Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Article information
Abstract
Colonoscopy plays an important role in reducing the incidence and mortality of colorectal cancer by detecting adenomas and other precancerous lesions. Image-enhanced endoscopy (IEE) increases lesion visibility by enhancing the microstructure, blood vessels, and mucosal surface color, resulting in the detection of colorectal lesions. In recent years, various IEE techniques have been used in clinical practice, each with its unique characteristics. Numerous studies have reported the effectiveness of IEE in the detection of colorectal lesions. IEEs can be divided into two broad categories according to the nature of the image: images constructed using narrow-band wavelength light, such as narrow-band imaging and blue laser imaging/blue light imaging, or color images based on white light, such as linked color imaging, texture and color enhancement imaging, and i-scan. Conversely, artificial intelligence (AI) systems, such as computer-aided diagnosis systems, have recently been developed to assist endoscopists in detecting colorectal lesions during colonoscopy. To gain a better understanding of the features of each IEE, this review presents the effectiveness of each type of IEE and their combination with AI for colorectal lesion detection by referencing the latest research data.
INTRODUCTION
The number of patients with colorectal cancer (CRC) is increasing worldwide. In 2020, there were approximately 1.9 million cases and 0.9 million deaths due to CRC worldwide.1 The adenoma–carcinoma pathway is considered the major pathway for CRC development because pre-existing adenomas develop into CRC over the years. Colorectal adenomatous polyp removal via colonoscopy has contributed to the reduction in the incidence and mortality of CRC.2 Serrated lesions, including sessile serrated lesions (SSLs) and sessile serrated adenoma/polyps (SSA/Ps), are considered CRC precursor lesions. Studies have reported that the presence of SSA/Ps or SSLs increases CRC risk by 3-fold and that the presence of such lesions with dysplasia increases the CRC risk by 5- to 10-fold compared with the risk among patients with no polyps.3,4 Therefore, screening or surveillance colonoscopies play an important role in the detection of colorectal adenomas and other precursor lesions to reduce CRC incidence and mortality.5-9
Image-enhanced endoscopy (IEE) is a modality that enhances lesion visibility by intensifying microstructure, blood vessels, and color, resulting in easier detection of colorectal lesions.10 A digital IEE that can be switched to conventional white light endoscopy (WLE) by clicking a button on the endoscope is available. First-generation IEEs, including first-generation narrow-band imaging (NBI) or Fujinon intelligent chromoendoscopy systems, did not show a good effect on improving the detection of colorectal lesions.11,12 Owing to recent advances in endoscopic technology, many types of IEE can be used in clinical practice, not only for colonoscopy13,14 but also for the endoscopic diagnosis of gastric diseases and pancreaticobiliary diseases.15,16
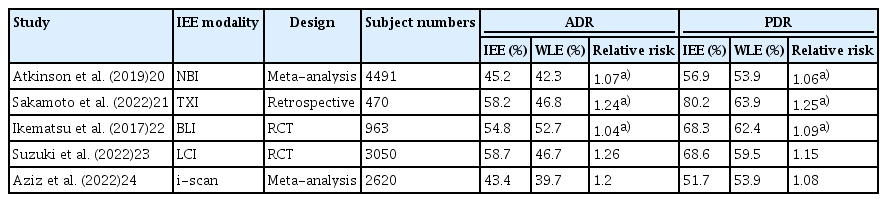
We reviewed the latest literature, mainly randomized controlled trials (RCTs) or meta-analyses published in the past five years, and showed the effectiveness of IEE in terms of adenoma detection rate (ADR) and polyp detection rate (PDR), which are established quality indicators in colonoscopy.17-19 The features of each IEE and the representative studies are summarized in Tables 1 and 2, respectively.20-24
NARROW-BAND IMAGING
NBI was developed by Olympus Corporation and emphasizes the microstructure and capillaries on the mucosal surface by modifying the center wavelength and bandwidth of light into narrow-band illumination at 415±30 nm within the hemoglobin absorption band.25 Imaging with WLE and NBI is shown in Figure 1A and 1B. NBI was originally developed for the accurate differentiation of neoplastic and non-neoplastic lesions.26 However, its ability to detect colorectal lesions remains controversial.

