Search
- Page Path
- HOME > Search
Review
- Forward viewing liner echoendoscopy for therapeutic interventions
- Kazuo Hara, Nozomi Okuno, Shin Haba, Takamichi Kuwahara
- Clin Endosc 2024;57(2):175-180. Published online February 29, 2024
- DOI: https://doi.org/10.5946/ce.2023.271
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Therapeutic endoscopic ultrasonography (EUS) procedures using the forward-viewing convex EUS (FV-EUS) have been reviewed based on the articles reported to date. The earliest reported procedure is the drainage of pancreatic pseudocysts using FV-EUS. However, the study on drainage of pancreatic pseudocysts focused on showing that drainage is possible with FV-EUS rather than leveraging its features. Subsequently, studies describing the characteristics of FV-EUS have been reported. By using FV-EUS in EUS-guided choledochoduodenostomy, double punctures in the gastrointestinal tract can be avoided. In postoperative modified anatomical cases, using the endoscopic function of FV-EUS, procedures such as bile duct drainage from anastomosis, pancreatic duct drainage from the afferent limb, and abscess drainage from the digestive tract have been reported. When a perpendicular puncture to the gastrointestinal tract is required or when there is a need to insert the endoscope deep into the gastrointestinal tract, FV-EUS is considered among the options.
- 2,871 View
- 167 Download

Original Articles
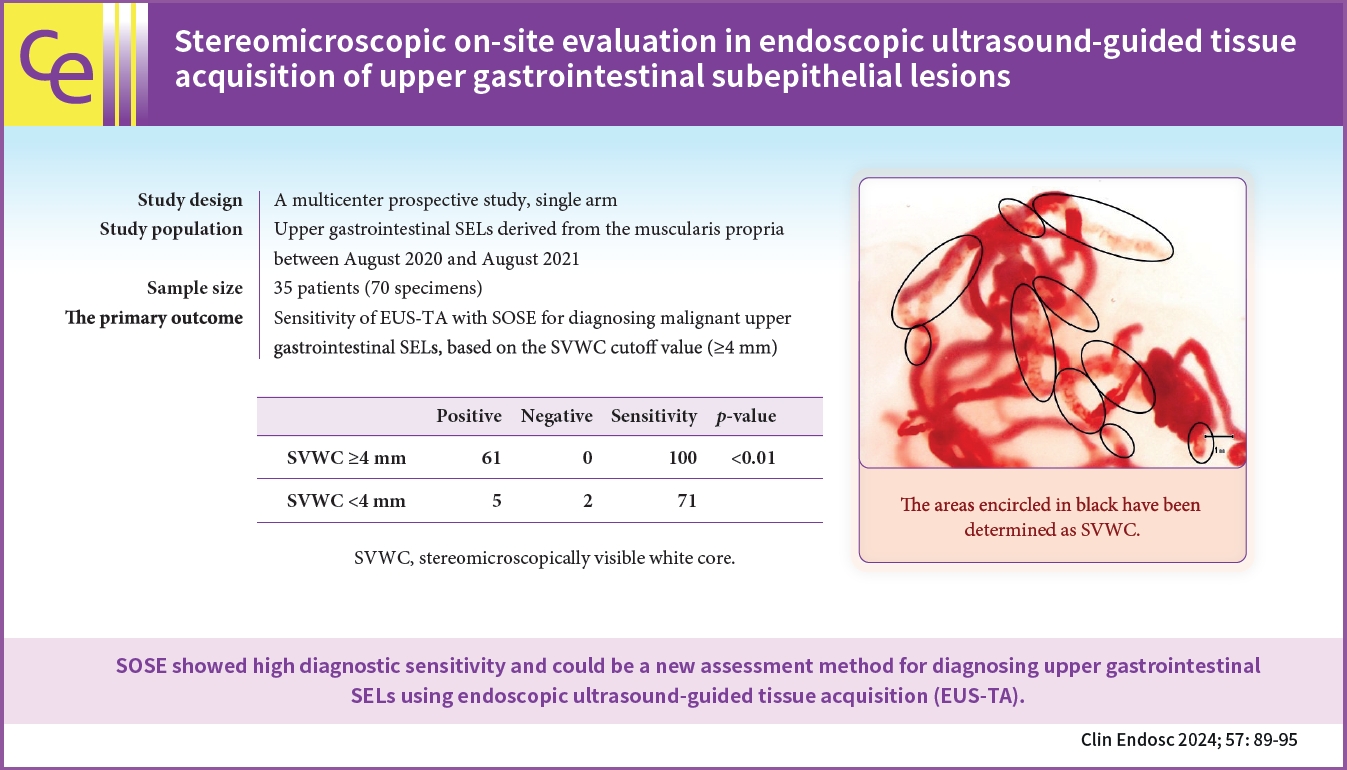
- Stereomicroscopic on-site evaluation in endoscopic ultrasound-guided tissue acquisition of upper gastrointestinal subepithelial lesions
- Seigo Nakatani, Kosuke Okuwaki, Masafumi Watanabe, Hiroshi Imaizumi, Tomohisa Iwai, Takaaki Matsumoto, Rikiya Hasegawa, Hironori Masutani, Takahiro Kurosu, Akihiro Tamaki, Junro Ishizaki, Ayana Ishizaki, Mitsuhiro Kida, Chika Kusano
- Clin Endosc 2024;57(1):89-95. Published online April 18, 2023
