Lee, Shin, Park, Kim, Jeon, Kim, Hong, Hong, Yang, Lee, Kim, Kim, Kim, Yang, Kim, and Multi-Society Task Force for Development of Guidelines for Colorectal Polyp Screening, Surveillance and Management: Korean Guideline for Colonoscopic Polypectomy
Abstract
There is indirect evidence to suggest that 80% of colorectal cancers (CRC) develop from adenomatous polyps and that, on average, it takes 10 years for a small polyp to transform into invasive CRC. In multiple cohort studies, colonoscopic polypectomy has been shown to significantly reduce the expected incidence of CRC by 76% to 90%. Colonoscopic polypectomy is performed frequently in primary outpatient clinics and secondary and tertiary medical centers in Korea. However, there are no evidence-based, procedural guidelines for the appropriate performance of this procedure, including the technical aspects. For the guideline presented here, PubMed, Medline, and Cochrane Library literature searches were performed. When little or no data from well-designed prospective trials were available, an emphasis was placed on the results from large series and reports from recognized experts. Thus, these guidelines for colonoscopic polypectomy are based on a critical review of the available data as well as expert consensus. Further controlled clinical studies are needed to clarify aspects of this statement, and revision may be necessary as new data become available. This guideline is intended to be an educational device to provide information that may assist endoscopists in providing care to patients. This guideline is not a rule and should not be construed as a legal standard of care or as encouraging, advocating, requiring, or discouraging any particular treatment. Clinical decisions for any particular case involve a complex analysis of the patient's condition and the available courses of action.
Keywords: Colonoscopy; Polypectomy; Guideline
INTRODUCTION
Need
Colorectal cancer (CRC) is the third most common cancer worldwide. According to the data 1 reported in 2008 by the Korean Collaborating Center for Cancer Registration, there were 22,623 cases of domestic CRC for men and women combined. Moreover, CRC represented 12.7% of all cancers and was the third most common type of newly diagnosed cancer. Among men, there were 13,536 cases of CRC, which made this the second most common cancer in men. In women, there were 9,087 cases of CRC, which made this the fourth most common cancer among women. Furthermore, the crude incidence rate of CRC is 45.8 cases per 100,000 individuals, and this incidence has been increasing steadily since the data analysis began in 1999. Eighty percent of CRCs originate as adenomatous polyps. Polyps are precancerous lesions and can develop into carcinomas over a period of 5 to 10 years through a process known as the "adenoma-carcinoma sequence." Therefore, if adenomatous polyps are detected and removed through aggressive screening, the mortality rate of CRC can be significantly reduced. Recently, as domestic awareness of CRC has increased, the number of colonoscopies performed has also increased rapidly. Polypectomy is commonly performed for polyps that are detected during colonoscopic examinations not only in secondary or tertiary medical centers but also in primary outpatient clinics. However, it is difficult to find domestic or international evidence-based guidelines regarding colonoscopic polypectomy procedures. Moreover, education and training for providers who perform colonoscopic polypectomy are available only at tertiary medical centers. Therefore, the development of an appropriate colonoscopic polypectomy guideline will assist numerous physicians who perform colonoscopic polypectomies within the Korean health care system. We hope that implementation of these guidelines will improve the utilization of limited medical resources and result in socioeconomic gain from the secondary prevention of CRC.
Purpose
This guideline has systematically incorporated the current domestic and foreign literature regarding 6 key questions related to colonoscopic polypectomy to establish an appropriate guideline to fit our country's current medical circumstances. Our objectives were to assist medical providers who perform colonoscopic polypectomy, to improve the quality of care, and to provide patients with appropriate and balanced information.
Limitations
The limited data on this subject presented an obstacle for compiling this domestic guideline for colonoscopic polypectomy. Most of the available data are from a limited number of North American and European studies, which evaluated epidemiologic characteristics that are not applicable to Korean patients. To overcome these limitations, we first created a draft treatment guideline based on the domestic and foreign research literature and then utilized a web-based survey to better understand the clinical practices of Korean endoscopists performing colonoscopic polypectomies. Based on this information, we summarized the opinions of domestic experts using the Delphi method.
However, because the Western researches that were used as the basis for half of the key questions were mostly comprised of observational studies rather than randomized controlled trials, the quality of the evidence for the recommendations was low. Therefore, the strength of the recommendations was evaluated mainly by collecting the opinions of domestic experts. Furthermore, even for those key questions where a meta-analysis of randomized controlled trials was available, the characteristics of the polyps were different, the number of patients included was relatively small considering the complication rates, and there were limitations due to differences in the statistical methods applied. Also, because this guideline cannot deal with every aspect of endoscopic treatment methods, a guideline with more diverse key questions should also be created. The 6 most relevant key questions for endoscopists regarding polypectomy are included in this guideline.
The participants and the process
The creation of the guideline began in June 2010 by forming the practice committee for the Colorectal Polyp Treatment Guidelines. This committee included academic experts from multiple societies: experts were recommended by the Korean Society of Gastroenterology, the Korean Society of Gastrointestinal Endoscopy, the Korean Association for the Study of Intestinal Diseases, and the Korean Society of Abdominal Radiology. The guidelines were divided into three topics: screening, surveillance, and treatment. Subsequently, a task force was assigned to each topic. No participant declared a conflict of interest.
Supply and practice
These guidelines will be published on the websites of the Korean Journal of Gastroenterology, the Korean Society of Gastrointestinal Endoscopy, the Korean Association for the Study of Intestinal Diseases, and the Korean Society of Abdominal Radiology. We also plan to prepare a summary consisting of important recommendations that would be supplied free of charge to front-line medical professionals.
METHODS
Selecting key questions
Because this guideline could not incorporate all issues relevant to colonoscopic polypectomy, the practice committee of the treatment task force selected 6 key questions.
Literature search
For the literature search, clinical trials, comparison studies, randomized controlled trials, meta-analyses, and treatment guidelines for colonoscopic polypectomy released in English between January 1, 2000 and September 2010, were searched using PubMed, Medline, and the Cochrane Library search engine. The key words that were used for the English search included the MeSH terminologies of hemorrhage, blood, endoscopy, mucous membrane, salicylic acid, aspirin, sodium chloride, epinephrine, vasoconstrictor agents, surgical instruments, and argon plasma. The general text words that were included in the search were acetylsalicylic acid, ASA, acetyl-salicylic acid, Migramax, Migpriv, Migrafin, Migravess, saline injections, epinephrine injections, adrenaline injections, post-polypectomy, endoscopic resection, endoscopic mucosal resection, diminutive polyp, small polyp, detachable snare, endoloop, endoclip, hemoclip, clip, and argon plasma. These additional terms were used because many relevant key words are not defined in the MeSH terminologies. The literature search results for each key question are included in the appendix. We excluded irrelevant pieces of literature by screening the titles and abstracts of the paper as well as the full text when necessary. We excluded 833 foreign papers and selected 52 papers for further analysis. Then, after a thorough examination of the full text of each paper, a standardized evidence table was created for the extraction of data relevant to the key questions.
