The Usefulness of Magnifying Endoscopy and Narrow-Band Imaging in Measuring the Depth of Invasion before Endoscopic Submucosal Dissection
Article information
Abstract
With the widespread application of endoscopic submucosal dissection for the treatment of gastrointestinal neoplasms, accurate determination of the invasion depth prior to intervention has become an indispensable part of treatment planning. Narrow-band imaging (NBI) is a novel endoscopic technique that may enhance the accuracy of diagnosis. Magnifying endoscopy with NBI has been shown to be effective for determining invasion depth for intrapapillary capillary loop classification of esophageal cancer and microvascular pattern of stomach cancer. Such precise pre-treatment staging of early neoplastic lesions in the gastrointestinal tract warrants timely initiation of disease-tailored treatment and, ultimately, better quality of life and improved patient survival.
INTRODUCTION
Endoscopic submucosal dissection (ESD) is currently accepted as standard treatment strategy for gastrointestinal neoplasms without evidence of lymph node metastasis, for ESD allows one-piece resection even in the presence of large or ulcerous lesions.1-3 According to the guidelines of the Japanese Esophageal Society, the indications for the diagnosis and treatment of esophageal squamous cell carcinoma are: 1) high-grade intraepithelial neoplasms, including noninvasive squamous cell carcinomas and 2) intramucosal invasive squamous cell carcinomas, limited to lamina propria mucosae (M2) and without evidence of vessel infiltration.4 Furthermore, the extended indications for endoscopic resection of early gastric cancer suggest that differentiated adenocarcinomas of 30 mm or larger in diameter are entirely free of nodal metastasis, when there is a lack of lymphatic-vascular capillary involvement or when the submucosal penetration is 500 µm or less.2 More recently, Hirasawa et al.5 reported that intramucosal undifferentiated adenocarcinomas of 20 mm or less in diameter, without lymphatic-vascular capillary involvement or ulcerous findings, present a negligible risk of lymph node metastasis. Based on these findings, more clinicians are recognizing the importance of accurately determining the depth of invasion prior to treatment. Consequently, increased attention has been given to making precise pre-treatment diagnosis to avoid unnecessary invasive procedures, such as surgical resection of mucosal cancers that are, in fact, eligible for endoscopic resection. Unfortunately, however, the exact determination of invasion depth of superficial gastrointestinal neoplasms remains challenging, and additional surgical resections are still required in several cases. Conventionally, the accurate assessment of invasion depth is achieved through a combination of several diagnostic modalities, for example using endoscopic ultrasound in adjunct to regular endoscopy.
The recent developments in endoscopic devices, namely the advent of magnifying endoscopy with narrow-band imaging (ME-NBI), have enabled better visualization of fine mucosal and vascular structures under magnified view. In particular, a certain consensus has been reached regarding the effectiveness of ME in determining invasion depth for intrapapillary capillary loop (IPCL) classification of esophageal cancer6 and pit-pattern classification of colon cancer.7 Moreover, ME-NBI has proven itself useful for qualitative diagnosis and for determining the range and tissue type of gastric cancer. In this review, we focused on the usefulness of ME-NBI in measuring depth of invasion of superficial upper gastrointestinal cancer.
MAGNIFYING ENDOSCOPY
ME has the capability of both standard video endoscopy and an adjustable image magnification. The red-green-blue (RGB) sequential system and the color charge coupled device (CCD) system differ in their magnification abilities. While the RGB sequential system allows optical magnification of images up to 80 times, the color CCD system has digital zooming power of 1.2 to 1.5 times magnification. High definition endoscopes, even the ones using the color CCD system, have physical zoom properties, allowing the tip of the endoscopes to approach the mucosal surface as close as 2 mm without compromising resolution. Such combination results in magnifying power of at least 50 times.8 Microvasculature and microsurface structures are anatomical structures that are observed when examining the gastrointestinal tract with ME. Only the microvasculature can be observed when using conventional white light, but when using NBI, both the microvasculature and microsurface structures can be clearly observed.