- DOI: https://doi.org/10.5946/ce.2022.288
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 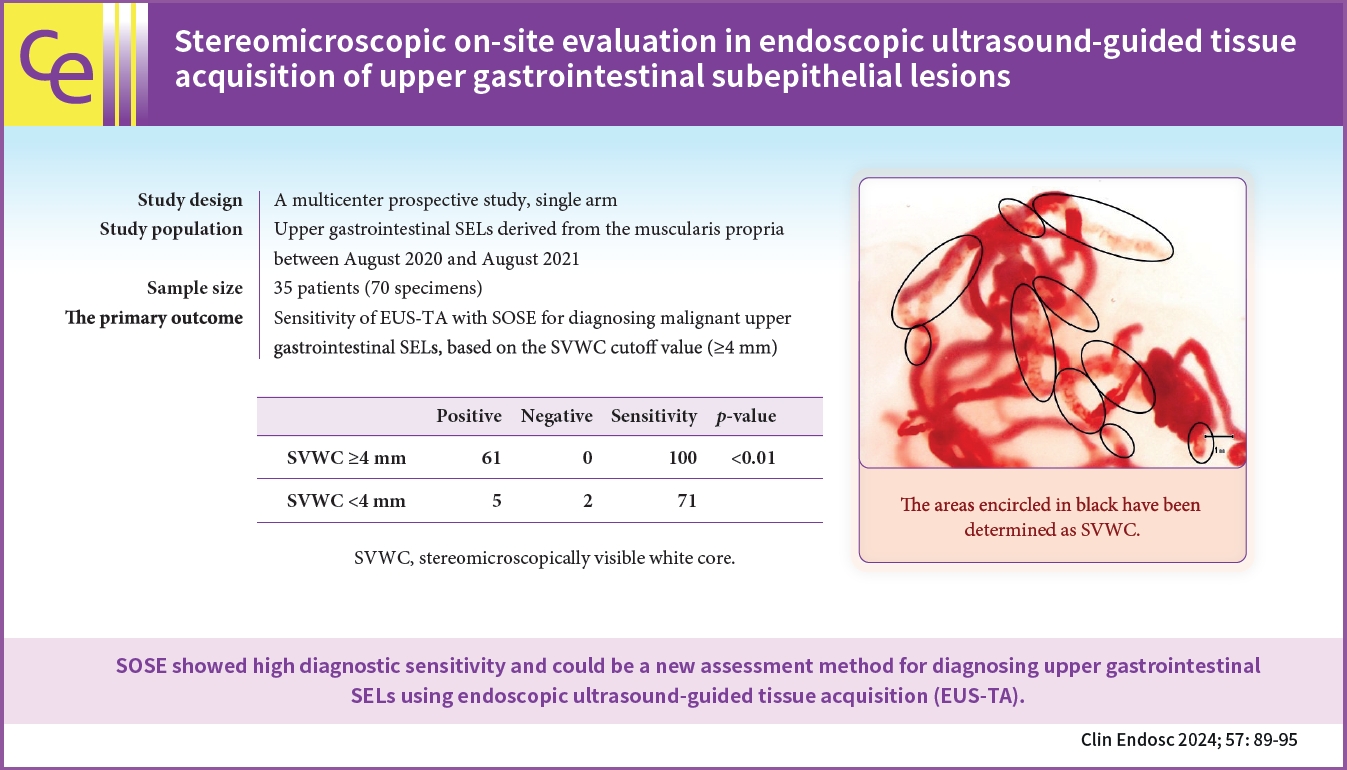
- Background
/Aims: In stereomicroscopic sample isolation processing, the cutoff value (≥4 mm) of stereomicroscopically visible white cores indicates high diagnostic sensitivity. We aimed to evaluate endoscopic ultrasound-guided tissue acquisition (EUS-TA) using a simplified stereomicroscopic on-site evaluation of upper gastrointestinal subepithelial lesions (SELs).
Methods
In this multicenter prospective trial, we performed EUS-TA using a 22-gauge Franseen needle in 34 participants with SELs derived from the upper gastrointestinal muscularis propria, requiring pathological diagnosis. The presence of stereomicroscopically visible white core (SVWC) in each specimen was assessed using stereomicroscopic on-site evaluation. The primary outcome was EUS-TA’s diagnostic sensitivity with stereomicroscopic on-site evaluation based on the SVWC cutoff value (≥4 mm) for malignant upper gastrointestinal SELs.
Results
The total number of punctures was 68; 61 specimens (89.7%) contained stereomicroscopically visible white cores ≥4 mm in size. The final diagnoses were gastrointestinal stromal tumor, leiomyoma, and schwannoma in 76.5%, 14.7%, and 8.8% of the cases, respectively. The sensitivity of EUS-TA with stereomicroscopic on-site evaluation based on the SVWC cutoff value for malignant SELs was 100%. The per-lesion accuracy of histological diagnosis reached the highest level (100%) at the second puncture.
Conclusions
Stereomicroscopic on-site evaluation showed high diagnostic sensitivity and could be a new method for diagnosing upper gastrointestinal SELs using EUS-TA. -
Citations
Citations to this article as recorded by- What method can we choose if rapid on-site evaluation is not available for the endoscopic ultrasound-guided tissue acquisition of upper gastrointestinal subepithelial lesions?
