The most common complication of laparoscopic cholecystectomy is iatrogenic perforation of the gallbladder, with gallstone spillage into the abdominal cavity. Also known as тdropped gallstonesт, this complication occurs in up to 30% of patients, but is clinically silent in the majority of cases.1 If symptoms arise, they are generally related to the complications of dropped gallstones such as abscess and fistulae formation, which often lead to significant morbidity.2,3 The most common location for abscess formation secondary to dropped gallstones is the subhepatic space, more specifically known as Morrisonтs pouch.4 The time from spillage of gallstones to abscess formation ranges from 5 days up to 5 years.4,5 Development of inflammatory masses resembling tumors, abdominal wall abscesses, and pleural empyema have also been reported as alternative presentations.1,5 Diagnosis of dropped gallstones is a challenge since majority of gallstones are radio-lucent on computed tomography (CT) and they have the propensity to migrate to different locations.2 Definitive treatment of dropped gallstones is often limited to laparotomy, since laparoscopic retrieval could be technically challenging. Both approaches expose patients to additional morbidity if they are surgical candidates.6
Herein, we report the technique and a patient who underwent laparoscopic cholecystectomy complicated by dropped gallstones leading to abscess formation and fistula development. Percutaneous endoscopy was utilized to visualize the dropped gallstones, which were then lithotripsied by bipolar electrohydraulic lithotripsy and retrieved using baskets. A 76-year-old female patient with a past medical history of congestive heart failure, type 2 diabetes mellitus, hypertension, and a body mass index of 77 was diagnosed with acute cholecystitis. The patient underwent a technically challenging cholecystectomy that required extensive lysis of adhesions and was complicated by spillage of the gallbladder contents. A surgical drain was placed in the gallbladder fossa. However, follow-up CT images 1 week later revealed an ovoid-shaped fluid collection of 8.6У5.0 cm in the surgical bed/gallbladder fossa (Fig. 1A). The patient was referred to interventional radiology for image-guided drainage of fluid collection.
Persistent abdominal pain, high drain output, and onset of unexplained diarrhea raised concerns of possible fistula development. A follow-up CT scan of the abdomen and pelvis revealed a retained gallstone at the cystic stump remnant, multiple dropped gallstones in the gallbladder fossa along the inferomedial edge of the right hepatic lobe, and an abscess (Fig. 1B).
Sinography through the gallbladder fossa drain opacified the cystic duct, common bile duct, and small bowel. In addition, multiple stones in the gallbladder fossa and a large stone at the cystic duct stump were visualized (Fig. 2A). Cone-beam CT confirmed the presence of multiple dropped gallstones (Fig. 2B), and suggested the possibility of fistulous tracts from the gallbladder fossa to the small bowel and colon.
After serial dilatation of the indwelling drain track to accommodate a 16-French (Fr) drain (Cook Medical, Bloomington, IN, USA), the patient returned for percutaneous endoscopy, lithotripsy, and lithotomy one month later. The indwelling 16-Fr drain was exchanged over a 0.035 inch 75 cm Amplatz wire (Boston Scientific, Marlborough, MA, USA) for a 16-Fr peel-away sheath (Cook Medical). A percutaneous endoscope (SpyGlass Discover; Boston Scientific) was introduced into the gallbladder fossa through a 16-Fr peel-away sheath (Fig. 3A). Intermittent normal saline irrigation was connected through the working channel of the percutaneous endoscope using the Klein Pump (HK Surgical Inc., San Clemente, CA, USA) set at a rate of 400 to 600 mL/min while a persistent low-pressure suction was connected to the other channel. However, subhepatic endoscopy was limited by the contracted space and multiple packed gallstones. A combination of fluoroscopy and direct visualization was utilized to guide a 1.9-Fr bipolar electrohydraulic lithotripsy probe (Autolith Touch Biliary EHL System; Boston Scientific) (Fig. 3B) through the working channel of the percutaneous endoscope.
