Articles
- Page Path
- HOME > Clin Endosc > Volume 48(3); 2015 > Article
- Original Article Diagnostic Accuracy of the Initial Endoscopy for Ampullary Tumors
- Hee Seung Lee1, Jong Soon Jang1, Seungho Lee1, Myeong Ho Yeon1, Ki Bae Kim1, Jae Geun Park1, Joo Young Lee1, Mi Jin Kim1, Joung-Ho Han1, Rohyun Sung2, Seon Mee Park1
-
Clinical Endoscopy 2015;48(3):239-246.
DOI: https://doi.org/10.5946/ce.2015.48.3.239
Published online: May 29, 2015
1Department of Internal Medicine, Medical Research Institute, Chungbuk National University College of Medicine, Cheongju, Korea.
2Department of Pathology, Medical Research Institute, Chungbuk National University College of Medicine, Cheongju, Korea.
- Correspondence: Seon Mee Park. Department of Internal Medicine, Chungbuk National University College of Medicine, 776 il sunhwan-ro, Heungdeok-gu, Cheongju 361-711, Korea. Tel: +82-43-269-6019, Fax: +82-43-273-3252, smpark@chungbuk.ac.kr
• Received: June 16, 2014 • Revised: August 4, 2014 • Accepted: August 5, 2014
Copyright © 2015 Korean Society of Gastrointestinal Endoscopy
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background/Aims
- Ampullary tumors come in a wide variety of malignant forms. We evaluated the diagnostic accuracy of endoscopy for ampullary tumors, and analyzed the causes of misdiagnosis.
-
Methods
- We compared endoscopic imaging and biopsy results to final diagnoses. Types of endoscope, numbers of biopsy specimens taken, and final diagnoses were evaluated as possible factors influencing diagnostic accuracy.
-
Results
- Final diagnoses were 19 adenocarcinomas, 18 normal or papillitis, 11 adenomas, two adenomyomas, one paraganglioma, and one neuroendocrine tumor. The diagnostic accuracy of endoscopic imaging or the initial biopsy was identical (67.3%). At least one test was concordant with the final diagnosis in all except two cases. Compared with the final diagnosis, endoscopic imaging tended to show more advanced tumors, whereas the initial biopsy revealed less advanced lesions. The diagnostic accuracy of the initial biopsy was influenced by the type of endoscope used and the final diagnosis, but not by the number of biopsies taken.
-
Conclusions
- Endoscopy has limited accuracy in the diagnosis of ampullary tumors. However, most cases with concordant endoscopic imaging and biopsy results are identical to the final diagnosis. Therefore, in cases where both of these tests disagree, re-evaluation with a side-viewing endoscope after resolution of papillitis is required.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
- 1. Hartel M, Wente MN, Sido B, Friess H, Büchler MW. Carcinoid of the ampulla of Vater. J Gastroenterol Hepatol 2005;20:676–681. 15853978.ArticlePubMed
- 2. Cho YS, Joo HJ, Seo EK, et al. A case of juxtapapillary gangliocytic paraganglioma treated with endoscopic resection. Korean J Med 2010;79:543–548.
