Corrosive Esophagitis Caused by Ingestion of Picosulfate
Article information
Abstract
Corrosive esophagitis is characterized by caustic injury due to the ingestion of chemical agents, mainly alkaline substances such as detergents. Esophageal bleeding, perforation, or stricture can be worsened by high-degree corrosive esophagitis. Picosulfate is a commonly used laxative frequently administered for bowel preparation before colonoscopy or colon surgery. Picosulfate powder should be completely dissolved in water before ingestion because the powder itself may cause chemical burning of the esophagus and stomach. Here, we report a case of corrosive esophagitis due to the ingestion of picosulfate powder that was not completely dissolved in water.
INTRODUCTION
Corrosive esophagitis is characterized by caustic injury following the ingestion of chemical agents, mainly alkaline substances such as detergents, cleaning compounds, and bleaches. The ingestion of acidic substances can also cause caustic injury, but these cases are less frequently reported than those caused by alkaline agents in the United States.1
Early endoscopic intervention is very useful in suspected cases of corrosive esophagitis, not only for determining the degree of mucosal injury and severity, but also for predicting prognosis.2 High-degree corrosive esophagitis may result in esophageal bleeding, perforation, and even death in the worst cases. In particular, esophageal stricture, one of the more serious complications of corrosive esophagitis, may require recurrent ballooning procedures, which are highly expensive. Moreover, the rates of esophageal carcinoma are 1,000 to 3,000 times higher in patients with esophageal complaints than those in healthy individual.3
Picosulfate (Picolight Powder; Pharmbio, Seoul, Korea), a widely used laxative, is used to prepare the intestine for colonoscopy or colon surgery. This laxative may induce side effects including abdominal pain, persistent diarrhea, or electrolyte imbalance. However, picosulfate is still considered to be relatively safe, as these complications only occur in rare cases. Generally, it is recommended that picosulfate powder should be completely dissolved in water and cooled before drinking because an exothermic reaction may occur immediately after the substance comes into contact with water, which can result in chemical burning of the esophagus and stomach.
Here, we report the first case of corrosive esophagitis due to the ingestion of picosulfate powder.
CASE REPORT
A 48-year-old man presented with hematemesis at the emergency department. He had ingested picosulfate that was not completely dissolved in water as preparation for colonoscopy. He had lost a cup of blood, but was hemodynamically stable and alert (blood pressure, 130/70 mm Hg; heart rate, 72 beats per minute). He had no further accompanying signs and symptoms. His initial hemoglobin level was 14.9 g/dL, and other laboratory tests results, including coagulation and electrolytes, were normal.
Fifteen hours after admission, the patient underwent upper gastrointestinal flexible endoscopy. During the procedure, we detected diffuse linear mucosal breaks with spontaneous blood oozing from the mid-esophagus to the esophagogastric junction caused by caustic esophageal injury. In addition, linear erosion at the gastric antrum and ulceration at the greater curvature of the gastric body were detected (Fig. 1). Finally, the patient was diagnosed with corrosive esophagitis caused by picosulfate.
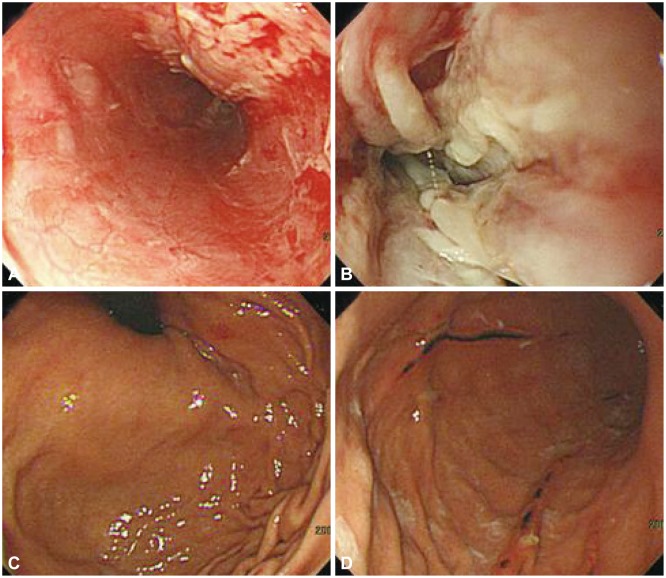
Endoscopy performed 15 hours after admission showing corrosive esophagitis. (A) Diffuse linear mucosal breaks with oozing and whitish exudates in the mid-esophagus. (B) Shallow ulcerations with oozing and whitish exudates at the esophagogastric junction. (C) No abnormal findings in fundus except mild erosion in cardia. (D) Linear ulcers with hematins from the mid-body to low-body.
