AbstractBackground/AimsAchalasia is a rare esophageal motility disorder. Recently, a novel endoscopic technique, peroral endoscopic myotomy (POEM), was introduced as an alternative treatment for achalasia. We report the results and short term outcomes of POEM for patients with achalasia.
MethodsPOEM was performed in 13 patients with achalasia. The procedure consisted of creating a submucosal tunnel followed by endoscopic myotomy of circular muscle bundles. The mucosal entry was closed by conventional hemostatic clips. A validated clinical symptom score (Eckardt score) and high resolution manometry were used to evaluate the outcomes.
ResultsBoth the clinical score of achalasia, as well as the resting lower esophageal sphincter (LES) pressure, were significantly reduced after POEM. Mean posttreatment Eckardt score was 0.4┬▒0.7, compared to 6.4┬▒1.9 prior to the treatment (p=0.001). The mean pretreatment and posttreatment LES pressure was 30.3 and 15.3 mm Hg, respectively (p=0.007). Following POEM, symptomatic relief from dysphagia without reflux symptoms was observed in all patients (13/13). No serious complications related to POEM were encountered.
INTRODUCTIONEsophageal achalasia is a motility disorder involving failure of the lower esophageal sphincter (LES) to relax in response to swallowing, resulting in aperistalsis of the esophageal body.1 Current treatments include muscle relaxants, endoscopic injection of botulinum toxin, pneumatic balloon dilation, and surgical myotomy.2 These first-line endoscopic treatments of achalasia are limited due to temporary relapse, and complications such as perforation and bleeding.3,4 In addition, surgical myotomy complications include gastroesophageal reflux (GER), stricture formation, and skin scarring.5,6 A potentially less invasive endoscopic method for division of the LES, using a needle-knife to cut the esophageal muscle from the luminal side, was described by Ortega et al.7 in 1980. Efforts to push the boundaries of flexible endoscopy and natural orifice transluminal endoscopic surgery led to the development of a novel treatment modality for achalasia. Pasricha et al.8 initially described the feasibility of an endoscopic submucosal esophageal myotomy in a pig model. The first report in humans was by Inoue et al.,9 who coined the term peroral endoscopic myotomy (POEM), and reported favorable results in 17 achalasia patients, in whom the submucosal route was used to access the muscular layer directly. Complications following POEM were reported by Ren et al.,10 but all complications were reported to be resolved through conservative treatment. We conducted a clinical study and described the technical steps and outcomes of POEM in patients, as a less invasive treatment option for the treatment of achalasia.
MATERIALS AND METHODSPatientsConsecutive patients diagnosed with primary achalasia by high resolution manometry (HRM) were enrolled (Fig. 1). The patients underwent POEM at Soonchunhyang University Hospital in Korea from November 2011 to December 2012. The inclusion criteria were symptomatic achalasia confirmed by contrast fluoroscopy, HRM and esophagoduodenoscopy. The exclusion criteria were active esophagitis, esophageal varices, pregnancy, esophageal stricture, esophageal malignancy, and other coagulopathy. Primary outcome was treatment success defined as symptom relief, based on an Eckardt score Ōēż3 after treatment.11 Secondary outcomes were procedure-related adverse events, pre- and post-POEM LES pressure and integrated relaxation pressure (IRP), myotomy length, and follow-up periods. The POEM procedure received approval from Institutional Review Board of Soonchunhyang University Hospital (approval number 2010-95, issued on September 29, 2010). Written informed consent was obtained from the patients.
