Endoscopic removal of common bile duct stones in nonagenarians: a tertiary center experience
Article information
Abstract
Background/Aims
There are few studies assessed the efficacy and mortality of endoscopic retrograde cholangiopancreatography (ERCP) for the removal of common bile duct (CBD) stones in the elderly aged ≥90 years. We aimed to assess the safety and efficacy of endoscopic removal of CBD stones in nonagenarians.
Methods
We retrospectively reviewed ERCP reports for CBD stone removal. The endoscopic and therapeutic outcomes were collected. The length of stay (LOS), the total number of adverse events, and mortality rate were compared between groups.
Results
A total of 125 nonagenarians were compared with 1,370 controls (65–89 years old individuals). The mean LOS for nonagenarians was significantly higher than in controls (13.6 days vs. 6.5 days). Completed intended treatment was similar in the nonagenarians and controls (89.8% and 89.5%, respectively). The overall complication rate did not differ between the groups. However, nonagenarians had a higher incidence of post-ERCP pneumonia (3.9%). None of the nonagenarians were readmitted to the hospital within 7 days. Four nonagenarians (3.2%) and 25 (1.8%) controls died within 30 days.
Conclusions
Advanced age alone did not affect the decision to perform the procedure. However, prompt diagnosis and treatment of post-ERCP pneumonia in nonagenarians could improve the outcomes and reduce mortality.
INTRODUCTION
It is estimated that one in four persons will belong to the >65 years age group by 2050.1 The number of patients older than 90 years admitted to hospitals has increased significantly, reflecting the impact of the aging population.2 Elderly patients are at high risk of developing gallstone disease.3 Approximately 5% of cholecystitis cases have coexisting common bile duct (CBD) stones with a higher prevalence in the elderly (10%–20%).4 Previous studies showed that biliary surgery was associated with an increased risk of morbidity and mortality.4,5 Therefore, there may be a tendency to adopt a more conservative approach in the very elderly patients, making endoscopic retrograde cholangiopancreatography (ERCP) an important non-surgical treatment and often the only method of choice in the elderly.6,7 This, together with the known increased incidence of gallstones in the elderly, it is likely that the number of ERCP procedures performed in the elderly will increase.8
ERCP is associated with several complications. The National Confidential Enquiry into Patient Outcome and Death report investigating the death of 237 patients post-ERCP showed that 82% of patients were aged ≥70 years and that 77% had at least an American Association of Anesthesiology (ASA) grade of 3.9 Despite this, there is a lack of large UK-based studies on ERCP outcomes in very elderly patients. Furthermore, few studies in the literature have investigated the efficacy and mortality of ERCP for the removal of CBD stones in the elderly aged ≥90 years. Therefore, we aimed to assess the safety and efficacy of endoscopic removal of CBD stones in the elderly aged ≥90 years and compared the outcomes to those aged 65 to 89 years.
METHODS
Patients’ cohort
We retrospectively reviewed reports of therapeutic ERCP procedures performed at our institution between January 2016 and December 2020. The inclusion criteria were ERCP procedures performed for CBD stone removal and patient age of >65 years. We have referred to patients aged ≥90 years as nonagenarians and patients aged 65 to 89 years as controls in this study.
Patients with known or suspected hepatopancreatobiliary tumors were excluded. Patients who underwent gastrectomy with Billroth II reconstruction or Roux-en-Y reconstruction were also excluded.
We compared the following patient characteristics: age, sex, ASA grade, absence or presence of antithrombotic therapy, and comorbidities. Comorbidities were classified into eight groups: cardiovascular diseases, respiratory diseases, chronic liver diseases, hematological disorders, chronic kidney disease (CKD), cerebrovascular accidents, diabetes mellitus, and the presence of cognitive impairment. Data on antithrombotic therapy included both anticoagulation and antiplatelet therapies except for aspirin.
The degree of urgency was divided into three categories: routine for outpatients, including those returning for stent removal; urgent for inpatients during their hospital stay except for cholangitis where it was performed as an emergency and within 24–72 hours. Some overlap may have occurred according to patient needs.
Endoscopic procedure
ERCP was performed under conscious sedation. Vital signs were monitored prior to the procedure, during the procedure, and during recovery. All patients were administered topical pharyngeal spray with 10% lidocaine (Xylocaine; AstraZeneca, Cambridge, UK) and sedated with intravenous fentanyl (25–100 μg) or pethidine (50 mg) and intravenous midazolam (1–4 mg) as initial doses. All patients received oxygen (2 L/min) via a nasal cannula throughout the procedure. Duodenal relaxation was achieved by intravenous administration of hyoscine butylbromide.