Yu Kyung Cho
Clinical Endoscopy.2024; 57(1): 53. CrossRef - Endoscopic Ultrasound-Guided Tissue Acquisition Using Fork-Tip Needle for Subepithelial Lesions: A Single-Center Validation Study
Masafumi Watanabe, Kosuke Okuwaki, Tomohisa Iwai, Mitsuhiro Kida, Hiroshi Imaizumi, Kai Adachi, Akihiro Tamaki, Junro Ishizaki, Taro Hanaoka, Chika Kusano
Digestive Diseases and Sciences.2024;[Epub] CrossRef - An Esophageal Leiomyoma with Cystic Degeneration Mimicking a Malignant Neoplasm
Gwang Ha Kim, Dong Chan Joo, Moon Won Lee, Bong Eun Lee, Kyungbin Kim
The Ewha Medical Journal.2023;[Epub] CrossRef
- What method can we choose if rapid on-site evaluation is not available for the endoscopic ultrasound-guided tissue acquisition of upper gastrointestinal subepithelial lesions?
- 1,837 View
- 140 Download
- 3 Web of Science
- 3 Crossref

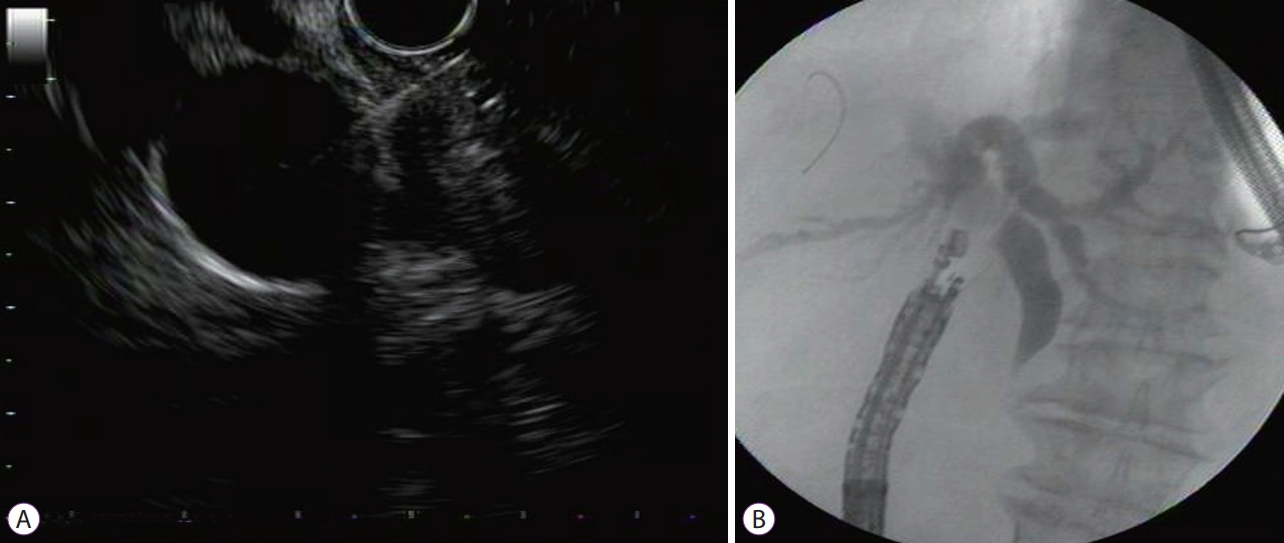
- Role of interventional endoscopic ultrasound in a developing country
- Hasan Maulahela, Nagita Gianty Annisa, Achmad Fauzi, Kaka Renaldi, Murdani Abdullah, Marcellus Simadibrata, Dadang Makmun, Ari Fahrial Syam
- Clin Endosc 2023;56(1):100-106. Published online January 17, 2023
- DOI: https://doi.org/10.5946/ce.2022.058

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic ultrasound (EUS) has become an essential diagnostic and therapeutic tool. EUS was introduced in 2013 in Indonesia and is considered relatively new. This study aimed to describe the current role of interventional EUS at our hospital as a part of the Indonesian tertiary health center experience.
Methods
This retrospective study included all patients who underwent interventional EUS (n=94) at our center between January 2015 and December 2020. Patient characteristics, technical success, clinical success, and adverse events associated with each type of interventional EUS procedure were evaluated.
Results
Altogether, 94 interventional EUS procedures were performed at our center between 2015 and 2020 including 75 cases of EUS-guided biliary drainage (EUS-BD), 14 cases of EUS-guided pancreatic fluid drainage, and five cases of EUS-guided celiac plexus neurolysis. The technical and clinical success rates of EUS-BD were 98.6% and 52%, respectively. The technical success rate was 100% for both EUS-guided pancreatic fluid drainage and EUS-guided celiac plexus neurolysis. The adverse event rates were 10.6% and 7.1% for EUS-BD and EUS-guided pancreatic fluid drainage, respectively.