MethodsPOEM was performed under general anesthesia. After general anesthesia, the patient was placed in the left lateral decubitus position. A forward-viewing endoscope with an outer diameter of 9.8 mm, which is routinely employed for upper gastrointestinal examination, was used with a transparent distal cap attachment. A Dual Knife (KD-650L; Olympus, Tokyo, Japan) was used to dissect the submucosal layer and to divide circular muscle bundles. Carbon dioxide gas was used for insufflation during the procedure, using a CO2 insufflator. Endoscopic air pressure was controlled by a CO2 insufflation machine (EndoCO2 PRO-500; MIRAEMEDICS, Seongnam, Korea) with a conventional insufflating tube, which maintained insufflation at a constant rate of 2 L per minute. This was used to prevent or decrease subcutaneous emphysema, which can occur when using O2 gas. For electrosurgery, a VIO 300D electrogenerator (ERBE, T├╝bingen, Germany) was used. Submucosal injection was performed at the level of the midesophagus, approximately 10 cm proximal to the gastroesophageal junction (GEJ). Approximately 10 mL of saline with 2.5 mL alginate was injected to lift the mucosa and expand the submucosal space, in order to facilitate safe mucosal incision. A 2-cm longitudinal mucosal incision was made on the mucosal surface to create a mucosal entry to the submucosal space using a Dual Knife (ENDO CUT: cut duration 2, cut interval 3, effect 3, Upmax 770 Vp). With the transparent cap attached on the endoscopic tip, we created a submucosal tunnel using the endoscopic submucosal dissection technique. A 2-cm longitudinal incision was performed on the mucosal surface for initiation of an entry point into the submucosal space (Fig. 2A). The tunnel was created ventrally to the 2 cm lower part of the GEJ by a Dual Knife (Fig. 2B). Initial measurement of the GEJ is helpful for optimal orientation. Submucosal tunneling was performed for approximately 12 cm. Upon tunnel completion, we dissected the esophageal circular muscle layer from the esophagus to GEJ at about 2 cm distal to the mucosal entry, approximately 8 cm above the GEJ, by using the Dual Knife and Hook Knife (KD-620LR; Olympus) (SWIFT coagulation: 40 W, effect 3, Upmax 1,210 Vp) (Fig. 2C). Endoscopic myotomy was performed for approximately 10 cm. The circular muscle bundle was cut using Dual Knife and Hook Knife, but the longitudinal muscle bundle was spared (Fig. 2D). The circular layer of muscle was cleanly incised in a distal-to-proximal fashion. Division of the sphincter muscle was continued from the proximal side towards the stomach until the endoscope passed through the narrow segment of the LES (Fig. 2E). When the tip of the endoscope reached the cardia, the submucosal space suddenly became wider. Additionally, changes in muscle structure from clear circular fibers to irregular fibers were also used to identify the cardia. Also, vessels became more irregular and dense at the cardia. After completion of the myotomy, smooth passage of an endoscope through the GEJ with minimal resistance was confirmed by conventional endoluminal endoscopy. After myotomy, the mucosal entry site was closed with seven hemostatic clips (Fig. 2F). At the end of the procedure, the endoscope was again inserted into the natural lumen down to the stomach, to confirm smooth passage through the GEJ. Following POEM the patient was fasted. A clear liquid diet was initiated after normalization of sequential chest X-rays, leukocyte count, and C-reactive protein levels. The mean time unto diet start was 4.4┬▒1.1 days following POEM. Three months after discharge all patients were scheduled to take follow-up symptom score questionnaires, HRM, and esophagography.
Statistical analysisWe used descriptive statistics to report the effectiveness of POEM in patients with achalasia. Mean values between baseline and follow-up were compared using Student's t-test for paired samples. A p-value of less than 0.05 was considered to be statistically significant. Data were analyzed using commercially available statistical software packages SPSS version 17.0 (SPSS Inc., Chicago, IL, USA).
RESULTSDuring the study period, POEM was successfully completed in 13 patients with symptomatic achalasia. Table 1 shows the baseline characteristics of the patients. The mean age┬▒standard deviation) was 39.6┬▒15.8 years and the male: female ratio was 3:10. Six patients had received prior treatment for achalasia; balloon dilatation (n=3), botulinum toxin injection (n=2), and laparoscopic Heller myotomy (n=1). On baseline, 11 patients were type 1 achalasia and other patients were type 2 (including 12 nonsigmoid and one sigmoid cases). Endoscopic findings included dilatation of the middle esophagus, and retention of large amounts of foods and water. Resistance of endoscopic passage in GEJ was observed secondary to excessive contraction (Fig. 3A). In the barium swallow study, stenosis was observed in the lower esophagus due to severe contraction of the LES. Additionally, the middle esophagus was dilated in a "bird beak" narrowing appearance, showing retention of barium (Fig. 3B). Barium was excreted slowly into the stomach after 30 minutes. Observed via endoscopic ultrasonography, the inner circular muscle of the lower esophagus demonstrated hypertrophy, with the mean thickest muscle layer measured at 4.0┬▒1.3 mm (normal range, <3). HRM was performed before and after the procedure. According to the manufacturer's data, the normal range for LES pressure with this device is 13 to 43 mm Hg.