- 3. Artaza T, Potenciano JM, Legaz M, Muñoz C, Talavera A, Sánchez E. Lymphangioma of Vater's ampulla: a rare cause of obstructive jaundice. Endoscopic therapy. Scand J Gastroenterol 1995;30:804–806. 7481550.ArticlePubMed
- 4. Culebras Fernández JM, González Bueno CM. Leiomyoma of Vater's ampulla. Rev Esp Enferm Apar Dig 1974;42:165–172. 4822683.PubMed
- 5. Choi YH, Kim MJ, Han JH, et al. Clinical, pathological, and immunohistochemical features of adenomyoma in the ampulla of vater. Korean J Gastroenterol 2013;62:352–358. 24365734.ArticlePubMed
- 6. Venu RP, Rolny P, Geenen JE, Hogan WJ, Komorowski RA. Ampullary hamartoma: endoscopic diagnosis and treatment. Gastroenterology 1991;100:795–798. 1993502.ArticlePubMed
- 7. Yamaguchi K, Enjoji M, Kitamura K. Endoscopic biopsy has limited accuracy in diagnosis of ampullary tumors. Gastrointest Endosc 1990;36:588–592. 2279648.ArticlePubMed
- 8. Rodríguez C, Borda F, Elizalde I, Jiménez Pérez FJ, Carral D. How accurate is preoperative diagnosis by endoscopic biopsies in ampullary tumours? Rev Esp Enferm Dig 2002;94:585–592. 12647408.PubMed
- 9. Menzel J, Poremba C, Dietl KH, Böcker W, Domschke W. Tumors of the papilla of Vater: inadequate diagnostic impact of endoscopic forceps biopsies taken prior to and following sphincterotomy. Ann Oncol 1999;10:1227–1231. 10586341.ArticlePubMedPDF
- 10. Elek G, Gyôri S, Tóth B, Pap A. Histological evaluation of preoperative biopsies from ampulla vateri. Pathol Oncol Res 2003;9:32–41. 12704445.ArticlePubMed
- 11. Grobmyer SR, Stasik CN, Draganov P, et al. Contemporary results with ampullectomy for 29 "benign" neoplasms of the ampulla. J Am Coll Surg 2008;206:466–471. 18308217.ArticlePubMed
- 12. Kimchi NA, Mindrul V, Broide E, Scapa E. The contribution of endoscopy and biopsy to the diagnosis of periampullary tumors. Endoscopy 1998;30:538–543. 9746162.ArticlePubMedPDF
- 13. DeOliveira ML, Triviño T, de Jesus Lopes Filho G. Carcinoma of the papilla of Vater: are endoscopic appearance and endoscopic biopsy discordant? J Gastrointest Surg 2006;10:1140–1143. 16966033.ArticlePubMed
- 14. Morales TG, Hixson LJ. Acute pancreatitis following endoscopic biopsy of the ampulla in a patient with Gardner's syndrome. Gastrointest Endosc 1994;40:367–369. 8056246.ArticlePubMed
- 15. Park JS, Kim MH, Lee SK, et al. The clinical significance of papillitis of the major duodenal papilla. Gastrointest Endosc 2002;55:877–882. 12024144.ArticlePubMed
- 16. Seifert E, Schulte F, Stolte M. Adenoma and carcinoma of the duodenum and papilla of Vater: a clinicopathologic study. Am J Gastroenterol 1992;87:37–42. 1728122.PubMed
- 17. Ponchon T, Berger F, Chavaillon A, Bory R, Lambert R. Contribution of endoscopy to diagnosis and treatment of tumors of the ampulla of Vater. Cancer 1989;64:161–167. 2471581.ArticlePubMed
- 18. Bourgeois N, Dunham F, Verhest A, Cremer M. Endoscopic biopsies of the papilla of Vater at the time of endoscopic sphincterotomy: difficulties in interpretation. Gastrointest Endosc 1984;30:163–166. 6735092.ArticlePubMed