Meta-analysis
A meta-analysis was performed only for key questions that could be informed by relevant randomized controlled trials. The odds ratios (OR) or the relative risk (RR) related to differences in treatment effects as well as the standard error and the 95% confidence interval (CI) were calculated. If the difference in the treatment effect was presented as a hazard ratio, it was included in the evidence table but excluded from the meta-analysis. Because the combined analysis included independent effects of individual risk factors from the unprocessed data of the included individual trials, the data were extracted with priority given to the individual trials. Therefore, the data extracted from individual trials that were included in the combined analysis were excluded from the meta-analysis. Studies were treated as observational studies, even when structured as randomized controlled trials, if the data were extracted from all cohorts participating in the research. Because of the heterogeneity in patient characteristics, research plans, follow-up periods, and purpose points among the trials selected for the meta-analysis, the random-effect model was used as the statistical model, and the inverse variance weighted estimation method was used for the effectiveness measurement to calculate pooled estimates. If the Cochrane Q-black test showed p-values of <0.1, statistical heterogeneity was considered to exist. The meta-analysis was performed using RevMan version 5.1 software (The Cochrane Collaboration, Oxford, UK).
Quality of evidence and strength of recommendations
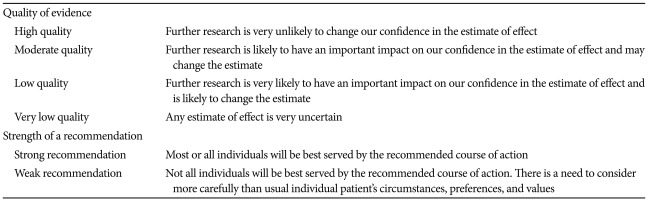
Recommendations are presented based on a systematic review of the selected literature and meta-analyses. The quality of evidence, indicating the degree to which each recommendation has scientific evidence, and the strength of the recommendations were determined following the methodology proposed by the Grading of Recommendations Assessment, Development and Evaluation Working Group ( Table 1). 2, 3
The quality of evidence was assessed to be "high" when evidence consisted of randomized controlled trials and "low" in cases where evidence included observational studies. However, in cases where studies used as evidence had limitations in the study design or execution, inconsistent results, indirect evidence, imprecise results or publication bias, the quality of evidence was adjusted downward. In cases of observational studies where large effects were observed, where reported effects might have been reduced due to confounding variables or where dose-response gradients existed, the quality of evidence was adjusted upward. The strength of each recommendation was assessed as "strong" or "weak" by considering the balance of desirable and undesirable consequences, the quality of the evidence, the confidence in the values and the references and the effective allocation of medical expenses and resources. That is, in cases where it was judged that following a specific recommendation would lead to significant health benefits or losses for most patients, the strength of the recommendation was classified as "strong". The strength of the recommendation was classified as "weak" in cases where it was judged that following the recommendation would lead to important benefits or loss in terms of the quality of the health of patients but where differences existed among patients, thus leading to the need to consider individual environments, preferences and values. 2, 3
GUIDELINES FOR COLONOSCOPIC POLYPECTOMY
Should aspirin be discontinued prior to the polypectomy due to the danger of post-polypectomy bleeding?
The use of aspirin should continue prior to the polypectomy for individuals with a high risk of developing thromboembolism. For those with a lower risk of developing thromboembolism, the aspririn treatment regimen should be determined according to the characteristics of the patients and their polyps. For those with no risk of developing thromboembolism, it is recommended that aspirin treatment be discontinued prior to polypectomy.
Quality of evidence: very low quality Strength of recommendation: weak recommendation Level of agreement: completely agree (7%), generally agree (75%), partially agree (18%), generally disagree (0%), completely disagree (0%)
When performing endoscopic procedures on patients taking anti-platelet agents, such as aspirin, the risk of bleeding due to the drug or the endoscopic procedure itself must be considered, and this risk should be compared to that of the development of thromboembolism following anti-platelet treatment discontinuation.
Aspirin causes the irreversible inactivation of cyclooxygenase (COX) in platelets and blocks the production of thromboxane, which is necessary for the agglutination reaction of platelets. The half-life of aspirin in the blood can be as short as 20 minutes, but its inhibition of COX is maintained for the lifespan of the platelet. Even after a single administration of low-dose aspirin, the inhibition of platelet agglutination is maintained for 7 to 10 days. A study that measured the bleeding times of 11 healthy individuals after taking aspirin or ticlopidine found that it took 3 days for the group who took aspirin, 5 days for the group who took ticlopidine, and 7 days for the group who took both aspirin and ticlopidine for the bleeding time to recover to that of baseline. 4
Colonoscopic polypectomy is considered to be a procedure with a high risk for bleeding, and these are commonly defined as procedures with a greater than 1% risk of clinically significant bleeding requiring transfusion, hospitalization, endoscopic hemostasis, or surgery.
