Previous issues
- Page Path
- HOME > Browse Articles > Previous issues
Commentarys
- Aberrant Expression of Epithelial-Mesenchymal Transition Markers in Early Gastric Cancer: Clinical Application
- Moon Kyung Joo
- Clin Endosc 2019;52(5):393-394. Published online September 23, 2019
- DOI: https://doi.org/10.5946/ce.2019.139
- 3,582 View
- 69 Download

- Endless Challenges in Overcoming Complications Associated with Endoscopic Submucosal Dissection
- Satoshi Ono, Shun Ito, Kenji Ogata
- Clin Endosc 2019;52(5):395-396. Published online September 3, 2019
- DOI: https://doi.org/10.5946/ce.2019.137
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Application of Hemocoagulase Bothrops Atrox in the submucosal injection for endoscopic submucosal dissection: a preliminary trial
Yiting Liu, Rui Li, Chenhuan Tan, Yifan Ma, Ji Feng, Qingpeng Xu, Jianing Sun
European Journal of Gastroenterology & Hepatology.2021; 33(1S): e681. CrossRef
- Application of Hemocoagulase Bothrops Atrox in the submucosal injection for endoscopic submucosal dissection: a preliminary trial
- 3,727 View
- 82 Download
- 1 Web of Science
- 1 Crossref

- Endoscopic Ultrasonography for Vascular Invasion in Pancreatic Cancer
- Seong-Hun Kim
- Clin Endosc 2019;52(5):397-398. Published online August 13, 2019
- DOI: https://doi.org/10.5946/ce.2019.142
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- The Role of Endoscopic Ultrasound and Ancillary Techniques in the Diagnosis of Autoimmune Pancreatitis: A Comprehensive Review
Flavio Metelli, Guido Manfredi, Nico Pagano, Elisabetta Buscarini, Stefano Francesco Crinò, Elia Armellini
Diagnostics.2024; 14(12): 1233. CrossRef - Semantic Segmentation of Pancreatic Cancer in Endoscopic Ultrasound Images Using Deep Learning Approach
Kangwon Seo, Jung-Hyun Lim, Jeongwung Seo, Leang Sim Nguon, Hongeun Yoon, Jin-Seok Park, Suhyun Park
Cancers.2022; 14(20): 5111. CrossRef
- The Role of Endoscopic Ultrasound and Ancillary Techniques in the Diagnosis of Autoimmune Pancreatitis: A Comprehensive Review
- 3,854 View
- 89 Download
- 1 Web of Science
- 2 Crossref

- Is the July Effect Real in Patients Undergoing Endoscopic Retrograde Cholangiopancreatography?
- Tae Yoon Lee, Yousuke Nakai
- Clin Endosc 2019;52(5):399-400. Published online July 25, 2019
- DOI: https://doi.org/10.5946/ce.2019.132
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Increased ERCP volume improves cholangiogram interpretation: a new performance measure for ERCP training?
Shyam Vedantam, Sunil Amin, Ben Maher, Saqib Ahmad, Shanil Kadir, Saad Khalid Niaz, Mark Wright, Nadeem Tehami
Clinical Endoscopy.2022; 55(3): 426. CrossRef
- Increased ERCP volume improves cholangiogram interpretation: a new performance measure for ERCP training?
- 3,933 View
- 63 Download
- 2 Web of Science
- 1 Crossref

Focused Review Series: Endoscopic Hemostasis: An Overviews of Principles and Recent Applications
- Endoscopic Hemostasis for Non-Variceal Upper Gastrointestinal Bleeding: New Frontiers
- Adam Kichler, Sunguk Jang
- Clin Endosc 2019;52(5):401-406. Published online July 16, 2019
- DOI: https://doi.org/10.5946/ce.2018.103
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Non-variceal upper gastrointestinal bleeding (NVUGIB) refers to blood loss from the gastrointestinal tract proximal to the ligament of Treitz due to lesions that are non-variceal in origin. The distinction of the bleeding source as non-variceal is important in numerous aspects, but none more so than endoscopic approaches for successful hemostasis. When a patient presents with acute overt blood loss, NVUGIB is a medical emergency, which requires immediate intervention. There have been major strides in pharmacologic and endoscopic interventions for successful induction and remission of hemostasis in the last two decades. Despite achieving tangible improvements, the burden of the disease and the consequent mortality remain high. To address endoscopic outcomes better, several new technologies have emerged and have been subsequently incorporated to the armamentarium of hemostatic tools. This study aims to provide a succinct review on novel technologies for endoscopic hemostasis.
-
Citations
Citations to this article as recorded by- Clinical characteristics of acute non-varicose upper gastrointestinal bleeding and the effect of endoscopic hemostasis
Xiao-Juan Wang, Yu-Peng Shi, Li Wang, Ya-Ni Li, Li-Juan Xu, Yue Zhang, Shuang Han
World Journal of Clinical Cases.2024; 12(9): 1597. CrossRef - Short Peptide Nanofiber Biomaterials Ameliorate Local Hemostatic Capacity of Surgical Materials and Intraoperative Hemostatic Applications in Clinics
Zehong Yang, Lihong Chen, Ji Liu, Hua Zhuang, Wei Lin, Changlong Li, Xiaojun Zhao
Advanced Materials.2023;[Epub] CrossRef - Accessory Splenic Artery Causing Massive Gastrointestinal Bleed
Priyesh Patel, Pravallika Chadalavada, Amandeep Singh, Ram Kishore Gurajala, Jean-Paul Achkar
ACG Case Reports Journal.2021; 8(3): e00550. CrossRef - Diode Laser—Can It Replace the Electrical Current Used in Endoscopic Submucosal Dissection? (with Video)
Yunho Jung, Gwang Ho Baik, Weon Jin Ko, Bong Min Ko, Seong Hwan Kim, Jin Seok Jang, Jae-Young Jang, Wan-Sik Lee, Young Kwan Cho, Sun Gyo Lim, Hee Seok Moon, In Kyung Yoo, Joo Young Cho
Clinical Endoscopy.2021; 54(4): 555. CrossRef -
In Vivo Investigation of Noncontact Rapid Photothermal Hemostasis on Venous and Arterial Bleeding
Myeongjin Kim, Van Gia Truong, Sungwon Kim, Hyejin Kim, Thomas Hasenberg, Hyun Wook Kang
IEEE Transactions on Biomedical Engineering.2021; 68(9): 2689. CrossRef - Comparison of high and low-dose epinephrine & endoclip application in peptic ulcer bleeding
Tamer Akay, Metin Leblebici
Medicine.2021; 100(52): e28480. CrossRef - Endoscopic Ultrasound-Guided Treatments for Non-Variceal Upper GI Bleeding: A Review of the Literature
Claudio Giovanni De Angelis, Pablo Cortegoso Valdivia, Stefano Rizza, Ludovica Venezia, Felice Rizzi, Marcantonio Gesualdo, Giorgio Maria Saracco, Rinaldo Pellicano
Journal of Clinical Medicine.2020; 9(3): 866. CrossRef - Preparation and Study of Hemostatic Materials Based on Chitosan and Chitin Nanofibrils
E. N. Maevskaia, E. N. Dresvyanina, A. S. Shabunin, I. P. Dobrovol’skaya, M. B. Paneyah, A. M. Fediuk, P. L. Sushchinskii, G. P. Smirnov, V. E. Yudin, E. V. Zinoviev
Nanotechnologies in Russia.2020; 15(7-8): 466. CrossRef
- Clinical characteristics of acute non-varicose upper gastrointestinal bleeding and the effect of endoscopic hemostasis
- 9,184 View
- 482 Download
- 9 Web of Science
- 8 Crossref

- Endoscopic Therapy and Radiologic Intervention of Acute Gastroesophageal Variceal Bleeding
- Jeong Eun Song, Byung Seok Kim
- Clin Endosc 2019;52(5):407-415. Published online September 30, 2019
- DOI: https://doi.org/10.5946/ce.2019.178

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Acute gastroesophageal variceal hemorrhage is a dreaded complication in patients with liver cirrhosis. Endoscopic therapy and radiologic intervention for gastroesophageal bleeding have rapidly developed in the recent decades. Endoscopic treatment is initially performed to stop variceal hemorrhage. For the treatment of esophageal variceal bleeding, endoscopic variceal ligation (EVL) is considered the endoscopic treatment of choice. In cases of gastric variceal hemorrhage, the type of gastric varices (GVs) is important in deciding the strategy of endoscopic treatment. Endoscopic variceal obturation (EVO) is recommended for fundal variceal bleeding. For the management of gastroesophageal varix type 1 bleeding, both EVO and EVL are available treatment options; however, EVO is preferred over EVL. If endoscopic management fails to control variceal hemorrhage, radiologic interventional modalities could be considered. Transjugular intrahepatic portosystemic shunt is a good option for rescue treatment in refractory variceal bleeding. In cases of refractory hemorrhage of GVs in patients with a gastrorenal shunt, balloon-occluded retrograde transvenous obliteration could be considered as a salvage treatment.
-
Citations
Citations to this article as recorded by- Transjugular intrahepatic portosystemic shunt for esophagojejunal variceal bleeding after total gastrectomy: A case report
Sang Un Kim, Jihoon Hong
Radiology Case Reports.2024; 19(8): 3231. CrossRef - Efficacy of early re-ligation after endoscopic gastric glue injection combined with endoscopic variceal ligation in preventing rebleeding of esophagogastric varices in patients with cirrhosis
Hui-Min Liu, Zhi-Bin Gong
World Chinese Journal of Digestology.2022; 30(17): 748. CrossRef - The Role of Interventional Radiology in Esophageal Varices and Hematemesis: Review Article
Qaed Salem Alhammami, Maisa Hamad Freaj Alanazi, Shahad Khalid A Bedaiwi, Ghazir Aneed N Alruwili, Shouq Fayed Khalaf Alanazi
Archives of Pharmacy Practice.2022; 13(4): 7. CrossRef - Comprehensive treatment of patients with gastric variceal bleeding
S.M. Chooklin, S.S. Chuklin
EMERGENCY MEDICINE.2022; 18(8): 14. CrossRef
- Transjugular intrahepatic portosystemic shunt for esophagojejunal variceal bleeding after total gastrectomy: A case report
- 8,252 View
- 320 Download
- 1 Web of Science
- 4 Crossref

