Education and Training Guidelines for the Board of the Korean Society of Gastrointestinal Endoscopy
Article information
Abstract
The Korean Society of Gastrointestinal Endoscopy (KSGE) developed a gastrointestinal (GI) endoscopy board in 1995 and related regulations. Although the KSGE has acquired many specialists since then, the education and training aims and guidelines were insufficient. During GI fellowship training, obtaining sufficient exposure to some types of endoscopic procedures is difficult. Fellows should acquire endoscopic skills through supervised endoscopic procedures during GI fellowship training. Thus, the KSGE requires training guidelines for fellowships that allow fellows to perform independent endoscopic procedures without supervision. This document is intended to provide principles that the Committee of Education and Training of the KSGE can use to develop practical guidelines for granting privileges to perform accurate GI endoscopy safely. The KSGE will improve the quality of GI endoscopy by providing guidelines for fellowships and supervisors.
INTRODUCTION
Since November 1995, the Korean Society of Gastrointestinal Endoscopy (KSGE) has launched a board of gastrointestinal (GI) endoscopy specialists, and many gastroenterologists have obtained the privilege of being GI endoscopists. The KSGE has established the goals and guidelines for educating trainees in 2011, and an updated version for both endoscopic faculties and trainees is now required to meet the need to catch up to the recent rapid changes in clinical practice [1]. GI endoscopy is the most valuable and final diagnostic tool used in gastroenterology. Education of endoscopic skills is an essential portion of the GI fellowship training program. The GI endoscopic field is now sub-classified as a part of the diagnostic and therapeutic procedures for the GI tract, including esophagogastroduodenoscopy (EGD), colonoscopy, endoscopic retrograde cholangiopancreatography (ERCP), and endoscopic ultrasound (EUS). Small bowel endoscopies, including balloon-assisted and capsule endoscopies, are now standard procedures for small bowel diseases; however, these procedures require specialized techniques and skills [2,3]. Furthermore, small bowel endoscopy is generally performed on rare occasions only in the limited referral centers in Korea. For these reasons, small bowel endoscopy is not included as a learning item in this guideline; however, further discussion is needed in the near feature. Considering the relatively short training duration in Korea, there can be limitations for trainees in acquiring adequate skills during their training course. Endoscopic procedures by fellows are initially performed under constant supervision by faculties; however, the endoscopic skills of trainees are expected to progress without supervision. Thus, there is a need to revise the guidelines and training programs to provide the acknowledgement of individual skill levels for performing procedures without supervision. The KSGE Education of Practice Committees develop revised educational guidelines and provide training goals for both endoscopic faculties and trainees designed to estimate the individual level of endoscopic skill for performing endoscopic procedures without supervision. This document describes each endoscopic technique, method of measuring quality indicators, education goals and updated guidelines on conscious sedation, EGD, colonoscopy, ERCP, and EUS, and quality control of endoscopic procedures and disinfection methods. To complete the training on GI endoscopy, trainees should be prepared to (1) perform effective and safe procedures, including conscious sedation and pre-procedure evaluation and monitoring of each patient; (2) describe endoscopic findings adequately and provide proper treatment accordingly; (3) identify procedure-related risks and complications to minimize the adverse effects in patients and manage complications appropriately when they occur; (4) acknowledge the indications or contraindications of endoscopic procedures and respond to or guide patients appropriately when consultation is needed; (5) identify their personal degree of skill, limitation, and when to request for a senior’s help; (6) identify the concepts of quality control and maintain qualified endoscopic procedures; and (7) acknowledge and maintain the protocol of disinfection and educate it to nursing staff.
SEDATION IN GI ENDOSCOPY (ESSENTIAL)
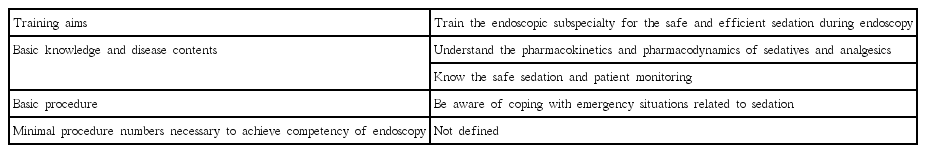
Sedation is an essential procedure for endoscopic specialist training because it decreases patients’ pain and discomfort levels and improves endoscopists’ performance and satisfaction. Since February 2017, sedation in GI endoscopy for treatments has been covered by the national health insurance. The guidelines of sedation for GI endoscopy have been introduced in the USA and Japan in 1995 [4,5]. In Korea, such guidelines have already been established [1]. The educational objectives of sedation in GI endoscopy are essential to train the endoscopic subspecialty for a safe and efficient sedation during endoscopy. The education and training guidelines of sedation in GI endoscopy are summarized in Table 1.