Imaging of colon cancer under white light endoscopy (WLE), narrow-band imaging (NBI), texture and color enhancement imaging (TXI) mode 1, and TXI mode 2. A type IIa+IIc early cancer is identified using (A) WLE, (B) NBI, (C) TXI mode 1, and (D) TXI mode 2.
A first-generation NBI system (EXERA; Olympus Corporation) was developed in 2006, and a second-generation NBI system (LUCERA; Olympus Corporation) in 2012. The second-generation model provides a brighter and higher image quality and significantly improves the distant-view image. A meta-analysis of 11 RCTs with 4,491 patients comparing adenoma detection between NBI and WLE on colonoscopy was published in 2019. This study demonstrated that ADR in NBI was significantly higher than that in WLE among all enrolled patients (45.2% vs. 42.3%, p=0.04). In the analysis stratified by the quality of bowel preparation, the difference in ADR was not significant when bowel preparation was adequate (43.2% vs. 41.4%, p=0.38), whereas NBI outperformed WLE when bowel preparation was optimal (50.2% vs. 44.4%, p=0.02). Furthermore, in an analysis stratified by the generation of NBI, NBI with a second-generation system provided better ADR than WLE (52.7% vs. 46.7%, p=0.02), whereas first-generation NBI did not (41.0% vs. 39.9%, p=0.48).20 By contrast, after the meta-analysis was published, several RCTs reported that adenoma detection in NBI was not superior to WLE or other IEE modalities. An RCT from Germany that compared the ADR between second-generation NBI and high-definition (HD) WLE in screening and surveillance colonoscopy reported that ADR (29.1% vs. 39.4%, p=0.02) and the number of polyps per patient (0.58 vs. 0.86, p=0.02) were significantly lower in second-generation NBI than in HD-WLE. Particularly, when inexperienced endoscopists performed the procedure, NBI was inferior to HD-WLE.27 A similar tandem RCT that compared second-generation NBI and HD-WLE was reported in Korea.28 The study demonstrated no differences in ADR or PDR observed between the two groups.
The utility of NBI for detecting serrated lesions is debatable. A multicenter RCT reported that the differences between NBI and HD-WLE were not remarkable in detection rates of SSL (7.5% NBI vs. 8.0% HD-WLE, p=0.852), ADR (41.0% NBI vs. 37.5% HD-WLE, p=0.531), and PDR (61.0% NBI vs. 54.0% HD-WLE, p=0.157).29 Another study investigated residual SSA detection using NBI after endoscopic resection. All lesions were randomized into the NBI and WLE groups to detect remnant tissue on the resected margin. The NBI and WLE groups showed no significant differences in the detection of remnant tissue (12.9% vs. 15.4%) or the proportion of SSA in remnant tissue (11.3% vs. 12.3%, respectively).30
NBI is widely used in the optical diagnostics of neoplastic or non-neoplastic colorectal polyps because NBI has an accuracy of >70%, either with or without magnified observation.31 NBI magnified observation also has an accuracy of >95% in diagnosing SSA/Ps, which is higher than the 74% accuracy of the histological diagnosis of a single biopsy specimen.32 Furthermore, NBI with magnified observation can be used to estimate invasive depth in colorectal tumors using the Japan NBI Expert Team (JNET) classification.33 However, based on these results, the detection performance of NBI in colonoscopy cannot be established because its darker image production than that associated with WLE is a potential drawback. The superiority of NBI in adenoma or other polyp detection might be limited by using a new-generation system that provides a brighter image and optimal bowel preparation. A study reported that adding a 30-second observation time improved lesion detection.34 A third-generation NBI system (EVIS X1; Olympus Corporation) was launched in 2020, and the polyp visibility score in this new NBI system was significantly higher than that in the WLE image.35 Such developments or modifications could improve the detection performance of NBI.