The detailed POEM procedure is shown in Fig. 2 and the overall outcome is shown in Table 2. Median submucosal tunnel length was 10.7 cm and median total myotomy length was 8.5 cm (esophageal, 7.0┬▒2.0 cm; gastric, 1.6┬▒0.5 cm). Symptom score follow-up was available for all study patients. Treatment success, as defined by a post-POEM Eckardt score Ōēż3,11 was achieved in 100% of cases. Mean posttreatment Eckardt score was 0.4┬▒0.7, compared to 6.4┬▒1.9 prior to the treatment (p=0.001). Baseline manometry data was available for all study patients. However, manometry follow-up was available in 11/13 cases. The mean LES pressure was 30.3 mm Hg prior to the treatment and 15.3 mm Hg after the treatment (p=0.007). The mean pre- and post-IRP was 26.0 and 10.8 mm Hg, respectively (p=0.008). Two patients refused to undergo follow-up manometry, due to discomfort related to the manometry procedure. A water-soluble esophagogram was obtained after POEM, and there were no incidences of esophageal leakage. Free flow of contrast into the stomach with no retention of barium in the esophagus (Fig. 4A) was observed in all patients. Posttreatment manometry was obtained, where relaxation and passage of LES was seen (Fig. 4B). There were no serious complications related to POEM. During follow-up, no specific complications, problems, or symptoms were encountered.
DISCUSSIONAchalasia is a motility disorder of the esophagus, with an estimated prevalence of 0.5 to 1.0/100,000 population per year.12 It is characterized by dysphagia of solids and liquids. Other features include regurgitation of undigested food, chest pain, weight loss, and respiratory symptoms.13,14 Manometry identifies early disease before esophageal dilatation and food retention are seen. Therefore, it is the most sensitive diagnostic test of esophageal motility, and distinguishes three subtypes of achalasia.15 Findings on esophageal manometry of achalasia include incomplete relaxation of LES on swallowing, absence of esophageal peristalsis, and elevated basal LES pressures.
No known way of preventing or reversing achalasia exists. Therapy is directed at reducing LES pressure to allow gravity and esophageal pressurization to promote esophageal emptying. Peristalsis rarely, if ever, returns. LES pressure can be reduced by pharmacological therapy (calcium channel blockers), forceful dilatation, or surgical myotomy. However, pharmacological therapy provides short-term clinical response with common side effects.16 Botulinum toxin, injected into the LES under endoscopic guidance, inhibits acetylcholine release from nerve endings and improves dysphagia in ~66% of cases, for at least 6 months.17 However, the response is temporary.3 The only durable therapies for achalasia are pneumatic dilatation and Heller myotomy.18,19 Pneumatic dilatation is an endoscopic technique, using a noncompliant, cylindrical balloon dilator, positioned across the LES, and inflated to a diameter of 3 to 4 cm. Pneumatic dilatation is widely performed because of its relative noninvasiveness, but it has a lower success rate and often causes submucosal microhemorrhages and perforation.4 The most common surgical procedure for achalasia is laparoscopic Heller myotomy, usually performed in conjunction with an antireflux procedure (partial fundoplication).19 The severe complication of both procedures is perforation, with the reported incidence of 1.6% after pneumatic dilatation, versus 0.7% after laparoscopic myotomy.20 Forty-eight percent of patients who had myotomy without a fundoplication suffered from pathologic GER; therefore, myotomy should always be combined with an antireflux procedure.21
POEM is as effective as the current alternative surgery, but requires further evaluation by objective testing. Inoue et al.9 reported a 70% drop in the LES pressure in patients with non-sigmoid esophagus, and a 50% drop in patients with sigmoid esophagus.9 POEM is a permanent procedure, as compared with botulinum toxin injection, so the relapse rate is low. Additionally, this procedure has a lower unexpected perforation risk than that of pneumatic dilatation. POEM resembles Heller's myotomy, but since it is performed endoscopically, selective myotomy over a long distance is possible, vagus nerve injury is prevented, and the operation field is broader than with Heller's myotomy. Additionally, it is less invasive and leaves no scars on the skin.