- 19. Leese T, Neoptolemos JP, West KP, Talbot IC, Carr-Locke DL. Tumours and pseudotumours of the region of the ampulla of Vater: an endoscopic, clinical and pathological study. Gut 1986;27:1186–1192. 3781332.ArticlePubMedPMC
- 20. Choi YR, Han JH, Cho YS, et al. Efficacy of cap-assisted endoscopy for routine examining the ampulla of Vater. World J Gastroenterol 2013;19:2037–2043. 23599622.ArticlePubMedPMC
- 21. Sivak MV. Clinical and endoscopic aspects of tumors of the ampulla of Vater. Endoscopy 1988;20(Suppl 1):211–217. 3049059.ArticlePubMedPDF
- 22. Blackman E, Nash SV. Diagnosis of duodenal and ampullary epithelial neoplasms by endoscopic biopsy: a clinicopathologic and immunohistochemical study. Hum Pathol 1985;16:901–910. 4029945.ArticlePubMed
- 23. Kim S, Lee NK, Lee JW, et al. CT evaluation of the bulging papilla with endoscopic correlation. Radiographics 2007;27:1023–1038. 17620465.ArticlePubMed
- 24. Manta R, Conigliaro R, Castellani D, et al. Linear endoscopic ultrasonography vs magnetic resonance imaging in ampullary tumors. World J Gastroenterol 2010;16:5592–5597. 21105192.ArticlePubMedPMC
- 25. Kalady MF, Clary BM, Clark LA, et al. Clinical utility of positron emission tomography in the diagnosis and management of periampullary neoplasms. Ann Surg Oncol 2002;9:799–806. 12374664.ArticlePubMed
- 26. Uchiyama Y, Imazu H, Kakutani H, et al. New approach to diagnosing ampullary tumors by magnifying endoscopy combined with a narrow-band imaging system. J Gastroenterol 2006;41:483–490. 16799891.ArticlePubMed
- 27. Ito K, Fujita N, Noda Y, Kobayashi G, Horaguchi J. Diagnosis of ampullary cancer. Dig Surg 2010;27:115–118. 20551654.ArticlePubMed
- 28. Sauvanet A, Chapuis O, Hammel P, et al. Are endoscopic procedures able to predict the benignity of ampullary tumors? Am J Surg 1997;174:355–358. 9324155.ArticlePubMed
REFERENCES
Fig. 1
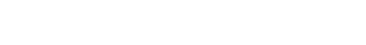
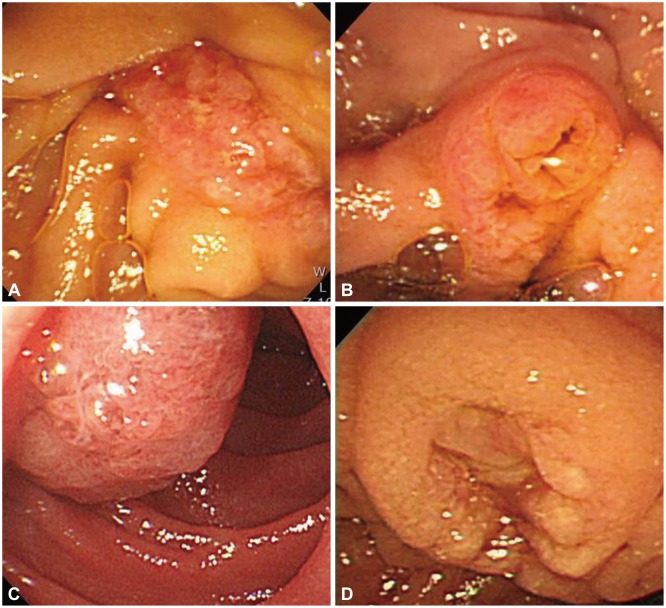
Representative endoscopic imaging of ampullary tumors. (A) Papillitis, bulging, and edematous papilla with petechia. (B) Adenoma, discolored lobular/pine cone like tumor. (C) Adenocarcinoma, a reddish coarse nodular tumor associated with erosion and ready bleeding. (D) Adenomyoma, an enlarged major papilla and villous granularities around the papillary orifice. (E) Paraganglioma, even and firm nodular mass with a granular and villous mucosa. (F) Neuroendocrine tumor, bulging of the papilla, which has a smooth surface.
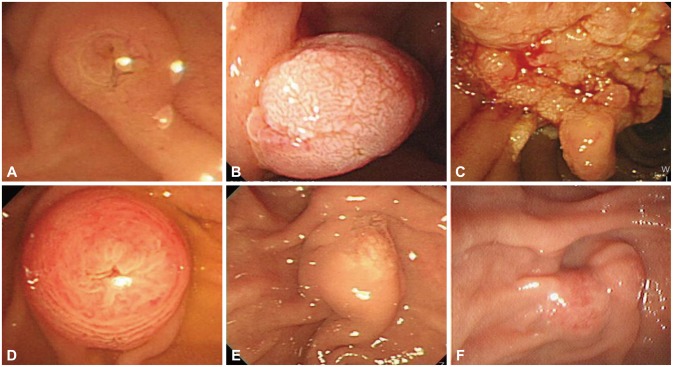
Fig. 2
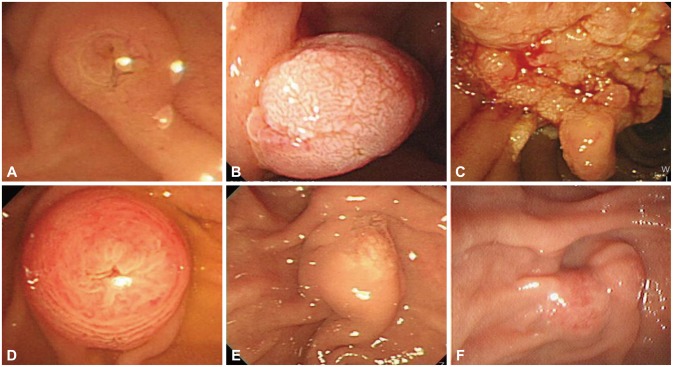
Representative pathologic findings of ampullary lesions. (A) Papillitis (H&E stain, ×200). (B) Tubular adenoma (H&E stain, ×50). (C) Villous adenoma (H&E stain, ×100). (D) Adenocarcinoma-intestinal type (H&E stain, ×100). (E) Adenocarcinoma-pancreaticobiliary type (H&E stain, ×100). (F) Adenomyoma (H&E stain, ×100). (G) Neuroendocrine tumor (H&E stain, ×100).