TEXTURE AND COLOR ENHANCEMENT IMAGING
Texture and color enhancement imaging (TXI) is a new IEE modality developed by Olympus and launched in 2020. TXI is a WLE-based IEE designed to improve the dimensional characterization of subtle surface irregularities and enhance brightness in images with dark areas and color changes.36 TXI has two modes in terms of enhancement factors: TXI mode 1 (texture, brightness, and color enhancement) (Fig. 1C) and TXI mode 2 (texture and brightness enhancement) (Fig. 1D). In TXI mode 1, the color contrast between red and white is greater than that in mode 2, and the mucosa appears redder. TXI mode 2 produces images that are closer to the WLE color tone.36,37
By December 2022, only one retrospective study conducted at three Japanese institutions had investigated lesion detection using TXI during colonoscopies. Sakamoto et al.21 evaluated colorectal lesion detection, including ADR and PDR, by employing TXI and HD-WLE and the factors related to the detection. The study showed that the ADR and PDR with TXI were 58.2% and 80.2%, respectively, which were higher than those associated with HD-WLE at 46.8% and 63.9%, respectively. Furthermore, using univariate and multivariate regression analyses, TXI was identified as a significant factor affecting ADR, along with age, withdrawal time, and colonoscopy type.
Other supportive studies assessing lesion visibility or color-difference scales using image datasets have also been published. A previous study evaluated the visibility score of 61 colorectal adenomas observed using TXI mode 1, WLE, NBI, and chromoendoscopy with indigo carmine dye. The visibility score for the tumor margin of TXI mode 1 was significantly higher than that of WLE (3.47 vs. 2.86, p<0.01) but lower than that of NBI (3.47 vs. 3.76, p<0.01). Another similar concept study evaluated the visibility score of 68 colorectal adenomas in a video recorded using TXI modes 1 and 2, WLE, and NBI.38 The study showed that the mean visualization scores using WLE, TXI mode 1, TXI mode 2, and NBI were 70.0, 80.5, 75.6, and 69.0, respectively, indicating that the visualization score of TXI mode 1 was significantly better than those of WLE, TXI mode 2, or NBI. Another study evaluated the visibility score for serrated colorectal polyps using endoscopic images observed with TXI mode 1, WLE, NBI, and chromoendoscopy with indigo carmine dye, similar to the other two studies.39 The visibility score of TXI mode 1 was significantly superior to that of WLE for all the 29 serrated polyps enrolled (2.93 vs. 2.27, p<0.01). However, the visibility score of TXI was inferior to that of chromoendoscopy for the imaging of serrated polyps (2.93 vs. 3.45, p<0.01) and sub-analysis of SSLs (2.90 vs. 3.45, p<0.01).
The results of these studies demonstrate that TXI mode 1 improves the visibility of colorectal adenomas and SSLs; therefore, it is possible that the detection of these lesions is improved. However, no prospective clinical trials, including RCT, have investigated lesion detection using this modality. Further clinical trials that directly compare lesion detection using WLE and other observational modes are required.
BLUE LASER IMAGING/BLUE LIGHT IMAGING
Blue laser imaging/blue light imaging (BLI) was installed in the LASEREO and ELUXEO endoscopic systems developed by the Fujifilm Corporation. WLE and BLI images are shown in Figure 2A and 2B, respectively. The LASEREO and ELUXEO have different light sources. The LASEREO endoscopic system is equipped with a laser light source, whereas ELUXEO is equipped with a light-emitting diode (LED) light source. Both laser-BLI and LED-BLI use a 410 nm narrow-band wavelength to contrast hemoglobin and visualize high-contrast mucosal superficial vessels and structures.40,41 The BLI-bright mode is generated by the appropriate combination of white and BLI light, which are controlled by adjusting the power of the light source. This mode enables endoscopists to obtain brighter images than those provided by the regular BLI mode and is expected to be useful for tumor detection.42 BLI is used to diagnose neoplastic or non-neoplastic polyps, sometimes in combination with magnifying observation, similar to NBI. A BLI-specific diagnostic classification of colorectal adenoma and serrated lesions proposed in Europe called BLI Adenoma Serrated International Classification has been reported to have a diagnostic accuracy of 87% to 94%.43,44 RCTs comparing the diagnostic ability of BLI and NBI for colorectal polyps have been reported.41,45 Laser-BLI, LED-BLI, and NBI showed similar diagnostic ability for colorectal neoplastic or non-neoplastic polyps in the JNET classification and the NBI International Colorectal Endoscopic classifications, thus indicating the non-inferiority of both BLIs to NBI for diagnosis.41 In addition, the diagnostic ability of BLI-bright and NBI for colorectal polyps was also similar.45

Imaging of a sessile serrated lesion under white light endoscopy (WLE), blue laser imaging/blue light imaging (BLI), and linked color imaging (LCI). Flat, elevated sessile serrated lesions are shown on (A) WLE, (B) BLI, and (C) LCI.
