Search
- Page Path
- HOME > Search
- Endoscopic stenting for malignant gastric outlet obstruction: focusing on comparison of endoscopic stenting and surgical gastrojejunostomy
- Sun Gyo Lim, Chan Gyoo Kim
- Received June 30, 2023 Accepted September 11, 2023 Published online February 23, 2024
- DOI: https://doi.org/10.5946/ce.2023.160 [Epub ahead of print]
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
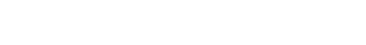
ePub - Malignant gastric outlet obstruction (GOO) is a condition characterized by blockage or narrowing where the stomach empties its contents into the small intestine due to primary malignant tumors or metastatic diseases. This condition leads to various symptoms such as nausea, vomiting, abdominal pain, and weight loss. To manage malignant GOO, different treatment options have been employed, including surgical gastrojejunostomy (SGJ), gastroduodenal stenting (GDS) using self-expandable metallic stent (SEMS), and endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ). This review focuses on comparing the clinical outcomes of endoscopic stenting (GDS and EUS-GJ) with SGJ for malignant GOO. Studies have shown that GDS with SEMS provides comparable clinical outcomes and safety for the palliation of obstructive symptoms. The choice between covered and uncovered SEMS remains controversial, as different studies have reported varying results. EUS-GJ, performed via endoscopic ultrasound guidance, has shown promising efficacy and safety in managing malignant GOO, but further studies are needed to establish it as the primary treatment option. Comparative analyses suggest that GDS has higher recurrence and reintervention rates compared to EUS-GJ and SGJ, with similar overall procedural complications. However, bleeding rates were lower with GDS than with SGJ. Randomized controlled trials are required to determine the optimal treatment approach for malignant GOO.
- 1,745 View
- 60 Download

-
Dedicated Cold Snare vs. Traditional Snare for Polypectomy of Diminutive and Small Lesions in a Porcine Model: A Research Group for Endoscopic Instruments and Stents (REIS) Study

- Han Hee Lee, Bo-In Lee, Jung-Wook Kim, Hyun Lim, Si Hyung Lee, Jun-Hyung Cho, Yunho Jung, Kyoung Oh Kim, Chan Gyoo Kim, Kee Myung Lee, Jong-Jae Park, Myung-Gyu Choi, Hoon Jai Chun, Ho Gak Kim
- Clin Endosc 2021;54(3):390-396. Published online September 10, 2020
- DOI: https://doi.org/10.5946/ce.2020.096
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: The aim of this in vivo animal study was to evaluate the effectiveness and safety of dedicated cold snare (DCS) compared with those of traditional snare (TS) for cold snare polypectomy (CSP).
Methods
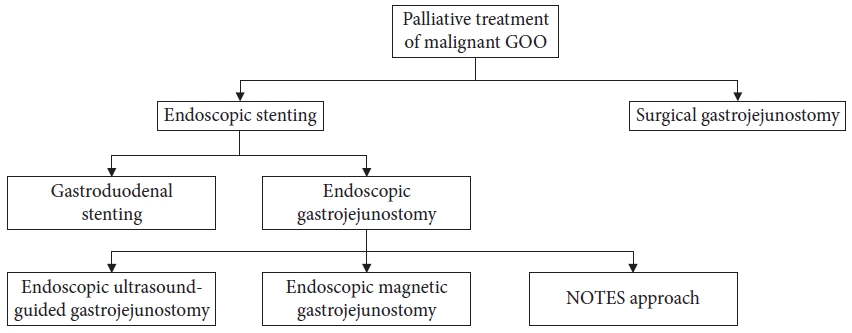
A total of 36 diminutive (5 mm) and 36 small (9 mm) pseudolesions were made by electrocoagulation in the colons of mini-pigs.
Results
For the diminutive lesions, there were no significant differences in technical success rate, procedure time, or complete resection rate between the DCS and TS groups; the rate of uneven resection margin in the DCS group was significantly lower than that of the TS group. For small lesions, technical success rate and complete resection rate were significantly higher in the DCS group than in the TS group (100% [18/18] vs. 55.6% [10/18], p=0.003; 94.4% [17/18] vs. 40% [4/10], p=0.006). In addition, the procedure duration was significantly shorter, and the rate of uneven resection margin was significantly lower in the DCS group (28.5 sec vs. 66.0 sec, p=0.006; 11.1% [2/18] vs. 100% [10/10], p<0.001). Two cases of perforation occurred in the DCS group. Multivariate analysis revealed that DCS use was independently associated with complete resection.