NBI
NBI is a novel endoscopic technique that may enhance the accuracy of diagnosis using narrow-band width filters in a RGB sequential illumination system.9 This technique produces different images at distinct levels of the mucosa and increases the contrast between the epithelial surface and the subjacent vascular pattern. NBI may provide the same contrast-enhancement abilities as chromoendoscopy without requiring the use of dye agents.10 The basic principle of NBI is that the depth of penetration into the mucosa depends on the wavelength being used: blue band for superficial layers, red band for deep layers, and green band for intermediate layers.11 Because gastrointestinal cancer originates from the mucosa, the use of blue-colored, short-wavelength visible light that can only penetrate into the mucosa, may be helpful in the detection of minute early expressions. In addition, cancers are associated with autonomous angiogenesis - a characteristic responsible for cancer growth and metastasis - and hence, abundant blood vessels. Therefore, the recognition of abnormal capillary beds may assist in cancer diagnosis.12 For short-wavelength visible light is mostly absorbed by hemoglobin in blood vessels, a black color is observed when blood vessels are illuminated with such light. Thus, the subtle differences in mucosal lesions can be discriminated by distinctive colors, and the capillary bed of the mucosal surface can be inspected more clearly when illuminated with narrow-band blue (415±15 nm) and green (540±15 nm) wavelengths.
The NBI system available in South Korea (EvisLucera Spectrum System, CV-260SL; Olympus Medical Systems Co., Ltd., Tokyo, Japan) has a filter that transmits only 415±15 and 540±15 nm wavelengths; when the switch for NBI is activated while observing the upper gastrointestinal system under white light, this filter is inserted, and only a narrow-band around these two wavelengths is transmitted. After the lesions are illuminated, the monochromatic CCD absorbs the reflected light and generates images. Because black and white images have a low resolution, the light absorbed by the monochromatic CCD is composited into RGB to generate color images. Consequently, the main image colors consist of brown and green, and the lesions can be observed in higher resolution than with black and white images.
ME-NBI
NBI observation without magnification has the disadvantage of producing conditions that are sometimes too dark to identify morphological and color changes. The reason for dark images is simply because the NBI system uses only two narrow illumination lights, whereas conventional white light imaging uses a broadband visible light. For these reasons, it is important that users understand the technical backgrounds of these newer endoscopic procedures. ME without NBI has been used for observation of gastric mucosa for many years.13 Unfortunately, modification of gastric mucosa by acid and chronic inflammation caused by Helicobacter pylori infection disturbs accurate evaluation of fine mucosal structures on magnified images, and for that reason the developments in this certain technique have been delayed. ME-NBI is expected to give maximum performance in making accurate diagnosis, and enhance the contrast detailed morphological changes in the mucosal surface and clearly visualizing the microvascular structures.
ESOPHAGEAL CANCER
Inoue et al.14,15 first reported the importance of morphological changes of the IPCL in making diagnosis of esophageal squamous cell carcinoma. IPCL is tennis racket-shaped dark-brown capillaries in the mucosa, derived from the side-branch blood vessels in the submucosal layer (Fig. 1). IPCLs demonstrate characteristic morphological changes according to the tissue atypism and cancer invasion depth. ME findings with regard to capillary pattern are classified into five types (I-V) according to the degree of change in the IPCL pattern, such as dilatation, tortuosity, caliber change in one IPCL, or various shapes in multiple IPCLs.15 Classifications include type I (normal mucosa), type II (regenerating epithelium or inflammation), type III (low-grade dysplasia), type IV (high-grade dysplasia), and type V (cancer). Type V (Figs. 2, 3) is further divided into types V-1 (M1), V-2 (M2), V-3 (M3, SM1), and VN (more invasion than SM2). They concluded that the endoscopic diagnosis of flat mucosal lesions was possible by classifying the IPCL pattern in the magnified images. They recommended periodic endoscopic surveillance for the IPCL type III, while treating lesions of higher than IPCL type IV needs endoscopic mucosal resection/ESD. However, it is difficult to assess the depth of invasion using ME with a regular system. Because NBI has capillary enhancing effects, the microscopic IPCL patterns are readily identified and evaluated by endoscopists with experience in ME. Based on their study of 263 esophageal cancers, Arima et al.16,17 reported that the diagnostic accuracy of ME in measuring depth of invasion was 98.8% for M1 and M2 cancers, 68% for M3 and SM1 cancers, and 84.0% for cancers invading into the middle third (SM2) and the lower third (SM3) of submucosal layer. They concluded that magnifying observation facilitated identification of lesion microinvasion, thereby increasing the proportion of correctly diagnosed M3 or SM1 cancers, in comparison with conventional endoscopic diagnosis. Kumagai et al.18 also reported that the rate of accurate diagnosis of invasion depth was 83.3% in cases where detailed pictures were obtained using ME. They mentioned about the possibility of distinguishing tumors that are shallower than M2 or deeper than M3. Yoshida et al.19 reported that ME-NBI improved the accuracy of invasion depth assessments for superficial esophageal cancer.
