Nasoenteric tubes are a commonly used form of enteral access for temporary enteral nutrition (EN).1 It comprises nasogastric and postpyloric (nasoduodenal and nasojejunal) tubes. Both nasogastric and nasojejunal tubes are equally effective in terms of safety and efficacy; however, nasojejunal tubes are preferred in patients with a high risk of aspiration and pancreatitis.2 Adverse events (AEs) are common with nasojejunal tubes and can be categorized as mechanical, infectious, and metabolic.1,3 Minor events related to the tubes include local discomfort, foreign body sensation, mild epistaxis, tube blockage, tube dislodgment, and kinking. Major AEs include perforation, fistula formation, and major bleeding episodes.3 Perforation can occur intraprocedural or postprocedure as a delayed complication. The risk of delayed perforation in the small bowel is higher because of thin walls.4 We report duodenal perforations in the nasojejunal tube at various centers.
After experiencing perforation in two patients with a specific nasojejunal tube (16 French, Shaili Endoscopy), we collected data from various centers. Five patients with nasojejunal tube-related perforations were retrospectively identified. These perforations were confirmed using computed tomography (CT) or endoscopy. Depending on the severity of symptoms and the availability of experts, the patients were managed. After the procedures, all patients were managed using a standard protocol, which included keeping them nil per os (NPO) and administration of proton pump inhibitors (PPIs), intravenous (IV) fluids, and antibiotics. The patients were gradually started on a liquid diet, followed by a semi-solid diet.
A total of 740 patients received a nasojejunal tube (16 Fr, Shaili Endoscopy; Fig. 1) for various indications at four centers in the last 12 years. Five patients (median age, 34 years; range, 16ã48, female, 4) were identified as having nasojejunal tube-related perforations in the last 1 year (2022) (Table 1). In all five patients, the tubes were placed at or just beyond the duodenojejunal flexure using a transnasal ultrathin scope (GIF-H190N; Olympus). No intraprocedural or immediate postprocedural complications were observed. Perforation was diagnosed using CT in four patients and endoscopy in one patient. The median time from nasojejunal tube placement to perforation detection was 5 days (range, 3ã9 days). Of the five patients, two underwent endoscopic closure, two required surgery, and one was managed conservatively. All patients were asymptomatic at a median follow-up of 4 months (range, 3ã12 months).
Case 1. A 48-year-old woman presented with retching followed by hematemesis for 1 day. Gastroscopy revealed a deep MalloryãWeiss tear in the lower esophagus with no high-risk stigmata. A nasojejunal tube was placed to provide nutrition. After 5 days, she complained of abdominal pain; therefore, a CT scan was performed which showed that a nasojejunal tube had perforated the duodenal second portion (D2) and entered the peritoneal cavity with a tip lying near the right lobe of the liver. Gastroscopy was performed and the tube was withdrawn under visual guidance. A small (5ã6 mm) defect was noticed in duodenal second portion, which was closed with an over-the-scope clip (OTSC, 12T; Ovesco Endoscopy; Fig. 2). On day 3, she was started on a liquid diet and discharged on PPI and antibiotics. At 3 months follow-up, the patient was asymptomatic.
Case 2. A 35-year-old man was diagnosed with acute pancreatitis, and a nasojejunal tube was placed for nutrition. After 5 days, the patient complained of increased abdominal pain and tube blockage. Gastroscopy revealed that the tube had dislodged from the jejunum into the duodenum with the tip penetrating the wall of duodenal second portion. Upon slow withdrawal of the tube, a full-thickness defect (5 mm) was noted in duodenal second portion, which was closed successfully with an OTSC clip (12t; Fig. 3). At 3 months follow-up, the patient was asymptomatic.
Case 3. A 16-year-old girl with acute pancreatitis underwent a nasojejunal tube placement for nutrition. On day 5, the patient complained of diffuse abdominal pain, and abdominal palpation revealed rigidity and guarding. A CT scan revealed that the nasojejunal tube had perforated the second part of the duodenum with the tip lying in the peritoneal cavity. She underwent emergency surgery, during which a small defect was noted in the lateral wall of the duodenal second part, which was repaired using an omental patch. At 1 year follow-up, the patient was doing well.