Conclusions
DCS is superior to TS in terms of technical success, complete resection, and reducing the duration of the procedure for CSP of small polyps. -
Citations
Citations to this article as recorded by- Comparison of complete resection rates in cold snare polypectomy using two different wire diameter snares: A randomized controlled study
Toshiki Horii, Sho Suzuki, Akihiro Sugita, Misa Yamauchi, Hisatomo Ikehara, Chika Kusano, Takuji Gotoda
Journal of Gastroenterology and Hepatology.2023; 38(5): 752. CrossRef - Comparison of the clinical efficacy of cold snare polypectomy using a thin-wire snare and thick-wire snare for small colorectal polyps
Hong Jin Yoon, Yunho Jung, Young Sin Cho, Il-Kwun Chung
International Journal of Gastrointestinal Intervention.2023; 12(4): 183. CrossRef - Big Issues on Small Polyps: An Ideal Device, But Is It for an Ideal Indication?
Yoji Takeuchi
Clinical Endoscopy.2021; 54(3): 297. CrossRef - Cold versus hot polypectomy/endoscopic mucosal resection–A review of current evidence
Raquel Ortigão, Jochen Weigt, Ahmed Afifi, Diogo Libânio
United European Gastroenterology Journal.2021; 9(8): 938. CrossRef
- Comparison of complete resection rates in cold snare polypectomy using two different wire diameter snares: A randomized controlled study
- 8,391 View
- 221 Download
- 4 Web of Science
- 4 Crossref

- Bleeding after Endoscopic Resection in Patients with End-Stage Renal Disease on Dialysis: A Multicenter Propensity Score-Matched Analysis
- In Kyung Yoo, Chan Gyoo Kim, Young Ju Suh, Younkyung Oh, Gwang Ho Baik, Sun Moon Kim, Young Dae Kim, Chul-Hyun Lim, Jung Won Jeon, Su Jin Hong, Byoung Wook Bang, Joon Sung Kim, Jun-Won Chung
- Clin Endosc 2020;53(4):452-457. Published online October 25, 2019
- DOI: https://doi.org/10.5946/ce.2019.107
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Frequent bleeding after endoscopic resection (ER) has been reported in patients with end-stage renal disease (ESRD). We aimed to evaluate the association and clinical significance of bleeding with ER in ESRD patients on dialysis.
Methods
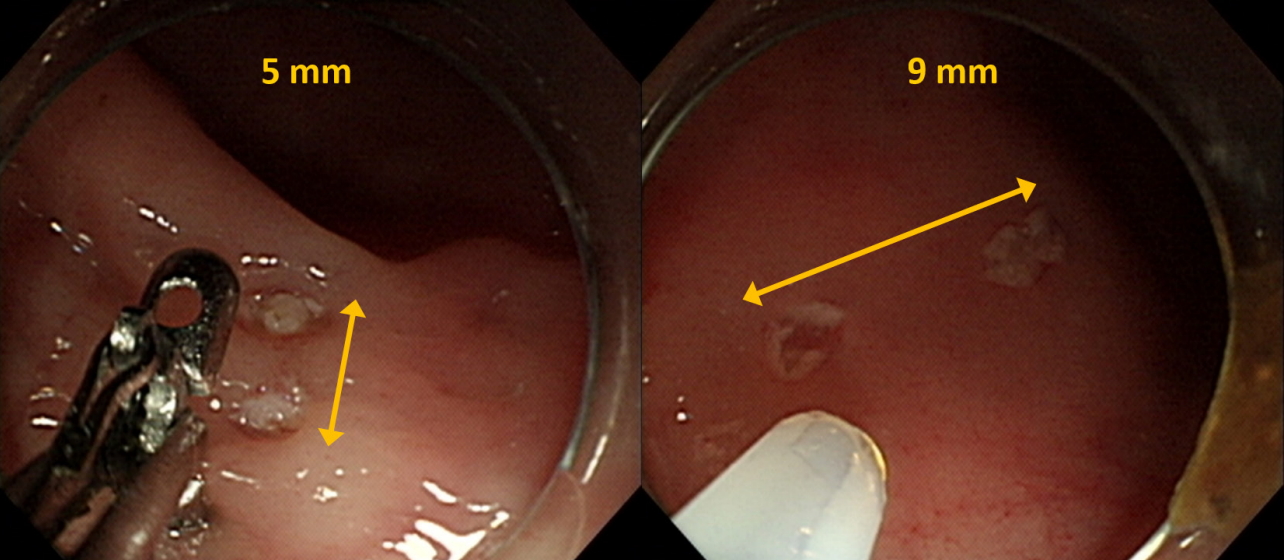
Between February 2008 and December 2018, 7,571 patients, including 47 ESRD patients on dialysis who underwent ER for gastric neoplasia, were enrolled. A total of 47 ESRDpatients on dialysis were propensity score-matched 1:10 to 470 non-ESRD patients, to adjust for between-group differences in variables such as age, sex, comorbidities, anticoagulation use, tumor characteristics, and ER method. Matching was performed using an optimal matching algorithm. For the matched data, clustered comparisons were performed using the generalized estimating equation method. Medical records were retrospectively reviewed. Frequency and outcomes of post-ER bleeding were evaluated.