- Endoscopic Management of Peptic Ulcer Bleeding: Recent Advances
- Philip WY Chiu
- Clin Endosc 2019;52(5):416-418. Published online August 13, 2019
- DOI: https://doi.org/10.5946/ce.2018.182

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Bleeding peptic ulcers remained as one of the commonest causes of hospitalization worldwide. While endoscopic hemostasis serves as primary treatment for bleeding ulcers, rebleeding after endoscopic hemostasis becomes more and more difficult to manage as patients are usually poor surgical candidates with multiple comorbidities. Recent advances in management of bleeding peptic ulcers aimed to further reduce the rate of rebleeding through—(1) identification of high risk patients for rebleeding and mortality; (2) improvement in primary endoscopic hemostasis and; (3) prophylactic angiographic embolization of major arteries. The technique and clinical evidences for these approaches will be reviewed in the current article.
-
Citations
Citations to this article as recorded by- Management of severe peri-operative bleeding: Guidelines from the European Society of Anaesthesiology and Intensive Care
Sibylle Kietaibl, Aamer Ahmed, Arash Afshari, Pierre Albaladejo, Cesar Aldecoa, Giedrius Barauskas, Edoardo De Robertis, David Faraoni, Daniela C. Filipescu, Dietmar Fries, Anne Godier, Thorsten Haas, Matthias Jacob, Marcus D. Lancé, Juan V. Llau, Jens Me
European Journal of Anaesthesiology.2023; 40(4): 226. CrossRef - Aspirin vs Clopidogrel: Antiplatelet Agent of Choice for Those With Recent Bleeding or at Risk for Gastrointestinal Bleed
Siddharth Gosavi, Gokul Krishnan, Raviraja V Acharya
Cureus.2023;[Epub] CrossRef - Effect of nano silver on gastroprotective activity against ethanol-induced stomach ulcer in rats
Ibrahim Abdel Aziz Ibrahim, Abbas I. Hussein, Mahmoud S. Muter, Abdulalah T. Mohammed, Morteta H. Al-Medhtiy, Suhayla Hamad Shareef, Peshawa Yunis Aziz, Nabaz Fisal Shakir Agha, Mahmood Ameen Abdulla
Biomedicine & Pharmacotherapy.2022; 154: 113550. CrossRef - Protective Effects of Radix Sophorae Flavescentis Carbonisata-Based Carbon Dots Against Ethanol‐Induced Acute Gastric Ulcer in Rats: Anti-Inflammatory and Antioxidant Activities
Jie Hu, Juan Luo, Meiling Zhang, Jiashu Wu, Yue Zhang, Hui Kong, Huihua Qu, Guoliang Cheng, Yan Zhao
International Journal of Nanomedicine.2021; Volume 16: 2461. CrossRef
- Management of severe peri-operative bleeding: Guidelines from the European Society of Anaesthesiology and Intensive Care
- 6,533 View
- 278 Download
- 4 Web of Science
- 4 Crossref

- Endoscopic Therapy for Acute Diverticular Bleeding
- Masayuki Kato
- Clin Endosc 2019;52(5):419-425. Published online August 20, 2019
- DOI: https://doi.org/10.5946/ce.2019.078
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
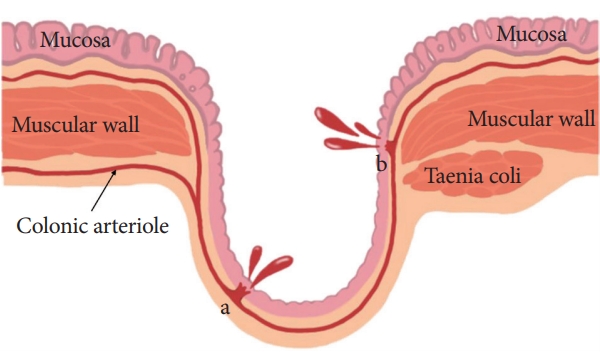
ePub - Diverticular bleeding accounts for approximately 26%–40% of the cases of lower gastrointestinal bleeding. Rupture of the vasa recta at the neck or dome of the diverticula can be the cause of this bleeding. Colonoscopy aids in not only the diagnosis but also the treatment of diverticular bleeding after a steady bowel preparation. Endoscopic hemostasis involves several methods, such as injection/thermal contact therapy, clipping, endoscopic band ligation (EBL), hemostatic powder, and over-the-scope clips. Each endoscopic method can provide a secure initial hemostasis. With regard to the clinical outcomes after an endoscopic treatment, the methods reportedly have no significant differences in the initial hemostasis and early recurring bleeding; however, EBL might prevent the need for transcatheter arterial embolization or surgery. In contrast, the long-term outcomes of the endoscopic treatments, such as a late bleeding and recurrent bleeding at 1 and 2 years, are not well known for diverticular bleeding. With regard to a cure for diverticular bleeding, there should be an improvement in both the endoscopic methods and the multilateral perspectives, such as diet, medicines, interventional approaches, and surgery.
-
Citations
Citations to this article as recorded by- A Review of Colonoscopy in Intestinal Diseases
Seung Hong, Dong Baek
Diagnostics.2023; 13(7): 1262. CrossRef - Short Peptide Nanofiber Biomaterials Ameliorate Local Hemostatic Capacity of Surgical Materials and Intraoperative Hemostatic Applications in Clinics
Zehong Yang, Lihong Chen, Ji Liu, Hua Zhuang, Wei Lin, Changlong Li, Xiaojun Zhao
Advanced Materials.2023;[Epub] CrossRef - A new band ligation device to treat colonic diverticular bleeding
Yunho Jung
Clinical Endoscopy.2022; 55(3): 367. CrossRef - Diagnosis and Treatment of Colonic Diverticular Disease
You Sun Kim
The Korean Journal of Gastroenterology.2022; 79(6): 233. CrossRef - Efficacy of Combination Therapy with Epinephrine Local Injection and Hemostatic Clips on Active Diverticular Bleeding
Seiji Hamada, Akira Teramoto, Ryuta Zukeyama, Shinobu Matsukawa, Tomofumi Fukuhara, Ryo Takaki, Takahiro Utsumi, Masamoto Nakamura, Kasen Kobashikawa, Nobufumi Uchima, Tomokuni Nakayoshi, Fukunori Kinjo
Journal of Clinical Medicine.2022; 11(17): 5195. CrossRef - Diverticular Bleeding: A Clinical Image
Christopher F Brewer, Yayha Al Abed
Cureus.2021;[Epub] CrossRef
- A Review of Colonoscopy in Intestinal Diseases
- 13,293 View
- 503 Download
- 6 Web of Science
- 6 Crossref

Special Review: Korean Society of Gastrointestinal Endoscopy “Accreditations of Qualified Endoscopy Unit” Guideline: Update 2019
- Accredited Endoscopy Unit Program of Korea: Overview and Qualification
- Jung-Wook Kim, Yu Kyung Cho, Jin-Oh Kim, Jae-Young Jang, the Quality Management Committee of Korean Society of Gastrointestinal Endoscopy
- Clin Endosc 2019;52(5):426-430. Published online September 30, 2019
- DOI: https://doi.org/10.5946/ce.2019.166
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The Korean Society of Gastrointestinal Endoscopy introduced the Accredited Endoscopy Unit Program to enhance endoscopy unit quality through systematic quality management in 2012. It was gradually expanded from training hospitals to institutions with 100+ beds, and the criteria for certification were applied according to the actual conditions of each institution. On the basis of the continuous communication with the institutions and feedback, the Accredited Endoscopy Unit Program certification criteria were revised in 2019 and introduced as follows: (1) the qualification criteria for endoscopy doctors and nurses; (2) facilities and equipment; (3) endoscopic examination process; (4) performance; (5) disinfection and infection control; and (6) endoscopic sedation. The assessment items consist of essential and recommended items. All essential items must be met for accreditation to be awarded. The assessment criteria for each evaluation area were revised as follows: (1) upgrading assessment criteria; (2) qualification of endoscopists and reinforcement of quality control education; (3) detailed standards for safety, disinfection, endoscopic sedation, and management instructions; and (4) presentation of new performance measurement of endoscopy and colonoscopy.
-
Citations
Citations to this article as recorded by- Safety of Gastrointestinal Endoscopy in Korea: A Nationwide Survey and Population-Based Study
Yunho Jung, Jung-Wook Kim, Jong Pil Im, Yu Kyung Cho, Tae Hee Lee, Jae-Young Jang
Journal of Korean Medical Science.2022;[Epub] CrossRef - Total polyp number may be more important than size and histology of polyps for prediction of metachronous high-risk colorectal neoplasms
Hyuk Yoon, Cheol Min Shin, Young Soo Park, Nayoung Kim, Dong Ho Lee
BMC Gastroenterology.2022;[Epub] CrossRef - Endoscopist-Driven Sedation Practices in South Korea: Re-evaluation Considering the Nationwide Survey in 2019
Seon-Young Park, Jun Kyu Lee, Chang-Hwan Park, Byung-Wook Kim, Chang Kyun Lee, Hong Jun Park, Byung Ik Jang, Dong Uk Kim, Jin Myung Park, Jae Min Lee, Young Sin Cho, Hyung Ku Chon, Seung Young Seo, Woo Hyun Paik
Gut and Liver.2022; 16(6): 899. CrossRef - Accreditation of digestive endoscopy services: a method of quality assuring?
Giancarlo Spinzi, Angelo Milano, Maurizio Capelli
Expert Review of Gastroenterology & Hepatology.2021; 15(1): 1. CrossRef - Important Quality Metrics and Standardization in Endoscopy
Tossapol Kerdsirichairat, Eun Ji Shin
Gastrointestinal Endoscopy Clinics of North America.2021; 31(4): 727. CrossRef - A Nationwide Survey on the Facilities and Personnel for Endoscopic Sedation: Results from 50 Qualified Endoscopy Units of Teaching Hospitals Accredited by the Korean Society of Gastrointestinal Endoscopy (KSGE)
Seon-Young Park, Jun Kyu Lee, Jung-Wook Kim, Tae Hee Lee, Chang-Hwan Park, Jae-Yong Jang, Byung-Wook Kim, Byung Ik Jang
Clinical Endoscopy.2021; 54(6): 843. CrossRef - Efficacy and Patient Tolerability Profiles of Probiotic Solution with Bisacodyl Versus Conventional Cleansing Solution for Bowel Preparation: A Prospective, Randomized, Controlled Trial
Youn I Choi, Jong-Joon Lee, Jun-Won Chung, Kyoung Oh Kim, Yoon Jae Kim, Jung Ho Kim, Dong Kyun Park, Kwang An Kwon
Journal of Clinical Medicine.2020; 9(10): 3286. CrossRef
- Safety of Gastrointestinal Endoscopy in Korea: A Nationwide Survey and Population-Based Study
- 3,990 View
- 105 Download
- 6 Web of Science
- 7 Crossref