Direct visualization and fragmentation of large gallstones was done using the lithotripsy system (Fig. 3C, Supplementary Video 1) with a voltage of 5 to 10 Watts. A 1 cm basket (NCompass Nitinol stone extractor; Cook Medical) was subsequently used to remove stones through the sheath (Fig. 3D). Completion cholangioscopy and cholangiography demonstrated numerous large residual gallstones in the gallbladder fossa, some of which appear more fragmented compared to initial imaging. The percutaneous endoscope and sheaths were removed, and a new 14-Fr drain (Cook Medical) was placed. The patient remained hospitalized and underwent two additional similar treatment sessions, one week apart. One week after the third session, contrast injection through the gallbladder fossa drain revealed no residual calculi and resolution of both duodenal and colonic fistulae. The drain was subsequently downsized to a 10-Fr destringed drain (MAC-LOC drain; Cook Medical), which was gradually withdrawn over three consecutive days as minimal drainage was observed. The drain was eventually removed, and the patient was discharged uneventfully 17 days after initial diagnosis.
Percutaneous peritonoscopy (SpyGlass Discover) in combination with bipolar electrohydraulic lithotripsy and use of retrieval baskets was able to successfully visualize and retrieve intraabdominal dropped gallstones. Ultimately, this approach helped resolve abscess and bowel fistulae which were a consequence of dropped gallstones after cholecystectomy.
Interventional radiologists have been removing gallstones since 1973.7 However, it was not until 1992 that the use of percutaneous endoscopy and electromagnetic lithotripsy was evaluated in 58 patients, achieving a success rate of 96%.8 This result compared favorably to extracorporeal shockwave lithotripsy; which resulted in recurrent cholelithiasis in 70% patients, and medical therapy; which resulted in recurrent cholelithiasis in 50% to 70% of patients.9 In the intervening years, percutaneous endoscopy has been widely accepted as a safe and effective modality for gallstone retrieval in patients with cholecystitis and contraindications for cholecystectomy,8 but has not been utilized to facilitate removal of dropped gallstones.
Previous studies have evaluated the use of percutaneous endoscopy and lithotripsy in patients with symptomatic cholelithiasis, reporting a mean of 1.2 sessions for 100% retrieval of gallstones.9 Another retrospective study of 323 patients reported a 93% to 100% technical success rates for cholecystoscopy and lithotripsy.10 The most common cause of technical failure was the presence of a stone lodged within the cystic duct. The complication rate was reported from 2.5% to 14%.10 Bile leak was the most frequently observed peri-procedural complication.10 Less common complications included acute pancreatitis, bleeding, perforation of the gallbladder wall, and transient cholangitis.10
Before introduction of percutaneous endoscopy, a majority of patients who are ineligible for cholecystectomy were dependent on placement of permanent cholecystostomy tubes.10 However, the introduction of cholecystoscopy and lithotripsy will allow successful removal of cholecystostomy tubes in patients with contraindications to cholecystectomy.11
Adding to the existing data on the application of percutaneous endoscopy and lithotripsy, we present the successful utilization of percutaneous endoscopy for visualization and a combination of bipolar electrohydraulic lithotripsy and retrieval baskets for removal of dropped gallstones. Dropped gallstones can increase risk of morbidity and mortality in this population, even years after surgery.12 The patient under study successfully underwent three sessions of percutaneous endoscopy and lithotripsy for retrieval of multiple large dropped gallstones. Moreover, lithotripsy and removal of retained cystic duct stones and dropped gallstones helped resolve fistulous tracts from the gallbladder fossa to the small and large bowel, patientтs pain, and diarrhea. At the conclusion of hospitalization, the patient was deemed symptom-free and tube-free.
Image-guided percutaneous endoscopy with lithotripsy and retrieval baskets could be used as an alternative to open surgery in the retrieval of dropped gallstones. In addition, this procedure is able to address complications associated with dropped gallstones. Future studies could assess the safety, efficacy and cost effectiveness of this technique to further delineate the role of this approach compared to open surgery in the treatment of dropped gallstones.
Supplementary MaterialSupplementary Video 1. Cholelithotripsy under direct video assisted visualization by Spyglass Discover percutaneous endoscope (https://doi.org/10.5946/ce.2021.278.v001). Supplementary materials related to this article can be found online at https://doi.org/10.5946/ce.2021.278.