Results
Bleeding was more frequent in the ESRD with dialysis group than in the non-ESRD group. ESRD with dialysis conferred a significant risk of post-ER bleeding (odds ratio, 6.1; 95% confidence interval, 2.7–13.6; p<0.0001). All post-ER bleeding events were controlled using endoscopic hemostasis except in 1 non-ESRD case that needed surgery.
Conclusions
ESRD with dialysis confers a bleeding risk after ER. However, all bleeding events could be managed endoscopically without sequelae. Concern about bleeding should not stop endoscopists from performing ER in ESRD patients on dialysis. -
Citations
Citations to this article as recorded by- Effect of renal insufficiency on the short‐ and long‐term outcomes of endoscopic submucosal dissection for early gastric cancer: Propensity score‐matched analysis
Tae‐Se Kim, Byung‐Hoon Min, Sun‐Young Baek, Kyunga Kim, Yang Won Min, Hyuk Lee, Poong‐Lyul Rhee, Jae J. Kim, Jun Haeng Lee
Digestive Endoscopy.2023; 35(7): 869. CrossRef - Safeness of Endoscopic Resection in Patients with End-Stage Renal Disease on Dialysis
Sun-Jin Boo
Clinical Endoscopy.2020; 53(4): 381. CrossRef
- Effect of renal insufficiency on the short‐ and long‐term outcomes of endoscopic submucosal dissection for early gastric cancer: Propensity score‐matched analysis
- 4,589 View
- 133 Download
- 2 Web of Science
- 2 Crossref

- Endoscopic Full-Thickness Resection Combined with Laparoscopic Surgery
- Chan Gyoo Kim
- Clin Endosc 2018;51(1):33-36. Published online January 12, 2018
- DOI: https://doi.org/10.5946/ce.2017.153
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic full-thickness resection combined with laparoscopic surgery was recently developed. These procedures could be categorized as “Cut first and then suture” and “Suture first and then cut”. “Cut first and then suture” includes laparoscopic and endoscopic cooperative surgery (LECS) and laparoscopy-assisted endoscopic full-thickness resection (LAEFR). Recent studies have demonstrated the safety and efficacy of LECS and LAEFR. However, these techniques are limited by the related exposure of the tumor and gastric mucosa to the peritoneal cavity and manipulation of these organs, which could lead to viable cancer cell seeding and the spillage of gastric juice into the peritoneal cavity. In the “Suture first and then cut” technique, the serosal side of the stomach is sutured to invert the stomach and subsequently endoscopic resection is performed. In this article, details of these techniques, including their advantages and limitations, are described.