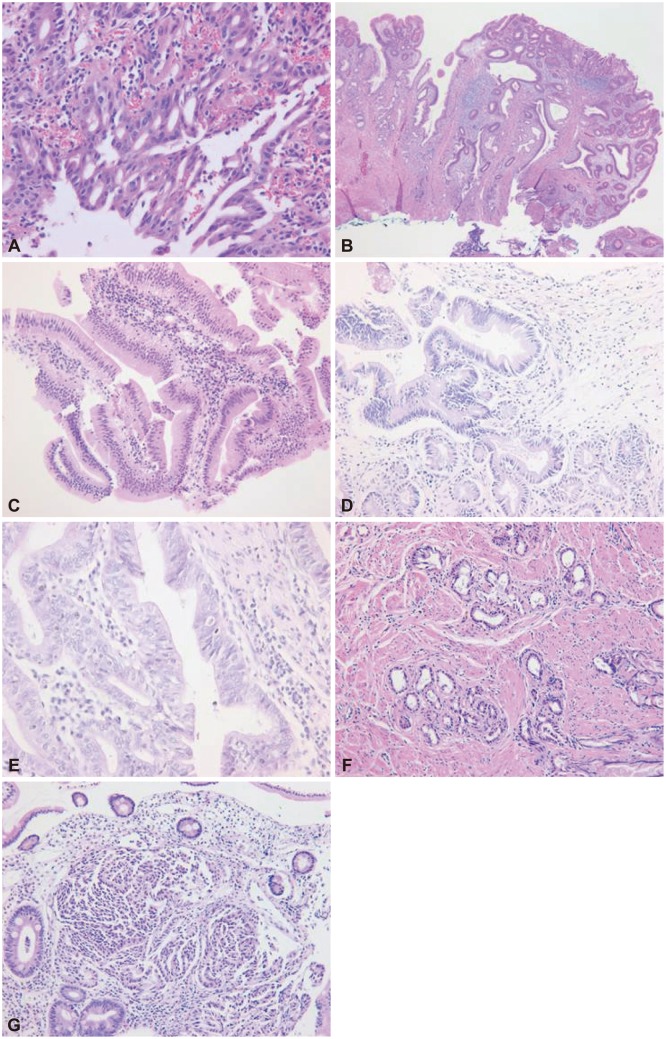
Fig. 3
Endoscopic images of misdiagnosed cases by gross appearance. (A, B) Papillitis misdiagnosed as adenoma. (C) Adenoma misdiagnosed as carcinoma. (D) Carcinoma misdiagnosed as adenoma.
