INTRODUCTION
Common bile duct (CBD) stones can cause complications such as pain, partial to complete obstruction that leads to obstructive jaundice, cholangitis, hepatic abscess, pancreatitis, secondary biliary cirrhosis, and sepsis [1]. Findings from the GallRiks study suggest that efforts should be made to clear the bile duct, because leaving the CBD stone ultimately leads to unfavorable outcomes [2].
Endoscopic retrograde cholangiopancreatography (ERCP) has been the treatment of choice for the management of CBD stones. However, in patients with surgically altered anatomy, ERCP may not be feasible because the ampulla of Vater cannot be reached [3,4]. Percutaneous transhepatic cholangioscopy and lithotripsy can be used to treat these cases. However, in cases with normal or minimal intrahepatic duct (IHD) dilatation, the percutaneous transhepatic approach is technically difficult and carries a high risk of complications [4-6].
We present the case of a patient with a distal CBD stone measuring 2 cm successfully removed by percutaneous transcholecystic cholangioscopy (PTCC).
CASE REPORT
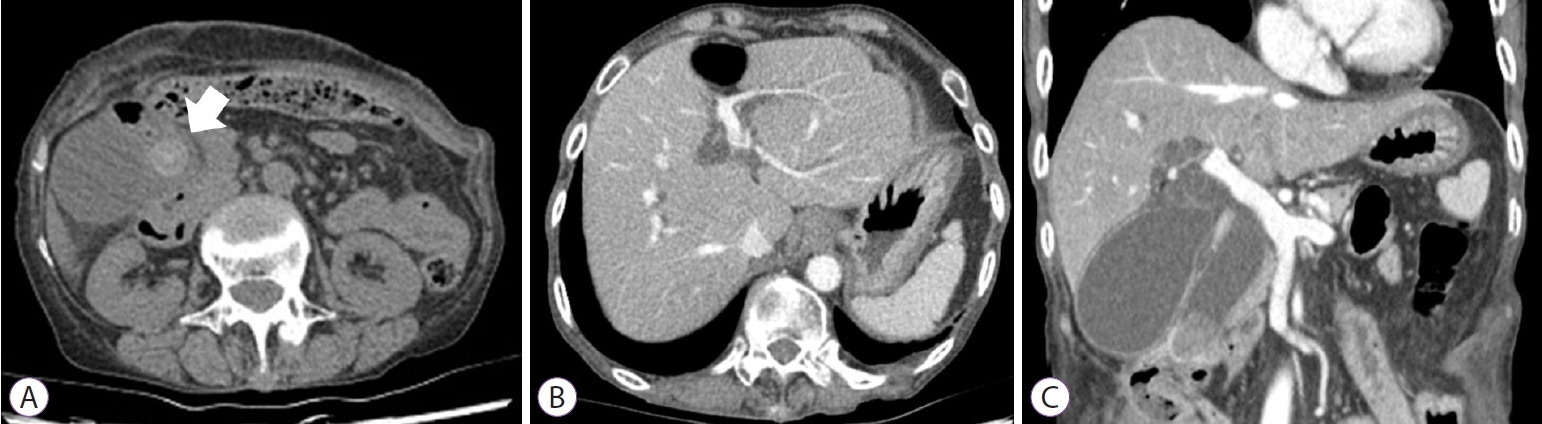
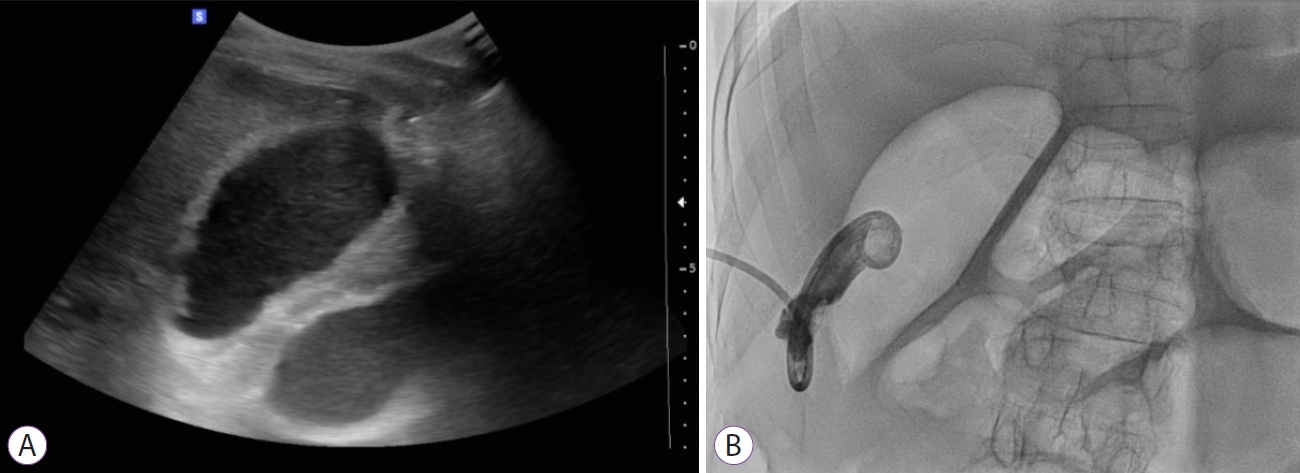
A 64-year-old woman visited the emergency department with a chief complaint of epigastric pain over the last three days. She was diagnosed with BehУЇetтs disease in 1983. In 1984, she underwent ileocecectomy due to intestinal obstruction and in 1993, she underwent colo-duodenal fistulectomy, gastrojejunostomy, and transverse colon segmental resection and anastomosis due to colo-duodenal