Endoscopic Management of Rectal Dieulafoy's Lesion: A Case Series and Optimal Treatment
Article information
Abstract
Rectal Dieulafoy's lesion (DL) is rare cause of lower gastrointestinal bleeding. Because of its rarity, there is no consensus on the optimal endoscopic hemostasis technique for rectal DL. We analyzed six patients who underwent endoscopic management for rectal DL after presenting with hematochezia at a single institute over 10 years. Of the six patients, three underwent endoscopic band ligation (EBL) and three underwent endoscopic hemoclip placement (EHP). Only one patient was treated with thermocoagulation. There were no immediate complications in any of the patients. None of the patients required a procedure or surgery for the treatment of rebleeding. Mean procedure times of EBL and EHP were 5.25 minutes and 7 minutes, respectively. Both EHP and EBL are shown to be effective in the treatment of bleeding rectal DL. We suggest that EBL may have potential as the preferred therapy owing to its superiority in technical and economic aspects, especially in elderly and high-risk patients.
INTRODUCTION
Rectal Dieulafoy's lesion (DL) is a rare cause of lower gastrointestinal bleeding. DLs are found mainly along the proximal body of the stomach, particularly at the lesser curvature. However, similar lesions have been reported in all regions of the gastrointestinal tract, including the esophagus, duodenum, jejunum, colon, and rectum.1
Owing to the small size of the ulceration and the massive bleeding associated with it, finding the lesion and treating it by endoscopy is often difficult. Therefore, in the past, patients were usually treated by surgical resection. However, the effectiveness of emergent endoscopic management, such as injection, coagulation, clipping, and band ligation, in the treatment of rectal DL has recently been demonstrated.2,3,4
Owing to its rarity, there is no consensus on the optimal endoscopic hemostasis technique for rectal DL. Therefore, we report on our experiences with endoscopic management for rectal DL at a single tertiary medical center between January 1, 2002 and December 31, 2011.
Endoscopic procedures
All patients underwent colonoscopy using a standard lower endoscope (CF-130I; Olympus, Tokyo, Japan and CFQ-260AI; Olympus). For endoscopic hemoclip placement (EHP), a hemostatic hemoclip (135-degree angle, HX-610-135; Olympus Optical Co., Ltd., Tokyo, Japan) was applied to the protruding vessels or adherent clots in the surrounding tissue. For endoscopic band ligation (EBL), a varioligator kit with a single-shot device (ConMed Cooperation, New York, NY, USA) was used. Endoscopic thermocoagulation was performed using a coagulation probe (MTW, Wesel, Germany).
CASE REPORTS
Case 1
A 65-year-old woman with a history of type 2 diabetes presented with profuse hematochezia while undergoing postoperative management of a femur neck fracture in a local medical center. She complained of constipation for 4 days. She was pale, with a blood pressure (BP) of 118/75 mm Hg and a pulse of 99 beats per minute. Her initial hemoglobin level was 6.3 g/dL, and she received three units of packed red blood cells (PRBCs). She was initially evaluated using flexible sigmoidoscopy, which did not reveal any evidence of bleeding. She did not complain of hematochezia for 3 days, and her vital signs were stable. She was transferred to the previous hospital, and we planned elective colonoscopy 2 weeks later. However, she was transferred to our hospital several hours later owing to repeated episodes of hematochezia. Our second evaluation included normal endoscopy and abdominal computed tomography (CT) scans, which reveal thickening of the rectum wall. She did not complain of hematochezia thereafter, and we carried out elective colonoscopy 3 days later. In this evaluation, multiple shallow erosions with a 3 mm protuberance and an adherent clot were identified. The lesion was treated with EBL. There had been no recurrence of bleeding after 2 months of follow-up.
Case 2
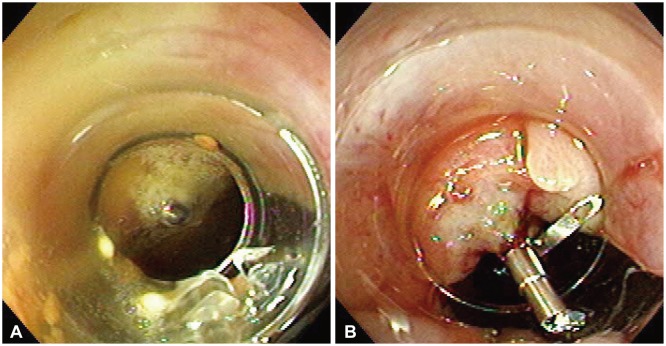
A 68-year-old man with a history of small cell lung cancer with multiple bone metastases presented with profuse hematochezia. He described a 2-month history of severe constipation after undergoing chemotherapy. Initial examination revealed a pale conjunctiva, a pulse of 95 beats per minute and a BP of 158/106 mm Hg. His initial hemoglobin level was 8.1 g/dL, requiring transfusion of two units of PRBCs. He experienced another large volume hematochezia and decreased BP of 74/54 mm Hg, and required further transfusion. Our initial examination included a normal abdominal CT scan, normal upper endoscopy, and emergent rectoscopy, which revealed a 2 mm protuberance with an adherent clot within a field of shallow ulceration in the rectum. EBL was performed but primary hemostasis failed. The lesion was subsequently treated with EHP (Fig. 1). No further bleeding had occurred after a follow-up of 6 months.