Ikematsu et al.22 reported an RCT that compared colorectal lesion detection between BLI-bright and WLE in 963 patients from eight Japanese institutions. The primary outcome of the mean number of adenomas per patient (MAP) was significantly higher in the BLI group than in the WLE group (1.27 vs. 1.01, p<0.01). Although the observation time was significantly longer in BLI (9.48 minutes vs. 8.42 minutes, p<0.01), the ADR (54.8% vs. 52.7%, p=0.52) and PDR (68.3% vs. 62.4%, p=0.06) in the BLI group were not significantly higher than those in the WLE group. Other studies also reported that the BLI-bright mode was not superior to WLE in terms of ADR and PDR.46-48 Two studies were three-arm trials that compared BLI-bright, WLE, and linked color imaging (LCI).47,48 The studies showed that LCI had the highest ADR, but the ADR between BLI-bright and WLE significantly differed. In contrast, only one RCT from Singapore demonstrated higher ADR and PDR in observations with BLI.49 This study also used BLI-bright mode, and the mode provided a significantly higher ADR (46.2% vs. 27.8%, p=0.01) and PDR (59.8% vs. 40.0%, p<0.01) than those associated with WLE. To date, no meta-analyses have investigated lesion detection using colonoscopy with BLI.
The BLI-bright mode, which provides the brightest images in the BLI series, was used in all trials. However, lesion detectability in BLI-bright mode does not seem sufficient. The reason for this may be that the image is darker in BLI-bright mode than in WLE or other observation modalities and does not enhance the color difference.
LINKED COLOR IMAGING
LCI is an IEE technology developed by Fujifilm (Fig. 2C). It improves the separation of the red color to enhance slight color differences in the mucosal membrane by using the narrow-band wavelength of 410 nm light combined with image processing.40 Some studies reported that LCI provided a better visibility score for colorectal polyps or a significant color difference between the lesion and surrounding mucosa.50-52 LCI is now available in either LASEREO or ELUXEO. There was no difference in colorectal polyp visibility between LCI with LED and laser colonoscopy.53
A recent systematic review and meta-analysis consisting of 10 RCTs (5,510 patients) comparing the ADR and PDR between LCI and WLE was published in 2022.54 This study reported that the use of LCI improved ADR, PDR, MAP, and mean number of polyps per patient (MPP) when compared with WLE (ADR: risk ratio [RR], 1.15; 95% confidence interval [CI], 1.07–1.23; p<0.01; PDR: RR, 1.15; 95% CI, 1.08–1.22, p<0.01; MAP: mean difference, 0.18; 95% CI, 0.09–0.28; p<0.01; MPP: mean difference, 0.13; 95% CI, 0.01–0.25; p=0.03). However, no statistically significant differences were found between the two groups in advanced ADR (RR, 1.03; 95% CI, 0.86–1.24; p=0.74) or SSL detection rate (RR, 1.21; 95% CI, 0.77–1.90; p=0.41). A potential reason for the lack of statistical differences in advanced ADR and SSL detection rates is the limited number of studies and participants included. A previous meta-analysis of seven studies published in 2020 reported similar results.55
After the publication of these meta-analyses, several data were presented that enhanced the SSL detection performance of LCI. LCI improves the visibility of colorectal serrated lesions by increasing the color difference of the ΔE* scale between serrated lesions and the surrounding mucosae in images compared with WLE.56 The color difference consists of lightness, red/green coordinates, and yellow/blue coordinates, and the calculated color difference is defined as ΔE*. Li et al.57 reported a parallel RCT that enrolled 884 patients and compared the SSL detection rate between LCI and WLE. This study demonstrated that the SSL detection rate was significantly higher in the LCI group than in the WLE group (11.3% vs. 5.9%, p<0.01). LCI use, withdrawal time, and operator experience were independent factors associated with SSL detection. Suzuki et al.23 reported a large international parallel RCT conducted in four Asian countries/regions. A total of 3,050 patients undergoing screening, diagnostic, and post-polypectomy surveillance colonoscopy were randomized into the LCI or HD-WLE groups. The detection of adenoma and other precursor lesions and the recommended post-colonoscopy surveillance schedule were compared between the LCI and HD-WLE groups. This study demonstrated that ADR (58.7% vs. 46.7%, p<0.01), PDR (68.6% vs. 59.5%, p<0.01), serrated PDR (7.3% vs. 4.0%, p<0.01), and SSL detection rates (4.8% vs. 2.0%, p<0.01) were significantly higher in LCI than in HD-WLE. The distribution of the recommended surveillance schedule categories differed significantly between the LCI and WLE groups (p<0.01); a greater number of patients who underwent colonoscopy with LCI had shorter recommended schedule durations. In the above two studies, a large number of participants (884 and 3,050) were enrolled, and all SSL were pathologically diagnosed by whole or partial lesion resection. These two advantages of the study design could have led to significantly higher SSL detection in patients with LCI than in patients with HD-WLE. The study data suggest that LCI is superior at detecting adenoma and other precursor lesions compared with WLE, potentially shortening the recommended surveillance schedule after colonoscopy.
