AbstractColonoscopy plays an important role in reducing the incidence and mortality of colorectal cancer by detecting adenomas and other precancerous lesions. Image-enhanced endoscopy (IEE) increases lesion visibility by enhancing the microstructure, blood vessels, and mucosal surface color, resulting in the detection of colorectal lesions. In recent years, various IEE techniques have been used in clinical practice, each with its unique characteristics. Numerous studies have reported the effectiveness of IEE in the detection of colorectal lesions. IEEs can be divided into two broad categories according to the nature of the image: images constructed using narrow-band wavelength light, such as narrow-band imaging and blue laser imaging/blue light imaging, or color images based on white light, such as linked color imaging, texture and color enhancement imaging, and i-scan. Conversely, artificial intelligence (AI) systems, such as computer-aided diagnosis systems, have recently been developed to assist endoscopists in detecting colorectal lesions during colonoscopy. To gain a better understanding of the features of each IEE, this review presents the effectiveness of each type of IEE and their combination with AI for colorectal lesion detection by referencing the latest research data.
INTRODUCTIONThe number of patients with colorectal cancer (CRC) is increasing worldwide. In 2020, there were approximately 1.9 million cases and 0.9 million deaths due to CRC worldwide.1 The adenomaŌĆōcarcinoma pathway is considered the major pathway for CRC development because pre-existing adenomas develop into CRC over the years. Colorectal adenomatous polyp removal via colonoscopy has contributed to the reduction in the incidence and mortality of CRC.2 Serrated lesions, including sessile serrated lesions (SSLs) and sessile serrated adenoma/polyps (SSA/Ps), are considered CRC precursor lesions. Studies have reported that the presence of SSA/Ps or SSLs increases CRC risk by 3-fold and that the presence of such lesions with dysplasia increases the CRC risk by 5- to 10-fold compared with the risk among patients with no polyps.3,4 Therefore, screening or surveillance colonoscopies play an important role in the detection of colorectal adenomas and other precursor lesions to reduce CRC incidence and mortality.5-9
Image-enhanced endoscopy (IEE) is a modality that enhances lesion visibility by intensifying microstructure, blood vessels, and color, resulting in easier detection of colorectal lesions.10 A digital IEE that can be switched to conventional white light endoscopy (WLE) by clicking a button on the endoscope is available. First-generation IEEs, including first-generation narrow-band imaging (NBI) or Fujinon intelligent chromoendoscopy systems, did not show a good effect on improving the detection of colorectal lesions.11,12 Owing to recent advances in endoscopic technology, many types of IEE can be used in clinical practice, not only for colonoscopy13,14 but also for the endoscopic diagnosis of gastric diseases and pancreaticobiliary diseases.15,16
We reviewed the latest literature, mainly randomized controlled trials (RCTs) or meta-analyses published in the past five years, and showed the effectiveness of IEE in terms of adenoma detection rate (ADR) and polyp detection rate (PDR), which are established quality indicators in colonoscopy.17-19 The features of each IEE and the representative studies are summarized in Tables 1 and 2, respectively.20-24
NARROW-BAND IMAGINGNBI was developed by Olympus Corporation and emphasizes the microstructure and capillaries on the mucosal surface by modifying the center wavelength and bandwidth of light into narrow-band illumination at 415┬▒30 nm within the hemoglobin absorption band.25 Imaging with WLE and NBI is shown in Figure 1A and 1B. NBI was originally developed for the accurate differentiation of neoplastic and non-neoplastic lesions.26 However, its ability to detect colorectal lesions remains controversial.
A first-generation NBI system (EXERA; Olympus Corporation) was developed in 2006, and a second-generation NBI system (LUCERA; Olympus Corporation) in 2012. The second-generation model provides a brighter and higher image quality and significantly improves the distant-view image. A meta-analysis of 11 RCTs with 4,491 patients comparing adenoma detection between NBI and WLE on colonoscopy was published in 2019. This study demonstrated that ADR in NBI was significantly higher than that in WLE among all enrolled patients (45.2% vs. 42.3%, p=0.04). In the analysis stratified by the quality of bowel preparation, the difference in ADR was not significant when bowel preparation was adequate (43.2% vs. 41.4%, p=0.38), whereas NBI outperformed WLE when bowel preparation was optimal (50.2% vs. 44.4%, p=0.02). Furthermore, in an analysis stratified by the generation of NBI, NBI with a second-generation system provided better ADR than WLE (52.7% vs. 46.7%, p=0.02), whereas first-generation NBI did not (41.0% vs. 39.9%, p=0.48).20 By contrast, after the meta-analysis was published, several RCTs reported that adenoma detection in NBI was not superior to WLE or other IEE modalities. An RCT from Germany that compared the ADR between second-generation NBI and high-definition (HD) WLE in screening and surveillance colonoscopy reported that ADR (29.1% vs. 39.4%, p=0.02) and the number of polyps per patient (0.58 vs. 0.86, p=0.02) were significantly lower in second-generation NBI than in HD-WLE. Particularly, when inexperienced endoscopists performed the procedure, NBI was inferior to HD-WLE.27 A similar tandem RCT that compared second-generation NBI and HD-WLE was reported in Korea.28 The study demonstrated no differences in ADR or PDR observed between the two groups.