Case 3
A 75-year-old man was transferred from an outlying hospital because of uncontrolled hematochezia. Evaluation at the prior hospital included normal upper endoscopy and colonoscopy, which revealed a minute rectal mucosal defect with an associated exposed vessel. The lesion was treated with an injection of epinephrine, but hematochezia recurred several hours later. On arrival, his vital signs and physical examination results were normal. His initial hemoglobin level was 10.0 g/dL and had fallen to 6.6 g/dL, requiring transfusion of three units of PRBCs during hemodialysis. Colonoscopy revealed a shallow ulcer with a large protruding vessel and adherent clot. The lesion was treated with three EHPs. No further bleeding occurred for 3 days and he was transferred to a local medical center.
Case 4
A 71-year-old-man with a history of intermittent hematochezia for 2 days was transferred from a local medical center. He was admitted to the intensive care unit to manage congestive heart failure, and pulmonary edema was treated using diuretics. However, owing to his delirious mentality, he was admitted to the intensive care unit for 15 days. On arrival, his vital signs were normal, and his hemoglobin level was 9.5 g/dL. Prepped colonoscopy was performed and revealed an exposed vessel with a minute mucosal defect in the distal rectum. The lesion was treated with EHP. However, after 4 days he passed approximately 100 mL of hematochezia. Colonoscopy detected no evidence of bleeding at the previously clipped lesion. However, another exposed vessel with a superficial ulcer was detected and treated using EBL. No further bleeding had occurred after 4 days and he was transferred to a secondary medical center.
Case 5
A 65-year-old woman experienced bright red rectal bleeding during postoperative care for tongue cancer in an intensive care unit, and was suffering from postoperative complications such as infection and bleeding of the anastomosis site. On arrival at our department, her vital signs and abdominal examination results were normal. Her hemoglobin level increased from 8.0 to 9.4 g/dL after the transfusion of two units of PRBCs. Colonoscopy identified a protruding vessel surrounded by normal mucosa, 8 cm above the anal verge. The lesion was treated with EBL (Fig. 2, Supplementary Video 1 [available online at http://www.e-ce.org/]). After 22 months of follow-up, the patient was in good health.
Case 6
A 68-year-old woman with hypertension was transferred to our hospital owing to recurrent episodes of hematochezia. She had been admitted for the evaluation of hematochezia including colonoscopy, which revealed a rectal ulcer and an internal hemorrhoid. Initial vital signs and physical examination results were normal. Her baseline hemoglobin level was 9.0 g/dL and had fallen to 6.4 g/dL, requiring multiple transfusions. Colonoscopy revealed multiple ulcers and a small adherent clot surrounded by relatively normal mucosa in the distal rectum. The lesion was treated with thermocoagulation by a heat probe. There was no further bleeding during hospitalization and after 1 month of follow-up.
