Impact of Moderate versus Deep Sedation and Trainee Participation on Adenoma Detection Rate-Analysis of a Veteran Population
Article information
Abstract
Background/Aims
The adenoma detection rate (ADR) is used as a quality indicator for screening and surveillance colonoscopy. The study aimed to determine if moderate versus deep sedation affects the outcomes of the ADR and other quality metrics in the veteran population.
Methods
A retrospective review of colonoscopies performed at Memphis Veterans Affairs Medical Center over a one-year period was conducted. A total of 900 colonoscopy reports were reviewed. After exclusion criteria, a total of 229 index, average-risk screening colonoscopies were identified. Data were collected to determine the impact of moderate (benzodiazepine plus opioids) versus deep (propofol) sedation on the ADR, polyp detection rate (PDR), and withdrawal time.
Results
Among 229 screening colonoscopies, 103 (44.9%) used moderate sedation while 126 (55%) were done under deep sedation. The ADR and PDR were not significantly different between moderate versus deep sedation at 35.9% vs. 37.3% (p=0.82) and 58.2% vs. 48.4% (p=0.13), respectively. Similarly, there was no significant difference in withdrawal time between moderate and deep sedation (13.4 min vs. 14 min, p=0.56) during screening colonoscopies.
Conclusions
In veterans undergoing index, average-risk screening colonoscopies, the quality metrics of the ADR, PDR, and withdrawal time are not influenced by deep sedation compared with moderate sedation.
INTRODUCTION
Colorectal cancer (CRC) is the second most common cause of cancer deaths among men and women in the United States [1]. The estimated lifetime risk of CRC is 5% [2]. Among the US veteran population, CRC accounts for about 9% of all cancers [3]. Relative to the general population, veterans are older with multiple high-risk comorbidities, impacting CRC risk [3,4]. In addition, certain lifestyle factors possibly impacting CRC risk include a higher smoking prevalence among veterans and poor diet [5,6]. Since, colonoscopy is a powerful tool in a gastroenterologist’s armamentarium, a quality examination is essential to prevent and diagnose CRC [7]. The detection and removal of adenomatous polyps during colonoscopy have been emphasized significantly to prevent progression to CRC.
According to the American Society for Gastrointestinal Endoscopy (ASGE) and the American College of Gastroenterology (ACG) task force on quality in endoscopy, the adenoma detection rate (ADR) is one of the priority quality metrics for average-risk index screening colonoscopies [8]. The proposed target ADR is 30% for men and 20% for women [8-10]. Multiple modalities have been studied to improve the ADR and polyp detection rate (PDR), including the quality of bowel preparation [11,12], withdrawal time after cecal intubation [13,14], sedation versus no sedation, and type of sedation, i.e., moderate sedation using a benzodiazepine and opioid versus deep sedation using propofol [15-19]. In a study of 52,506 patients undergoing screening colonoscopies, there was no difference in the ADR and PDR when patients who received sedation versus those without sedation were compared; however, sedation led to a higher cecal intubation rate (CIR) [20]. There are conflicting prior reports on the effects on the ADR and PDR by moderate sedation compared with deep sedation [15-21]. We aimed to study the impact of moderate and deep sedation on the ADR, PDR, and withdrawal time in average-risk, screening and non-screening colonoscopies in a veteran population. We also aimed to study the impact of the type of trainee participation on these parameters.
MATERIALS AND METHODS
A retrospective review of all colonoscopies performed at Memphis Veterans Affairs (VA) Medical Center, Memphis, TN, USA, during a 12-month period, between October 2018 and September 2019, was conducted. As shown in Fig. 1, a total of 900 colonoscopy reports were identified. After excluding high-risk patients (i.e., those with a family history of colon cancer or genetic syndromes), surveillance examinations for colon polyps, diagnostic examinations for the evaluation of gastrointestinal symptoms, and patients who had undergone prior colon resection, a total of 229 index, average-risk screening colonoscopy reports were identified. The colonoscopies were performed with or without the participation of a gastroenterology (GI) fellow under the supervision of an attending physician. Moderate sedation was administered by the trained nursing staff under the supervision of an attending physician, while deep sedation was administered by an anesthesiologist or a certified nurse anesthetist supervised by an anesthesiologist. Moderate sedation included benzodiazepine plus opioids (i.e., midazolam and fentanyl), while deep sedation included propofol. All patients were evaluated to assess their risk for sedation prior to the procedure. An American Society of Anesthesiologists (ASA) class associated with a risk of adverse events during GI procedures was determined for each patient [22]. The patients in ASA class I, II, or III were administered moderate sedation. In the presence of an anesthesia provider, deep sedation (propofol-based sedation) was administered for patients in ASA class I, II, or III for additional comfort, patient safety, procedural efficiency, or an anticipated intolerance to the moderate sedation. Deep sedation was also directed to patients with an increased risk of adverse events due to comorbidities (ASA class IV). The age, gender, body mass index (BMI), ASA class, type of sedation used, quality of bowel preparation, and number and pathology of polyps were recorded from review of patient charts.