The utility of NBI for detecting serrated lesions is debatable. A multicenter RCT reported that the differences between NBI and HD-WLE were not remarkable in detection rates of SSL (7.5% NBI vs. 8.0% HD-WLE, p=0.852), ADR (41.0% NBI vs. 37.5% HD-WLE, p=0.531), and PDR (61.0% NBI vs. 54.0% HD-WLE, p=0.157).29 Another study investigated residual SSA detection using NBI after endoscopic resection. All lesions were randomized into the NBI and WLE groups to detect remnant tissue on the resected margin. The NBI and WLE groups showed no significant differences in the detection of remnant tissue (12.9% vs. 15.4%) or the proportion of SSA in remnant tissue (11.3% vs. 12.3%, respectively).30
NBI is widely used in the optical diagnostics of neoplastic or non-neoplastic colorectal polyps because NBI has an accuracy of >70%, either with or without magnified observation.31 NBI magnified observation also has an accuracy of >95% in diagnosing SSA/Ps, which is higher than the 74% accuracy of the histological diagnosis of a single biopsy specimen.32 Furthermore, NBI with magnified observation can be used to estimate invasive depth in colorectal tumors using the Japan NBI Expert Team (JNET) classification.33 However, based on these results, the detection performance of NBI in colonoscopy cannot be established because its darker image production than that associated with WLE is a potential drawback. The superiority of NBI in adenoma or other polyp detection might be limited by using a new-generation system that provides a brighter image and optimal bowel preparation. A study reported that adding a 30-second observation time improved lesion detection.34 A third-generation NBI system (EVIS X1; Olympus Corporation) was launched in 2020, and the polyp visibility score in this new NBI system was significantly higher than that in the WLE image.35 Such developments or modifications could improve the detection performance of NBI.
TEXTURE AND COLOR ENHANCEMENT IMAGINGTexture and color enhancement imaging (TXI) is a new IEE modality developed by Olympus and launched in 2020. TXI is a WLE-based IEE designed to improve the dimensional characterization of subtle surface irregularities and enhance brightness in images with dark areas and color changes.36 TXI has two modes in terms of enhancement factors: TXI mode 1 (texture, brightness, and color enhancement) (Fig. 1C) and TXI mode 2 (texture and brightness enhancement) (Fig. 1D). In TXI mode 1, the color contrast between red and white is greater than that in mode 2, and the mucosa appears redder. TXI mode 2 produces images that are closer to the WLE color tone.36,37
By December 2022, only one retrospective study conducted at three Japanese institutions had investigated lesion detection using TXI during colonoscopies. Sakamoto et al.21 evaluated colorectal lesion detection, including ADR and PDR, by employing TXI and HD-WLE and the factors related to the detection. The study showed that the ADR and PDR with TXI were 58.2% and 80.2%, respectively, which were higher than those associated with HD-WLE at 46.8% and 63.9%, respectively. Furthermore, using univariate and multivariate regression analyses, TXI was identified as a significant factor affecting ADR, along with age, withdrawal time, and colonoscopy type.
Other supportive studies assessing lesion visibility or color-difference scales using image datasets have also been published. A previous study evaluated the visibility score of 61 colorectal adenomas observed using TXI mode 1, WLE, NBI, and chromoendoscopy with indigo carmine dye. The visibility score for the tumor margin of TXI mode 1 was significantly higher than that of WLE (3.47 vs. 2.86, p<0.01) but lower than that of NBI (3.47 vs. 3.76, p<0.01). Another similar concept study evaluated the visibility score of 68 colorectal adenomas in a video recorded using TXI modes 1 and 2, WLE, and NBI.38 The study showed that the mean visualization scores using WLE, TXI mode 1, TXI mode 2, and NBI were 70.0, 80.5, 75.6, and 69.0, respectively, indicating that the visualization score of TXI mode 1 was significantly better than those of WLE, TXI mode 2, or NBI. Another study evaluated the visibility score for serrated colorectal polyps using endoscopic images observed with TXI mode 1, WLE, NBI, and chromoendoscopy with indigo carmine dye, similar to the other two studies.39 The visibility score of TXI mode 1 was significantly superior to that of WLE for all the 29 serrated polyps enrolled (2.93 vs. 2.27, p<0.01). However, the visibility score of TXI was inferior to that of chromoendoscopy for the imaging of serrated polyps (2.93 vs. 3.45, p<0.01) and sub-analysis of SSLs (2.90 vs. 3.45, p<0.01).
The results of these studies demonstrate that TXI mode 1 improves the visibility of colorectal adenomas and SSLs; therefore, it is possible that the detection of these lesions is improved. However, no prospective clinical trials, including RCT, have investigated lesion detection using this modality. Further clinical trials that directly compare lesion detection using WLE and other observational modes are required.