Case 4. A 34-year-old woman with sigmoid achalasia presented with chest pain and mild hematemesis. CT chest showed a dilated esophagus with a possible site of perforation and a loculated right pleural effusion (Fig. 4). Gastroscopy revealed a dilated esophagus with a full-thickness defect in the mid-esophagus and mild narrowing at the gastro-esophageal junction. The nasojejunal tube is placed under endoscopic guidance for nutrition. However, 3 days later, the patient complained of abdominal pain and tube blockage. A CT scan of the abdomen revealed a small, loculated collection, with the tip of the tube penetrating the wall of the duodenum in the third to fourth regions and lying just outside the lumen (Fig. 5). The tube was removed, and the patient was managed conservatively with NPO, IV fluids, and antibiotics. The pain gradually subsided, and on day 3, she was started on liquids. At 6 months follow-up, the patient underwent laparoscopic Heller myotomy for achalasia.
Case 5. A-19-year-old woman suspected of having superior mesenteric artery syndrome had nasojejunal tube placed. After 9 days, the patient complained of abdominal pain. CT showed that the nasojejunal tube had perforated the second part of the duodenal wall, with the tip lying in the peritoneal cavity. She underwent emergency duodenojejunostomy. At 4 months of follow-up, the patient was asymptomatic.
Nasoenteric tubes are preferred to oroenteral tubes for EN. These tubes include nasogastric, nasoduodenal, and nasojejunal tubes, which are primarily used for temporary nutrition (4ã6 weeks). No difference was noted between the nasoduodenal and nasojejunal tubes; however, the placement of the nasojejunal tubes was more difficult owing to the longer distance of the jejunum from the nose and the difficulty in navigating the tubes across the bowel loops, making it a time-consuming process. Conversely, nasoduodenal tubes have a higher risk of dislodging into the stomach. Nasojejunal tubes are primarily used in patients at high risk for aspiration and acute pancreatitis.1,3 Nasojejunal tubes are placed blindly at the bedside or under endoscopic or fluoroscopic guidance. However, very high failure rates have been reported with blind placement (40%ã50%). Fluoroscopic and endoscopic methods of placement have been shown to be successful in >90% of cases.5 Although the fluoroscopic method was associated with a shorter time, with endoscopic techniques and increasing experience, more distal placement was possible within a shorter time.5 Many techniques have been described for endoscopic nasojejunal tube placement, including the drag and pull, over-the-guidewire, transnasal, and through-the-scope methods. In our study, all nasojejunal tubes were placed under endoscopic guidance with a transnasal scope and over-the-guidewire.
The characteristics of various nasojejunal tubes varies in material (polyvinyl chloride, polyurethane, polyethylene, and silicone), size (3.5 Fr to 16 Fr in diameter), length (150 to 170 cm), tip (weighted and non-weighted), removable guidewire, and additional features such as radiopaque markers and suture loops.6 An randomized controlled trial compared endoscopically placed two common polyurethane tubes, which differed in weighted tip and general stiffness. A stiffer tube was placed in the jejunum more frequently, and more flexible tube required a significantly longer procedure time and resulted in lower nursing satisfaction because of frequent leakage and dislodgment.7 Rigid tubes have a higher chance of distal placement (into the jejunum) than flexible tubes. The tube used in this case series was made of polyethylene and was stiff with a non-weighted tip and removable guidewire (Fig. 1). Data comparing tubes made from different materials are lacking.
AEs related to feeding tubes are common and reported in 0.5% to 32%.3,6,8 These AEs are classified as mechanical (tube related), infectious, and metabolic.3 Nasojejunal tubes can lead to mucosal ulceration, bleeding, and bowel perforation due to continuous friction with the mucosa during peristalsis. The reported perforation sites due to tubes are the nasal septum, intracranial, pyriform fossa, esophagus, stomach, and small bowel.8 Although bowel perforation is a rare phenomenon, it can occur and is associated with high morbidity. In this case series, duodenal perforation was noticed in 0.67% of the patients. There is a dearth of data comparing nasoduodenal and nasojejunal tube-induced small bowel perforations. The majority of bowel perforations through nasojejunal/nasoduodenal tubes are reported in the duodenum followed by the jejunum.8,9 Superior and inferior flexures of the descending duodenum are at the highest risk of perforation by the rigid tube.10 Another possible reason for perforation could be the hardening of the nasoenteric tubes in the small bowel due to which, the tube will have difficulty in navigating the curved and relatively fixed duodenum. Continuous friction between the hard tube and duodenal mucosa with peristalsis can lead to mucosal ulceration and perforation. Therefore, it is advisable to place the tube in a more mobile jejunum.10 However pushing a stiff tube beyond the duodenum may not always be possible and is risky. Hence, avoiding blind insertion of the tube and using fluoroscopy or endoscopy for jejunal insertion are recommended. Although the tube was placed near and beyond the duodenojejunal flexure, all perforations occurred in the duodenum. This could be due to dislodgement of the tube in the duodenum as it was not inserted deep into the jejunum.