A standard duodenoscope (TJF 260V; Olympus Optical Co., Tokyo, Japan) was used. After cholangiographic confirmation of choledocholithiasis, endoscopic sphincterotomies (EST) were performed using Dreamtome RX 44 and RX ERCP Cannula (Boston Scientific, Marlborough, MA, USA). Precut papillotomy was performed using MicroKnife XL Triple-Lumen Needle Knife (Boston Scientific). An Erbe VIO 3 electrocautery unit (Erbe Electromedizin, Tubingen, Germany) was used.
Extractor Pro RX Retrieval Balloon Catheters (Boston Scientific) were used to clear the bile duct. If stones could not be removed, double-pigtail 7-Fr 7 cm or 7-Fr 5 cm stents were inserted into the CBD with rescheduling for a further attempt at duct clearance within 3 months.
Clinical parameters and outcomes
Endoscopic and therapeutic outcomes were collected, including the occurrence of ERCP for the first time (native papilla), completed intended treatment, CBD cannulation, unintentional pancreatic duct cannulation, EST, precut papillotomy, large stone extraction (>10 mm), and presence of periampullary diverticulum (PAD). Completed intended treatment was defined as cases in which an endoscopist considered the scheduled purpose of ERCP had been obtained, including duct clearance or stent insertion. Monitoring information was collected on oxygen saturation levels, the total dose of sedation agents administered, and comfort scores. The length of stay (LOS) was defined as the time between admission and discharge.
Adverse events (AEs) were recorded using discharge summaries. Acute post-ERCP pancreatitis (PEP) was defined as worsening abdominal pain with elevated serum amylase levels. Post-ERCP bleeding severity was classified as mild, moderate, or severe according to the European Society of Gastrointestinal Endoscopy guidelines.10 Perforation was detected by either endoscopy or computed tomography. Cholangitis was defined as a high-grade temperature, abdominal pain, and elevated hepatobiliary enzyme levels. Cardiovascular events included cardiac arrhythmias and acute ischemic events. In this study, post-ERCP pneumonia was defined as clinical and radiological evidence of pneumonia for ≤48 hours after ERCP. This would include hospital-acquired pneumonia, as it is sometimes challenging to differentiate between them.
Readmission within 7 days, the total number of AEs, and mortality rate (%) were calculated and compared between groups. Post-ERCP death within 30 days was calculated for both groups.
Statistical analyses
All results are reported as mean and standard deviation for continuous variables. Categorical variables were analyzed using the chi-square test. Statistical significance was set at p≤0.05. Statistical analyses were performed using IBM SPSS ver. 25 (IBM Corp., Armonk, NY, USA).
Ethical statements
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by our local Clinical Effectiveness Unit (CEU 10488), Sheffield Teaching Hospitals. Ethical review and approval were waived for this study, due to the retrospective nature of the study and all the procedures being performed were part of the routine care.
RESULTS
A total of 1498 ERCP procedures were included in the study (128 nonagenarians and 1,370 controls). Significantly more nonagenarians underwent inpatient ERCP (89.1%) than the controls (62.3%) (Table 1). Moreover, most procedures were graded as urgent in nonagenarians and controls (75% and 55.8%, respectively). Most nonagenarians had ASA grade 3 compared with ASA grade 2 in the controls. Although there were no significant differences in the total number of comorbidities between the groups, cardiovascular diseases, cerebrovascular diseases, hematological disorders, CKD, and cognitive impairment were significantly higher in nonagenarians. A significantly higher number of nonagenarians received antithrombotic therapy. The mean LOS for nonagenarians was significantly higher than that in controls (13.6 days vs. 6.5 days).
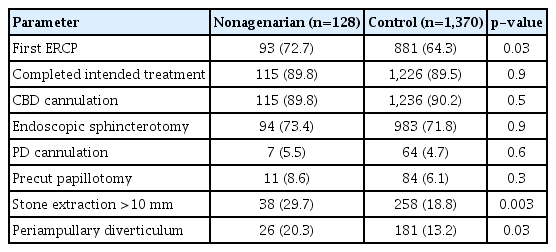
Most procedures were performed for the first time with a higher tendency in nonagenarians (72.7%) (Table 2). Documented CBD cannulation was achieved in 89.8% of the nonagenarians and 90.2% of the controls. There were significantly more larger stones (>10 mm) in nonagenarians (29.7%) than in the controls (18.8%). Almost one in five nonagenarians had a PAD, which was significantly higher than that in the controls. Completed intended treatment was similar in both the nonagenarians and controls (89.8% and 89.5%, respectively).