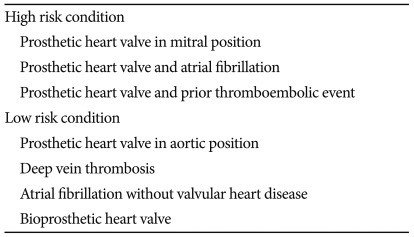
If antithrombotic treatment is discontinued prior to an endoscopic procedure, the risk of developing thromboembolism is related to the patient's underlying disease, and patients can be classified into either high- or low-risk groups ( Table 2). 5 For example, when antithrombotic treatment is withheld from patients with prosthetic valve replacements, the risk of serious thromboembolism is 4/100 patients per year; 6 however, if the patients receive an antiplatelet drug, such as aspirin, this risk is reduced to 2.2/100 patients per year. 7
To date, no randomized controlled trial has evaluated whether the risk of bleeding is increased if aspirin is taken prior to a colonoscopic polypectomy, although there have been 2 published prospective studies 8, 9 and 3 published retrospective studies 10- 12 ( Table 3). The primary outcomes of these studies differed, as they included immediate bleeding, delayed bleeding, as well as both immediate and delayed bleeding. Also, the definition of bleeding was not consistent; in some studies, bleeding was defined only as clinically significant bleeding requiring transfusion or endoscopic hemostasis, whereas others included imperceptible bleeding that did not require any special treatments. These inconsistencies make the level of available evidence difficult to determine. In a prospective cross-sectional study by Shiffman et al., 8 the occurrence of delayed bleeding was more pronounced in the group that took either aspirin or nonsteroidal anti-inflammatory drugs compared to the group that took no drugs (22/228 [9.6%] vs. 8/236 [3.4%]). However, most bleeding events consisted of imperceptible amounts of bleeding with low clinical importance (22/228 [8.8%] vs. 6/236 [2.5%]; p=0.006), and the rates of critical bleeding for both groups were below 1%. In two retrospective case-control studies and one retrospective cross-sectional study, aspirin was not shown to be a risk factor for bleeding (OR, 1.1 [95% CI, 0.5 to 2.2] to 1.4 [95% CI, 0.68 to 3.04]). Therefore, as aspirin consumption prior to polypectomy procedures does not appear to be a risk factor for clinically significant delayed bleeding, aspirin does not need to be discontinued before this procedure. In a prospective cross-sectional study by Kim et al., 9 there was no difference between patients with or without immediate bleeding regarding their intake history of aspirin (6/215 [2.8%] vs. 131/4,937 [2.5%]; p=0.9), and aspirin was not a risk factor for the development of immediate bleeding. However, the incidence of immediate bleeding that required endoscopic treatment was 0.2% for patients with polyps between 5 to 10 mm in size, 1.0% for those with polyps of 11 to 19 mm, and 1.5% for those with polyps greater than 20 mm. Because the incidence of immediate bleeding increased as the size of the polyp increased (OR, 2.38; 95% CI, 1.78 to 3.18; p<0.001), one could consider discontinuing aspirin for 5 to 7 days prior to the procedure in patients with polyps larger than 10 mm and a low risk of thromboembolism. Furthermore, we suggest that it is unnecessary for patients with no risk of thromboembolism to continue aspirin treatment prior to polypectomy. Recently, due to the increased incidence of cardiovascular disease, the rates of administration of combined therapies with aspirin and anticoagulant or antiplatelet agents, such as clopidogrel, ticlopidine, or warfarin, have increased. It is difficult to evaluate the effects of these drugs on the risk of post-polypectomy bleeding due to limited data, although it would be appropriate to compare the patient's risk of thromboembolism to the risk of post-polypectomy bleeding.
In conclusion, aspirin should be taken by patients with a high risk of developing thromboembolism. For patients with a low risk of thromboembolism, the discontinuation of aspirin for 5 to 7 days prior to the treatment should be considered if the polyp is greater than 10 mm in size. For patients with no risk of embolism, aspirin therapy should be discontinued, if possible. However, the physician who prescribed the aspirin treatment should be consulted before discontinuing the drug.
When diminutive polyps are found, is hot biopsy a recommended method for their complete and safe removal?
Considering its complete resection rate, safety, and histological quality, hot biopsy is not recommended method for removing diminutive polyps.
Quality of evidence: low quality Strength of recommendation: strong recommendation Agreement level: completely agree (42%), generally agree (37%), partially agree (11%), generally disagree (5%), completely disagree (5%)
As the use of high-definition endoscopes has increased, the detection of diminutive polyps (<5 mm) has also increased. According to recent reports, diminutive polyps are detected in more than half of screening tests, and more than half of these detected cases are diagnosed as adenomas. 13, 14
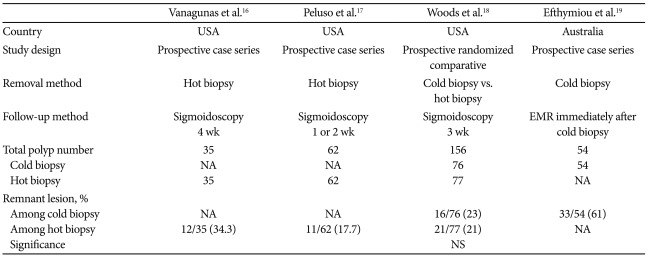
The natural history of diminutive polyps may be different from that of adenomas larger than 6 mm, and endoscopic diagnosis and removal techniques remain controversial. 15 Issues related to the removal of diminutive polyps can be summarized as follows: 1) whether the diminutive polyp is completely removed, 2) the safety of the diminutive polyp removal, and 3) the histological quality of the removed diminutive polyp. The methods that are currently used to remove diminutive polyps include cold biopsy, hot biopsy, and cold snaring. Only limited reports are available regarding the complete resection rate of diminutive polyps. From a randomized prospective comparison study that compared the complete resection rate of hot and cold biopsy, residual lesions were detected in 21% of patients administered hot biopsies and 29% of those given cold biopsies at the 3-week follow-up examination. There was no significant difference in the rate of residual disease in patients given either of these two methods. 16 In two studies involving hot biopsy only, residual lesions were detected in 13% to 17% of patients. 17, 18 Also, a recent prospective study found that when a lesion that had been completely removed by cold biopsy was re-excised with endoscopic submucosal resection, 61% of the lesion remained. 19 Because a 31% to 61% rate of residual disease exists for both hot biopsy and cold biopsy, these techniques are not recommended for complete resection ( Table 4). Furthermore, there are no existing reports detailing the complete removal rate of the cold snaring procedure. In addition, there have been no reported randomized comparison studies to date regarding the safety of diminutive polyp removal. From 2 observational studies that included 288 cold snaring cases and 907 hot biopsy cases, no observations were made regarding complications such as perforation or significant bleeding. 20, 21 However, in a retrospective study that compared 436 cases of cold biopsy with 1,525 cases of hot biopsy, significant bleeding (0.39%) occurred in only 6 hot biopsy cases. 22 In a retrospective survey study that examined 12,367 cases of hot biopsy, the rate of significant bleeding was 0.37%, and that of perforation was 0.05%. 23 Ultimately, because all of the reported complications were related to hot biopsy, this procedure is not recommended ( Table 5). In a randomized, prospective comparison study that evaluated the quality of the removed tissue, 39 (86.6%) out of 45 lesions from hot biopsies and 42 (97.6%) out of 43 lesions from cold biopsies satisfied histological quality measures, and this difference was statistically significant. Therefore, cold biopsy is the recommended method for optimal histological quality. 24
In conclusion, due to the low complete resection rate, safety, and histological quality of hot biopsy, this procedure is not recommended for the removal of diminutive polyps.
Does submucosal injection help to prevent post-polypectomy bleeding?
Submucosal injection during polypectomy helps to prevent early bleeding, but the preventative effect on delayed bleeding is not clear.
Quality of evidence: moderate quality Level of agreement: completely agree (13%), generally agree (53%), partially agree (16%), generally disagree (16%), completely disagree (2%)
For convenience and to reduce the danger of post-polypectomy bleeding, the submucosal injection of a variety of drugs has been developed. A mixture of normal saline and epinephrine is the most commonly used solution.
