INTRODUCTION
Improving the quality of screening colonoscopy is key to detecting adenomas and preventing colorectal cancer. If polyps are found during screening colonoscopies, distinguishing between non-neoplastic and neoplastic lesions can improve the efficiency of the colonoscopy and reduce unnecessary resection. When a malignant lesion is encountered, prediction of the depth of invasion can help decide whether to perform endoscopic resection or surgery. To meet these clinical needs, image-enhanced endoscopy (IEE), including dye-assisted conventional chromoendoscopy and virtual chromoendoscopy, is continually evolving. In this review, we summarize the types and characteristics of existing IEE techniques and discuss the current clinical usefulness and future prospects of IEE.
DYE-ASSISTED CONVENTIONAL CHROMOENDOSCOPY
Conventional chromoendoscopy is a classical procedure that can be performed only with standard endoscopy. A pit, an orifice of the colonic crypt, is observed in the colonic mucosa and shows specific arrangements in different types of lesions, referred to as the pit pattern. The visualization of the pit pattern of the colonic mucosa can be enhanced by application of a dye.
Indigo carmine is the most widely used dye in conventional chromoendoscopy. It is a contrast dye that is not absorbed by the mucosal glands and that stains depressed areas, including mucosal pits and grooves. A diluted solution (0.1% to 0.5%) of indigo carmine is most often used. It can be sprayed directly onto the colonic mucosa through the working channel of the endoscope or with a dye-spray catheter.
Crystal violet is an absorptive dye that stains epithelial cells in the colonic mucosal glands, making the pit looks white after dyeing. It is generally used at a concentration of 0.05%. After spraying onto the colonic mucosa, staining takes 2ŌĆō3 minutes.
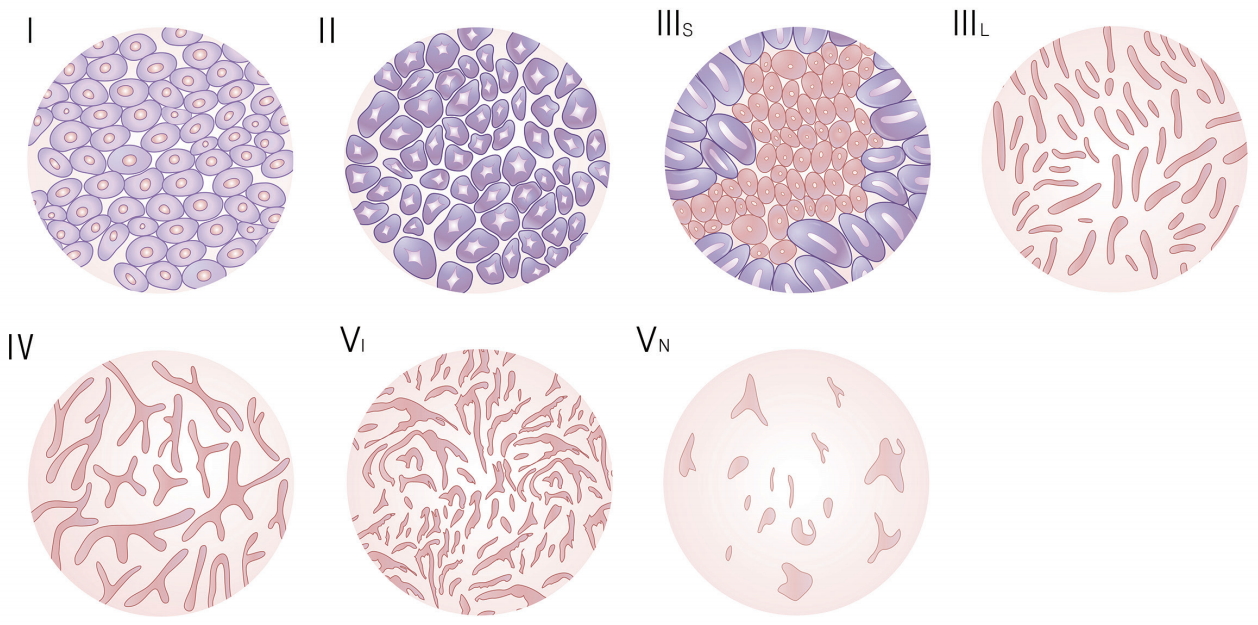
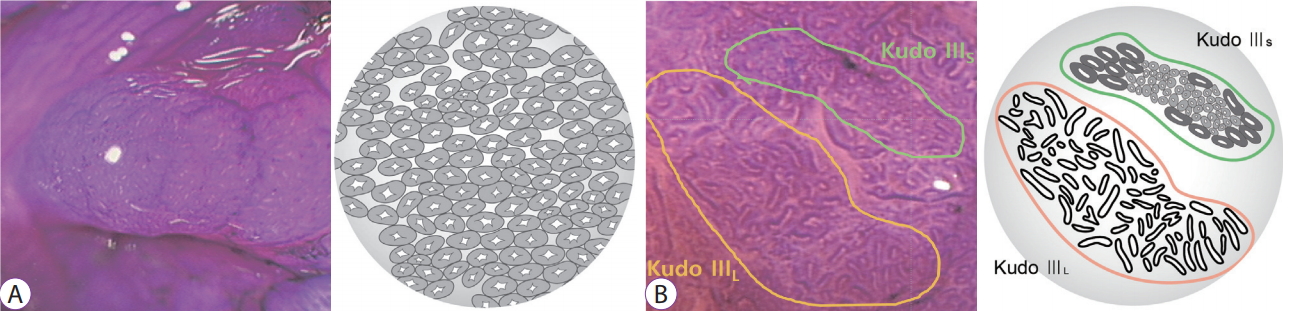
Pit-pattern characterization using a magnifying colonoscope follows KudoŌĆÖs classification [1]. This classification categorizes the pit pattern into six groups: types I, II, IIIL, IIIS, IV, and V (Fig. 1). Type I has pits of normal mucosa that are round and regular in size and arrangement. Type II has pits of hyperplastic polyps that are star-shaped or onion-like and regularly arranged. Types I and II are classified as non-neoplastic lesions. Types III and IV are classified as adenomatous lesions. Type IIIL shows elongated pits that usually reflect tubular adenoma with