BLUE LASER IMAGING/BLUE LIGHT IMAGINGBlue laser imaging/blue light imaging (BLI) was installed in the LASEREO and ELUXEO endoscopic systems developed by the Fujifilm Corporation. WLE and BLI images are shown in Figure 2A and 2B, respectively. The LASEREO and ELUXEO have different light sources. The LASEREO endoscopic system is equipped with a laser light source, whereas ELUXEO is equipped with a light-emitting diode (LED) light source. Both laser-BLI and LED-BLI use a 410 nm narrow-band wavelength to contrast hemoglobin and visualize high-contrast mucosal superficial vessels and structures.40,41 The BLI-bright mode is generated by the appropriate combination of white and BLI light, which are controlled by adjusting the power of the light source. This mode enables endoscopists to obtain brighter images than those provided by the regular BLI mode and is expected to be useful for tumor detection.42 BLI is used to diagnose neoplastic or non-neoplastic polyps, sometimes in combination with magnifying observation, similar to NBI. A BLI-specific diagnostic classification of colorectal adenoma and serrated lesions proposed in Europe called BLI Adenoma Serrated International Classification has been reported to have a diagnostic accuracy of 87% to 94%.43,44 RCTs comparing the diagnostic ability of BLI and NBI for colorectal polyps have been reported.41,45 Laser-BLI, LED-BLI, and NBI showed similar diagnostic ability for colorectal neoplastic or non-neoplastic polyps in the JNET classification and the NBI International Colorectal Endoscopic classifications, thus indicating the non-inferiority of both BLIs to NBI for diagnosis.41 In addition, the diagnostic ability of BLI-bright and NBI for colorectal polyps was also similar.45
Ikematsu et al.22 reported an RCT that compared colorectal lesion detection between BLI-bright and WLE in 963 patients from eight Japanese institutions. The primary outcome of the mean number of adenomas per patient (MAP) was significantly higher in the BLI group than in the WLE group (1.27 vs. 1.01, p<0.01). Although the observation time was significantly longer in BLI (9.48 minutes vs. 8.42 minutes, p<0.01), the ADR (54.8% vs. 52.7%, p=0.52) and PDR (68.3% vs. 62.4%, p=0.06) in the BLI group were not significantly higher than those in the WLE group. Other studies also reported that the BLI-bright mode was not superior to WLE in terms of ADR and PDR.46-48 Two studies were three-arm trials that compared BLI-bright, WLE, and linked color imaging (LCI).47,48 The studies showed that LCI had the highest ADR, but the ADR between BLI-bright and WLE significantly differed. In contrast, only one RCT from Singapore demonstrated higher ADR and PDR in observations with BLI.49 This study also used BLI-bright mode, and the mode provided a significantly higher ADR (46.2% vs. 27.8%, p=0.01) and PDR (59.8% vs. 40.0%, p<0.01) than those associated with WLE. To date, no meta-analyses have investigated lesion detection using colonoscopy with BLI.
The BLI-bright mode, which provides the brightest images in the BLI series, was used in all trials. However, lesion detectability in BLI-bright mode does not seem sufficient. The reason for this may be that the image is darker in BLI-bright mode than in WLE or other observation modalities and does not enhance the color difference.
LINKED COLOR IMAGINGLCI is an IEE technology developed by Fujifilm (Fig. 2C). It improves the separation of the red color to enhance slight color differences in the mucosal membrane by using the narrow-band wavelength of 410 nm light combined with image processing.40 Some studies reported that LCI provided a better visibility score for colorectal polyps or a significant color difference between the lesion and surrounding mucosa.50-52 LCI is now available in either LASEREO or ELUXEO. There was no difference in colorectal polyp visibility between LCI with LED and laser colonoscopy.53
A recent systematic review and meta-analysis consisting of 10 RCTs (5,510 patients) comparing the ADR and PDR between LCI and WLE was published in 2022.54 This study reported that the use of LCI improved ADR, PDR, MAP, and mean number of polyps per patient (MPP) when compared with WLE (ADR: risk ratio [RR], 1.15; 95% confidence interval [CI], 1.07ŌĆō1.23; p<0.01; PDR: RR, 1.15; 95% CI, 1.08ŌĆō1.22, p<0.01; MAP: mean difference, 0.18; 95% CI, 0.09ŌĆō0.28; p<0.01; MPP: mean difference, 0.13; 95% CI, 0.01ŌĆō0.25; p=0.03). However, no statistically significant differences were found between the two groups in advanced ADR (RR, 1.03; 95% CI, 0.86ŌĆō1.24; p=0.74) or SSL detection rate (RR, 1.21; 95% CI, 0.77ŌĆō1.90; p=0.41). A potential reason for the lack of statistical differences in advanced ADR and SSL detection rates is the limited number of studies and participants included. A previous meta-analysis of seven studies published in 2020 reported similar results.55
After the publication of these meta-analyses, several data were presented that enhanced the SSL detection performance of LCI. LCI improves the visibility of colorectal serrated lesions by increasing the color difference of the ΔE* scale between serrated lesions and the surrounding mucosae in images compared with WLE.56 The color difference consists of lightness, red/green coordinates, and yellow/blue coordinates, and the calculated color difference is defined as ΔE*. Li et al.57 reported a parallel RCT that enrolled 884 patients and compared the SSL detection rate between LCI and WLE. This study demonstrated that the SSL detection rate was significantly higher in the LCI group than in the WLE group (11.3% vs. 5.9%, p<0.01). LCI use, withdrawal time, and operator experience were independent factors associated with SSL detection. Suzuki et al.23 reported a large international parallel RCT conducted in four Asian countries/regions. A total of 3,050 patients undergoing screening, diagnostic, and post-polypectomy surveillance colonoscopy were randomized into the LCI or HD-WLE groups. The detection of adenoma and other precursor lesions and the recommended post-colonoscopy surveillance schedule were compared between the LCI and HD-WLE groups. This study demonstrated that ADR (58.7% vs. 46.7%, p<0.01), PDR (68.6% vs. 59.5%, p<0.01), serrated PDR (7.3% vs. 4.0%, p<0.01), and SSL detection rates (4.8% vs. 2.0%, p<0.01) were significantly higher in LCI than in HD-WLE. The distribution of the recommended surveillance schedule categories differed significantly between the LCI and WLE groups (p<0.01); a greater number of patients who underwent colonoscopy with LCI had shorter recommended schedule durations. In the above two studies, a large number of participants (884 and 3,050) were enrolled, and all SSL were pathologically diagnosed by whole or partial lesion resection. These two advantages of the study design could have led to significantly higher SSL detection in patients with LCI than in patients with HD-WLE. The study data suggest that LCI is superior at detecting adenoma and other precursor lesions compared with WLE, potentially shortening the recommended surveillance schedule after colonoscopy.