Training aims
Understand the pharmacokinetics, pharmacodynamics, antagonists, side effects, and contraindications of sedatives and analgesics
Know safe sedation and patient monitoring
Have the ability to know and respond to emergencies related to sedation
Training details
Prior to endoscopic sedation, patients’ consent should be obtained, and patients’ up-to-date medical history and physical examination results should be assessed. Endoscopic sedation should be performed with knowledge on sedative drugs, degree of sedation, patient monitoring, complications of sedation, and post-sedation care. Appropriate management of the adverse events related to sedation should also be reminded.
Knowledge of sedative drugs
Understand the types of sedative drugs used in endoscopy, their pharmacokinetics, initial and maintenance doses, antagonists, complications, contraindications, and drug interactions of each drug.
Select a sedative and consider the dose, taking into account the patients’ underlying disease and current medication.
Understand situations where proper analgesics should be used with appropriate sedation.
Pre-sedation assessment
1. Agreement
(1) Let the patients understand the purpose, procedure, effects, risk, side effects, and how to treat the complications with your explanation and provide consent voluntarily.
(2) Taking their medical and social histories related to sedation.
i) Major organ disease
ii) Side effects and allergic reaction to sedatives or analgesics
iii) Current medication and its interaction with sedative drugs
iv) Duration of nothing by mouth (NPO)
v) Habits of smoking and/or alcohol and drug abuse
2. Understand the classification of the patients’ physical states as suggested by the American Society of Anesthesiologists before sedation [6].
3. Judge whether the patients’ condition is normal by measuring the vital signs, including the state of consciousness and blood pressure before sedation.
(1) Physical examination
i) Mental status
ii) Vital signs and body weight
iii) Auscultation of the heart and lung
iv) Airway
Assessment of the degree of sedation and monitoring
1. Assessment of the degree of sedation
(1) Assess the degree of sedation according to the level of sedation.
i) Be aware of the continuum of anesthesia: mild sedation, moderate sedation, and deep sedation, and be aware of the changes in the physiology of each sedation [7].
ii) Induce desired level of sedation, and understand its biomechanics.
2. Monitoring
(1) Perform appropriate monitoring according to endoscopic procedure and type.
(2) Continuously or periodically monitor the blood pressure, pulse oximetry, and heart beat using electrocardiogram (ECG).
(3) The patients’ consciousness state should be checked periodically according to the Modified Observer’s Assessment of Alertness/Sedation Scale [8].
(4) Depending on the patients’ condition, determine whether to administer proper oxygen.
Post-sedation care
1. Ensure proper monitoring until the patients recover from the sedation.
2. If necessary, determine whether antagonists of the sedative drugs should be administered.
3. To determine discharge status from the endoscopic unit, the patients’ condition should be evaluated according to the Aldrete’s score [9].
4. Explain the precautions after discharge.
Special conditions
1. Determine safe sedation according to the cases of a child, elderly, pregnant woman, and lactating woman.
2. Be aware of the risks and sedation-related adverse events in patients with liver cirrhosis and other chronic illnesses.
Emergent management (respond to emergent conditions accurately and quickly)