The patient was treated with conservative methods, including total parenteral nutrition and an intravenous proton pump inhibitor (esomeprazole, 40 mg). After endoscopy, the patient only had mild fever without any other symptoms. We regarded the fever as transient, but administered antibiotics (cefotaxime, 2 g) because we could not rule out the possibility of infection.
Seven days after admission, the patient had no more hematemesis or melena. Ten days after admission, the patient underwent follow-up upper gastrointestinal endoscopy. Linear ulcerations and signs of healing were detected in the esophagus, but there were no more visible oozing lesions or stricture (Fig. 2). After this endoscopic procedure, he started eating a soft diet and stopped taking antibiotics and intravenous esomeprazol. He was stable and had no further symptoms, and was discharged with no complications.

Endoscopy performed (A-C) after 10 days, and (D-F) after 5 months of treatment, showing the healing state of corrosive esophagitis. (A) Linear ulcer scars in the mid-esophagus. (B) Linear ulcers with blood clots. No stricture at the esophagogastric junction. (C) Linear healing ulcers in the low-body. (D, E) No mucosal abnormality in the esophagus and stomach. (F) A linear whitish scar in the stomach.
After 5 months, the patient underwent follow-up upper gastrointestinal endoscopy. There were no mucosal abnormalities in the esophagus and stomach, except for a linear whitish scar in the stomach (Fig. 2).
DISCUSSION
Picosulfate is a stimulant laxative that improves bowel peristalsis and increases bowel mucosal secretions. Generally, this laxative is dissolved with water before drinking, and activated by hydrolysis of arylsulfate, an enzyme derived from colonic bacillus plexus.4 This mechanism facilitates peristalsis, blocks the absorption of water in the intestine, and finally induces diarrhea.4 Picosulfate is widely used, and many physicians mix it with magnesium and citric acid for bowel preparation before colonoscopy or bowel surgery.5 However, side effects such as abdominal pain, thirst, vomiting, or electrolyte imbalance can follow the use of picosulfate.6 Electrolyte disturbances, mainly hyponatremia, are present in 7.5% of patients, and can lead to seizures and rhabdomyolysis in severe cases.6
Corrosive esophagitis is often caused by ingestion of alkaline agents, but rarely by the ingestion of acidic agents. Although cases of corrosive esophagitis caused by acidic agents are very rare compared to those caused by alkaline agents, higher rates of side effects and complications such as perforation and stricture have been reported for acidic agent-driven corrosive esophagitis.1,2 Additionally, a case of corrosive esophagitis due to the ingestion of liquid glue, which includes toluene,6 and diluted pendimethalin, a herbicide, have also been reported.7
As previously stated, both alkaline and acidic substances can induce corrosive esophagitis, but the effects of these two types of agents are explained by different pathophysiologic theories. Alkaline agents cause liquefaction necrosis, which leads to the destruction of mucosa within a few seconds. One or 2 days after the ingestion of alkaline substances, destruction of the mucosa is exacerbated by thrombosis in small vessels and the production of heat. In contrast, acidic agents cause coagulation necrosis with eschar formation, which may limit tissue penetration.1
Once picosulfate is dissolved in water, the substance is acidic and releases hydrogen ions by hydrolysis. To reduce the possibility of corrosive esophagitis occurring, dissolving picosulfate in a high volume of water is strongly recommended because this renders the dissolved picosulfate less acidic. On the other hand, dissolving picosulfate in a low volume of water produces a more strongly acidic liquid, which more frequently leads to corrosive esophagitis.1 Furthermore, picosulfate powder itself may cause chemical burning in the esophagus and stomach by an exothermic reaction after it has been dissolved in water. Presumably, the present case was caused by strong acidity due to incomplete dilution, and chemical burning from an exothermic reaction.
Although each study has some different criteria, grade of corrosive esophagitis is in general classified according to endoscopic findings according to Zagar's grade.8 The present case was regarded as grade 2a corrosive esophagitis (hemorrhage, exudates, and superficial [not deep] ulceration).9 Esophageal stricture can be complicated in grades 2 to 3.10,11 However, in the present case, esophageal stricture did not occur after the event. It can be inferred that crucial esophageal muscular damage did not occur after corrosive injury.
All things considered, we report here the first case of corrosive esophagitis due to the ingestion of picosulfate powder incompletely dissolved in water due to the patient not taking sufficient care, diagnosed through endoscopy in the early stage, and completely cured without complications by conservative treatment. Endoscopists should inform patients not to take picosulfate powder itself for colonoscopic preparation.
Notes
The authors have no financial conflicts of interest.