I-SCANThe i-scan, a digital contrast method, was developed by the Pentax Corporation. This technology enhances the visibility of surface structures and vascular patterns via post-processing computer algorithms. The i-scan has four modes of image enhancement: surface enhancement (SE), contrast enhancement (CE), tone enhancement (TE), and optical enhancement (OE). Compared with the WLE (Fig. 3A), the imaging of the four modes is shown in Figure 3BŌĆōF. SE, CE, and TE can switch among the six enhancement levels. As the three modes are arranged in series, two or more of these three modes can be applied simultaneously. Switching the levels or modes of enhancement can be performed in real time without any time lag by pushing a relevant button, thus enabling efficient endoscopic observation.58,59 OE is a new mode in the i-scan generated by the combination of band-limited light and image enhancement processing technology. OE enhances the surface structure of blood vessels and mucous membranes with higher contrast than that provided by white light and supports the detection and diagnosis of lesions. OE has two modes (modes 1 and 2). OE mode 1 is designed to improve the visualization of surface microvessels by an optical filter in which the main wavelength of spectral transmission corresponds to the peak of the hemoglobin absorption spectrum (Fig. 3E).60 Mode 2 is designed to improve the contrast of white-light observation by bringing the color tone using another optical filter in which the main wavelengths of the short and mid-wavelengths correspond to the peaks of the hemoglobin absorption spectrum (Fig. 3F).60
A meta-analysis evaluated the effect of the i-scan in improving ADR compared with HD-WLE in colonoscopy. This study included five RCTs or cohort studies with 2,620 patients that directly compared the i-scan and HD-WLE. ADR was significantly higher with i-scan (RR, 1.20; 95% CI, 1.06ŌĆō1.34; p<0.01) than with HD-WLE. Subgroup analysis demonstrated that ADR was significantly higher using i-scan with SE and CE modes only (RR, 1.25; 95% CI, 1.07ŌĆō1.47; p<0.01).24 The utility of i-scan for patients with inflammatory bowel disease undergoing surveillance colonoscopy was reported. This multicenter RCT from the United Kingdom enrolled 188 patients with ulcerative colitis or CrohnŌĆÖs disease and analyzed the neoplasia detection rates between i-scan and HD-WLE.61 There was no significant difference between i-scan and HD-WLE in neoplasia detection (14.9% vs. 24.2%, p=0.14).
One study reported the diagnostic efficacy of the i-scan for the histologic prediction of colorectal polyps and compared the results with those of NBI. The overall diagnostic accuracies in the i-scan and NBI groups were 75.8% and 73.7%, respectively, with no statistical significance between the two modalities (p=0.74). Furthermore, the JNET classification had a similar level of interobserver agreement for i-scan and NBI.59
Because fewer studies have investigated i-scans than they have studied other IEEs, their effectiveness in colonoscopy is not fully understood. One meta-analysis suggested that i-scan could potentially improve the detection of colorectal lesions; however, further investigation is warranted.
ARTIFICIAL INTELLIGENCE SYSTEM/COMPUTER-ASSISTED DIAGNOSIS WITH IEEArtificial intelligence (AI), including computer-aided diagnosis (CAD) systems, has recently been developed to assist endoscopists in detecting lesions62 and predicting lesion histology.63 Recent meta-analyses have validated the efficacy of AI systems for detecting colorectal lesions. AI-assisted colonoscopies provided a 1.4 to 1.5-fold higher ADR than conventional colonoscopies.64-66 A network meta-analysis demonstrated that AI-assisted colonoscopies had a 1.2-higher ADR than advanced imaging techniques, including mucosal visualization systems or chromoendoscopy.67 A meta-analysis of nine RCTs comparing colonoscopy with or without AI detection aids showed an improvement in adenoma/polyp detection. In addition, it also showed the increased proportion of patients requiring intensive colonoscopy surveillance, defined as colonoscopy surveillance after three years based on the guidelines, by approximately 35% in the United States (RR, 1.35; 95% CI, 1.16ŌĆō1.57) and 22% in Europe (RR, 1.22; 95% CI, 1.01ŌĆō1.47).68 Therefore, AI is an important technology that improves colonoscopy quality, and some AI systems are currently used in clinical practice.