Prior publications have addressed the impact of trainee participation on quality metrics in colonoscopies [23-28]. As the colonoscopies in our study population were performed at a training center for the GI fellowship program at the University of Tennessee Health Science Center, the impact of trainee participation on the ADR, PDR, and procedure times was analyzed.
Data were analyzed to determine the impact of moderate versus deep sedation on the ADR, PDR, and withdrawal time. In a separate analysis, we also analyzed all 900 colonoscopies, including non-screening examinations, to assess the impact of the type of sedation on the aforementioned parameters. Statistical analysis was performed using Stata 15.1 (StataCorp LLC, College Station, TX, USA). Using descriptive statistics, a two-tailed unpaired t-test was used for continuous data, while the chi-squared test was used for categorical data. A p-value of <0.05 was considered statistically significant. This study was approved by the Institutional Review Board of the VA Medical Center.
RESULTS
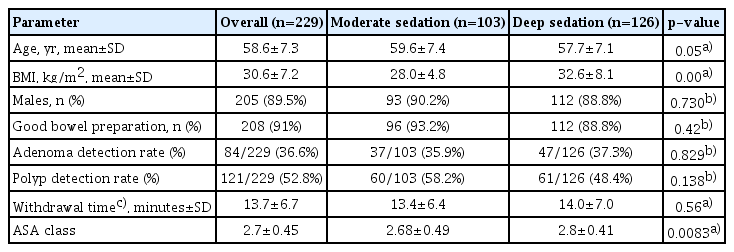
A total of 229 index, average-risk screening colonoscopies were identified, with 103 (44.9%) patients receiving moderate sedation and 126 (55%) receiving deep sedation. As shown in Table 1, the overall mean age of patients undergoing index screening colonoscopies was 58.6 ±7.3 years, and the mean BMI was 30.6 ±7.2 kg/m2. Patients who received deep sedation had a higher BMI than the moderate sedation group (32.6±8.1 kg/m2 vs. 28.0±4.8 kg/m2, p<0.00). Since this study was conducted in a veteran population, the patients were predominantly male (89.5%). Patients with a higher ASA class were more likely to get deep sedation than moderate sedation (2.8±0.41 vs. 2.68±0.49, p<0.0083). As shown in Fig. 2, the overall ADR was 36.6% and PDR was 52.8% in the index colonoscopy group. The ADR and PDR were not significantly different between the moderate and deep sedation groups (35.9% vs. 37.3%, p=0.82 and 58.2% vs. 48.4%, p=0.13, respectively). There was no significant difference in withdrawal time between moderate and deep sedation (13.4 min vs. 14 min, p=0.56) during screening colonoscopies.
Similarly, as shown in Table 2, when all 900 colonoscopies were analyzed, there was no significant difference in the ADR and PDR between the moderate and deep sedation groups (45.8% vs. 50.2%, p=0.18 and 60.2% vs. 59.6%, p=0.89, respectively). In addition, there was no significant difference in withdrawal time between the two groups (16.3 min vs. 15.0 min, p=0.09). Patients who received deep sedation had a higher BMI than the moderate sedation group (31.5±7.1 kg/m2 vs. 27.9±4.8 kg/m2, p<0.00), and similarly, patients with a higher ASA class were more likely to get deep sedation than moderate sedation (2.9±0.37 vs. 2.7±0.49, p<0.000).
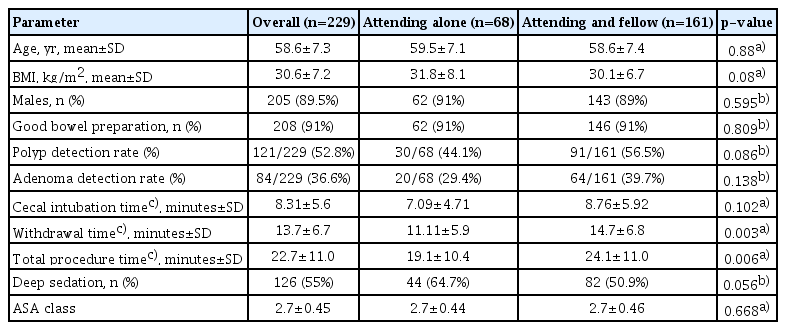
As shown in Table 3, in the total of 229 index screening colonoscopies, 68 (29.6%) were performed by an attending physician alone, and 161 (70.3%) were performed by a GI fellow supervised by one of the same six GI attending physicians. The ADR was 29.4% when the procedure was performed by a GI attending physician alone, while it increased to 39.7% with GI fellow participation, although this difference was not statistically significant (p=0.13). Similarly, the PDR with GI fellow participation was 56.5% compared with 44.1% for GI attending physician alone (p=0.086). The cecal intubation time, withdrawal time, and total procedure time were longer when a fellow was involved.
