Submucosal Endoscopy, a New Era of Pure Natural Orifice Translumenal Endoscopic Surgery (NOTES)
Article information
Abstract
Natural orifice translumenal endoscopic surgery (NOTES) involves the intentional perforation of the viscera with an endoscope to access the abdominal cavity and perform an intraabdominal operation. In a brief time period, NOTES has been shown to be feasible in laboratory animal and human studies. Easy access to the peritoneal cavity and complete gastric closure should be secured before NOTES can be recommended as an acceptable alternative in clinical practice. The concept of submucosal endoscopy has been introduced as a solution to overcome these two primary barriers to human NOTES application. Its offset entry/exit access method effectively prevents contamination and allows the rapid closure of the entry site with a simple mucosal apposition. In addition, it could be used as an endoscopic working space for various submucosal conditions. Herein, the detailed procedures, laboratory results and human application of the submucosal endoscopy will be reviewed.
INTRODUCTION
Since Kalloo's publication of transgastic peritoneoscopy (TGP)1 in 2004, the field of natural orifice translumenal endoscopic surgery (NOTES) has progressed beyond the laboratory to the clinical field. The old dogma of "a big surgeon makes a big incision" is no longer compatible with current evolving practice, as the benefits of smaller and fewer incisions are recognized. NOTES has shown feasibility in numerous laboratory animal studies. Furthermore, several large-scale clinical trials and registries using NOTES are currently being conducted. However, surgeons and endoscopists are still as far away as ever from embracing the consolidated significance of NOTES. Surgeons regard NOTES as a tabloid procedure of the minimally invasive surgery, while endoscopists regard it as an extension of the endoscopic resection. Considering these disparate points of view, transvaginal hybrid-NOTES to resect intraabdominal organs, has been a major priority in Western countries (surgeon-directed NOTES). On the contrary, transgastric pure-NOTES, whether for the exploration of the peritoneal cavity or for the endoscopic full-thickness resection (EFTR) of an intraluminal neoplasm or endoscopic myotomy, have been more of a priority in Eastern countries (endoscopist-directed NOTES).
To perform pure-NOTES in human cases, easy access to the peritoneal cavity and complete gastric closure should be guaranteed. Since Sumiyama et al.2 introduced submucosal endoscopy with a mucosal flap safety valve (SEMF) technique, this technique has earned much attention as a solution to overcome these two primary barriers to human application of NOTES. In the present review, we present the detailed procedures, laboratory results and human application of submucosal endoscopy.
THE CONCEPT OF SUBMUCOSAL ENDOSCOPY
The technique of SEMF was developed based on the concept of using the submucosa as a practical working space for endoscopic interventions, such as the resection of mucosal neoplasias and submucosal tumors, as well as for the acquisition or dissection of muscular tissue for motility disorders. In addition, the overlying mucosal layer of the submucosal space could be a sealant flap between an offset entry point (mucosa) into and an exit point (muscularis propria) out of the peritoneal cavity. SEMF provides a protective submucosal tunnel preventing peritoneal soiling.
Because the intraluminal incision was made only within mucosa, not full-thickness, the entry point could be easily closed with endoscopic clipping devices. Therefore, submucosal endoscopy can be an ideal endoscopic working space that provides safe, protected peritoneal access.
THE DETAILED PROCEDURE
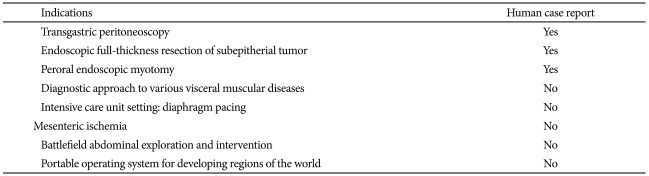
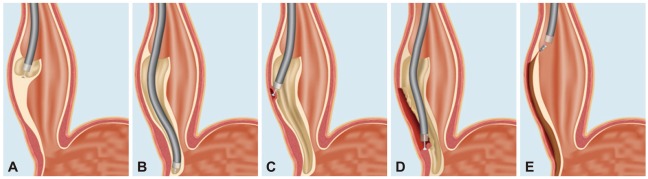
The initial SEMF technique described by Sumiyama et al.3 was performed step by step as follows (Fig. 1): 1) a small submucosal bleb of injected saline was created, 2) high-pressure bursts of CO2 were injected into the bleb dissecting the submucosa, 3) hydroxypropyl methylcellulose was then injected to prevent gas escape and to maintain the bleb, 4) mucosal incision (10 mm) was made at one margin of the bleb with a needle knife, 5) submucosal dissection could be created with CO2 injection with or without the assistance of a 15 mm biliary retrieval balloon, 6) opposite the mucosal entry point (by an average distance of 5 cm), the muscular layer was snare-resected by the cap-assisted endoscopic mucosal resection technique to create an open entry into the peritoneal cavity, and 7) upon withdrawal of the endoscope, the mucosal entry can be closed by mucosal apposition using clips. With this initial technique, however, rapid injection of CO2 created a large submucosal working space as well as ulceration in some cases due to partial necrosis of the overlying free mucosa.
