To the Editor,
I read with interest the article by Ono et al.1 and the corresponding editorial by Noh and Kim2 published in the recent issue of Clinical Endoscopy. Ono et al.1 studied patients with hypopharyngeal squamous cell carcinoma scheduled for transoral resection under general anesthesia and found more lesions (1.47 lesions/patient) during detailed assessment just before resection compared to previous transoral endoscopy (1.17 lesions/patient) done with or without sedation. They showed that newly detected lesions were small and characterized by few changes, color, and surface ruggedness.1 These findings are important but not surprising, considering that transoral endoscopy with topical anesthesia can be uncomfortable. Even with conscious sedation, it can easily induce the gag reflex and make subsequent examination difficult. Importantly, this study reinforces the need to examine the hypopharynx, a region that is often neglected or not carefully examined in daily transoral endoscopy practice. In addition, we should also consider assessing the nasopharynx, especially if the situation permits (general anesthesia or conscious sedation) or requires it (i.e., at-risk patients, older patients for whom the pathology of the nasopharynx is more common, nasopharyngeal symptoms, history, or family history of nasopharyngeal carcinoma).
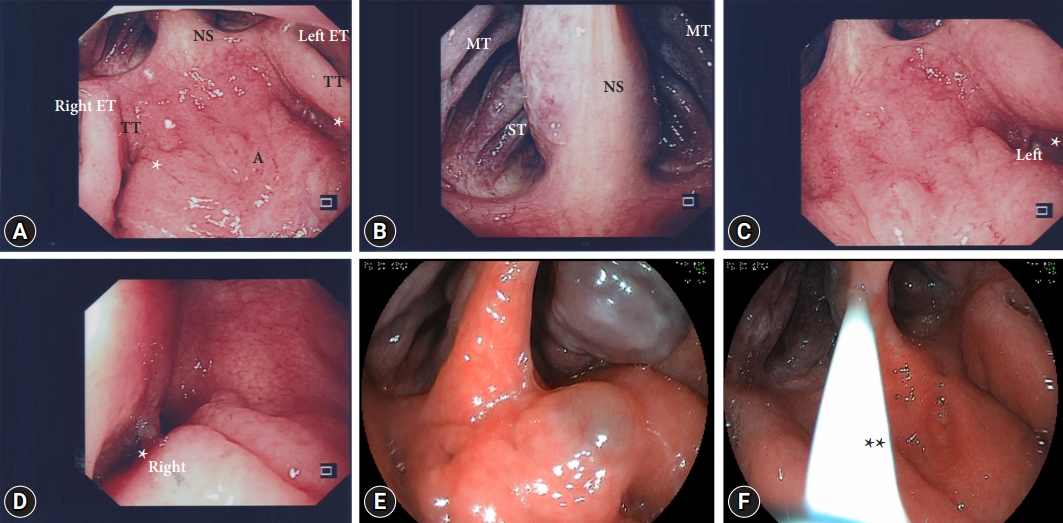
Since this year, I have routinely attempted to assess the nasopharynx during transoral endoscopy. After advancing the endoscope past the palatal arch and near or just after the palatine tonsil, the endoscope is retroflexed slowly and turned clockwise or counterclockwise until the posterior border of the soft palate or nasopharynx comes into view. The endoscope is then slightly retracted, and the nasopharynx is examined with clockwise or counterclockwise movements without touching the mucosal surface, if possible. The choana, posterior parts of the nasal septum, middle and superior turbinates, roof of the nasopharynx (adenoid pad), and eustachian tubes can be seen (Fig. 1); however, the images are inverted, top and bottom, and left and right. The fossa of Rosenmuller, may be more difficult to visualize, especially so on the right side. However, with small, gentle movement, the tip of the scope can be manipulated to visualize the floor of the fossa. This is easier when transoral endoscopy is performed under general anesthesia or conscious sedation. Even without sedation, examinations can be performed, albeit with greater difficulty. The examination usually takes less than 1 min to complete. Under general anesthesia (propofol) without intubation and in sedated patients, this can be done at the start or end of endoscopy and is probably best done at the end in unsedated patients (topical anesthesia only), depending on the patientŌĆÖs tolerance. Not unexpectedly, examination is easier with smaller-caliber endoscopes. From personal experience, nasopharyngeal examination is slightly more difficult than examination of the hypopharynx but shares similar challenges, as it can be uncomfortable.
In countries where nasopharyngeal pathologies, especially nasopharyngeal carcinoma remains common, it is useful to include examinations of the nasopharynx when patients undergo transoral endoscopy. However, several questions need to be considered and addressed when introducing an examination, either new or expanding the scope of routine examinations into daily practice. Some of these questions include: (1) how does it compare to standard practice, in this case, transnasal examinations performed by otorhinolaryngologists; (2) yields and cost effectiveness; (3) possible complications; (4) what is the learning curve; and (5) does examination of the nasopharynx impact the examination of the digestive tract? Compared to the current standard for evaluating the nasopharynx, there are differences: forward viewing for transnasal endoscopy and retroflexed viewing for transoral examination with available gastroscopes, equipment differences (caliber of endoscopes and field of vision), and the effect of the examination position (sitting or reclined supine for standard procedures and left lateral for transoral endoscopy). Furthermore, only the nasopharynx will be examined and does not include the examination of the anterior nasal space during retroflexion. However, the purpose of the proposed method is to examine the nasopharynx. The yield and cost-effectiveness require further study and will likely depend on the prevalence of nasopharyngeal pathologies. Complications are unknown but based on personal experience, these include irritation, coughing, induction of the gag reflex, and trauma to the mucosa causing bleeding or epistaxis, which, to date, have been self-limiting. However, other possible complications require further investigation. For an experienced endoscopist, learning this technique is not very difficult. However, this may not be the case for endoscopists in training. Recognizing anatomy and pathologies from retroflexed views can be easily learnt despite images being inverted. Whether the resultant discomfort induced during the examination of the nasopharynx impacts the examination of the gastrointestinal tract depends on when the examination of the nasopharynx is attempted. This is likely to be only an issue only when attempting at the start of procedure. From personal experience, even if nasopharyngeal examination had been attempted at the start and had caused some discomfort, the issue was only temporary, and examinations of the upper gastrointestinal tract could proceed and have not been compromised.
It is important to note that the proposed incorporation of nasopharynx and hypopharynx examinations into routine transoral endoscopies for now at least, should be considered as an opportunistic screening. Given that many patients undergo transoral endoscopic examinations in our daily practice, the inclusion of nasopharynx and hypopharynx examinations, even if only in selected patients, provides an opportunity to screen patients who may not necessarily undergo transnasal endoscopic examination. Patients with abnormalities should be referred for a formal evaluation. However, studies are required to assess the questions as discussed regarding incorporation of nasopharyngeal and hypopharyngeal examinations into routine transoral upper gastrointestinal endoscopies, given that the incidence of nasopharyngeal and oral cancers (i.e., lip, oral cavity, hypopharyngeal, oropharyngeal, and laryngeal cancers) varies between countries and regions.3,4