1. Know the situations that require you to stop the sedation in endoscopy.
(1) Severe hypoxia
(2) Paradoxical reaction
(3) Hemodynamic instability
2. Be aware of the use of emergency medications and equipment for emergency resuscitation.
EGD (ESSENTIAL)
EGD is the most important tool for the diagnosis and treatment of upper GI tract diseases and is one of the most frequently performed tests in Korea where the prevalence of gastric cancer is high. As the national cancer screening project started in 1999, and the number of affected patients increased gradually, the national cancer screening rate reached 67.3% in 2014. As the demand for endoscopy increases, the demand for doctors to perform endoscopy surges, and a large number of endoscopic specialists are released every year. Therefore, the KSGE was established in 2011 to provide detailed guidelines for upper GI endoscopic subspecialty training and appropriate endoscopic education during the entire period of GI fellowship training. At present, training regulations of subspecialty in the KSGE are prescribed as recommendations of at least 1,000 times of upper GI endoscopy (more than 100 times in case of trainees who majored in pediatrics) and more than 30 times of endoscopic treatment procedures. The purpose of this upper GI endoscopic training is to provide a new guideline that summarizes the items to be acquired during the endoscopic training period by referring to the recently revised endoscopic training guidelines of other countries. Based on this guideline, we would like to create a fruitful education on upper GI endoscopy. The education and training guidelines of EGD are summarized in Table 2.
Training aims
Understand the anatomy of the upper GI tract and normal endoscopic findings
Learn the indications, limitations, and contraindications of EGD Understand the method of preparation for EGD, adverse events associated with the procedure, and countermeasures to use in such situations
Understand upper GI tract diseases, differentiation of endoscopic findings, and differentiation between benign and malignant neoplasms
Understand the indications, limitations, and contraindications for EGD treatment and procedures, and consider alternatives to treatments
Understand the prior consent of the EGD and related ethical issues
Learn newer skills and knowledge pertaining to EGD
Understand the indications for the use of prophylactic antibiotics for EGD
Understand and be aware of the risk of cerebrovascular complications in patients who receive anti-thrombotic agents and management of bleeding risk according to endoscopic procedures
Training details
Gain basic knowledge on EGD
1. Learn the endoscopic features and causes of malfunctions and how to solve them.
2. Learn common diseases depending on the sites.
3. Learn the principles of lesion observation and image recording.
Diagnostic EGD
1. Esophageal disease
(1) Understand the normal esophagus structure and deformation.
(2) Learn to distinguish endoscopic findings from the etiology of infectious esophagitis.
(3) Learn the endoscopic classification of reflux esophagitis.
(4) Learn to distinguish esophageal varices according to color change, site, morphology, and erosion.
(5) Understand the endoscopic findings of Barrett’s esophagus.
(6) Understand the endoscopic findings of esophageal hernia.
(7) Diagnose esophageal cancer using chromoscopy, and learn to distinguish it from benign tumors.
2. Stomach disease
(1) Understand the normal stomach structure and deformation.
(2) Learn to classify gastritis and describe various endoscopic findings associated with it.
(3) Learn to classify and describe gastric ulcers with progress.
(4) Understand the features and accompanying deformities of gastric ulcer according to sites.
(5) Learn to distinguish benign gastric ulcers from malignant lesions.
(6) Understand the endoscopic features of advanced gastric cancer and early gastric cancer.
(7) Learn to determine recurrence at the anastomotic site of the remnant stomach.
(8) Learn to classify gastric polyps.
(9) Understand the endoscopic findings of submucosal tumors, and distinguish them from external compression.
3. Duodenal disease
(1) Understand the normal duodenal structure and deformation.
(2) Understand the endoscopic findings of duodenal inflammatory diseases and duodenal tumors.
(3) Endoscopic findings of duodenal varices, vascular dysplasia, amyloidosis, and lymphangiectasis can be described.
4. Target biopsy
(1) Understand the indications for biopsy.
(2) Understand the biopsy method and sequence according to lesion location.
(3) Understand the number and location of biopsy by lesion.
(4) Learn about possible complications after biopsy and how to deal with them.
Therapeutic EGD
1. Upper GI bleeding
(1) Understand the causes of upper GI bleeding.
(2) Learn the treatment for patients with GI bleeding.
(3) Understand the clinical judgment of indications for emergency endoscopic hemostasis.
(4) Understand effective endoscopic therapy for each disease.
i) Treatment of non-variceal upper GI bleeding: hemoclipping, electric coagulation treatment, argon plasma coagulation treatment, and injection therapy
ii) Treatment of variceal upper GI bleeding: band ligation and sclerotherapy
(5) Understand the endoscopic classification of hemorrhagic lesions.
(6) Endoscopic hemostasis is performed 10 times or more under supervision, and single-handed treatment is recommended 10 times or more.
