INTRODUCTION
Fibrovascular polyp (FVP) is a very rare, intraluminal, submucosal, pedunculated tumor-like lesion which is composed of loose or dense fibrous tissue, adipose tissue, and vascular structures and is covered by normal squamous epithelium.1 In the past, FVP was referred to as lipoma, fibroma, fibrolipoma, fibromyxoma, or fibroepithelial polyp, according to histologic components.2 It generally occurs in middle-aged or elderly males, although some cases have occurred in children, infants, and women.2,3 It occurs mostly in the upper cervical esophagus, hypopharynx, and occasionally in the oropharynx.4,5 However, a report of FVP arising from stomach has not been published. To our knowledge, this case is the first English-written report of a FVP presenting with melena, found under endoscopy and later excised surgically.
CASE REPORT
A 36-year-old male patient visited the emergency room with the chief complaint of melena which began 10 days ago. The patient did not have any medical history, family history, or social history. On his initial visit, his body temperature was 36.5т, pulse rate was 82 beats per minute, respiratory rate was 18 breaths per minute, and blood pressure was 110/80 mm Hg.
In a physical examination, his conjunctiva was pale, and there was tenderness in his epigastric region with normal bowel sound and no palpable abdominal mass. In a laboratory test, hemoglobin level was 6.7 g/dL and the other findings were within normal limits.
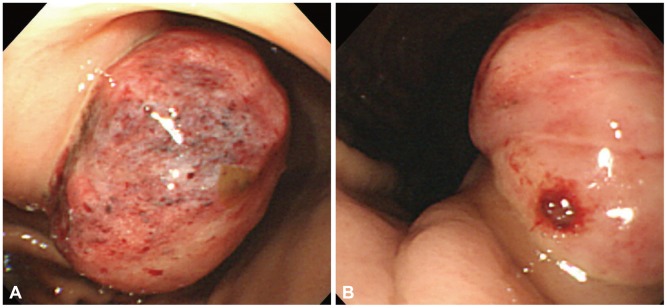
Emergency upper gastrointestinal endoscopy was performed and a pedunculated polyp about 45 mm in diameter, accompanied with ulcer at the base of the polyp, was observed in the gastric antrum. Prominent vascularity with hemorrhagic ulceration on the surface and easy bleeding to light touch with forceps was noted at the proximal side of the lesion, and irregular friable surface with one exposed vessel was noted at the distal side of the lesion (Fig. 1). This was presumed due to thinning or disappearance of swollen gastric mucosa by hemorrhagic, ulcerative change of large submucosal tumor with hypervascular nature. The hemorrhage was controlled with injection of epinephrine followed by thermocoagulation, and intravenous proton pump inhibitor (PPI) and transfusion were started.
In his abdominal computed tomography (CT), about 3.5У5 cm-sized pedunculated mass was located in the lesser curvature of the stomach with partial mucosal wall disruption (Fig. 2). The patient was admitted and observed whether melena persisted. His hemoglobin level, which increased up to the normal value after transfusion, later decreased to 9.7 g/dL and a laparoscopic wedge resection was scheduled for uncontrolled bleeding after failing of endoscopic and supportive managements. Under a laparoscopic exploration, the polyp was located in the lesser curvature of the stomach. The right gastric artery was cut, and wedge resection was performed with a boundary of 4 cm from the margin of the polyp. The surgical specimen was a protruding 4У4У3 cm polyp accompanied with ulcer, and its cross section showed a mucosal lesion in the mixture of gray and yellow colors.
In microscopic findings, overlying gastric mucosa was nearly disappeared and the surface was replaced by exposed submucosal tissue with ulceration and inflammation. The submucosal tissue was composed of many irregular blood vessels, loose connective tissues, and adipose cells that are consistent with FVP (Fig. 3). After the surgery, the patient has been followed up on an outpatient basis until now for about 1 year without any evidence of gastrointestinal bleeding and antral stricture on endoscopy.
DISCUSSION
About 25% of esophageal cases could be missed because of its normal, intact squamous epithelium lining the polyp, especially when the examiner rapidly withdraws the endoscope. Compared to esophageal lesions, gastric submucosal lesions, such as a large pedunculated type like the one in our case, could be clearly seen on endoscopic exam, regardless of the location.2,6 Similarly, in this case, gastrointestinal bleeding was reported in the case of esophageal ulcerated FVP.2 The symptoms of esophageal FVP usually develop when polyp reaches a large size enough to cause dysphagia, substernal discomfort, sensation of mass, and even asphyxiation.1,2,7 In this case, acute blood loss leading to anemia was caused by the ulceration with increased vascularity of large gastric FVP, which was managed surgically due to the risk of constant bleeding.3
FVP is a very rare, slowly growing, malignant transformation, but malignant change has been reported in esophageal polyps.2,3 It is usually presented as a solitary mass, but a case of two synchronous FVP of the hypopharynx has been reported.3
Diagnosis of FVP can be made by a combination of clinical history and various investigations including barium swallow examination, endoscopy, endoscopic ultrasound, CT, and magnetic resonance imaging (MRI).2,8 The differential diagnoses of benign esophageal polyp include leiomyoma, squamous papilloma, and hemangioma.9
The histology of the FVP consists of a mixture of fibrous tissue, adipose tissue, and vascular structures. The proportions of these three components of FVP may vary depending on the lesion and area within the same lesion.10 Various terminologies of FVP, such as fibroepithelial polyp, fibrolipoma, fibromyxoma, lipoma, and fibroma, are all now collectively classified as FVP by World Health Organisation.2
The treatment of choice for FVP is surgical resection. Small polyps less than 2 cm in diameter with a thin pedicle can be removed by endoscopic ligation and electrocoagulation, but care must be taken to ensure that the prominent vessels in the stalk are completely ligated and coagulated.1,2,8 EUS can be a useful adjunct as it provides information on the origin of the stalk and vascularity of the polyp.2 CT and MRI can demonstrate the predominant adipose tissue contents, with respect to fibrovascular tissue, and in such a case, endoscopic treatment may be preferred, especially in older patients with multiple comorbidities.3 A polyp of a diameter of less than 5 cm and no lymph node involvement on abdominal imaging like the one in this case could be an indication for laparoscopic wedge resection, which was performed in our patient.11,12 Although metastasis has never been reported from the polyp, recurrence of resected FVP of the esophagus has been reported, most probably due to incomplete excision of the stalk and residual tissue around the pedicle's base.2,7
In summary, we reported the first case of large gastric FVP presenting with melena. Although recurrent bleeding occurred after endoscopic coagulation and intensive intravenous PPI treatment, the bleeding could be controlled successfully with laparoscopic wedge resection.