Conclusions
EUS is an effective and safe tool for the treatment of gastrointestinal and biliary diseases. It has a low rate of adverse events, even in developing countries. -
Citations
Citations to this article as recorded by- EUS-guided interventional therapies for pancreatic diseases
Rongmin Xu, Kai Zhang, Nan Ge, Siyu Sun
Frontiers in Medicine.2024;[Epub] CrossRef
- EUS-guided interventional therapies for pancreatic diseases
- 2,055 View
- 135 Download
- 1 Web of Science
- 1 Crossref

- Endoscopic Ultrasound-Guided, Percutaneous, and Transjugular Liver Biopsy: A Comparative Systematic Review and Meta-Analysis
- Thomas R. McCarty, Ahmad Najdat Bazarbashi, Basile Njei, Marvin Ryou, Harry R. Aslanian, Thiruvengadam Muniraj
- Clin Endosc 2020;53(5):583-593. Published online September 29, 2020
- DOI: https://doi.org/10.5946/ce.2019.211

-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: Percutaneous liver biopsy (PCLB) or transjugular liver biopsy (TJLB) have traditionally been performed to obtain a sample of hepatic tissue; however, endoscopic ultrasound-guided liver biopsy (EUSLB) has become an attractive alternative. The aim of this study was to compare the efficacy and safety of EUSLB, PCLB, and TJLB.
Methods
Search strategies were developed in accordance with PRISMA and MOOSE guidelines. Major outcomes included the following: adequacy of biopsy specimens (i.e., complete portal triads [CPT], total specimen length [TSL] in mm, and length of longest piece [LLP]) in mm), and rate of adverse events. Only studies comparing all biopsy approaches (i.e., EUSLB, PCLB, and TJLB) were included.
Results
Five studies (EUSLB [n=301]; PCLB [n=176]; and TJLB [n=179]) were included. Biopsy cumulative adequacy rates for EUSLB, PCLB, and TJLB were 93.51%, 98.27%, and 97.61%, respectively. Based on the subgroup analysis limited to EUS biopsy needles in current clinical practice, there was no difference in biopsy adequacy or adverse events for EUSLB compared to PCLB and TJLB (all p>0.050). A comparison of EUSLB and PCLB revealed no difference between specimens regarding both CPT (p=0.079) and LLP (p=0.085); however, a longer TSL (p<0.001) was observed. Compared to TJLB, EUSLB showed no difference in LLP (p=0.351), fewer CPT (p=0.042), and longer TSL (p=0.005).
Conclusions
EUSLB appears to be a safe, minimally invasive procedure that is comparable to PCLB and TJLB regarding biopsy specimens obtained and rate of adverse events associated with each method. -
Citations
Citations to this article as recorded by- Endoscopic procedures in hepatology: Current trends and new developments
Wim Laleman, Emma Vanderschueren, Zain Seyad Mehdi, Reiner Wiest, Andres Cardenas, Jonel Trebicka
Journal of Hepatology.2024; 80(1): 124. CrossRef - Gut-liver axis: Pathophysiological concepts and medical perspective in chronic liver diseases
Susana G. Rodrigues, Schalk van der Merwe, Aleksander Krag, Reiner Wiest
Seminars in Immunology.2024; 71: 101859. CrossRef - Comparison of diagnostic outcomes, safety, and cost of Franseen-tip 19G versus 22G needles for endoscopic ultrasound-guided liver biopsies
Ankit Dalal, Nagesh Kamat, Gaurav Patil, Amol Vadgaonkar, Sanil Parekh, Sehajad Vora, Amit Maydeo
Endoscopy International Open.2024; 12(02): E291. CrossRef - Endoscopic ultrasound-guided liver biopsy in liver transplant recipients: A preliminary experience
Wei Rao, Yue-Ping Jiang, Jin-Zhen Cai, Man Xie
Hepatobiliary & Pancreatic Diseases International.2024;[Epub] CrossRef - Comparison of Diagnostic Accuracy and Diagnostic Adequacy Between Endoscopic Ultrasound-Guided and Percutaneous Liver Biopsies: A Meta-Analysis of Randomized Controlled Trials and Observational Studies
Mansoor Ahmad, Taslova Tahsin Abedin, Faria Khilji, Kinan Obeidat, Lam Vinh Sieu, Sandipkumar S Chaudhari, Divine Besong Arrey Agbor, Danish Allahwala
Cureus.2024;[Epub] CrossRef - Comparative accuracy of endosonographic shear wave elastography and transcutaneous liver stiffness measurement: a pilot study
Divyanshoo R. Kohli, Daniel Mettman, Nevene Andraws, Erin Haer, Jaime Porter, Ozlem Ulusurac, Steven Ullery, Madhav Desai, Mohammad S. Siddiqui, Prateek Sharma
Gastrointestinal Endoscopy.2023; 97(1): 35. CrossRef - EUS-guided versus percutaneous liver biopsy: A comprehensive review and meta-analysis of outcomes
Saurabh Chandan, Smit Deliwala, ShahabR Khan, BabuP Mohan, BanreetS Dhindsa, Jay Bapaye, Hemant Goyal, LenaL Kassab, Faisal Kamal, HarlanR Sayles, GursimranS Kochhar, DouglasG Adler
Endoscopic Ultrasound.2023; 12(2): 171. CrossRef - Advances in Endoscopic Ultrasound (EUS)-Guided Liver Biopsy
Daryl Ramai, Viraaj Pannu, Antonio Facciorusso, Banreet Dhindsa, Joseph Heaton, Andrew Ofosu, Saurabh Chandan, Marcello Maida, Barbara Lattanzi, Eduardo Rodriguez, Vicky H. Bhagat, Jayanta Samanta, Monique T. Barakat
Diagnostics.2023; 13(4): 784. CrossRef - Endoscopic Advances in Hepatology