2. Foreign body removal
(1) Understand the clinical features and adaptation of endoscopic treatment according to specific foreign bodies.
(2) Learn the complications of the presence of foreign bodies.
(3) Understand the removal method according to the location and type of foreign objects, selection of accessory equipment necessary for removal, secondary damage, and prevention of damage.
(4) Endoscopic removal of foreign bodies should be performed five times or more under the supervision of the instructor, and single-handed procedures should be recommended five times or more.
3. Esophageal dilation: pneumatic dilatation, balloon dilatation, and bougie dilation
(1) Understand the indications that require esophageal dilatation.
(2) Understand the various methods used for esophageal dilatation.
(3) Learn the complications and preventive measures after esophageal dilatation.
4. Percutaneous endoscopic gastrostomy
(1) Understand the indications for percutaneous endoscopic gastrostomy.
(2) Understand the procedures and preparation materials necessary for percutaneous endoscopic gastrostomy.
(3) Understand the complications after percutaneous endoscopic gastrostomy.
5. Polypectomy
(1) Understand the indications for polypectomy.
(2) Understand the types of instruments used in polypectomy and how to use them.
(3) Understand the procedures and preparations before polypectomy.
(4) Understand the management and follow-up methods after polypectomy.
6. Endoscopic mucosal resection and endoscopic submucosal dissection
(1) Understand the indications for endoscopic mucosal resection and endoscopic submucosal dissection.
(2) Understand the preparation materials, equipment, and procedure of endoscopic mucosal resection and endoscopic submucosal dissection.
(3) Learn the complications and management of endoscopic mucosal resection and endoscopic submucosal dissection.
(4) Interpret and understand the pathologic findings after resection.
7. Stent insertion: esophagus and pylorus
(1) Understand the indications for the treatment of stent.
(2) Understand the preparations, instruments, and procedures for stent insertion.
(3) Understand the types of stents and their advantages and disadvantages.
(4) Understand the complications and managements of stent insertion.
COLONOSCOPY (ESSENTIAL)
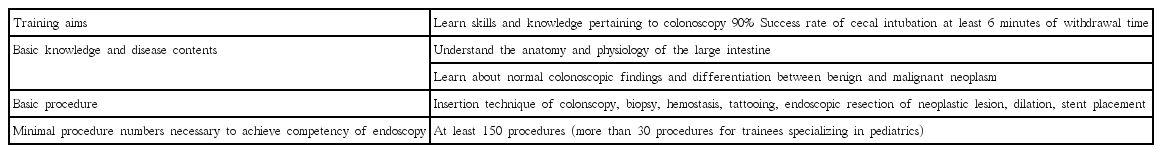
During the training period of GI endoscopic fellowship, colonoscopy is an interesting and rewarding process to learn the most accurate and useful diagnostic method for colonic diseases, as well as establish a basis for endoscopic therapy. It is also important to understand the indications and contraindications for accurate diagnosis and treatment, understand the patients’ condition before the procedure, learn to monitor the patients properly during the procedure, learn to select a procedure that would minimize inconvenience to the patients, learn proper evaluation of endoscopic findings, understand how to identify and minimize risk factors associated with the procedure, prevent complications, and take appropriate remedial measures [10]. The KSGE has mandated that at least 150 colonoscopic procedures be performed by trainees (recommendation of more than 30 colonoscopic procedures for trainees specializing in pediatrics). The number of colorectal endoscopy procedures that can be performed safely, accurately, and comfortably is incumbent on the individual abilities of trainees, interest of the educator, ability to use educational equipment, and work milieu [11-15]. There are no systematic training goals or guidelines available for colonoscopies. The KSGE intends to prescribe specific knowledge qualifications related to colonoscopy for trainees during the training period for them to acquire and use the desired skills. The education and training guidelines of colonoscopy are summarized in Table 3.