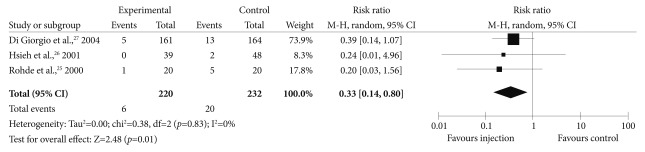
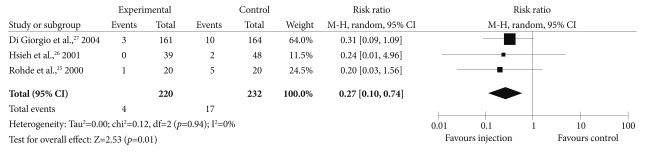
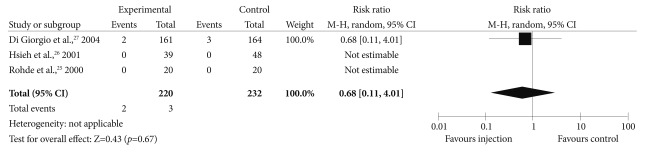
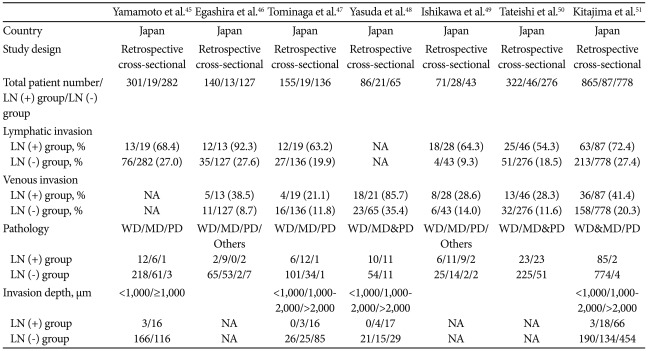
Our meta-analysis of 3 randomized prospective studies that compared post-polypectomy bleeding among patient groups that did or did not receive submucosal injection 25- 27 found that overall bleeding, including early bleeding (developing within 24 hours of the procedure) and delayed bleeding (developing more than 24 hours after the procedure), developed in 6 (2.7%) out of 220 patients in the group that received submucosal injection and in 20 (8.6%) of the 232 patients in the control group (RR, 0.33; 95% CI, 0.14 to 0.80; p<0.01) ( Fig. 1). A subgroup analysis showed that early bleeding was experienced by 4 (1.8%) out of 220 patients in the group the received the injection and by 17 (7.3%) out of the 232 patients in the control group (RR, 0.27; 95% CI, 0.10 to 0.74; p<0.01) ( Fig. 2). However, 2 (0.9%) out of 220 patients in the injection group developed delayed bleeding, as compared to 3 (1.3%) out of 232 patients in the control group, and the two groups did not show any significant differences (RR, 0.68; 95% CI, 0.11 to 4.01; p<0.67) ( Fig. 3). The submucosal injection of epinephrine is known to prevent bleeding due to its effects of vascoconstriction and mechanical compression of blood vessels. Because this effect only lasts for a few hours, submucosal injection is thought to be effective only for early bleeding. 26- 28
The concentration of epinephrine that was used for all 3 of the randomized prospective studies was 0.01%, but the injected volumes were between 1 and 10 mL and differed between studies. Due to differences in the size and the shape of polyps, we are unable to conclude that submucosal injection should be performed for the prevention of early bleeding in all patients with polyps. Also, because submucosal injection can be effective not only preventing bleeding, but also increasing the ease of polyp removal and reducing electrical tissue damage, decisions regarding its use should be left to the appropriate clinical judgment of the endoscopist.
In conclusion, submucosal injection during polypectomy can be helpful for preventing early bleeding, but it does not appear to have a clear effect on delayed bleeding.
Are prophylactic procedures prior to polypectomies for large (>1 cm), pedunculated polyps helpful in preventing post-polypectomy bleeding?
Prophylactic procedures (e.g., loop or clip placement) help to prevent early bleeding during the removal of large (>1 cm), pedunculated polyps, but the preventative effects of these procedures for delayed bleeding is not clear.
Quality of evidence: moderate quality Level of agreement: completely agree (0%), generally agree (42%), partially agree (47%), generally disagree (11%), completely disagree (0%)
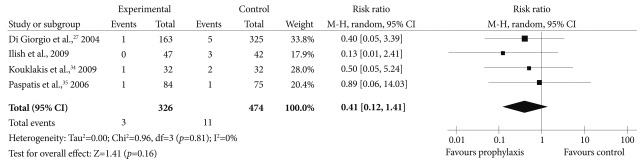
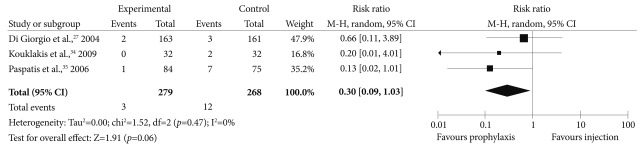
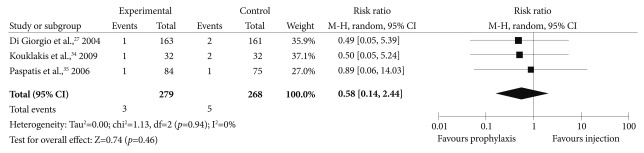
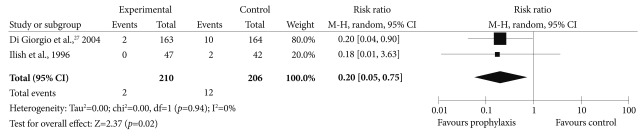
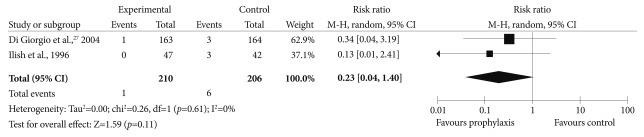
The known risk factors for post-polypectomy bleeding consist of patient-related factors, such as advanced age, medical comorbidities, and drug regimens, as well as polyp-related factors, such as shape, location, size, and grade of malignancy. 11, 29- 32 Because large, pedunculated polyps are likely to have an associated thick feeding vessel within the neck, the risk of post-polypectomy bleeding in these cases is high. 31 Endoscopic loop placement can mechanically compress the feeding vessel within the neck, and clips have also been used for the same purpose. 33 However, there have been few randomized prospective studies that have compared the preventive effects of these mechanical compression methods to the effects of submucosal injection, and the few reported studies are inconsistent in terms of the selection of the prophylactic method and the comparison methods. When a meta-analysis was performed on 4 prospective randomized studies that had researched the risk of post-polypectomy bleeding associated with large (>1 cm), pedunculated polyps treated with or without prophylactic procedures (loop or clip internment) prior to polyp removal, 27, 34- 36 early bleeding occurred in 3 (0.9%) out of the 326 patients who were given the prophylactic procedure, as compared to 24 (5.1%) out of the 474 patients in the comparison group (RR, 0.22; 95% CI, 0.08 to 0.62; p=0.004) ( Fig. 4). Delayed bleeding also developed in 3 (0.9%) of the 326 patients who were given the prophylactic procedure, as compared to 11 (2.3%) of the 474 patients in the comparison group (RR, 0.41; 95% CI, 0.12 to 1.41; p=0.16) ( Fig. 5). However, because the comparison group consisted of cases that had and had not received submucosal injection, different results were obtained in the subgroup analysis. When we separated these patients who had received submucosal injections, 34, 35 3 (1.1%) out of 279 patients who had received the prophylactic procedure were found to have developed early bleeding, whereas 12 (4.5%) out of 268 patients in the comparison group developed early bleeding. There was a decreased occurrence of early bleeding in the prophylactic group, but this difference was not statistically significant (RR, 0.0; 95% CI, 0.09 to 1.03; p=0.06) ( Fig. 6). Delayed bleeding developed in 3 (1.1%) of the patients who had undergone the prophylactic procedure and in 5 (1.9%) patients in the comparison group. This difference was not significant (RR, 0.58; 95% CI, 0.14 to 2.44; p=0.46) ( Fig. 7). Furthermore, early bleeding developed in 2 (0.95%) out of 210 patients who received snaring polypectomies without submucosal injection, 27, 36 whereas this occurred in 12 (5.8%) out of the 206 patients in the comparison group, and this difference was significant (RR, 0.20; 95% CI, 0.05 to 0.75; p=0.02) ( Fig. 8). However, delayed bleeding developed in 1 patient (0.48%) in the procedural group and in 6 patients (2.9%) in the comparing group, indicating that there was no significant preventive effect regarding delayed bleeding (RR, 0.23; 95% CI, 0.04 to 1.40; p=0.11) ( Fig. 9). In other words, for the removal of large pedunculated polyps, the use of loops, clips, or submucosal injections should be considered because all of these techniques have been shown to prevent early bleeding. Endoscopists should select which method to use by considering the characteristics of the polyp, such as its location and shape. In conclusion, prophylactic procedures that utilize loops or clips can prevent early bleeding during the removal of large (>1 cm) pedunculated polyps, although the preventive effect of these procedures on delayed bleeding is not clear.