- Updates on the Facilities, Procedures, and Performance of the Accredited Endoscopy Unit
- Tae Hee Lee, Jin Young Yoon, Chang Nyol Paik, Hyuk Soon Choi, Jae-Young Jang, The Quality Management Committee of The Korean Society of Gastrointestinal Endoscopy
- Clin Endosc 2019;52(5):431-442. Published online September 30, 2019
- DOI: https://doi.org/10.5946/ce.2019.164
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic quality indicators can be classified into three categories, namely facilities and equipment, endoscopic procedures, and outcome measures. In 2019, the Korean Society of Gastrointestinal Endoscopy updated the accreditation of qualified endoscopy unit assessment items for these quality indicators to establish competence and define areas of continuous quality improvement. Here, we presented the updated program guidelines on the facilities, procedures, and performance of the accredited endoscopy unit. Many of these items have not yet been validated. However, the updated program will help in establishing competence and defining areas of continuous quality improvement in Korean endoscopic practice.
-
Citations
Citations to this article as recorded by- Safety of Gastrointestinal Endoscopy in Korea: A Nationwide Survey and Population-Based Study
Yunho Jung, Jung-Wook Kim, Jong Pil Im, Yu Kyung Cho, Tae Hee Lee, Jae-Young Jang
Journal of Korean Medical Science.2022;[Epub] CrossRef - Efficacy of sigmoidoscopy for evaluating disease activity in patients with ulcerative colitis
Su Bum Park, Seong-Jung Kim, Jun Lee, Yoo Jin Lee, Dong Hoon Baek, Geom Seog Seo, Eun Soo Kim, Sang-Wook Kim, So Yeong Kim
BMC Gastroenterology.2022;[Epub] CrossRef - Endoscopist-Driven Sedation Practices in South Korea: Re-evaluation Considering the Nationwide Survey in 2019
Seon-Young Park, Jun Kyu Lee, Chang-Hwan Park, Byung-Wook Kim, Chang Kyun Lee, Hong Jun Park, Byung Ik Jang, Dong Uk Kim, Jin Myung Park, Jae Min Lee, Young Sin Cho, Hyung Ku Chon, Seung Young Seo, Woo Hyun Paik
Gut and Liver.2022; 16(6): 899. CrossRef - Guidelines for accreditation of endoscopy units: quality measures from the Korean Society of Coloproctology
Rumi Shin, Seongdae Lee, Kyung-Su Han, Dae Kyung Sohn, Sang Hui Moon, Dong Hyun Choi, Bong-Hyeon Kye, Hae-Jung Son, Sun Il Lee, Sumin Si, Won-Kyung Kang
Annals of Surgical Treatment and Research.2021; 100(3): 154. CrossRef - A Nationwide Survey on the Facilities and Personnel for Endoscopic Sedation: Results from 50 Qualified Endoscopy Units of Teaching Hospitals Accredited by the Korean Society of Gastrointestinal Endoscopy (KSGE)
Seon-Young Park, Jun Kyu Lee, Jung-Wook Kim, Tae Hee Lee, Chang-Hwan Park, Jae-Yong Jang, Byung-Wook Kim, Byung Ik Jang
Clinical Endoscopy.2021; 54(6): 843. CrossRef - SAFETY IN THE GASTROENTEROLOGY SETTING
Gastroenterology Nursing.2021; 44(6): 467. CrossRef - Duodenal Hyperplastic Polyp Masquerading as Tumor of the Ampulla of Vater
Jin Myung Park, Chang Don Kang
The Korean Journal of Pancreas and Biliary Tract.2020; 25(2): 135. CrossRef - Efficacy and Patient Tolerability Profiles of Probiotic Solution with Bisacodyl Versus Conventional Cleansing Solution for Bowel Preparation: A Prospective, Randomized, Controlled Trial
Youn I Choi, Jong-Joon Lee, Jun-Won Chung, Kyoung Oh Kim, Yoon Jae Kim, Jung Ho Kim, Dong Kyun Park, Kwang An Kwon
Journal of Clinical Medicine.2020; 9(10): 3286. CrossRef
- Safety of Gastrointestinal Endoscopy in Korea: A Nationwide Survey and Population-Based Study
- 4,894 View
- 104 Download
- 7 Web of Science
- 8 Crossref

- Updates on the Disinfection and Infection Control Process of the Accredited Endoscopy Unit
- Jeong Eun Shin, Yunho Jung, Jeong Hoon Lee, Byoung Kwan Son, Jae-Young Jang, Hyung-Keun Kim, Byung Ik Jang, The Quality Management Committee and the Disinfection Management Committee of Korean Society of Gastrointestinal Endoscopy
- Clin Endosc 2019;52(5):443-450. Published online September 30, 2019
- DOI: https://doi.org/10.5946/ce.2019.173
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - A thorough disinfection and infection control process associated with gastrointestinal endoscopy is highly important for the health and safety of the examinee and the medical staff involved in the procedure. Endoscopic reprocessing and disinfection are two of the most important steps in quality control of endoscopy. In 2019, the Korean Society of Gastrointestinal Endoscopy updated the Accreditation of Qualified Endoscopy Unit assessment items for these quality indicators. Assessment of disinfection and infection control comprises 28 mandatory items in the categories of disinfection education, pre-cleaning, cleaning, disinfection, rinsing, drying, reprocessing, storage, endoscopic accessories, water bottle and connectors, space/facilities, personal protective equipment, disinfection ledger, and regulations regarding infection control and disinfection.
The updated Accreditation of Qualified Endoscopy Unit assessment items are useful for improving the quality of endoscopy by ensuring thorough inspection of endoscopic disinfection and infection control. -
Citations
Citations to this article as recorded by- Analysis of sterilization efficiency and application cost of three low temperature sterilization methods
Hui Chen, Jiawei Liu, Aiying Zeng, Nian Qin
Review of Scientific Instruments.2024;[Epub] CrossRef - Infection control in the bronchoscopy suite: effective reprocessing and disinfection of reusable bronchoscopes
Mamta S. Chhabria, Fabien Maldonado, Atul C. Mehta
Current Opinion in Pulmonary Medicine.2023; 29(1): 21. CrossRef - Endoscopy in surgery
María Rita Rodríguez-Luna, Silvana Perretta
Frontiers in Gastroenterology.2023;[Epub] CrossRef - Safety of Gastrointestinal Endoscopy in Korea: A Nationwide Survey and Population-Based Study
Yunho Jung, Jung-Wook Kim, Jong Pil Im, Yu Kyung Cho, Tae Hee Lee, Jae-Young Jang
Journal of Korean Medical Science.2022;[Epub] CrossRef - A nationwide survey on the effectiveness of training on endoscope reprocessing within the national cancer screening program in Korea
Hye Young Shin, Da Hun Jang, Jae Kwan Jun
American Journal of Infection Control.2021; 49(8): 1031. CrossRef - Effectiveness Between Daily and After-Each-Case Room Disinfection of the Endoscopy Unit
Bo Jin, Yue Hu, Liang Huang, Xiaoyun Cheng, Jin Zhao, Xuejing Yang, Xiling Sun, Tieer Gan, Bin Lu
Frontiers in Public Health.2021;[Epub] CrossRef - Sans Standardization: Effective Endoscope Reprocessing
Sameer K. Avasarala, Lawrence F. Muscarella, Atul C. Mehta
Respiration.2021; 100(12): 1208. CrossRef - Sharing Our Experience of Operating an Endoscopy Unit in the Midst of a COVID-19 Outbreak
Jimin Han, Eun Young Kim
Clinical Endoscopy.2020; 53(2): 243. CrossRef
- Analysis of sterilization efficiency and application cost of three low temperature sterilization methods
- 4,582 View
- 148 Download
- 7 Web of Science
- 8 Crossref

