INTRODUCTION
Pancreatic pseudocyst is a well-known complication of acute and chronic pancreatitis. Most pseudocysts spontaneously regress with conservative treatment [1]. However, serious complications, including cystic rupture, hemorrhage, infection, and pseudoaneurysm rupture, may increase the risk of morbidity and mortality [2]. In particular, spontaneous rupture of a hemorrhagic pancreatic pseudocyst may be life-threatening. Herein, we report a rare case of a spontaneous rupture of a hemorrhagic pancreatic pseudocyst in a patient with chronic pancreatitis, which was successfully treated with endoscopic ultrasound (EUS)-guided gastrocystostomy with a fully covered self-expandable metallic stent (FCSEMS).
CASE REPORT
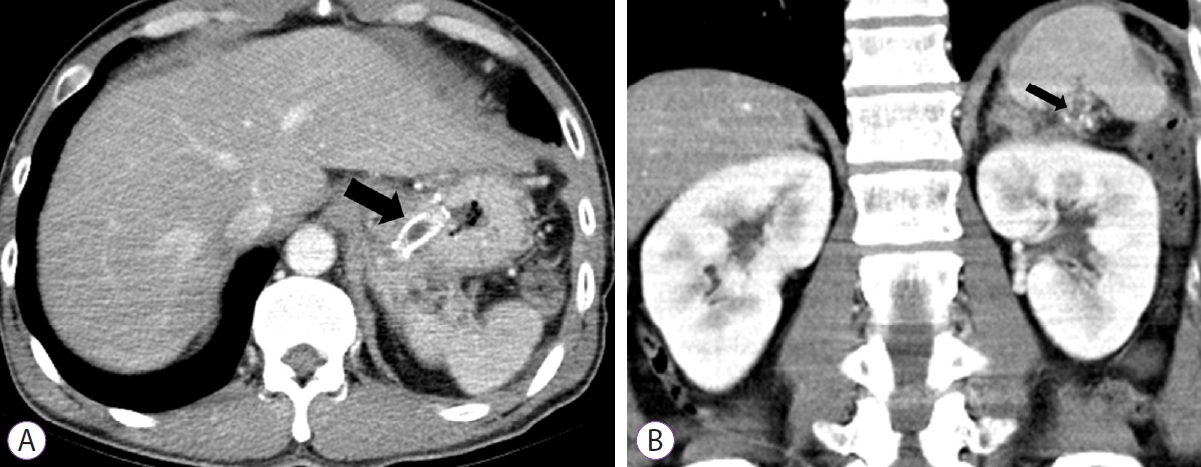
A 46-year-old man with alcoholic chronic pancreatitis was admitted to our hospital with severe upper abdominal pain and high fever (temperature up to 38.5ТАC) for 1 day. A week ago, he was scheduled to undergo EUS-guided intervention for a pseudocyst in the pancreatic tail, about 9 cm in size, which was identified on magnetic resonance imaging (Fig. 1A). Laboratory tests revealed low hemoglobin (9.8 g/dL) and elevated inflammatory markers (white blood cell count 17,500/ТЕL and C-reactive protein 324.56 mg/L). Abdominal computed tomography revealed that the hemorrhagic pancreatic pseudocyst had ruptured, with direct extension to the splenorenal ligament and subcapsular splenic space. However, there was no evidence of active contrast extravasation (Fig. 1B, C). EUS showed an anechoic thick-walled cystic lesion, 9 cm in size (Fig. 2A). Transgastric wall puncture was performed using a 19-gauge needle for fine-needle aspiration (EZ shot 3plusTM; Olympus, Tokyo, Japan), avoiding intervening vessels (Fig. 2B). Thick and turbid bloody fluid with debris was aspirated, and a 0.025-inch guidewire (VisiglideТЎ; Olympus Medical Systems, Tokyo, Japan) was coiled into the pseudocyst cavity under fluoroscopic guidance (Fig. 2C). Subsequently, tract dilation was performed using a 6-Fr cystotome (Wilson-Cook Medical Inc., Bloomington, IN, USA), and an FCSEMS (BONA-ALТЎ 10 mm diameter, 5 cm total length; Standard Sci Tech Inc., Seoul, Korea) with a 7-Fr nasocystic drainage tube was inserted for additional lavage and aspiration (Fig. 2D, E). The patient inadvertently removed the nasocystic tube 2 days after the procedure, but the FCSEMS was found to be well positioned on the X-ray. The clinical hallmarks improved, and the patient was discharged 12 days later. An abdominal computed tomography scan 4 weeks later showed complete resolution of the ruptured pseudocyst and perisplenic fluid collection (Fig. 3A, B). The metal stent that was placed for gastrocystostomy was removed. The patient recovered without any recurrent symptoms.
DISCUSSION
Spontaneous rupture of a hemorrhagic pancreatic pseudocyst is rare; however, it can be fatal if not properly managed. The exact mechanism is still unknown. One possible explanation of its occurrence in the current case could be that the pathologic changes, such as its erosion or disruption due to either severe inflammation or the activated lytic enzymes in the pseudocyst, in a superficial vessel may have weakened the pseudocyst wall, subsequently resulting in the spontaneous rupture of the hemorrhagic pseudocyst [3]. Pseudocyst rupture into the gastrointestinal tract may lead to bleeding or spontaneous regression; however, rupture into the peritoneal cavity may result in peritonitis or shock that requires urgent surgical intervention [4,5]. The presence of a high concentration of enzymes, such as amylase, lipase, and other proteolytic enzymes, in the pseudocyst can lead to its invasion into adjacent structures [6]. Traditional management of a ruptured pancreatic pseudocyst involves surgical treatment such as Roux-en-Y cystojejunostomy, distal pancreatectomy, and lavage [7].
EUS-guided drainage has been reported to be a valuable treatment option for pancreatic pseudocysts [8]. However, its usefulness in treating ruptured pancreatic pseudocysts is limited. In the present case, hemorrhagic cystic fluid from the ruptured pancreatic pseudocyst only occupied the area between the pancreatic tail and the perisplenic space because of the splenorenal and the gastrosplenic ligaments. Therefore, EUS-guided drainage was considered as the primary treatment, and complete resolution of the ruptured pseudocyst was achieved after the procedure. Substantial controversies remain regarding the use of plastic stents or FCSEMS during EUS-guided pseudocyst drainage. FCSEMSs conserve more time, are technically easier to use, have a higher treatment success rate, and require a shorter period for pseudocyst resolution than plastic stents [9]. In particular, in pseudocysts with thick debris, as in our patient, an FCSEMS may be a more suitable option with EUS-guided drainage.
In conclusion, according to our experience, EUS-guided drainage with an FCSEMS may be considered an effective alternative to surgery in cases where there is a localized fluid collection due to the ruptured pancreatic pseudocyst.