Clinical outcomes of nonvariceal upper gastrointestinal bleeding in nonagenarians and octogenarians: a comparative nationwide analysis
Article information
Abstract
Background/Aims
Nonagenarians will purportedly account for 10% of the United States population by 2050. However, no studies have assessed the outcomes of nonvariceal upper gastrointestinal bleeding (NVUGIB) in this age group.
Methods
The National Inpatient Sample database between 2016 and 2020 was used to compare the clinical outcomes of NVUGIB in nonagenarians and octogenarians and evaluate predictors of mortality and the use of esophagogastroduodenoscopy (EGD).
Results
Nonagenarians had higher in-hospital mortality than that of octogenarians (4% vs. 3%, p<0.001). EGD utilization (30% vs. 48%, p<0.001) and blood transfusion (27% vs. 40%, p<0.001) was significantly lower in nonagenarians. Multivariate logistic regression analysis revealed that nonagenarians with NVUGIB had higher odds of mortality (odds ratio [OR], 1.5; 95% confidence interval [CI], 1.3–1.7) and lower odds of EGD utilization (OR, 0.86; 95% CI, 0.83–0.89) than those of octogenarians.
Conclusions
Nonagenarians admitted with NVUGIB have a higher mortality risk than that of octogenarians. EGD is used significantly in managing NVUGIB among nonagenarians; however, its utilization is comparatively lower than in octogenarians. More studies are needed to assess predictors of poor outcomes and the indications of EGD in this growing population.
INTRODUCTION
Nonvariceal upper gastrointestinal bleeding (NVUGIB), defined as bleeding not secondary to ruptured esophageal or gastric varices proximal to the ligament of Trietz, is a common cause of hospital admission with an incidence of approximately 80 to 100 cases per 100,000 adults per year and an estimated mortality rate of 2% to 15%.1-4 Age is an important predictor of NVUGIB’s severity, as the mortality rate of NVUGIB among patients aged <60 years is approximately zero.4-6
Recent studies have shown that the prevalence of NVUGIB is more common among elderly patients aged >65 years. As our elderly population grows rapidly, more hospitalizations from upper gastrointestinal (GI) bleeding can be reasonably expected.7 However, despite projections that nonagenarians will comprise 10% of the United States (US) population by 2050, predictors of outcomes and complications among nonagenarians suffering from NVUGIB have not been studied.7-9 This study primarily aimed to analyze clinical outcomes and predictors of disease severity and mortality in nonagenarians compared to those in octogenarians admitted to the hospital for NVUGIB.
METHODS
Study design
We conducted a retrospective cross-sectional study utilizing pooled data from the US National Inpatient Sample (NIS) between 2016 and 2020. Our study included patients aged ≥80 years admitted to the hospital with a principal diagnosis of NVUGIB. The Agency for Healthcare Research and Quality maintains the NIS database as a part of the Healthcare Cost and Utilization Project (HCUP). This database is the largest all-payer database obtained from acute-care hospitals across the US. The database contains approximately 40 discharge diagnoses and 25 procedures for every patient based on the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes.
Study population
Patients aged ≥80 years with a primary diagnosis indicating active bleeding from an upper GI source were included in our study cohort. If the primary diagnosis did not specify the source of the upper GI bleeding, a possible source of the upper GI bleeding (UGIB) had to be associated with a secondary diagnosis. This methodology has been validated in previous studies [1]. The ICD-10 codes used to generate the variables are included in Supplementary Table 1. Patients aged <80 years and elective admissions were excluded from our study. Patients were categorized into those aged ≥90 years (“nonagenarians”) or 80 to 89 years (“octogenarians”).
Study variables and clinical outcomes
Variables, including age, sex, race, insurance status, mortality, and length of stay, were provided by the NIS database. Variables that provided hospital-level information, such as hospital size, location, and teaching status, were also included in the database. The comorbidity variables were generated from ICD-10 codes using Exlixhauser’s Comorbidity Software Refined for ICD-10-CM ver. 2021.1, a software developed by the HCUP.10 The primary outcome was in-hospital mortality. The secondary outcomes included mean length of stay and total cost of hospitalization. The two study groups were compared in terms of the proportion of patients who had undergone esophagogastroduodenoscopy (EGD), mechanical ventilation or received blood transfusion. Subgroup analysis compared the outcomes of nonagenarians who had undergone EGD with those who had not. Moreover, multivariate logistic regression analyses were performed for predictors of mortality and EGD utilization.