Do prophylactic procedures for polypectomy-induced artificial ulcers decrease delayed bleeding?
Prophylactic procedures (e.g., argon plasma coagulation or clip placement) for polypectomy-induced artificial ulcers do not decrease the occurrence of delayed bleeding.
Qualify of evidence: moderate quality Level of agreement: completely agree (13%), generally agree (33%), partially agree (31%), generally disagree (23%), completely disagree (0%)
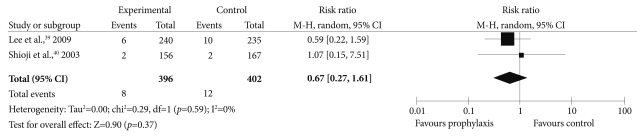
Bleeding is the most common complication of polypectomy. 37 Several recent reports have documented bleeding frequencies between 0.4% and 0.9%, and these are lower than they have been in the past. 9, 12 However, delayed bleeding causes significant clinical problems (e.g., the need for hospitalization, transfusion, repeated endoscopy or surgery). 38 To prevent delayed bleeding, many methods, such as submucosal injections and clip or loop placements, have been used clinically. However, prospective comparison studies are scarce, and there is currently no established guideline. Because the rate of delayed bleeding is typically below 1%, a large number of patients are required to demonstrate beneficial effects of a given prophylactic procedure. Furthermore, many factors related to bleeding, such as the polyp, patient, and procedural characteristics, are known to interact in a complex fashion. Prospective data regarding the use of prophylactic procedures for polypectomy-induced artificial ulcers, excluding procedures for pedunculated polyps, are very limited. A meta-analysis was performed on 2 prospective randomized studies that evaluated argon plasma coagulation and hemoclipping, 39, 40 and this report found that 8 (0.02%) out of 396 patients who received the prophylactic procedure developed delayed bleeding, as compared to 12 (0.03%) of the 402 patients in the control group, and this difference between groups was not statistically significant (RR, 0.67; 95% CI, 0.27 to 1.61; p=0.37) ( Fig. 10). Both of these studies were performed on patients with polyps between 0.5 and 2 cm in size. In the study that evaluated the use of argon plasma coagulation, all of the 803 polyps examined were non-peduculated. However, in the study that used clips, patients with pedunculated polyps (31 cases, 0.08%) were included in the total of 413 patients with polyps. And also in both studies, cases with immediate bleeding were excluded, which enables this result to be applied to cases of non-pedunculated polyps (<2 cm) without immediate bleeding.
In conclusion, prophylactic procedures using argon plasma or clips to prevent polypectomy-induced artificial ulcers do not decrease the occurrence of delayed bleeding.
When do we request additional colon resection to exclude the possibility of lymph node metastasis for cases where the histology is positive for adenocarcinoma with submucosal invasion and where complete excision (negative resection margin) has been obtained following the polypectomy?
If the histology indicates the presence of adenocarcinoma with submucosal invasion and complete excision (negative resection margin) was achieved following the polypectomy, the additional surgical excision should be considered because the danger of lymph node metastasis increases if there is lymphatic or venous invasion, poor differentiation, or deep submucosal invasion.
Quality of evidence: low quality Strength of recommendation: strong recommendation Agreement level: completely agree (26%), generally agree (55%), partially agree (19%), generally disagree (0%), completely disagree (0%)
Malignant polyps occur when the cancer cells penetrate through the muscularis mucosae and invade the submucosa. 41 These lesions differ from intramucosal cancer, for which a follow-up is performed without additional resection because the risk of lymph node metastasis is very low. If cancer cells invade the submucosa, which contains many lymphatic and blood vessels, the possibility of lymph node metastasis is relatively high. The treatment of this condition is therefore controversial. 42- 44
However, there have been few well-designed prospective studies regarding malignant polyps. Most studies are retrospective analyses of patients who underwent surgical excision for early CRC. When these retrospective studies were analyzed ( Table 6), 45- 51 67.5% (143/212) of the cases with lymph node metastases had lymphatic invasion of the excision tissue, which is significantly higher than the 24.7% (406/1,642) of patients in the group without lymph node metastases who demonstrated invasion (OR, 7.33; 95% CI, 5.29 to 10.15). Venous invasion was present in 39.3% (84/214) of patients with lymph node metastases, which is significantly higher than the 17.3% rate of venous invasion (246/1,425) in the group without lymph node metastases (OR, 3.24; 95% CI 2.34 to 4.48). Also, the well-differentiated (WD), moderately differentiated (MD), and poorly differentiated (PD) cases represented 59/146 (40.4%), 38/79 (48.1%), and 13/166 (7.8%) cases in the group with lymph node metastases, respectively, and 688/929 (74.1%), 162/588 (27.6%), and 12/1,366 (0.9%) cases in the group without lymph node metastases, respectively. The proportion of differentiated cancers in the group with lymph node metastasis was low (OR in WD, 0.23; 95% CI, 0.15 to 0.34; OR in MD, 2.39; 95% CI 1.43 to 3.98; OR in PD, 6.31; 95% CI, 2.52 to 15.79). The rates of submucosal invasion that was less than 1,000 ┬Ąm, between 1,000 and 2,000 ┬Ąm, or greater than 2,000 ┬Ąm were 19/146 (13.0%), 25/127 (19.7%), and 99/127 (78.0%) for the group with lymph node metastases, respectively, and 403/1,261 (32.0%), 174/979 (17.8%), and 539/979 (55.1%) for the group without lymph node metastases, respectively. Therefore, there was deeper submucosal invasion as the metastasis of the lymph nodes progressed (OR in <1,000 ┬Ąm, 0.31; 95% CI, 0.18 to 0.54; OR in 1,000 to 2,000 ┬Ąm, 1.10; 95% CI, 0.69 to 1.76; OR in >2,000 ┬Ąm, 3.39; 95% CI, 2.19 to 5.25). However, as the actual risk for lymph nodes metastasis in patients with high risk factors is approximately 10% to 15%, careful decision making is required prior to the recommendation for additional surgery. Furthermore, the effects of medical comorbidities and patient age should also be considered.