Emma Vanderschueren, Jonel Trebicka, Wim Laleman
Seminars in Liver Disease.2023; 43(02): 176. CrossRef - Quality of Tissue Samples Obtained by Endoscopic Ultrasound-Guided Liver Biopsy: A Randomized, Controlled Clinical Trial
José Lariño-Noia, Javier Fernández-Castroagudín, Daniel de la Iglesia-García, Héctor Lázare, Laura Nieto, Sol Porto, Nicolau Vallejo-Senra, Esther Molina, Alba San Bruno, Xurxo Martínez-Seara, Julio Iglesias-García, Silvia García-Acuña, J. Enrique Domíngu
American Journal of Gastroenterology.2023; 118(10): 1821. CrossRef - Endo-hepatology: Updates for the clinical hepatologist
Frances Lee, Tarun Rustagi, R. Todd Frederick
Clinical Liver Disease.2023; 22(2): 42. CrossRef - Technical Success, Sample Adequacy, and Complications of Pediatric Transjugular Liver Biopsy: A Systematic Review and Meta-Analysis
Karen Smayra, Shahid Miangul, Nathanael Yap, Ao Shi, Fatma Abdulsalam, Maamoun Adra, Hayato Nakanishi, Jake Ball, Tara A. Betts, Christian A. Than, Aneeta Parthipun
Digestive Diseases and Sciences.2023; 68(10): 3846. CrossRef - Role of endoscopic ultrasound and endoscopic ultrasound-guided tissue acquisition in diagnosing hepatic focal lesions
Hussein Hassan Okasha, Hanane Delsa, Abdelmoneim Alsawaf, Ahmed Morad Hashim, Hani M Khattab, Dalia Abdelfatah, Abeer Abdellatef, Amr Albitar
World Journal of Methodology.2023; 13(4): 287. CrossRef - Chinese expert consensus on multidisciplinary diagnosis and treatment of pancreatic neuroendocrine liver metastases
Yihebali Chi, Liming Jiang, Susheng Shi, Shun He, Chunmei Bai, Dan Cao, Jianqiang Cai, Qichen Chen, Xiao Chen, Yiqiao Deng, Shunda Du, Zhen Huang, Li Huo, Yuan Ji, Jie Li, Wenhui Lou, Jie Luo, Xueying Shi, Lijie Song, Bei Sun, Huangying Tan, Feng Wang, Xu
Journal of Pancreatology.2023; 6(4): 139. CrossRef - Distinct ways to perform a liver biopsy: The core technique setups and updated understanding of these modalities
Chao Sun, Xingliang Zhao, Lei Shi, Xiaofei Fan, Xiaolong Qi
Endoscopic Ultrasound.2023; 12(6): 437. CrossRef - Endo-Hepatology: The Buzz Goes Much beyond Liver Biopsy—A Narrative Review
Rajesh Puri, Zubin Sharma, Swapnil Dhampalwar, Abhishek Kathuria, Bimal Sahu
Journal of Digestive Endoscopy.2023; 14(04): 227. CrossRef - Diagnostic yield of endoscopic ultrasound-guided liver biopsy in comparison to percutaneous liver biopsy: a systematic review and meta-analysis
Antonio Facciorusso, Stefano Francesco Crinò, Daryl Ramai, Carlo Fabbri, Benedetto Mangiavillano, Andrea Lisotti, Nicola Muscatiello, Christian Cotsoglou, Pietro Fusaroli
Expert Review of Gastroenterology & Hepatology.2022; 16(1): 51. CrossRef - Endoscopic Ultrasound-Guided Liver Biopsy Using Newer 19G FNB Needles Compared to Percutaneous and Transjugular Liver Biopsy: A Tertiary Center Experience
Harsh K. Patel, George Therapondos, Gretchen Galliano, Ricardo. Romero, John Evans, Ari Cohen, Muhammad F. Mubarak, Janak N. Shah, Abdul Hamid El Chafic
Techniques and Innovations in Gastrointestinal Endoscopy.2022; 24(2): 127. CrossRef - Role of endoscopic ultrasound-guided liver biopsy: a meta-analysis
Keyu Zeng, Zhenpeng Jiang, Jie Yang, Kefei Chen, Qiang Lu
Scandinavian Journal of Gastroenterology.2022; 57(5): 545. CrossRef - Endoscopic ultrasound guided interventions in the management of pancreatic cancer
Tossapol Kerdsirichairat, Eun Ji Shin
World Journal of Gastrointestinal Endoscopy.2022; 14(4): 191. CrossRef - Endohepatology – current status
Jerome C. Edelson, Natalie E. Mitchell, Don C. Rockey
Current Opinion in Gastroenterology.2022; 38(3): 216. CrossRef - Diagnostic and interventional EUS in hepatology: An updated review
Vaneet Jearth, Sridhar Sundaram, SurinderSingh Rana
Endoscopic Ultrasound.2022; 11(5): 355. CrossRef - A Gene Expression Signature to Select Hepatocellular Carcinoma Patients for Liver Transplantation
Hugo Pinto-Marques, Joana Cardoso, Sílvia Silva, João L. Neto, Maria Gonçalves-Reis, Daniela Proença, Marta Mesquita, André Manso, Sara Carapeta, Mafalda Sobral, Antonio Figueiredo, Clara Rodrigues, Adelaide Milheiro, Ana Carvalho, Rui Perdigoto, Eduardo
Annals of Surgery.2022; 276(5): 868. CrossRef - Endo‐hepatology: The changing paradigm of endoscopic ultrasound in cirrhosis
Achintya Dinesh Singh, Ahmad Najdat Bazarbashi, Christina C. Lindenmeyer
Clinical Liver Disease.2022; 20(6): 209. CrossRef - Feasibility and Safety of Transjugular Liver Biopsy for Japanese Patients with Chronic Liver Diseases
Makoto Iijima, Takahiro Arisaka, Akira Yamamiya, Keiichi Tominaga, Kazunori Nagashima, Akira Kanamori, Satoshi Masuyama, Yuichi Majima, Kenichi Goda, Kazuyuki Ishida, Atsushi Irisawa
Diagnostics.2021; 11(1): 131. CrossRef - Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clinical Endoscopy.2021; 54(5): 633. CrossRef - Role of Endoscopic Ultrasound in Liver Disease: Where Do We Stand?
