CME for
KSGE members
Hong, Park, and Baek: Rare cause of granulomatous enteritis
Quiz
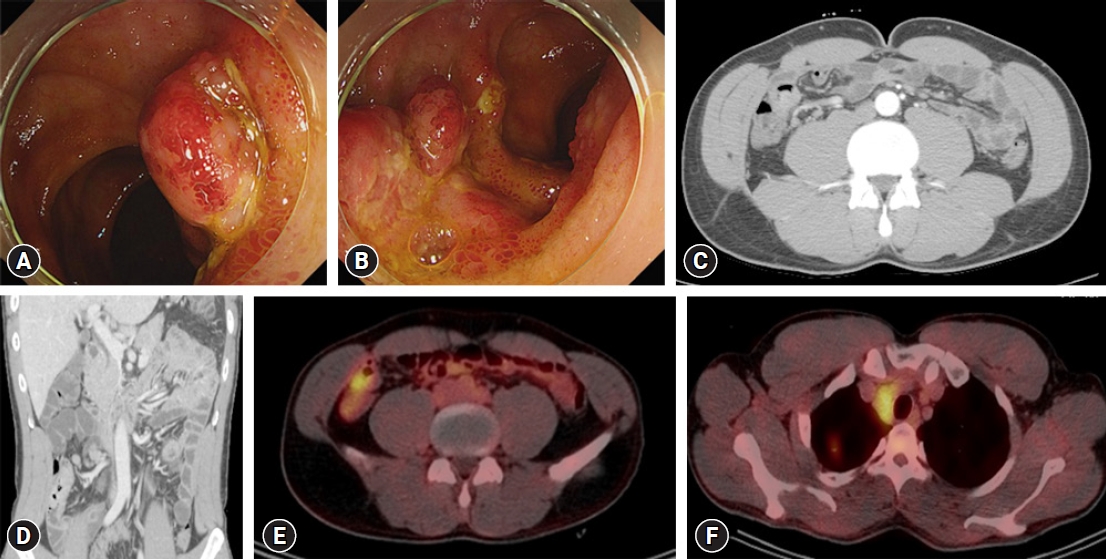
A 42-year-old man was referred to our department for the evaluation of multiple polypoid masses with ulcers and hyperemia in the terminal ileum (TI), which was incidentally detected on screening colonoscopy ( Fig. 1A, B). The patient had no relevant medical, surgical, or family history. He had no abdominal symptoms, such as nausea, vomiting, diarrhea, or abdominal pain. Physical examination results were unremarkable. Initial laboratory test results, including routine blood tests, liver function tests, carcinoembryonic antigens, and inflammatory markers, were within normal ranges. Both tuberculosis-stimulating specific antigen (interferon-╬│) and tuberculin skin tests were negative. Stool studies were negative for ova, parasites, Gram staining, and culture. Examination of the ileocolonoscopic biopsy specimen revealed noncaseating granulomatous inflammation. Contrast-enhanced abdominal computed tomography revealed a polypoid mass in the TI with marked enhancement ( Fig. 1C). Regional lymph node enlargement was also observed ( Fig. 1D). Positron emission tomography revealed increased fluorodeoxyglucose uptake in the TI and regional lymph nodes ( Fig. 1E). Increased fluorodeoxyglucose uptake was also observed in the right upper lobe and mediastinal lymph nodes ( Fig. 1F). Based on this information, what is the most likely diagnosis?