In conclusion, when histology indicates the presence of adenocarcinoma with submucosal invasion and when complete excision (negative resection margin) has been achieved following the polypectomy, additional surgical excision should be considered if there is lymphatic or venous invasion, if the polyp is PD, or if there is deep submucosal invasion.
SUMMARY
The use of aspirin should continue prior to the polypectomy for individuals with a high risk of developing thromboembolism. For those with a lower risk of developing thromboembolism, the aspririn treatment regimen should be determined according to the characteristics of the patients and their polyps. For those with no risk of developing thromboembolism, it is recommended that aspirin treatment be discontinued prior to polypectomy. Considering its complete resection rate, safety, and histological quality, hot biopsy is not recommended for removing diminutive polpys. Submucosal injection during polypectomy helps to prevent early bleeding, but the preventative effect on delayed bleeding is not clear. Prophylactic procedures (e.g., loop or clip placement) help to prevent early bleeding during the removal of large (>1 cm), pedunculated polyps, but the preventative effects of these procedures for delayed bleeding is not clear. Prophylactic procedures (e.g., argon plasma coagulation or clip placement) for polypectomy-induced artificial ulcers do not decrease the occurrence of delayed bleeding. If the histology indicates the presence of adenocarcinoma with submucosal invasion and complete excision (negative resection margin) was achieved following the polypectomy, the additional surgical excision should be considered because the danger of lymph node metastasis increases if there is lymphatic or venous invasion, poor differentiation, or deep submucosal invasion.
Acknowledgments
We express my deep appreciation for the unsparing advice and the help with the construction of this guideline provided by Professor Kim, Jin Oh from Soonchunhyang Medical School, Professor Park, Young Sook from Eulji Medical School, and Professor Kim, Eun Young from Daegu Catholic Medical School. We also give great thanks to the Korean Association of Internal Medicine and Korean Physicians Association for their agreement with final version of these guidelines.
This study was initiated with the support of the Korean Society of Gastroenterology, the Korean Society of Gastrointestinal Endoscopy, and the Korean Association for the Study of Intestinal Disease. This study was supported by a grant for the Korean Health Technology R&D Project with the Ministry for Health and Welfare of the Republic of Korea (A102065-23).
References
1. Korea Collaborating Center for Cancer Registration. National Cancer Registry Report in 2008. 2010. Seoul: Ministry of Health and Welfare.
4. Komatsu T, Tamai Y, Takami H, Yamagata K, Fukuda S, Munakata A. Study for determination of the optimal cessation period of therapy with anti-platelet agents prior to invasive endoscopic procedures. J Gastroenterol 2005;40:698ŌĆō707. 16082586.   5. ASGE Standards of Practice Committee. Anderson MA, Ben-Menachem T, et al. Management of antithrombotic agents for endoscopic procedures. Gastrointest Endosc 2009;70:1060ŌĆō1070. 19889407.   6. Cannegieter SC, Rosendaal FR, Bri├½t E. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation 1994;89:635ŌĆō641. 8313552.   7. Stein PD, Alpert JS, Copeland J, Dalen JE, Goldman S, Turpie AG. Antithrombotic therapy in patients with mechanical and biological prosthetic heart valves. Chest 1992;102(4 Suppl):445SŌĆō455S. 1395828.  8. Shiffman ML, Farrel MT, Yee YS. Risk of bleeding after endoscopic biopsy or polypectomy in patients taking aspirin or other NSAIDS. Gastrointest Endosc 1994;40:458ŌĆō462. 7926536.   9. Kim HS, Kim TI, Kim WH, et al. Risk factors for immediate postpolypectomy bleeding of the colon: a multicenter study. Am J Gastroenterol 2006;101:1333ŌĆō1341. 16771958.   10. Yousfi M, Gostout CJ, Baron TH, et al. Postpolypectomy lower gastrointestinal bleeding: potential role of aspirin. Am J Gastroenterol 2004;99:1785ŌĆō1789. 15330919.   11. Hui AJ, Wong RM, Ching JY, Hung LC, Chung SC, Sung JJ. Risk of colonoscopic polypectomy bleeding with anticoagulants and antiplatelet agents: analysis of 1657 cases. Gastrointest Endosc 2004;59:44ŌĆō48. 14722546.   12. Sawhney MS, Salfiti N, Nelson DB, Lederle FA, Bond JH. Risk factors for severe delayed postpolypectomy bleeding. Endoscopy 2008;40:115ŌĆō119. 18253906.   13. Rex DK, Helbig CC. High yields of small and flat adenomas with high-definition colonoscopes using either white light or narrow band imaging. Gastroenterology 2007;133:42ŌĆō47. 17631129.   15. Hewett DG, Rex DK. Colonoscopy and diminutive polyps: hot or cold biopsy or snare? Do I send to pathology? Clin Gastroenterol Hepatol 2011;9:102ŌĆō105. 20951831.   16. Vanagunas A, Jacob P, Vakil N. Adequacy of "hot biopsy" for the treatment of diminutive polyps: a prospective randomized trial. Am J Gastroenterol 1989;84:383ŌĆō385. 2648816.  17. Peluso F, Goldner F. Follow-up of hot biopsy forceps treatment of diminutive colonic polyps. Gastrointest Endosc 1991;37:604ŌĆō606. 1756918.   18. Woods A, Sanowski RA, Wadas DD, Manne RK, Friess SW. Eradication of diminutive polyps: a prospective evaluation of bipolar coagulation versus conventional biopsy removal. Gastrointest Endosc 1989;35:536ŌĆō540. 