NOTESFig.Т 1.(A) Coronal computed tomography (CT) image of abdomen demonstrates a collection (arrow) in the gallbladder fossa. (B) Follow-up CT image shows a persistent collection with multiple dropped stones (arrow) abutting the lower and medial edge of the right hepatic lobe. 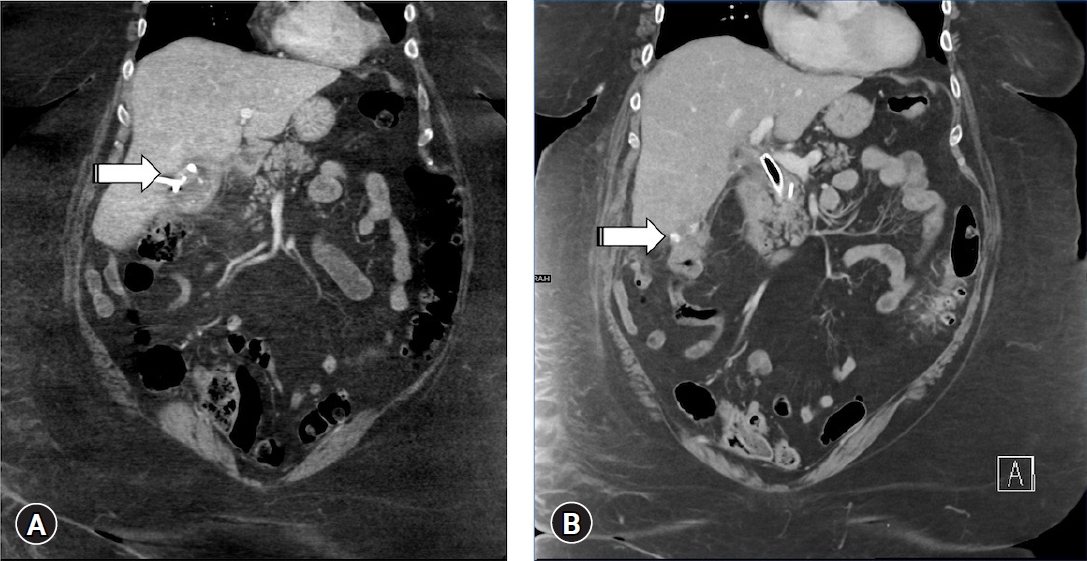
Fig.Т 2.(A) Contrast injection through the existing tube demonstrates multiple dropped gallstones (white arrow) in the gallbladder fossa and along the right hepatic lobe, a stone in the residual gallbladder neck (black arrow), patent cystic duct (white arrowhead) draining into the common bile duct, and a fistula from the gallbladder fossa to the ascending colon. (B) Cone-beam computed tomography demonstrates multiple dropped gallstones (white arrow) in the gallbladder fossa and along the right hepatic lobe and the stone in the residual gallbladder neck (black arrow). 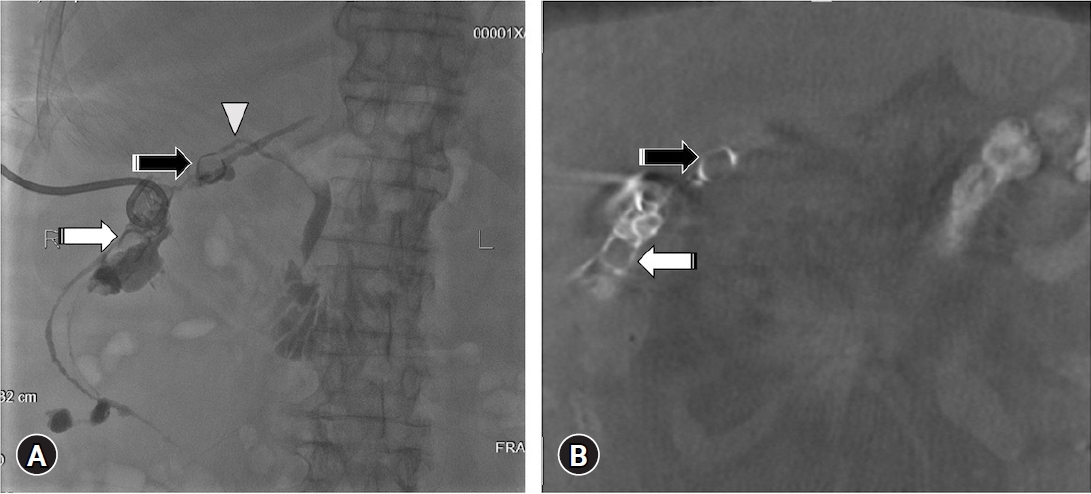
Fig.Т 3.(A) The Spyglass Discover percutaneous endoscope was used to visualize the gallstones percutaneously, while a bipolar electrohydraulic lithotripsy system (B, C) was used for lithotripsy. (D) Fragments of gallstones lithotripsied by bipolar electrohydraulic lithotripsy system, retrieved by a 1 cm basket. 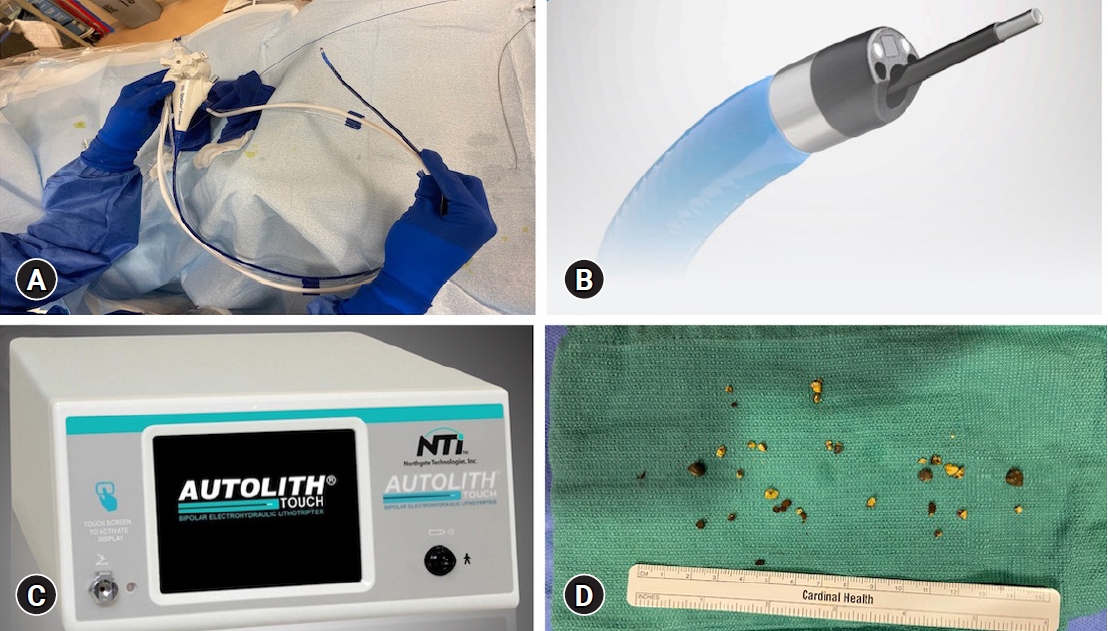
REFERENCES1. Casillas S, Kittur DS. Late abscess formation after spilled gallstones masquerading as a liver mass. Surg Endosc 2003;17:833.