Training aims
Understand the anatomy of the large intestines and normal endoscopic findings
Learn the indications, limitations, and contraindications of colonoscopy
Understand the method of preparation for colonoscopy, adverse events associated with the procedure, and countermeasures to use in such situations
Gain knowledge pertaining to types of anesthetics with respect to pharmacokinetics, antagonists, complications, and contraindications to their use
Understand the techniques for safe insertion of a colonoscope
Gain knowledge regarding colonic diseases, effective interpretation of endoscopic findings, and differentiation between benign and malignant neoplasms detected endoscopically
Learn the indications, limitations, and contraindications of therapeutic colonoscopy
Understand the complications associated with therapeutic colonoscopic procedures and how to deal with them
Understand the issues pertaining to consent and ethical concerns related to colonoscopy
Learn newer skills and knowledge pertaining to colonoscopy
Understand and be aware of the quality indicators of colonoscopy [16]
Training details
Gain basic knowledge on colonoscopy
1. Learn a particular colonoscopic specification, and learn to cope with malfunctions of the instrument.
2. Understand the types, principles, methods, evaluation, advantages, and disadvantages, as well as contraindications of colonic preparation.
3. Understand the methods and principles of insertion of a colonoscope and how to eliminate/reduce looping.
4. Understand the principles of observation of lesions and recording of images.
5. Learn the indications and use of prophylactic antibiotics.
6. The adenoma detection rates should be maintained at 20% for women and 30% for men in the at-risk group, with the mean age being above 50 years [16].
7. In patients who have not undergone colonic resection or intestinal surgery, the colonoscope withdrawal time should be at least 6 minutes.
8. The success rate of cecal intubation should be maintained above 90% with no stenosis and good preparation.
9. Understand and be mindful of the screening interval and follow-up colonoscopy required for each patient.
Diagnostic colonoscopy
1. Colon cancer
(1) Learn about precancerous lesions and factors contributing to an increased risk of colorectal cancer.
(2) Learn the basic principles of screening and follow-up required for colorectal cancer.
(3) Understand the clinical features, staging, and principles of treatment for colorectal cancer.
(4) Understand the surgical principles and prognosis of colorectal cancer and follow-up examinations.
(5) Understand the endoscopic treatment of colorectal cancer.
(6) Understand the classification based on early and advanced colorectal cancers.
(7) Understand the classification and clinical characteristics of laterally spreading tumors.
(8) Learn to classify changes in colon pits, and understand the clinical characteristics using a magnifying endoscopy and narrow-band imaging [17].
(9) Learn to identify the endoscopic findings of metastatic colorectal cancer, invasive cancer from surrounding organs, lymphomas, and carcinoid tumors.
2. Colonic polyps
(1) Understand the pathology, endoscopic classification, and principles of treatment of colonic polyps.
(2) Be aware of the fact that the risk of malignant transformation depends upon the size of adenomatous polyps.
(3) Learn the classification of polyposis and its clinical features.
(4) Be aware of genetic abnormalities associated with, clinical manifestations, endoscopic findings, follow-up examination, and principles of treatment for familial adenomatous polyposis.
3. Chronic inflammatory bowel disease
(1) Understand the types and definitions of chronic inflammatory bowel disease.
(2) Study the pathophysiology, clinical features, complications, and treatment methods for ulcerative colitis and Crohn’s disease.
(3) Understand endoscopic findings based on the stage of ulcerative colitis, and learn to classify its activity level.
(4) Be aware of the fact that Crohn’s disease should be diagnosed on the basis of the endoscopic findings and the differential diagnosis of other diseases.
(5) Be aware of and measure the disease activity level of Crohn’s disease.
(6) Understand the types, indications, and contraindications of drugs used to treat inflammatory bowel disease.
(7) Learn the surgical indications for the treatment of ulcerative colitis and Crohn’s disease.
(8) Identify risks, and familiarize oneself with principles to monitor for the development of cancer in ulcerative colitis and Crohn’s disease.
(9) Study Behcet’s enteritis with respect to definition, pathological findings, clinical features, and endoscopic findings.
4. Vascular diseases of the colon
(1) Learn the clinical manifestations, sites of occurrence, and endoscopic findings of ischemic bowel disease.
(2) Understand the diagnosis and principles of treatment of ischemic bowel disease.
(3) Study angiodysplasia in the colon with respect to its clinical features, endoscopic findings, and treatment.
5. Miscellaneous
(1) Learn to identify endoscopic findings, and learn the treatment modalities for amoebic, pseudomembranous, and other infectious enteritis.
(2) Learn the endoscopic findings and treatment modalities for radiation enteritis.