Our study was performed successfully for the first time in humans in Korea. Our results showed that POEM resulted in a significant decrease in the achalasia symptom score. Both mean LES pressure and IRP were significantly improved in all patients. However, POEM is still in its early stages, and data regarding the long-term results are limited. Therefore, POEM needs long-term follow-up as compared with other treatments. After 2 years of follow-up, laparoscopic Heller's myotomy, as compared with pneumatic dilatation, was not associated with superior rates of therapeutic success.22 Despite laparoscopic Heller's myotomy being an invasive therapy, the treatment follow-up data for both were similar. Thus, POEM follow-up data will be expected. POEM is also indicated in operable young people and refractory achalasia patients who failed to respond to established treatments.
Our study has several limitations. First is the small sample size, with only 13 enrolled patients. Further large scale studies or multicenter studies are required to demonstrate effectiveness of POEM for achalasia patients. However, given the low prevalence of achalasia, multicenter studies in specialized center seems more appealing. Another limitation is that manometry follow-up was not available in all patients. Two patients refused to undergo follow-up manometry, due to discomfort related to the manometry procedure. Finally, our study only included one patient with sigmoid type achalasia. Nevertheless, this study has significance as the first human study in Korea demonstrating the effectiveness of POEM.
In conclusion, POEM seems to be a very effective approach to treat esophageal achalasia. POEM is a less invasive endoscopic procedure for esophageal achalasia, and shows good short-term results without serious complications. Future studies should focus on larger-scale multicenter studies, and long-term results of POEM.
References1. Achem SR, Crittenden J, Kolts B, Burton L. Long-term clinical and manometric follow-up of patients with nonspecific esophageal motor disorders. Am J Gastroenterol 1992;87:825ŌĆō830. 1615935.
2. Pehlivanov N, Pasricha PJ. Achalasia: botox, dilatation or laparoscopic surgery in 2006. Neurogastroenterol Motil 2006;18:799ŌĆō804. 16918758.
3. Muehldorfer SM, Schneider TH, Hochberger J, Martus P, Hahn EG, Ell C. Esophageal achalasia: intrasphincteric injection of botulinum toxin A versus balloon dilation. Endoscopy 1999;31:517ŌĆō521. 10533734.
4. Karamanolis G, Sgouros S, Karatzias G, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol 2005;100:270ŌĆō274. 15667481.
5. Kilic A, Schuchert MJ, Pennathur A, Gilbert S, Landreneau RJ, Luketich JD. Long-term outcomes of laparoscopic Heller myotomy for achalasia. Surgery 2009;146:826ŌĆō831. 19789044.
6. Eldaif SM, Mutrie CJ, Rutledge WC, et al. The risk of esophageal resection after esophagomyotomy for achalasia. Ann Thorac Surg 2009;87:1558ŌĆō1562. 19379905.
7. Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc 1980;26:8ŌĆō10. 7358270.
8. Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 2007;39:761ŌĆō764. 17703382.
9. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010;42:265ŌĆō271. 20354937.
10. Ren Z, Zhong Y, Zhou P, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc 2012;26:3267ŌĆō3272. 22609984.
11. von Renteln D, Inoue H, Minami H, et al. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol 2012;107:411ŌĆō417. 22068665.
12. Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil 2010;22:e256ŌĆōe261. 20465592.
13. Hirano I, Tatum RP, Shi G, Sang Q, Joehl RJ, Kahrilas PJ. Manometric heterogeneity in patients with idiopathic achalasia. Gastroenterology 2001;120:789ŌĆō798. 11231931.
15. Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2008;135:1526ŌĆō1533. 18722376.
16. Francis DL, Katzka DA. Achalasia: update on the disease and its treatment. Gastroenterology 2010;139:369ŌĆō374. 20600038.
17. Annese V, Bassotti G, Coccia G, et al. GISMAD Achalasia Study Group. A multicentre randomised study of intrasphincteric botulinum toxin in patients with oesophageal achalasia. Gut 2000;46:597ŌĆō600. 10764700.
18. West RL, Hirsch DP, Bartelsman JF, et al. Long term results of pneumatic dilation in achalasia followed for more than 5 years. Am J Gastroenterol 2002;97:1346ŌĆō1351. 12094848.
19. Hunter JG, Trus TL, Branum GD, Waring JP. Laparoscopic Heller myotomy and fundoplication for achalasia. Ann Surg 1997;225:655ŌĆō664. 9230806.
20. Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 2009;249:45ŌĆō57. 19106675.