I-SCAN
The i-scan, a digital contrast method, was developed by the Pentax Corporation. This technology enhances the visibility of surface structures and vascular patterns via post-processing computer algorithms. The i-scan has four modes of image enhancement: surface enhancement (SE), contrast enhancement (CE), tone enhancement (TE), and optical enhancement (OE). Compared with the WLE (Fig. 3A), the imaging of the four modes is shown in Figure 3B–F. SE, CE, and TE can switch among the six enhancement levels. As the three modes are arranged in series, two or more of these three modes can be applied simultaneously. Switching the levels or modes of enhancement can be performed in real time without any time lag by pushing a relevant button, thus enabling efficient endoscopic observation.58,59 OE is a new mode in the i-scan generated by the combination of band-limited light and image enhancement processing technology. OE enhances the surface structure of blood vessels and mucous membranes with higher contrast than that provided by white light and supports the detection and diagnosis of lesions. OE has two modes (modes 1 and 2). OE mode 1 is designed to improve the visualization of surface microvessels by an optical filter in which the main wavelength of spectral transmission corresponds to the peak of the hemoglobin absorption spectrum (Fig. 3E).60 Mode 2 is designed to improve the contrast of white-light observation by bringing the color tone using another optical filter in which the main wavelengths of the short and mid-wavelengths correspond to the peaks of the hemoglobin absorption spectrum (Fig. 3F).60
Imaging of an adenoma under i-scan. A protruding adenoma lesion is shown with i-scan: (A) white-light endoscopy, (B) surface enhancement, (C) contrast enhancement, (D) tone enhancement, (E) optical enhancement mode 1, and (F) optical enhancement mode 2.
A meta-analysis evaluated the effect of the i-scan in improving ADR compared with HD-WLE in colonoscopy. This study included five RCTs or cohort studies with 2,620 patients that directly compared the i-scan and HD-WLE. ADR was significantly higher with i-scan (RR, 1.20; 95% CI, 1.06–1.34; p<0.01) than with HD-WLE. Subgroup analysis demonstrated that ADR was significantly higher using i-scan with SE and CE modes only (RR, 1.25; 95% CI, 1.07–1.47; p<0.01).24 The utility of i-scan for patients with inflammatory bowel disease undergoing surveillance colonoscopy was reported. This multicenter RCT from the United Kingdom enrolled 188 patients with ulcerative colitis or Crohn’s disease and analyzed the neoplasia detection rates between i-scan and HD-WLE.61 There was no significant difference between i-scan and HD-WLE in neoplasia detection (14.9% vs. 24.2%, p=0.14).
One study reported the diagnostic efficacy of the i-scan for the histologic prediction of colorectal polyps and compared the results with those of NBI. The overall diagnostic accuracies in the i-scan and NBI groups were 75.8% and 73.7%, respectively, with no statistical significance between the two modalities (p=0.74). Furthermore, the JNET classification had a similar level of interobserver agreement for i-scan and NBI.59
Because fewer studies have investigated i-scans than they have studied other IEEs, their effectiveness in colonoscopy is not fully understood. One meta-analysis suggested that i-scan could potentially improve the detection of colorectal lesions; however, further investigation is warranted.