The overall complication rate did not differ significantly between the groups (Table 3). There were no significant differences between the groups with respect to bleeding, perforation, PEP, cholangitis, and cardiovascular events. However, nonagenarians showed a higher incidence of pneumonia after ERCP (3.9%). None of the nonagenarians were readmitted to the hospital within 7 days of the procedure. Thirty-two controls were readmitted to the hospital for the following reasons: abdominal pain not related to a procedural complication (n=9), PEP (n=5), melena (n=4), biliary sepsis (n=3), chest infection (n=3), duodenal perforation (n=1), repeat ERCP (n=1), chest pain (n=1), fluid overload (n=1), urosepsis (n=1), ureteric calculi (n=1), urinary tract infection (n=1), and neck pain (n=1).
The causes of death in nonagenarians were as follows: coronavirus disease 2019 (COVID-19) pneumonia (n=2), multiorgan failure (n=1), and complications of small bowel obstructions (n=1). The causes of death in the control group were as follows: pneumonia (n=3), multiorgan failure (n=3), pancreatitis (n=2), COVID-19 pneumonia (n=2), decompensated chronic liver disease (n=2), sepsis (n=2), lung cancer (n=2), frailty syndrome (n=2), PEP (n=1), aspiration pneumonia (n=1), cholangitis (n=1), CKD (n=1), ischemic heart disease (n=1), intracranial hemorrhage (n=1), and colorectal cancer (n=1).
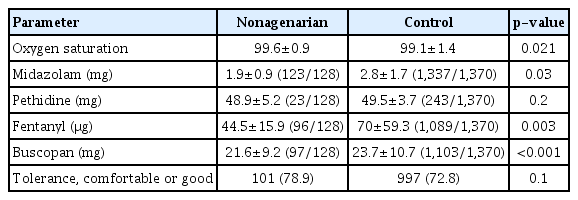
The controls received significantly higher doses of midazolam and fentanyl (Table 4). Despite this, the comfort scores were comparable between the groups.
A total of 242 procedures were performed during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic between March 2020 and December 2020. Of the 242 procedures, 21 procedures were performed on nonagenarians. Three nonagenarians developed COVID-19 pneumonia (>48 hours post-ERCP), and two died within 30 days during this period.
DISCUSSION
Our study showed that the efficacy of endoscopic removal of CBD stones in very elderly patients (≥90 years) was comparable to those aged 65–89 years, as high as 89%. Our study also showed that ERCP was associated with a higher risk of postprocedural pneumonia. However, other ERCP-related complications, including PEP, bleeding, and perforations were not different between nonagenarians and the 65–89 years old group. The 30-day mortality rate was comparable to those aged 65–89 years. To the best of our knowledge, this is the first large UK-based study to assess the safety and efficacy of endoscopic removal of CBD stones in nonagenarians.
Several previous studies have assessed the efficacy and safety of ERCP in the elderly; however, most of these studies included patients with malignant diseases (Table 5).11-23
We excluded patients with malignant obstruction because of the nature of the disease, which usually has a poor prognosis.24,25 The study by Saito et al.22 was similar to our study with respect to the size of the nonagenarian cohort. In their study, CBD cannulation was achieved in 98% of the patients, with a success rate of 81% for CBD stone removal. In their study, 36.5% of patients aged ≥90 years had PAD with a precut sphincterotomy rate of 4.9%. PAD is one of the causes of difficult cannulation and is common in the elderly population. Difficult cannulation increased the risk of PEP (odds ratio, 3.4).26 We had a lower incidence of PAD (20.3%) but a higher rate of performing precut sphincterotomy (8.6%). A smaller study (n=22) found comparable outcomes in technical success and complication rates with no deaths reported in patients >90 years compared with (n=381) those aged 70–89 years.11 Another study from Spain (n=126) with mixed benign and malignant biliary obstructions showed a similar success rate of 90.5% with a complication rate of 2.5% and 30-day mortality of 0.7%.12
Only one nonagenarian patient in our cohort developed PEP who had PAD with unsuccessful CBD cannulation. We observed similar findings in other studies reporting a lower rate of PEP in elderly patients aged >90 years, with an incidence rate of 0%–3%.17,20,22,23 Finkelmeier et al.27 grouped their patients into three categories 20–39 years, 40–60 years, and 61–80 years, and found that those between 20–39 years had a higher incidence of PEP. The reason for this observation remains unclear. A possible explanation is the reduced size of the pancreas and reduced enzyme production in the elderly.27-29
Although the number of comorbidities was comparable between the groups, our cohort of nonagenarians had significantly higher rates of cardiovascular diseases, cerebrovascular accidents, hematological disorders, CKD, and cognitive impairment. Respiratory diseases were less prevalent than those in the 65–89 years old group, and, given the higher post-ERCP respiratory complications, one would conclude that preprocedural screening would have excluded those with significant respiratory diseases in the elderly. Despite the lower burden of respiratory diseases, our nonagenarians were at a higher risk of developing post-ERCP pneumonia. The increased prevalence of post-ERCP pneumonia in the elderly has been studied previously, with findings similar to our nonagenarians.30,31 Kollman et al.31 assessed and compared factors associated with post-endoscopy pneumonia in patients >65 years old and a younger group and found older age was the most significant factor associated with pneumonia. Friedrich et al.30 reported an increased risk in those with a history of intraprocedural cough and vomiting. Other factors that could have contributed to the increased risk of post-ERCP pneumonia in our cohort including an increased ASA grade, high prevalence of PAD, and higher prevalence of large stones, which could have contributed to a longer procedure time.