(3) Learn the endoscopic findings and treatment of rectal ulcers.
(4) Learn the endoscopic findings and treatment modalities for hemorrhoids and fistulas.
(5) Learn the endoscopic findings and principles of treatment for colonic diverticula and related diseases.
(6) Understand endoscopic tattooing of colonic lesions [18].
Therapeutic colonoscopy
1. Colonoscopic hemostasis
(1) Learn about the general treatment in patients with GI bleeding.
(2) Understand the etiology, risk factors, and complications associated with lower GI bleeding.
(3) Understand the characteristics of, as well as the advantages and disadvantages of performing endoscopic hemostasis.
(4) Learn to determine indications for emergency endoscopic hemostasis, and familiarize oneself with the types and characteristics of different methods of endoscopic treatment.
(5) Learn to recognize the clinical characteristics of the cause of hemorrhage, and select effective endoscopic therapy.
2. Polypectomy
(1) Gain knowledge on the indications for polypectomy.
(2) Familiarize oneself with the types and proper instrumentation for polypectomy.
(3) Understand the pre-treatment procedures and appropriate preparation for polypectomy.
(4) Familiarize oneself with the complications and adverse events associated with polypectomy and their management.
(5) Learn the management and follow-up methods after polypectomy.
(6) During training, a trainee will perform 10 supervised polypectomies under the guidance of a specialist and 10 independent polypectomies.
3. Mucosal resection and submucosal dissection
(1) Understand the indications of mucosal resection and submucosal dissection for colorectal lesions.
(2) Gain knowledge on the preparation required for mucosal resection and submucosal dissection and the instruments and procedures used for these techniques.
(3) Understand the complications, risk factors, and treatment options for mucosal resection and submucosal dissection.
(4) Understand the advantages and disadvantages of mucosal resection and submucosal dissection.
(5) Analyze and understand the interpretation of pathological findings of resected specimens.
4. Colonic stent insertion
(1) Understand the indications for colonic stent insertion therapy.
(2) Understand the pre-procedural preparation required, instruments used, and the actual procedure.
(3) Understand the types of artificial stents and advantages and disadvantages of their use.
(4) Learn to identify complications, risk factors, and countermeasures to manage adverse events that can occur after insertion of a stent effectively.
ERCP (OPTIONAL)
ERCP is an advanced endoscopic procedure that is used for the management of various biliary and pancreatic diseases. This procedure is one of the most technically demanding and highest-risk procedures performed by endoscopists. Therefore, training in ERCP requires technical and cognitive skills over and above routine endoscopy and significant time and effort to attain competency [19]. In the American Society of Gastrointestinal Endoscopy (ASGE) guideline, trainees who opt to pursue additional training in ERCP to attain procedural competence should have completed at least 18 months of a standard gastroenterology training program [20]. Similarly, many other countries also require competency in general endoscopy before ERCP training [21,22]. Our previous guideline also suggested that ERCP training should begin after completion of the 1-year fellowship training of GI endoscopy [1]. According to this aspect, our guideline suggests that ERCP training is not essential for the fellowship training of general GI endoscopy; however, all trainees require some exposure to ERCP to develop an understanding of the diagnostic and therapeutic role of ERCP during the first year of training. The education and training guidelines of ERCP are summarized in Table 4.
Training aims
For the acceptable level of competence to perform independent ERCP after training, the ASGE guidelines emphasize objective measures over case volume itself, that is, achievement of selective cannulation in at least 90% of procedures [23]. In addition, trainees should be expected to perform at least 80 independent sphincterotomies and 60 biliary stent placements [23]. This level of success may not be achievable within 1 year of ERCP training or even after 200 supervised independent ERCP procedures, which is the threshold number of cases before competency can be evaluated [23]. In the UK, trainees should perform at least 180 ERCPs under supervision, and they cannot be considered competent in ERCP until they can cannulate the desired duct in over 90% of cases [24,25]. In Canada, the competence for ERCP can be assessed after 200 procedures and include 85% success rate of selective cannulation and 85% success rate of biliary stone removal or biliary drainage [22]. Because each trainee has different abilities and learning curves, this minimum number does not guarantee competence. In 2017, the Korean Pancreatobiliary Association (KPBA) published ERCP educational guidelines for fellows. In these guidelines, the goal of training is to achieve success rates of 80% of selective cannulation and 85% of biliary stone removal [26]. Although the KPBA did not define the minimum number of supervised procedures needed for credentialing, this needs to be discussed in the near future.
