Search
- Page Path
- HOME > Search
- Surveillance for metachronous cancers after endoscopic resection of esophageal squamous cell carcinoma
- Ryu Ishihara
- Received October 10, 2023 Accepted December 17, 2023 Published online May 10, 2024
- DOI: https://doi.org/10.5946/ce.2023.263 [Epub ahead of print]

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The literature pertaining to surveillance following treatment for esophageal squamous cell carcinoma (SCC) was reviewed and summarized, encompassing the current status and future perspectives. Analysis of the standardized mortality and incidence ratios for these cancers indicates an elevated risk of cancer in the oral cavity, pharynx, larynx, and lungs among patients with esophageal SCC compared to the general population. To enhance the efficacy of surveillance for these metachronous cancers, risk stratification is needed. Various factors, including multiple Lugol-voiding lesions, multiple foci of dilated vascular areas, young age, and high mean corpuscular volume, have been identified as predictors of metachronous SCCs. Current practice involves stratifying the risk of metachronous esophageal and head/neck SCCs based on the presence of multiple Lugol-voiding lesions. Endoscopic surveillance, scheduled 6–12 months post-endoscopic resection, has demonstrated effectiveness, with over 90% of metachronous esophageal SCCs treatable through minimally invasive modalities. Narrow-band imaging emerges as the preferred surveillance method for esophageal and head/neck SCC based on comparative studies of various imaging techniques. Innovative approaches, such as artificial intelligence-assisted detection systems and radiofrequency ablation of high-risk background mucosa, may improve outcomes in patients following endoscopic resection.
- 1,537 View
- 35 Download

- Recent advances in surveillance colonoscopy for dysplasia in inflammatory bowel disease
- Soo-Young Na, Won Moon
- Clin Endosc 2022;55(6):726-735. Published online November 18, 2022
- DOI: https://doi.org/10.5946/ce.2022.132

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Inflammatory bowel disease (IBD) has a global presence with rapidly increasing incidence and prevalence. Patients with IBD including those with ulcerative colitis and Crohn’s disease have a higher risk of developing colorectal cancer (CRC) compared to the general population. Risk factors for CRC in patients with IBD include long disease duration, extensive colitis, primary sclerosing cholangitis, family history of CRC, stricture, and prior dysplasia. Surveillance colonoscopy for CRC in patients with IBD should be tailored to individualized risk factors and requires careful monitoring every year to every five years. The current surveillance techniques are based on several guidelines. Chromoendoscopy with targeted biopsy is being recommended increasingly, and high-definition colonoscopy is gradually replacing standard-definition colonoscopy. However, it remains unclear whether chromoendoscopy, virtual chromoendoscopy, or white-light endoscopy has better efficiency when a high-definition scope is used. With the development of new endoscopic instruments and techniques, the paradigm of surveillance strategy has gradually changed. In this review, we discuss cutting-edge surveillance colonoscopy in patients with IBD including a review of literature.
-
Citations
Citations to this article as recorded by- Inflammatory bowel disease and primary sclerosing cholangitis: One disease or two?
Kim N. van Munster, Annika Bergquist, Cyriel Y. Ponsioen
Journal of Hepatology.2024; 80(1): 155. CrossRef - Extrachromosomal Circular DNA: An Emerging Potential Biomarker for Inflammatory Bowel Diseases?
Valentina Petito, Federica Di Vincenzo, Lorenza Putignani, Maria T. Abreu, Birgitte Regenberg, Antonio Gasbarrini, Franco Scaldaferri
Genes.2024; 15(4): 414. CrossRef - A Review of Colonoscopy in Intestinal Diseases
Seung Hong, Dong Baek
Diagnostics.2023; 13(7): 1262. CrossRef - Potential Oral Microbial Markers for Differential Diagnosis of Crohn’s Disease and Ulcerative Colitis Using Machine Learning Models
Sang-Bum Kang, Hyeonwoo Kim, Sangsoo Kim, Jiwon Kim, Soo-Kyung Park, Chil-Woo Lee, Kyeong Ok Kim, Geom-Seog Seo, Min Suk Kim, Jae Myung Cha, Ja Seol Koo, Dong-Il Park
Microorganisms.2023; 11(7): 1665. CrossRef - Update on Endoscopic Dysplasia Surveillance in Inflammatory Bowel Disease
Nayantara Coelho-Prabhu, James D. Lewis
American Journal of Gastroenterology.2023; 118(10): 1748. CrossRef
- Inflammatory bowel disease and primary sclerosing cholangitis: One disease or two?
- 2,919 View
- 206 Download
- 5 Web of Science
- 5 Crossref

- Korean guidelines for postpolypectomy colonoscopic surveillance: 2022 revised edition
- Su Young Kim, Min Seob Kwak, Soon Man Yoon, Yunho Jung, Jong Wook Kim, Sun-Jin Boo, Eun Hye Oh, Seong Ran Jeon, Seung-Joo Nam, Seon-Young Park, Soo-Kyung Park, Jaeyoung Chun, Dong Hoon Baek, Mi-Young Choi, Suyeon Park, Jeong-Sik Byeon, Hyung Kil Kim, Joo Young Cho, Moon Sung Lee, Oh Young Lee, Korean Society of Gastrointestinal Endoscopy, Korean Society of Gastroenterology, Korean Association for the Study of Intestinal Diseases
- Clin Endosc 2022;55(6):703-725. Published online October 13, 2022
- DOI: https://doi.org/10.5946/ce.2022.136
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
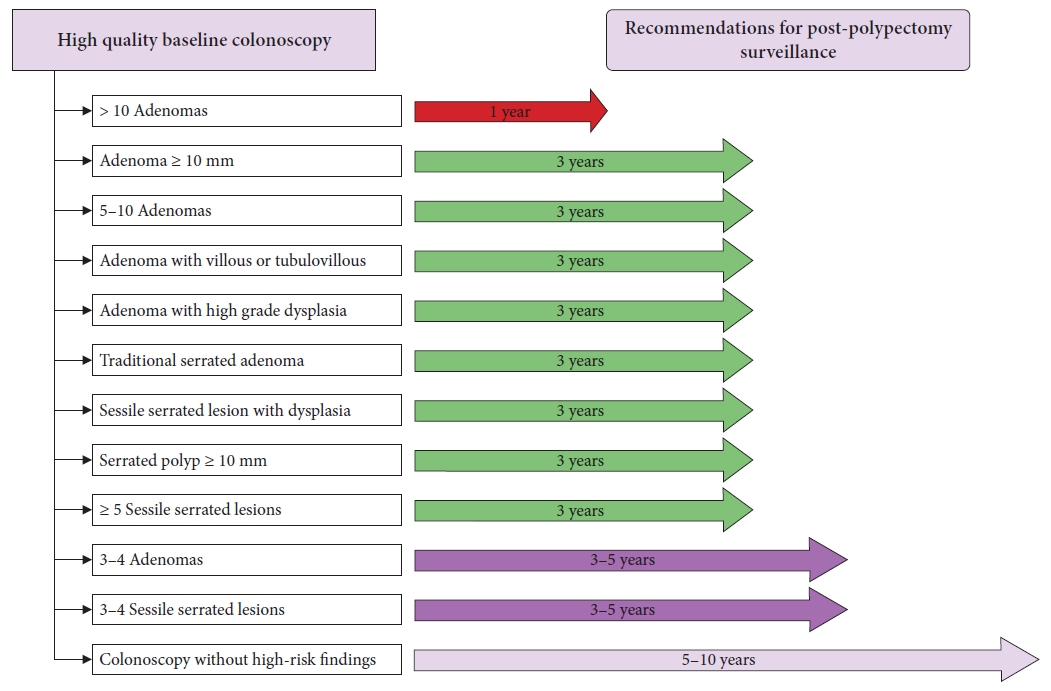
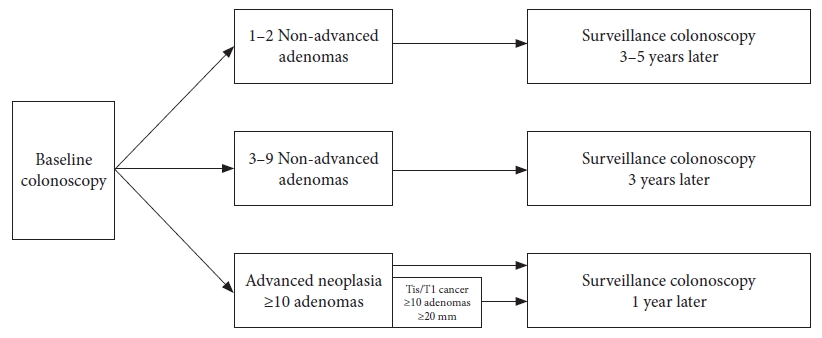
ePub - Colonoscopic polypectomy is effective in decreasing the incidence and mortality of colorectal cancer (CRC). Premalignant polyps discovered during colonoscopy are associated with the risk of metachronous advanced neoplasia. Postpolypectomy surveillance is the most important method for the management of advanced metachronous neoplasia. A more efficient and evidence-based guideline for postpolypectomy surveillance is required because of limited medical resources and concerns regarding colonoscopy complications. In these consensus guidelines, an analytic approach was used to address all reliable evidence to interpret the predictors of CRC or advanced neoplasia during surveillance colonoscopy. The key recommendations state that the high-risk findings for metachronous CRC following polypectomy are as follows: (1) adenoma ≥10 mm in size; (2) 3 to 5 (or more) adenomas; (3) tubulovillous or villous adenoma; (4) adenoma containing high-grade dysplasia; (5) traditional serrated adenoma; (6) sessile serrated lesion (SSL) containing any grade of dysplasia; (7) serrated polyp of at least 10 mm in size; and (8) 3 to 5 (or more) SSLs. More studies are needed to fully comprehend the patients most likely to benefit from surveillance colonoscopy and the ideal surveillance interval to prevent metachronous CRC.
-
Citations
Citations to this article as recorded by- Association between Atherosclerosis and High-Risk Colorectal Adenomas based on Cardio-Ankle Vascular Index and Ankle-Brachial Index
Jung Ho Lee, Hyunseok Cho, Sang Hoon Lee, Sung Joon Lee, Chang Don Kang, Dae Hee Choi, Jin Myung Park, Seung-Joo Nam, Tae Suk Kim, Ji Hyun Kim, Sung Chul Park
The Korean Journal of Gastroenterology.2024; 83(4): 143. CrossRef - A survey of current practices in post-polypectomy surveillance in Korea
Jeongseok Kim, Tae-Geun Gweon, Min Seob Kwak, Su Young Kim, Seong Jung Kim, Hyun Gun Kim, Eun Ran Kim, Sung Noh Hong, Eun Sun Kim, Chang Mo Moon, Dae Seong Myung, Dong Hoon Baek, Shin Ju Oh, Hyun Jung Lee, Ji Young Lee, Yunho Jung, Jaeyoung Chun, Dong-Hoo
Intestinal Research.2024; 22(2): 186. CrossRef - Korean Guidelines for Postpolypectomy Colonoscopic Surveillance: 2022 Revision
Su Young Kim
The Korean Journal of Medicine.2023; 98(3): 102. CrossRef - Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Mizuki Nagai, Sho Suzuki, Yohei Minato, Fumiaki Ishibashi, Kentaro Mochida, Ken Ohata, Tetsuo Morishita
Clinical Endoscopy.2023; 56(5): 553. CrossRef - Understanding colorectal polyps to prevent colorectal cancer
Dong-Hoon Yang
Journal of the Korean Medical Association.2023; 66(11): 626. CrossRef - Classification and endoscopic diagnosis of colorectal polyps
Ji Hyun Kim, Sung Chul Park
Journal of the Korean Medical Association.2023; 66(11): 633. CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef - Strategy for post-polypectomy colonoscopy surveillance: focus on the revised Korean guidelines
Yong Soo Kwon, Su Young Kim
Journal of the Korean Medical Association.2023; 66(11): 652. CrossRef
- Association between Atherosclerosis and High-Risk Colorectal Adenomas based on Cardio-Ankle Vascular Index and Ankle-Brachial Index
- 5,241 View
- 515 Download
- 8 Web of Science
- 8 Crossref

- Post-polypectomy surveillance: the present and the future
- Masau Sekiguchi, Takahisa Matsuda, Kinichi Hotta, Yutaka Saito
- Clin Endosc 2022;55(4):489-495. Published online July 11, 2022
- DOI: https://doi.org/10.5946/ce.2022.097
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - An appropriate post-polypectomy surveillance program requires the effectiveness of reducing colorectal cancer and safety. In addition, the post-polypectomy surveillance program should consider the burden of limited medical resource capacity, cost-effectiveness, and patient adherence. In this sense, a risk-stratified surveillance program based on baseline colonoscopy results is ideal. Major international guidelines for post-polypectomy surveillance, such as those from the European Union and the United States, have recommended risk-stratified surveillance programs. Both guidelines have recently been updated to better differentiate between high- and low-risk individuals. In both updated guidelines, more individuals have been downgraded to lower-risk groups that require less frequent or no surveillance. Furthermore, increased attention has been paid to the surveillance of patients who undergo serrated polyp removal. Previous guidelines in Japan did not clearly outline the risk stratification in post-polypectomy surveillance. However, the new colonoscopy screening and surveillance guidelines presented by the Japan Gastroenterological Endoscopy Society include a risk-stratified post-polypectomy surveillance program. Further discussion and analysis of unresolved issues in this field, such as the optimal follow-up after the first surveillance, the upper age limit for surveillance, and the ideal method for improving adherence to surveillance guidelines, are warranted.
-
Citations
Citations to this article as recorded by- Protocolo diagnóstico del seguimiento de pólipos colónicos
S. Redondo Evangelista, M. Sierra Morales, I. Bartolomé Oterino, P. García Centeno, A. Santos Rodríguez
Medicine - Programa de Formación Médica Continuada Acreditado.2024; 14(4): 219. CrossRef - Metabolic‐associated fatty liver disease is associated with colorectal adenomas in young and older Korean adults
Jiwon Chang, Yoosoo Chang, Yoosun Cho, Hyun‐Suk Jung, Dong‐Il Park, Soo‐Kyung Park, Soo‐Youn Ham, Sarah H. Wild, Christopher D. Byrne, Seungho Ryu
Liver International.2023; 43(11): 2548. CrossRef - Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Mizuki Nagai, Sho Suzuki, Yohei Minato, Fumiaki Ishibashi, Kentaro Mochida, Ken Ohata, Tetsuo Morishita
Clinical Endoscopy.2023; 56(5): 553. CrossRef - Strategy for post-polypectomy colonoscopy surveillance: focus on the revised Korean guidelines
Yong Soo Kwon, Su Young Kim
Journal of the Korean Medical Association.2023; 66(11): 652. CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef - Understanding colorectal polyps to prevent colorectal cancer
Dong-Hoon Yang
Journal of the Korean Medical Association.2023; 66(11): 626. CrossRef
- Protocolo diagnóstico del seguimiento de pólipos colónicos
- 3,554 View
- 249 Download
- 5 Web of Science
- 6 Crossref