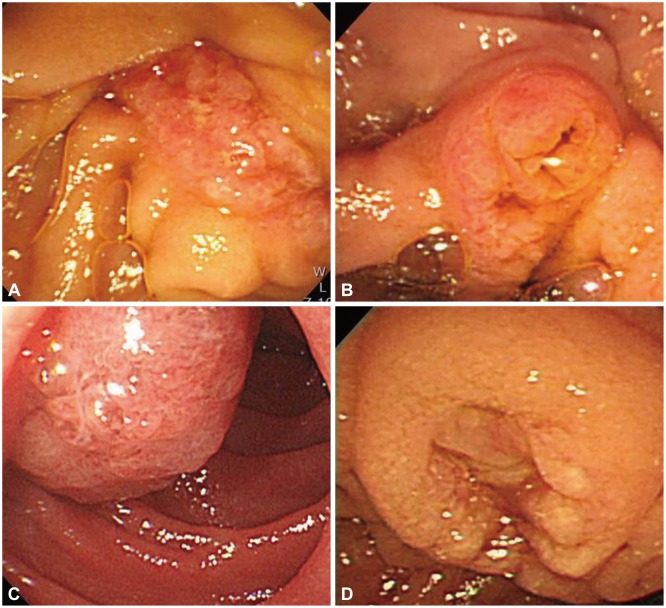
Fig. 4
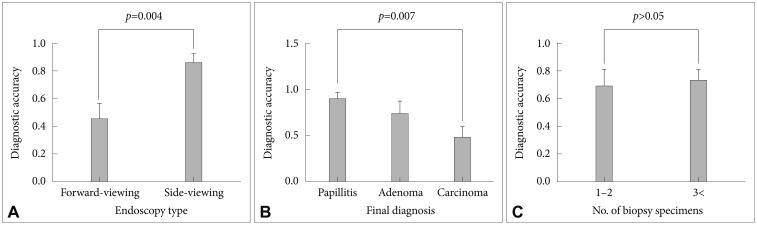
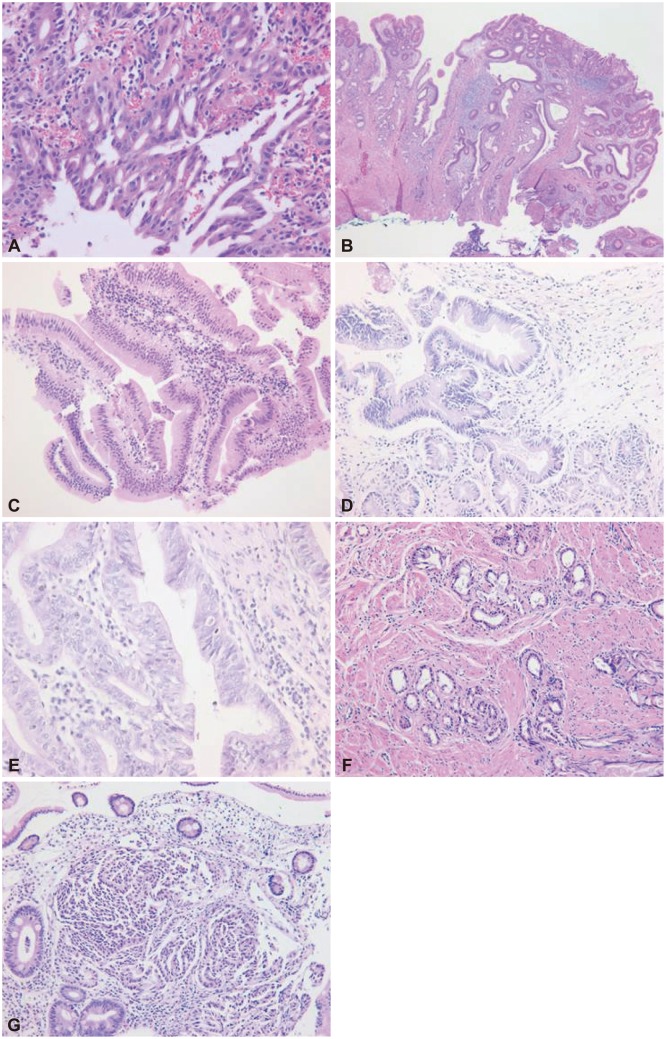
The diagnostic accuracy of biopsy was influenced by the type of endoscope used. (A) Side-viewing versus forward-viewing endoscope (85.7% vs. 45.0%, p=0.004). (B) Final diagnosis, normal or papillitis versus adenoma versus adenocarcinoma (88.9% vs. 72.7% vs. 47.4%, p=0.007). (C) Number of biopsy specimens (2 vs. ≥3, 56.3% vs. 75.0%; p>0.05).