fistula. The patientтs abdomen was non-tender, soft, flat, and had normoactive bowel sounds. Her initial blood pressure was 79/49 mm Hg, pulse rate was 129 times/min, respiratory rate was 20 times/min, and body temperature was 38.2ТАC. Her laboratory test results were as follows: white blood cell count, 10,280/mm3; serum hemoglobin, 12.8 g/dL; aspartate transaminase, 268 U/L; alanine transaminase, 679 U/L; alkaline phosphatase, 180 U/L; gamma-glutamyl transpeptidase, 180 U/L; total bilirubin, 4.3 mg/dL; blood urea nitrogen/creatinine, 8/0.4 mg/dL; C-reactive protein, 3.8 mg/dL. Abdominal computed tomography showed a radiopaque stone measuring 2 cm at the distal end of the CBD, marked dilatation of the upstream CBD, and several gallstones in the distended gallbladder. There was no definite evidence of acute cholecystitis (Fig. 1). Intravenous fluid support and empirical antimicrobial therapy, including ceftriaxone and metronidazole, were initiated immediately. Considering her hemodynamic instability and surgically altered anatomy, we planned percutaneous drainage instead of an endoscopic approach. We planned to gain percutaneous transhepatic biliary access, but the IHDs were not sufficiently dilated to insert a drainage catheter. Therefore, percutaneous cholecystostomy was performed with an 8.5 Fr Dawson-Mueller drainage catheter (Cook Medical, Bloomington, IN, USA) (Fig. 2). Two days after the procedure, when the patient improved clinically, ERCP was attempted. However, we failed to identify the ampulla of Vater due to the previous gastrojejunostomy.