- Contamination Rates in Duodenoscopes Reprocessed Using Enhanced Surveillance and Reprocessing Techniques: A Systematic Review and Meta-Analysis
- Shivanand Bomman, Munish Ashat, Navroop Nagra, Mahendran Jayaraj, Shruti Chandra, Richard A Kozarek, Andrew Ross, Rajesh Krishnamoorthi
- Clin Endosc 2022;55(1):33-40. Published online January 3, 2022
- DOI: https://doi.org/10.5946/ce.2021.212
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
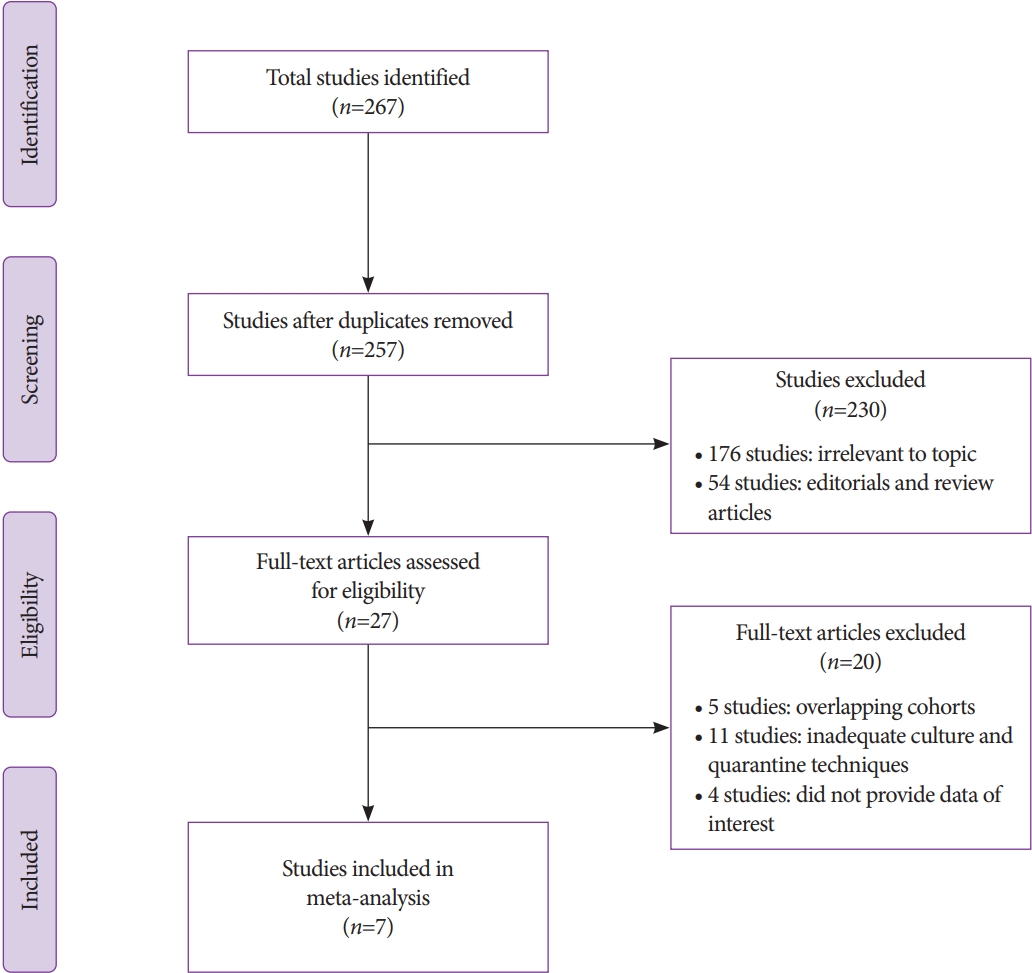
/Aims: Multiple outbreaks of multidrug-resistant organisms have been reported worldwide due to contaminated duodenoscopes. In 2015, the United States Food and Drug Administration recommended the following supplemental enhanced surveillance and reprocessing techniques (ESRT) to improve duodenoscope disinfection: (1) microbiological culture, (2) ethylene oxide sterilization, (3) liquid chemical sterilant processing system, and (4) double high-level disinfection. A systematic review and meta-analysis was performed to assess the impact of ESRT on the contamination rates.
Methods
A thorough and systematic search was performed across several databases and conference proceedings from inception until January 2021, and all studies reporting the effectiveness of various ESRTs were identified. The pooled contamination rates of post-ESRT duodenoscopes were estimated using the random effects model.
Results
A total of seven studies using various ESRTs were incorporated in the analysis, which included a total of 9,084 post-ESRT duodenoscope cultures. The pooled contamination rate of the post-ESRT duodenoscope was 5% (95% confidence interval [CI]: 2.3%–10.8%, inconsistency index [I2]=97.97%). Pooled contamination rates for high-risk organisms were 0.8% (95% CI: 0.2%–2.7%, I2=94.96).
Conclusions
While ESRT may improve the disinfection process, a post-ESRT contamination rate of 5% is not negligible. Ongoing efforts to mitigate the rate of contamination by improving disinfection techniques and innovations in duodenoscope design to improve safety are warranted. -
Citations
Citations to this article as recorded by- Recommendations and guidelines for endoscope reprocessing: Current position statement of digestive endoscopic society of Taiwan
Wei-Kuo Chang, Chen-Ling Peng, Yen-Wei Chen, Cheuk-Kay Sun, Chieh-Chang Chen, Tao-Chieh Liu, Yin-Yi Chu, I-Fang Tsai, Chen-Shuan Chung, Hsiao-Fen Lin, Fang-Yu Hsu, Wei-Chen Tai, Hsi-Chang Lee, Hsu-Heng Yen, E-Ming Wang, Shu-Hui Chen, Cheng-Hsin Chu, Ming-
Journal of Microbiology, Immunology and Infection.2024; 57(2): 211. CrossRef - Duodenoscopes With Disposable Elevator Caps—An Incremental Reduction in Infection Risk for Patients
Melinda Wang, Graham M. Snyder
JAMA Internal Medicine.2023; 183(3): 200. CrossRef - Transmission of oral microbiota to the biliary tract during endoscopic retrograde cholangiography
Maria Effenberger, Ramona Al-Zoairy, Ronald Gstir, Ivo Graziadei, Hubert Schwaighofer, Herbert Tilg, Heinz Zoller
BMC Gastroenterology.2023;[Epub] CrossRef - Role of peroral cholangioscopy and pancreatoscopy in the diagnosis and treatment of biliary and pancreatic disease: past, present, and future
Harishankar Gopakumar, Neil R. Sharma
Frontiers in Gastroenterology.2023;[Epub] CrossRef - Performance of single-use duodenoscopes for ERCP: a systematic review and meta-analysis
Harishankar Gopakumar, Ishaan Vohra, Neil R. Sharma, Srinivas R. Puli
iGIE.2022; 1(1): 77. CrossRef
- Recommendations and guidelines for endoscope reprocessing: Current position statement of digestive endoscopic society of Taiwan
- 3,829 View
- 221 Download
- 4 Web of Science
- 5 Crossref

- Assessment of Endoscopic Gastric Atrophy according to the Kimura-Takemoto Classification and Its Potential Application in Daily Practice
- Duc Trong Quach, Toru Hiyama
- Clin Endosc 2019;52(4):321-327. Published online July 22, 2019
- DOI: https://doi.org/10.5946/ce.2019.072

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The assessment of endoscopic gastric atrophy (EGA) according to the Kimura-Takemoto classification has been reported to correlate well with histological assessment. Although agreement among beginner endoscopists was less than that among experienced endoscopists, it has been shown that agreement level could markedly improve and remained stable after proper training. Several cohort studies have consistently shown that the severity of EGA at baseline is significantly associated with the presence of advanced precancerous gastric lesions and gastric cancer, as well as the development of gastric cancer in future. Patients with moderate-to-severe EGA still have high risk of gastric cancer even after successful Helicobacter pylori eradication and should be candidates for gastric cancer surveillance. The assessment of EGA, therefore, could be used as a preliminary tool to identify individuals at high risk for gastric cancer. In this paper, we review the agreement on mucosal atrophy assessment between the Kimura-Takemoto classification and histology as well as the potential application of this endoscopic classification to identify precancerous gastric lesions and gastric cancer in daily practice.
-
Citations
Citations to this article as recorded by- Endoscopic diagnosis and prevalence of early gastric cancer in India: A prospective study
Ashutosh Mohapatra, Sonmoon Mohapatra, Shruti Mahawar, Krushna Chandra Pani, Nachiketa Mohapatra, Mohan Ramchandani, Nageshwar Reddy, Mahesh K. Goenka, Noriya Uedo
DEN Open.2024;[Epub] CrossRef - Clinical and morphological characteristics of patients with chronic gastritis and high risk of gastric cancer
A. S. Tertychnyy, D. D. Protsenko, N. V. Pachuashvili, D. P. Nagornaya, P. V. Pavlov, A. P. Kiruhin, A. A. Fedorenko
Experimental and Clinical Gastroenterology.2024; (9): 107. CrossRef - Comparison between the GastroPanel test and the serum pepsinogen assay interpreted with the ABC method—A prospective study
Sun‐Young Lee, Yeon‐Sun Ahn, Hee‐Won Moon
Helicobacter.2024;[Epub] CrossRef - The value of LCI-based modified Kyoto classification risk scoring system in predicting the risk of early gastric cancer
Chao Gao, Guanpo Zhang, Jin Zheng, Yunmeng Zheng, Wulian Lin, Guilin Xu, Yixiang You, Dazhou Li, Wen Wang
Scandinavian Journal of Gastroenterology.2024; : 1. CrossRef - Identification of serum microRNAs as potential diagnostic biomarkers for detecting precancerous lesions of gastric cancer
Hajime Otsu, Sho Nambara, Qingjiang Hu, Yuichi Hisamatsu, Takeo Toshima, Kazuki Takeishi, Yusuke Yonemura, Takaaki Masuda, Eiji Oki, Koshi Mimori
Annals of Gastroenterological Surgery.2023; 7(1): 63. CrossRef - Evolution of the Correa's cascade steps: A long-term endoscopic surveillance among non-ulcer dyspepsia and gastric ulcer after H. pylori eradication
Hsiu-Chi Cheng, Yao-Jong Yang, Hsiao-Bai Yang, Yu-Ching Tsai, Wei-Lun Chang, Chung-Tai Wu, Hsin-Yu Kuo, Yu-Ting Yu, Er-Hsiang Yang, Wei-Chun Cheng, Wei-Ying Chen, Bor-Shyang Sheu
Journal of the Formosan Medical Association.2023; 122(5): 400. CrossRef - Vietnam Association of Gastroenterology (VNAGE) consensus on the management of Helicobacter pylori infection
Duc Trong Quach, Bang Hong Mai, Mien Kieu Tran, Long Van Dao, Huy Van Tran, Khanh Truong Vu, Khien Van Vu, Ho Thi-Thu Pham, Hoang Huu Bui, Dung Dang-Quy Ho, Dung Tuan Trinh, Vinh Thuy Nguyen, Thai Hong Duong, Tuong Thi-Khanh Tran, Ha Thi-Viet Nguyen, Thin
Frontiers in Medicine.2023;[Epub] CrossRef - Endoscopic Screening for Missed Lesions of Synchronous Multiple Early Gastric Cancer during Endoscopic Submucosal Dissection
Jiangnan Wan, Yi Fang, Haizhong Jiang, Bujiang Wang, Lei Xu, Chunjiu Hu, Honghui Chen, Xiaoyun Ding, Tatsuya Toyokawa
Gastroenterology Research and Practice.2023; 2023: 1. CrossRef - Morphometric features of gastric mucosa in atrophic gastritis: A different pattern between corpus and antrum
Xue-Mei Lin, Li Wang, Chun-Hui Xi, Jun Wang, Xian-Fei Wang, Qiong Wang, Cong Yuan
Medicine.2023; 102(14): e33480. CrossRef - Predicting reflux symptom recurrence: The impact of gastroesophageal junction indicators and body mass index among outpatients
Qing Wang, Junhui Lu, Yue Sui, Jing Fan, Jinnan Ren, Zhenzhen Wang, Xing Chen
Experimental and Therapeutic Medicine.2023;[Epub] CrossRef -
Helicobacter pylori intragastric colonization and migration: Endoscopic manifestations and potential mechanisms
Tong Mu, Zhi-Ming Lu, Wen-Wen Wang, Hua Feng, Yan Jin, Qian Ding, Li-Fen Wang
World Journal of Gastroenterology.2023; 29(30): 4616. CrossRef - Factors associated with heterochronic gastric cancer development post-endoscopic mucosal dissection in early gastric cancer patients
Bing Xie, Yun Xia, Xia Wang, Yan Xiong, Shao-Bo Chen, Jie Zhang, Wei-Wei He
World Journal of Gastrointestinal Oncology.2023; 15(9): 1644. CrossRef - Kimura–Takemoto Classification: A Tool to Predict Gastric Intestinal Metaplasia Progression to Advanced Gastric Neoplasia
Leyla Maric, Daniel Castaneda, Harjinder Singh, Pablo Bejarano, Brenda Jimenez Cantisano, Fernando J. Castro
Digestive Diseases and Sciences.2022; 67(8): 4092. CrossRef - Consistency between the endoscopic Kyoto classification and pathological updated Sydney system for gastritis: A cross‐sectional study
Osamu Toyoshima, Toshihiro Nishizawa, Shuntaro Yoshida, Tatsuya Matsuno, Nariaki Odawara, Akira Toyoshima, Kosuke Sakitani, Hidenobu Watanabe, Mitsuhiro Fujishiro, Hidekazu Suzuki
Journal of Gastroenterology and Hepatology.2022; 37(2): 291. CrossRef - Diagnostic Accuracy of H. pylori Status by Conventional Endoscopy: Time-Trend Change After Eradication and Impact of Endoscopic Image Quality
Duc Trong Quach, Rika Aoki, Akiko Iga, Quang Dinh Le, Toru Kawamura, Ken Yamashita, Shinji Tanaka, Masaharu Yoshihara, Toru Hiyama
Frontiers in Medicine.2022;[Epub] CrossRef - Relevance of pepsinogen, gastrin, and endoscopic atrophy in the diagnosis of autoimmune gastritis
Hiroshi Kishikawa, Kenji Nakamura, Keisuke Ojiro, Tadashi Katayama, Kyoko Arahata, Sakiko Takarabe, Aya Sasaki, Soichiro Miura, Yukie Hayashi, Hitomi Hoshi, Takanori Kanai, Jiro Nishida
Scientific Reports.2022;[Epub] CrossRef - Tauroursodeoxycholic Acid Inhibits Nuclear Factor Kappa B Signaling in Gastric Epithelial Cells and Ameliorates Gastric Mucosal Damage in Mice
Su Hwan Kim, Ji Won Kim, Seong-Joon Koh, Sang Gyun Kim, Jeong Mo Bae, Jung Ho Kim, Jeong Hwan Park, Mee Soo Chang, Kee Don Choi, Hyoun Woo Kang, Byeong Gwan Kim, Kook Lae Lee
The Korean Journal of Gastroenterology.2022; 79(4): 161. CrossRef - Serum pepsinogen: A potential non-invasive screening method for moderate and severe atrophic gastritis among an asian population
Cong Long Nguyen, Tran Tien Dao, Thi-Thuy Ngan Phi, The Phuong Nguyen, Van Tuyen Pham, Truong Khanh Vu
Annals of Medicine and Surgery.2022; 78: 103844. CrossRef - Risk factors for early gastric cancer: focus on Helicobacter pylori gastritis
Hee Seok Moon
Journal of the Korean Medical Association.2022; 65(5): 259. CrossRef - Current status of the gastric cancer screening program in Korea
Young-Il Kim, Il Ju Choi
Journal of the Korean Medical Association.2022; 65(5): 250. CrossRef - Endoscopic diagnosis of early gastric cancer
Dong Chan Joo, Gwang Ha Kim
Journal of the Korean Medical Association.2022; 65(5): 267. CrossRef - Current Evidence for a Paradigm Shift in Gastric Cancer Prevention From Endoscopic Screening toHelicobacter pyloriEradication in Korea
Young-Il Kim, Il Ju Choi
Journal of Gastric Cancer.2022; 22(3): 169. CrossRef - Need for improvement in the evaluation of pre‐malignant upper gastro‐intestinal lesions in India: Results of a nationwide survey
Deepak Madhu, Veeraraghavan Krishnamurthy, Thirumoorthi Natarajan, Sundeep Lakhtakia
Journal of Gastroenterology and Hepatology.2022; 37(11): 2113. CrossRef - Usefulness of the Kyoto Classification Score for Prediction of Current Helicobacter pylori Infection
Heejun Kang, Chul-Hyun Lim, Sukil Kim, Arum Choi, Jung-Hwan Oh
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2022; 22(4): 281. CrossRef - The simplified Kyoto classification score is consistent with the ABC method of classification as a grading system for endoscopic gastritis
Toshihiro Nishizawa, Osamu Toyoshima, Ryo Kondo, Kazuma Sekiba, Yosuke Tsuji, Hirotoshi Ebinuma, Hidekazu Suzuki, Chizu Tanikawa, Koichi Matsuda, Kazuhiko Koike
Journal of Clinical Biochemistry and Nutrition.2021; 68(1): 101. CrossRef - Endoscopic grading of gastric atrophy on risk assessment of gastric neoplasia: A systematic review and meta‐analysis
Shiyu Xiao, Yihan Fan, Zhihao Yin, Liya Zhou
Journal of Gastroenterology and Hepatology.2021; 36(1): 55. CrossRef - Gastritis: The clinico-pathological spectrum
Massimo Rugge, Edoardo Savarino, Marta Sbaraglia, Ludovica Bricca, Peter Malfertheiner
Digestive and Liver Disease.2021; 53(10): 1237. CrossRef - Efficacy of Seven-Day Potassium-Competitive Acid Blocker-Based First-LineHelicobacter PyloriEradication Therapy Administered with Bismuth
Ji Yeon Kim, Sun-Young Lee, Hyobin Kim, Jeong Hwan Kim, In-Kyung Sung, Hyung Seok Park
Yonsei Medical Journal.2021; 62(8): 708. CrossRef - Second-Line Bismuth-Containing Quadruple Therapy for Helicobacterpylori Infection: A 12-Year Study of Annual Eradication Rates
Kiwon Shin, Min-Jae Cho, Jung-Hwan Oh, Chul-Hyun Lim
Journal of Clinical Medicine.2021; 10(15): 3273. CrossRef - Predictive Significance of Promoter DNA Methylation of Cysteine Dioxygenase Type 1 (CDO1) in Metachronous Gastric Cancer
Yo Kubota, Satoshi Tanabe, Mizutomo Azuma, Kazue Horio, Yoshiki Fujiyama, Takafumi Soeno, Yasuaki Furue, Takuya Wada, Akinori Watanabe, Kenji Ishido, Chikatoshi Katada, Keishi Yamashita, Wasaburo Koizumi, Chika Kusano
Journal of Gastric Cancer.2021; 21(4): 379. CrossRef - Gastrointestinal Microbiota Changes in Patients With Gastric Precancerous Lesions
Dehua Liu, Si Chen, Yawen Gou, Wenyong Yu, Hangcheng Zhou, Rutong Zhang, Jinghao Wang, Fei Ye, Yingling Liu, Baolin Sun, Kaiguang Zhang
Frontiers in Cellular and Infection Microbiology.2021;[Epub] CrossRef - Use of endoscopic assessment of gastric atrophy for gastric cancer risk stratification to reduce the need for gastric mapping
Duc Trong Quach, Toru Hiyama, Huy Minh Le, Trung Sao Nguyen, Takuji Gotoda
Scandinavian Journal of Gastroenterology.2020; 55(4): 402. CrossRef - Influence of hypergastrinemia secondary to long-term proton pump inhibitor treatment on ECL cell tumorigenesis in human gastric mucosa
Atsushi Tatsuguchi, Shintaro Hoshino, Noriyuki Kawami, Katya Gudis, Tsutomu Nomura, Akira Shimizu, Katsuhiko Iwakiri
Pathology - Research and Practice.2020; 216(10): 153113. CrossRef - Chronic atrophic gastritis detection with a convolutional neural network considering stomach regions
Misaki Kanai, Ren Togo, Takahiro Ogawa, Miki Haseyama
World Journal of Gastroenterology.2020; 26(25): 3650. CrossRef - Naiv Helicobacter pylori pozitif ve negatif hastaların klinik, demografik ve endoskopik karakteristikleri: Retrospektif analiz
Muhammet AYDIN
Endoskopi Gastrointestinal.2020; 28(2): 39. CrossRef - Gastrointestinal Microbiota Changes in Patients With Gastric Precancerous Lesions
Dehua Liu, Si Chen, Yawen Gou, Wenyong Yu, Hangcheng Zhou, Rutong Zhang, Jinghao Wang, Fei Ye, Yingling Liu, Baolin Sun, Kaiguang Zhang
SSRN Electronic Journal .2020;[Epub] CrossRef
- Endoscopic diagnosis and prevalence of early gastric cancer in India: A prospective study
- 10,729 View
- 465 Download
- 34 Web of Science
- 36 Crossref

