A Case of Giant Lipoma Causing Chronic Recurrent Intussusception of the Colon
Article information
Abstract
Colonic lipomas, which often occur in elderly women, usually have small size and occur mainly in the cecum and ascending colon. Most colonic lipomas are asymptomatic and identified incidentally at the time of endoscopy or surgery. However, they may cause symptoms such as bleeding, obstruction or intussusception as their size increases. Intermittent episodes of intussusception are uncommon but may be caused by large pedunculated lipoma. In a 68-year-old woman suffering intermittent abdominal pain, 5.5×4.5×3.8-cm huge mass was found by colonoscopy at proximal ascending colon, which was intussuscepted to proximal transverse colon on abdominal computed tomography. Segmental right colonic resection was conducted. We report a case of symptomatic giant pedunculated colonic lipoma causing intussusception requiring surgical intervention, with a successful recovery after surgery.
INTRODUCTION
Most of colonic lipomas, which often occur in elderly wo-men, have small sizes and occur mainly in the cecum and ascending colon.1 Most of them are shown as single lesion but sometimes they are occurred in multiple lesions.2 The colonic lipoma is a common benign tumor of colon next to the hyperplastic and adenomatous polyps.3 Most of the colonic lipomas are asymptomatic in small size, but about 30% of them reaches 2 cm or larger size and may produce symptoms such as anemia, abdominal pain, constipation, diarrhea, bleeding, or intussusception.1,4
Although intussusception is a common disease for children, intermittent intussusception caused by colonic lipoma is rare in adults, and is caused usually by large pedunculated lipoma. It accounts for 5% of all cases in adults and 90% of intussusception occurs secondary to mass-like lesions such as lipoma or malignant tumor.5 Adult intussusception sometimes presents as chronic intermittent abdominal pain, obstruction and bleeding, but unlike children's cases, the symptoms are nonspecific and various, so these features are hardly useful for diagnosis prior to surgery.6
We report a case of chronic abdominal pain due to proximal ascending-proximal transverse colonic intussusception caused by giant proximal ascending colonic lipoma which was managed successfully by the right colonic segmental resection.
CASE REPORT
A 68-year-old female patient visited our hospital because of intermittent abdominal pain and dyspepsia which started a month before. Her medical history was nonspecific excluding hypertension which has lasted for 1 year by that time. The blood pressure was 120/80 mm Hg, pulse 88/min, respiration rate 20/min, and body temperature 36.7℃. There were no specific findings in physical examination. Complete blood count results showed white blood cell 11,200/mm3, hemoglobin 12.9 g/dL, and platelet 275,000/mm3. The blood chemistry was analyzed as total protein 7.6 g/dL, albumin 4.2 g/dL, total bilirubin 0.47 mg/dL, AST 23 IU/L, ALT 13 IU/L, ALP 51 IU/L, BUN 16.4 mg/dL, serum creatinine 0.8 mg/dL, total cholesterol 189 mg/dL, and fasting blood glucose 84 mg/dL. The carcinoembryonic antigen level was 2.1 ng/mL.
In the colonoscopy, a large hyperemic round mass occupying more than three-quarters of the lumen was observed at the proximal ascending colon. The mass was covered with large superficial ulcer with small exposed blood vessels, and was firmly originated at the counter-mesenteric border side of 2 to 3 cm distal part of ileocecal valve, suggesting malignant gastrointestinal stromal tumor (GIST). There was another small ulcer near the base of the mass (Fig. 1).
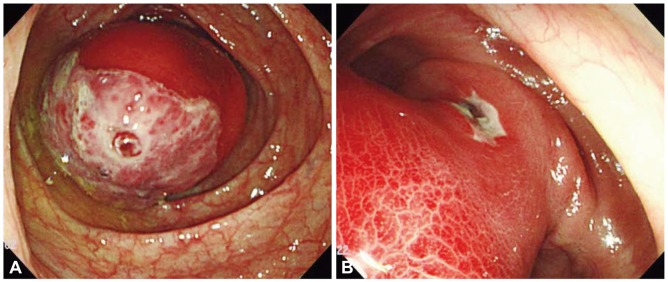
Colonoscopic findings. (A) Huge, round, hyperemic mass covered with superficial ulcer is observed at proximal ascending colon. On the center of ulcer, the exposed vessels are seen. (B) It shows another small ulcer near the base of the mass, and inflammated hyperemic mucosa is seen on the body of the mass.
In the abdominal computed tomography (CT) on the next day, a concentric multi-layered mass was shown at the proximal ascending colon, which extended to proximal transverse colon along the shortened ascending colon, and an introcession from the cecum, about 6×4 cm low density mass on the proximal transverse colon was observed (Fig. 2).