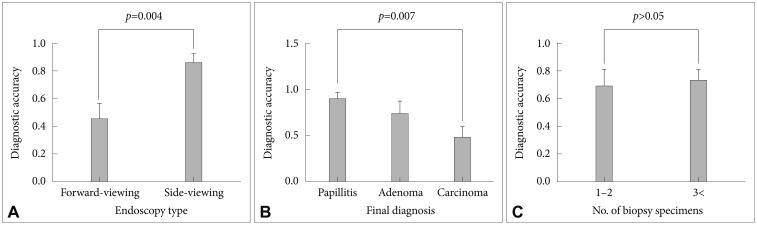
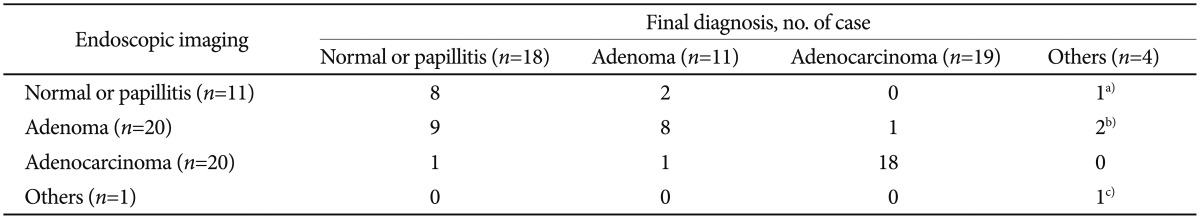
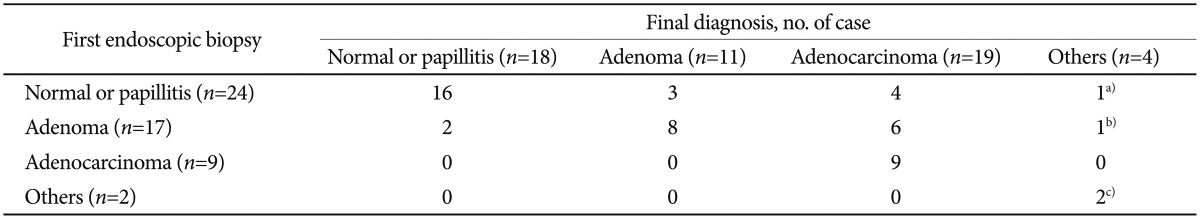
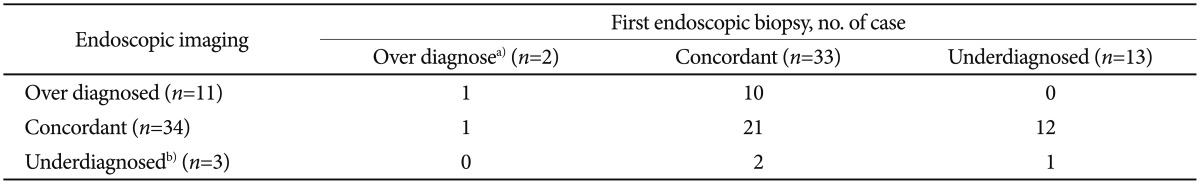
Table 4
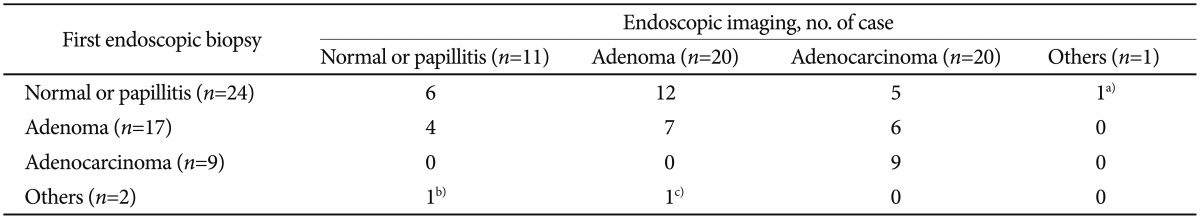
Comparison of Diagnosis by Endoscopic Imaging and First Biopsy in 52 Patients with Ampullary Tumors
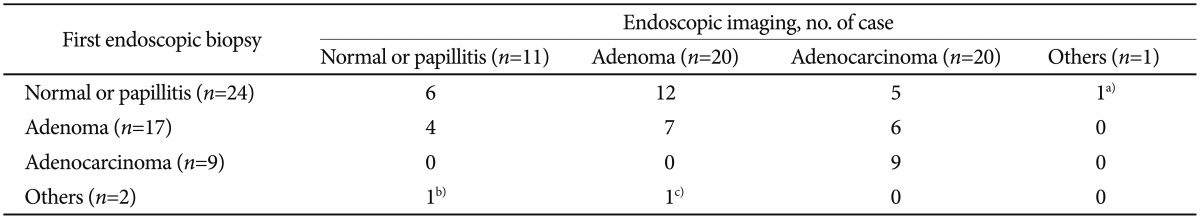
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Outcomes of endoscopic papillectomy of ampullary carcinoma and factors affecting additional surgery
Yoshihisa Takada, Takuya Ishikawa, Kentaro Yamao, Yasuyuki Mizutani, Tadashi Iida, Kota Uetsuki, Noriaki Gibo, Eizaburo Ohno, Hiroki Kawashima
Journal of Hepato-Biliary-Pancreatic Sciences.2024; 31(2): 110. CrossRef - The Optimal Cutoff Value of Tumor Markers for Prognosis Prediction in Ampullary Cancer
Seungho Lee, Hongbeom Kim, Heeju Sohn, Mirang Lee, Hyesol Jung, Youngjae Jo, Youngmin Han, Wooil Kwon, Jin-Young Jang
Cancers.2023; 15(8): 2281. CrossRef - Obstrucción biliar por adenomioma de la ampolla de Vater
Francisco Ramos-Muñoz, Luis Carlos Hinojosa-Arco, Jorge Francisco Roldán-de la Rúa, Ana Isabel García-Salguero, Miguel Ángel Suárez-Muñoz
Gastroenterología y Hepatología.2022; 45: 69. CrossRef - Adenomatous neoplasia in the papilla of Vater endoscopic and/or surgical resection?
Erik Haraldsson, Asif Halimi, Elena Rangelova, Roberto Valente, J. Matthias Löhr, Urban Arnelo
Surgical Endoscopy.2022; 36(4): 2401. CrossRef - Endoscopic Papillectomy
Sara Teles de Campos, Marco J. Bruno
Gastrointestinal Endoscopy Clinics of North America.2022; 32(3): 545. CrossRef - Efficacy and Safety of Exploring Deeper Sections of the Infrapapillary Area of the Duodenum by Using Sedative Esophagogastroduodenoscopy
Ming-Tse Hsu, Chi-Yi Chen, Kai-Sheng Liao, Wei-Sheng Chung, Tatsuya Toyokawa
Gastroenterology Research and Practice.2022; 2022: 1. CrossRef - Ampullary Adenocarcinoma: a Mini-Review and a Case Report of a Clinically Stable Disease Patient Treated with Herbal Supplements
Khin Maung Lwin, Ye Htut Linn, Yamin Kyaw Swar Dee
Journal of Gastrointestinal Cancer.2021; 52(2): 750. CrossRef - Proposed nomogram predicting neoplastic ampullary obstruction in patients with a suspected ampulla of Vater lesion on CT