- Metachronous Gastric Cancer Following Curative Endoscopic Resection of Early Gastric Cancer
- Seiichiro Abe, Ichiro Oda, Takeyoshi Minagawa, Masau Sekiguchi, Satoru Nonaka, Haruhisa Suzuki, Shigetaka Yoshinaga, Amit Bhatt, Yutaka Saito
- Clin Endosc 2018;51(3):253-259. Published online September 18, 2017
- DOI: https://doi.org/10.5946/ce.2017.104
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - This review article summarizes knowledge about metachronous gastric cancer (MGC) occurring after curative endoscopic resection (ER) of early gastric cancer (EGC), treatment outcomes of patients who developed MGC, and efficacy of Helicobacter pylori eradication to prevent MGC. The incidence of MGC following curative ER increases over time and is higher than in patients undergoing gastrectomy. Increasing age and multifocal EGC are independent risk factors for developing MGC. An MGC following curative ER is usually a small (<20 mm) and differentiated intramucosal cancer. Most MGC lesions are found at an early stage on semiannual or annual surveillance endoscopy and are successfully treated by further ER, with excellent long-term outcomes. Eradication of H. pylori may reduce the risk of MGC following ER of EGC, but further prospective studies with long-term outcomes are required. Surveillance endoscopy following gastric ER should be continued indefinitely, due to the risk of MGC even after successful H. pylori eradication. Risk stratification and tailored endoscopic surveillance schedules need to be developed.
-
Citations
Citations to this article as recorded by- Impact of endoscopy intervals on metachronous gastric cancer after endoscopic submucosal dissection: Comparison between 1 year and half‐a‐year
Yuichiro Ozeki, Kingo Hirasawa, Atsushi Sawada, Ryosuke Ikeda, Masafumi Nishio, Takehide Fukuchi, Ryosuke Kobayashi, Chiko Sato, Shin Maeda
Digestive Endoscopy.2024; 36(3): 332. CrossRef - High risk of multiple gastric cancers in Japanese individuals with Lynch syndrome
Nobuhiko Kanaya, Thijs A. van Schaik, Hideki Aoki, Yumiko Sato, Fumitaka Taniguchi, Kunitoshi Shigeyasu, Kokichi Sugano, Kiwamu Akagi, Hideyuki Ishida, Kohji Tanakaya
Annals of Gastroenterological Surgery.2024;[Epub] CrossRef - Risk assessment of metachronous gastric cancer development using OLGA and OLGIM systems after endoscopic submucosal dissection for early gastric cancer: a long-term follow-up study
Yun Suk Na, Sang Gyun Kim, Soo-Jeong Cho
Gastric Cancer.2023; 26(2): 298. CrossRef - Metachronous lesions after gastric endoscopic submucosal dissection: first assessment of the FAMISH prediction score
Andreia Rei, Raquel Ortigão, Mariana Pais, Luís P. Afonso, Pedro Pimentel-Nunes, Mário Dinis-Ribeiro, Diogo Libânio
Endoscopy.2023; 55(10): 909. CrossRef - Variation in the rate of detection of minute and small early gastric cancers at diagnostic endoscopy may reflect the performance of individual endoscopists
Daisuke Murakami, Masayuki Yamato, Yuji Amano, Takayoshi Nishino, Makoto Arai
BMJ Open Gastroenterology.2023; 10(1): e001143. CrossRef - Decision to perform additional surgery after non-curative endoscopic submucosal dissection for gastric cancer based on the risk of lymph node metastasis: a long-term follow-up study
Seunghan Lee, Sang Gyun Kim, Soo-Jeong Cho
Surgical Endoscopy.2023; 37(10): 7738. CrossRef - Helicobacter pylori Eradication Can Reverse Rho GTPase Expression in Gastric Carcinogenesis
Jue Lie Kim, Sang Gyun Kim, Enerelt Natsagdorj, Hyunsoo Chung, Soo-Jeong Cho
Gut and Liver.2023; 17(5): 741. CrossRef - Risk assessment of metachronous gastric cancer after endoscopic submucosal dissection based on endoscopic intestinal metaplasia
Chino Iizuka, Soichiro Sue, Sho Onodera, Aya Ikeda, Ryosuke Ikeda, Yoshihiro Goda, Kuniyasu Irie, Hiroaki Kaneko, Shin Maeda
JGH Open.2023; 7(11): 783. CrossRef - Second gastric cancer after curative endoscopic resection of differentiated-type early gastric cancer: post-hoc analysis of a single-arm confirmatory trial
Masao Yoshida, Kohei Takizawa, Noriaki Hasuike, Hiroyuki Ono, Narikazu Boku, Tomohiro Kadota, Junki Mizusawa, Ichiro Oda, Naohiro Yoshida, Yusuke Horiuchi, Kingo Hirasawa, Yoshinori Morita, Yoshinobu Yamamoto, Manabu Muto, Masao Yoshida, Kohei Takizawa, H
Gastrointestinal Endoscopy.2022; 95(4): 650. CrossRef - Therapeutic approach to non-curative resection after endoscopic treatment in early gastric cancer
Eun Jeong Gong, Chang Seok Bang
Journal of the Korean Medical Association.2022; 65(5): 284. CrossRef - Assessment of Outcomes From 1-Year Surveillance After Detection of Early Gastric Cancer Among Patients at High Risk in Japan
Yoshinobu Yamamoto, Naohiro Yoshida, Tomonori Yano, Takahiro Horimatsu, Noriya Uedo, Noboru Kawata, Hiromitsu Kanzaki, Shinichiro Hori, Kenshi Yao, Seiichiro Abe, Chikatoshi Katada, Chizu Yokoi, Ken Ohata, Hisashi Doyama, Kenichi Yoshimura, Hideki Ishikaw
JAMA Network Open.2022; 5(8): e2227667. CrossRef - Management of patients with multiple primary сancer in the practice of a modern oncologist. Case report and literature review
D. A. Khlanta, G. P. Gens
Siberian journal of oncology.2022; 21(4): 147. CrossRef - Assigning a different endoscopist for each annual follow-up may contribute to improved gastric cancer detection rates
Shuhei Unno, Kimihiro Igarashi, Hiroaki Saito, Dai Hirasawa, Toru Okuzono, Yukari Tanaka, Masato Nakahori, Tomoki Matsuda
Endoscopy International Open.2022; 10(10): E1333. CrossRef - Statistical proof of Helicobacter pylori eradication in preventing metachronous gastric cancer after endoscopic resection in an East Asian population
Mohsen Karbalaei, Masoud Keikha
World Journal of Gastrointestinal Surgery.2022; 14(8): 867. CrossRef - Follow-up after endoscopic resection for early gastric cancer in 3 French referral centers
Bernadette de Rauglaudre, Mathieu Pioche, Fabrice Caillol, Jean-Philippe Ratone, Anna Pellat, Romain Coriat, Jerôme Rivory, Thomas Lambin, Laetitia Dahan, Marc Giovanini, Maximilien Barret
iGIE.2022; 1(1): 49. CrossRef - Documento de posicionamiento de la AEG, la SEED y la SEAP sobre cribado de cáncer gástrico en poblaciones con baja incidencia
Joaquín Cubiella, Ángeles Pérez Aisa, Miriam Cuatrecasas, Pilar Díez Redondo, Gloria Fernández Esparrach, José Carlos Marín-Gabriel, Leticia Moreira, Henar Núñez, M. Luisa Pardo López, Enrique Rodríguez de Santiago, Pedro Rosón, José Miguel Sanz Anquela,
Gastroenterología y Hepatología.2021; 44(1): 67. CrossRef - Incidence of metachronous cancer after endoscopic submucosal dissection: a comparison between undifferentiated-type and differentiated-type early gastric cancer
Mitsuaki Ishioka, Toshiyuki Yoshio, Yuji Miyamoto, Ken Namikawa, Yoshitaka Tokai, Shoichi Yoshimizu, Yusuke Horiuchi, Akiyoshi Ishiyama, Toshiaki Hirasawa, Tomohiro Tsuchida, Junko Fujisaki
Gastrointestinal Endoscopy.2021; 93(3): 557. CrossRef - Gastric cancer screening in low incidence populations: Position statement of AEG, SEED and SEAP
Joaquin Cubiella, Ángeles Pérez Aisa, Miriam Cuatrecasas, Pilar Díez Redondo, Gloria Fernández Esparrach, José Carlos Marín-Gabriel, Leticia Moreira, Henar Núñez, M. Luisa Pardo López, Enrique Rodríguez de Santiago, Pedro Rosón, José Miguel Sanz Anquela,
Gastroenterología y Hepatología (English Edition).2021; 44(1): 67. CrossRef - Molecular risk markers related to local tumor recurrence at histological margin-free endoscopically resected early gastric cancers: A pilot study
Ho Suk Kang, Mi Jung Kwon, Premi Haynes, Yan Liang, Yuqi Ren, Hyun Lim, Jae Seung Soh, Nan Young Kim, Hye Kyung Lee
Pathology - Research and Practice.2021; 222: 153434. CrossRef - Characteristics of metachronous gastric neoplasms after curative endoscopic submucosal dissection for early gastric neoplasms
Shan-Shan Xu, Ning-Li Chai, Xiao-Wei Tang, En-Qiang Linghu, Sha-Sha Wang, Bao Li
Chinese Medical Journal.2021; 134(21): 2603. CrossRef - Consenso mexicano sobre detección y tratamiento del cáncer gástrico incipiente
M.E. Icaza-Chávez, M.A. Tanimoto, F.M. Huerta-Iga, J.M. Remes-Troche, R. Carmona-Sánchez, A. Ángeles-Ángeles, F.J. Bosques-Padilla, J.M. Blancas-Valencia, G. Grajales-Figueroa, O.V. Hernández-Mondragón, A.I. Hernández-Guerrero, M.A. Herrera-Servín, F.D. H
Revista de Gastroenterología de México.2020; 85(1): 69. CrossRef - The Mexican consensus on the detection and treatment of early gastric cancer
M.E. Icaza-Chávez, M.A. Tanimoto, F.M. Huerta-Iga, J.M. Remes-Troche, R. Carmona-Sánchez, A. Ángeles-Ángeles, F.J. Bosques-Padilla, J.M. Blancas-Valencia, G. Grajales-Figueroa, O.V. Hernández-Mondragón, A.I. Hernández-Guerrero, M.Á. Herrera-Servín, F.D. H
Revista de Gastroenterología de México (English Edition).2020; 85(1): 69. CrossRef - Long‐term follow up of serum pepsinogens in patients with gastric cancer or dysplasia after Helicobacter pylori eradication
Gitark Noh, Nayoung Kim, Yonghoon Choi, Hye Seung Lee, Young Jae Hwang, Hee Jin Kim, Hyuk Yoon, Cheol Min Shin, Young Soo Park, Dong Ho Lee
Journal of Gastroenterology and Hepatology.2020; 35(9): 1540. CrossRef - Metachronous Gastric Cancer: Another Hurdle for Successful Endoscopic Treatment for Early Gastric Cancer?
Moon Won Lee, Gwang Ha Kim
Gut and Liver.2020; 14(2): 145. CrossRef - Clinical Outcomes of Metachronous Gastric Cancer after Endoscopic Resection for Early Gastric Cancer
Jue Lie Kim, Sang Gyun Kim, Jung Kim, Jae Yong Park, Hyo-Joon Yang, Hyun Ju Kim, Hyunsoo Chung
Gut and Liver.2020; 14(2): 190. CrossRef - Chemoprevention of gastric cancer development after Helicobacter pylori eradication therapy in an East Asian population: Meta-analysis
Mitsushige Sugimoto, Masaki Murata, Yoshio Yamaoka
World Journal of Gastroenterology.2020; 26(15): 1820. CrossRef - MULTIFOCAL EARLY GASTRIC CANCER IN A PATIENT WITH ATROPHIC GASTRITIS AND PERNICIOUS ANEMIA
Tommaso Zurleni, Michele Altomare, Giovanni Serio, Filippo Catalano
International Journal of Surgery Case Reports.2020;[Epub] CrossRef - Impact of the timing of Helicobacter pylori eradication on the risk of development of metachronous lesions after treatment of early gastric cancer: a population-based cohort study
Hyun Ju Kim, Yun Jin Kim, Seung In Seo, Woon Geon Shin, Chan Hyuk Park
Gastrointestinal Endoscopy.2020; 92(3): 613. CrossRef - Gastric cancer prevention strategies: A global perspective
Leonardo Henry Eusebi, Andrea Telese, Giovanni Marasco, Franco Bazzoli, Rocco Maurizio Zagari
Journal of Gastroenterology and Hepatology.2020; 35(9): 1495. CrossRef - Metachronous Gastric Cancer Occurring after Endoscopic Resection of Early Gastric Cancer
Gwang Ha Kim
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2020; 20(4): 295. CrossRef - Somatic alterations and mutational burden are potential predictive factors for metachronous development of early gastric cancer
Kazuhiro Sakuta, Yu Sasaki, Yasuhiko Abe, Hidenori Sato, Masakuni Shoji, Takao Yaoita, Makoto Yagi, Naoko Mizumoto, Yusuke Onozato, Takashi Kon, Ayumi Koseki, Sonoko Sato, Ryoko Murakami, Yuki Miyano, Yoshiyuki Ueno
Scientific Reports.2020;[Epub] CrossRef - Clinicopathologic Characteristics of Patients with Gastric Superficial Neoplasia and Risk Factors for Multiple Lesions after Endoscopic Submucosal Dissection in a Western Country
Gisela Brito-Gonçalves, Diogo Libânio, Pedro Marcos, Inês Pita, Rui Castro, Inês Sá, Mário Dinis-Ribeiro, Pedro Pimentel-Nunes
GE - Portuguese Journal of Gastroenterology.2020; 27(2): 76. CrossRef - Helicobacter pylori status and risks of metachronous recurrence after endoscopic resection of early gastric cancer: a systematic review and meta-analysis
Shiyu Xiao, Sizhu Li, Liya Zhou, Wenjun Jiang, Jinzhe Liu
Journal of Gastroenterology.2019; 54(3): 226. CrossRef - Helicobacter pylori Eradication for Metachronous Gastric Cancer: An Unsuitable Methodology Impeding Broader Clinical Usage
Alexios-Fotios A. Mentis, Efthimios Dardiotis
Frontiers in Oncology.2019;[Epub] CrossRef - Common Locations of Gastric Cancer: Review of Research from the Endoscopic Submucosal Dissection Era
Su Jin Kim, Cheol Woong Choi
Journal of Korean Medical Science.2019;[Epub] CrossRef - UEG Week 2019 Poster Presentations
United European Gastroenterology Journal.2019; 7(S8): 189. CrossRef - Helicobacter pylori Infection following Endoscopic Resection of Early Gastric Cancer
Lan Li, Chaohui Yu
BioMed Research International.2019; 2019: 1. CrossRef - Prophylaxis and early diagnosis of stomach cancer
I. G. Bakulin, S. S. Pirogov, N. V. Bakulina, E. A. Stadnik, N. N. Golubev
Dokazatel'naya gastroenterologiya.2018; 7(2): 44. CrossRef - Linked Color Imaging and Blue Laser Imaging for Upper Gastrointestinal Screening
Hiroyuki Osawa, Yoshimasa Miura, Takahito Takezawa, Yuji Ino, Tsevelnorov Khurelbaatar, Yuichi Sagara, Alan Kawarai Lefor, Hironori Yamamoto
Clinical Endoscopy.2018; 51(6): 513. CrossRef
- Impact of endoscopy intervals on metachronous gastric cancer after endoscopic submucosal dissection: Comparison between 1 year and half‐a‐year
- 9,505 View
- 283 Download
- 35 Web of Science
- 39 Crossref