Tajana Pavic, Ivana Mikolasevic, Dominik Kralj, Nina Blazevic, Anita Skrtic, Ivan Budimir, Ivan Lerotic, Davor Hrabar
Diagnostics.2021; 11(11): 2021. CrossRef
- Endoscopic procedures in hepatology: Current trends and new developments
- 6,133 View
- 174 Download
- 23 Web of Science
- 27 Crossref

Focused Review Series: Endoscopic Hemostasis: An Overview of Principles and Recent Applications
- Endoscopic Therapy and Radiologic Intervention of Acute Gastroesophageal Variceal Bleeding
- Jeong Eun Song, Byung Seok Kim
- Clin Endosc 2019;52(5):407-415. Published online September 30, 2019
- DOI: https://doi.org/10.5946/ce.2019.178

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Acute gastroesophageal variceal hemorrhage is a dreaded complication in patients with liver cirrhosis. Endoscopic therapy and radiologic intervention for gastroesophageal bleeding have rapidly developed in the recent decades. Endoscopic treatment is initially performed to stop variceal hemorrhage. For the treatment of esophageal variceal bleeding, endoscopic variceal ligation (EVL) is considered the endoscopic treatment of choice. In cases of gastric variceal hemorrhage, the type of gastric varices (GVs) is important in deciding the strategy of endoscopic treatment. Endoscopic variceal obturation (EVO) is recommended for fundal variceal bleeding. For the management of gastroesophageal varix type 1 bleeding, both EVO and EVL are available treatment options; however, EVO is preferred over EVL. If endoscopic management fails to control variceal hemorrhage, radiologic interventional modalities could be considered. Transjugular intrahepatic portosystemic shunt is a good option for rescue treatment in refractory variceal bleeding. In cases of refractory hemorrhage of GVs in patients with a gastrorenal shunt, balloon-occluded retrograde transvenous obliteration could be considered as a salvage treatment.
-
Citations
Citations to this article as recorded by- Transjugular intrahepatic portosystemic shunt for esophagojejunal variceal bleeding after total gastrectomy: A case report
Sang Un Kim, Jihoon Hong
Radiology Case Reports.2024; 19(8): 3231. CrossRef - Efficacy of early re-ligation after endoscopic gastric glue injection combined with endoscopic variceal ligation in preventing rebleeding of esophagogastric varices in patients with cirrhosis
Hui-Min Liu, Zhi-Bin Gong
World Chinese Journal of Digestology.2022; 30(17): 748. CrossRef - The Role of Interventional Radiology in Esophageal Varices and Hematemesis: Review Article
Qaed Salem Alhammami, Maisa Hamad Freaj Alanazi, Shahad Khalid A Bedaiwi, Ghazir Aneed N Alruwili, Shouq Fayed Khalaf Alanazi
Archives of Pharmacy Practice.2022; 13(4): 7. CrossRef - Comprehensive treatment of patients with gastric variceal bleeding
S.M. Chooklin, S.S. Chuklin
EMERGENCY MEDICINE.2022; 18(8): 14. CrossRef
- Transjugular intrahepatic portosystemic shunt for esophagojejunal variceal bleeding after total gastrectomy: A case report
- 8,252 View
- 320 Download
- 1 Web of Science
- 4 Crossref

Reviews
- Review of Simultaneous Double Stenting Using Endoscopic Ultrasound-Guided Biliary Drainage Techniques in Combined Gastric Outlet and Biliary Obstructions
- Hao Chi Zhang, Monica Tamil, Keshav Kukreja, Shashideep Singhal
- Clin Endosc 2020;53(2):167-175. Published online August 13, 2019
- DOI: https://doi.org/10.5946/ce.2019.050
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Concomitant malignant gastric outlet obstruction and biliary obstruction may occur in patients with advanced cancers affecting these anatomical regions. This scenario presents a unique challenge to the endoscopist in selecting an optimal management approach. We sought to determine the efficacy and safety of endoscopic techniques for treating simultaneous gastric outlet and biliary obstruction (GOBO) with endoscopic ultrasound (EUS) guidance for biliary drainage. An extensive literature search for peer-reviewed published cases yielded 6 unique case series that either focused on or included the use of EUS-guided biliary drainage (EUS-BD) with simultaneous gastroduodenal stenting. In our composite analysis, a total of 51 patients underwent simultaneous biliary drainage through EUS, with an overall reported technical success rate of 100% for both duodenal stenting and biliary drainage. EUS-guided choledochoduodenostomy or EUS-guided hepaticogastrostomy was employed as the initial technique. In 34 cases in which clinical success was ascribed, 100% derived clinical benefit. The common adverse effects of double stenting included cholangitis, stent migration, bleeding, food impaction, and pancreatitis. We conclude that simultaneous double stenting with EUS-BD and gastroduodenal stenting for GOBO is associated with high success rates. It is a feasible and practical alternative to percutaneous biliary drainage or surgery for palliation in patients with associated advanced malignancies.