Fig.┬Ā1Esophageal high resolution manometry. Lower esophageal sphincter (LES) pressure was increased. If swallowing was induced, relaxation of LES was not seen and peristalsis was absent. Type I achalasia exhibited minimal pressurization of the esophageal body. 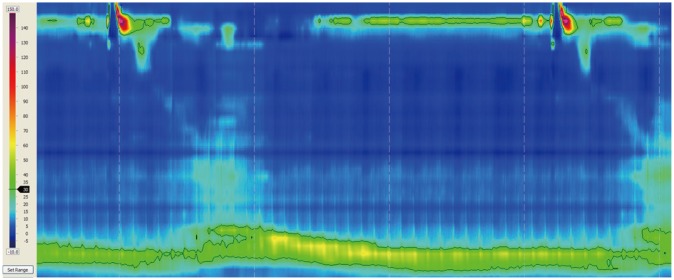
Fig.┬Ā2(A) A 2-cm longitudinal incision was performed on the mucosal surface for initiation of an entry point into the submucosal space. (B) In the submucosal space, an endoscopic tunnel is created primarily by careful electrocoagulation using a Dual Knife. (C) Endoscopic myotomy was begun 2 cm distal to the mucosal entry using Dual Knife and Hook Knife. (D) After dissection of the circular muscle bundles, outer longitudinal muscle bundles were endoscopically identified. (E) Completion of endoscopic myotomy. Circular muscle bundles were dissected and the 10-cm myotomy was completed. (F) After complete myotomy, the mucosal entry site is closed using standard endoscopic clips. 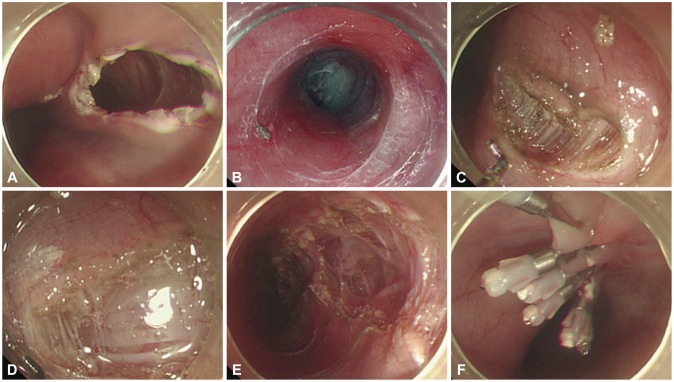
Fig.┬Ā3(A) Endoscopic findings of achalasia. Note dilatation in the middle esophagus and retention of water in the lower esophagus. (B) Esophagogram. Note achalasia with esophageal dilatation with an air-fluid level, tapering at the esophagogastric junction, providing a "bird beak" narrowing appearance. 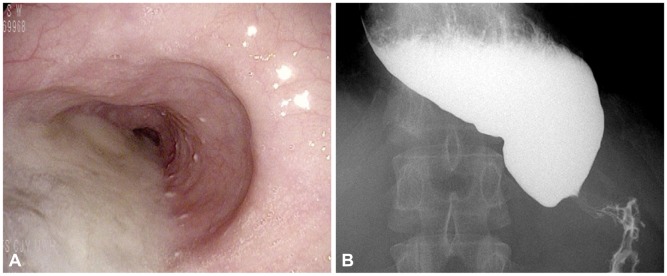
Fig.┬Ā4(A) Esophagogram after peroral endoscopic myotomy (POEM): barium passed and was excreted quickly through lower esophageal sphincter (LES). (B) High resolution manometry after POEM (3 months later): LES pressure was decreased, and if swallowing was induced, relaxation and passage of LES was seen. 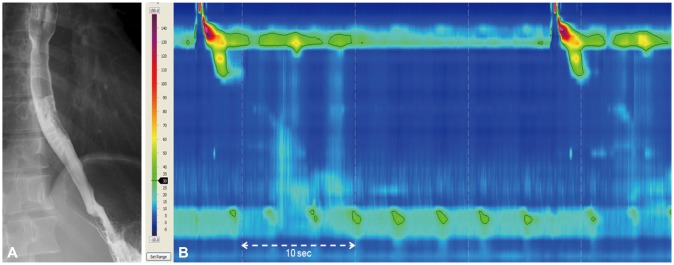
|
|
||||||||||||||||||||||||||||||||||||