low-grade dysplasia. Type IIIS shows compactly arranged pits that are smaller than normal pits, indicating tubular adenoma with high-grade dysplasia or intramucosal cancer. Type IV has branched pits of villous adenoma. Type V is classified as a cancerous lesion and is divided into two subtypes: type VI (irregular) and type VN (non-structural). Type VI is observed in both invasive and non-invasive cancers, whereas type VN strongly suggests deep submucosal cancers. Thus, pit patterns are useful in assessing on the histological structures of a lesion (Fig. 2).
VIRTUAL CHROMOENDOSCOPY
Although conventional chromoendoscopy has advantages over standard colonoscopy, the procedure is more complicated than equipment-based virtual chromoendoscopy. Endoscopists can easily perform virtual chromoendoscopy through single-button operation. Virtual chromoendoscopy is used to observe the capillaries of the lesion and the mucosal epithelium of the microstructure.
Narrow-band imaging
The conventional red/green/blue gastrointestinal endoscope system has 3 broadband optical filters covering the visible wavelength range from 400 to 800 nm. The narrow-band imaging (NBI) system has two narrow-band illuminations of 415 nm and 540 nm using a special optical filter [2]. Because mucosal hemoglobin selectively absorbs 415-nm blue light, thin capillary vessels can be seen most clearly at this wavelength. On using this narrow spectrum, the contrast of the microvascular structure on the surface of the lesions is markedly improved [3].
Although pit pattern characterization was almost standardized by KudoŌĆÖs classification, there are a variety of NBI magnifying observation classifications for colorectal tumors.
In 2009, Sano et al. reported the first NBI classification of the capillary pattern (CP) using magnifying colonoscopy [4]. In SanoŌĆÖs classification, the CP is described as the arrangement of the meshed capillary surrounding a pit. CP was classified into three different types (CP types I, II, and IIIA/B). Assessment of CP by magnifying NBI is simple and reliable for differentiating colorectal non-neoplastic from colorectal neoplastic polyps, depending on the presence of meshed capillary vessels [4]. It has great accuracy in differentiating between low-grade dysplasia and high-grade dysplasia/invasive cancer depending on the regularity of the existing meshed capillary vessels [5]. Identification of CP types IIIA and IIIB is also useful for predicting the invasion depth of early colorectal neoplasms [6].
