INTRODUCTION
Annually, there are approximately 1,000 newly diagnosed cases of pharyngeal cancer in Korea. Hypopharyngeal cancer comprises one-third of these cases and is usually diagnosed at an advanced stage, leading to extensive surgical resection, post-surgical loss of function of swallowing and/or speaking, and poor prognosis.1-3 With the initiation of the National Cancer Screening program, routine diagnostic endoscopy is increasing in Korea. However, the oropharyx is commonly overlooked in many cases due to patient discomfort or under-appreciation of this anatomical region by endoscopists.4 Current developments in high definition endoscopy and novel imaging endoscopy, such as narrow band imaging (NBI), magnifying endoscopy and the i-scan, have enabled gastrointestinal (GI) endoscopists to detect hypopharyngeal carcinoma at an early stage.5,6 Patients with such early lesions can be treated with endoscopic resection. There have been only a few reports of successful endoscopic resection for hypopharyngeal cancer, almost exclusively from Japan.1-5
CASE REPORT
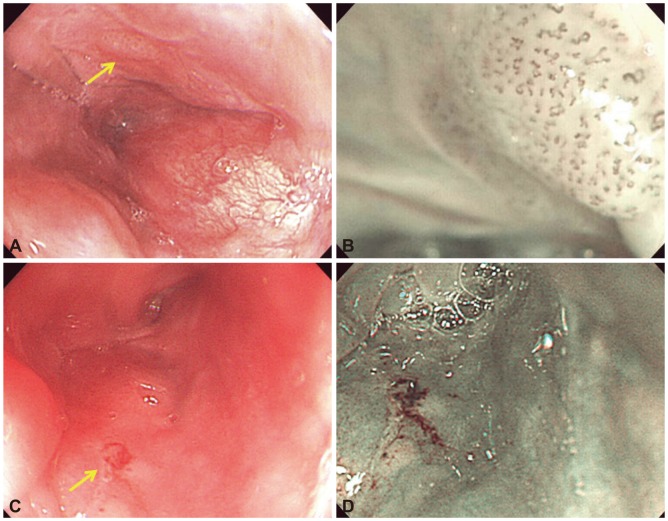
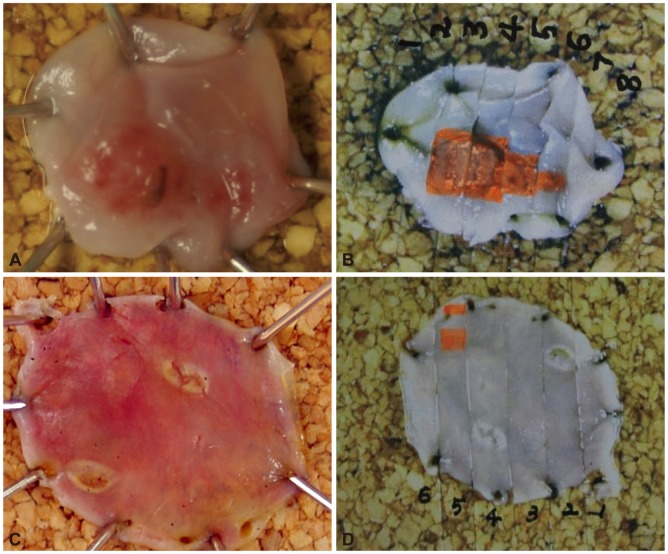
A 55-year-old Asian male was referred to our department for the management of suspicious hypopharyngeal cancer diagnosed by endoscopic biopsy at a primary medical clinic. The patient was not present with symptoms related to hypopharyngeal disease, such as dysphagia or throat discomfort. He was a 40-pack/year current smoker and consumed alcohol on a regular basis (>3 times per week). He had previously undergone Ivor-Lewis operation for esophageal squamous cell carcinoma (pT1N0M0) 1 year ago. Pathologic review of the biopsy specimen from the referring clinic showed squamous cell carcinoma. Endoscopic examination disclosed a round slightly elevated hyperemic mucosal lesion, approximately 8 mm at the longest diameter, at the right pyriform recess (Fig. 1A). NBI showed dilated, tortuous and irregular intrapapillary ca-pillary loops (IPCL), consistent with type V IPCL pattern described by Inoue et al. (Fig. 1B).7 Contrast enhanced neck and chest computed tomography (CT) scans showed no evidence of focal lesions or lymph node enlargement in the head and neck region, and positron emission tomography-CT scans were unrevealing. Based on these findings we diagnosed stage I early hypopharyngeal squamous cell carcinoma (cT1N0M0). The patient refused extensive resection and endoscopic resection was planned. Endoscopic resection was performed under general anesthesia. A cap fitted, forward-viewing, sterilized endoscope (EG2001i; Pentax Medical Systems Corp., Tokyo, Japan) was used for the entire procedure. Lugol's solution was applied for demarcation of the lesion, and marking around the lesion was performed with the Dual knife (KD-650Q; Olympus, Tokyo, Japan). Saline solution with 0.001% epinephrine and 0.004% indigo carmine dye was injected with a 23-gauge needle (NM-200L-0423; Olympus) into the submucosa under and around the lesion for mucosal elevation. After sufficient mucosal elevation around the lesion had been achieved, a snare was introduced into the accessory channel and suction was applied. The lesion was ensnared and resected en bloc using the cap assisted endoscopic mucosal resection (EMR-C) technique. The total procedure time was 35 minutes, and no complications occurred during the procedure. The resected specimen measured 10У9 mm and an erythematous elevated lesion was observed in the center of the specimen (Fig. 2A, B).