Schematic drawings of submucosal endoscopy with mucosal flap technique. (A) The submucosal plane is isolated with injection of CO2 gas injection, (B) repeated balloon dissection of the submucosa. (C) The endoscope is inserted into the submucosal space, a myotomy exit site is made with modified cap EMR technique. (D) The peritoneal cavity is accessed via the myotomy. (E) The endoscopic entry point into the submucosal space is closed (Adopted from Sumiyama et al. Minim Invasive Ther Allied Technol 2008;17:365-369).3
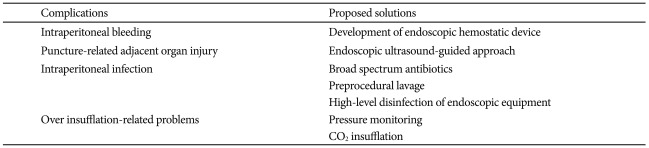
Yoshizumi et al.4 modified this technique (Fig. 2) using endoscopic submucosal dissection (ESD) as follows: 1) inject 5 mL of normal saline solution into the submucosal layer, 2) a 2 cm mucosal incision was made over this submucosal cushion with a flex knife (KD-630L; Olympus Optical Co., Ltd., Tokyo, Japan) and an insulation-tipped electrosurgical knife (IT-knife, KD-610L; Olympus, Tokyo, Japan) 3) submucosal dissection was performed using an IT-knife to create a submucosal tunnel of approximately 5 cm in length, 4) a small incision of the seromuscular layer at the distal end of the submucosal tunnel was made using the flex knife, 5) a 15-mm dilation balloon (CRE5842; Boston Scientific, Natick, MA, USA) was inserted through the seromuscular incision, into the peritoneal cavity, to enlarge the opening, and 6) upon withdrawal of the endoscope from the submucosal tunnel, the mucosal incision site was closed using clips.
Schematic drawings of modified endoscopic submucosal dissection (ESD) technique. (A) Submucosal injection with normal saline solution. (B) Creation of a longitudinal narrow submucosal tunnel using ESD. (C) Advancement of an endoscope into the peritoneal cavity. (D) Closure of the mucosal incision site using endoclips (Adopted from Yoshizumi et al. Endoscopy 2009;41:707-711).4
This modified method using the ESD technique appears to have several advantages. First, the long and narrow submucosal tract can minimize intraperitoneal leakage of gastric contents during the NOTES procedure, by having a tighter relationship between the endoscope and tunnel. Second, after the endoscope has been withdrawn into the stomach, gastric distension can be maintained, thereby allowing the easy placement of clips. Finally, the two approximated surfaces of the narrow longitudinal tunnel heal rapidly. Therefore, most current reports have used this modified method for NOTES procedures using a submucosal tunnel.
ANIMAL STUDIES WITH SUBMUCOSAL ENDOSCOPY
Studies using animal models have demonstrated the possibility of applying NOTES using sumucosal endoscopy, such as transesophageal mediastinoscopy, transesophageal thoracoscopy, transesophageal epicardial coagulation, transesophageal cardiomyotomy, peroral endoscopic esophageal myotomy, TGP and transgastric cholecystectomy.2,5-10 For diagnosis of the intrathoracic or mediastinal pathology, traditional options for tissue accrual are percutaneous pleural biopsy, endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA), video-assisted thoracoscopic surgery (VATS), or open thoracotomy. In contrast to EUS-FNA and percutaneous pleural biopsy approaches, the transesophageal NOTES approach allows direct visualization for tissue sampling. Also, in contrast to VATS, transesophageal thoracoscopy begins near the hilar surface of the lung, thus providing a superior access point for evaluating central lesions of the lung.
In terms of securing access closure, von Delius et al.11 evaluated the effectiveness of various methods of transgastric access/closure with regard to leak pressures, in an ex vivo model. An extended submucosal tunnel of 5 cm showed the best leak resistance compared with other standard transgastric access methods. Most recently, a report from Moyer et al.12 demonstrates that submucosal endoscopy allows safe abdominal access, a reliable means of closure, directed endoscope positioning, and long-lasting durability in complex NOTES procedures. In this study, the submucosal tunnel remained fully intact in all of the 14 animals after organ resection (7 cholecystectomies, 7 uterine horn resections).