- Optimal Colonoscopy Surveillance Interval after Polypectomy
- Tae Oh Kim
- Clin Endosc 2016;49(4):359-363. Published online July 29, 2016
- DOI: https://doi.org/10.5946/ce.2016.080
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The detection and removal of adenomatous polyps and postpolypectomy surveillance are considered important for the control of colorectal cancer (CRC). Surveillance using colonoscopy is an effective tool for preventing CRC after colorectal polypectomy, especially if compliance is good. In current practice, the intervals between colonoscopies after polypectomy are variable. Different recommendations for recognizing at risk groups and defining surveillance intervals after an initial finding of colorectal adenomas have been published. However, high-grade dysplasia and the number and size of adenomas are known major cancer predictors. Based on this, a subgroup of patients that may benefit from intensive surveillance colonoscopy can be identified.
-
Citations
Citations to this article as recorded by- Gender disparities in colorectal polyps
A. K. Safiyeva
Klinicheskaia khirurgiia.2021; 88(1-2): 57. CrossRef - Three-year colonoscopy surveillance after polypectomy in Korea: a Korean Association for the Study of Intestinal Diseases (KASID) multicenter prospective study
Won Seok Choi, Dong Soo Han, Chang Soo Eun, Dong Il Park, Jeong-Sik Byeon, Dong-Hoon Yang, Sung-Ae Jung, Sang Kil Lee, Sung Pil Hong, Cheol Hee Park, Suck-Ho Lee, Jeong-Seon Ji, Sung Jae Shin, Bora Keum, Hyun Soo Kim, Jung Hye Choi, Sin-Ho Jung
Intestinal Research.2018; 16(1): 126. CrossRef
- Gender disparities in colorectal polyps
- 9,614 View
- 209 Download
- 2 Web of Science
- 2 Crossref

- Colon Cancer Screening and Surveillance in Inflammatory Bowel Disease
- Song I Bae, You Sun Kim
- Clin Endosc 2014;47(6):509-515. Published online November 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.6.509
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Patients with inflammatory bowel disease (IBD) have an increased risk of developing colorectal cancer (CRC). Accordingly, the duration and anatomic extent of the disease have been known to affect the development of IBD-related CRC. When CRC occurs in patients with IBD, unlike in sporadic CRC, it is difficult to detect the lesions because of mucosal changes caused by inflammation. In addition, the tumor types vary with ill-circumscribed lesions, and the cancer is difficult to diagnose and remedy at an early stage. For the diagnosis of CRC in patients with IBD, screening endoscopy is recommended 8 to 10 years after the IBD diagnosis, and surveillance colonoscopy is recommended every 1 to 2 years thereafter. The recent development of targeted biopsies using chromoendoscopy and relatively newer endoscopic techniques helps in the early diagnosis of CRC in patients with IBD. A total proctocolectomy is advisable when high-grade dysplasia or multifocal low-grade dysplasia is confirmed by screening endoscopy or surveillance colonoscopy or if a nonadenoma-like dysplasia-associated lesion or mass is detected. Currently, pharmacotherapies are being extensively studied as a way to prevent IBD-related CRC.
-
Citations
Citations to this article as recorded by- Risk of Cancer in Inflammatory Bowel Disease and Pitfalls in Oncologic Therapy
Renata D. Peixoto, Artur R. Ferreira, James M. Cleary, João P. Fogacci, João P. Vasconcelos, Alexandre A. Jácome
Journal of Gastrointestinal Cancer.2023; 54(2): 357. CrossRef - A20 Restricts NOS2 Expression and Intestinal Tumorigenesis in a Mouse Model of Colitis-Associated Cancer
David W. Basta, Mandy Vong, Adolat Beshimova, Brooke N. Nakamura, Iulia Rusu, Michael G. Kattah, Ling Shao
Gastro Hep Advances.2023; 2(1): 96. CrossRef - Association of inflammatory bowel disease in first‐degree relatives with risk of colorectal cancer: A nationwide case‐control study in Sweden
Kai Wang, Ola Olén, Louise Emilsson, Hamed Khalili, Jonas Halfvarson, Mingyang Song, Jonas F. Ludvigsson
International Journal of Cancer.2023; 152(11): 2303. CrossRef - Evaluation of intestinal ultrasound for disease activity assessment in patients with inflammatory bowel disease: A cross-sectional study at a tertiary centre in Malaysia
Kuan Yee Lim, Raja Affendi Raja Ali, Zhiqin Wong, Faizah Mohd Zaki, Juliana Fairuz Maktar, Khairul Najmi Muhammad Nawawi
Saudi Journal of Gastroenterology.2023; 29(5): 300. CrossRef - Implementing a Combined Phone and Mail Recall to Increase Screening Colonoscopy Rates in Adults With Chronic Ulcerative Colitis
Gypsy Glover
Gastroenterology Nursing.2023; 46(4): 275. CrossRef - Impact of previous diverticulitis on 5-year survival and recurrence rates in patients with colorectal cancer
Hannah Sahli, Cecilia Dahlbäck, Marie-Louise Lydrup, Pamela Buchwald
Scandinavian Journal of Gastroenterology.2023; 58(11): 1280. CrossRef - Colorectal cancer screening
Burton James Mollman
JAAPA.2023; 36(8): 15. CrossRef - Age- and sex-specific risk of colorectal cancer in incident ulcerative colitis during the first 10 years after diagnosis: a nationwide population-based study
Hee Man Kim, Ji Hoon Kim, Jung Kuk Lee, Dae Ryong Kang, Hyunil Kim, Su Young Kim, Hyun-Soo Kim
Scandinavian Journal of Gastroenterology.2021; 56(11): 1279. CrossRef - Risks and Safety of Advanced Therapies and Biologics in Inflammatory Bowel Disease
Cynthia Morvillo, Katherine Vinci, Lauren Hedenschoug, Leah Mancini, Carrie Mize, Kayce Tugg, Steven Stein
Gastroenterology Nursing.2020; 43(4): E159. CrossRef - Diagnosis and survival values of neutrophil-lymphocyte ratio (NLR) and red blood cell distribution width (RDW) in esophageal cancer
Fuyan Han, Yiqing Liu, Shiqing Cheng, Zhaohui Sun, Chenchen Sheng, Xiya Sun, Xuming Shang, Wenjun Tian, Xiaoying Wang, Jiamei Li, Dong Liu, Yong Wang, Bingchang Zhang, Ying Ju
Clinica Chimica Acta.2019; 488: 150. CrossRef - Haem iron reshapes colonic luminal environment: impact on mucosal homeostasis and microbiome through aldehyde formation
Océane C. B. Martin, Maïwenn Olier, Sandrine Ellero-Simatos, Nathalie Naud, Jacques Dupuy, Laurence Huc, Sylviane Taché, Vanessa Graillot, Mathilde Levêque, Valérie Bézirard, Cécile Héliès-Toussaint, Florence Blas Y. Estrada, Valérie Tondereau, Yannick Li
Microbiome.2019;[Epub] CrossRef - Optical Diagnosis of Colorectal Cancer
红梅 于
Medical Diagnosis.2019; 09(02): 52. CrossRef - Surgical Management of Dysplasia and Cancer in Inflammatory Bowel Disease
James Ansell, Fabian Grass, Amit Merchea
Surgical Clinics of North America.2019; 99(6): 1111. CrossRef - Methods of extraction of optical properties from diffuse reflectance measurements of ex-vivo human colon tissue using thin film silicon photodetector arrays
Ben LaRiviere, N. Lynn Ferguson, Katherine S. Garman, Deborah A. Fisher, Nan M. Jokerst
Biomedical Optics Express.2019; 10(11): 5703. CrossRef - Intestinal and Extraintestinal Cancers Associated With Inflammatory Bowel Disease
Minna Chang, Liisa Chang, Hanna M. Chang, Fuju Chang
Clinical Colorectal Cancer.2018; 17(1): e29. CrossRef - N-Methylcytisine Ameliorates Dextran-Sulfate-Sodium-Induced Colitis in Mice by Inhibiting the Inflammatory Response
Yan-Fang Jiao, Min Lu, Yu-Ping Zhao, Ning Liu, Ya-Ting Niu, Yang Niu, Ru Zhou, Jian-Qiang Yu
Molecules.2018; 23(3): 510. CrossRef - Cancer Risk in Patients with Intestinal Behçet’s Disease: A Nationwide Population-Based Study
Minkyung Han, Yoon Suk Jung, Won Ho Kim, Jae Hee Cheon, Sohee Park
Gut and Liver.2018; 12(4): 433. CrossRef - Endoscopy in Pediatric Inflammatory Bowel Disease
Salvatore Oliva, Mike Thomson, Lissy de Ridder, Javier Martín‐de‐Carpi, Stephanie Van Biervliet, Christian Braegger, Jorge Amil Dias, Sanja Kolacek, Erasmo Miele, Stephan Buderus, Jiri Bronsky, Harland Winter, Víctor Manuel Navas‐López, Amit Assa, Sonny K
Journal of Pediatric Gastroenterology and Nutrition.2018; 67(3): 414. CrossRef - Getting a Low Grade for Missing High-Grade Dysplasia and Colorectal Cancer in IBD
James R. Conner, Robert H. Riddell
Digestive Diseases and Sciences.2017; 62(12): 3594. CrossRef - Tianfoshen oral liquid: a CFDA approved clinical traditional Chinese medicine, normalizes major cellular pathways disordered during colorectal carcinogenesis
Siliang Wang, Hengbin Wang, Yin Lu
Oncotarget.2017; 8(9): 14549. CrossRef - Cancer surveillance in ulcerative colitis and Crohnʼs disease
Bincy P. Abraham
Current Opinion in Gastroenterology.2016; 32(1): 32. CrossRef - C-glycosyl flavonoid orientin improves chemically induced inflammatory bowel disease in mice
Aning Sun, Gaiyan Ren, Chao Deng, Jingjing Zhang, Xiaoping Luo, Xiaojun Wu, Sridhar Mani, Wei Dou, Zhengtao Wang
Journal of Functional Foods.2016; 21: 418. CrossRef - Colorectal Cancer in Patients With Inflammatory Bowel Disease: The Need for a Real Surveillance Program
Rosario Fornaro, Michela Caratto, Elisa Caratto, Giuseppe Caristo, Francesco Fornaro, Davide Giovinazzo, Camilla Sticchi, Marco Casaccia, Enzo Andorno
Clinical Colorectal Cancer.2016; 15(3): 204. CrossRef - A Comprehensive Meta-Analysis of MicroRNAs for Predicting Colorectal Cancer
Lin Yan, Wenhua Zhao, Haihua Yu, Yansen Wang, Yuanshui Liu, Chao Xie
Medicine.2016; 95(9): e2738. CrossRef - The continuing uncertainty about cancer risk in inflammatory bowel disease
Hans-Olov Adami, Michael Bretthauer, Louise Emilsson, Miguel A Hernán, Mette Kalager, Jonas F Ludvigsson, Anders Ekbom
Gut.2016; 65(6): 889. CrossRef - Risk factors for developing colorectal cancer in Japanese patients with ulcerative colitis: a retrospective observational study—CAPITAL (Cohort and Practice for IBD total management in Kyoto-Shiga Links) study I
Takuya Yoshino, Hiroshi Nakase, Tomohisa Takagi, Shigeki Bamba, Yusuke Okuyama, Takuji Kawamura, Teruki Oki, Hirozumi Obata, Chiharu Kawanami, Shinji Katsushima, Toshihiro Kusaka, Tomoyuki Tsujikawa, Yuji Naito, Akira Andoh, Takafumi Kogawa
BMJ Open Gastroenterology.2016; 3(1): e000122. CrossRef - Introducing Vedolizumab to Clinical Practice: Who, When, and How?
RV Bryant, WJ Sandborn, SPL Travis
Journal of Crohn's and Colitis.2015; 9(4): 356. CrossRef - Interaction analysis of IL-12A and IL-12B polymorphisms with the risk of colorectal cancer
Ruifen Sun, Fu Jia, Yundan Liang, Lijuan Li, Peng Bai, Fang Yuan, Linbo Gao, Lin Zhang
Tumor Biology.2015; 36(12): 9295. CrossRef - Utility of Peripheral Blood Parameters in Predicting Breast Cancer Risk
Yildiz Okuturlar, Meral Gunaldi, Elif Eda Tiken, Bugra Oztosun, Yesim Ozdem Inan, Tarik Ercan, Savas Tuna, Ali Osman Kaya, Ozlem Harmankaya, Abdulbaki Kumbasar
Asian Pacific Journal of Cancer Prevention.2015; 16(6): 2409. CrossRef - Interval colorectal carcinoma: An unsolved debate
Mark Benedict
World Journal of Gastroenterology.2015; 21(45): 12735. CrossRef
- Risk of Cancer in Inflammatory Bowel Disease and Pitfalls in Oncologic Therapy
- 10,961 View
- 129 Download
- 34 Web of Science
- 30 Crossref