The Hiroshima classification, published in 2008, comprehensively evaluates both the pit-like surface pattern and CP on NBI magnifying endoscopy [7]. Types A, B and C are categorized according to the regularity of the surface pattern. Type C is subclassified into categories C1-C3 according to the heterogeneity of the vascular diameter and distribution. The positive predictive value of type C3 for the diagnosis of carcinomas with massive submucosal invasion was 100%.
The Showa classification, proposed in 2009, is a more intuitive classification that is based on morphological characteristics [8]. This classification includes a total of 6 categories: normal, faint, network, dense, irregular, and sparse patterns. Irregular and sparse patterns are presumed to suggest massively invasive submucosal cancer.
The NBI International Colorectal Endoscopic (NICE) classification was proposed in 2009 as a simple international NBI endoscopic classification for colorectal tumors (Table 1). The NICE classification is based on the color, vessels, and surface pattern of the colorectal tumors observed on non-magnifying endoscopy. International validation studies have demonstrated the usefulness of the NICE classification in diagnosing colorectal polyp histology and predicting deep submucosal invasion of carcinomas [9,10]. The Japan NBI Expert Team classification was proposed in 2014 after selected NBI specialists reached a consensus on establishing a universal NBI magnifying endoscopic classification (Table 2) [11].
Fuji intelligent color enhancement, blue light imaging, and linked color imaging
Fuji intelligent color enhancement (FICE) is a computed spectral estimation technology that emphasizes subtle mucosal changes through reconstruction of certain wavelengths. Unlike NBI, it has a processing system instead of optical filter for adjusting wavelength. FICE can process the captured images according to the most appropriate wavelength for examination. However, most prospective randomized studies failed to demonstrate that FICE improves the adenoma detection rate (ADR) or miss rate in comparison with white light endoscopy (WLE) [12-14].
Blue light imaging (BLI) is a new IEE system released by Fujifilm [15,16]. It focuses on the characteristics of short wavelength absorption of hemoglobin (at 410 nm) combined with specific white light spectral colors. It uses a new high-performance 4-LED multi-light system as the light source instead of xenon light. This system generates brighter images than those obtained on using xenon light, which enhances the visibility of both the microvascular and superficial mucosal patterns. Therefore, mucosal surface images become clearer.
Linked color imaging (LCI) was developed on the basis of the BLI technique. Although BLI has brighter endoscopic views than xenon-lamp-based IEE, the images are still darker than those obtained from white light imaging (WLI), which can result in low diagnostic rates. To overcome this, LCI utilizes additional red-wavelength information compared with BLI [17]. Therefore, LCI is able to produce images of sufficient brightness and that are similar to those produced by WLI. Furthermore, LCI enhances the differences in the red color spectrum because the increased contrast in red color leads to lesions being more easily identified under endoscopy. A red color discovered in purple color is the key finding for detection.
i-Scan
i-Scan uses a post-processing filter technology similar to that of FICE. It generates high-definition images using three image enhancement modes: contrast enhancement, surface enhancement, and tone enhancement. The study results of i-Scan are conflicting. Of two randomized prospective studies, one reported that high-definition colonoscopy with i-Scan is better than standard video colonoscopy in detecting colorectal neoplastic lesions [18], whereas the other demonstrated that i-Scan did not improve the ADR and failed to prevent missed polyps compared with high-definition WLE [18,19].
CLINICAL APPLICATIONS OF IEE
Detection of colorectal polyps
Dye-assisted conventional chromoendoscopy may increase the detection of colorectal polyps. In a systematic review and meta-analysis including seven randomized controlled trials comparing polyp detection in patients assigned to white light colonoscopy or dye-assisted chromoendoscopy, dye-assisted chromoendoscopy was significantly preferred for all detection outcomes [20]. However, pancolonic chromoendoscopy takes much more time and effort. Considering that the mean withdrawal times were much longer in the chromoendoscopy group than in the WLE group, the improvement in the polyp detection rate (PDR) may be because of the increased observation time rather than the dye [21]. Thus, pancolonic chromoendoscopy might not be beneficial for routine application.