HUMAN APPLICATIONS WITH SUBMUCOSAL ENDOSCOPY
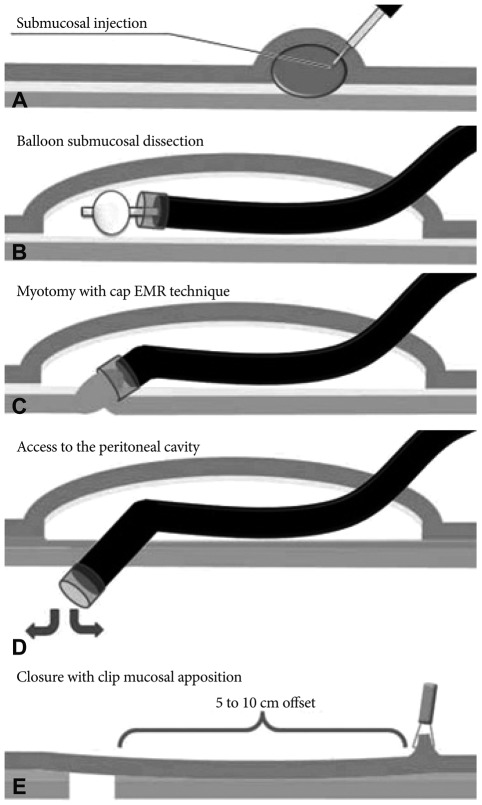
Although many positive results from animal studies were reported, human application with submucosal endoscopy has been limited. Lee et al.13 reported the first human case of diagnostic TGP using submucosal endoscopy in a patient with ascites of uncertain etiology. The investigators employed the modified method from Yoshizumi, and performed a successful 5 minute intraperitoneal exploration and attained multiple forceps biopsies of scattered intraperitoneal nodules, without any complication (Fig. 3). This NOTES procedure was performed under conscious sedation in the endoscopic unit. Unpublished data from the same group include four additional cases using a modified technique with CO2 pressure control, all successfully done without complication. Kitano et al.14 performed TGP for preoperative staging in a pancreatic cancer patient. They used submucosal endoscopy to ensure safe peritoneal access and secure closure of the gastric incision site, under general anesthesia. After confirming no liver or peritoneal metastasis, the patient underwent standard open operation.

Peroral transgastric peritoneoscopy. (A) A mucosal incision at the submucosal bleb. (B) A submucosal tunnel created using endoscopic submucosal dissection. (C) Balloon dilation after a small puncture of the seromuscular layer. (D) Endoscopic forceps biopsy from the metastatic nodules in the peritoneum.
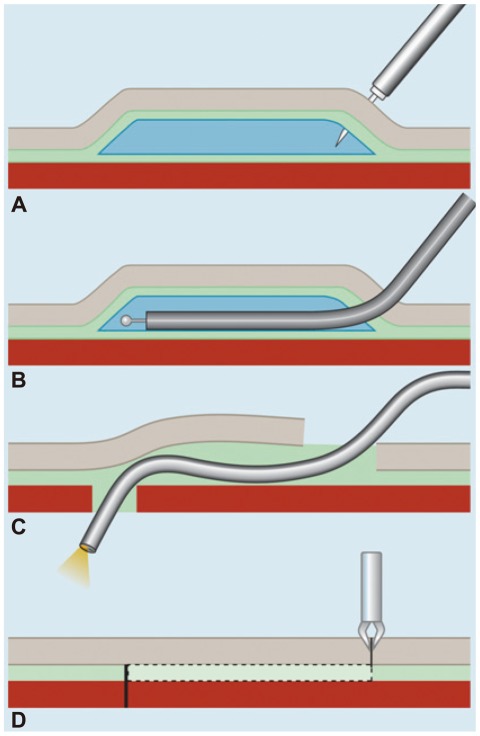
Besides being an access route into the peritoneal cavity for diagnostic purposes (diagnostic TGP), submucosal endoscopy has also been used as an endoscopic working space for the resection of subepithelial tumors (SET). Lee et al.15 demonstrated that EFTR using submucosal endoscopy enables the en bloc whole-layer resection of gastric SET, without laparoscopic assistance (Fig. 4). In this procedure, when the endoscope reached the tumor through the submucosal tunnel, further dissection was made around the tumor for securing working space. After endoscopic full-thickness incision of approximately three-fourths of the circumference of the tumor was accomplished, the tumor was resected with a snare. All procedures were performed under conscious sedation in the endoscopic unit. Another report using submucosal endoscopy as a working space is peroral endoscopic myotomy (POEM) in patients with esophageal achalasia. Inoue et al.16 reported 17 consecutive human cases with POEM (Fig. 5). A long submucosal tunnel was created (mean length 12.4 cm), followed by endoscopic myotomy of circular muscle bundles of a mean total length of 8.1 cm (6.1 cm in distal esophagus and 2.0 cm in cardia). In all cases POEM significantly reduced the dysphagia symptom score and the resting lower esophageal sphincter pressure, without serious complications.