-
Citations
Citations to this article as recorded by- ‘The parachute method’: A novel technique for laparoscopic tumour handling
Noriaki Kashu, Noriyuki Nishiwaki, Tetsuya Kagawa, Tomokazu Kakishita, Shinji Hato
Journal of Minimal Access Surgery.2024; 20(1): 111. CrossRef - Endoscopic Full Thickness Resection: A Systematic Review
Partha Pal, Mohan Ramchandani, Pradev Inavolu, Duvvuru Nageshwar Reddy, Manu Tandan
Journal of Digestive Endoscopy.2022; 13(03): 152. CrossRef - Choice of LECS Procedure for Benign and Malignant Gastric Tumors
Jae-Seok Min, Kyung Won Seo, Sang-Ho Jeong
Journal of Gastric Cancer.2021; 21(2): 111. CrossRef - Combined surgical and endoscopic approaches to full-thickness resection
Thomas C. Tsai, Ozanan R. Meireles
Techniques in Gastrointestinal Endoscopy.2019; 21(1): 26. CrossRef - Combined Laparoscopic-Endoscopic Techniques for Removal of Small Gastric Tumors: Advantages and Tricks
Eva Intagliata, Rosario Vecchio
Clinical Endoscopy.2019; 52(4): 390. CrossRef - Laparoscopic and endoscopic cooperative surgery for gastric tumors: Perspective for actual practice and oncological benefits
Yuki Aisu, Daiki Yasukawa, Yusuke Kimura, Tomohide Hori
World Journal of Gastrointestinal Oncology.2018; 10(11): 381. CrossRef
- ‘The parachute method’: A novel technique for laparoscopic tumour handling
- 5,757 View
- 201 Download
- 8 Web of Science
- 6 Crossref

- Efficacy of the Over-the-Scope Clip System for Treatment of Gastrointestinal Fistulas, Leaks, and Perforations: A Korean Multi-Center Study
- Hang Lak Lee, Joo Young Cho, Jun-Hyung Cho, Jong Jae Park, Chan Gyoo Kim, Seong Hwan Kim, Joung-Ho Han
- Clin Endosc 2018;51(1):61-65. Published online August 29, 2017
- DOI: https://doi.org/10.5946/ce.2017.027
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Currently, a new over-the-scope clip (OTSC) system has been introduced. This system has been used for gastrointestinal perforations and fistulas in other countries. The aim of our study is to examine the therapeutic success rate of endoscopic treatment using the OTSC system in Korea.
Methods
This was a multicenter prospective study. A total of seven endoscopists at seven centers performed this procedure.
Results
A total of 19 patients were included, with gastrointestinal leakages from anastomosis sites, fistulas, or esophageal perforations due to Boerhaave’s syndrome. Among these, there were three gastrojejunostomy sites, three esophagojejunostomy sites, four esophagogastrostomy sites, one esophagocolonostomy site, one jejuno-jejunal site, two endoscopic full thickness resection site closures, one Boerhaave’s syndrome, two esophago-bronchial fistulas, one gastrocolonic fistula, and one colonopseudocyst fistula. The size of the leakage ranged from 5 to 30 mm. The median procedure time was 16 min. All cases were technically successful. Complete closure of the leak was achieved in 14 of 19 patients using OTSC alone.
Conclusions
The OTSC system is a safe and effective method for the management of gastrointestinal leakage, especially in cases of anastomotic leakage after surgery. -
Citations
Citations to this article as recorded by- Bariatric surgery and reproduction-implications for gynecology and obstetrics
Isaac A. Babarinsa, Mohammed Bashir, Husham AbdelRahman Ahmed, Badreldeen Ahmed, Justin C. Konje
Best Practice & Research Clinical Obstetrics & Gynaecology.2023; 90: 102382. CrossRef - Current status in endoscopic management of upper gastrointestinal perforations, leaks and fistulas
Shannon Melissa Chan, Kitty Kit Ying Auyeung, Siu Fung Lam, Philip Wai Yan Chiu, Anthony Yuen Bun Teoh
Digestive Endoscopy.2022; 34(1): 43. CrossRef - Endoscopic vacuum therapy (EVT) for acute esophageal perforation: Could it replace surgery?