Statistical analysis
STATA ver. 15 (StataCorp.) was used to perform statistical analysis. The data analysis results were weighted, given the sampling design of the NIS database. Linear variables were compared between the two groups using the Student t-test. Chi-square tests were used to compare categorical variables. Univariate regression analysis was used to calculate the unadjusted odds ratio (OR) for the primary outcomes. Variables with p<0.2 in the univariate analysis were used to build a multivariate logistic analysis model to adjust for potential confounders. Statistical significance was set at p<0.05.
Ethical statements
According to Health Insurance Portability and Accountability Act regulations, the study was exempt from Institutional Review Board approval, given that the study source is a limited, anonymous dataset.
RESULTS
The number of patients aged ≥80 years admitted with NVUGIB between 2016 and 2020 was 279,022, with 78,462 and 200,560 patients in the nonagenarian and octogenarian groups, respectively. The mean age of patients in the octogenarians group was 84 years. The mean age of those in the nonagenarian group was not measured, as all patients aged ≥90 years in the NIS database were 90 years old. Compared with the octogenarians, the nonagenarians were more likely to be white, female, and to have a Charlson’s comorbidity index (CCI) of ≥3 (Table 1). CCI is a morbidity score extracted from the NIS database’s ICD-10-CM codes, and it calculates mortality risk.11 The nonagenarians were less likely to be admitted to a large, urban, or teaching hospital. The inpatient mortality was higher in nonagenarians (4% vs. 3%, p<0.001). Nonagenarians had 50% higher odds of mortality than that of octogenarians in the multivariate logistic regression analysis performed to adjust for confounders (OR, 1.5; 95% confidence interval [CI], 1.3–1.7; p<0.001). The cost of hospitalization was lower in nonagenarians (16,812 US dollars (USD) vs. 18,658 USD), and there was a statistically significant slight increase in the mean length of stay compared with that of octogenarians. Nonagenarians were less likely to undergo EGD (30% vs. 48%, p<0.001), mechanical ventilation (2% vs. 4%, p<0.0001), or receive a blood transfusion (27% vs. 40%, p<0.0001) than octogenarians were (Table 2). A higher proportion of nonagenarians had palliative care consults than octogenarians did (5% vs. 4%, p<0.0001).
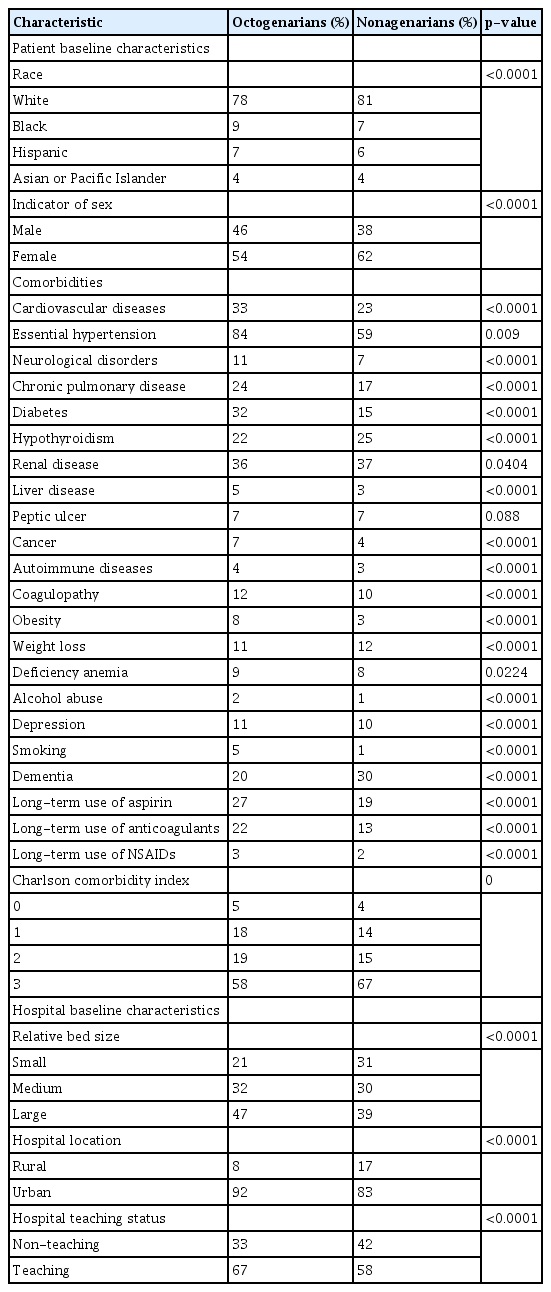
Baseline characteristics of the octogenarians and nonagenarians with nonvariceal upper gastrointestinal bleeding
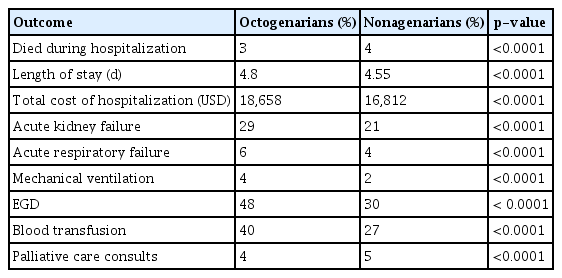
Clinical outcomes of octogenarians and nonagenarians with nonvariceal upper gastrointestinal bleeding
Predictors of EGD utilization were measured using multivariate logistic regression analysis. Nonagenarians had lower odds of undergoing EGD after adjusting for multiple patient and hospital factors than octogenarians had (OR, 0.86; 95% CI, 0.83–0.89). The analysis also showed that men and white patients were more likely to undergo EGD (Fig. 1).