2. Jabbari Nooghabi A, Hassanpour M, Jangjoo A. Consequences of lost gallstones during laparoscopic cholecystectomy: a review article. Surg Laparosc Endosc Percutan Tech 2016;26:183т192.
3. Nayak L, Menias CO, Gayer G. Dropped gallstones: spectrum of imaging findings, complications and diagnostic pitfalls. Br J Radiol 2013;86:20120588.
4. Singh AK, Levenson RB, Gervais DA, et al. Dropped gallstones and surgical clips after cholecystectomy: CT assessment. J Comput Assist Tomogr 2007;31:758т762.
5. McPherson I, McSorley ST, Cannings E, et al. Dropped gallstones causing abdominal wall abscess and pleural empyema: a case series. Scott Med J 2019;64:67т70.
6. Kafadar MT, Cetinkaya I, Aday U, et al. Acute abdomen due to spilled gallstones: a diagnostic dilemma 10 years after laparoscopic cholecystectomy. J Surg Case Rep 2020;2020:rjaa275.
7. Burhenne HJ. Nonoperative retained biliary tract stone extraction: a new roentgenologic technique. Am J Roentgenol Radium Ther Nucl Med 1973;117:388т399.
8. Ohashi S. Percutaneous transhepatic cholecystoscopic lithotomy in the management of acute cholecystitis caused by gallbladder stones. Diagn Ther Endosc 1998;5:19т29.
9. Patel N, Chick JF, Gemmete JJ, et al. Interventional radiology-operated cholecystoscopy for the management of symptomatic cholelithiasis: approach, technical success, safety, and clinical outcomes. AJR Am J Roentgenol 2018;210:1164т1171.
10. Kim SK, Mani NB, Darcy MD, et al. Percutaneous cholecystolithotomy using cholecystoscopy. Tech Vasc Interv Radiol 2019;22:139т148.
|
|
|||||||||||||||||||||||||||||||||||||||||
