Search
- Page Path
- HOME > Search
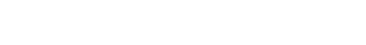
- Technical Reports of Endoscopic Retrograde Cholangiopancreatography Guidewires on the Basis of Physical Properties
- Chang-Il Kwon, Dong Hee Koh, Tae Jun Song, Won Suk Park, Dong Hang Lee, Seok Jeong
- Clin Endosc 2020;53(1):65-72. Published online August 6, 2019
- DOI: https://doi.org/10.5946/ce.2019.114
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Using an appropriate guidewire can increase the success rate of selective cannulation in endoscopic retrograde cholangiopancreatography. The purpose of this technical study was to investigate the characteristics of each guidewire type and to evaluate its efficiency and rapidity of insertion.
Methods
We conducted a three-point bending test using a universal testing machine to investigate the flexibility and bending features of each guidewire. 3D-printed silicone tubes with various types of stricture and a hand-made biliary tree silicone model with six-stranded intrahepatic ducts were used to evaluate the success rate and insertion time of each guidewire.
Results
In the three-point bending test, the characteristics of each guidewire were classified. We found that the bending strengths and times were independent of shaft thickness. Using two in vitro biliary duct models, we determined that the success rate and total insertion time were better for guidewires with a resilient shaft and angled tip than for other types of guidewires (p<0.001). Although thickness of the guidewire affected the success rate (p<0.05), it did not affect the total insertion time (p≥0.05).
Conclusions
Among several types of guidewire, some factors (resilient shaft, highly flexible, and angled tip) appeared to be associated with the efficiency and rapidity of the guidewire insertion. -
Citations
Citations to this article as recorded by- Structural factors influencing the clinical performance of 0.025-inch guidewires for pancreatobiliary endoscopy: An experimental study
Takehiko Koga, Naoaki Tsuchiya, Yusuke Ishida, Takanori Kitaguchi, Keisuke Matsumoto, Makoto Fukuyama, Satoki Kojima, Norihiro Kojima, Fumihito Hirai
Endoscopy International Open.2024; 12(05): E666. CrossRef - Guidewire Impaction in the Main Pancreatic Duct in a Patient with Chronic Pancreatitis: A Case Report
Soyoung Kim, Hoonsub So, Seok Won Jung, Sung Jo Bang
The Korean Journal of Gastroenterology.2023; 81(1): 36. CrossRef - Efficacy of a newly developed guidewire for selective biliary access
Do Hyun Park, Joung-Ho Han, Tae Hoon Lee, Jae Kook Yang, Ji Sung Lee, Yong Hun Lee, Mamoru Takenaka, Sang-Heum Park
Scientific Reports.2023;[Epub] CrossRef - Efficacy of a Newly Developed Guidewire for Selective Biliary Cannulation: A Multicenter Randomized Controlled Trial
Sung Yong Han, Sung Ill Jang, Dong Hee Koh, Jong Hyun Lee, Dong Uk Kim, Jae Hee Cho, Kyong Joo Lee, Seong-Hun Kim, Min Je Sung, Chang-Il Kwon
Journal of Clinical Medicine.2023; 12(10): 3440. CrossRef - Comparison of Two Types of Guidewires for Malignant Hilar Biliary Obstruction by Endoscopic Retrograde Cholangiopancreatography: A Randomized Controlled Trial
Sung Yong Han, Jung Wan Choe, Dong Uk Kim, Jong Jin Hyun, Joung-Ho Han, Hoonsub So, Sung Jo Bang, Dong Hee Koh, Seok Jeong
Journal of Clinical Medicine.2023; 12(10): 3590. CrossRef - Comparison of guidewires for successful cannulation of biliary stenosis and targeting of biliary branches in ERCP
Masanori Kobayashi, Hiromune Katsuda, Kazuo Ohtsuka, Ryuichi Okamoto
Endoscopy International Open.2023; 11(09): E805. CrossRef - Impact of guidewire caliber on ERCP outcomes: Systematic review and meta-analysis comparing 0.025- and 0.035-inch guidewires
Muhammad Aziz, Amna Iqbal, Zohaib Ahmed, Saad Saleem, Wade Lee-Smith, Hemant Goyal, Faisal Kamal, Yaseen Alastal, Ali Nawras, Douglas G. Adler
Endoscopy International Open.2022; 10(07): E990. CrossRef - Experimental study of loop shape using 0.025-inch ERCP guidewires (with videos)
Takeshi Ogura, Saori Ueno, Atsushi Okuda, Nobu Nishioka, Tadahiro Yamada, Masanori Yamada, Kazuya Ueshima, Jun Matsuno, Yoshitaro Yamamoto, Kazuhide Higuchi
Endoscopy International Open.2021; 09(03): E427. CrossRef - Technical Review of Developments in Endoscopic Ultrasound-Guided Hepaticogastrostomy
Takeshi Ogura, Kazuhide Higuchi
Clinical Endoscopy.2021; 54(5): 651. CrossRef - Difficult Biliary Cannulation in Endoscopic Retrograde Cholangiopancreatography: Definitions, Risk Factors, and Implications
Brian M. Fung, Teodor C. Pitea, James H. Tabibian
EMJ Hepatology.2021; : 64. CrossRef - Production of ERCP training model using a 3D printing technique (with video)
Chang-Il Kwon, Yeonsun Shin, Jaeok Hong, Minje Im, Guk Bae Kim, Dong Hee Koh, Tae Jun Song, Won Suk Park, Jong Jin Hyun, Seok Jeong
BMC Gastroenterology.2020;[Epub] CrossRef - Clinical Evaluation of a Newly Developed Guidewire for Pancreatobiliary Endoscopy
Shigeto Ishii, Toshio Fujisawa, Hiroyuki Isayama, Shingo Asahara, Shingo Ogiwara, Hironao Okubo, Hisafumi Yamagata, Mako Ushio, Sho Takahashi, Hiroki Okawa, Wataru Yamagata, Yoshihiro Okawa, Akinori Suzuki, Yusuke Takasaki, Kazushige Ochiai, Ko Tomishima,
Journal of Clinical Medicine.2020; 9(12): 4059. CrossRef
- Structural factors influencing the clinical performance of 0.025-inch guidewires for pancreatobiliary endoscopy: An experimental study
- 6,554 View
- 308 Download
- 10 Web of Science
- 12 Crossref