Observing the mucosa using IEE in combination with AI may further improve the detection rate of colorectal lesions. CAD EYE (Fujifilm Corporation) is an AI-aided colorectal lesion detection system designed for both HD-WLE and LCI. Therefore, a total colonoscopy can be performed by combining LCI and AI assistance. A study evaluated a CAD system in combination with LCI for colorectal polyp detection.69 A CAD system for colorectal polyp detection based on a convolutional neural network was trained using endoscopy videos of HD-WLE and LCI. This study validated the system for colorectal polyps by recording endoscopic videos in LCI mode. This study demonstrated that the sensitivity of the CAD EYE used in LCI mode was 100%, i.e., no lesions were missed. The detection rate for SSL with the CAD EYE used in LCI mode was also 100%. Another single-center retrospective study examined the utility of CAD in HD-WLE and LCI using normal and high-speed observations. The respective detection rates of CAD EYE with normal and high-speed observations were 85.0% and 67.0% for WLE, respectively, and 89.0% and 75.0% for LCI, respectively.70
Published data on the combined use of AI and IEE are limited. ENDO-AID CADe and EndoBRAIN-EYE (Olympus Corporation) are other AI-aided colorectal lesion detection systems designed to work with HD-WLE and TXI. However, no study has shown that the combined use of ENDO-AID CADe or EndoBRAIN-EYE and TXI can improve colorectal lesion detection. Future research that facilitates the development of an AI model to detect colorectal polyps (particularly SSLs) using IEE is warranted.
CONCLUSIONSIn this review, we outline the efficacy of each IEE modality with a focus on colorectal lesion detection, referencing the latest research data, mainly meta-analyses and RCTs. IEEs can be divided into two broad categories based on the nature of the image: achromatic color images constructed using narrow-band wavelength light, such as NBI and BLI, and color images based on WLE, such as TXI, LCI, and i-scan. Although NBI and BLI can improve the contrast of microstructures or microvessels on mucosal surfaces, their effectiveness in detecting lesions is limited because of their achromatic color and darker image quality. Color image IEEs, such as TXI, LCI, and i-scan, support the detection of lesions by providing brighter images and higher color contrast between the lesion and the surrounding normal mucosa. Recently, the number of reports on the effectiveness of AI in the field of endoscopy has increased. The combined use of AI and IEE can improve lesion detection. We hope that the knowledge of AI- and IEE-assisted endoscopy will further increase in the future.
NOTESConflicts of Interest
Sho Suzuki received honoraria for his lectures from Fujifilm Corporation, MC Medical Inc., and Olympus Corporation. Other authors have no potential conflicts of interest.
Author Contributions
Conceptualization: MN, SS; Data curation: MN, SS, YM, FI, KM; Formal analysis: MN, SS; Investigation: MN, SS; Methodology: MN, SS; Project administration: MN, SS; Resources: MN, SS, YM, FI, KM; Software: MN, SS; Supervision: KO, TM; Validation: SS, YM; Visualization: MN, SS; WritingŌĆōoriginal draft: MN; WritingŌĆōreview & editing: all authors.
Fig.┬Ā1.Imaging of colon cancer under white light endoscopy (WLE), narrow-band imaging (NBI), texture and color enhancement imaging (TXI) mode 1, and TXI mode 2. A type IIa+IIc early cancer is identified using (A) WLE, (B) NBI, (C) TXI mode 1, and (D) TXI mode 2. 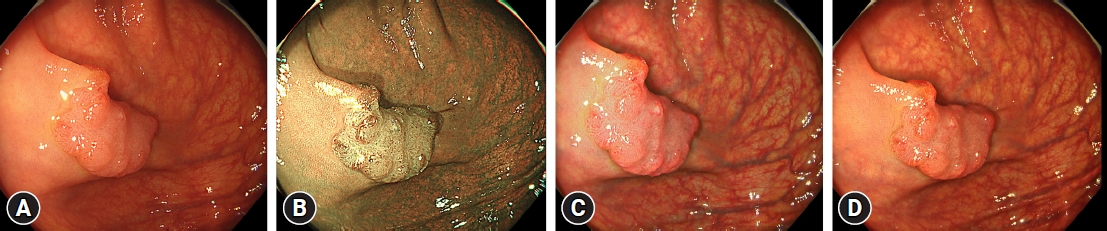
Fig.┬Ā2.Imaging of a sessile serrated lesion under white light endoscopy (WLE), blue laser imaging/blue light imaging (BLI), and linked color imaging (LCI). Flat, elevated sessile serrated lesions are shown on (A) WLE, (B) BLI, and (C) LCI. 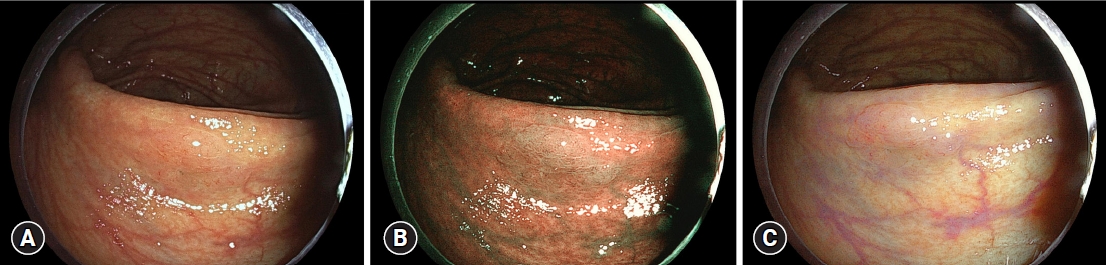
Fig.┬Ā3.Imaging of an adenoma under i-scan. A protruding adenoma lesion is shown with i-scan: (A) white-light endoscopy, (B) surface enhancement, (C) contrast enhancement, (D) tone enhancement, (E) optical enhancement mode 1, and (F) optical enhancement mode 2. 