- Updates on the Sedation for Gastrointestinal Endoscopy
- Jun Kyu Lee, Yoo Jin Lee, Jun Hyung Cho, Jong Pil Im, Chang-Hwan Park, Jae-Young Jang, Byung Ik Jang, the Quality Management Committee and the Disinfection Management/Conscious Sedation Committee of Korean Society of Gastrointestinal Endoscopy (KSGE)
- Clin Endosc 2019;52(5):451-457. Published online September 30, 2019
- DOI: https://doi.org/10.5946/ce.2019.172

-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Sedation, defined as the depressed level of consciousness, induced by drug administration, is widely used for gastrointestinal endoscopy to relieve a patient’s anxiety and discomfort. In addition, successful procedure is anticipated with control of unintended movements. Endoscopic sedation, however, cannot be free from the risk of serious adverse events, e.g., cardiopulmonary compromise. Therefore, principles on personnel, facility and equipment, as well as performance itself, should be followed to prevent unfavorable incidents. In this article, sedation guidelines for the Accreditation of Qualified Endoscopy Units, issued by the Korean Society of Gastrointestinal Endoscopy, are presented.
-
Citations
Citations to this article as recorded by- Nurse-Administered Propofol Sedation Training Curricula and Propofol Administration in Digestive Endoscopy Procedures
Andrea Minciullo, Lucia Filomeno
Gastroenterology Nursing.2024; 47(1): 33. CrossRef - Propofol Alone versus Propofol in Combination with Midazolam for Sedative Endoscopy in Patients with Paradoxical Reactions to Midazolam
Ji Hyung Nam, Dong Kee Jang, Jun Kyu Lee, Hyoun Woo Kang, Byung-Wook Kim, Byung Ik Jang
Clinical Endoscopy.2022; 55(2): 234. CrossRef - Endoscopist-Driven Sedation Practices in South Korea: Re-evaluation Considering the Nationwide Survey in 2019
Seon-Young Park, Jun Kyu Lee, Chang-Hwan Park, Byung-Wook Kim, Chang Kyun Lee, Hong Jun Park, Byung Ik Jang, Dong Uk Kim, Jin Myung Park, Jae Min Lee, Young Sin Cho, Hyung Ku Chon, Seung Young Seo, Woo Hyun Paik
Gut and Liver.2022; 16(6): 899. CrossRef - Drugs used for sedation in gastrointestinal endoscopy
Jun Kyu Lee
Journal of the Korean Medical Association.2022; 65(11): 735. CrossRef - Pain Intensity at Injection Site during Esophagogastroduodenoscopy Using Long- and Medium-Chain versus Long-Chain Triglyceride Propofol: A Randomized Controlled Double-Blind Study
Joon Seop Lee, Eun Soo Kim, Kwang Bum Cho, Kyung Sik Park, Yoo Jin Lee, Ju Yup Lee
Gut and Liver.2021; 15(4): 562. CrossRef - A Nationwide Survey on the Facilities and Personnel for Endoscopic Sedation: Results from 50 Qualified Endoscopy Units of Teaching Hospitals Accredited by the Korean Society of Gastrointestinal Endoscopy (KSGE)
Seon-Young Park, Jun Kyu Lee, Jung-Wook Kim, Tae Hee Lee, Chang-Hwan Park, Jae-Yong Jang, Byung-Wook Kim, Byung Ik Jang
Clinical Endoscopy.2021; 54(6): 843. CrossRef - Risk Factors for Prolonged Hospital Stay after Endoscopy
Toshihiro Nishizawa, Shuntaro Yoshida, Osamu Toyoshima, Tatsuya Matsuno, Masataka Irokawa, Toru Arano, Hirotoshi Ebinuma, Hidekazu Suzuki, Takanori Kanai, Kazuhiko Koike
Clinical Endoscopy.2021; 54(6): 851. CrossRef
- Nurse-Administered Propofol Sedation Training Curricula and Propofol Administration in Digestive Endoscopy Procedures
- 6,070 View
- 232 Download
- 8 Web of Science
- 7 Crossref

Original Articles
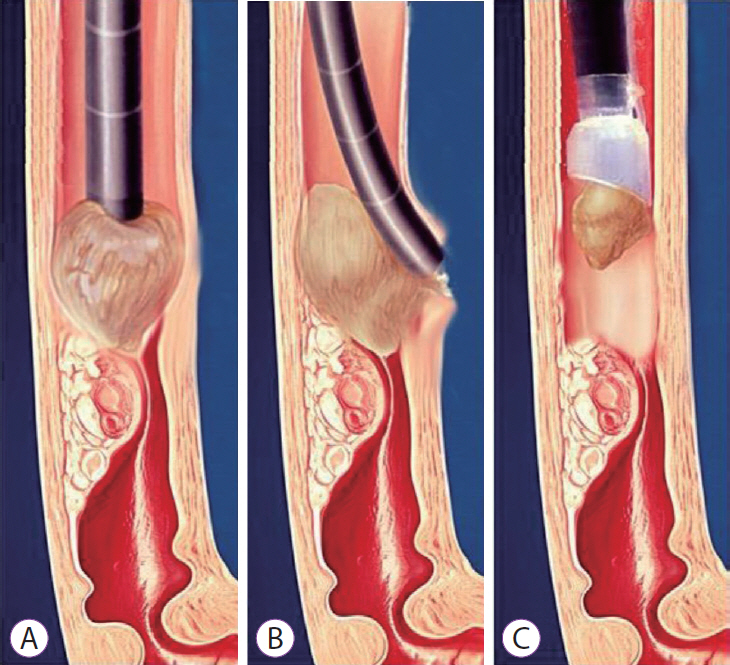
- Cap-Assisted Technique versus Conventional Methods for Esophageal Food Bolus Extraction: A Comparative Study
- Mahmoud Wahba, Ghada Habib, Ahmed El Mazny, May Fawzi, Mohamed A. Elfeki, Seham Sabry, Mahommad ELbaz, Sayed M Seif El Nasr
- Clin Endosc 2019;52(5):458-463. Published online July 8, 2019
- DOI: https://doi.org/10.5946/ce.2019.042
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Food bolus impaction is the most common form of esophageal foreign body impaction observed in adults. Clinical guidelines recommend using the push technique or retrieval methods in such cases. The push technique can cause injuries in certain clinical situations. Notably, conventional retrieval methods are time and effort consuming. Cap-assisted endoscopic extraction of an impacted food bolus is an easy and effective technique; however, more data are needed for its validation. This study compared the capassisted extraction technique with conventional methods.
Methods
This prospective observational multicenter study compared the success and en bloc removal rates, total procedure time, and adverse events in both techniques..
Results
The study included 303 patients who underwent food bolus extraction. The push technique was used in 87 patients (28.7%) and a retrieval procedure in 216 patients (71.3%). Cap-assisted extraction was performed in 106 patients and retrieval using conventional methods in 110 patients. The cap-assisted technique was associated with a higher rate of en bloc removal (80.2% vs. 15%, p<0.01), shorter procedure time (6.9±3.5 min vs. 15.7±4.1 min, p<0.001), and fewer adverse events (0/106 vs. 9/110, p<0.001).
Conclusions
Cap-assisted extraction showed no adverse events, higher efficacy, and a shorter procedure time compared with conventional retrieval procedures. -
Citations
Citations to this article as recorded by- Cap-Assisted Endoscopic Esophageal Foreign Body Removal Is Safe and Efficacious Compared to Conventional Methods
Zohaib Ahmed, Syeda Faiza Arif, Stephanie Lin Ong, Joyce Badal, Wade Lee-Smith, Anas Renno, Yaseen Alastal, Ali Nawras, Muhammad Aziz
Digestive Diseases and Sciences.2023; 68(4): 1411. CrossRef - Cap-assisted endoscopy for esophageal foreign bodies: A meta-analysis
Zahid Ijaz Tarar, Umer Farooq, Matthew L Bechtold, Yezaz A Ghouri
World Journal of Meta-Analysis.2023; 11(1): 38. CrossRef - Endoscopy in Pediatric Eosinophilic Esophagitis
Ramy Sabe, Girish Hiremath, Kenneth Ng
Gastrointestinal Endoscopy Clinics of North America.2023; 33(2): 323. CrossRef - Bolusobstruktionen im Ösophagus – Eine Analyse über 5 Jahre
Jürgen Heise, Christian Kreysel, Michael Blank, Philipp Euler, Ilka Melchior, Michaela Johnen, Manfred Planker, Antje Ballauff, Martina Czypull, Thomas Frieling
Zeitschrift für Gastroenterologie.2023; 61(12): 1603. CrossRef - Comparable Efficacy for Push Versus Pull Technique in Esophageal Food Impaction: Systematic Review with Meta-Analysis
Manesh Kumar Gangwani, Muhammad Aziz, Dushyant Singh Dahiya, Abeer Aziz, Fnu Priyanka, Rahul Karna, Wade Lee-Smith, Zohaib Ahmed, Faisal Kamal, Sumant Inamdar, Yaseen Alastal, Douglas Adler
Digestive Diseases and Sciences.2023; 68(8): 3354. CrossRef - Distal Endoscopic Attachments
Pankaj N. Desai, Chintan N. Patel, Mayank Kabrawala, Subhash Nanadwani, Rajiv Mehta, Ritesh Prajapati, Nisharg Patel, Mohit Sethia
Journal of Digestive Endoscopy.2022; 13(04): 243. CrossRef - Comparison of Cap-Assisted vs Conventional Endoscopic Technique for Management of Food Bolus Impaction in the Esophagus: Results of a Multicenter Randomized Controlled Trial
Marie Ooi, Tuan Duong, Richard Holman, Dep Huynh, Abdulnasser Lafta, Florian Grimpen, Mark Appleyard, Chris K. Rayner, Nam Q. Nguyen
American Journal of Gastroenterology.2021; 116(11): 2235. CrossRef - Üst gastrointestinal sistem yabancı cisimleri ve gıda takılmalarında endoskopi deneyimimiz
Tolga DÜZENLİ, Hüseyin KÖSEOĞLU
Endoskopi Gastrointestinal.2020; 28(Sayı: 3): 95. CrossRef
- Cap-Assisted Endoscopic Esophageal Foreign Body Removal Is Safe and Efficacious Compared to Conventional Methods
- 6,060 View
- 154 Download
- 6 Web of Science
- 8 Crossref