DISCUSSION
CRC is the second leading cause of cancer-related death, and monitoring quality metrics for screening colonoscopy is essential to reduce morbidity and mortality [1-4]. This is the first study, to the best of our knowledge, to evaluate the effect of moderate sedation compared with deep sedation on the ADR and PDR in the veteran population. Our results indicate that in veterans undergoing index screening colonoscopies, the quality metrics of the ADR, PDR, and withdrawal time are not influenced by deep sedation compared with moderate sedation. Similarly, adenoma and PDRs in non-screening colonoscopies are similar between the two groups. In addition, trainee participation led to a trend towards increased adenoma detection in colonoscopies, although this was not statistically significant.
Previous studies have evaluated the effect of sedation on several quality metrics such as the ADR, PDR, and CIR [15-21]. Initially, Bannert et al. [20] showed sedation not influencing the ADR and PDR; however, leading to a higher CIR. Radaelli et al. performed a study using the survey of the Italian Association of Hospital Gastroenterologists, evaluating all colonoscopies done at 278 endoscopy centers in a two-week period and showed that moderate versus deep sedation did not affect the ADR and PDR [17]. In their study population, screening colonoscopies constituted 13% of all total colonoscopies performed with 3.1% of the patients receiving propofol. [17] Due to the distribution of patients receiving moderate versus deep sedation, it is inadequate to draw conclusions regarding the effects of sedation on colonoscopy quality metrics. The studies done by Metwally et al. [15] and Nakshabendi et al. [16] demonstrated that moderate sedation compared with deep sedation had no significant effect on the ADR and PDR. In contrast, Wang et al. studied the effect of sedation, in all screening and surveillance colonoscopies, identifying “advanced lesions” as >9 mm or a suspected malignant tumor [21]. It was concluded that moderate sedation contributed to a higher PDR, and deep sedation contributed to the identification of “advanced lesions”. Thirumurthi et al. showed that the ADR is higher with deep sedation than with moderate sedation (46.3% vs. 41.2%, p=0.01) [18]. This study included colonoscopies of non-gastrointestinal cancers, and a specific criterion was used to eliminate patients from getting moderate sedation (i.e., patient with comorbid conditions). These potential confounding variables could have influenced the results of their study. Finally, Turse et al. performed a retrospective study at an outpatient endoscopy center, including 585 average-risk patients [19]. The study concluded that the ADR and PDR were not significantly affected by moderate sedation compared with deep sedation [19]. The PDR was slightly higher in the moderate sedation group despite the lack of significance, similar to the findings in our study. Our study further validates these findings providing data from a veteran population. The lack of statistical significance, between these two groups, could be secondary to the procedural technique similar for each senior endoscopist despite the level of sedation of the patient. Daily patient volume was the same for each endoscopist. The factors possibly influencing the ADR and PDR, such as the quality of the bowel preparation and the withdrawal times, were similar between the groups.
Prior studies have shown conflicting results on the impact of trainee participation on quality metrics in colonoscopies [23-28]. Studies done by Rogart et al., Peters et al., and Qayed et al. demonstrated that fellow participation leads to a higher ADR compared to procedures done by an attending physician alone [24,26,28]. In contrast, Bitar et al. demonstrated fellow participation having no impact on the ADR [27]. Similarly, Buchner et al. showed that there was a trend toward increased adenoma detection when a fellow was present; however, these findings were not statistically significant (30% vs. 26%, p=0.11) [25]. The findings of Buchner et al. are similar to the findings in our study, which showed a trend toward an increased adenoma detection in colonoscopies with the presence of a fellow compared with the attending physician alone (39.7 vs. 29.4, p=0.138) [25]. The withdrawal time is an important factor for improving the ADR [25]. In this cohort, the procedure time and withdrawal time were significantly higher with the involvement of a GI fellow. Fellows in training tend to have a higher procedural time than that of attending physician(s), as they are learning the technique and enhancing their detection of polyps and adenomas. This is consistent with the previous study, which showed the involvement of a GI fellow leading to prolonged procedure times; however, improvement was noted as the fellow progressed through training [29]. In our study, despite the lack of significance in the ADR and PDR with the addition of a GI fellow, there was a trend toward higher values. Presence of an additional observer could lead to an increased detection of polyps. Previous studies have shown having a nurse observer leading to a higher polyp and adenoma detection during colonoscopy [30-32]. Similarly, the presence of a GI fellow can lead to an improved polyp detection and ADR.
The strength of our study includes having patients with comparable demographics in the moderate and deep sedation groups, undergoing index, average-risk screening colonoscopy. Potential limitations of our study include a retrospective analysis and inclusion of patients from a single center. However, prior studies on this topic have also been retrospective. Also, since our study population predominantly comprised men, it is difficult to draw a conclusion based on our results in women.
In conclusion, our study did not find a difference in the ADR and PDR when using deep sedation compared with moderate sedation in a veteran population. However, further randomized control trials are needed to validate these results.
Notes
Conflicts of Interest: The authors have no potential conflicts of interest.
Funding
None.
Author Contributions
Conceptualization: Hemnishil K. Marella, Nasir Saleem, Claudio Tombazzi
Data curation: HKM, NS, CT
Formal analysis: HKM, NS, CT
Writing-original draft: HKM, NS, CT
Writing-review&editing: HKM, NS, CT