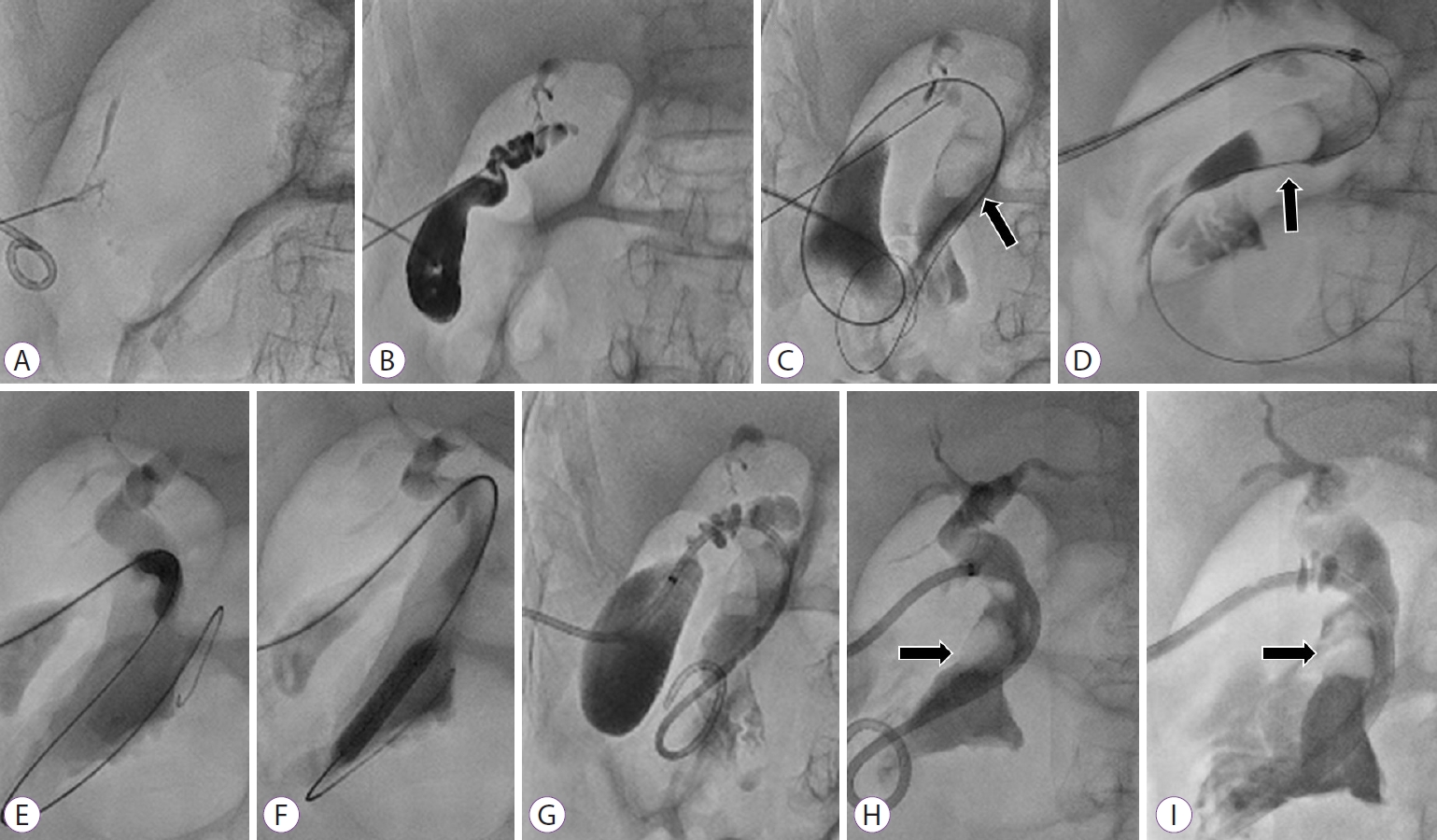
We made a second attempt to gain percutaneous transhepatic biliary access, but this was not feasible because IHDs were not dilated (Fig. 3A). Therefore, we proceeded with fluoroscopy-guided CBD stone removal via cholecystostomy. Kumpe catheters and guidewire (Cook Medical) were used to navigate the cystic duct and CBD (Fig. 3B, C). We inserted an 8.5 Fr tube (Cook Medical) through the cystic duct, CBD, to the duodenum (Fig. 3D). Partial stone removal was performed with a basket and balloon. The space between the remaining stone and the CBD wall was too little and the stone could not be grasped with the basket; thus, a large stone remained in the CBD (Fig. 3E-G). A 12 Fr tube (Cook Medical) was left behind (Fig. 3H).