Predictors of esophagogastroduodenoscopy utilization in patients ≥80 years with nonvariceal upper gastrointestinal bleeding.
A subgroup analysis to compare nonagenarians who had undergone EGD with those who had been managed without EGD revealed a lower percentage of patients with CCI ≥3 in the EGD group. The EGD group had a lower percentage of patients with dementia but a higher percentage of patients on long-term aspirin or anticoagulation. The EGD group had a higher rate of acute renal failure, acute respiratory failure, mechanical ventilation, and blood transfusion (Table 3). The two groups’ mortality rate was the same (4% vs. 4%, p=0.48).
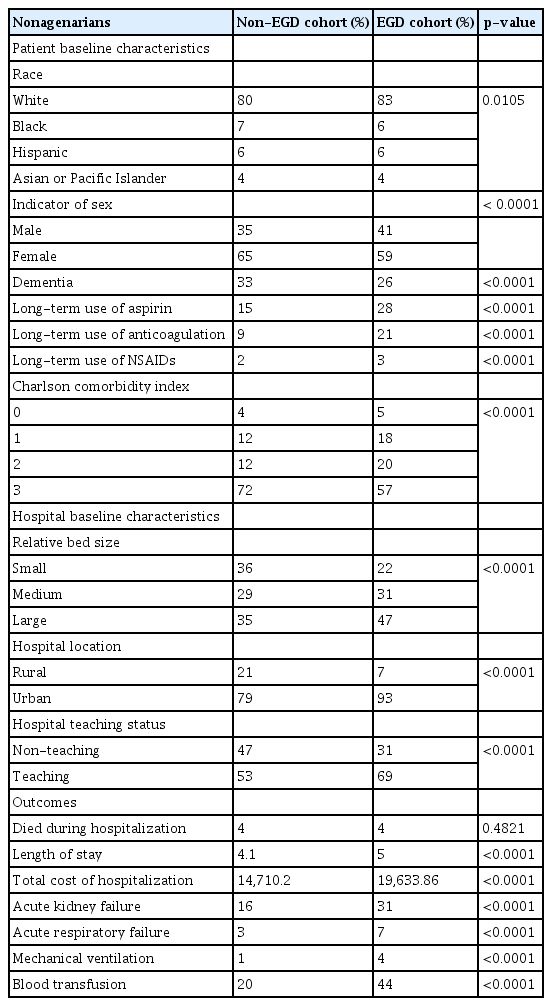
Baseline demographic characteristics and hospital outcomes of the two cohorts of nonagenarians with NVUGIB (non-EGD vs. EGD cohort)
Multivariate logistic regression analysis was performed to assess the clinical factors impacting mortality in elderly patients undergoing EGD. It revealed that hypertension and long-term use of aspirin and anticoagulants were associated with improved mortality (Fig. 2). Conversely, higher mortality was associated with cardiovascular diseases, liver disease, cancer, and other factors (Fig. 2).
DISCUSSION
Nonagenarians are expected to account for 10% of the US population by the year 2050, and the proportion of elderly adults suffering from acute upper GI bleeds continues to increase.12,13 Ultimately, an increase in age often comes with greater comorbidities, some of which require patients to adhere to life-long antiplatelet and anticoagulant medication, placing them at a higher risk of GI bleeding.14 Fortunately, endoscopic intervention for acute upper GI bleeding is well-tolerated and effective in most patients, and the severity of acute UGIBs between octogenarians and younger patients is similar.7,13,14 However, until now, no studies have assessed the outcomes of NVUGIB in nonagenarians. In this study, we analyzed the clinical outcomes of nonagenarians compared with octogenarians admitted to the hospital for NVUGIB. We also analyzed demographic and clinical factors to understand better disease severity and mortality predictors in this age group.