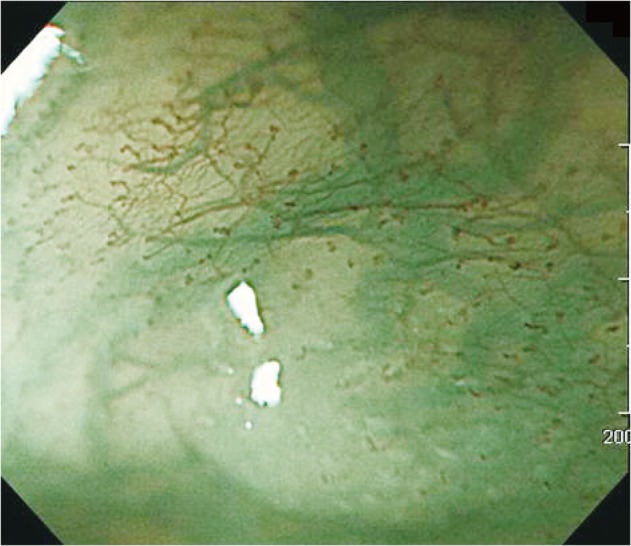
The intrapapillary capillary loop (IPCL) image of normal esophageal mucosa in magnifying endoscopy with narrow-band imaging. Branching vessel which are located at the surface of muscularis mucosa are shown as a green vascular network. The IPCL is observed as a brown vessel which is positioned in the most superficial layer and is derived upright from the branching vessel.
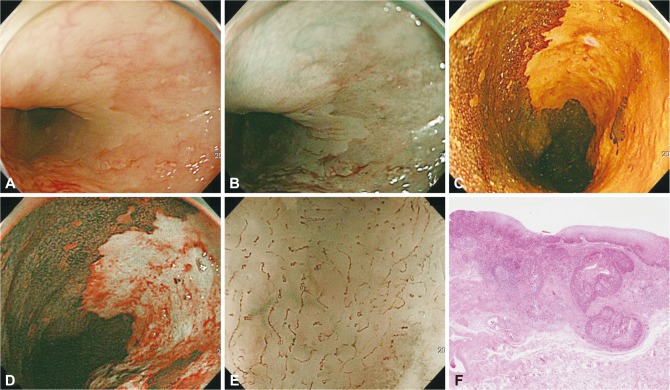
Esophageal squamous cell carcinoma. (A) A slightly depressed lesion with redness extending from 3 to 7 o'clock is observed at the upper esophagus. (B) Under narrow-band imaging (NBI), the lesion is shown as a dark brown color. (C) With iodine staining, it is shown as an iodine-void area with a well-defined boundary. (D) Shiny silver sign. In a couple of minutes after iodine staining, this lesion appears shiny silver under NBI. (E) Magnifying endoscopy with NBI image. Transversely running and irregular-shaped blood vessels as intrapapillary capillary loop (IPCL) deformation are found. The pattern of the vessel is categorized as IPCL V-3. (F) Histopathological image. Squamous cancer, SM1 invasion with lymphatic metastasis (H&E stain, ×100).
Esophageal squamous cell carcinoma. (A) A depressed lesion with irregular nodularity and redness is noted at the mid esophagus. (B) With iodine staining, it is shown as an iodine-void area with a well-defined boundary. (C) Magnifying endoscopy with narrow-band image. With the center of the lesion, intrapapillary capillary loop type V-2 and V-3 are observed. (D) Esophagectomy was performed. This lesion was diagnosed as SM1 invasion with lymphatic metastasis (H&E stain, ×25).
In summary, a number of reports recognizes the practical values ME-NBI, and the usefulness of ME-NBI in measuring the depth of invasion for esophageal squamous cell carcinoma have been corroborated in several studies. However, because analyzing the IPCL results requires considerable amount of time, energy, and experience, ME-NBI cannot always be readily employed. The problem of accessibility remains to be solved.
GASTRIC CANCER
ME has been shown to be effective in distinguishing benign from malignant tumors, establishing tissue types, and determining the extent of gastric cancer.20-23 But its usefulness in measuring gastric cancer invasion depth is yet to be verified.