-
Citations
Citations to this article as recorded by- Endoscopic Management of Malignant Biliary Obstruction
Woo Hyun Paik, Do Hyun Park
Gastrointestinal Endoscopy Clinics of North America.2024; 34(1): 127. CrossRef - Long‐term outcomes of endoscopic double stenting using an anti‐reflux metal stent for combined malignant biliary and duodenal obstruction
Takashi Sasaki, Tsuyoshi Takeda, Yuto Yamada, Takeshi Okamoto, Chinatsu Mori, Takafumi Mie, Akiyoshi Kasuga, Masato Matsuyama, Masato Ozaka, Naoki Sasahira
Journal of Hepato-Biliary-Pancreatic Sciences.2023; 30(1): 144. CrossRef - A Systematic Review of Endoscopic Treatments for Concomitant Malignant Biliary Obstruction and Malignant Gastric Outlet Obstruction and the Outstanding Role of Endoscopic Ultrasound-Guided Therapies
Giacomo Emanuele Maria Rizzo, Lucio Carrozza, Dario Quintini, Dario Ligresti, Mario Traina, Ilaria Tarantino
Cancers.2023; 15(9): 2585. CrossRef - EUS-guided gallbladder drainage using a lumen-apposing metal stent as rescue treatment for malignant distal biliary obstruction: a large multicenter experience
Cecilia Binda, Andrea Anderloni, Alessandro Fugazza, Arnaldo Amato, Germana de Nucci, Alessandro Redaelli, Roberto Di Mitri, Luigi Cugia, Valeria Pollino, Raffaele Macchiarelli, Benedetto Mangiavillano, Edoardo Forti, Mario Luciano Brancaccio, Roberta Bad
Gastrointestinal Endoscopy.2023; 98(5): 765. CrossRef - Choledochoduodenostomy Versus Hepaticogastrostomy in Endoscopic Ultrasound-guided Drainage for Malignant Biliary Obstruction: A Meta-analysis and Systematic Review
Kejie Mao, Binbin Hu, Feng Sun, Kaiming Wan
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2022; 32(1): 124. CrossRef - Efficacy and safety of endoscopic duodenal stent versus endoscopic or surgical gastrojejunostomy to treat malignant gastric outlet obstruction: systematic review and meta-analysis
Rajesh Krishnamoorthi, Shivanand Bomman, Petros Benias, Richard A. Kozarek, Joyce A. Peetermans, Edmund McMullen, Ornela Gjata, Shayan S. Irani
Endoscopy International Open.2022; 10(06): E874. CrossRef
- Endoscopic Management of Malignant Biliary Obstruction
- 4,832 View
- 212 Download
- 5 Web of Science
- 6 Crossref

- Current Status of Endoscopic Gallbladder Drainage
- Joey Ho Yi Chan, Anthony Yuen Bun Teoh
- Clin Endosc 2018;51(2):150-155. Published online November 17, 2017
- DOI: https://doi.org/10.5946/ce.2017.125
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The gold standard for treatment of acute cholecystitis is laparoscopic cholecystectomy. However, cholecystectomy is often not suitable for surgically unfit patients who are too frail due to various co-morbidities. As such, several less invasive endoscopic treatment modalities have been developed to control sepsis, either as a definitive treatment or as a temporizing modality until the patient is stable enough to undergo cholecystectomy at a later stage. Recent developments in endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) with endoscopic ultrasound (EUS)-specific stents having lumen-apposing properties have demonstrated potential as a definitive treatment modality. Furthermore, advanced gallbladder procedures can be performed using the stents as a portal. With similar effectiveness as percutaneous transhepatic cholecystostomy and lower rates of adverse events reported in some studies, EUS-GBD has opened exciting possibilities in becoming the next best alternative in treating acute cholecystitis in surgically unfit patients. The aim of this review article is to provide a summary of the various methods of gallbladder drainage (GBD) with particular focus on EUS-GBD and the many new prospects it allows.