To our knowledge, our study is the first to show that nonagenarians are at higher risk of mortality from UGIB than octogenarians are. This age group has a higher risk of mortality after adjustment for confounders. This novel finding is fascinating, given that in similar studies evaluating the safety and efficacy of endoscopic intervention for acute UGIB secondary to peptic ulcer disease, no differences in mortality between octogenarians and younger patients were found.15,16 The mortality rate observed in our study was lower as we only assessed the same-admission mortality. In addition, the mortality of NVUGIB has been down-trending over the last two decades.1 We also observed that nonagenarians underwent EGD and mechanical ventilation at much lower rates and received fewer blood transfusions than octogenarians did. Given that higher rates of palliative care consults were observed within the nonagenarian group compared with those in octogenarians and that nonagenarians tended to have higher CCIs, it is reasonable to assume that invasive interventions were not as frequently pursued due to differences in goals of care associated with advanced age. This can help explain the higher mortality observed in the nonagenarian group.
We conducted a subgroup analysis to compare nonagenarians with NVUGIB who underwent EGD with those who did not. The analysis of baseline characteristics revealed that the EGD group had a lower burden of comorbidities and lower prevalence of dementia (Table 3), suggesting that these patients might have been selected based on better functional status compared with those of patients who had not undergone EGD. In addition, a higher percentage of patients in the EGD group were admitted to teaching and large hospitals, likely due to the higher complexity and severity of admissions in these settings. The EGD group exhibited higher rates of mechanical ventilation and blood transfusion, which can be attributed to the selection of sicker patients for the procedure. One possible explanation for the higher severity of NVUGIB in the EGD group is the higher use of aspirin or anticoagulation (Table 3).
Nevertheless, the mortality rate was similar between the two groups, supporting the safety of EGD in nonagenarians. The factors that could have led to similar mortality between both groups despite the differences in the association of aspirin and anticoagulation use, which was more prevalent in the EGD group, with lower mortality, and the association of dementia, which was more prevalent in the non-EGD group, with higher mortality in patients with NVUGIB (Fig. 2). Moreover, the more aggressive management of the sicker patients in the EGD group could have contributed to comparable outcomes. Notably, patients who underwent inpatient EGD might have been affected by coding bias, as their admission to the intensive care unit could have resulted in a higher likelihood of coding for acute organ failure. The large sample size and depth of information collected on our patients’ cohort is a strength of this study. However, one of the study’s limitations was our inability to review electronic medical records to better understand patient-tailored medical decision-making during hospital admission. Moreover, despite identifying various factors through our multivariate analysis that influence mortality in octogenarians and nonagenarians undergoing EGD (Fig. 2), it is challenging to determine the specific indications for EGD in this population based on our retrospective analysis.
In conclusion, managing NVUGIB in elderly patients is complex, as older patients carry significantly more morbidities and may require medications that predispose them to NVUGIB. Our study revealed that nonagenarians are at a higher risk of NVUGIB mortality than octogenarians are. Moreover, while EGDs were used significantly in managing NVUGIB among nonagenarians, their utilization was comparatively lower than in octogenarians. Moreover, we highlighted different clinical factors that impacted mortality in elderly patients undergoing EGDs. More studies are needed to assess predictors of poor outcomes and indications for EGD among nonagenarians; however, gastroenterologists should be prepared to encounter a rising number of NVUGIB necessitating endoscopic treatment in this rapidly-growing population.
Supplementary Material
Supplementary Table 1. International Classification of Diseases, Tenth Revision (ICD-10) diagnostic and procedural codes utilized in the study.
Supplementary materials related to this article can be found online at https://doi.org/10.5946/ce.2023.130.
Notes
Conflicts of Interest
Michel Kahaleh, MD received grant support from Boston Scientific, Fujinon, Apollo Endosurgery, Cook Endoscopy, Olympus, and MI Tech. He is a consultant for Boston Scientific, ABBvie. None of these funds were related to this study. The other authors have no potential conflicts of interest.
Funding
None.
Author Contributions
Conceptualization: KE, MK; Methodology: KE, JL, EE, FJ, SN; Supervision: MK, SH; Writing–original draft: JL, KE, EE; Writing–review & editing: KE, JL, FJ, SN, SH, MK.