Training details
The cognitive aspects of ERCP are important and include an understanding of the indications and contraindications of the procedure and appropriateness of different diagnostic and therapeutic modalities in the management of pancreatobiliary diseases. Further, trainees should know about informed consent, sedation, and reporting. Understanding the risks and benefits of ERCP in certain patient groups, as well as alternative investigations, such as computed tomography, magnetic resonance cholangiopancreatography, and EUS, is paramount for an adequate management of patients with biliary and pancreatic disorders.
Basic knowledge and skills of ERCP
1. Be competent in diagnostic and therapeutic upper and lower endoscopies before ERCP training.
2. Have thorough knowledge on the anatomy and physiology of the pancreas and the biliary tree, including common variants in anatomy.
3. Be knowledgeable on side-viewing endoscopes, and be competent in passing the side-viewing endoscope into the duodenal papilla.
4. Be knowledgeable on the indications and contraindications for ERCP, procedure-related complications, risk stratification, and management of complications.
5. Be competent in proper positioning of the duodenoscope and the maneuvers that facilitate successful cannulation of the bile duct and pancreatic duct.
6. Understand low-pressure injection of contrasts.
7. Understand the various maneuvers to optimize fluoroscopic images.
8. Interpret and record the endoscopic and radiological findings.
Knowledge of the common features of cholangiography in biliary disorders
1. Normal anatomy and common anatomic variations
2. Diagnosis of biliary stones
3. Features of benign and malignant strictures
4. Features and classification of choledochal cysts
5. Classification of Klatskin tumor
6. Features of primary sclerosing cholangitis and primary biliary cirrhosis
Knowledge of the common features of pancreatography in pancreatic disorders
1. Diagnosis of chronic pancreatitis
2. Features of pancreatic ductal adenocarcinoma
3. Features of various pancreatic cystic lesions
4. Features of pancreas divisum
5. Features of anomalous union of the pancreatobiliary duct
Knowledge of therapeutic ERCP
1. Biliary and pancreatic sphincterotomies
(1) Understand the indications of each sphincterotomy.
(2) Understand the risks and how to modify them.
(3) Practical competency for sphincterotomy technique
(4) Understand the complications and their management.
(5) Understand the indications and techniques for pre-cut sphincterotomy.
2. Bile duct stone management
(1) Understand the indications for stone removal using ERCP.
(2) Understand extraction techniques.
(3) Gain proficiency in stone removal tools and techniques.
(4) Understand the techniques of mechanical lithotripsy.
(5) Understand the complications during stone removal and their management.
3. Dilation
(1) Understand the indications for sphincter and stricture dilations.
(2) Gain proficiency in dilation tools and techniques.
(3) Understand the complications during and after dilation and their management.
4. Stent placement
(1) Understand the indications and risks of stent placement.
(2) Be knowledgeable on stent types, materials, sizes, and their relative strengths and weaknesses.
(3) Gain proficiency in stent placement tools and techniques.
(4) Understand the complications and their management.
EUS (OPTIONAL)
With the introduction of EUS and the technical progress over the past decade, the role of EUS in the diagnosis and treatment of GI tract lesions and lesions in its vicinity is constantly increasing. However, since there are a limited number of facilities that can perform EUS and much effort and time are required to become proficient in EUS, EUS is not a prerequisite during the 1-year GI fellowship program in Korea. The ASGE recommends that training on EUS should be provided to those who have completed at least 18 to 24 months of basic GI endoscopy training [27,28]. Although acquiring sufficient skills on advanced endoscopy, such as EUS, is not realistic considering the relatively short GI fellowship program currently employed in Korea, basic knowledge and understanding on EUS are fundamental in taking care of the patients as a GI specialist. Therefore, the KSGE recommends the following requirements to be met during the trainees’ endoscopy training program as a tool to facilitate understanding on the diagnostic and therapeutic role of endoscopy. The education and training guidelines of EUS are summarized in Table 5.