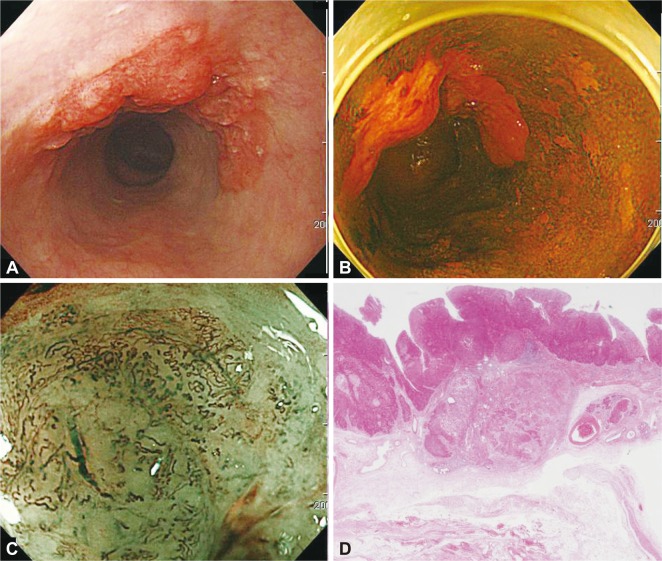
Yao et al.20 reported that magnifying observation of microvascular architecture was useful for discriminating flat reddened carcinoma from gastritis. They proposed unique endoscopic findings for intestinal type gastric cancers: 1) presence of a demarcation line between the reddish lesion and the surrounding mucosa; 2) disappearance of the regular subepithelial capillary network; and 3) the presence of an irregular microvascular pattern within the flat lesions (Fig. 4).20 These characteristics based on mucosal and microvascular architecture are also reliable markers for differentiation between depressed gastric cancer and benign lesions. Nakayoshi et al.21 classified the microvascular pattern of superficial gastric cancers into three groups based on their ME-NBI images (Fig. 5): 1) fine network pattern; 2) corkscrew pattern; and 3) unclassified pattern. They also compared the endoscopic pattern to the histological findings. Fine network pattern and corkscrew pattern were useful in identifying differentiated adenocarcinoma and undifferentiated adenocarcinoma, respectively. ME-NBI was also found to be useful in detecting the lateral extension of superficial gastric cancer.21 This quality is very important in detailed assessment of the safety margin and it enables improved targeting of neoplastic lesions during endoscopic treatment.
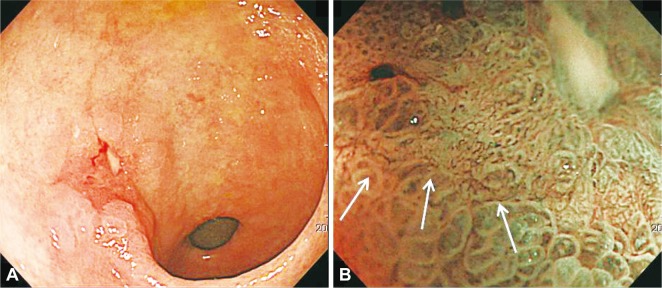
Type 0-IIc early gastric cancer. (A) A reddish depressed lesion is noted at the gastric antrum. (B) Magnifying endoscopy with narrow-band imaging demonstrates loss of fine mucosal structure, loss of subepithelial capillary network and presence of an irregular microvascular pattern. At the margin of the carcinoma, demarcation line is noted (arrows).
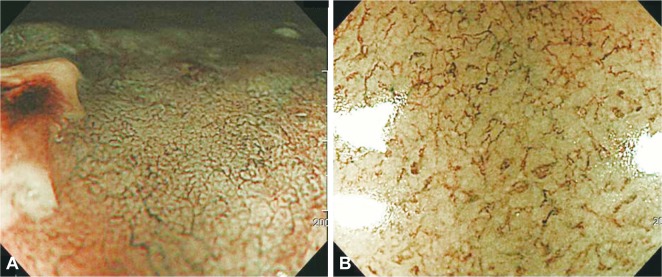
Classification of microvascular patterns in superficial depressed gastric cancer. (A) Fine network pattern looks like a mesh, in which abundant microvessels connect with one another. (B) Corkscrew pattern has isolated and tortuous microvessels, in which scanty microvessels do not connect with one another.