Soo Young Jang, Jin Sil Kim, Seung Yon Baek, Hye Ah Lee, Jeong Kyong Lee
Abdominal Radiology.2021; 46(7): 3128. CrossRef - Long‐term outcomes of endoscopic papillectomy for early‐stage cancer in duodenal ampullary adenoma: Comparison to surgical treatment
Jun Seong Hwang, Hoonsub So, Dongwook Oh, Tae Jun Song, Do Hyun Park, Dong‐Wan Seo, Sung Koo Lee, Myung‐Hwan Kim, Seung‐Mo Hong, Jungho Yang, Sang Soo Lee
Journal of Gastroenterology and Hepatology.2021; 36(8): 2315. CrossRef - Endoscopic management of ampullary tumors: European Society of Gastrointestinal Endoscopy (ESGE) Guideline
Geoffroy Vanbiervliet, Marin Strijker, Marianna Arvanitakis, Arthur Aelvoet, Urban Arnelo, Torsten Beyna, Olivier Busch, Pierre H. Deprez, Lumir Kunovsky, Alberto Larghi, Gianpiero Manes, Alan Moss, Bertrand Napoleon, Manu Nayar, Enrique Pérez-Cuadrado-Ro
Endoscopy.2021; 53(04): 429. CrossRef - Predictive factor of recurrence after endoscopic papillectomy for ampullary neoplasms
Kosuke Takahashi, Eisuke Ozawa, Ichiro Yasuda, Naohiro Komatsu, Hisamitsu Miyaaki, Ken Ohnita, Takuji Yamao, Kazuo Oba, Tatsuki Ichikawa, Kazuhiko Nakao
Journal of Hepato-Biliary-Pancreatic Sciences.2021; 28(7): 625. CrossRef - Surgical ampullectomy: A comprehensive review
Darren L Scroggie, Vasileios K Mavroeidis
World Journal of Gastrointestinal Surgery.2021; 13(11): 1338. CrossRef - Endoscopic treatment of benign ampullary tumors
I.Y. Nedoluzhko, E.I. Khon, K.V. Shishin, L.V. Shumkina, N.A. Kurushkina
Dokazatel'naya gastroenterologiya.2021; 10(4): 67. CrossRef - Methods and outcome of the endoscopic treatment of ampullary tumors
Jan-Werner Poley, Sara Campos
Therapeutic Advances in Gastrointestinal Endoscopy.2020; 13: 263177451989978. CrossRef - Signet-ring cell carcinoma of the ampulla of Vater: a case diagnosed via repeated biopsies
Chisaki Ikeda, Naohiko Makino, Akiko Matsuda, Yasuharu Kakizaki, Tetsuya Ishizawa, Toshikazu Kobayashi, Shinpei Sugahara, Mayo Nishiduka, Michihiko Tsunoda, Junichiroh Haga, Rikiya Tsunoda, Yoshiyuki Ueno
Clinical Journal of Gastroenterology.2020; 13(4): 607. CrossRef - New experience of endoscopic papillectomy for ampullary neoplasms
Shuling Li, Zikai Wang, Fengchun Cai, Enqiang Linghu, Gang Sun, Xiangdong Wang, Jiangyun Meng, Hong Du, Yunsheng Yang, Wen Li