- Immunohistochemical Expression of Epithelial-Mesenchymal Transition Markers in Early Gastric Cancer: Cancer Tissue versus Noncancer Tissue
- Hee Jae Jung, Su Jin Hong, Shin Hee Kim
- Clin Endosc 2019;52(5):464-471. Published online May 22, 2019
- DOI: https://doi.org/10.5946/ce.2018.181
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
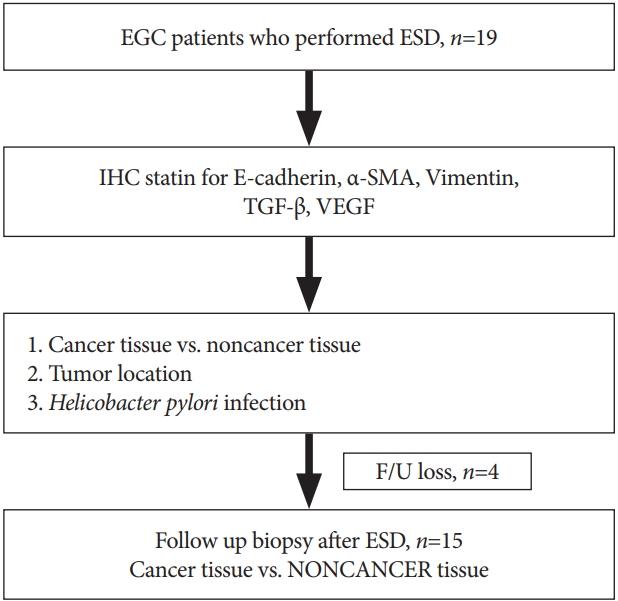
ePub - Background
/Aims: Epithelial-mesenchymal transition (EMT) is a developmental process, wherein the epithelial cells show reduced intercellular adhesions and acquire migratory fibroblastic properties. EMT is associated with downregulation in epithelial marker expression, abnormal translocation of E-cadherin, and upregulation in mesenchymal marker expression. Here, we investigated the immunohistochemical (IHC) expression of EMT markers in early gastric cancer (EGC) between cancer and noncancer tissues.
Methods
Tissue samples were prospectively obtained from 19 patients with EGC that underwent endoscopic submucosal dissection (ESD). We compared the expression level of transforming growth factor (TGF)-β, vascular endothelial growth factor (VEGF), E-cadherin, α-smooth muscle actin (α-SMA), and vimentin between cancer and noncancer tissues using IHC. Among the 19 patients, 15 patients had follow-up biopsy at 3 months after ESD for EGC.
Results
Cancer tissues presented higher values of EMT mesenchymal markers (α-SMA/vimentin/TGF-β/VEGF) than the noncancerous tissues (p<0.05) that were significantly low after ESD (p<0.05). No significant correlation was reported for tumor location and initial Helicobacter pylori infection.
Conclusions
The mesenchymal expression of EMT markers was higher in the cancerous tissues than in the noncancer tissues. -
Citations
Citations to this article as recorded by- Gastric Carcinoma with low ROR alpha, low E- Cadherin and High LAPTM4B Immunohistochemical Profile; is associated with unfavorable prognosis in Egyptian patients
Shereen Nagib El Mashad, Mona Abd El Halim Kandil, Taysseer Abd El-Hamid Talab, Abd El Naby Saied Abd El Naby, Mervat Mahmoud Sultan, Ahmed Sohaib, Aiat Shaban Hemida
Journal of Immunoassay and Immunochemistry.2024; 45(1): 50. CrossRef - MiR-522-3p Targets Transcription Factor 4 to Overcome Cisplatin Resistance of Gastric Cells
Guofeng Ma, Wen Xue, Jie Ni, Ran Tao, Xiangya Ding
Journal of Oncology.2022; 2022: 1. CrossRef - Investigating Helicobacter pylori-related pyloric hypomotility: functional, histological, and molecular alterations
Aya Aly Ashraf, Sarah Mahmoud Gamal, Hend Ashour, Basma Emad Aboulhoda, Laila Ahmed Rashed, Inas Anas Harb, Gaber Hassan Abdelfattah, Eman Ahmed El-Seidi, Heba Mohamed Shawky
American Journal of Physiology-Gastrointestinal and Liver Physiology.2021; 321(5): G461. CrossRef
- Gastric Carcinoma with low ROR alpha, low E- Cadherin and High LAPTM4B Immunohistochemical Profile; is associated with unfavorable prognosis in Egyptian patients
- 5,475 View
- 154 Download
- 4 Web of Science
- 3 Crossref

- Effectiveness of Autologous Platelet-Rich Plasma for the Healing of Ulcers after Endoscopic Submucosal Dissection
- Eunju Jeong, In kyung Yoo, Ozlem Ozer Cakir, Hee Kyung Kim, Won Hee Kim, Sung Pyo Hong, Joo Young Cho
- Clin Endosc 2019;52(5):472-478. Published online May 17, 2019
- DOI: https://doi.org/10.5946/ce.2018.152
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
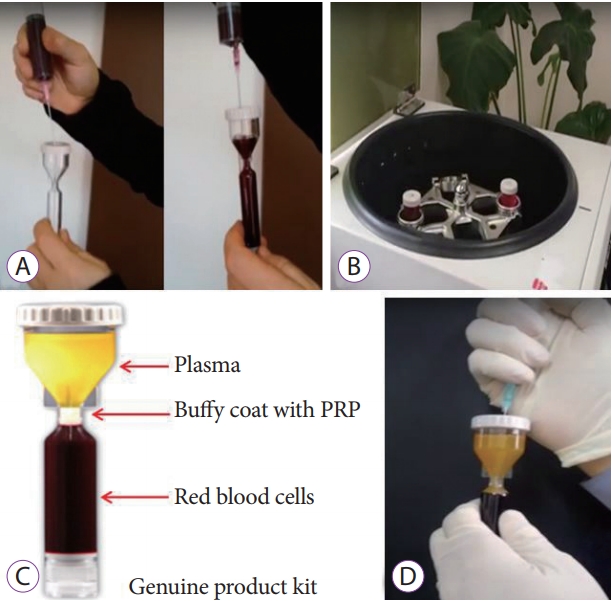
ePub - Background
/Aims: Platelet-rich plasma (PRP) has been used for wound healing in various medical fields. The aim of this study was to evaluate the clinical efficacy and safety of local PRP injections after endoscopic submucosal dissection (ESD).
Methods
Patients were non-randomly divided into the following two groups: (1) control group in which patients were administered only an intravenous proton pump inhibitor (PPI), and (2) a study group in which patients were administered an intravenous PPI and a topical PRP injection. We assessed the reduction in the ulcer area and stage of the ulcer after the procedure (24 hours, 48 hours, and 28 days after endoscopic surgery).
Results
We enrolled 7 study and 7 control patients. In the study group, the rate of ulcer reduction was 59% compared to 52% in the control group (p=0.372), 28 days after ESD. There were 5 patients in the S stage and 2 patients in the H stage in the study group compared to no patient in the S stage and 7 patients in the H stage in the control group (p=0.05), 28 days after ESD. There were no serious complications in either group.
Conclusions
The local injection of PRP is a safe and effective procedure for ulcer healing after ESD. -
Citations
Citations to this article as recorded by- Clinical efficacy of blood derivatives on wound healing: A systematic review and network meta‐analysis
Yanhong Wu, Guang Peng, Yuzhi Wang, Jianwu Chen, Bin Zhang, Jianbing Tang, Biao Cheng
International Wound Journal.2024;[Epub] CrossRef - Endoscopic Shielding With Platelet-rich Plasma After Resection Of Large Colorectal Lesions
Vicente Lorenzo-Zúñiga, Vicente Moreno de Vega, Ramón Bartolí
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2021; 31(3): 376. CrossRef - The Additive Effect of Platelet-Rich Plasma in the Treatment of Actively Bleeding Peptic Ulcer
Waseem M. Seleem, Amr Shaaban Hanafy
Clinical Endoscopy.2021; 54(6): 864. CrossRef - Endless Challenges in Overcoming Complications Associated with Endoscopic Submucosal Dissection
Satoshi Ono, Shun Ito, Kenji Ogata
Clinical Endoscopy.2019; 52(5): 395. CrossRef
- Clinical efficacy of blood derivatives on wound healing: A systematic review and network meta‐analysis
- 6,540 View
- 139 Download
- 4 Web of Science
- 4 Crossref