Petros Stathopoulos, Malte Zumblick, Sabine Wächter, Leif Schiffmann, Thomas M. Gress, Detlef Bartsch, Guido Seitz, Ulrike W. Denzer
Endoscopy International Open.2022; 10(05): E686. CrossRef - Acquired Benign Tracheoesophageal Fistula
Hasnain S. Bawaadam, Matthew Russell, Yaron B. Gesthalter
Journal of Bronchology & Interventional Pulmonology.2022; 29(3): e38. CrossRef - Exclusión pilórica con dispositivo Ovesco (over-thescope) en caso de fístula yeyunal en obstrucción duodenal de etiología maligna
Raul Eduardo Pinilla Morales, Helena Facundo Navia, Elio Fabio Sánchez Cortés, Ivette C. Jiménez Lafourie, Álvaro Eduardo Sánchez Hernández, Luis Carlos Llorente Portillo
Revista colombiana de Gastroenterología.2022; 37(3): 320. CrossRef - Endoscopic management of leaks and fistulas after bariatric surgery: a systematic review and meta-analysis
Pawel Rogalski, Agnieszka Swidnicka-Siergiejko, Justyna Wasielica-Berger, Damian Zienkiewicz, Barbara Wieckowska, Eugeniusz Wroblewski, Andrzej Baniukiewicz, Magdalena Rogalska-Plonska, Grzegorz Siergiejko, Andrzej Dabrowski, Jaroslaw Daniluk
Surgical Endoscopy.2021; 35(3): 1067. CrossRef - Endoscopic management of gastro‐bronchial fistula following two‐stage esophagectomy using over‐the‐scope‐clip (OTSC): Case series
Chih Y. Tan, Htet A. Kyaw, Neda Farhangmehr, Cheuk‐Bong Tang, Naga V. Jayanthi
Advances in Digestive Medicine.2021; 8(2): 84. CrossRef - Over-the-Scope Clip Closure of Persistent Gastrocutaneous Fistula After Percutaneous Endoscopic Gastrostomy Tube Removal: A Report of Two Cases
Shigenori Masaki, Keishi Yamada
Cureus.2021;[Epub] CrossRef - Over‐the‐scope clip: a novel approach to the management of a colorectal anastomotic leak
Stephanie G. Jordan, Gregory J. Nolan
ANZ Journal of Surgery.2021; 91(11): 2534. CrossRef - Conservative treatment of patients with small bowel fistula
A.V. Vodyasov, D.M. Kopaliani, P.A. Yartsev, O.Kh. Kaloeva
Khirurgiya. Zhurnal im. N.I. Pirogova.2021; (4): 78. CrossRef - An Approach to Accelerate Healing and Shorten the Hospital Stay of Patients With Anastomotic Leakage After Esophagectomy: An Explorative Study of Systematic Endoscopic Intervention
LeQi Zhong, JiuDi Zhong, ZiHui Tan, YiTong Wei, XiaoDong Su, ZheSheng Wen, TieHua Rong, Yi Hu, KongJia Luo
Frontiers in Oncology.2021;[Epub] CrossRef - AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review
Jeffrey H. Lee, Prashant Kedia, Stavros N. Stavropoulos, David Carr-Locke
Clinical Gastroenterology and Hepatology.2021; 19(11): 2252. CrossRef - Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clinical Endoscopy.2021; 54(5): 633. CrossRef - Diagnostic challenge and surgical management of Boerhaave’s syndrome: a case series
Jiayue Wang, Degang Wang, Jianjiao Chen
Journal of Medical Case Reports.2021;[Epub] CrossRef - Over-the-scope clip management of non-acute, full-thickness gastrointestinal defects
David J. Morrell, Joshua S. Winder, Ansh Johri, Salvatore Docimo, Ryan M. Juza, Samantha R. Witte, Vamsi V. Alli, Eric M. Pauli
Surgical Endoscopy.2020; 34(6): 2690. CrossRef - Use of the Over the Scope Clip to Close Perforations and Fistulas
Panida Piyachaturawat, Parit Mekaroonkamol, Rungsun Rerknimitr
Gastrointestinal Endoscopy Clinics of North America.2020; 30(1): 25. CrossRef - Therapie der Ösophagusleckagen
Jutta Weber-Eibel
Journal für Gastroenterologische und Hepatologische Erkrankungen.2020; 18(1): 8. CrossRef - Successful Closure of a Benign Refractory Tracheoesophageal Fistula Using an Over-the-Scope Clip after Failed Esophageal Stent Placement and Surgical Management