Surgical Endoscopy.2019; 33(2): 612. CrossRef - Differentiation of benign and malignant ampullary obstruction by multi-row detector CT
Wirana Angthong, Kran Jiarakoop, Kaan Tangtiang
Japanese Journal of Radiology.2018; 36(8): 477. CrossRef - How to Improve Diagnostic Accuracy in Suspicious Ampullary Lesions?
Woo Hyun Paik, Jin-Hyeok Hwang
Clinical Endoscopy.2015; 48(3): 185. CrossRef - Papilla biyopsisinin tanısal değeri
Ali Rıza KÖKSAL, Hüseyin ALKIM, Salih BOĞA, İlker ŞEN, Mehmet BAYRAM, Özgür BOSTANCI, Banu YILMAZ ÖZGÜVEN, Canan ALKIM
Endoskopi Gastrointestinal.2015; 23(2): 35. CrossRef
Diagnostic Accuracy of the Initial Endoscopy for Ampullary Tumors




Fig. 1 Representative endoscopic imaging of ampullary tumors. (A) Papillitis, bulging, and edematous papilla with petechia. (B) Adenoma, discolored lobular/pine cone like tumor. (C) Adenocarcinoma, a reddish coarse nodular tumor associated with erosion and ready bleeding. (D) Adenomyoma, an enlarged major papilla and villous granularities around the papillary orifice. (E) Paraganglioma, even and firm nodular mass with a granular and villous mucosa. (F) Neuroendocrine tumor, bulging of the papilla, which has a smooth surface.
Fig. 2 Representative pathologic findings of ampullary lesions. (A) Papillitis (H&E stain, ×200). (B) Tubular adenoma (H&E stain, ×50). (C) Villous adenoma (H&E stain, ×100). (D) Adenocarcinoma-intestinal type (H&E stain, ×100). (E) Adenocarcinoma-pancreaticobiliary type (H&E stain, ×100). (F) Adenomyoma (H&E stain, ×100). (G) Neuroendocrine tumor (H&E stain, ×100).
Fig. 3 Endoscopic images of misdiagnosed cases by gross appearance. (A, B) Papillitis misdiagnosed as adenoma. (C) Adenoma misdiagnosed as carcinoma. (D) Carcinoma misdiagnosed as adenoma.
Fig. 4 The diagnostic accuracy of biopsy was influenced by the type of endoscope used. (A) Side-viewing versus forward-viewing endoscope (85.7% vs. 45.0%, p=0.004). (B) Final diagnosis, normal or papillitis versus adenoma versus adenocarcinoma (88.9% vs. 72.7% vs. 47.4%, p=0.007). (C) Number of biopsy specimens (2 vs. ≥3, 56.3% vs. 75.0%; p>0.05).

 KSGE
KSGE

 PubReader
PubReader ePub Link
ePub Link Cite
Cite