- Endoscopic Gastric Cancer Screening and Surveillance in High-Risk Groups
- Il Ju Choi
- Clin Endosc 2014;47(6):497-503. Published online November 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.6.497
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Gastric cancer remains a major cancer problem world-wide and future incidence will likely increase due to rapidly aging population demographics. Population-based screening is being undertaken in Korea and Japan, where gastric cancer incidence rates are high, and seems to be effective in reducing mortality from gastric cancer. However, such strategies are difficult to implement in countries with a low incidence or limited resources. Thus, screening strategies should be directed towards high-risk population subgroups. Gastric cancer has a relatively long mean sojourn time, and prognosis of early-stage disease is excellent. In general population, screening at 2-year interval in Korea seems to be effective for early-stage diagnosis. In subjects with atrophic gastritis or intestinal metaplasia, surveillance is recommended at 1 to 3 years intervals according to European and Japanese recommendation. Screening intervals for family members with sporadic gastric cancer has not yet been adequately evaluated, but 1-year interval is recommended for hereditary diffuse gastric cancer family-members. Gastric cancer patients treated by endoscopic resection are the highest-risk group, and 1-year interval surveillance can detect most metachronous gastric cancers at an early stage. Future gastric cancer surveillance strategies using endoscopy should be guided by risk-stratification assessment, and further refinement of optimal surveillance intervals is needed.
-
Citations
Citations to this article as recorded by- Quantitative risk factor analysis of prior disease condition and socioeconomic status with the multiple myeloma development: nationwide cohort study
Suein Choi, Eunjin Kim, Jinhee Jung, Sung-Soo Park, Chang-Ki Min, Seunghoon Han
Scientific Reports.2024;[Epub] CrossRef - Trends in Gastric Cancer Mortality in Montenegro, 1990–2018: Joinpoint Regression
Mirjana Nedović Vuković, Marina Jakšić, Brigita Smolović, Miloš Lukić, Zoran Bukumirić
Oncology.2024; : 1. CrossRef - Prevalence of Gastric Preneoplastic Lesions in First-Degree Relatives of Patients with Gastric Cancer: a Cross-Sectional Study
Sergio Sotelo, Carlos Manterola, Tamara Otzen, Erik Morales, Iván Castillo
Journal of Gastrointestinal Cancer.2023; 54(2): 513. CrossRef - The NCC mathematical modeling framework for decision-making of six major cancers
Changfa Xia, Wanqing Chen
Journal of the National Cancer Center.2023; 3(1): 35. CrossRef - Second gastric cancer after curative endoscopic resection of differentiated-type early gastric cancer: post-hoc analysis of a single-arm confirmatory trial
Masao Yoshida, Kohei Takizawa, Noriaki Hasuike, Hiroyuki Ono, Narikazu Boku, Tomohiro Kadota, Junki Mizusawa, Ichiro Oda, Naohiro Yoshida, Yusuke Horiuchi, Kingo Hirasawa, Yoshinori Morita, Yoshinobu Yamamoto, Manabu Muto, Masao Yoshida, Kohei Takizawa, H
Gastrointestinal Endoscopy.2022; 95(4): 650. CrossRef - Effect of Hericium Evimaccus Alcohol Extracts on the Expression of Gastrin 17 and PKM2, and Cell Apoptosis in Rats with Gastric Cancer
Na Li, Mingxuan Jia, Ce Yin, Ge Feng
Science of Advanced Materials.2022; 14(1): 155. CrossRef - Dyspepsia Challenge in Primary Care Gastroenterology
Vladimir Milivojevic, Ivan Rankovic, Miodrag N. Krstic, Tomica Milosavljevic
Digestive Diseases.2022; 40(3): 270. CrossRef - Metabolomics study identified bile acids as potential biomarkers for gastric cancer: A case control study
Chen Pan, Dawei Deng, Tianfu Wei, Zeming Wu, Biao Zhang, Qihang Yuan, Guogang Liang, Yanfeng Liu, Peiyuan Yin
Frontiers in Endocrinology.2022;[Epub] CrossRef - Role of Endoscopy in Management of Upper Gastrointestinal Cancers
Jeff Liang, Yi Jiang, Yazan Abboud, Srinivas Gaddam
Diseases.2022; 11(1): 3. CrossRef - Scoring model for discriminating gastric cancer risk in patients with negative serum pepsinogen and anti‐Helicobacter pylori antibody results
Jun‐Hyung Cho, So‐Young Jin, Suyeon Park
Journal of Gastroenterology and Hepatology.2021; 36(12): 3345. CrossRef - Burden of Gastric Cancer
Aaron P. Thrift, Hashem B. El-Serag
Clinical Gastroenterology and Hepatology.2020; 18(3): 534. CrossRef - CD2AP inhibits metastasis in gastric cancer by promoting cellular adhesion and cytoskeleton assembly
Wangkai Xie, Chao Chen, Zheng Han, Jingjing Huang, Xin Liu, Hongjun Chen, Teming Zhang, Sian Chen, Chenbin Chen, Mingdong Lu, Xian Shen, Xiangyang Xue
Molecular Carcinogenesis.2020; 59(4): 339. CrossRef - Pepsinogen Serology and Gastritis OLGA Staging in Mucosal Atrophy Assessment: A Cross-Sectional Study Involving East China Endoscopy Population
Junjun Xia, Zhenzhen Liu, Kaiguang Zhang
Gastroenterology Research and Practice.2020; 2020: 1. CrossRef - Optimized diagnosis of Helicobacter pylori and tailored eradication therapy for preventing gastric cancer: a proposal for SHAKE strategy
Jun-Hyung Cho, So-Young Jin
Expert Review of Gastroenterology & Hepatology.2020; 14(7): 553. CrossRef - A protocol of systematic review and meta-analysis of narrow band imaging endoscopy in detection of early gastric cancer
Xiao-yu Liu, Jun Zhang
Medicine.2020; 99(29): e21269. CrossRef - Real-world treatment attrition rates in advanced esophagogastric cancer
Erica S Tsang, Howard J Lim, Daniel J Renouf, Janine M Davies, Jonathan M Loree, Sharlene Gill
World Journal of Gastroenterology.2020; 26(39): 6027. CrossRef - Gastrointestinal Endoscopy for Patients with High Levels of Serum CEA and CA19-9
Norihiro SUZUKI, Atsushi KATAGIRI, Shinya NAKATANI, Kazuo KIKUCHI, Toshihiko GOCHO, Fumito YANAGISAWA, Kazuya INOKI, Kenichi KONDA, Masayuki TOJO, Yutaro KUBOTA, Kazuo KONISHI, Fuyuhiko YAMAMURA, Hitoshi YOSHIDA
The Showa University Journal of Medical Sciences.2020; 32(2): 115. CrossRef - Evaluation of serum markers for gastric cancer and its precursor diseases among high incidence and mortality rate of gastric cancer area
Boldbaatar Gantuya, Khasag Oyuntsetseg, Dashdorj Bolor, Yansan Erdene-Ochir, Ruvjir Sanduijav, Duger Davaadorj, Tegshee Tserentogtokh, Tomohisa Uchida, Yoshio Yamaoka
Gastric Cancer.2019; 22(1): 104. CrossRef - Clinical advantages of robotic gastrectomy for clinical stage I/II gastric cancer: a multi-institutional prospective single-arm study
Ichiro Uyama, Koichi Suda, Masaya Nakauchi, Takahiro Kinoshita, Hirokazu Noshiro, Shuji Takiguchi, Kazuhisa Ehara, Kazutaka Obama, Shiro Kuwabara, Hiroshi Okabe, Masanori Terashima
Gastric Cancer.2019; 22(2): 377. CrossRef - Identifying high-risk individuals for gastric cancer surveillance from western and eastern perspectives: Lessons to learn and possibility to develop an integrated approach for daily practice
Duc Trong Quach, Toru Hiyama, Takuji Gotoda
World Journal of Gastroenterology.2019; 25(27): 3546. CrossRef - Cáncer gástrico: una enfermedad prevenible. Estrategias para intervención en la historia natural
Ricardo Oliveros, Raúl Eduardo Pinilla Morales, Helena Facundo Navia, Ricardo Sánchez Pedraza
Revista Colombiana de Gastroenterología.2019; 34(2): 177. CrossRef - Menopause and sexuality: characterization of sexual dysfunctions during climacteric, in women of Quindío (Colombia)
Franklin José Espitia-De la Hoz
Obstetrics & Gynecology International Journal.2019;[Epub] CrossRef - Endoscopic resection of early gastric cancer: a review article
Adrian Murillo Zolezzi, Mascareño-Ortega H, Martínez-López J, Vite-Mata D, Díaz-Castro F
Gastroenterology & Hepatology: Open Access.2019; 10(4): 168. CrossRef - Endoscopic screening for hereditary diffuse gastric cancer: one size does not fit all
Everson Luiz de Almeida Artifon, Fábio Ramalho Tavares Marinho
Gastrointestinal Endoscopy.2018; 87(2): 405. CrossRef - Diagnostic test pepsinogen I and combination with tumor marker CEA in gastric cancer
J Sembiring, K Sarumpaet, R A Ganie
IOP Conference Series: Earth and Environmental Science.2018; 125(1): 012138. CrossRef - Cost-effectiveness and short-term clinical outcomes of argon plasma coagulation compared with endoscopic submucosal dissection in the treatment of gastric low-grade dysplasia
Bomin Kim, Beom Jin Kim, Il-Kook Seo, Jae Gyu Kim
Medicine.2018; 97(15): e0330. CrossRef - Optimal Endoscopic Screening Interval for Early Detection of Gastric Cancer: a Single-Center Study
Sun Jin, Seong Woo Jeon, Yonghwan Kwon, Su Youn Nam, Seong Jae Yeo, Sang Hoon Kwon, Sang Jik Lee
Journal of Korean Medical Science.2018;[Epub] CrossRef - The prevalence of Helicobacter pylori infection and other risk factors among Mongolian dyspeptic patients who have a high incidence and mortality rate of gastric cancer
Oyuntsetseg Khasag, Gantuya Boldbaatar, Tserentogtoh Tegshee, Davaadorj Duger, Azzaya Dashdorj, Tomohisa Uchida, Takeshi Matsuhisa, Yoshio Yamaoka
Gut Pathogens.2018;[Epub] CrossRef - Screening Upper Endoscopy for Early Detection of Gastric Cancer
Jeong Seop Moon
Journal of Korean Medical Science.2018;[Epub] CrossRef - Characteristics of Synchronous and Metachronous Multiple Gastric Tumors after Endoscopic Submucosal Dissection of Early Gastric Neoplasm
Hyun Jik Lee, Yoo Jin Lee, Ju Yup Lee, Eun Soo Kim, Woo Jin Chung, Byoung Kuk Jang, Kyung Sik Park, Jae Seok Hwang, Kwang Bum Cho
Clinical Endoscopy.2018; 51(3): 266. CrossRef - Diffuse Gastric Cancer: A Summary of Analogous Contributing Factors for Its Molecular Pathogenicity
Shamshul Ansari, Boldbaatar Gantuya, Vo Tuan, Yoshio Yamaoka
International Journal of Molecular Sciences.2018; 19(8): 2424. CrossRef - Factors Affecting Endoscopic Curative Resection of Gastric Cancer in the Population-Based Screening Era
Yoon Gwon Mun, Myung-Gyu Choi, Chul-Hyun Lim, Han Hee Lee, Dong Hoon Kang, Jae Myung Park, Kyo Young Song
Clinical Endoscopy.2018; 51(5): 478. CrossRef - Emerging role of long non-coding RNA in the development of gastric cancer
Hang Yu, Long Rong
World Journal of Gastrointestinal Oncology.2018; 10(9): 260. CrossRef - How Do We Bridge the West and the East in the Treatment for Gastric Cancer?
Koichi Suda, Yuko Kitagawa
Annals of Surgical Oncology.2017; 24(4): 864. CrossRef - Long-term follow-up of pepsinogen I/II ratio after eradication of Helicobacter pylori in patients who underwent endoscopic mucosal resection for gastric cancer
Su Youn Nam, Seong Woo Jeon, Hyun Seok Lee, Yong Hwan Kwon, Haeyoon Park, Jin Woo Choi
Digestive and Liver Disease.2017; 49(5): 500. CrossRef - Application of oral contrast trans-abdominal ultrasonography for initial screening of gastric cancer in rural areas of China
Li Shen, Chenfei Zhou, Lan Liu, Li Zhang, Dianyuan Lu, Jianrong Cai, Liying Zhao, Rongrong Chu, Junyu Zhou, Jun Zhang
Digestive and Liver Disease.2017; 49(8): 918. CrossRef - Gastric Cancer as Preventable Disease
Massimo Rugge, Robert M. Genta, Francesco Di Mario, Emad M. El-Omar, Hashem B. El-Serag, Matteo Fassan, Richard H. Hunt, Ernst J. Kuipers, Peter Malfertheiner, Kentaro Sugano, David Y. Graham
Clinical Gastroenterology and Hepatology.2017; 15(12): 1833. CrossRef - The potential value of serum pepsinogen for the diagnosis of atrophic gastritis among the health check-up populations in China: a diagnostic clinical research
Yuling Tong, Yulian Wu, Zhenya Song, Yingying Yu, Xinyan Yu
BMC Gastroenterology.2017;[Epub] CrossRef - The serum pepsinogen levels for risk assessment of gastric neoplasms
Jun-Hyung Cho, Seong Ran Jeon, Hyun Gun Kim, So-Young Jin, Suyeon Park
Medicine.2017; 96(29): e7603. CrossRef - Risk factors for early metachronous tumor development after endoscopic resection for early gastric cancer
Jae Yong Park, Sang Gyun Kim, Jung Kim, Seung Jun Han, Sooyeon Oh, Ji Min Choi, Joo Hyun Lim, Hyunsoo Chung, Hyun Chae Jung, John Green
PLOS ONE.2017; 12(9): e0185501. CrossRef - The Characteristics and Prognosis of Diffuse-Type Early Gastric Cancer Diagnosed during Health Check-Ups
Ji Young Lee, Eun Jeong Gong, Eun Ju Chung, Hye Won Park, Suh Eun Bae, Eun Hee Kim, Jaeil Kim, Yoon Suh Do, Tae Hyup Kim, Hye-Sook Chang, Ho June Song, Jaewon Choe, Hwoon-Yong Jung
Gut and Liver.2017; 11(6): 807. CrossRef - Relationship between atrophic gastritis, gastric intestinal metaplasia and Helicobacter pylori on endoscopic screening of upper gastrointestinal tract and a brief review of the literature
M. Z. Üçüncü, E. Kabul Gürbulak, B. Gürbulak, O. A. Savaş, B. Özütürk, A. C. Dural, A. Haşlak
European Surgery.2016; 48(2): 99. CrossRef - Evaluation of the diagnostic value of 64 simultaneously measured autoantibodies for early detection of gastric cancer
Simone Werner, Hongda Chen, Julia Butt, Angelika Michel, Phillip Knebel, Bernd Holleczek, Inka Zörnig, Stefan B. Eichmüller, Dirk Jäger, Michael Pawlita, Tim Waterboer, Hermann Brenner
Scientific Reports.2016;[Epub] CrossRef - Job Stress and Job Satisfaction among Health-Care Workers of Endoscopy Units in Korea
Seung-Joo Nam, Hoon Jai Chun, Jeong Seop Moon, Sung Chul Park, Young-Jae Hwang, In Kyung Yoo, Jae Min Lee, Seung Han Kim, Hyuk Soon Choi, Eun Sun Kim, Bora Keum, Yoon Tae Jeen, Hong Sik Lee, Chang Duck Kim
Clinical Endoscopy.2016; 49(3): 266. CrossRef - Robotic surgery for upper gastrointestinal cancer: Current status and future perspectives
Koichi Suda, Masaya Nakauchi, Kazuki Inaba, Yoshinori Ishida, Ichiro Uyama
Digestive Endoscopy.2016; 28(7): 701. CrossRef - Current Perspectives on Gastric Cancer
Juan M. Marqués-Lespier, María González-Pons, Marcia Cruz-Correa
Gastroenterology Clinics of North America.2016; 45(3): 413. CrossRef - DNA Methylation as Surrogate Marker For Gastric Cancer
Jung-Hwan Oh, Sung-Hoon Jung, Seung-Jin Hong, Mun-Gan Rhyu
Journal of Cancer Prevention.2015; 20(3): 172. CrossRef - Detection of gastric cancer using transabdominal ultrasonography is associated with tumor diameter and depth of invasion
MINORU TOMIZAWA, FUMINOBU SHINOZAKI, KAZUNORI FUGO, RUMIKO HASEGAWA, YOSHINORI SHIRAI, YASUFUMI MOTOYOSHI, TAKAO SUGIYAMA, SHIGENORI YAMAMOTO, TAKASHI KISHIMOTO, NAOKI ISHIGE
Experimental and Therapeutic Medicine.2015; 10(5): 1835. CrossRef - Significance of Serum Pepsinogens as a Biomarker for Gastric Cancer and Atrophic Gastritis Screening: A Systematic Review and Meta-Analysis
Ya-kai Huang, Jian-chun Yu, Wei-ming Kang, Zhi-qiang Ma, Xin Ye, Shu-bo Tian, Chao Yan, Hiromu Suzuki
PLOS ONE.2015; 10(11): e0142080. CrossRef - Magnifying narrow-band imaging endoscopy is superior in diagnosis of early gastric cancer
Hang Yu
World Journal of Gastroenterology.2015; 21(30): 9156. CrossRef
- Quantitative risk factor analysis of prior disease condition and socioeconomic status with the multiple myeloma development: nationwide cohort study
- 9,994 View
- 199 Download
- 52 Web of Science
- 50 Crossref