-
Citations
Citations to this article as recorded by- Acute cholecystitis management in high-risk, critically ill, and unfit-for-surgery patients: the Italian Society of Emergency Surgery and Trauma (SICUT) guidelines
Federico Coccolini, Eugenio Cucinotta, Andrea Mingoli, Mauro Zago, Gaia Altieri, Alan Biloslavo, Roberto Caronna, Ismail Cengeli, Enrico Cicuttin, Roberto Cirocchi, Luigi Cobuccio, Gianluca Costa, Valerio Cozza, Camilla Cremonini, Giovanni Del Vecchio, Gi
Updates in Surgery.2024; 76(2): 331. CrossRef - Lumen-apposing-metal stent misdeployment in endoscopic ultrasound-guided drainages: A systematic review focusing on issues and rescue management
Elia Armellini, Flavio Metelli, Andrea Anderloni, Anna Cominardi, Giovanni Aragona, Michele Marini, Fabio Pace
World Journal of Gastroenterology.2023; 29(21): 3341. CrossRef - Nonsurgical Gallbladder Drainage: Percutaneous and Endoscopic Approaches
Gregory Toy, Douglas G. Adler
Techniques and Innovations in Gastrointestinal Endoscopy.2022; 24(1): 90. CrossRef - Current status of endoscopic management of cholecystitis
Se Woo Park, Sang Soo Lee
Digestive Endoscopy.2022; 34(3): 439. CrossRef - Lumen Apposition: A Changing Landscape in Therapeutic Endoscopy
Thomas R. McCarty, Christopher C. Thompson
Digestive Diseases and Sciences.2022; 67(5): 1660. CrossRef - EUS-guided drainage of the gallbladder using a novel 0.018-inch guidewire for preventing bile leakage (with video)
Mamoru Takenaka, Shunsuke Omoto, Masatoshi Kudo
Endoscopic Ultrasound.2022; 11(6): 520. CrossRef - Endoscopic Ultrasound-Guided Gallbladder Drainage
Zain A. Sobani, Christina Ling, Tarun Rustagi
Digestive Diseases and Sciences.2021; 66(7): 2154. CrossRef - Endoscopic gallbladder drainage for symptomatic gallbladder disease: a cumulative systematic review meta-analysis
Thomas R. McCarty, Kelly E. Hathorn, Ahmad Najdat Bazarbashi, Kunal Jajoo, Marvin Ryou, Christopher C. Thompson
Surgical Endoscopy.2021; 35(9): 4964. CrossRef - Acute biliary interventions
T.C. See
Clinical Radiology.2020; 75(5): 398.e9. CrossRef - Safety and efficacy of endoscopic ultrasound‐guided gallbladder drainage combined with endoscopic retrograde cholangiopancreatography in the same session
Raul Torres Yuste, Francisco Javier Garcia‐Alonso, Ramón Sanchez‐Ocana, Marta Cimavilla Roman, Irene Peñas Herrero, Ana Yaiza Carbajo, Marina De Benito Sanz, Natalia Mora Cuadrado, Carlos De la Serna Higuera, Manuel Perez‐Miranda
Digestive Endoscopy.2020; 32(4): 608. CrossRef - Endoscopic ultrasonography-guided gallbladder drainage using lumen-apposing metal stents
Rajesh Krishnamoorthi, Shayan Irani
Techniques and Innovations in Gastrointestinal Endoscopy.2020; 22(1): 19. CrossRef - A Rare Fatal Bile Peritonitis after Malposition of Endoscopic Ultrasound-Guided 5-Fr Naso-Gallbladder Drainage
Tae Hyung Kim, Hyun Jin Bae, Seung Goun Hong
Clinical Endoscopy.2020; 53(1): 97. CrossRef - EUS-guided versus endoscopic transpapillary gallbladder drainage in high-risk surgical patients with acute cholecystitis: a systematic review and meta-analysis
Rajesh Krishnamoorthi, Mahendran Jayaraj, Viveksandeep Thoguluva Chandrasekar, Dhruv Singh, Joanna Law, Michael Larsen, Andrew Ross, Richard Kozarek, Shayan Irani
Surgical Endoscopy.2020; 34(5): 1904. CrossRef - Recent development of endoscopic ultrasound-guided gallbladder drainage
Brian Kin Hang Lam, Anthony Yuen Bun Teoh
International Journal of Gastrointestinal Intervention.2020; 9(4): 148. CrossRef - 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis
Michele Pisano, Niccolò Allievi, Kurinchi Gurusamy, Giuseppe Borzellino, Stefania Cimbanassi, Djamila Boerna, Federico Coccolini, Andrea Tufo, Marcello Di Martino, Jeffrey Leung, Massimo Sartelli, Marco Ceresoli, Ronald V. Maier, Elia Poiasina, Nicola De
World Journal of Emergency Surgery.2020;[Epub] CrossRef - A Guidewire May Save the Day
Rajat Garg, Mohammed Barawi
The Korean Journal of Gastroenterology.2018; 72(2): 83. CrossRef
- Acute cholecystitis management in high-risk, critically ill, and unfit-for-surgery patients: the Italian Society of Emergency Surgery and Trauma (SICUT) guidelines
- 7,952 View
- 335 Download
- 18 Web of Science
- 16 Crossref

- Linear Array Endoscopic Ultrasonography
- Eun Young Kim, M.D.
- Korean J Gastrointest Endosc 2009;38(1):1-8. Published online January 30, 2009
-
 Abstract
Abstract
 PDF
PDF - Endoscopic ultrasonography (EUS) was first developed to observe the pancreas more clearly without interference from the air and the abdominal wall. EUS is currently being used as an important diagnostic and therapeutic tool for various gastrointestinal diseases. Until recently, a radial echoendoscope with a vertical scanning plane has been mainly used, but a linear echoendoscope (linear EUS) with a parallel scanning plane has been recently developed. With the introduction of linear EUS, it is possible to perform many interventional procedures, including fine needle aspiration, and the field of EUS has been greatly expanded. This article briefly reviews the accepted procedures and the new trials using linear EUS. (Korean J Gastrointest Endosc 2009;38:1-8)
- 1,902 View
- 10 Download


 KSGE
KSGE


 First
First Prev
Prev