Table┬Ā1.Brief explanation of each image-enhanced endoscopy Table┬Ā2.Studies comparing adenoma and polyp detection with IEE and WLE
REFERENCES1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71:209ŌĆō249.
2. Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012;366:687ŌĆō696.
3. Erichsen R, Baron JA, Hamilton-Dutoit SJ, et al. Increased risk of colorectal cancer development among patients with serrated polyps. Gastroenterology 2016;150:895ŌĆō902.
4. Li D, Doherty AR, Raju M, et al. Risk stratification for colorectal cancer in individuals with subtypes of serrated polyps. Gut 2022;71:2022ŌĆō2029.
5. Sekiguchi M, Matsuda T, Hotta K, et al. Post-polypectomy surveillance: the present and the future. Clin Endosc 2022;55:489ŌĆō495.
6. Kim SY, Kwak MS, Yoon SM, et al. Korean guidelines for postpolypectomy colonoscopic surveillance: 2022 revised edition. Clin Endosc 2022;55:703ŌĆō725.
7. Saito Y, Oka S, Kawamura T, et al. Colonoscopy screening and surveillance guidelines. Dig Endosc 2021;33:486ŌĆō519.
8. Gupta S, Lieberman D, Anderson JC, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2020;115:415ŌĆō434.
9. Patel SG, May FP, Anderson JC, et al. Updates on age to start and stop colorectal cancer screening: recommendations from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2022;117:57ŌĆō69.
10. Chang WY, Chiu HM. Can image-enhanced endoscopy improve adenoma detection rate? Dig Endosc 2022;34:284ŌĆō296.
11. Aminalai A, R├Čsch T, Aschenbeck J, et al. Live image processing does not increase adenoma detection rate during colonoscopy: a randomized comparison between FICE and conventional imaging (Berlin Colonoscopy Project 5, BECOP-5). Am J Gastroenterol 2010;105:2383ŌĆō2388.
12. Omata F, Ohde S, Deshpande GA, et al. Image-enhanced, chromo, and cap-assisted colonoscopy for improving adenoma/neoplasia detection rate: a systematic review and meta-analysis. Scand J Gastroenterol 2014;49:222ŌĆō237.
13. Murakami T, Kurosawa T, Fukushima H, et al. Sessile serrated lesions: clinicopathological characteristics, endoscopic diagnosis, and management. Dig Endosc 2022;34:1096ŌĆō1109.
14. Maeda Y, Kudo SE, Ogata N, et al. Use of advanced endoscopic technology for optical characterization of neoplasia in patients with ulcerative colitis: systematic review. Dig Endosc 2022;34:1297ŌĆō1310.
15. Lee W. Application of current image-enhanced endoscopy in gastric diseases. Clin Endosc 2021;54:477ŌĆō487.
16. Lee YN, Moon JH, Choi HJ. Role of image-enhanced endoscopy in pancreatobiliary diseases. Clin Endosc 2018;51:541ŌĆō546.
17. Park SB, Cha JM. Quality indicators in colonoscopy: the chasm between ideal and reality. Clin Endosc 2022;55:332ŌĆō338.
18. Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 2010;362:1795ŌĆō1803.
19. Waldmann E, Kammerlander AA, Gessl I, et al. Association of adenoma detection rate and adenoma characteristics with colorectal cancer mortality after screening colonoscopy. Clin Gastroenterol Hepatol 2021;19:1890ŌĆō1898.
20. Atkinson NS, Ket S, Bassett P, et al. Narrow-band imaging for detection of neoplasia at colonoscopy: a meta-analysis of data from individual patients in randomized controlled trials. Gastroenterology 2019;157:462ŌĆō471.
21. Sakamoto T, Ikematsu H, Tamai N, et al. Detection of colorectal adenomasa with texture and color enhancement imaging: multicenter observational study. Dig Endosc 2023;35:529ŌĆō537.
22. Ikematsu H, Sakamoto T, Togashi K, et al. Detectability of colorectal neoplastic lesions using a novel endoscopic system with blue laser imaging: a multicenter randomized controlled trial. Gastrointest Endosc 2017;86:386ŌĆō394.