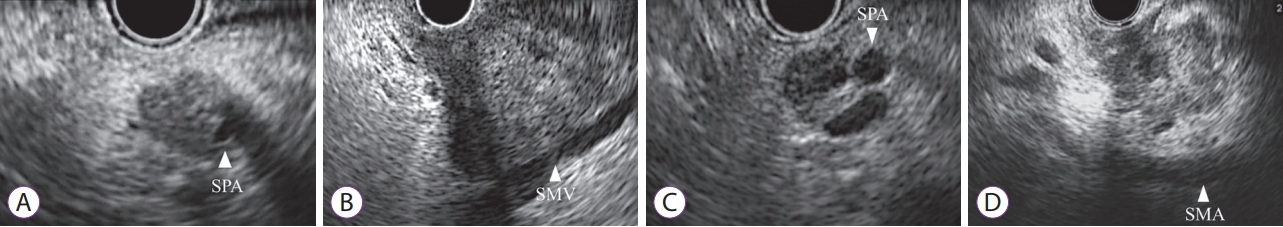
- Diagnostic Ability of Convex-Arrayed Endoscopic Ultrasonography for Major Vascular Invasion in Pancreatic Cancer
- Yuki Fujii, Kazuyuki Matsumoto, Hironari Kato, Yosuke Saragai, Saimon Takada, Sho Mizukawa, Shinichiro Muro, Daisuke Uchida, Takeshi Tomoda, Shigeru Horiguchi, Noriyuki Tanaka, Hiroyuki Okada
- Clin Endosc 2019;52(5):479-485. Published online May 16, 2019
- DOI: https://doi.org/10.5946/ce.2018.163
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: This study aimed to examine the diagnostic ability of endoscopic ultrasonography (EUS) for major vascular invasion in pancreatic cancer and to evaluate the relationship between EUS findings and pathological distance.
Methods
In total, 57 consecutive patients who underwent EUS for pancreatic cancer before surgery were retrospectively reviewed. EUS image findings were divided into four types according to the relationship between the tumor and major vessel (types 1 and 2: invasion, types 3 and 4: non-invasion). We also compared the EUS findings and pathologically measured distances between the tumors and evaluated vessels.
Results
The sensitivity, specificity, and accuracy of EUS diagnosis for vascular invasion were 89%, 92%, and 91%, respectively, in the veins and 83%, 94%, and 93%, respectively, in the arteries. The pathologically evaluated distances of cases with type 2 EUS findings were significantly shorter than those of cases with type 3 EUS findings in both the major veins (median [interquartile range], 96 [0–742] µm vs. 2,833 [1,076–5,694] µm, p=0.012) and arteries (623 [0–854] µm vs. 3,097 [1,396–6,000] µm, p=0.0061). All cases with a distance of ≥1,000 µm between the tumors and main vessels were correctly diagnosed.
Conclusions
Tumors at a distance ≥1,000 µm from the main vessels were correctly diagnosed by EUS. -
Citations
Citations to this article as recorded by- Role of Endoscopic Ultrasound in Staging and Vascular Assessment of Pancreatic Cancer
Mohammed A El-Nady, Khalid A Ead, Mustafa A Haridy, Nour Shaheen, Abdulqadir J Nashwan, Saad R Abdelwahid, Mohammed F Mohammed, Omran Mohamed, Safwat S Sawy, Emad Abdelrazzak, Amro M Hassan
Cureus.2024;[Epub] CrossRef - The diagnostic accuracy of endoscopic ultrasound vs. contrast-enhanced computed tomography in local staging of pancreatic adenocarcinoma: a bi-national multicenter study
Wisam Sbeit, Mahmoud Salman, Abed Khalaileh, Ahmad Zoabi, Zakhar Bramnik, David Hovel, Mahmud Mahamid, Eran Israeli, Lior Katz, Reem Khoury, Nama Mubariki, Andrea Lisotti, Halim Awadie, Tawfik Khoury
European Journal of Gastroenterology & Hepatology.2023; 35(9): 974. CrossRef - Role of Endoscopic Ultrasound in Diagnosis of Pancreatic Ductal Adenocarcinoma
Abhirup Chatterjee, Jimil Shah
Diagnostics.2023; 14(1): 78. CrossRef - The expanding role of endoscopic ultrasound elastography
Jahnvi Dhar, Jayanta Samanta
Clinical Journal of Gastroenterology.2022; 15(5): 841. CrossRef - Experience of introduction of endoscopic ultrasonography into daily clinical practice in a surgical hospital
A.V. Zhdanov, E.G. Solonitsyn, E.A. Korymasov
Endoskopicheskaya khirurgiya.2020; 26(5): 24. CrossRef - Endoscopic Ultrasonography for Vascular Invasion in Pancreatic Cancer
Seong-Hun Kim
Clinical Endoscopy.2019; 52(5): 397. CrossRef
- Role of Endoscopic Ultrasound in Staging and Vascular Assessment of Pancreatic Cancer
- 5,059 View
- 116 Download
- 5 Web of Science
- 6 Crossref

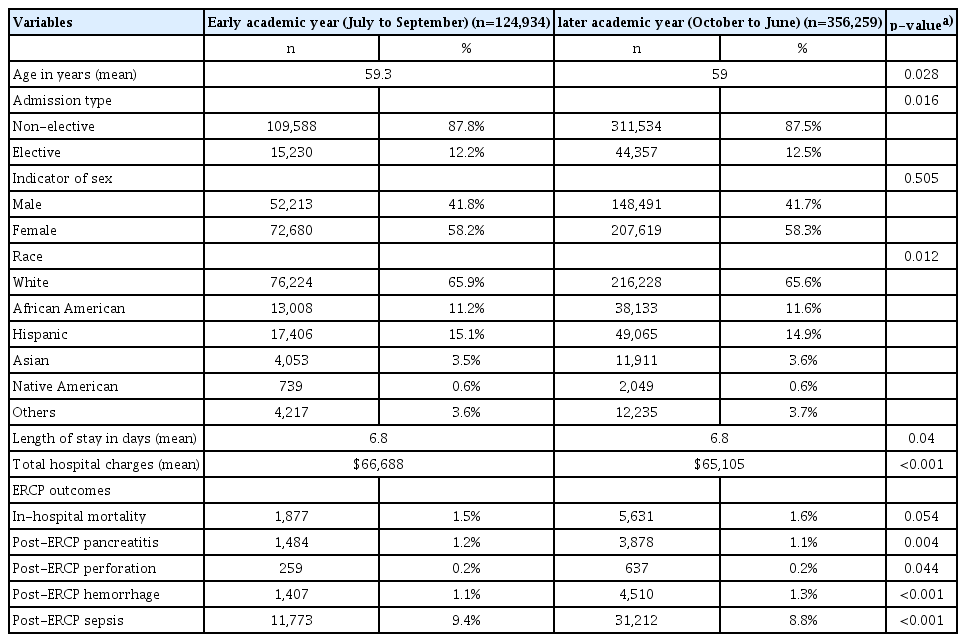
- A Nationwide Assessment of the “July Effect” and Predictors of Post-Endoscopic Retrograde Cholangiopancreatography Sepsis at Urban Teaching Hospitals in the United States
- Rupak Desai, Upenkumar Patel, Shreyans Doshi, Dipen Zalavadia, Wardah Siddiq, Hitanshu Dave, Mohammad Bilal, Vikas Khullar, Hemant Goyal, Madhav Desai, Nihar Shah
- Clin Endosc 2019;52(5):486-496. Published online May 27, 2019
- DOI: https://doi.org/10.5946/ce.2018.190
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: To analyze the incidence of post-endoscopic retrograde cholangiopancreatography (ERCP) sepsis in the early (July to September) and later (October to June) academic months to assess the “July effect”.
Methods
The National Inpatient Sample (2010–2014) was used to identify ERCP-related adult hospitalizations at urban teaching hospitals by applying relevant procedure codes from the International Classification of Diseases, 9th revision, Clinical Modification. Post-ERCP outcomes were compared between the early and later academic months. A multivariate analysis was performed to evaluate the odds of post-ERCP sepsis and its predictors.
Results
Of 481,193 ERCP procedures carried out at urban teaching hospitals, 124,934 were performed during the early academic months. The demographics were comparable for ERCP procedures performed during the early and later academic months. A higher incidence (9.4% vs. 8.8%, p<0.001) and odds (odds ratio [OR], 1.07) of post-ERCP sepsis were observed in ERCP performed during the early academic months. The in-hospital mortality rate (7% vs. 7.5%, p=0.072), length of stay, and total hospital charges in patients with post-ERCP sepsis were also equivalent between the 2 time points. Pre-ERCP cholangitis (OR, 3.20) and post-ERCP complications such as cholangitis (OR, 6.27), perforation (OR, 3.93), and hemorrhage (OR, 1.42) were significant predictors of higher post-ERCP sepsis in procedures performed during the early academic months.
Conclusions
The July effect was present in the incidence of post-ERCP sepsis, and academic programs should take into consideration the predictors of post-ERCP sepsis to lower health-care burden. -
Citations
Citations to this article as recorded by- A Nationwide Study of the “July Effect” Concerning Postpartum Hemorrhage and Its Risk Factors at Teaching Hospitals across the United States
Zahra Shahin, Gulzar H. Shah, Bettye A. Apenteng, Kristie Waterfield, Hani Samawi
Healthcare.2023; 11(6): 788. CrossRef - July effect in clinical outcomes of esophagogastroduodenoscopy performed at teaching hospitals in the United States
Karthik Gangu, Sanket Basida, Rehmat Ullah Awan, Mohammad Ali Butt, Austin Reed, Rao Afzal, Rahul Shekhar, Harleen Kaur Chela, Ebubekir S. Daglilar, Abu Baker Sheikh
Baylor University Medical Center Proceedings.2023; 36(4): 478. CrossRef - Increased ERCP volume improves cholangiogram interpretation: a new performance measure for ERCP training?
Shyam Vedantam, Sunil Amin, Ben Maher, Saqib Ahmad, Shanil Kadir, Saad Khalid Niaz, Mark Wright, Nadeem Tehami
Clinical Endoscopy.2022; 55(3): 426. CrossRef - Post-ERCP Pancreatitis: Prevention, Diagnosis and Management
Oscar Cahyadi, Nadeem Tehami, Enrique de-Madaria, Keith Siau
Medicina.2022; 58(9): 1261. CrossRef - Risk factors for infections after endoscopic retrograde cholangiopancreatography (ERCP): a retrospective cohort analysis of US Medicare Fee-For-Service claims, 2015–2021
Susan Hutfless, Yasutoshi Shiratori, Daniel Chu, Simon Liu, Anthony Kalloo
BMJ Open.2022; 12(9): e065077. CrossRef - Clinical coaches and patient safety – Just in time: A descriptive exploratory study
Lorraine Thompson, Frances Lin, Annette Faithfull-Byrne, Judith Gonzalez, Amanda Naumann, Kathryn Geisler, Cheryle Moss
Nurse Education in Practice.2021; 54: 103134. CrossRef - Is the July Effect Real in Patients Undergoing Endoscopic Retrograde Cholangiopancreatography?
Tae Yoon Lee, Yousuke Nakai
Clinical Endoscopy.2019; 52(5): 399. CrossRef
- A Nationwide Study of the “July Effect” Concerning Postpartum Hemorrhage and Its Risk Factors at Teaching Hospitals across the United States
- 5,771 View
- 81 Download
- 7 Web of Science
- 7 Crossref