The patient was bedridden at that time and had multiple abdominal surgeries, so we reserved surgery as our last option. We dilated the tract by using an 18 Fr percutaneous transhepatic cholangioscopy tube (Sumitomo Bakelite Co., Ltd., Tokyo, Japan) one week later (Fig. 3I). Percutaneous transcholecystic cholangioscopic (CHF-V; Olympus Optical Co., Tokyo, Japan) removal of the CBD stone was performed by fragmentation of the stone with the aid of electrohydraulic lithotripsy (EHL) and saline flushing of the debris (Fig. 4A-C). Follow-up cholangiography showed good flow of contrast medium to the duodenum, and abdominal computed tomography confirmed absence of residual radiopaque CBD stones (Fig. 4D-F). Tube removal was performed three days after clamping, and the patient was discharged.
DISCUSSION
ERCP is the gold standard for removing CBD stones, but it is not always successful, especially in certain situations such as patients with surgically altered anatomy. When ERCP is not feasible, percutaneous transhepatic biliary access is commonly used to remove CBD stones in surgically unfit patients. However, some patients with CBD stones have minimal or no dilatation of the IHDs, and percutaneous transhepatic biliary drainage is technically demanding and risky. In such circumstances, the transcholecystic approach can be an alternative but data on transcholecystic cholangioscopic removal of CBD stones are scarce.
In general, cholangioscopy allows direct visualization of the CBD stone and uses various tools, such as EHL, making it easier and safer to break down the stone. However, cholangioscopy is traditionally performed through the transhepatic tract rather than the transcholecystic tract since it requires overcoming additional obstacles such as gallstones and a tortuous cystic duct with spiral valves of Heister [7]. There is also a risk of cystic duct rupture during the procedure because it usually has a narrow and serpentine course. The diameter of the normal cystic ducts is only 1 mm to 5 mm, while the outer diameters of cholangioscopes are around 5 mm [8]. The passage of baskets, forceps, and cholangioscopes during fragmentation of stones using EHL might cause injury and even rupture of the cystic duct, leading to an emergency operation. For these reasons, there have only been a few reports on transcholecystic cholangioscopic CBD stone removal.
Likewise, interventional radiologists have not commonly used the percutaneous transcholecystic approach in fluoroscopy-guided CBD stone removal. However, a recent retrospective study including 114 patients who underwent percutaneous transcholecystic removal of CBD stones reported encouraging results, suggesting that it might be a technically safe, feasible, and effective procedure [5]. In that study, percutaneous cholecystostomy was chosen over percutaneous transhepatic biliary drainage because of a lack of non-dilated IHDs (n=90) or combined acute cholecystitis (n=24). When performed by two expert interventional radiologists, the technical success rate was 84.2%, and there were no major procedure-related complications even with the use of large-bore catheters. The most common reason for technical failure was unsuccessful cystic duct cannulation (61.1%), followed by proximal migration (16.7%) and multiplicity of CBD stones (16.7%). In this study, acute cholecystitis accompanied 50% of all cases, contributing to the failure of cystic duct cannulation. However, in our case, the cystic duct was not obstructed but somewhat slightly dilated due to distal CBD obstruction, resulting in a more comfortable and safer cannulation of the cystic duct.
Nevertheless, only partial stone removal was possible radiographically because the stone was too large and compact, and further definitive treatment was needed. Because our patient was unfit for surgery, PTCC was the only alternative. Based on the safety profile of the transcholecystic approach suggested by previous studies, our team decided to perform PTCC, which was successful. Finally, the cholangioscope was safely passed through the dilated cystic duct, and the remaining CBD stone was successfully removed without acute complications.
In summary, we report a case of successful CBD stone removal with PTCC in a surgically high-risk patient. The patient had previously undergone gastro-jejunostomy, which made ERCP impossible. Dilatation of IHDs was insufficient, so percutaneous transhepatic biliary access was not possible. The fluoroscopy-guided transcholecystic approach could not remove the stone because the stone was too big and compact. The stone was successfully removed using PTCC and EHL. This case presents a practical alternative to managing CBD stones using cholangioscopy in patients who do not have IHD dilatation, or who already have a percutaneous cholecystostomy tract due to acute cholecystitis. However, a multidisciplinary teamтs judicious decision is required when attempting this procedure because its safety and efficacy are not yet fully established.