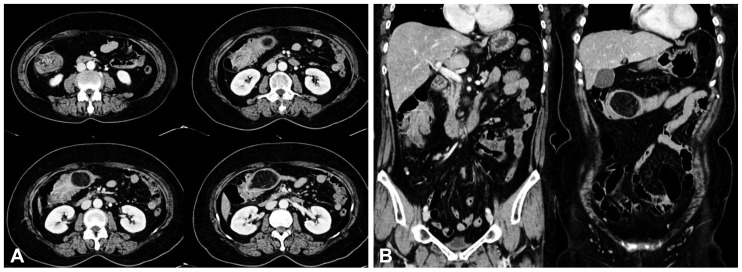
Abdominal computed tomography findings. (A) It shows a concentric multi-layered mass at the proximal A-colon, which extended to proximal T-colon, and 6×4 cm sized well defined low density mass in proximal T-colon, suggesting colo-colic intussusception caused by lipoma. (B) In the coronal images, introcession from the cecum and shortened A-colon are seen.
Although the colonoscopic findings were not typical for lipoma, she was diagnosed with ascending-transverse colonic intussusception caused by unusual giant lipoma originated at the proximal ascending colon. She was deemed to require a surgery, which led to the right colonic segmental resection.
In the excised colonic specimen, around 5.5×4.5×3.8 cm of polypoid mass of clear boundary was observed, and the cross section of this mass was bright yellow (Fig. 3). On microscopic examination, the mass consisted of matured fatty cells, and there was no evidence of malignancy, thus it was diagnosed to be a lipoma (Fig. 4). She was discharged without special complications after the surgical operation.
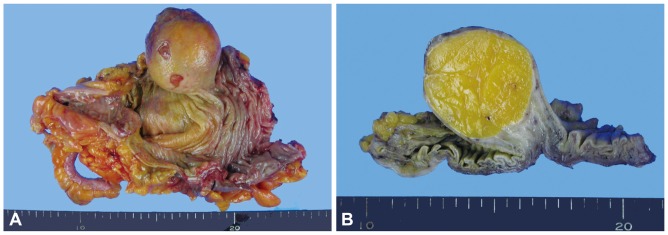
Gross findings. (A) The polypoid submucosal mass is identified in the cecum. (B) The mass is confined to the submucosa, and the cut surface appears bright yellow and soft.
DISCUSSION
The gastrointestinal lipoma is a relatively rare disease, and originates from the submucosa of the gastrointestinal tract and occurs the most frequently in the cecum and ascending colon.1
The colonic lipoma is a common benign tumor of colon next to the hyperplastic and adenomatous polyps.3 This lipoma is limited into the submucosa at 90% of cases with a form of submucosal tumor, but occurs rarely as subserosal tumor.3 Histologically, it has a normal fat tissue covered with normal colonic mucosa while having a well defined capsule with clear boundary between the submucosa and mucosa, and mainly consists of matured adipocytes and a little of fibrous tissues.7 This occurs commonly in the elderly, and more common in women.4 Lipoma often occurs as a solitary mass but 10% to 25% of cases carry multiple masses.2 Most of them are small and asymptomatic, which is why they are usually found incidnetally at the time of endoscopy or autopsy.8,9 For management, a follow-up is sufficient for a small lesion since the possibility of malignant degeneration is rare when there are no symptoms.7 However, in a case where histologic diagnosis is needed since the lipoma is not well-differentiated from other malignant tumors, especially in a patient who has symptoms like abdominal pain, constipation, intestinal hemorrhage, and ileus, operation is a necessity. In addition, it is known that lipoma occurring in the ileocecal valve can cause obstruction in the small intestine.10 A larger lipoma may cause obstruction and intussusception, which leads to symptoms in most cases, and when lipoma is accompanied by mucosal changes, it may be mistaken for an adenoma or malignant tumor, and sometimes causes a mucosal ulcer resulting in bleeding.8,11
Intussusception is a common cause of ileus in children, but it rarely occurs in adults; about 80% of adult cases are caused by mass lesion such as a large polyp.5 In particular, it is known that 66% of colonic intussusception results from malignant tumors.12
A symptomatic lipoma or asymptomatic but more than 2-cm size lipoma, with fair possibility of causing symptoms, should be considered for elimination. Recently, there were some cases with a relatively large lipoma, which were managed by the endoscopic resection.13
The lipoma in this patient's case was found at the proximal ascending colon in the colonoscopy without intussusception, while it was observed in the proximal part of transverse colon with intussuscepted state by the abdominal CT on the next day. This suggests spontaneous air reduction during colonoscopic procedure or repeated spontaneous intussusceptions and reductions by colonic peristalsis causing intermittent recurrent abdominal pain at each event. Although lipoma was considered in the abdominal CT, the colonoscopic findings suggested a malignant GIST rather than a lipoma. The firm hyperemic surface mucosa unlike lipoma might be due to mucosal damage caused by repeated intussusceptions and peristaltic forces, and superficial mucosal ulceration and exposed vessel would be made at some stage. Although similar cases were already reported to Korean journals,14 this GIST-like colonic mass might be considered as an unusual type of lipoma during the colonoscopy. Although surgical resection was conducted in this case, colonoscopic resection could be carefully considered if we knew it was a lipoma beforehand.
Notes
The authors have no financial conflicts of interest.