Answer 
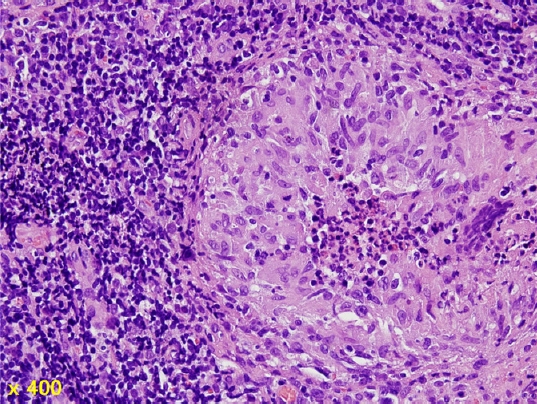
Video-assisted thoracic wedge resection of the right upper lobe with mediastinal lymph node dissection was performed ( Fig. 2). Histological examination revealed noncaseating granulomatous inflammation in the submucosal layer ( Fig. 3). These features were also observed in the mediastinal lymph nodes. ZiehlŌĆōNeelsen staining did not reveal acid-fast bacilli. No other organisms or foreign bodies have been detected. Finally, the patient was diagnosed with sarcoidosis involving the gastrointestinal tract. Sarcoidosis is an inflammatory disease of unknown etiology that invades various organs and is characterized by the formation of multiple noncaseating granulomas, resulting in structural damage and normal tissue dysfunction. 1 Since granulomas are not specific to sarcoidosis, they can be diagnosed only after excluding other diseases that can cause granuloma. Sarcoidosis can occur in all races and ages; it develops before the age of 50 years and has an incidence of 20 to 40 per 100,000 population. 2 Although sarcoidosis is continuously increasing in Korea, the incidence is 0.13 per 100,000 people, which is very low compared to other countries. Among them, 33% of patients in their 30s showed the highest age of onset, and women were found to be more affected (64.6%) in the sex comparison. 3
Sarcoidosis mainly affects organs, such as the lungs, skin, and lymph nodes, systemically, but can involve other organs in 30% to 50% of cases. 4 Gastrointestinal involvement is a rare extrathoracic involvement of sarcoidosis, with a frequency of approximately 5% to 10% in asymptomatic cases, and symptomatic cases are even rarer, reported at approximately 1%. 5-7 Although reported locations range from the esophagus to the rectum, the stomach is the most commonly involved part of the gastrointestinal tract. Small-bowel sarcoidosis is the rarest form of gastrointestinal sarcoidosis, with only a few cases reported in the literature. 8,9 No cases of small-bowel sarcoidosis have been reported in Korea. Gastrointestinal involvement is usually associated with concomitant pulmonary disease and is commonly asymptomatic. Several intestinal diseases should be routinely investigated and ruled out in patients with suspected small-bowel sarcoidosis, including inflammatory, infectious, and neoplastic diseases. In the present case, a noncaseating granuloma in the TI was observed on histological examination, and sarcoidosis was identified in the pulmonary and mediastinal areas. Serum calcium level was normal, but the angiotensin-converting enzyme level was elevated to 98 U/L (normal range, 8ŌĆō52 U/L). In summary, although ileal sarcoidosis is rare, it should be considered in the differential diagnosis of polypoid and ulcerative ileal lesions.
Fig.┬Ā1.
(A, B) Colonoscopy showing multiple polypoid masses with ulcers and hyperemia in the terminal ileum. (C, D) Contrast-enhanced abdominal computed tomography showing a polypoid mass in the terminal ileum with marked enhancement and enlargement of the regional lymph nodes. (E, F) Positron emission tomography scan showing increased fluorodeoxyglucose uptake in the terminal ileum, regional lymph nodes, right upper lobe, and mediastinal lymph nodes. 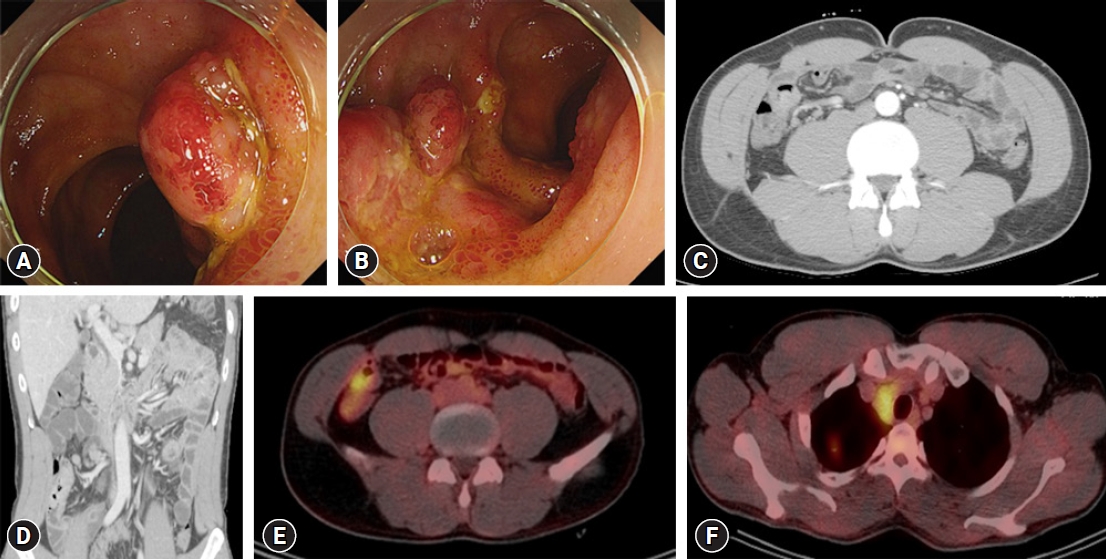
Fig.┬Ā2.
