted to mixed types of minimal change. So, 29 of 156 patients were upgraded after i-scan tone enhancement (TE) esophagus (e) mode, they were account for 19% (95% confidence interval [CI], 0.13 to 0.25) (Table 4). And interobserver agreement was very high, kappa value 0.84 (95% CI, 0.77 to 0.92) (Table 3).
Even restricted to 96 patients showing typical gastroesophageal reflux symptoms, the number of minimal change was found to further significantly increase from 60 to 69 after applying i-scan endoscopy. Nine patients were upgraded from initially normal in conventional endoscopy to minimal change after i-scan TE esophagus (e) mode, they were account for 9.4% (ЮК=0.80, p<0.0001) (Table 5).
DISCUSSIONPENTAX i-scan is a next generation image enhancement technology, which is also called virtual chromoendoscopy or endoscopic PhotoshopТЎ. Through the application of cutting edge computer-based enhancement filters, dynamic multiple modes reveal the hidden colors, vascularity, pit patterns, topography and architecture of possible problematic tissue, all at the mere touch of a button. This consists of three types of algorithms: surface enhancement (SE), contrast enhancement (CE), and tone enhancement (TE). SE enhances light-dark contrast by obtaining luminance intensity data for each pixel and applying an algorithm that allows detailed observation of a mucosal surface structure. CE digitally adds blue color in relatively dark areas, by obtaining luminance intensity data for each pixel and applying an algorithm that allows detailed observation of subtle irregularities around the surface. Lastly, tone enhancement makes color tone and structure more evident, which may be used to assess the necessity of more detailed test by means of dye spraying, magnified observation, or biopsy. TE is classified into 6 modes, which are TE pattern (p), TE vessel (v), TE barrett (b), TE esophagus (e), TE gastric (g), and TE colon (c). TE esophagus (e) mode was used for this study. This mode emphasizes relatively dark red color and white part of the mucosa in the image by digitally fading the red color, which makes it suitable for esophagus by emphasizing the vessel structure and the subtle mucosal color changes. For this reason, we can assume that 'erythema (E)' subtype would be commonly detected under TE esophagus (e) mode. In result, among additionally detected 29 patients, 15 patients were demonstrated erythema (E) subtype.
About 60% patients with GERD reveal no visible abnormality on conventional endoscopy, so it is difficult to diagnose GERD under the standard white light endoscopy.15 Various studies on evolved endoscopic techniques to improve the detection rate of GERD are published in the recent few years, one of which reported that NBI (Olympus Co., Tokyo, Japan) might be more effective for detecting NERD than conventional endoscopy. Sharma et al.10 demonstrated that reflux esophagitis group had significantly more intraepithelial papillary loops, dilatation, tortuosity, microerosion and vascularity of squamocolumnar junction than control group. In 2009, Hoffman et al.11 reported that chromoendoscopy with Lugol's solution in conjunction with HD endoscopy significantly improved the detection rate of erosive reflux disease, and i-scan endoscopy also was able to detect indistinct blood vessels and mucous structures clearly.
Despite the promising results of previous studies, there was no report to improve the detection rate of GERD especially where only minimal change is involved. Minimal change is a significant clinical problem as it is difficult to diagnose but nevertheless need adequate therapy. This study found that detection rate of minimal changes was significantly increased by 19% using i-scan. Furthermore, in NERD patient with typical gastroesophageal reflux symptoms, 9.6% patients was more precisely diagnosed by i-scan. There is a considerable discrepancy between endoscopic abilities to detect even minute lesions and their clinical relevance. But, i-scan endoscopy showed good interobserver agreement with kappa value of 0.84 (95% CI, 0.77 to 0.92).
In summary, i-scan endoscopy is simple and useful for diagnosis of minimal change with GERD. I-scan could be appealing for the endoscopist, because it is easy, safer, rapid and more accurate method for a detection of the minimal change with GERD. And it may also assist in a rational use of proton pump inhibitor therapy and facilitate the assessment of response to antireflux therapies. However, i-scan leads to visibility of new mucosal detail that is of little clinical relevance and has to be evaluated in further studies.
References1. DeVault KR, Castell DO. American College of Gastroenterology. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol 2005;100:190т200. 15654800.
2. Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology 1997;112:1448т1456. 9136821.
3. Kim HY, Kim N, Kim SM, et al. Clinical spectrum and risk factors of erosive and non-erosive GERD in health check-up subjects. Korean J Med 2006;71:491т500.
4. Youn YH, Kang YW, Ahn SH, Park SK. Prevalence alteration of reflux esophagitis in recent years. Korean J Gastrointest Endosc 2001;23:144т148.
5. Jeon SG, Sohn CI, Kim JE, et al. Prevalence of gastroesophageal reflux in routine check-up subjects. Korean J Med 2000;58:145т151.
6. Rhee PI. Evidence based guideline for diagnosis and treatment: diagnostic guideline for GERD. Korean J Neurogastroenterol Motil 2005;11:5т12.