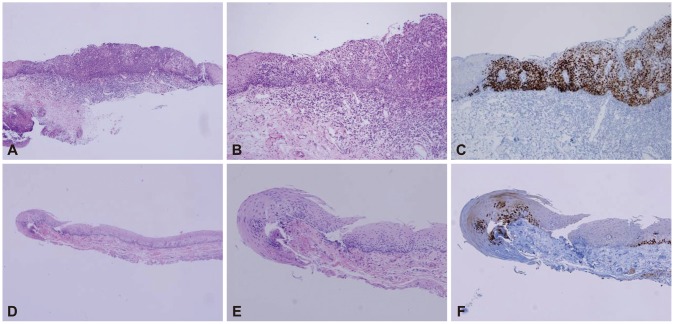
Immunohistochemical staining and pathologic analysis was consistent with squamous cell carcinoma in situ with p53 protein overexpression in the full thickness of the epithelial layer (Fig. 3A-C). Both lateral and vertical resection margins were free from involvement of the tumor. The patient recovered without incident and was discharged on the 6th postoperative day. Six months later on routine endoscopic follow-up, a slightly depressed hyperemic lesion was observed at the opposite left pyriform sinus (Fig. 1C). Although endoscopic biopsy was negative, NBI showed an irregular vascular pattern (Fig. 1D) and additional EMR-C was performed (Fig. 2C, D). Final pathologic results showed low grade dysplasia with focal p53 protein overexpression confined to the lower one-third of the epithelial layer (Fig. 3D-F).
DISCUSSION
Diagnostic screening endoscopy is performed routinely in Korea, and with it the incidence of early stage GI cancers is increasing. Although the detection of early stage hypopharyngeal carcinoma is difficult, such lesions can be identified as demarcated reddish areas on careful endoscopic examination.4,5 High definition imaging and new endoscopic imaging modalities such as NBI, magnifying endoscopy, and i-scan technology can further enhance the detection of such lesions. Muto et al.4 reported that NBI was superior to conventional endoscopy for detection of early stage oropharyngeal and hypopharyngeal cancer. Endoscopy may also play an important role for the surveillance and early detection of synchronous and/or metachronous squamous cell carcinoma of the oropharynx and esophagus in previously treated patients. As in our case, these cancers are known to have a high risk of developing second primary malignancies (field cancerization). The reported overall incidence of second primary malignancies, which is higher in smokers and alcohol drinkers than in non-smokers and nondrinkers, ranges between 5% and 30%, with an annual incidence of 1.5% to 7% per year, even in long-term survivors. Squamous cell carcinoma of the hypopharynx and oropharynx are known to be associated to secondary primary malignancies in the esophagus, and tumors at the same location.8,9
Currently in Korean and Japan, endoscopic resection of early gastric cancer is considered a standard therapy. However, the indication for endoscopic resection in the case of hypopharyngeal carcinoma is unclear because experience of surgical resection for early stage hypopharyngeal carcinoma is rare. Furthermore, the muscularis mucosa, which divides the GI mucosa from the submucosa, does not exist in the hypopharynx. Some authors have suggested that carcinoma in situ or slightly invaded carcinoma may be an indication for endoscopic resection.1-5 However, there is limited data to support this hypothesis. Therefore, strict informed consent and careful patient selection is needed prior to treatment.
Endoscopic resection of early stage hypopharyngeal cancer is less invasive, and has the potential to improve patients' quality of life with regard to swallowing disorder, aspiration pneumonia, speech, and cosmetic defects associated with extensive resection. However, for further expansion of endoscopic resection in cases of early stage hypopharyngeal carcinoma, multicenter studies aimed at establishing indication with regard to depth of invasion, tumor size, and frequency of complications are needed. Although further evidence is needed, the authors believe that endoscopic resection, preferably en bloc resection, is a viable option for early stage cancer or carcinoma in situ of the hypopharynx.