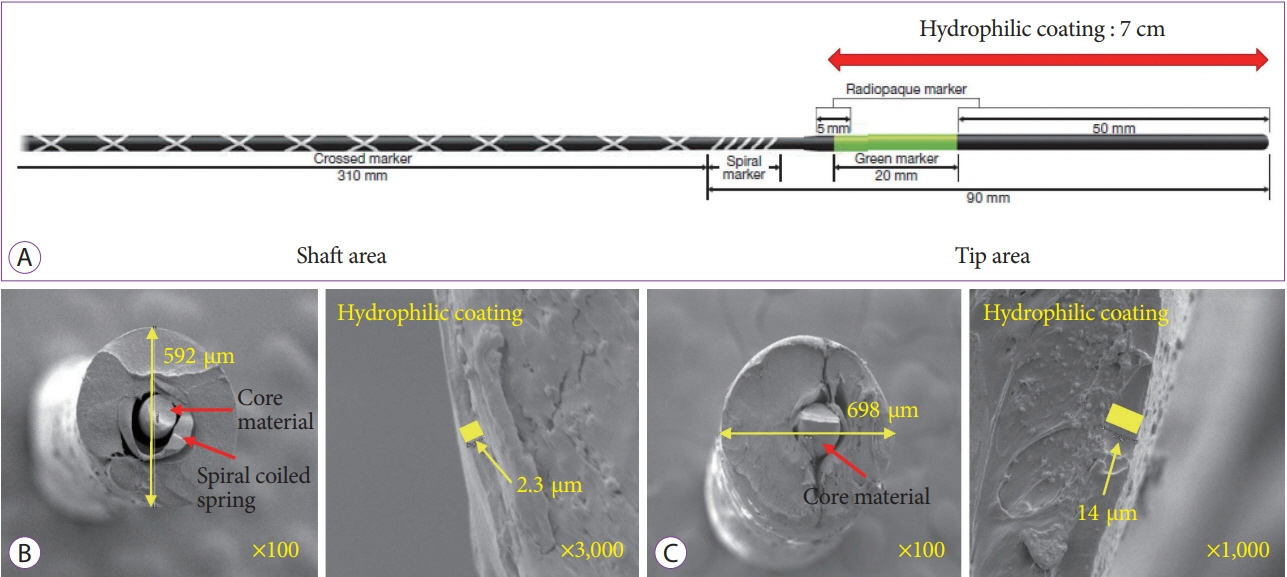
- Endoscopic Submucosal Dissection Followed by Concurrent Chemoradiotherapy in Patients with Early Esophageal Cancer with a High Risk of Lymph Node Metastasis
- Hee Kyung Kim, Weon Jin Ko, Chang-Il Kwon, Ga Won Song, In Kyun Yoo, Ji Hyun Song, Hak Su Kim, Joo Young Cho
- Clin Endosc 2019;52(5):502-505. Published online May 14, 2019
- DOI: https://doi.org/10.5946/ce.2018.176
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic submucosal dissection is recommended as an alternative therapy for early esophageal cancer. However, achieving curative resection in this procedure remains controversial since precise prediction of lymph node metastasis can be difficult. Here, we present the preliminary results of endoscopic submucosal dissection followed by concurrent chemoradiotherapy for early esophageal cancer with a high risk of lymph node metastasis. From May 2006 to January 2014, six patients underwent concurrent chemoradiotherapy after endoscopic submucosal dissection with a median follow-up period of 63 months. No complications were encountered during concurrent chemoradiotherapy. Although local recurrence did not occur in all patients, two patients were diagnosed with metachronous cancer. Overall, the survival rate was 100%. Thus, endoscopic submucosal dissection followed by concurrent chemoradiotherapy may be a feasible treatment for early esophageal cancer in patients with a high risk of lymph node metastasis. Future prospective large-scale studies are warranted to confirm our results.
-
Citations
Citations to this article as recorded by- Unveiling Therapeutic Targets for Esophageal Cancer: A Comprehensive Review
Rakesh Acharya, Ananya Mahapatra, Henu Kumar Verma, L. V. K. S. Bhaskar
Current Oncology.2023; 30(11): 9542. CrossRef - Editorial “Discrepancy Between the Clinical and Final Pathological Findings of Lymph Node Metastasis in Superficial Esophageal Cancer”
Rian M. Hasson, Joseph D. Phillips
Annals of Surgical Oncology.2019; 26(9): 2662. CrossRef
- Unveiling Therapeutic Targets for Esophageal Cancer: A Comprehensive Review
- 4,348 View
- 92 Download
- 1 Web of Science
- 2 Crossref