Case Reports
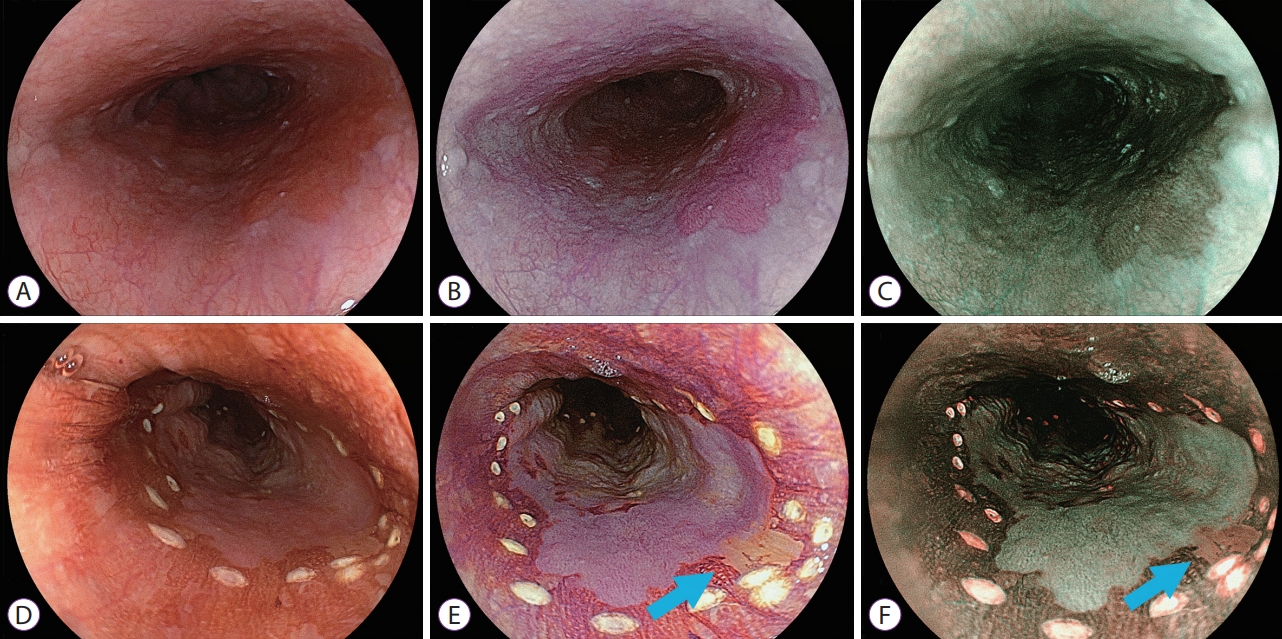
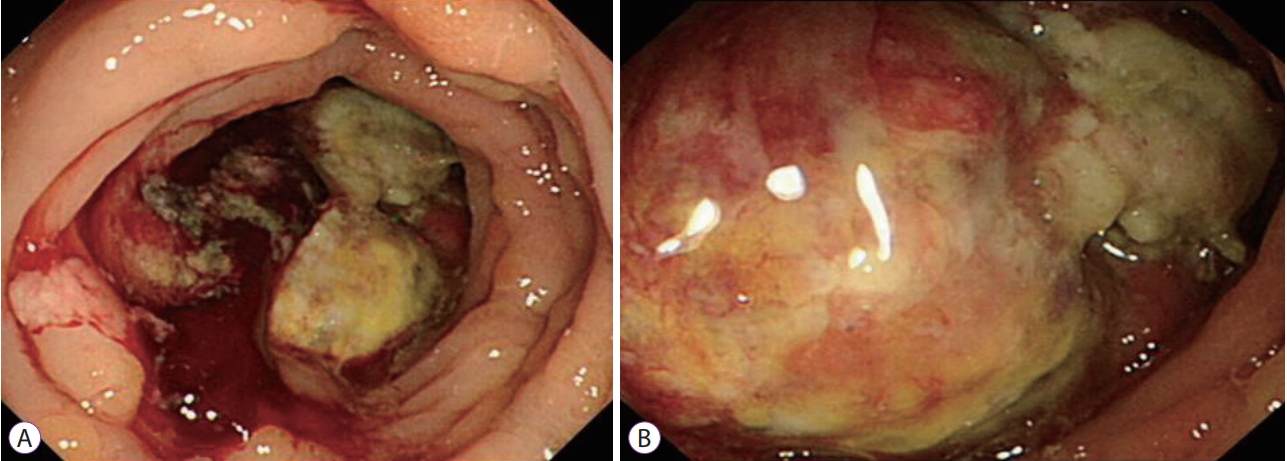
- New Diagnostic Approach for Esophageal Squamous Cell Neoplasms Using Linked Color Imaging and Blue Laser Imaging Combined with Iodine Staining
- Masato Tsunoda, Yoshimasa Miura, Hiroyuki Osawa, Tsevelnorov Khurelbaatar, Mio Sakaguchi, Hisashi Fukuda, Alan Kawarai Lefor, Hironori Yamamoto
- Clin Endosc 2019;52(5):497-501. Published online April 16, 2019
- DOI: https://doi.org/10.5946/ce.2018.195
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - A 62-year-old man with a flat early esophageal cancer was referred for endoscopic treatment. White light imaging revealed a pale red lesion, whereas linked color imaging (LCI) and blue laser imaging (BLI) yielded purple and brown images, respectively. Iodine staining demonstrated a large unstained area with a homogenous but very weak pink-color sign. This area appeared more clearly as purple and green on LCI and BLI, respectively; however, a different colored portion was observed at the 4 o’clock position inside the iodineunstained area. Histopathology findings of the resected specimen revealed squamous intraepithelial neoplasia at the 4 o’clock position and an esophageal squamous cell carcinoma in the remaining iodine-unstained area. LCI and BLI combined with iodine staining produce characteristic images that overcomes the pink-color sign, reflecting the histological features of a flat esophageal neoplasm. This new method is useful for detailed evaluation of early flat squamous cell neoplasms.
-
Citations
Citations to this article as recorded by- Linked color imaging vs Lugol chromoendoscopy for esophageal squamous cell cancer and precancerous lesion screening: A noninferiority study
Zi-Xin Wang, Long-Song Li, Song Su, Jin-Ping Li, Bo Zhang, Nan-Jun Wang, Sheng-Zhen Liu, Sha-Sha Wang, Shuai Zhang, Ya-Wei Bi, Fei Gao, Qun Shao, Ning Xu, Bo-Zong Shao, Yi Yao, Fang Liu, En-Qiang Linghu, Ning-Li Chai
World Journal of Gastroenterology.2023; 29(12): 1899. CrossRef - Usefulness of linked color imaging in the early detection of superficial esophageal squamous cell carcinomas
Koki Nakamura, Yuji Urabe, Shiro Oka, Naoko Nagasaki, Naoki Yorita, Kosaku Hata, Kazuhiko Masuda, Mio Kurihara, Takahiro Kotachi, Tomoyuki Boda, Shinji Tanaka, Kazuaki Chayama
Esophagus.2021; 18(1): 118. CrossRef - Inter‐observer variability of experts and trainees for the diagnosis of reflux esophagitis: Comparison of linked color imaging, blue laser imaging, and white light imaging
Sang Pyo Lee, Sea Hyub Kae, Hyun Joo Jang, Dong Hee Koh, Eun Suk Jung
Journal of Digestive Diseases.2021; 22(7): 425. CrossRef
- Linked color imaging vs Lugol chromoendoscopy for esophageal squamous cell cancer and precancerous lesion screening: A noninferiority study
- 5,242 View
- 147 Download
- 3 Web of Science
- 3 Crossref