Patients with cardiovascular comorbidities pose a significant risk during ERCP, and this risk is accentuated by prolonged procedure time. A study found that 11.3% of those aged >65 years had increased cardiac troponin enzyme levels after ERCP.32 Liver diseases, including compensated chronic liver disease, were found to be associated with increased LOS and bleeding during ERCP.33 Those with CKD have a higher risk of PEP and increased LOS.34 One of the possible explanations is the papillary edema secondary to fluid retention in CKD hindering successful CBD cannulation.34
The LOS for nonagenarians was longer than that for the controls. In a Japanese study of 66 patients who underwent ERCP, the average hospital stay was 28.9 days; however, a third of their procedures were for malignant diseases, which could explain the longer LOS compared with our cohort.23 A study investigated 172 patients with acute cholangitis who underwent ERCP and found that an increased ASA grade and the presence of comorbidities were associated with LOS beyond 10 days.35 Our nonagenarian cohort had a higher ASA grade compared with the 65–89 years old group, which could have contributed to longer LOS.
Our lower rate of sphincterotomy compared with CBD cannulation is because our cohort is comprised of individuals requiring their first ERCP and those requiring a repeat ERCP.
Our study covered the period during which the World Health Organization declared SARS-CoV-2 a global pandemic on March 11, 2020. We collected data until the end of December 2020; therefore, we included data of 9 months during the SARS-CoV-2 pandemic. COVID-19 is a highly contagious infection caused by SARS-CoV-2. It is associated with an increased risk of respiratory tract infection.36 Three patients developed COVID-19 pneumonia. The only patient who tested positive for SARS-CoV-2 at <48 hours post-ERCP was an inpatient who was admitted 8 days prior to ERCP. Although COVID-19 can be transmitted via the airborne route during aerosol-generated procedures, including ERCP,37 the chest radiography report was consistent with COVID-19 pneumonia rather than aspiration pneumonia. Therefore, we believe that the patient had COVID-19 pneumonia rather than post-ERCP pneumonia. The hospital policy for endoscopy during COVID-19 was followed, including the use of complete personal protective equipment and downtime of 20 minutes between patients, followed by complete cleaning of the room.
The appropriate choice of sedative agents and doses are essential for the success of ERCP. Complications associated with sedation in gastrointestinal endoscopy include respiratory depression, airway obstruction, and aspiration.38 The risk of complications tends to be higher in elderly patients; therefore, caution should be exercised. We performed conscious sedation with monitoring of vital signs at our institution. Nonagenarians received less midazolam and fentanyl compared with individuals belonging to the 65–89 years old group; however, their tolerance was comparable to that of the controls.
There are several limitations to the current study, mainly owing to its retrospective nature. We did not collect information on intraprocedural cough or vomiting which is linked to increased risk of pneumonia. We were also unable to report the rectal diclofenac administered in our study because this information was stored in the hospital notes. We have relied on digitally stored information for this study. In addition, the practice of administering rectal diclofenac at our institution started in 2019. Furthermore, we believe that the incidence of PEP in both cohorts is comparable to that reported in the literature. In addition, it would have been useful to compare our groups to a third group of nonagenarians who were found to have CBD stones on cross-sectional imaging but did not undergo ERCP to compare the 7-day readmission and mortality. Lastly, we could not minimize the interobserver variability of the ASA grading.
In conclusion, endoscopic CBD stone removal in nonagenarians is achievable with a high success rate. Complications such as PEP, bleeding, and perforation were comparable with patients aged 65–89 years. However, nonagenarians are at a higher risk of developing post-ERCP pneumonia; therefore, careful assessment is required for early detection and treatment. We believe this study will present a starting point for further studies investigating the causes of post-ERCP pneumonia in the elderly.
Notes
Conflicts of Interest
The authors have no potential conflicts of interest.
Funding
None.
Author Contributions
Conceptualization: MJ, AAJ; Data curation: MJ, AK, SI; Formal analysis: MJ, MG, YES, AAJ; Investigation: YES, AAJ; Methodology: MJ, YES, AAJ; Supervision: AAJ; Writing–original draft: MJ; Writing–review & editing: all authors.