DISCUSSION
DL, which was first described by Dieulafoy in 1898, is categorized as superficial erosion overlying a large, tortuous, thick-walled artery in the muscularis mucosa.5 DL, a relatively rare cause of gastrointestinal bleeding, is typically found within the upper gastrointestinal tract.1 However, it has recently been reported within the entire length of the gastrointestinal tract, including the rectum.5
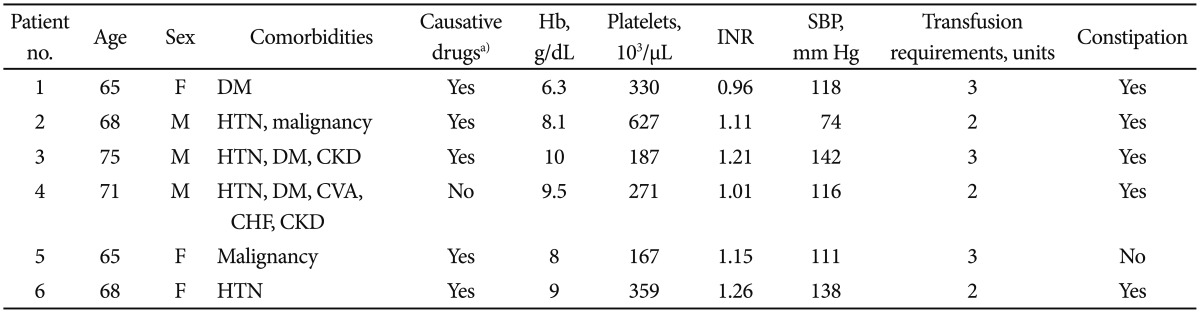
DL is more common in middle-aged men, with a median age of 52 years at presentation.5 In our reported cases, there were equal numbers of males and females, and all patients were over 65 years old (Table 1). Patients with DL are usually divided into young and old groups.6 Significant comorbidities, including diabetes, hypertension, CKD, cardiovascular disease, and excessive consumption of alcohol are usually observed in the older patient group. These factors suggest that the triggering events of bleeding are caused by the combined effects of age-related mucosal damage and comorbidities.7 In our study, most patients suffered from constipation (five of six patients) and three of six patients were in an immobile state. Therefore, unlike for other locations of DL, constipation is more strongly related to rectal DL in elderly patients with underlying diseases.8 Although there is little direct evidence indicating that aspirin, warfarin, and nonsteroidal anti-inflammatory drugs cause DL, the use of such medications has been reported in more than 50% of DL patients.5
DL is usually diagnosed endoscopically. However, because the lesion can be small and the bleeding intermittent, locating the lesion can be difficult and repeated colonoscopy is often needed. With the improvement of CT, multidetector CT, basis of the success of urgent colonoscopy, is another option for localization of rectal DL, and allows the endoscopist to perform a more targeted colonoscopic examination.3
Identification of the source of bleeding is often difficult during the operation and development of endoscopic techni-ques. Therefore, DL is usually treated by endoscopic hemostasis, and mechanical endoscopic methods are superior to other types of endoscopic hemostasis such as injection and thermal therapy.9,10 Several recent reports have demonstrated the efficacy of EBL and EHP for DL in the upper gastrointestinal tract.9,10,11 There are several case reports of the successful treatment of rectal DL by EBL or EHP.3,4,6,12,13,14,15 However, opinions concerning EBL and EHP are conflicted. One recent study reported that EBL could lead to ulcer formation and cause rebleeding and perforation.12 On the other hand, a different study suggested that EBL could be an effective modality for the control of bleeding in rectal DL, even after the failure of other endoscopic treatments, such as EHP.4
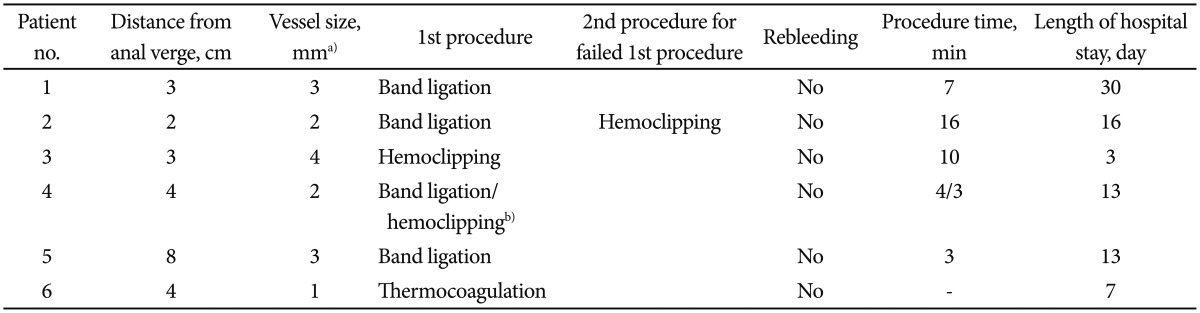
In our reported cases, if a mechanical endoscopic method was available, primary hemostasis was almost always successful (Table 2). However, in addition to the outcomes of hemostasis, technical simplicity and duration of endoscopic procedure may be important factors of hemostatic efficacy. In general, EBL is simple, readily available, and relatively inexpensive and may be more effective in patients with coagulopathy.16 In addition, the relatively short procedure time of EBL may prevent any potential immediate complications during endoscopic procedures in elderly patients with rectal DL, who often suffer from many underlying diseases.
However, a limitation of this study is that delayed bleeding was not followed up as two of the patients were transferred to other institutions.
In conclusion, the effectiveness of both EHP and EBL for the treatment of bleeding in rectal DL was demonstrated. Being superior in both technical and economic aspects, we suggest the potential for the use of EBL as the preferred therapy, especially in elderly and high-risk patients.
Notes
The authors have no financial conflicts of interest.