In patients receiving nasojejunal feeding, perforation should be suspected when new-onset abdominal pain or a change in the characteristics of the present abdominal pain is observed. In the case of tube blockage, avoid fiddling with the tube blindly and use fluoroscopy or endoscopy to ensure the position. If the tube does not follow a routine curve on fluoroscopy, ingestion of contrast is avoided, and the tube should not be removed before performing any imaging. Tube-related perforations are usually small (5ã6 mm) and are likely to be missed during intervention. Therefore, withdraw the tube visually during the intervention (surgery or endoscopy) to avoid missing the defect (Fig. 3).
The management of tube-induced perforations depends on the severity of symptoms and the presence or absence of peritonitis. Tube-related perforations are usually small; therefore, endoscopic closure can be achieved in patients without peritonitis and by the experts. In this case series, two patients underwent endoscopic closure. All patients are currently asymptomatic; however, because of these incidences, the use of this tube has been restricted.
The decision to use a nasojejunal feeding tube should be carefully considered and individualized. Although data on the choice of nasojejunal tubes are lacking, the availability of the tube, patient preference, patient performance status, and endoscopistãs experience should be considered. Tubes can be placed in the horizontal part of the duodenum or jejunum over the guidewire under endoscopic or fluoroscopic guidance. Post-insertion, the position of the tube was confirmed using fluoroscopy by injecting contrast. The patient's vital signs and clinical condition were frequently monitored, especially after insertion of the nasojejunal tube. The position of nasojejunal tube was checked regularly by using auscultation, pH, and radiographic confirmation to ensure proper placement. Routine radiography is neither necessary nor cost-effective for all patients with nasojejunal tubes. However, imaging studies may be useful in specific situations, such as suspected complications or changes in the patientãs clinical condition.
After discharge, patients receiving nasojejunal feeding should be followed closely, either on phone calls or regular physical visits at the clinic. Educate patients and caregivers regarding the signs and symptoms of nasojejunal feeding complications and when to promptly seek medical attention.
One limitation of this study was that it was a retrospective study with a small sample size. Further evaluation is needed to determine whether the stiffness of the tube is responsible for the perforations.
Nasojejunal tube-related perforation is a rare and serious complication that requires prompt medical attention. To reduce the risk of perforation, it is important to carefully choose the tube and closely monitor patients receiving tube feeding.
NOTESAuthor Contributions
Conceptualization: RC; Data curation: RC, CG, KKR, CS; Formal analysis: RC; Investigation: RC, CG; Methodology: SR, KKR, NP; Project administration: RC: Resources: RC; Supervision: SR; Validation: KKR, CS; Visualization: SR; Writingãoriginal draft: RC; Writingãreview & editing: all authors.
Fig.ô 1.Nasojejunal feeding tube (16 Fr) from Shaili endoscopy. (A) Whole tube with removal guidewire. (B) Tip of nasojejunal tube. (C) Removable guidewire. 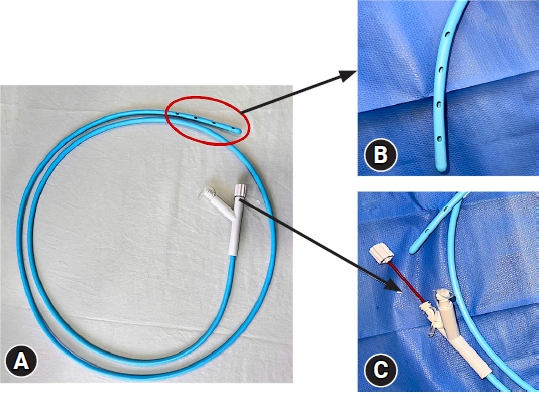
Fig.ô 2.Detection of perforation on computed tomography scan and closure with over-the-scope clip (OTSC) in case 1. (A) Contrast-enhanced computed tomography of the abdomen showed the tube had perforated the duodenum and lying in the subhepatic area (red circle). (B) Full-thickness defect in the duodenum in D2. (C) Mild suction was applied, and the defect was pulled in cap of the OTSC device. (D) OTSC was applied, and complete closure of the defect was achieved. 