- The Effect of the Bowel Preparation Status on the Risk of Missing Polyp and Adenoma during Screening Colonoscopy: A Tandem Colonoscopic Study
- Sung Noh Hong, In Kyung Sung, Jeong Hwan Kim, Won Hyeok Choe, Byung Kook Kim, Soon Young Ko, Jung Hyun Lee, Dong Choon Seol, Su Young Ahn, Sun-Young Lee, Hyung Seok Park, Chan Sup Shim
- Clin Endosc 2012;45(4):404-411. Published online November 30, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.4.404
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Although a small amount of fecal material can obscure significant colorectal lesions, it has not been well documented whether bowel preparation status affects the missing risk of colorectal polyps and adenomas during a colonoscopy.
Methods We prospectively enrolled patients with one to nine colorectal polyps and at least one adenoma of >5 mm in size at the screening colonoscopy. Tandem colonoscopy with polypectomy was carried out within 3 months.
Results A total of 277 patients with 942 polyps and 714 adenomas completed index and tandem examinations. At the index colonoscopy, 187 polyps (19.9%) and 127 adenomas (17.8%) were missed. The per-patient miss rate of polyps and adenomas increased significantly as the bowel cleansing rate declined from excellent to poor/inadequate on the Aronchick scale (polyps,
p =0.024; adenomas,p =0.040). The patients with poor/inadequate bowel preparation were independently associated with an increased risk of having missed polyps (odds ratio [OR], 3.21; 95% confidence interval [CI], 1.13 to 9.15) or missed adenomas (OR, 3.04; 95% CI, 1.04 to 8.88) compared to the patients with excellent bowel preparation.Conclusions The risk of missing polyps and adenomas during screening colonoscopy is significantly affected by bowel preparation status. It seems appropriate to shorten the colonoscopy follow-up interval for patients with suboptimal bowel preparation.
-
Citations
Citations to this article as recorded by- What are the priority quality indicators for colonoscopy in real‐world clinical practice?
Kasenee Tiankanon, Satimai Aniwan
Digestive Endoscopy.2024; 36(1): 30. CrossRef - Sleep Disturbances, Bowel Movement Kinetics, and Travel Interruption With Bowel Preparation: A Bowel CLEANsing National Initiative Substudy
Carmen Tse, Alan Barkun, Myriam Martel, Zoann Nugent, Ian Epstein, Michael Sey, Sultanian Richard, Daniel von Renteln, Harminder Singh
American Journal of Gastroenterology.2023; 118(1): 87. CrossRef - Computer-assisted detection versus conventional colonoscopy for proximal colonic lesions: a multicenter, randomized, tandem-colonoscopy study
Thomas K.L. Lui, Dao Viet Hang, Stephen K.K. Tsao, Cynthia K.Y. Hui, Loey Lung Yi Mak, Michael K.L. Ko, Ka Shing Cheung, M.Y. Thian, R. Liang, Vivien W.M. Tsui, Chung Kwong Yeung, L.V. Dao, Wai K. Leung
Gastrointestinal Endoscopy.2023; 97(2): 325. CrossRef - ColonNet: A novel polyp segmentation framework based on LK-RFB and GPPD
Dong Sui, Weifeng Liu, Yue Zhang, Yang Li, Gongning Luo, Kuanquan Wang, Maozu Guo
Computers in Biology and Medicine.2023; 166: 107541. CrossRef - The necessity of intensive surveillance colonoscopy for patients with a remaining right colon after resection of colorectal cancer: a retrospective cohort study
Mitsuru Yokota, Jun Muto, Kazuki Hashida, Yoshio Nagahisa, Michio Okabe, Hirohisa Kitagawa, Kazuyuki Kawamoto
Surgery Today.2022; 52(3): 502. CrossRef - Efficacy and safety of split-dose bowel preparation with 1 L polyethylene glycol and ascorbate compared with 2 L polyethylene glycol and ascorbate in a Korean population: a phase IV, multicenter, randomized, endoscopist-blinded study
Sung Noh Hong, Chang Kyun Lee, Jong Pil Im, Chang Hwan Choi, Jeong-Sik Byeon, Young-Seok Cho, Sung-Ae Jung, Tae Il Kim, Yoon Tae Jeen
Gastrointestinal Endoscopy.2022; 95(3): 500. CrossRef - Relationship between Health Literacy and Knowledge, Compliance with Bowel Preparation, and Bowel Cleanliness in Older Patients Undergoing Colonoscopy
Minju Gwag, Jaeyong Yoo
International Journal of Environmental Research and Public Health.2022; 19(5): 2676. CrossRef - Oral sulfate solution benefits polyp and adenoma detection during colonoscopy: Meta‐analysis of randomized controlled trials
Cheng Chen, Mengyang Shi, Zhongli Liao, Weiqing Chen, Yongzhong Wu, Xu Tian
Digestive Endoscopy.2022; 34(6): 1121. CrossRef - Rectal Evacuation Disorders are Associated With Poor Bowel Preparation in Patients With Chronic Constipation
Mythili P. Pathipati, Casey J. Silvernale, Kenneth G. Barshop, Jasmine B. Ha, James M. Richter, Kyle D. Staller
Journal of Clinical Gastroenterology.2022; 56(5): 438. CrossRef - Impact of looping on premalignant polyp detection during colonoscopy
Osamu Toyoshima, Toshihiro Nishizawa, Shuntaro Yoshida, Tatsuya Matsuno, Toru Arano, Ryo Kondo, Kazunori Kinoshita, Yuki Yasumi, Yosuke Tsuji, Mitsuhiro Fujishiro
World Journal of Gastrointestinal Endoscopy.2022; 14(11): 694. CrossRef - New insights on missed colonic lesions during colonoscopy through artificial intelligence–assisted real-time detection (with video)
Thomas K.L. Lui, Cynthia K.Y. Hui, Vivien W.M. Tsui, Ka Shing Cheung, Michael K.L. Ko, Dominic C.C. Foo, Lung Yi Mak, Chung Kwong Yeung, Tim HW Lui, Siu Yin Wong, Wai K. Leung
Gastrointestinal Endoscopy.2021; 93(1): 193. CrossRef - Colonoscopy in poorly prepped colons: a cost effectiveness analysis comparing standard of care to a new cleansing technology
Jeffrey Voigt, Michael Mosier, Ian M. Gralnek
Cost Effectiveness and Resource Allocation.2021;[Epub] CrossRef - Multidirectional Colonoscopy Quality Improvement Increases Adenoma Detection Rate: Results of the Seoul National University Hospital Healthcare System Gangnam Center Colonoscopy Quality Upgrade Project (Gangnam-CUP)
Ji Yeon Seo, Eun Hyo Jin, Jung Ho Bae, Joo Hyun Lim, Goh Eun Chung, Changhyun Lee, Min-Sun Kwak, Hae Yeon Kang, Ji Hyun Song, Sun Young Yang, Jong In Yang, Seon Hee Lim, Jeong Yoon Yim, Joo Sung Kim, Su Jin Chung
Digestive Diseases and Sciences.2020; 65(6): 1806. CrossRef - Berberine versus placebo for the prevention of recurrence of colorectal adenoma: a multicentre, double-blinded, randomised controlled study
Ying-Xuan Chen, Qin-Yan Gao, Tian-Hui Zou, Bang-Mao Wang, Si-De Liu, Jian-Qiu Sheng, Jian-Lin Ren, Xiao-Ping Zou, Zhan-Ju Liu, Yan-Yan Song, Bing Xiao, Xiao-Min Sun, Xiao-Tan Dou, Hai-Long Cao, Xiao-Ning Yang, Na Li, Qian Kang, Wei Zhu, Hong-Zhi Xu, Hui-M
The Lancet Gastroenterology & Hepatology.2020; 5(3): 267. CrossRef - Improving the quality of bowel preparation through an app for inpatients undergoing colonoscopy: A randomized controlled trial
Bingmei Guo, Xiuli Zuo, Zhen Li, Jun Liu, Na Xu, Xiaohui Li, Aifang Zhu
Journal of Advanced Nursing.2020; 76(4): 1037. CrossRef - A Randomized, Endoscopist-Blinded, Prospective Trial to Compare the Efficacy and Patient Tolerability between Bowel Preparation Protocols Using Sodium Picosulfate Magnesium Citrate and Polyethylene-Glycol (1 L and 2 L) for Colonoscopy
Sang Hoon Kim, Ji Hyeong Kim, Bora Keum, Han Jo Jeon, Se Hyun Jang, Seong Ji Choi, Seung Han Kim, Jae Min Lee, Hyuk Soon Choi, Eun Sun Kim, Yoon Tae Jeen, Hong Sik Lee, Hoon Jai Chun, Chang Duck Kim
Gastroenterology Research and Practice.2020; 2020: 1. CrossRef - Efficacy of low‐dose versus high‐dose simethicone with polyethylene glycol for bowel preparation: A prospective randomized controlled trial
De‐feng Li, Ming‐han Luo, Qing‐qing Du, Hai‐yang Zhang, Yan‐hui Tian, Ting‐ting Liu, Rui‐yue Shi, Feng Xiong, Ming‐guang Lai, Ying‐xue Li, Su Luo, Yang Song, Ben‐hua Wu, Zheng‐lei Xu, Ding‐guo Zhang, Jun Yao, Li‐sheng Wang
Journal of Gastroenterology and Hepatology.2020; 35(9): 1488. CrossRef - Optimal Laxatives for Oral Colonoscopy Bowel Preparation: from High-volume to Novel Low-volume Solutions
Soo-Young Na, Won Moon
The Korean Journal of Gastroenterology.2020; 75(2): 65. CrossRef - Impact of Inadequate Bowel Cleansing on Colonoscopic Findings in Routine Screening Practice
Tobias Niedermaier, Efrat L. Amitay, Anton Gies, Korbinian Weigl, Michael Hoffmeister, Hermann Brenner
Clinical and Translational Gastroenterology.2020; 11(4): e00169. CrossRef - Reinforced education improves the quality of bowel preparation for colonoscopy: An updated meta-analysis of randomized controlled trials
Xiaoyang Guo, Xin Li, Zhiyan Wang, Junli Zhai, Qiang Liu, Kang Ding, Yanglin Pan, Antonio Z Gimeno-Garcia
PLOS ONE.2020; 15(4): e0231888. CrossRef - Comparison of Oral Sulfate Solution and Polyethylene Glycol Plus Ascorbic Acid on the Efficacy of Bowel Preparation
Ji Hyung Nam, Seok Bo Hong, Yun Jeong Lim, Seongju Lee, Hyoun Woo Kang, Jae Hak Kim, Jin Ho Lee
Clinical Endoscopy.2020; 53(5): 568. CrossRef - Relationship between serrated polyps and synchronous and metachronous advanced neoplasia: A retrospective study
En‐Wei Tao, Yong Feng Wang, Tian Hui Zou, Yun Cui, Ying Xuan Chen, Qin Yan Gao
Journal of Digestive Diseases.2020; 21(10): 558. CrossRef - Efficacy and Patient Tolerability Profiles of Probiotic Solution with Bisacodyl Versus Conventional Cleansing Solution for Bowel Preparation: A Prospective, Randomized, Controlled Trial
Youn I Choi, Jong-Joon Lee, Jun-Won Chung, Kyoung Oh Kim, Yoon Jae Kim, Jung Ho Kim, Dong Kyun Park, Kwang An Kwon
Journal of Clinical Medicine.2020; 9(10): 3286. CrossRef - Bowel preparation for colonoscopy
Parth J. Parekh, Edward C. Oldfield, David A. Johnson
Current Opinion in Gastroenterology.2019; 35(1): 51. CrossRef - Standards of diagnostic colonoscopy for early‐stage neoplasia: Recommendations by an Asian private group
Yasushi Sano, Han‐Mo Chiu, Xiao‐bo Li, Supakij Khomvilai, Pises Pisespongsa, Jonard Tan Co, Takuji Kawamura, Nozomu Kobayashi, Shinji Tanaka, David G. Hewett, Yoji Takeuchi, Kenichiro Imai, Takahiro Utsumi, Akira Teramoto, Daizen Hirata, Mineo Iwatate, Ra
Digestive Endoscopy.2019; 31(3): 227. CrossRef - Comparison Between an Oral Sulfate Solution and a 2 L of Polyethylene Glycol/Ascorbic Acid as a Split Dose Bowel Preparation for Colonoscopy
Han Hee Lee, Chul-Hyun Lim, Jin Su Kim, Yu Kyung Cho, Bo-In Lee, Young-Seok Cho, In Seok Lee, Myung-Gyu Choi
Journal of Clinical Gastroenterology.2019; 53(10): e431. CrossRef - Multicentre endoscopist-blinded randomised clinical trial to compare two bowel preparations after a colonoscopy with inadequate cleansing: a study protocol
Michael Sai Lai Sey, Daniel von Renteln, Richard Sultanian, Cassandra McDonald, Myriam Martel, Alan Barkun
BMJ Open.2019; 9(7): e029573. CrossRef - Predictive factors for missed adenoma on repeat colonoscopy in patients with suboptimal bowel preparation on initial colonoscopy: A KASID multicenter study
Ji Young Chang, Chang Mo Moon, Hyun Jung Lee, Hyo-Joon Yang, Yunho Jung, Sang Wook Kim, Sung-Ae Jung, Jeong-Sik Byeon, Frank T. Kolligs
PLOS ONE.2018; 13(4): e0195709. CrossRef - A novel summary report of colonoscopy: timeline visualization providing meaningful colonoscopy video information
Minwoo Cho, Jee Hyun Kim, Hyoun Joong Kong, Kyoung Sup Hong, Sungwan Kim
International Journal of Colorectal Disease.2018; 33(5): 549. CrossRef - The use of chromoendoscopy for surveillance of inflammatory bowel disease
Gary R. Lichtenstein, Michael F. Picco, Sanjeev Solomon, Stephen J. Bickston
VideoGIE.2018; 3(2): 35. CrossRef - Readability of information on colonoscopy preparation on the internet
Sarah A. MacLean, Corey H Basch, Ashley Clark, Charles E Basch
Health Promotion Perspectives.2018; 8(2): 167. CrossRef - Adenoma miss rate determined by very shortly repeated colonoscopy
Cheng-Long Wang, Zhi-Ping Huang, Kai Chen, Fei-Hu Yan, Liang-Liang Zhu, Yong-Qi Shan, Yong-Jun-Yi Gao, Bai-Rong Li, Hao Wang, En-Da Yu, Zi-Ye Zhao
Medicine.2018; 97(38): e12297. CrossRef - Impact of Video Aid on Quality of Bowel Preparation Among Patients Undergoing Outpatient Screening Colonoscopy
Sanna Fatima, Deepanshu Jain, Christopher Hibbard
Clinical Medicine Insights: Gastroenterology.2018; 11: 117955221880330. CrossRef - Frequency and Characteristics of Interval Colorectal Cancer in Actual Clinical Practice: A KASID Multicenter Study
Kyeong Ok Kim, Kyu Chan Huh, Sung Pil Hong, Won Hee Kim, Hyuk Yoon, Sang Wook Kim, Yeon Soo Kim, Jong Ha Park, Jun Lee, Bum Jae Lee, Young Sook Park
Gut and Liver.2018; 12(5): 537. CrossRef - Risk factors of missed colorectal lesions after colonoscopy
Jeonghun Lee, Sung Won Park, You Sun Kim, Kyung Jin Lee, Hyun Sung, Pil Hun Song, Won Jae Yoon, Jeong Seop Moon
Medicine.2017; 96(27): e7468. CrossRef - Enhanced education for bowel preparation before colonoscopy: A state‐of‐the‐art review
Zhu Liu, Ming Ming Zhang, Yue Yue Li, Li Xiang Li, Yan Qing Li
Journal of Digestive Diseases.2017; 18(2): 84. CrossRef - Polyp missing rate and its associated risk factors of referring hospitals for endoscopic resection of advanced colorectal neoplasia
Jae Gyu Shin, Hyung Wook Kim, Su Bum Park, Cheol Woong Choi, Dae Hwan Kang, Su Jin Kim, Hyeong Seok Nam, Dae Gon Ryu
Medicine.2017; 96(19): e6742. CrossRef - Split‐dose bowel preparation with polyethylene glycol for colonoscopy performed under propofol sedation. Is there an optimal timing?
Alaa Alghamry, Sureshkumar K Ponnuswamy, Aditya Agarwal, Hadi Moattar, Stephanie T Yerkovich, Ann E Vandeleur, James Thomas, John Croese, Tony Rahman, Ruth Hodgson
Journal of Digestive Diseases.2017; 18(3): 160. CrossRef - Miss rate of colorectal neoplastic polyps and risk factors for missed polyps in consecutive colonoscopies
Nam Hee Kim, Yoon Suk Jung, Woo Shin Jeong, Hyo-Joon Yang, Soo-Kyung Park, Kyuyong Choi, Dong Il Park
Intestinal Research.2017; 15(3): 411. CrossRef - Training in Endoscopy: Colonoscopy
Hyun Joo Jang
Clinical Endoscopy.2017; 50(4): 322. CrossRef - Effect of Low-Volume Split-Dose Purgative on the Quality of Bowel Prep for Colonoscopy on the Hospitalized Patient
Judy A. Corliss
Gastroenterology Nursing.2017; 40(6): 448. CrossRef - Quantification of Adequate Bowel Preparation for Screening or Surveillance Colonoscopy in Men
Brian T. Clark, Petr Protiva, Anil Nagar, Avlin Imaeda, Maria M. Ciarleglio, Yanhong Deng, Loren Laine
Gastroenterology.2016; 150(2): 396. CrossRef - A novel quality scoring system for the evaluation of individual colonoscopy: A multicenter retrospective study
Qiang Zhan, Li Xiang, Xinhua Zhao, Shengli An, Yadong Wang, Yangzhi Xu, Aimin Li, Wei Gong, Yang Bai, Yali Zhang, Side Liu
Journal of Gastroenterology and Hepatology.2016; 31(1): 172. CrossRef - Providing Hospitalized Patients With an Educational Booklet Increases the Quality of Colonoscopy Bowel Preparation
William F. Ergen, Trisha Pasricha, Francie J. Hubbard, Tina Higginbotham, Tonya Givens, James C. Slaughter, Keith L. Obstein
Clinical Gastroenterology and Hepatology.2016; 14(6): 858. CrossRef - Izinova®, nouvelle préparation orale à diluer pour lavage colique
Acta Endoscopica.2016; 46(1-2): 74. CrossRef - Factors associated with colorectal cancer occurrence after colonoscopy that did not diagnose colorectal cancer
Danny Cheung, Felicity Evison, Prashant Patel, Nigel Trudgill
Gastrointestinal Endoscopy.2016; 84(2): 287. CrossRef - Impact of bowel preparation type on the quality of colonoscopy: a multicenter community-based study
Daniel Martin, Saqib Walayat, Zohair Ahmed, Sonu Dhillon, Carl V. Asche, Srinivas Puli, Jinma Ren
Journal of Community Hospital Internal Medicine Pe.2016; 6(2): 31074. CrossRef - Comparative Study on Bowel Preparation Efficacy of Ascorbic Acid Containing Polyethylene Glycol by Adding Either Simethicone or 1 L of Water in Health Medical Examination Patients: A Prospective Randomized Controlled Study
Se Hwan Yeo, Jae Hoon Kwak, Yeo Un Kim, Tae Ho Kwon, Jeong Bae Park, Jun Hyung Park, Yong Kook Lee, Yun Jeong Lim, Chang Heon Yang
The Korean Journal of Gastroenterology.2016; 67(4): 189. CrossRef - Advanced colonic neoplasia in the first degree relatives of colon cancer patients: A colonoscopy‐based study
Hamideh Salimzadeh, Faraz Bishehsari, Mohammad Amani, Reza Ansari, Masoud Sotoudeh, Alireza Delavari, Reza Malekzadeh
International Journal of Cancer.2016; 139(10): 2243. CrossRef - Video on Diet Before Outpatient Colonoscopy Does Not Improve Quality of Bowel Preparation: A Prospective, Randomized, Controlled Trial
Sean C Rice, Tina Higginbotham, Melanie J Dean, James C Slaughter, Patrick S Yachimski, Keith L Obstein
American Journal of Gastroenterology.2016; 111(11): 1564. CrossRef - Meta-Analysis of the Effect of Bowel Preparation on Adenoma Detection: Early Adenomas Affected Stronger than Advanced Adenomas
Michael C. Sulz, Arne Kröger, Meher Prakash, Christine N. Manser, Henriette Heinrich, Benjamin Misselwitz, Irving Coy Allen
PLOS ONE.2016; 11(6): e0154149. CrossRef - Seeing better - Evidence based recommendations on optimizing colonoscopy adenoma detection rate
Javier Aranda-Hernández
World Journal of Gastroenterology.2016; 22(5): 1767. CrossRef - Predictors of Inadequate Inpatient Colonoscopy Preparation and Its Association with Hospital Length of Stay and Costs
Rena Yadlapati, Elyse R. Johnston, Dyanna L. Gregory, Jody D. Ciolino, Andrew Cooper, Rajesh N. Keswani
Digestive Diseases and Sciences.2015; 60(11): 3482. CrossRef - Endoscopists with low adenoma detection rates benefit from high-definition endoscopy
Elisabeth Waldmann, Martha Britto-Arias, Irina Gessl, Georg Heinze, Petra Salzl, Daniela Sallinger, Michael Trauner, Werner Weiss, Arnulf Ferlitsch, Monika Ferlitsch
Surgical Endoscopy.2015; 29(2): 466. CrossRef - Preparación para colonoscopia. ¿Algún avance significativo en el horizonte?
Liseth Rivero-Sánchez, María Pellisé
Gastroenterología y Hepatología.2015; 38(4): 287. CrossRef - Risk factors for polyp retrieval failure in colonoscopy
Carlos Fernandes, Rolando Pinho, Iolanda Ribeiro, Joana Silva, Ana Ponte, João Carvalho
United European Gastroenterology Journal.2015; 3(4): 387. CrossRef - Impact of the Quality of Bowel Cleansing on the Efficacy of Colonic Cancer Screening: A Prospective, Randomized, Blinded Study
Jürgen Pohl, Marc Halphen, Hans Rudolf Kloess, Wolfgang Fischbach, John Green
PLOS ONE.2015; 10(5): e0126067. CrossRef - Electrolyte changes after bowel preparation for colonoscopy: A randomized controlled multicenter trial
Kyong Joo Lee
World Journal of Gastroenterology.2015; 21(10): 3041. CrossRef - Improved bowel preparation increases polyp detection and unmasks significant polyp miss rate
Ioannis S Papanikolaou
World Journal of Clinical Cases.2015; 3(10): 880. CrossRef - Factors Influencing the Miss Rate of Polyps in a Tandem Colonoscopy Study
Han Na Choi, Hyun Hee Kim, Jang Seok Oh, Hee Sang Jang, Hyun Sik Hwang, Eun Young Kim, Joong Goo Kwon, Jin Tae Jung
The Korean Journal of Gastroenterology.2014; 64(1): 24. CrossRef - Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the U.S. Multi-Society Task Force on Colorectal Cancer
David A. Johnson, Alan N. Barkun, Larry B. Cohen, Jason A. Dominitz, Tonya Kaltenbach, Myriam Martel, Douglas J. Robertson, C. Richard Boland, Frances M. Giardello, David A. Lieberman, Theodore R. Levin, Douglas K. Rex
Gastrointestinal Endoscopy.2014; 80(4): 543. CrossRef - Optimizing Adequacy of Bowel Cleansing for Colonoscopy: Recommendations From the US Multi-Society Task Force on Colorectal Cancer
David A Johnson, Alan N Barkun, Larry B Cohen, Jason A Dominitz, Tonya Kaltenbach, Myriam Martel, Douglas J Robertson, Richard C Boland, Frances M Giardello, David A Lieberman, Theodore R Levin, Douglas K Rex
American Journal of Gastroenterology.2014; 109(10): 1528. CrossRef - Optimizing Adequacy of Bowel Cleansing for Colonoscopy: Recommendations From the US Multi-Society Task Force on Colorectal Cancer
David A. Johnson, Alan N. Barkun, Larry B. Cohen, Jason A. Dominitz, Tonya Kaltenbach, Myriam Martel, Douglas J. Robertson, C. Richard Boland, Frances M. Giardello, David A. Lieberman, Theodore R. Levin, Douglas K. Rex
Gastroenterology.2014; 147(4): 903. CrossRef - Importance of the Time Interval between Bowel Preparation and Colonoscopy in Determining the Quality of Bowel Preparation for Full-Dose Polyethylene Glycol Preparation
Tae Kyung Kim, Hyung Wook Kim, Su Jin Kim, Jong Kun Ha, Hyung Ha Jang, Young Mi Hong, Su Bum Park, Cheol Woong Choi, Dae Hwan Kang
Gut and Liver.2014; 8(6): 625. CrossRef - The effect of different patient education methods on quality of bowel cleanliness in outpatients receiving colonoscopy examination
Feng-Chi Hsueh, Han-Chih Wang, Chien-An Sun, Chia-Chen Tseng, Tung-Chen Han, Szu-Mei Hsiao, Cheng-Yu Wei, Chien-Hua Chen, Tsan Yang
Applied Nursing Research.2014; 27(2): e1. CrossRef - Rural–urban differences in the long-term risk of colorectal cancer after adenoma removal: A population-based study
Isabelle Fournel, Vanessa Cottet, Christine Binquet, Valérie Jooste, Jean Faivre, Anne-Marie Bouvier, Claire Bonithon-Kopp
Digestive and Liver Disease.2014; 46(4): 376. CrossRef - What Are the Factors Influencing the Miss Rate of Polyps in a Tandem Colonoscopic Study?
Young-Eun Joo
The Korean Journal of Gastroenterology.2014; 64(1): 1. CrossRef - Prerequisites of Colonoscopy
Kyong Hee Hong, Yun Jeong Lim
Clinical Endoscopy.2014; 47(4): 324. CrossRef - Colonoscopy quality improvement: practice to public health
James M. Richter
Gastrointestinal Endoscopy.2013; 78(6): 919. CrossRef - Recommended Intervals Between Screening and Surveillance Colonoscopies
Todd H. Baron, Thomas C. Smyrk, Douglas K. Rex
Mayo Clinic Proceedings.2013; 88(8): 854. CrossRef - Clinical Practice of Surveillance Colonoscopy according to the Classification of Colorectal Intraepithelial Neoplasia in Korea: High-grade Dysplasia/CarcinomaIn SituVersus Intramucosal Carcinoma
Sung Pil Hong, Tae Il Kim, Hyun Gun Kim, Hyun-Soo Kim, Seong-Eun Kim, Kyu Chan Huh, Jeong Eun Shin, Jae Myung Cha, Suck-Ho Lee
Intestinal Research.2013; 11(4): 276. CrossRef - Inadequate Bowel Preparation Increases Missed Polyps
Hyung Wook Kim
Clinical Endoscopy.2012; 45(4): 345. CrossRef
- What are the priority quality indicators for colonoscopy in real‐world clinical practice?
- 9,622 View
- 121 Download
- 72 Crossref