Training aims
Be able to insert the EUS after being fully aware of its structural differences from regular upper and lower endoscopes
Obtain adequate knowledge and fundamental concepts on basic EUS imaging, i.e., Doppler imaging and relationship between sound wave frequency and penetration depth
Know the characteristics of the different types of EUS and their applications
Understand the indications and contraindications of EUS
Understand the anatomy of the GI tract and its surrounding structures using images obtained from the different types of EUS, and differentiate the normal anatomy, anatomical variation, and abnormal findings
Training details
Staging of malignant tumors of the upper and lower GI tract
1. Describe the invasion depth of the tumor.
2. Discern the presence of lymph node metastasis.
3. Differentiate the lesion from surrounding structures, and determine the presence of invasion to the surrounding structures.
Evaluation of subepithelial lesions (SELs) in the GI tract
1. Distinguish the layer from which the SELs originate.
2. Differentiate SELs according their EUS characteristics, i.e., echogenicity, size, margin, and heterogenicity.
Evaluation of pancreaticobiliary lesions
1. Differentiate various types of pancreatic cysts.
2. Assess the involvement of surrounding structures based on the mass lesion and its associated findings.
3. Evaluate the presence of stones or polyps/masses in the bile duct and gallbladder.
4. Know the different types of diagnostic and therapeutic procedures that can be performed by EUS, i.e., EUS- fine needle aspiration (FNA), celiac plexus neurolysis, pseudocyst drainage, necrosectomy, and tumor ablation.
5. Understand the indications, contraindications, and complications related to EUS intervention.
ENDOSCOPIC QUALITY CONTROL AND REPROCESSING (ESSENTIAL)
GI endoscopic procedures are not only dependent on the performance of individual endoscopists, but can also be influenced by the quality control of endoscopic equipment and facilities. Therefore, it is important to abide by the guidelines on endoscopic quality control and endoscope reprocessing for efficient endoscopic procedures [29,30]. It is well known that the result of endoscopic procedures is likely to be suboptimal when the procedure is performed by an individual who is not fully trained.
In Korea, an endoscopic quality assessment program was established in 2009, which was demonstrated to improve the efficiency of endoscopic procedures by raising recognition of continuous quality control among endoscopists [31]. All trainees should fully recognize the purpose of training and importance of quality control, apply the concept into their daily practice, determine the drawbacks of the current system, and improve the quality of endoscopic procedures [32-34].
Reprocessing of endoscopic devices should be performed completely. In addition, all endoscopists should be able to educate the endoscope cleansing and disinfection guidelines by the KSGE and perform the process themselves [30]. All endoscopists should be able to perform all steps of endoscope reprocessing, which is composed of cleaning, disinfection, rinsing, and drying stages [35-37]. Reprocessing of endoscopic accessory equipment is also mandatory. It is recommended that all endoscopists should not only understand and comply with the endoscope cleaning and disinfection guidelines, but also actively participate in the endoscopic quality improvement program [38].
ASSESSMENT OF COMPETENCE
A GI endoscopic subspecialty trainee should satisfy a minimum number of procedures, as recommended by the KSGE, conducted under the supervision of a GI endoscopic education supervisor, meet the requirements of basic knowledge and clinical techniques of endoscopy, as defined in the self-evaluation form, and have a specialty to pass the qualification examination for the GI endoscopic subspecialty conducted by the KSGE. In each training hospital, competence is assessed via a direct observation of the clinical techniques of the trainee by an education supervisor, overall training evaluation by education officials, and case-based discussions.
CONCLUSIONS
Recently, all the GI endoscopic procedures have been widely performed as the public interest in early screening is growing with the advanced endoscopic diagnostic tools and therapeutic techniques. The KSGE has made a great effort to improve the quality of endoscopies and has rearranged the fundamental educational goals and guidelines for accurate and safe endoscopic procedures during fellowship training. The educational goals and guidelines for sedative endoscopies, EGD, and colonoscopy are mandatory, and those for ERCP and EUS are optional. A GI endoscopic subspecialty should obey the guidelines for quality management and disinfection and be able to educate that process. In the future, these educational goals for GI endoscopies should be modified and supplemented on the basis of the technological advancements of endoscopic instruments and techniques.
Notes
Conflicts of Interest: The authors have no financial conflicts of interest.