Nonthalee Pausawasdi, Chotirot Angkurawaranon, Tanyaporn Chantarojanasiri, Arunchai Chang, Wanchai Wongkornrat, Somchai Leelakusolvong, Asada Methasate
Clinical Endoscopy.2020; 53(3): 361. CrossRef - Clinical efficacy of the over-the-scope clip device: A systematic review
Nicholas Bartell, Krystle Bittner, Vivek Kaul, Truptesh H Kothari, Shivangi Kothari
World Journal of Gastroenterology.2020; 26(24): 3495. CrossRef - Endoscopic devices and techniques for the management of bariatric surgical adverse events (with videos)
Allison R. Schulman, Rabindra R. Watson, Barham K. Abu Dayyeh, Manoop S. Bhutani, Vinay Chandrasekhara, Pichamol Jirapinyo, Kumar Krishnan, Nikhil A. Kumta, Joshua Melson, Rahul Pannala, Mansour A. Parsi, Guru Trikudanathan, Arvind J. Trindade, John T. Ma
Gastrointestinal Endoscopy.2020; 92(3): 492. CrossRef - Gastrointestinal tract injuries after thermal ablative therapies for hepatocellular carcinoma: A case report and review of the literature
Teresa Marzia Rogger, Andrea Michielan, Sandro Sferrazza, Cecilia Pravadelli, Luisa Moser, Flora Agugiaro, Giovanni Vettori, Sonia Seligmann, Elettra Merola, Marcello Maida, Francesco Antonio Ciarleglio, Alberto Brolese, Giovanni de Pretis
World Journal of Gastroenterology.2020; 26(35): 5375. CrossRef - Over‐the‐scope clip system: A review of 1517 cases over 9 years
Hideki Kobara, Hirohito Mori, Noriko Nishiyama, Shintaro Fujihara, Keiichi Okano, Yasuyuki Suzuki, Tsutomu Masaki
Journal of Gastroenterology and Hepatology.2019; 34(1): 22. CrossRef - Recent advancements in the minimally invasive management of esophageal perforation, leaks, and fistulae
Shirin Siddiqi, Dean P. Schraufnagel, Hafiz Umair Siddiqui, Michael J. Javorski, Adam Mace, Abdulrhman S. Elnaggar, Haytham Elgharably, Patrick R. Vargo, Robert Steffen, Saad M. Hasan, Siva Raja
Expert Review of Medical Devices.2019; 16(3): 197. CrossRef - Diagnosis and endoscopic treatment of esophageal leakage: a systematic review
Bram D. Vermeulen, Peter D. Siersema
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 58. CrossRef - Management of esophagojejunal anastomosis leakage after total gastrectomy
Pablo Priego, Pietro Giordano, Marta Cuadrado, Araceli Ballestero, Julio Galindo, Eduardo Lobo
European Surgery.2018; 50(6): 262. CrossRef - Endoluminal Therapies for Esophageal Perforations and Leaks
Jeffrey R. Watkins, Alexander S. Farivar
Thoracic Surgery Clinics.2018; 28(4): 541. CrossRef - Esophageal leaks: I thought that glue was not effective
Ignacio Fernández-Urién, Juan Vila
Endoscopy International Open.2018; 06(09): E1100. CrossRef
- Bariatric surgery and reproduction-implications for gynecology and obstetrics
- 7,580 View
- 324 Download
- 26 Web of Science
- 27 Crossref

- Endoscopic Removal of a Migrated Coil after Embolization of a Splenic Pseudoaneurysm: A Case Report
- Yoo Min Han, Jong Yeul Lee, Il Ju Choi, Chan Gyoo Kim, Soo-Jeong Cho, Jun Ho Lee, Hyun Beom Kim, Ji Min Choi
- Clin Endosc 2014;47(2):183-187. Published online March 31, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.2.183
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Splenic artery pseudoaneurysms can be caused by pancreatitis, trauma, or operation. Traditionally, the condition has been managed through surgery; however, nowadays, transcatheter arterial embolization is performed safely and effectively. Nevertheless, several complications of pseudoaneurysm embolization have been reported, including coil migration. Herein, we report a case of migration of the coil into the jejunal lumen after transcatheter arterial embolization of a splenic artery pseudoaneurysm. The migrated coil was successfully removed by performing endoscopic intervention.