23. Suzuki S, Aniwan S, Chiu HM, et al. Linked-color imaging detects more colorectal adenoma and serrated lesions: an international randomized controlled trial. Clin Gastroenterol Hepatol 2023;21:1439ŌĆō1502.
24. Aziz M, Ahmed Z, Haghbin H, et al. Does i-scan improve adenoma detection rate compared to high-definition colonoscopy? A systematic review and meta-analysis. Endosc Int Open 2022;10:E824ŌĆōE831.
25. Emura F, Saito Y, Ikematsu H. Narrow-band imaging optical chromocolonoscopy: advantages and limitations. World J Gastroenterol 2008;14:4867ŌĆō4872.
26. Machida H, Sano Y, Hamamoto Y, et al. Narrow-band imaging in the diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy 2004;36:1094ŌĆō1098.
27. B├╝rger M, Weber M, Petersen I, et al. Adenoma detection rate using narrow-band imaging is inferior to high-definition white light colonoscopy in screening and surveillance colonoscopies in daily clinical care: a randomized controlled trial. Medicine (Baltimore) 2022;101:e29858.
28. Kim H, Goong HJ, Ko BM, et al. Randomized, back-to-back trial of a new generation NBI with a high-definition white light (HQ290) for detecting colorectal polyps. Scand J Gastroenterol 2019;54:1058ŌĆō1063.
29. Staudenmann D, Liu K, Varma P, et al. Narrow band imaging versus white light for detecting sessile serrated lesion: a prospective randomized multicenter study. DEN Open 2021;2:e44.
30. Jung Y, Moon JR, Jeon SR, et al. Usefulness of narrow-band imaging for the detection of remnant sessile-serrated adenoma (SSA) tissue after endoscopic resection: the KASID multicenter study. Surg Endosc 2021;35:5217ŌĆō5224.
31. Netinatsunton N, Cheewasereechon N, Pattarapuntakul T, et al. Optical diagnosis by near-focus versus normal-focus narrow band imaging colonoscopy in colorectal polyps based on combined NICE and WASP classification: a randomized controlled trial. Clin Endosc 2022;55:645ŌĆō654.
32. Yamashina T, Setoyama T, Sakamoto A, et al. Prospective comparison of diagnostic performance of magnifying endoscopy and biopsy for sessile serrated adenoma/polyp. Ann Gastroenterol 2022;35:414ŌĆō419.
33. Lee BI, Matsuda T. Estimation of invasion depth: the first key to successful colorectal ESD. Clin Endosc 2019;52:100ŌĆō106.
34. Yoshida N, Inoue K, Yasuda R, et al. An additional 30-s observation of the right-sided colon with narrow band imaging decreases missed polyps: a pilot study. Dig Dis Sci 2018;63:3457ŌĆō3464.
35. Yoshida N, Inoue K, Dohi O, et al. Analysis of texture and color enhancement imaging for improving the visibility of non-polypoid colorectal lesions. Dig Dis Sci 2022;67:5657ŌĆō5665.
36. Abe S, Makiguchi ME, Nonaka S, et al. Emerging texture and color enhancement imaging in early gastric cancer. Dig Endosc 2022;34:714ŌĆō720.
37. Dobashi A, Ono S, Furuhashi H, et al. Texture and color enhancement imaging increases color changes and improves visibility for squamous cell carcinoma suspicious lesions in the pharynx and esophagus. Diagnostics (Basel) 2021;11:1971.
38. Tamai N, Horiuchi H, Matsui H, et al. Visibility evaluation of colorectal lesion using texture and color enhancement imaging with video. DEN Open 2022;2:e90.
39. Nishizawa T, Toyoshima O, Yoshida S, et al. TXI (Texture and Color Enhancement Imaging) for serrated colorectal lesions. J Clin Med 2021;11:119.
40. Sakamoto T, Cho H, Saito Y. Clinical applications of linked color imaging and blue laser/light imaging in the screening, diagnosis, and treatment of superficial colorectal tumors. Clin Endosc 2021;54:488ŌĆō493.
41. Higurashi T, Ashikari K, Tamura S, et al. Comparison of the diagnostic performance of NBI, Laser-BLI and LED-BLI: a randomized controlled noninferiority trial. Surg Endosc 2022;36:7577ŌĆō7587.
42. Yoshida N, Dohi O, Inoue K, et al. Blue laser imaging, blue light imaging, and linked color imaging for the detection and characterization of colorectal tumors. Gut Liver 2019;13:140ŌĆō148.
43. Subramaniam S, Hayee B, Aepli P, et al. Optical diagnosis of colorectal polyps with blue light imaging using a new international classification. United European Gastroenterol J 2019;7:316ŌĆō325.
44. Bisschops R, Hassan C, Bhandari P, et al. BASIC (BLI Adenoma Serrated International Classification) classification for colorectal polyp characterization with blue light imaging. Endoscopy 2018;50:211ŌĆō220.
45. Chang A, Munjit P, Sriprayoon T, et al. Comparison of blue laser imaging and narrow band imaging for the differentiation of diminutive colorectal polyps: a randomized controlled trial. Surg Endosc 2022;36:5743ŌĆō5752.