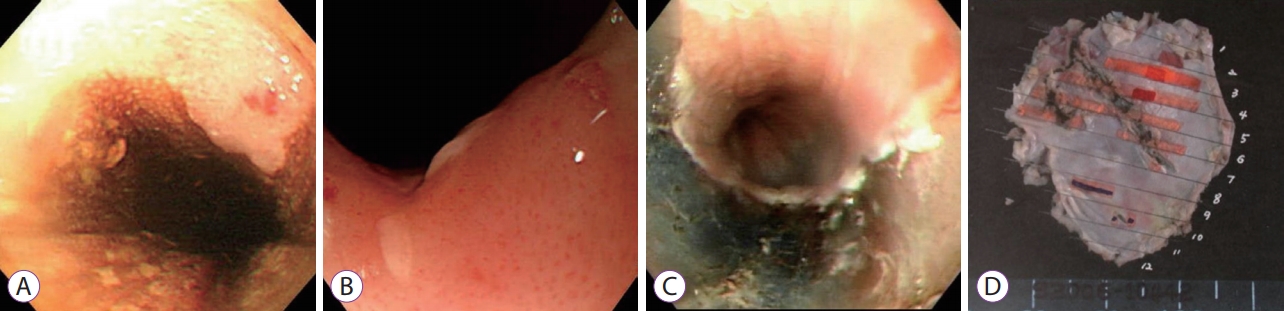
- Endoscopic Submucosal Dissection Followed by Concurrent Chemoradiotherapy in Patients with Early Esophageal Cancer with a High Risk of Lymph Node Metastasis
- Hee Kyung Kim, Weon Jin Ko, Chang-Il Kwon, Ga Won Song, In Kyun Yoo, Ji Hyun Song, Hak Su Kim, Joo Young Cho
- Clin Endosc 2019;52(5):502-505. Published online May 14, 2019
- DOI: https://doi.org/10.5946/ce.2018.176
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic submucosal dissection is recommended as an alternative therapy for early esophageal cancer. However, achieving curative resection in this procedure remains controversial since precise prediction of lymph node metastasis can be difficult. Here, we present the preliminary results of endoscopic submucosal dissection followed by concurrent chemoradiotherapy for early esophageal cancer with a high risk of lymph node metastasis. From May 2006 to January 2014, six patients underwent concurrent chemoradiotherapy after endoscopic submucosal dissection with a median follow-up period of 63 months. No complications were encountered during concurrent chemoradiotherapy. Although local recurrence did not occur in all patients, two patients were diagnosed with metachronous cancer. Overall, the survival rate was 100%. Thus, endoscopic submucosal dissection followed by concurrent chemoradiotherapy may be a feasible treatment for early esophageal cancer in patients with a high risk of lymph node metastasis. Future prospective large-scale studies are warranted to confirm our results.
-
Citations
Citations to this article as recorded by- Unveiling Therapeutic Targets for Esophageal Cancer: A Comprehensive Review
Rakesh Acharya, Ananya Mahapatra, Henu Kumar Verma, L. V. K. S. Bhaskar
Current Oncology.2023; 30(11): 9542. CrossRef - Editorial “Discrepancy Between the Clinical and Final Pathological Findings of Lymph Node Metastasis in Superficial Esophageal Cancer”
Rian M. Hasson, Joseph D. Phillips
Annals of Surgical Oncology.2019; 26(9): 2662. CrossRef
- Unveiling Therapeutic Targets for Esophageal Cancer: A Comprehensive Review
- 4,351 View
- 92 Download
- 1 Web of Science
- 2 Crossref

- Ascending Colon Cancer with Pathologically Confirmed Tumor Thrombosis of Superior Mesenteric Vein: A Case Report
- Sung Eun Kim, Sang Jin Lee, Jun Young Cha, Sang Won Yi, Tae Sun Kim, Il Leon Cho, Jae Young Kwak, Kwang Hoon Oh
- Clin Endosc 2019;52(5):506-509. Published online April 17, 2019
- DOI: https://doi.org/10.5946/ce.2018.135
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Colon cancer is very rarely accompanied by tumor thrombosis of the superior mesenteric vein (SMV). A 46-year-old patient had been diagnosed with SMV tumor thrombosis related to colon cancer without hepatic metastasis and underwent right hemicolectomy with SMV tumor thrombectomy. Tumor thrombosis was pathologically confirmed as metastatic colon cancer. There has been no recurrence for 12 months with 12 cycles of adjuvant-chemotherapy.
-
Citations
Citations to this article as recorded by- Superior mesenteric vein tumour thrombus in a patient with caecal adenocarcinoma: a rare and important finding
Janki Trivedi, Heinrich Bouwer, Tom Sutherland
BJR|case reports.2021; 7(2): 20200147. CrossRef - Isolated Malignant Portal Vein Thrombus in Colon Carcinoma: A Rare Finding on 18F-FDG PET/CECT
Tarun Kumar Jain, Ajay Yadav, Hemant Malhotra, Nitin Khunteta, Guman Singh
Journal of Nuclear Medicine Technology.2021; 49(2): 190. CrossRef - Ascending colon cancer accompanied by tumor thrombosis in the superior mesenteric vein: A case report
Yoshiaki Fujii, Kenji Kobayashi, Sho Kimura, Shuhei Uehara, Shuji Takiguchi
International Journal of Surgery Case Reports.2020; 73: 239. CrossRef - Treatment of tumor thrombus in the superior mesenteric vein due to advanced colon cancer with complete surgical resection and chemotherapy: a case report
Yoshitsugu Yanagida, Takahiro Amano, Ryuji Akai, Akira Toyoshima, Jotaro Kobayashi, Takuya Hashimoto, Eiji Sunami, Toshio Kumasaka, Shin Sasaki
Surgical Case Reports.2020;[Epub] CrossRef
- Superior mesenteric vein tumour thrombus in a patient with caecal adenocarcinoma: a rare and important finding
- 4,688 View
- 101 Download
- 4 Web of Science
- 4 Crossref

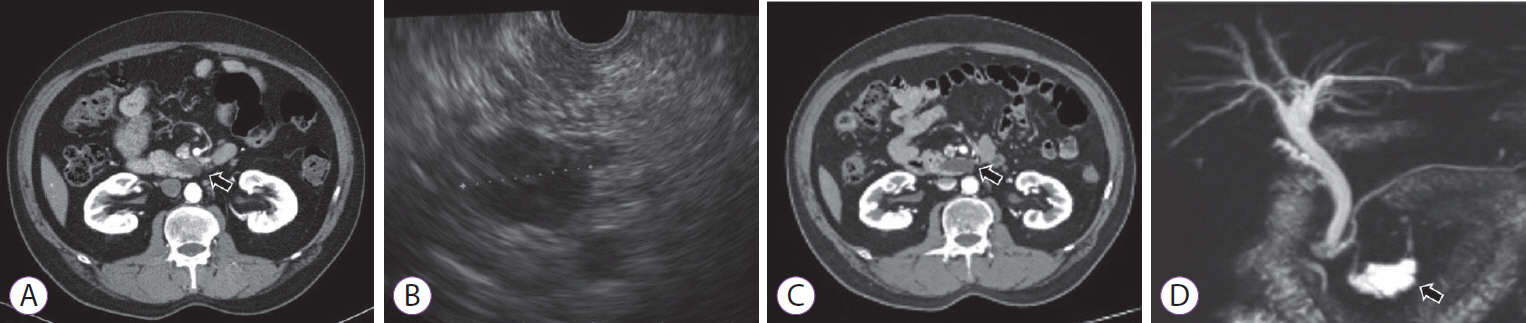
- Duodenal Stricture due to Necrotizing Pancreatitis following Endoscopic Ultrasound-Guided Ethanol Ablation of a Pancreatic Cyst: A Case Report
- Jung Won Chun, Sang Hyub Lee, Jin Ho Choi, Woo Hyun Paik, Ji Kon Ryu, Yong-Tae Kim
- Clin Endosc 2019;52(5):510-515. Published online July 4, 2019
- DOI: https://doi.org/10.5946/ce.2018.191
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The frequency of incidental detection of pancreatic cystic lesions (PCLs) is increasing because of the frequent use of cross-sectional imaging. The appropriate treatment for PCLs is challenging, and endoscopic ultrasound-guided ablation for PCLs has been reported in several studies. Although the feasibility and efficacy of this therapeutic modality have been shown, the safety issues associated with the procedure are still a concern. We present a case of a 61-year-old man who underwent ultrasound-guided ethanol ablation for PCL and needed repeated endoscopic balloon dilatation for severe duodenal stricture caused by necrotizing pancreatitis after the cyst ablation therapy.
-
Citations
Citations to this article as recorded by- Benign Duodenal Stricture Treated with Surgical Correction and Dietary Therapy in a Golden Retriever
John C. Rowe, Alice A. Huang, Jin Heo, Nolie K. Parnell, Adam J. Rudinsky
Case Reports in Veterinary Medicine.2020; 2020: 1. CrossRef - Endoscopic ultrasound-guided injective ablative treatment of pancreatic cystic neoplasms
Chen Du, Ning-Li Chai, En-Qiang Linghu, Hui-Kai Li, Xiu-Xue Feng
World Journal of Gastroenterology.2020; 26(23): 3213. CrossRef
- Benign Duodenal Stricture Treated with Surgical Correction and Dietary Therapy in a Golden Retriever
- 4,502 View
- 104 Download
- 1 Web of Science
- 2 Crossref

Brief Report
- Re-Visiting Metoclopramide to Optimize Visualization with Gastrointestinal Bleeding – Mobilizing Existing Data
- Derek J. Estes, Shivali Berera, Amar R. Deshpande, Daniel A. Sussman
- Clin Endosc 2019;52(5):516-517. Published online July 16, 2019
- DOI: https://doi.org/10.5946/ce.2019.046
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Emergency medicine updates: Upper gastrointestinal bleeding
Brit Long, Michael Gottlieb
The American Journal of Emergency Medicine.2024; 81: 116. CrossRef - The Use of Pre-Endoscopic Metoclopramide Does Not Prevent the Need for Repeat Endoscopy: A U.S. Based Retrospective Cohort Study
Mark Ayoub, Carol Faris, Julton Tomanguillo, Nadeem Anwar, Harleen Chela, Ebubekir Daglilar
Life.2024; 14(4): 526. CrossRef - Gastrointestinal Bleeding in the Neonate: Updates on Diagnostics, Therapeutics, and Management
Patrick T. Reeves, La’Toya James-Davis, Muhammad A. Khan
NeoReviews.2023; 24(7): e403. CrossRef
- Emergency medicine updates: Upper gastrointestinal bleeding
- 4,000 View
- 117 Download
- 2 Web of Science
- 3 Crossref


 KSGE
KSGE




 First
First Prev
Prev