-
Citations
Citations to this article as recorded by- Gastric Bleeding Caused by Migrated Coil: A Rare Complication of Splenic Artery Coil Embolization
Tian Li, Bayan Alsuleiman, Manuel Martinez
Gastro Hep Advances.2022; 1(1): 67. CrossRef - Down to the Wire: A Case of Gastrointestinal Bleeding After Splenic Artery Coiling
John P. Haydek, Augustin R. Attwell
ACG Case Reports Journal.2022; 9(7): e00835. CrossRef - Intraluminal Endovascular Coil Migration: A Rare Complication Post-Embolization of the Gastroduodenal Artery for a Previously Bleeding Duodenal Ulcer
Yassin Naga, Mahendran Jayaraj, Yousif Elmofti, Annie Hong, Gordon Ohning
Cureus.2021;[Epub] CrossRef - Wire from the major papilla: Migration of endovascular coil into the main pancreatic duct
Sho Kitagawa, Shori Ishikawa, Hiroyuki Miyakawa
Digestive Endoscopy.2021;[Epub] CrossRef - Injectable hydrogels for vascular embolization and cell delivery: The potential for advances in cerebral aneurysm treatment
Seungil Kim, Kamil W. Nowicki, Bradley A. Gross, William R. Wagner
Biomaterials.2021; 277: 121109. CrossRef - A Rare Case of Coil Migration into the Duodenum after Embolization of a Right Colic Artery Pseudoaneurysm
Jeongmin Choi, Young Moon Kim
Clinical Endoscopy.2021; 54(6): 920. CrossRef - Embolization coil migration in the stomach and spontaneous excretion: a case report and review of the literature
Yasuo Matsubara, Lay Ahyoung Lim, Yasuki Hijikata, Yoshihiro Hirata, Hiroshi Yotsuyanagi
Radiology Case Reports.2020; 15(7): 1018. CrossRef - Migration of Gastric Varix Coil After Balloon-Occluded Antegrade Transvenous Obliteration
Antoinette J. Pusateri, Mina S. Makary, Khalid Mumtaz
ACG Case Reports Journal.2020; 7(10): e00472. CrossRef - Clinical Outcome of the Visible Coil During Endoscopy After Transcatheter Arterial Embolization for Gastrointestinal Bleeding
Jong-Joon Shim, Hee Ho Chu, Ji Hoon Shin, Jong Woo Kim, Do Hoon Kim, Hwoon-Yong Jung, Ji Yong Ahn
CardioVascular and Interventional Radiology.2019; 42(11): 1537. CrossRef - Migrated embolization coil causes intestinal obstruction
W. Preston Hewgley, David L. Webb, H. Edward Garrett
Journal of Vascular Surgery Cases, Innovations and Techniques.2018; 4(1): 8. CrossRef - Laparoscopic endoscopic combined surgery for removal of migrated coil after embolization of ruptured splenic artery aneurysm
Akshay Pratap, Bhavani Pokala, Luciano M Vargas, Dmitry Oleynikov, Vishal Kothari
Journal of Surgical Case Reports.2018;[Epub] CrossRef - Coil Migration to the Duodenum 1 Year Following Embolisation of a Ruptured Giant Common Hepatic Artery Aneurysm
Yoshikatsu Nomura, Yasuko Gotake, Takuya Okada, Masato Yamaguchi, Koji Sugimoto, Yutaka Okita
EJVES Short Reports.2018; 39: 33. CrossRef - Surgical Removal of Migrated Coil after Embolization of Jejunal Variceal Bleeding: A Case Report
Junhwan Kim, Danbi Lee, Kyunghwan Oh, Mingee Lee, Seol So, Dong-Hoon Yang, Chan-Wook Kim, Dong Il Gwon, Young-Hwa Chung
The Korean Journal of Gastroenterology.2017; 69(1): 74. CrossRef - Vascular coil erosion into hepaticojejunostomy following hepatic arterial embolisation
Soondoos Raashed, Manju D Chandrasegaram, Khaled Alsaleh, Glen Schlaphoff, Neil D Merrett
BMC Surgery.2015;[Epub] CrossRef
- Gastric Bleeding Caused by Migrated Coil: A Rare Complication of Splenic Artery Coil Embolization
- 7,626 View
- 61 Download
- 12 Web of Science
- 14 Crossref

- Tissue Acquisition in Gastric Epithelial Tumor Prior to Endoscopic Resection
- Chan Gyoo Kim
- Clin Endosc 2013;46(5):436-440. Published online September 30, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.5.436
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Endoscopic forceps biopsy is essential before planning an endoscopic resection of upper gastrointestinal epithelial tumors. However, forceps biopsy is limited by its superficiality and frequency of sampling errors. Histologic discrepancies between endoscopic forceps biopsies and resected specimens are frequent. Factors associated with such histologic discrepancies are tumor size, macroscopic type, surface color, and the type of medical facility. Precise targeting of biopsies is recommended to achieve an accurate diagnosis, curative endoscopic resection, and a satisfactory oncologic outcome. Multiple deep forceps biopsies can induce mucosal ulceration in early gastric cancer. Endoscopic resection for early gastric cancer with ulcerative findings is associated with piecemeal resection, incomplete resection, and a risk for procedure-related complications such as bleeding and perforation. Such active ulcers caused by forceps biopsy and following submucosal fibrosis might also be mistaken as an indication for more aggressive procedures, such as gastrectomy with D2 lymph node dissection. Proton pump inhibitors might be prescribed to facilitate the healing of biopsy-induced ulcers if an active ulcer is predicted after deep biopsy. It is unknown which time interval from biopsy to endoscopic resection is appropriate for a safe procedure and a good oncologic outcome. Further investigations are needed to conclude the appropriate time interval.