46. Shimoda R, Sakata Y, Fujise T, et al. The adenoma miss rate of blue-laser imaging vs. white-light imaging during colonoscopy: a randomized tandem trial. Endoscopy 2017;49:186ŌĆō190.
47. Oliveira Dos Santos CE, Malaman D, Pereira-Lima JC, et al. Impact of linked-color imaging on colorectal adenoma detection. Gastrointest Endosc 2019;90:826ŌĆō834.
48. Dos Santos CE, Malaman D, Arciniegas Sanmartin ID, et al. Effect of linked-color imaging on the detection of adenomas in screening colonoscopies. J Clin Gastroenterol 2022;56:e268ŌĆōe272.
49. Ang TL, Li JW, Wong YJ, et al. A prospective randomized study of colonoscopy using blue laser imaging and white light imaging in detection and differentiation of colonic polyps. Endosc Int Open 2019;7:E1207ŌĆōE1213.
50. Yamasaki Y, Harada K, Yamamoto S, et al. Blue laser imaging and linked color imaging improve the color difference value and visibility of colorectal polyps in underwater conditions. Dig Endosc 2020;32:791ŌĆō800.
51. Yoshida N, Hisabe T, Ikematsu H, et al. Comparison between linked color imaging and blue laser imaging for improving the visibility of flat colorectal polyps: a multicenter pilot study. Dig Dis Sci 2020;65:2054ŌĆō2062.
52. Yoshida N, Naito Y, Yasuda R, et al. Linked color imaging improves the visibility of various featured colorectal polyps in an endoscopist's visibility and color difference value. Int J Colorectal Dis 2017;32:1253ŌĆō1260.
53. Yoshida N, Hayashi Y, Kashida H, et al. Images of laser and light-emitting diode colonoscopy for comparing large colorectal lesion visibility with linked color imaging and white-light imaging. Dig Endosc 2022;34:1413ŌĆō1421.
54. Wang J, Ye C, Wu K, et al. The effect of linked color imaging for adenoma detection. A meta-analysis of randomized controlled studies. J Gastrointestin Liver Dis 2022;31:67ŌĆō73.
55. Shinozaki S, Kobayashi Y, Hayashi Y, et al. Colon polyp detection using linked color imaging compared to white light imaging: systematic review and meta-analysis. Dig Endosc 2020;32:874ŌĆō881.
56. Murakami T, Kamba E, Nomura K, et al. Linked color imaging improves visibility of colorectal serrated lesion by high color contrast to surrounding mucosa. Dig Endosc 2022;34:1422ŌĆō1432.
57. Li J, Zhang D, Wei Y, et al. Colorectal sessile serrated lesion detection using linked color imaging: a multicenter, parallel randomized controlled trial. Clin Gastroenterol Hepatol 2023;21:328ŌĆō336.
58. Kodashima S, Fujishiro M. Novel image-enhanced endoscopy with i-scan technology. World J Gastroenterol 2010;16:1043ŌĆō1049.
59. Lee JS, Jeon SW, Kwon YH. Comparative study of narrow-band imaging and i-scan for predicting the histology of intermediate-to-large colorectal polyps: a prospective, randomized pilot study. Clin Endosc 2021;54:881ŌĆō887.
60. Neumann H, Fujishiro M, Wilcox CM, et al. Present and future perspectives of virtual chromoendoscopy with i-scan and optical enhancement technology. Dig Endosc 2014;26 Suppl 1:43ŌĆō51.
61. Kandiah K, Subramaniam S, Thayalasekaran S, et al. Multicentre randomized controlled trial on virtual chromoendoscopy in the detection of neoplasia during colitis surveillance high-definition colonoscopy (the VIRTUOSO trial). Gut 2021;70:1684ŌĆō1690.
62. Milluzzo SM, Cesaro P, Grazioli LM, et al. Artificial intelligence in lower gastrointestinal endoscopy: the current status and future perspective. Clin Endosc 2021;54:329ŌĆō339.
63. Racz I, Horvath A, Kranitz N, et al. Artificial intelligence-based colorectal polyp histology prediction by using narrow-band image-magnifying colonoscopy. Clin Endosc 2022;55:113ŌĆō121.
64. Sivananthan A, Nazarian S, Ayaru L, et al. Does computer-aided diagnostic endoscopy improve the detection of commonly missed polyps? A meta-analysis. Clin Endosc 2022;55:355ŌĆō364.
65. Hassan C, Spadaccini M, Iannone A, et al. Performance of artificial intelligence in colonoscopy for adenoma and polyp detection: a systematic review and meta-analysis. Gastrointest Endosc 2021;93:77ŌĆō85.
66. Barua I, Vinsard DG, Jodal HC, et al. Artificial intelligence for polyp detection during colonoscopy: a systematic review and meta-analysis. Endoscopy 2021;53:277ŌĆō284.
67. Spadaccini M, Iannone A, Maselli R, et al. Computer-aided detection versus advanced imaging for detection of colorectal neoplasia: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol 2021;6:793ŌĆō802.
68. Mori Y, Wang P, L├Ėberg M, et al. Impact of artificial intelligence on colonoscopy surveillance after polyp removal: a pooled analysis of randomized trials. Clin Gastroenterol Hepatol 2023;21:949ŌĆō959.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