2689263.   20. Mann NS, Mann SK, Alam I. The safety of hot biopsy forceps in the removal of small colonic polyps. Digestion 1999;60:74ŌĆō76. 9892802.   21. Tappero G, Gaia E, De Giuli P, Martini S, Gubetta L, Emanuelli G. Cold snare excision of small colorectal polyps. Gastrointest Endosc 1992;38:310ŌĆō313. 1607081.   22. Tsai CJ, Lu DK. Small colorectal polyps: histopathology and clinical significance. Am J Gastroenterol 1995;90:988ŌĆō994. 7771436.  23. Wadas DD, Sanowski RA. Complications of the hot biopsy forceps technique. Gastrointest Endosc 1988;34:32ŌĆō37. 3258260.   24. M├Čnkem├╝ller KE, Fry LC, Jones BH, Wells C, Mikolaenko I, Eloubeidi M. Histological quality of polyps resected using the cold versus hot biopsy technique. Endoscopy 2004;36:432ŌĆō436. 15100953.   25. Rohde H, Guenther MW, Budde R, M├╝hlhofer H. Randomized trial of prophylactic epinephrine-saline injection before snare polypectomy to prevent bleeding. Endoscopy 2000;32:1004ŌĆō1005. 11147936.  26. Hsieh YH, Lin HJ, Tseng GY, et al. Is submucosal epinephrine injection necessary before polypectomy? A prospective, comparative study. Hepatogastroenterology 2001;48:1379ŌĆō1382. 11677969.  27. Di Giorgio P, De Luca L, Calcagno G, Rivellini G, Mandato M, De Luca B. Detachable snare versus epinephrine injection in the prevention of postpolypectomy bleeding: a randomized and controlled study. Endoscopy 2004;36:860ŌĆō863. 15452780.   29. Randall GM, Jensen DM, Hirabayashi K, Machicado GA. Controlled study of different sclerosing agents for coagulation of canine gut arteries. Gastroenterology 1989;96(5 Pt 1):1274ŌĆō1281. 2784774.   31. Dobrowolski S, Dobosz M, Babicki A, Glowacki J, Nalecz A. Blood supply of colorectal polyps correlates with risk of bleeding after colonoscopic polypectomy. Gastrointest Endosc 2006;63:1004ŌĆō1009. 16733117.   32. Watabe H, Yamaji Y, Okamoto M, et al. Risk assessment for delayed hemorrhagic complication of colonic polypectomy: polyp-related factors and patient-related factors. Gastrointest Endosc 2006;64:73ŌĆō78. 16813806.   33. Hachisu T. A new detachable snare for hemostasis in the removal of large polyps or other elevated lesions. Surg Endosc 1991;5:70ŌĆō74. 1948617.   34. Kouklakis G, Mpoumponaris A, Gatopoulou A, Efraimidou E, Manolas K, Lirantzopoulos N. Endoscopic resection of large pedunculated colonic polyps and risk of postpolypectomy bleeding with adrenaline injection versus endoloop and hemoclip: a prospective, randomized study. Surg Endosc 2009;23:2732ŌĆō2737. 19430833.   35. Paspatis GA, Paraskeva K, Theodoropoulou A, et al. A prospective, randomized comparison of adrenaline injection in combination with detachable snare versus adrenaline injection alone in the prevention of postpolypectomy bleeding in large colonic polyps. Am J Gastroenterol 2006;101:2805. 17026560.   36. Iishi H, Tatsuta M, Narahara H, Iseki K, Sakai N. Endoscopic resection of large pedunculated colorectal polyps using a detachable snare. Gastrointest Endosc 1996;44:594ŌĆō597. 8934168.   37. Nelson DB, McQuaid KR, Bond JH, Lieberman DA, Weiss DG, Johnston TK. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc 2002;55:307ŌĆō314. 11868001.   38. Waye JD, Lewis BS, Yessayan S. Colonoscopy: a prospective report of complications. J Clin Gastroenterol 1992;15:347ŌĆō351. 1294644.   39. Lee CK, Lee SH, Park JY, et al. Prophylactic argon plasma coagulation ablation does not decrease delayed postpolypectomy bleeding. Gastrointest Endosc 2009;70:353ŌĆō361. 19386307.   40. Shioji K, Suzuki Y, Kobayashi M, et al. Prophylactic clip application does not decrease delayed bleeding after colonoscopic polypectomy. Gastrointest Endosc 2003;57:691ŌĆō694. 12709699.   41. Cooper HS. Surgical pathology of endoscopically removed malignant polyps of the colon and rectum. Am J Surg Pathol 1983;7:613ŌĆō623. 6638257.   42. Coverlizza S, Risio M, Ferrari A, Fenoglio-Preiser CM, Rossini FP. Colorectal adenomas containing invasive carcinoma. Pathologic assessment of lymph node metastatic potential. Cancer 1989;64:1937ŌĆō1947. 2477139.   43. Hassan C, Zullo A, Risio M, Rossini FP, Morini S. Histologic risk factors and clinical outcome in colorectal malignant polyp: a pooled-data analysis. Dis Colon Rectum 2005;48:1588ŌĆō1596. 15937622.   44. Kyzer S, B├®gin LR, Gordon PH, Mitmaker B. The care of patients with colorectal polyps that contain invasive adenocarcinoma. Endoscopic polypectomy or colectomy? Cancer 1992;70:2044ŌĆō2050. 1394034.   45. Yamamoto S, Watanabe M, Hasegawa H, et al. The risk of lymph node metastasis in T1 colorectal carcinoma. Hepatogastroenterology 2004;51:998ŌĆō1000. 15239233.  47. Tominaga K, Nakanishi Y, Nimura S, Yoshimura K, Sakai Y, Shimoda T. Predictive histopathologic factors for lymph node metastasis in patients with nonpedunculated submucosal invasive colorectal carcinoma. Dis Colon Rectum 2005;48:92ŌĆō100. 15690664.   48. Yasuda K, Inomata M, Shiromizu A, Shiraishi N, Higashi H, Kitano S. Risk factors for occult lymph node metastasis of colorectal cancer invading the submucosa and indications for endoscopic mucosal resection. Dis Colon Rectum 2007;50:1370ŌĆō1376. 17661146.   49. Ishikawa Y, Akishima-Fukasawa Y, Ito K, et al. Histopathologic determinants of regional lymph node metastasis in early colorectal cancer. Cancer 2008;112:924ŌĆō933. 18181096.  