ARTIFICIAL INTELLIGENCE SYSTEM/COMPUTER-ASSISTED DIAGNOSIS WITH IEE
Artificial intelligence (AI), including computer-aided diagnosis (CAD) systems, has recently been developed to assist endoscopists in detecting lesions62 and predicting lesion histology.63 Recent meta-analyses have validated the efficacy of AI systems for detecting colorectal lesions. AI-assisted colonoscopies provided a 1.4 to 1.5-fold higher ADR than conventional colonoscopies.64-66 A network meta-analysis demonstrated that AI-assisted colonoscopies had a 1.2-higher ADR than advanced imaging techniques, including mucosal visualization systems or chromoendoscopy.67 A meta-analysis of nine RCTs comparing colonoscopy with or without AI detection aids showed an improvement in adenoma/polyp detection. In addition, it also showed the increased proportion of patients requiring intensive colonoscopy surveillance, defined as colonoscopy surveillance after three years based on the guidelines, by approximately 35% in the United States (RR, 1.35; 95% CI, 1.16–1.57) and 22% in Europe (RR, 1.22; 95% CI, 1.01–1.47).68 Therefore, AI is an important technology that improves colonoscopy quality, and some AI systems are currently used in clinical practice.
Observing the mucosa using IEE in combination with AI may further improve the detection rate of colorectal lesions. CAD EYE (Fujifilm Corporation) is an AI-aided colorectal lesion detection system designed for both HD-WLE and LCI. Therefore, a total colonoscopy can be performed by combining LCI and AI assistance. A study evaluated a CAD system in combination with LCI for colorectal polyp detection.69 A CAD system for colorectal polyp detection based on a convolutional neural network was trained using endoscopy videos of HD-WLE and LCI. This study validated the system for colorectal polyps by recording endoscopic videos in LCI mode. This study demonstrated that the sensitivity of the CAD EYE used in LCI mode was 100%, i.e., no lesions were missed. The detection rate for SSL with the CAD EYE used in LCI mode was also 100%. Another single-center retrospective study examined the utility of CAD in HD-WLE and LCI using normal and high-speed observations. The respective detection rates of CAD EYE with normal and high-speed observations were 85.0% and 67.0% for WLE, respectively, and 89.0% and 75.0% for LCI, respectively.70
Published data on the combined use of AI and IEE are limited. ENDO-AID CADe and EndoBRAIN-EYE (Olympus Corporation) are other AI-aided colorectal lesion detection systems designed to work with HD-WLE and TXI. However, no study has shown that the combined use of ENDO-AID CADe or EndoBRAIN-EYE and TXI can improve colorectal lesion detection. Future research that facilitates the development of an AI model to detect colorectal polyps (particularly SSLs) using IEE is warranted.
CONCLUSIONS
In this review, we outline the efficacy of each IEE modality with a focus on colorectal lesion detection, referencing the latest research data, mainly meta-analyses and RCTs. IEEs can be divided into two broad categories based on the nature of the image: achromatic color images constructed using narrow-band wavelength light, such as NBI and BLI, and color images based on WLE, such as TXI, LCI, and i-scan. Although NBI and BLI can improve the contrast of microstructures or microvessels on mucosal surfaces, their effectiveness in detecting lesions is limited because of their achromatic color and darker image quality. Color image IEEs, such as TXI, LCI, and i-scan, support the detection of lesions by providing brighter images and higher color contrast between the lesion and the surrounding normal mucosa. Recently, the number of reports on the effectiveness of AI in the field of endoscopy has increased. The combined use of AI and IEE can improve lesion detection. We hope that the knowledge of AI- and IEE-assisted endoscopy will further increase in the future.
Notes
Conflicts of Interest
Sho Suzuki received honoraria for his lectures from Fujifilm Corporation, MC Medical Inc., and Olympus Corporation. Other authors have no potential conflicts of interest.
Funding
None.
Author Contributions
Conceptualization: MN, SS; Data curation: MN, SS, YM, FI, KM; Formal analysis: MN, SS; Investigation: MN, SS; Methodology: MN, SS; Project administration: MN, SS; Resources: MN, SS, YM, FI, KM; Software: MN, SS; Supervision: KO, TM; Validation: SS, YM; Visualization: MN, SS; Writing–original draft: MN; Writing–review & editing: all authors.