Fig.ô 3.Nasojejunal tube-related duodenal perforation closure was performed with over-the-scope clip (OTSC) in case 2. (A) Tip of the tube was seen penetrating the duodenal wall. (B) After withdrawal of the tube, full-thickness defect was noticed. (C) OTSC device was taken, and the defect was sucked into the cap with mild suction. (D) Complete closure was achieved with the OTSC clip. 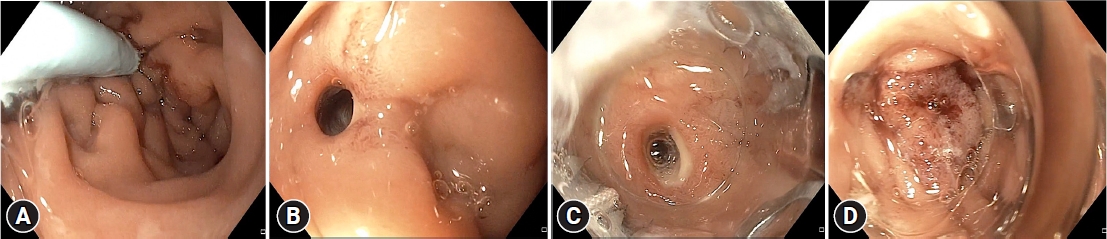
Fig.ô 4.Chest computed tomography showing dilated esophagus with possible site of perforation and right-sided loculated pleural effusion. 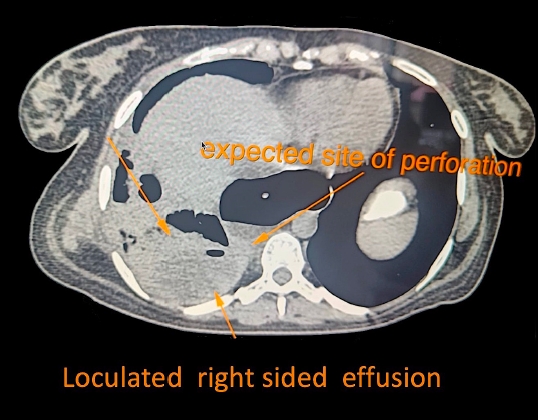
Fig.ô 5.Detection of perforation on contrast-enhanced computed tomography (CT) abdomen in case 4. (A) CT abdomen axial image showed small loculated collection around the tip at the third to fourth part of the duodenum. (B) CT abdomen axial image showed the tip of the tube penetrating the wall and lying just outside the lumen. 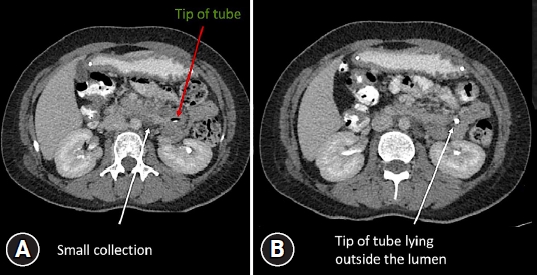
Tableô 1.Characteristics of patients with nasojejunal tube-related perforation REFERENCES1. Pearce CB, Duncan HD. Enteral feeding. Nasogastric, nasojejunal, percutaneous endoscopic gastrostomy, or jejunostomy: its indications and limitations. Postgrad Med J 2002;78:198ã204.
2. Sajid MS, Harper A, Hussain Q, et al. An integrated systematic review and meta-analysis of published randomized controlled trials evaluating nasogastric against postpyloris (nasoduodenal and nasojejunal) feeding in critically ill patients admitted in intensive care unit. Eur J Clin Nutr 2014;68:424ã432.
3. Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol 2014;20:8505ã8524.
4. Halkic N, Guerid S, Blanchard A, et al. Small-bowel perforation: a consequence of feeding jejunostomy. Can J Surg 2005;48:161ã162.
5. Fang JC, Hilden K, Holubkov R, et al. Transnasal endoscopy vs. fluoroscopy for the placement of nasoenteric feeding tubes in critically ill patients. Gastrointest Endosc 2005;62:661ã666.
6. ASGE Technology Committee, Kwon RS, Banerjee S, et al. Enteral nutrition access devices. Gastrointest Endosc 2010;72:236ã248.
7. Schwab D, Mû¥hldorfer S, Nusko G, et al. Endoscopic placement of nasojejunal tubes: a randomized, controlled, prospective trial comparing suitability and technical success for two different tubes. Gastrointest Endosc 2002;56:858ã863.
8. Prabhakaran S, Doraiswamy VA, Nagaraja V, et al. Nasoenteric tube complications. Scand J Surg 2012;101:147ã155.
|
|
||||||||||||||||||||||||||||||||||||||||