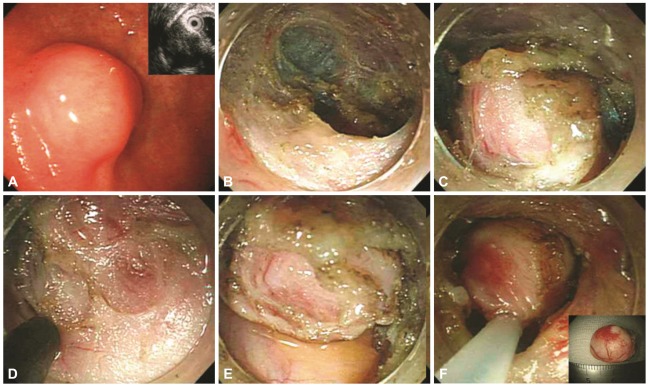
Endoscopic full-thickness resection of subepitherial tumor (SET). (A) A SET at the anterior wall of the low body. (B) A submucosal tunnel created using endoscopic submucosal dissection. (C) The exposed tumor within the submucosal tunnel. (D) Full-thickness incision around the tumor. (E) Full-thickness dissection of the seromuscular layer. (F) The final snare resection of the tumor.
Peroral endoscopic myotomy. (A) Entry to submucosal space. (B) Submucosal tunneling. (C) Endoscopic myotomy, with a total length of 10 cm. (D) Long endoscopic myotomy of inner circular muscle bundles, leaving the outer longitudinal muscle layer intact. (E) Closure of mucosal entry (Adopted from Inoue et al. Endoscopy 2010;42:265-271).16
THE FUTURE OF SUBMUCOSAL ENDOSCOPY, ENDOSCOPIC SUBMUCOSAL SURGERY (ESS)
As mentioned previously, submucosal endoscopy can currently be applied for TGP, EFTR of SET's, and POEM. However, the potential to apply submucosal endoscopy to other conditions and even established procedures is vast. "Endoscopic submucosal surgery" (ESS) can be used to collectively describe such novel procedures that utilize submucosal endoscopy for treatment of early GI cancers, or other benign conditions. Possible applications of ESS are ESD using submucosal endoscopy or "reverse ESD." This technique involves creating a submucosal tunnel beneath the tumor prior to circumferential incision and en-bloc resection. Potential dvantanges of "reverse ESD" are minimization of bleeding and perforation with regard to the submucosal tunnel method, and uniform depth of dissection, resulting in better pathologic interpretation. Enucleation of 3rd layer SET's can also be performed by creating a submucosal tunnel under the SET. Another possible application of ESS is stricturotomy of refractory benign esophageal strictures. Stricturotomy can be performed using submucosal endoscopy to dissect the inner circular muscle layers.
In the future, considering the portability of NOTES equipment and the requirement for only conscious sedation, submucosal endoscopy is ideally suited for the intensive care unit (ICU). In an ICU setting, we can apply this portable procedure to find various intraperitoneal pathologies such as mesenteric ischemia, the origin of bleeding, and the source of infection. Table 1 shows the proposed indications of submu-cosal endoscopy.
The main obstacle of clinical submucosal endoscopy is the risk of procedure-related complications. There are many considerations; four main complications need to be addressed before submucosal endoscopy can proceed further. First, endoscopic hemostatic accessories cannot not be effective tools for profuse intraperitoneal bleeding. Second, the blind puncture of the visceral wall can be associated with the serious injury of intervening vessels and organs. Third, an intraperitoneal infection, colonization due to a transient viscerotomy, or an incomplete closure can be developed. Fourth, various complications related to over insufflation should be considered. Table 2 shows the complications associated with submucosal endoscopy and their proposed solutions.
CONCLUSIONS
It is evident that a great deal of advance is still required before NOTES can be considered for widespread application, and patient safety should come first among others. From this point of view, submucosal endoscopy has provided a meaningful opportunity to explore and treat intraperitoneal lesions with a reliable platform of access and closure. Its offset entry/exit access method effectively prevents contamination and allows rapid closure of the entry site with a simple mucosal apposition. In addition, it could be used as an endoscopic working space for various submucosal conditions. Early human experience, as described above, reports good initial results and few complications. Submucosal endoscopy has truly made it possible to perform NOTES without laparoscopic assistance. Irresistible desire to provide scarless endoscopic surgery is driving modern invasive treatment to a new era, in spite of all current criticism to NOTES. In the center of this desire, pure-NOTES using submucosal endoscopy might play an important role.
Acknowledgments
We thank Mark A. Gromski, MD. (Harvard Medical School) for manuscript editing.
Notes
The authors have no financial conflicts of interest.