- Colonoscopic Cancer Surveillance in Inflammatory Bowel Disease: What's New Beyond Random Biopsy?
- James E. East
- Clin Endosc 2012;45(3):274-277. Published online August 22, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.3.274
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Colonoscopy based colitis surveillance is widely accepted to try to prevent development of and ensure early detection of colitis-associated colorectal cancer. Traditionally this has been performed with quadrantic random biopsies throughout the colon. Chromoendoscopy "dye-spray" with targeted biopsies only has been shown to increase dysplasia detection 4 to 5 fold on a per lesion basis. It has therefore been suggested that random biopsies should be abandoned as they do not increase dysplasia detection nor change patient clinical course. Recent British guidelines for colitis surveillance have strongly endorsed chromoendoscopy. This short review summarizes current international guidelines and looks at how to optimize white light colonoscopy in colitis considering: bowel preparation, withdrawal time, high definition, and structure enhancement. Data for advanced imaging techniques are reviewed including positive evidence in favor of chromoendoscopy, and limited data suggesting autofluoresence imaging may be promising. Narrow band imaging does not increase dysplasia detection in colitis. Confocal endomicroscopy might potentially reduce biopsies beyond that of chromoendoscopy but does not offer a clear detection advantage. Pan-colonic chromoendoscopy with targeted biopsies increases dysplasia detection and is the standard of care in the United Kingdom. It is likely that the use of chromoendoscopy for colitis surveillance will become widely accepted internationally.
-
Citations
Citations to this article as recorded by- Colon Cancer
Sherief Shawki, Jean Ashburn, Steven A. Signs, Emina Huang
Surgical Oncology Clinics of North America.2018; 27(2): 269. CrossRef - Advanced endoscopic imaging for diagnosis of inflammatory bowel diseases: Present and future perspectives
Visvakanth Sivanathan, Gian Eugenio Tontini, Markus Möhler, Peter R. Galle, Helmut Neumann
Digestive Endoscopy.2018; 30(4): 441. CrossRef - Chromoendoscopy for Dysplasia Surveillance in Inflammatory Bowel Disease
Ann D Flynn, John F Valentine
Inflammatory Bowel Diseases.2018; 24(7): 1440. CrossRef - Early detection of ulcerative colitis-associated colorectal cancer
Yu Zhen, Chengxin Luo, Hu Zhang
Gastroenterology Report.2018; 6(2): 83. CrossRef - Screening and surveillance methods for dysplasia in inflammatory bowel disease patients: Where do we stand?
Michail Galanopoulos, Emmanouela Tsoukali, Filippos Gkeros, Marina Vraka, Georgios Karampekos, Gerassimos J Matzaris
World Journal of Gastrointestinal Endoscopy.2018; 10(10): 250. CrossRef - The rectal remnant after total colectomy for colitis – intra-operative,post-operative and longer-term considerations
Kalle Landerholm, Christopher Wood, Alexander Bloemendaal, Nicolas Buchs, Bruce George, Richard Guy
Scandinavian Journal of Gastroenterology.2018; 53(12): 1443. CrossRef - Crohn's disease: risk factor for colorectal cancer
Sandra Cristina Dias dos Santos, Laura Elisabete Ribeiro Barbosa
Journal of Coloproctology.2017; 37(01): 055. CrossRef - Chromoendoscopy for Surveillance in Ulcerative Colitis and Crohn’s Disease: A Systematic Review of Randomized Trials
Andrea Iannone, Marinella Ruospo, Germaine Wong, Mariabeatrice Principi, Michele Barone, Giovanni F.M. Strippoli, Alfredo Di Leo
Clinical Gastroenterology and Hepatology.2017; 15(11): 1684. CrossRef - Chinese consensus on the prevention of colorectal cancer (2016, Shanghai)
Jing‐Yuan Fang, Yong Quan Shi, Ying Xuan Chen, Jing Nan Li, Jian Qiu Sheng
Journal of Digestive Diseases.2017; 18(2): 63. CrossRef - Advanced imaging and therapeutic endoscopy
Chaitanya Pant, Mojtaba S. Olyaee, Amit Rastogi
Techniques in Gastrointestinal Endoscopy.2017; 19(3): 151. CrossRef - Improving the utility of colonoscopy: Recent advances in practice
Crispin J Corte, Rupert W Leong
Journal of Gastroenterology and Hepatology.2016; 31(1): 32. CrossRef - Colorectal Cancer in Patients With Inflammatory Bowel Disease: The Need for a Real Surveillance Program
Rosario Fornaro, Michela Caratto, Elisa Caratto, Giuseppe Caristo, Francesco Fornaro, Davide Giovinazzo, Camilla Sticchi, Marco Casaccia, Enzo Andorno
Clinical Colorectal Cancer.2016; 15(3): 204. CrossRef - How to Optimize Colon Cancer Surveillance in Inflammatory Bowel Disease Patients
Jill K. J. Gaidos, Stephen J. Bickston
Inflammatory Bowel Diseases.2016; 22(5): 1219. CrossRef - Endoscopy in the Diagnosis and Management of Complications of Inflammatory Bowel Disease
Benjamin Tharian, Nayana George, Udayakumar Navaneethan
Inflammatory Bowel Diseases.2016; 22(5): 1184. CrossRef - Surveillance of patients with inflammatory bowel disease
Jessica X. Yu, James E. East, Tonya Kaltenbach
Best Practice & Research Clinical Gastroenterology.2016; 30(6): 949. CrossRef - The role of endoscopy in inflammatory bowel disease
Amandeep K. Shergill, Jenifer R. Lightdale, David H. Bruining, Ruben D. Acosta, Vinay Chandrasekhara, Krishnavel V. Chathadi, G. Anton Decker, Dayna S. Early, John A. Evans, Robert D. Fanelli, Deborah A. Fisher, Lisa Fonkalsrud, Kimberly Foley, Joo Ha Hwa
Gastrointestinal Endoscopy.2015; 81(5): 1101. CrossRef - Chromoendoscopy for Colorectal Cancer Surveillance in Patients with Inflammatory Bowel Disease
Samir A. Shah, David T. Rubin, Francis A. Farraye
Current Gastroenterology Reports.2014;[Epub] CrossRef - Toward a Consensus on Endoscopic Surveillance of Patients with Colonic Inflammatory Bowel Disease
Amandeep K. Shergill, Francis A. Farraye
Gastrointestinal Endoscopy Clinics of North America.2014; 24(3): 469. CrossRef - Achieving the best bowel preparation for colonoscopy
Adolfo Parra-Blanco, Alex Ruiz, Manuel Alvarez-Lobos, Ana Amorós, Juan Cristóbal Gana, Patricio Ibáñez, Akiko Ono, Takahiro Fujii
World Journal of Gastroenterology.2014; 20(47): 17709. CrossRef - Colorectal cancer in inflammatory bowel disease: The risk, pathogenesis, prevention and diagnosis
Eun Ran Kim
World Journal of Gastroenterology.2014; 20(29): 9872. CrossRef - Highlights of the 48th Seminar of Korean Society of Gastrointestinal Endoscopy
Kwang An Kwon, Il Ju Choi, Eun Young Kim, Seok Ho Dong, Ki Baik Hahm
Clinical Endoscopy.2013; 46(3): 203. CrossRef
- Colon Cancer
- 6,528 View
- 40 Download
- 21 Crossref