Yagi et al.24 assessed the relationships between microvessels, pits, and histological patterns using ME-NBI. They found that the magnified view of the cancerous area showed three types of patterns (Fig. 6): 1) a mesh pattern (consisting of mesh-like connected microvessels); 2) a loop pattern (consisting of loop-like microvessels that were not connected and had tubule-like mucosal structures along them); and 3) an interrupted pattern (consisting of interrupted thick or thin vessel without mucosal structures). Most (94.9%) lesions showing a mesh or loop pattern were mucosal cancers, whereas 92.3% of lesions showing an interrupted pattern were submucosal differentiated adenocarcinoma. The authors clarified the characteristic features of the magnified view of mucosal differentiated gastric adenocarcinoma and the characteristics of invasive changes, including submucosal invasion.24 Kobara et al.25 reported the usefulness of ME-NBI in determining gastric cancer invasion depth. They defined the following three findings as diagnostic indicators of SM2: non-structure, scattery vessels, and multi-caliber vessels (Fig. 7). In differentiated depressed gastric cancer, all three indicators were present more frequently in SM2 than in SM1 (p<0.05). All depressed gastric cancer with ≥2 points were SM2, demonstrating a significant difference in score distribution between SM1 and SM2 (p<0.05).25 Several investigators have reported that SM cancer is associated with the appearance of non-structure areas in fine mucosal structure, irregularly-shaped, dilated, or extended microvessels and evidence of a hypovascular tumor.26,27
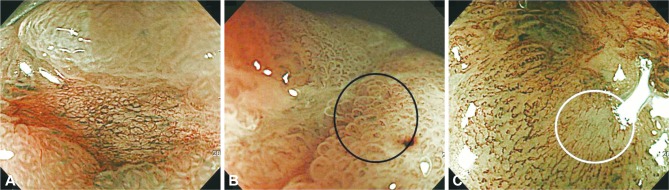
Another classification of microvascular patterns in the gastric cancer. (A) Mesh pattern. (B) Loop pattern (black circle). (C) Interrupted pattern (white circle).
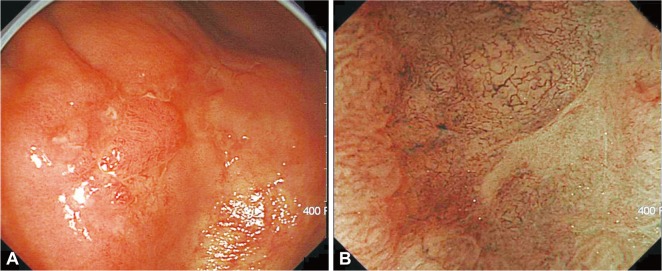
Type 0-IIc early gastric cancer. (A) An irregular shaped, depressed lesion with central nodularity is noted in the gastric body. (B) Magnifying endoscopy with narrow-band imaging demonstrates non-structure, scattery vessels and multi-caliber vessels. This lesion was diagnosed as SM2 cancer.
In summary, the studies on gastric cancer support the usefulness of ME-MBI in cancer differentiation and cancer margin establishment. The studies on the usefulness of ME-MBI in measuring invasion depth for gastric cancers have several limitations. For one, the absolute number of reports is too small to reach any kind of significance or consensus. Also, only the depressed type cancers and differentiated type cancers have been studied so far. Moreover, the lack of standardized parameter makes it difficult to accurately describe the depth of submucosal invasion. However, one can suspect submucosal invasion when there is appearance of non-structure areas, when hypovascularity is recognized and when irregularly shaped and dilated microvessel are present.
CONCLUSIONS
NBI is becoming a promising endoscopic technology that enables better detection and accurate diagnosis of neoplastic lesions in the gastrointestinal tract. However, most studies conducted so far have been limited to a single center study, carried out by one or a few observers. Overcoming the diagnostic discrepancies that occur among clinicians is a task that must be solved in the future. A large scale, prospective, randomized trial should be conducted to obtain more detailed information on ME-NBI. The characteristic features of the microvascular pattern and microsurface structure of gastrointestinal neoplasms may allow endoscopists to diagnose gastrointestinal cancer more accurately. If differentiating mucosal cancer from submucosal cancer by ME-NBI becomes applicable, this technique will contribute to making clinical decisions regarding the treatment options for gastrointestinal tract neoplasms, avoiding unnecessary operations and ultimately, better quality of life and improved patient survival.
Notes
The author has no financial conflicts of interest.