Fig.┬Ā1
Efficacy of prophylactic saline with epinephrine injection prior to snare polypectomy for the prevention of overall bleeding (early and late). CI, confidence interval. 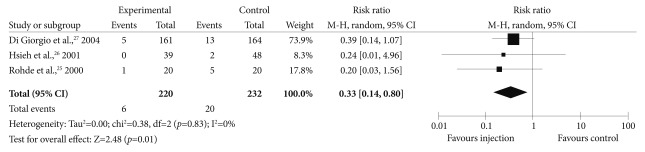
Fig.┬Ā2
Efficacy of prophylactic saline with epinephrine injection prior to snare polypectomy for the prevention of early bleeding. CI, confidence interval. 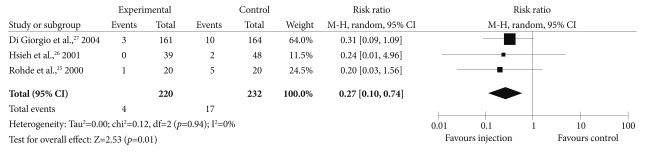
Fig.┬Ā3
Efficacy of prophylactic saline with epinephrine injection prior to snare polypectomy for the prevention of late bleeding. CI, confidence interval. 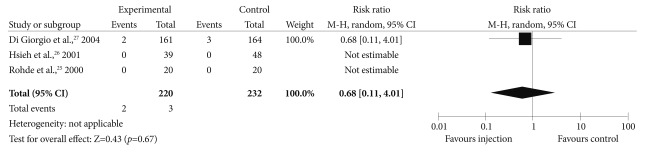
Fig.┬Ā4
Efficacy of the prophylactic method (endoloop or clip application) for the prevention of early bleeding in cases with large pedunculated polyps. CI, confidence interval. 
Fig.┬Ā5
Efficacy of the prophylactic method (endoloop or clip application) for the prevention of delayed bleeding in cases with large pedunculated polyps. CI, confidence interval. 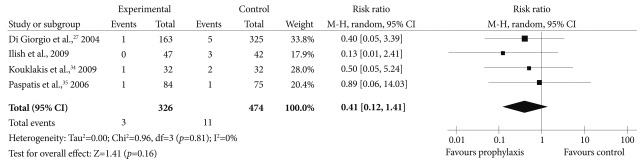
Fig.┬Ā6
Subgroup analysis of prophylactic methods versus submucosal injections for the prevention of early bleeding. CI, confidence interval. 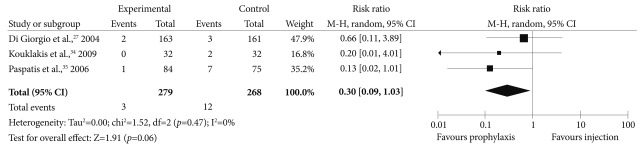
Fig.┬Ā7
Subgroup analysis of prophylactic methods versus submucosal injections for the prevention of delayed bleeding. CI, confidence interval. 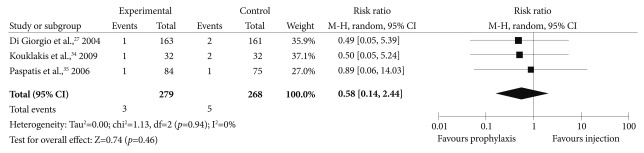
Fig.┬Ā8
Subgroup analysis of the prophylactic method versus no injection for the prevention of early bleeding. CI, confidence interval. 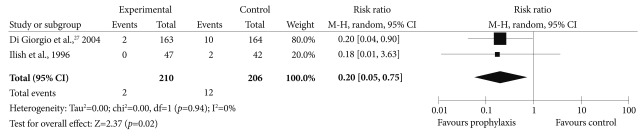
Fig.┬Ā9
Subgroup analysis of the prophylactic method versus no injection for the prevention of delayed bleeding. CI, confidence interval. 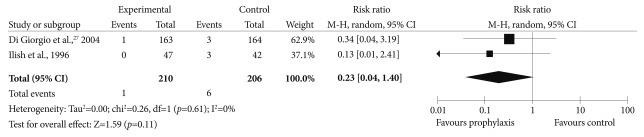
Fig.┬Ā10
Efficacy of the prophylactic method (argon plasma coagulation or clip application) for the prevention of delayed bleeding. CI, confidence interval. 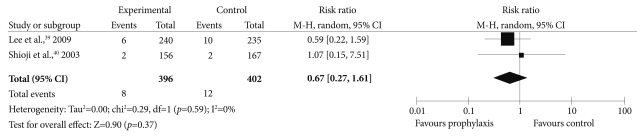
Table┬Ā1
Quality of Evidence and the Strength of the Recommendation 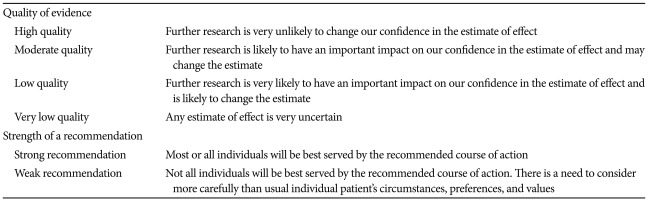
Table┬Ā2
Risk Stratification for Thromboembolism 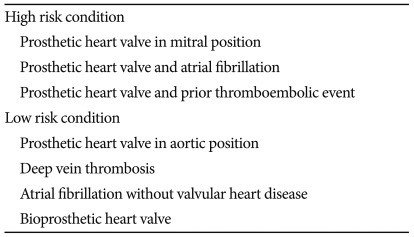
Table┬Ā3
Studies on Aspirin Use Prior to Colon Polypectomy 
Table┬Ā4
Residual Rate after the Removal of Diminutive Polyps 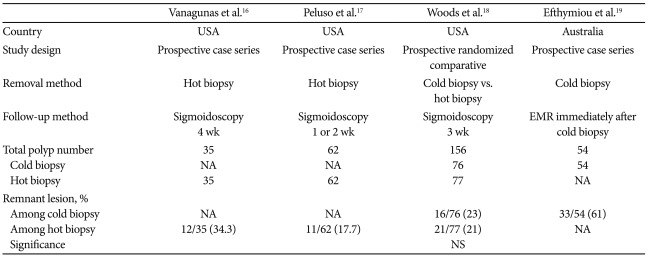
Table┬Ā5
Complication Rates after the Removal of Diminutive Polyps 
Table┬Ā6
Studies of Malignant Polyp Invading the Submucosa in Surgically Resected Colorectal Specimens 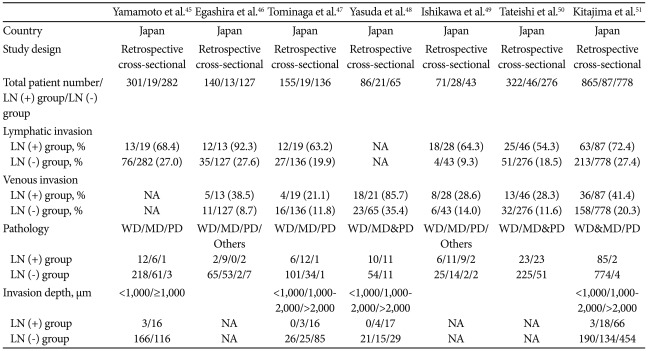
|
|