7. Jones R. Gastro-oesophageal reflux disease in general practice. Scand J Gastroenterol Suppl 1995;211:35т38. 8545629.
8. Kim WJ, Cho JY, Jeong SW, et al. Comparison of autofluorescence imaging endoscopic findings with pathologic findings after endoscopic submucosal dissection of gastric neoplasms. Gut Liver 2008;2:186т192. 20485645.
9. Chaiteerakij R, Rerknimitr R, Kullavanijaya P. Role of digital chromoendoscopy in detecting minimal change esophageal reflux disease. World J Gastrointest Endosc 2010;2:121т129. 21160727.
10. Sharma P, Wani S, Bansal A, et al. A feasibility trial of narrow band imaging endoscopy in patients with gastroesophageal reflux disease. Gastroenterology 2007;133:454т464. 17681166.
11. Hoffman A, Basting N, Goetz M, et al. High-definition endoscopy with i-Scan and Lugol's solution for more precise detection of mucosal breaks in patients with reflux symptoms. Endoscopy 2009;41:107т112. 19214887.
12. Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 1999;45:172т180. 10403727.
13. Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol 2006;41:95т99. 16568367.
Fig.Т 1Endoscopic findings. Comparison between conventional and i-scan tone enhancement (TE) esophagus (e) method in erythema of minimal change. (A) In conventional endoscopic examination, normal mucosa of esophagus was shown. (B) Erythema of minimal change was detected in i-scan endoscopic examination. 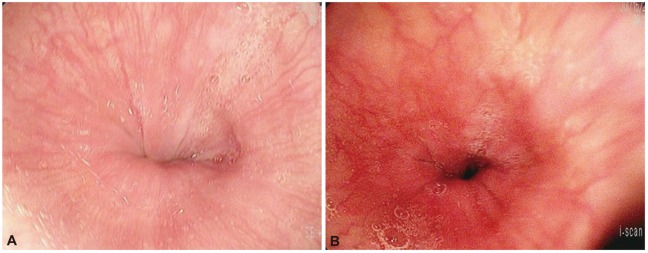
Fig.Т 2Endoscopic findings. Comparison between conventional and i-scan tone enhancement (TE) esophagus (e) method in mixed type of minimal change. (A) Only blurring of minimal change was shown in conventional endoscopic examination. (B) In i-scan endoscopic examination, ectopic gastric mucosal islet was more detected. 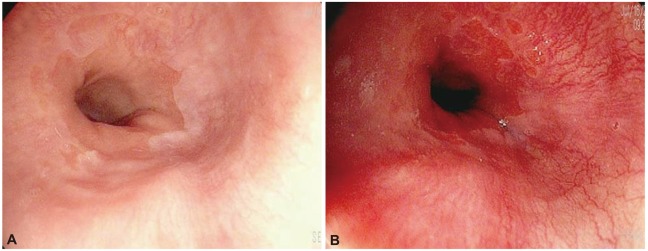
TableТ 1Patients Characteristics 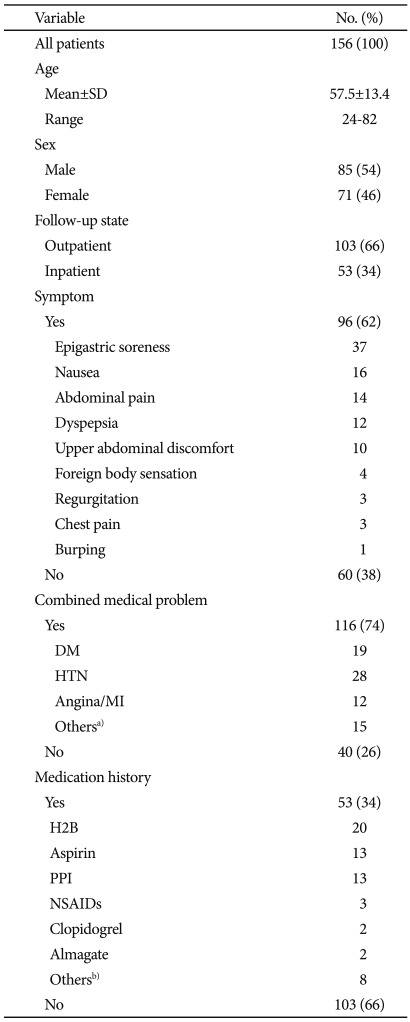 SD, standard deviation; DM, diabetes mellitus; HTN, hypertension; MI, myocardial infarction; H2B, H2 blocker; PPI, proton pump inhibitor; NSAIDs, nonsteroidal anti-inflammatory drugs. a)Colon cancer, liver cirrhosis, stroke, chronic renal failure; b)Teperone (SelbexТЎ), Benexate betadex (UlgutТЎ), Ecabet sodium (Gastrex ТЎ). |
|
|||||||||||||||||||||||||||||||||||||||||||