- Korean Guidelines for Postpolypectomy Colonoscopy Surveillance
- Dong-Hoon Yang, Sung Noh Hong, Young-Ho Kim, Sung Pil Hong, Sung Jae Shin, Seong-Eun Kim, Bo In Lee, Suck-Ho Lee, Dong Il Park, Hyun-Soo Kim, Suk-Kyun Yang, Hyo Jong Kim, Se Hyung Kim, Hyun Jung Kim, Multi-Society Task Force for Development of Guidelines for Colorectal Polyp Screening, Surveillance and Management
- Clin Endosc 2012;45(1):44-61. Published online March 31, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.1.44
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub Postpolypectomy surveillance has become a major indication for colonoscopy as a result of increased use of screening colonoscopy in Korea. In this report, a careful analytic approach was used to address all available evidences to delineate the predictors for advanced neoplasia at surveillance colonoscopy and we elucidated the high risk findings of the index colonoscopy as follows: 3 or more adenomas, any adenoma larger than 10 mm, any tubulovillous or villous adenoma, any adenoma with high-grade dysplasia, and any serrated polyps larger than 10 mm. Surveillance colonoscopy should be performed five years after the index colonoscopy for those without any high-risk findings and three years after the index colonoscopy for those with one or more high risk findings. However, the surveillance interval can be shortened considering the quality of the index colonoscopy, the completeness of polypectomy, the patient's general condition, and family and medical history.
-
Citations
Citations to this article as recorded by- Post-colonoscopy colorectal cancers in a national fecal immunochemical test-based colorectal cancer screening program
Pieter H. A. Wisse, Sybrand Y. de Boer, Marco Oudkerk Pool, Jochim S Terhaar sive Droste, Claudia Verveer, Gerrit A. Meijer, Evelien Dekker, Manon C. W. Spaander
Endoscopy.2024; 56(05): 364. CrossRef - Recurrence rates of advanced colorectal neoplasia (ACN) in subjects with baseline ACN followed up at different surveillance intervals
Martin C.S. Wong, Eman Yee-man Leung, Sam C.C. Chun, Yunyang Deng, Thomas Lam, Raymond S.Y. Tang, Junjie Huang
Digestive and Liver Disease.2023; 55(12): 1742. CrossRef - Risk of recurrent advanced colorectal neoplasia in individuals with baseline non‐advanced neoplasia followed up at 5 vs 7–10 years
Martin C. S. Wong, Eman Yee‐man Leung, Sam C. C. Chun, Yunyang Deng, Thomas Lam, Raymond S. Y. Tang, Junjie Huang
Journal of Gastroenterology and Hepatology.2023; 38(12): 2122. CrossRef - Third Asia-Pacific consensus recommendations on colorectal cancer screening and postpolypectomy surveillance
Joseph J Y Sung, Han-Mo Chiu, David Lieberman, Ernst J Kuipers, Matthew D Rutter, Finlay Macrae, Khay-Guan Yeoh, Tiing Leong Ang, Vui Heng Chong, Sneha John, Jingnan Li, Kaichun Wu, Simon S M Ng, Govind K Makharia, Murdani Abdullah, Nozomu Kobayashi, Masa
Gut.2022; 71(11): 2152. CrossRef - Optimization of the surveillance strategy in patients with colorectal adenomas: A combination of clinical parameters and index colonoscopy findings
Chan Hyuk Park, Yoon Suk Jung, Nam Hee Kim, Jung Ho Park, Dong Il Park, Chong Il Sohn
Journal of Gastroenterology and Hepatology.2021; 36(4): 974. CrossRef - Increasing changes in visceral adiposity is associated with higher risk for colorectal adenoma: Multilevel analysis in a prospective cohort
Jung Min Moon, Jong Pil Im, Donghee Kim, Yoo Min Han, Hosim Soh, Ji Hyun Song, Sun Young Yang, Young Sun Kim, Jeong Yoon Yim, Seon Hee Lim, Joo Sung Kim
Journal of Gastroenterology and Hepatology.2021; 36(7): 1836. CrossRef - Strategies for colorectal cancer screening and post-polypectomy surveillance for young adults under age 50
Yoon Suk Jung
Precision and Future Medicine.2021; 5(2): 69. CrossRef - Adherence to Surveillance Guidelines after the Removal of Colorectal Polyps: A Multinational, Multicenter, Prospective Survey
Chang Kyo Oh, Satimai Aniwan, Panida Piyachaturawat, Zhiqin Wong, Thida Soe, Bayasgalan Luvsandagva, Quang Trung Tran, Achmad Fauzi, Jeong-Sik Byeon, Young-Seok Cho
Gut and Liver.2021; 15(6): 878. CrossRef - Colon Polyp Detection in Primary Health Care Institutions of Korea: Detection Rate and Issues with Following the Guidelines
Sang Hyun Park, Kwang Il Hong, Hyun Chul Park, Young Sun Kim, Gene Hyun Bok, Kyung Ho Kim, Dong Suk Shin, Jae Yong Han, Young Kwan Kim, Yeun Jong Choi, Soo Hoon Eun, Byung Hoon Lim, Kyeong Kun Kwack
The Korean Journal of Gastroenterology.2021; 78(6): 328. CrossRef - Effect of Cotinine-Verified Change in Smoking Status on Risk of Metachronous Colorectal Neoplasia After Polypectomy
Yoon Suk Jung, Nam Hee Kim, Mi Yeon Lee, Jung Ho Park, Dong Il Park, Chong Il Sohn
Clinical Gastroenterology and Hepatology.2020; 18(1): 163. CrossRef - Risk of developing metachronous advanced colorectal neoplasia after resection of low-risk diminutive versus small adenomas
Nam Hee Kim, Yoon Suk Jung, Jung Ho Park, Dong Il Park, Chong Il Sohn
Gastrointestinal Endoscopy.2020; 91(3): 622. CrossRef - Colorectal sessile serrated lesion with large size or synchronous neoplasm: a prospective study
Laxmi B. Chavali, Kun Hu, Anish Sheth, Nan Gao, Wei Xiong, Lanjing Zhang
European Journal of Gastroenterology & Hepatology.2020; 32(2): 199. CrossRef - Colorectal Polyp Prevalence According to Alcohol Consumption, Smoking and Obesity
Kyujin Lee, Yong Hwan Kim
International Journal of Environmental Research and Public Health.2020; 17(7): 2387. CrossRef - Comparative systematic review and meta-analysis of 1- to 5-mm versus 6- to 9-mm adenomas on the risk of metachronous advanced colorectal neoplasia
Yoon Suk Jung, Tae Jun Kim, Eunwoo Nam, Chan Hyuk Park
Gastrointestinal Endoscopy.2020; 92(3): 692. CrossRef - The current capacity and quality of colonoscopy in Korea
Jae Ho Choi, Jae Myung Cha, Jin Young Yoon, Min Seob Kwak, Jung Won Jeon, Hyun Phil Shin
Intestinal Research.2019; 17(1): 119. CrossRef - Appropriate Surveillance Interval after Colonoscopic Polypectomy in Patients Younger than 50 Years
Yoon Suk Jung, Nam Hee Kim, Jung Ho Park, Dong Il Park, Chong Il Sohn
Journal of Korean Medical Science.2019;[Epub] CrossRef - Terminology, Molecular Features, Epidemiology, and Management of Serrated Colorectal Neoplasia
Seth D. Crockett, Iris D. Nagtegaal
Gastroenterology.2019; 157(4): 949. CrossRef - Risk of Developing Metachronous Advanced Colorectal Neoplasia After Polypectomy in Patients With Multiple Diminutive or Small Adenomas
Nam Hee Kim, Yoon Suk Jung, Mi Yeon Lee, Jung Ho Park, Dong Il Park, Chong Il Sohn
American Journal of Gastroenterology.2019; 114(10): 1657. CrossRef - Visceral obesity as a risk factor for colorectal adenoma occurrence in surveillance colonoscopy
Jong Pil Im, Donghee Kim, Su Jin Chung, Eun Hyo Jin, Yoo Min Han, Min Jung Park, Ji Hyun Song, Sun Young Yang, Young Sun Kim, Jeong Yoon Yim, Seon Hee Lim, Joo Sung Kim
Gastrointestinal Endoscopy.2018; 88(1): 119. CrossRef - Guideline Adherence to Colonoscopic Surveillance Intervals after Polypectomy in Korea: Results from a Nationwide Survey
Seri Hong, Mina Suh, Kui Son Choi, Boyoung Park, Jae Myung Cha, Hyun-Soo Kim, Jae Kwan Jun, Dong Soo Han
Gut and Liver.2018; 12(4): 426. CrossRef - Risk factors of nonadherence to colonoscopy surveillance after polypectomy and its impact on clinical outcomes: a KASID multicenter study
Chung Hyun Tae, Chang Mo Moon, Seong-Eun Kim, Sung-Ae Jung, Chang Soo Eun, Jae Jun Park, Geom Seog Seo, Jae Myung Cha, Sung Chul Park, Jaeyoung Chun, Hyun Jung Lee, Yunho Jung, Jin Oh Kim, Young-Eun Joo, Dong Il Park
Journal of Gastroenterology.2017; 52(7): 809. CrossRef - Unusual Local Recurrence with Distant Metastasis after Successful Endoscopic Submucosal Dissection for Colorectal Mucosal Cancer
Hyo Jeong Lee, Byong Duk Ye, Jeong-Sik Byeon, Jihun Kim, Young Soo Park, Yong Sang Hong, Yong Sik Yoon, Dong-Hoon Yang
Clinical Endoscopy.2017; 50(1): 91. CrossRef - Determining the optimal surveillance interval after a colonoscopic polypectomy for the Korean population?
Jung Lok Lee, Jae Myung Cha, Hye Min Lee, Jung Won Jeon, Min Seob Kwak, Jin Young Yoon, Hyun Phil Shin, Kwang Ro Joo, Joung Il Lee, Dong Il Park
Intestinal Research.2017; 15(1): 109. CrossRef - Advanced Colonic Neoplasia at Follow-up Colonoscopy According to Risk Components and Adenoma Location at Index Colonoscopy: A Retrospective Study of 1,974 Asymptomatic Koreans
Su Jung Baik, Hyojin Park, Jae Jun Park, Hyun Ju Lee, So Young Jo, Yoo Mi Park, Hye Sun Lee
Gut and Liver.2017; 11(5): 667. CrossRef - The Serrated Polyp Pathway: Is It Time to Alter Surveillance Guidelines?
Brendon O’Connell, Nazar Hafiz, Seth Crockett
Current Gastroenterology Reports.2017;[Epub] CrossRef - Optimizing post‐polypectomy surveillance: A practical guide for the endoscopist
Roel Bogie, Silvia Sanduleanu
Digestive Endoscopy.2016; 28(3): 348. CrossRef - Cap-assisted EMR for rectal neuroendocrine tumors: comparisons with conventional EMR and endoscopic submucosal dissection (with videos)
Dong-Hoon Yang, Yangsoon Park, Sang Hyoung Park, Kyung-Jo Kim, Byong Duk Ye, Jeong-Sik Byeon, Seung-Jae Myung, Suk-Kyun Yang
Gastrointestinal Endoscopy.2016; 83(5): 1015. CrossRef - Colorectal cancer screening of the general population in East Asia
Yasushi Sano, Jeong‐Sik Byeon, Xiao‐Bo Li, Martin C.S. Wong, Han‐Mo Chiu, Rungsun Rerknimitr, Takahiro Utsumi, Santa Hattori, Wataru Sano, Mineo Iwatate, Philip Chiu, Joseph Sung
Digestive Endoscopy.2016; 28(3): 243. CrossRef - Surveillance colonoscopy after endoscopic treatment for colorectal neoplasia: From the standpoint of the Asia–Pacific region
Takahisa Matsuda, Han‐Mo Chiu, Yasushi Sano, Takahiro Fujii, Akiko Ono, Yutaka Saito
Digestive Endoscopy.2016; 28(3): 342. CrossRef - Long-Term Outcome and Surveillance Colonoscopy after Successful Endoscopic Treatment of Large Sessile Colorectal Polyps
Bun Kim, A Ra Choi, Soo Jung Park, Jae Hee Cheon, Tae Il Kim, Won Ho Kim, Sung Pil Hong
Yonsei Medical Journal.2016; 57(5): 1106. CrossRef - Probability of High-Risk Colorectal Neoplasm Recurrence Based on the Results of Two Previous Colonoscopies
Hye Won Park, Seungbong Han, Ji Young Lee, Hye-Sook Chang, Jaewon Choe, Yunsik Choi, Hoonsub So, Dong-Hoon Yang, Seung-Jae Myung, Suk-Kyun Yang, Jin-Ho Kim, Jeong-Sik Byeon
Digestive Diseases and Sciences.2015; 60(1): 226. CrossRef - Distribution of the Colonoscopic Adenoma Detection Rate According to Age: Is Recommending Colonoscopy Screening for Koreans Over the Age of 50 Safe?
Taeseok Bae, Yunhyung Ha, Changkyun Kim, Jihyun Lee, Kwangil Ha, Sanghyun Shin, Youngcheol Lee, Yoonsik Kang
Annals of Coloproctology.2015; 31(2): 46. CrossRef - Risk of adenomas with high‐risk characteristics based on two previous colonoscopy
Kang‐Heum Suh, Ja Seol Koo, Jong Jin Hyun, Jungsoon Choi, Jang Soo Han, Seung Young Kim, Sung Woo Jung, Yoon Tae Jeen, Sang Woo Lee, Jai Hyun Choi
Journal of Gastroenterology and Hepatology.2014; 29(12): 1985. CrossRef - Only the Size of Resected Polyps Is an Independent Risk Factor for Delayed Postpolypectomy Hemorrhage: A 10-Year Single-Center Case-Control Study
Hee Seok Moon, Sun Wook Park, Dong Hwan Kim, Sun Hyung Kang, Jae Kyu Sung, Hyun Yong Jeong
Annals of Coloproctology.2014; 30(4): 182. CrossRef - Prevalence of and Risk Factors for Gastrointestinal Diseases in Korean Americans and Native Koreans Undergoing Screening Endoscopy
Hee Sun Kim, Su Jung Baik, Kyung Hee Kim, Cho Rong Oh, Jung Hyun Lee, Wan Jae Jo, Hye Kyoung Kim, Eun Young Kim, Min Jung Kim
Gut and Liver.2013; 7(5): 539. CrossRef - Proximal colon cancer and serrated adenomas – hunting the missing 10%
Pelvender Gill, Hannah Rafferty, David Munday, Adam Bailey, Lai Mun Wang, James E East, Runjan Chetty, Simon J Leedham
Clinical Medicine.2013; 13(6): 557. CrossRef - Relationship of Non-Alcoholic Fatty Liver Disease to Colorectal Neoplasia
Jue Yong Lee, Ja Won Kim
Korean Journal of Medicine.2013; 84(3): 363. CrossRef - Highlights of International Digestive Endoscopy Network 2013
Kwang An Kwon, Il Ju Choi, Eun Young Kim, Seok Ho Dong, Ki Baik Hahm
Clinical Endoscopy.2013; 46(5): 425. CrossRef
- Post-colonoscopy colorectal cancers in a national fecal immunochemical test-based colorectal cancer screening program
- 10,175 View
- 161 Download
- 38 Crossref

- Postpolypectomy Colonoscopy Surveillance
- Hyun Soo Kim, M.D.
- Korean J Gastrointest Endosc 2009;39(5):257-264. Published online November 30, 2009
-
 Abstract
Abstract
 PDF
PDF - Colonoscopy and polypectomy are increasingly being used as the most effective interventions for preventing colorectal cancer (CRC), which has resulted in a growing cohort of patients who require postpolypectomy surveillance (PPS). The goal of PPS is to prevent the development of significant metachronous adenomas and CRCs. The surveillance interval depends on an accurate assessment of the individual patient's risk of developing subsequent colonic neoplasm. The newly developed consensus guidelines (CG) emphasize the concept of 'risk stratification' and these guidelines are more user-friendly than the previous ones, thus eliminate conflicting recommendations that are a barrier to physicians using the guideline. Despite the development of CGs, many specialists and non-specialists overutilize colonoscopy for PPS, which causes an ineffective large burden of cost and it strains already limited resources. The safest and most cost-effective approach by colonoscopists to preventing CRC is to maximize the effectiveness of colonoscopy for clearing the colon and then follow the recommended intervals between procedures, including extended intervals for the low-risk cohorts. Educating colonoscopists and the widespread implementation of continuous quality improvement programs are required to bridge the gap between the guidelines and their clinical application. (Korean J Gastrointest Endosc 2009;39:257-264)
- 2,189 View
- 17 Download

- Barrett's Esophagus - With Emphasis on Endoscopic Disgnosis
- Jun Haeng Lee, M.D.
- Korean J Gastrointest Endosc 2009;39(4):185-198. Published online October 30, 2009
-
 Abstract
Abstract
 PDF
PDF - Barrett's esophagus is a metaplastic change of the esophageal mucosa, such that the normal squamous epithelium is replaced by specialized columnar epithelium. During the last decades, there has been a significant change in the definition, endoscopic diagnosis, pathologic diagnosis, surveillance and management of Barrett's esophagus. Because of the rising prevalence of gastroesophgeal reflux disease in Korea, problems related to Barrett's esophagus are expected to be much more common in the near future. In this review, methods of endoscopic diagnosis of Barrett's esophagus are discussed in detail. Management strategies in the context of Korean epidemiology are also suggested. (Korean J Gastrointest Endosc 2009; 39:185-198)
- 2,212 View
- 12 Download

- A Survey on the Interval of Post-polypectomy Surveillance Colonoscopy
- Mun Su Kang, M.D., Dong Il Park, M.D., Jung Ho Park, M.D., Hong Joo Kim, M.D., Yong Kyun Cho, M.D., Chong Il Sohn, M.D., Woo Kyu Jeon, M.D. and Byung Ik Kim, M.D.
- Korean J Gastrointest Endosc 2006;33(6):339-345. Published online December 30, 2006
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: Colonoscopy is the golden standard used as a surveillance test and screen for colon cancer, and the current demand for colonoscopy exceeds its availability. This study is an assessment of the colonoscopic surveillance intervals currently practiced. Methods: A multiple choice survey of the colonoscopic surveillance interval used in six case scenarios [hyperplastic polyp; two 0.5 cm tubular adenomas (TAs); a 1.5 cm TA; 0.8 cm triple TAs; a 1.5 cm TA with high grade dysplasia; current normal exam after polypectomy of a <1 cm sized TA 3 years ago] was sent via e-mail to members of the KASID. Results: A total of 131 colonoscopists (104 men, 27 women) replied, and the mean age of the respondents was 36 years (range 28∼58). All respondents were board- certified in their respective specialties (internal medicine 75, general surgery 3, and GI subspecialty 53). When compared with the AGA guidelines, 90.1∼99.2% of the respondents performed the first post-polypectomy surveillance colonoscopy prematurely, and 75.6% of respondents performed the second surveillance prematurely. Conclusions: Most post-polypectomy surveillance colonoscopies were performed prematurely. It is quite possible that unnecessary surveillance may account for a significant portion of the demand for colonoscopy. (Korean J Gastrointest Endosc 2006;33:339345)
- 2,444 View
- 19 Download

- 원저 : 식도 위장관 ; 융모성 종양의 특성과 대책 ( Original Articles : Esophagus , Stomach & Intestine ; Tubulovillous and Villous Adenomas of the Colon and Rectum - Endoscopic Characteristics and Management - )
- Korean J Gastrointest Endosc 1998;18(4):506-519. Published online November 30, 1997
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: A villous tumor, histologically villous or tubulovillous adenoma, is a clinical challenge because of its higher potential for malignancy and higher recurrence rate. However, information and experience with these tumors in the Korean people is still lacking. For that reason, we designed this study to review and analyze the colonoscopic features, the potential for malignancy, and the treatiment with respect to the confirmation of guidelines for the accurate diagnosis and reasonable management of such tumors in the Korean population. Materials and Methods: We performed 753 polypectomies, including 4 transanal excisions and several bowel resections, from January 1996 to May 1997 at Song-Do Colorectal Hospital in Seoul, Among them, 447 cases (59.4%) were adenomas, comprising 405 (53.8%) tubular adenomas, 31 (4.1%) tubulovillous adenomas, and 11 (1.5%) villous adenomas. We analyzed the 42 (5.6%) tubulovillous and villous adenomas. (Korean J Gastraintest Endosc 18: 506-519, 1998) (continue)
- 1,547 View
- 2 Download


 KSGE
KSGE


 First
First Prev
Prev