-
Citations
Citations to this article as recorded by- Success rate of current human-derived gastric cancer organoids establishment and influencing factors: A systematic review and meta-analysis
Kai-Lin Jiang, Xiang-Xiang Wang, Xue-Jiao Liu, Li-Kun Guo, Yong-Qi Chen, Qing-Ling Jia, Ke-Ming Yang, Jiang-Hong Ling
World Journal of Gastrointestinal Oncology.2024; 16(4): 1626. CrossRef - Clinical value and influencing factors of establishing stomach cancer organoids by endoscopic biopsy
Jie Li, Yan Chen, Yingyi Zhang, Xiaobo Peng, Meihong Wu, Ling Chen, Xianbao Zhan
Journal of Cancer Research and Clinical Oncology.2023; 149(7): 3803. CrossRef - Chinese integrated guideline on the management of gastric precancerous conditions and lesions
Ping Wang, Peng Li, Yingxuan Chen, Li Li, Yuanyuan Lu, Weixun Zhou, Liqun Bian, Beihua Zhang, Xiaolan Yin, Junxiang Li, Jie Chen, Shutian Zhang, Yongquan Shi, Xudong Tang
Chinese Medicine.2022;[Epub] CrossRef - Clinical applicability of gastroscopy with narrow-band imaging for the diagnosis of Helicobacter pylori gastritis, precancerous gastric lesion, and neoplasia
Jun-Hyung Cho, Seong Ran Jeon, So-Young Jin
World Journal of Clinical Cases.2020; 8(14): 2902. CrossRef - Gastric Cancer Caused by Adenoma: Predictive Factors Associated with Lesions Other Than the Expanded Indications
Seong Hwan Park, Kee Don Choi, Kyoungwon Jung, Yangsoon Park, Sunpyo Lee, Eun Jeong Gong, Hee Kyong Na, Ji Yong Ahn, Kee Wook Jung, Jeong Hoon Lee, Do Hoon Kim, Ho June Song, Gin Hyug Lee, Hwoon-Yong Jung
Gut and Liver.2018; 12(3): 246. CrossRef - Risk factors associated with histological upgrade of gastric low‐grade dysplasia on pretreatment biopsy
Lang Yang, Peng Jin, Xin Wang, Tong Zhang, Yu Qi He, Xiao Jun Zhao, Na Li, Guang Zhi Yang, Jian Qiu Sheng
Journal of Digestive Diseases.2018; 19(10): 596. CrossRef - Endoscopic predictors for undifferentiated histology in differentiated gastric neoplasms prior to endoscopic resection
Ji Min Choi, Sang Gyun Kim, Hyo-Joon Yang, Joo Hyun Lim, Jeongmin Choi, Jong Pil Im, Joo Sung Kim, Woo Ho Kim, Hyun Chae Jung
Surgical Endoscopy.2016; 30(1): 89. CrossRef - Guidance on the effective use of upper gastrointestinal histopathology
Maurice B Loughrey, Brian T Johnston
Frontline Gastroenterology.2014; 5(2): 88. CrossRef - Endoscopic features suggesting gastric cancer in biopsy-proven gastric adenoma with high-grade neoplasia
Jung Ho Kim
World Journal of Gastroenterology.2014; 20(34): 12233. CrossRef
- Success rate of current human-derived gastric cancer organoids establishment and influencing factors: A systematic review and meta-analysis
- 5,529 View
- 36 Download
- 9 Crossref


 KSGE
KSGE

 First
First Prev
Prev