Video-assisted thoracic wedge resection of the right upper lobe with mediastinal lymph node dissection. (A) Diffused dense pleural adhesions and anthracotic pigmentation of parenchyma. (B) Pulmonary nodule of the right upper lobe and multiple enlarged conglomerated mediastinal lymph nodes. (C) Resected pulmonary nodule in the right upper lobe. 
Fig.┬Ā3.
Histopathological examination reveals noncaseating granulomatous inflammation in the submucosal layer (hematoxylin and eosin stain, ├Ś400). 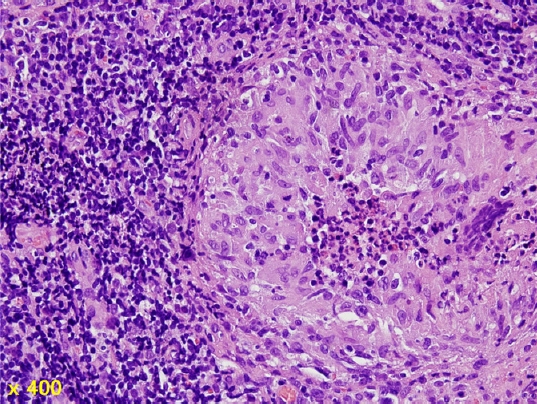
REFERENCES
1. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med 2007;357:2153ŌĆō2165.   2. Rybicki BA, Iannuzzi MC. Epidemiology of sarcoidosis: recent advances and future prospects. Semin Respir Crit Care Med 2007;28:22ŌĆō35.   3. Kim DS. Sarcoidosis in Korea: report of the Second Nationwide Survey. Sarcoidosis Vasc Diffuse Lung Dis 2001;18:176ŌĆō180.  4. Baughman RP, Teirstein AS, Judson MA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med 2001;164(10 Pt 1):1885ŌĆō1889.  5. Bulger K, O'Riordan M, Purdy S, O'Brien M, Lennon J. Gastrointestinal sarcoidosis resembling Crohn's disease. Am J Gastroenterol 1988;83:1415ŌĆō1417.  6. Veitch AM, Badger I. Sarcoidosis presenting as colonic polyposis: report of a case. Dis Colon Rectum 2004;47:937ŌĆō939.   7. Tobi M, Kobrin I, Ariel I. Rectal involvement in sarcoidosis. Dis Colon Rectum 1982;25:491ŌĆō493.  8. Ebert EC, Kierson M, Hagspiel KD. Gastrointestinal and hepatic manifestations of sarcoidosis. Am J Gastroenterol 2008;103:3184ŌĆō3192; quiz 3193.   9. Sprague R, Harper P, McClain S, Trainer T, Beeken W. Disseminated gastrointestinal sarcoidosis. Case report and review of the literature. Gastroenterology 1984;87:421ŌĆō425.  
|
|