Virtual chromoendoscopy also showed no definite benefits in the detection of colorectal polyps or adenomas. Several meta-analyses comparing NBI with WLE in the detection of colorectal adenomas showed there was no significant difference in ADR between these two modalities [22-26]. FICE/i-Scan also demonstrated no benefit over WLE in a meta-analysis including five randomized studies [26].
The novel NBI system with near focus might be better for polyp and adenoma detection. This new generation NBI using the 190 (Exera) or 290 (Lucera) system provides two-fold brighter images in full high-definition, compared with the old version [27]. This new NBI showed significantly increased ADR and PDR compared with high-definition WLE [28].
There are limited studies on BLI and LCI because these modalities were only recently released. In one study, BLI bright mode was found to improve the visibility of colonic lesions compared to that on WLI [29]. In addition, colonoscopies using BLI resulted in lower colon adenoma miss rates than those using WLI in a recent randomized tandem trial [30]. LCI increases the visibility of flat lesions such as sessile serrated polyps and improves the detection rate of these types of lesions [31].
Polyp characterization
As previously stated, NBI differentiates neoplastic and non-neoplastic polyps by enhancing mucosal vasculature and surface patterns. FICE and i-Scan also emphasize the mucosal pattern of polyps by reconstructing images at different wavelengths using spectral estimation technology. Meta-analysis proved that these three endoscopic imaging techniques have reliable rates of sensitivity, specificity, and negative predictivity in the differentiation of non-neoplastic and neoplastic colorectal lesions when they are used by appropriately trained endoscopists [32]. These results have enabled endoscopists to speculate the histopathological type of colorectal polyps in vivo and allowed them to discard diminutive polyps after resection, reducing the costs of histological analysis [33].
The diagnostic effectiveness of BLI magnification for the diagnosis of colorectal neoplasms is comparable to that of NBI magnification [34].
Prediction of the depth of invasion
With the recent rapid development of endoscopic treatments, endoscopic submucosal dissection (ESD) has become an important minimally invasive treatment for early colorectal cancer [35]. To decide whether to perform surgery or ESD, it is essential to make an accurate endoscopic prediction of the depth of invasion.
As stated earlier in this review, IEE can also help predict the invasion depth of colorectal cancer. Magnifying chromoendoscopy with crystal violet or indigo carmine can identify the neoplastic invasive pattern, which is defined as KudoŌĆÖs type VI with a demarcated area and type VN [36]. Determination of an invasive pattern by this method is highly effective in differentiating superficial or intramucosal submucosal cancers (<1,000 ╬╝m) from deep submucosal cancers (Ōēź1,000 ╬╝m). Variable classifications of NBI can also predict the depth of invasion (Fig. 3). We have summarized the criteria for deep submucosal cancer by IEE in Table 3.
On the basis of the capability of predicting the invasiveness of colonic lesions by IEE, a three-step strategy for management of these lesions has been suggested (Fig. 4) [37]. The first step is to identify the lesion by conventional colonoscopy. The second step is to observe capillary and surface patterns of the identified lesion by NBI. The third step is to examine the pit pattern of the lesion by dye-assisted chromoendoscopy.
LCI high-magnification colonoscopy combined with crystal violet staining is expected to enhance the accuracy of endoscopic prediction of invasion depth in early-stage colorectal cancer [38].
CONCLUSIONS
Colorectal cancer screening programs are increasing worldwide, increasing the importance of high-quality colonoscopies. IEE plays distinctive roles in the histologic characterization of colorectal polyps and prediction of the invasion depth of colorectal cancers. The latest advancements in IEE, such as new-generation NBI, BLI, or LCI, have the potential for increasing ADR and PDR in screening colonoscopy. More robust and rigorous clinical trials must be conducted to support the routine use of IEE for screening average-risk populations. In addition, efforts to educate and train community-based gastroenterologists who are not familiar with IEE on the IEE technique should be continued.