- Will New Instruments for Endoscopic Ultrasound-Guided Tissue Acquisition Make Us Happy?
- Chang-Il Kwon
- Clin Endosc 2018;51(6):510-512. Published online November 23, 2018
- DOI: https://doi.org/10.5946/ce.2018.164

-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Endoscopic Ultrasonography-Guided Fine-Needle Biopsy for Patients with Resectable Pancreatic Malignancies
Ming-Sheng Chien, Ching-Chung Lin, Jian-Han Lai
Gastroenterology Insights.2024; 15(2): 375. CrossRef - Randomized controlled trial comparing a conventional needle and a novel needle for endoscopic ultrasound (EUS)-guided histology of peripancreatic masses
Hyoun Wook Lee, Kwang Min Kim
Medicine.2021; 100(10): e25106. CrossRef - Microforceps-Assisted Diagnosis of Cystic Pancreatic Neuroendocrine Tumor
Guru Trikudanathan, Dale Snover, Shawn J Mallery
Clinical Endoscopy.2019; 52(3): 293. CrossRef - Which Needle Needs to Be Chosen for Better Outcome of Endoscopic Ultrasound-Guided Tissue Acquisition?
Dong Wook Lee, Eun Young Kim
Gut and Liver.2019; 13(3): 223. CrossRef - Present and Future of Endoscopic Ultrasound-Guided Tissue Acquisition in Solid Pancreatic Tumors
Jae Keun Park, Kwang Hyuck Lee
Clinical Endoscopy.2019; 52(6): 541. CrossRef
- Endoscopic Ultrasonography-Guided Fine-Needle Biopsy for Patients with Resectable Pancreatic Malignancies
- 5,281 View
- 88 Download
- 5 Web of Science
- 5 Crossref

- An Unusual Mimicker of a Pancreatic Pseudocyst
- Sang Ah Choi, Chang-Il Kwon, Gwangil Kim, Daejung Kim, Sung Hoon Choi
- Clin Endosc 2018;51(3):304-305. Published online March 22, 2018
- DOI: https://doi.org/10.5946/ce.2017.160
- 4,332 View
- 122 Download

- Immediate Endoscopic Management of an Intramural Hematoma Developed during Colonoscopy
- Chang-Il Kwon, Duck Hwan Kim, Sung Pyo Hong
- Clin Endosc 2017;50(5):508-509. Published online August 3, 2017
- DOI: https://doi.org/10.5946/ce.2017.037
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Systemic AL amyloidosis with multiple submucosal hematomas of the colon: a case report and literature review
Makomo Makazu, Akiko Sasaki, Chikamasa Ichita, Chihiro Sumida, Takashi Nishino, Miki Nagayama, Shinichi Teshima
Clinical Journal of Gastroenterology.2024; 17(1): 69. CrossRef - Perspectives and Management Strategies for Acute Colonic Intramural Hematoma
Reham Samir, Mohamed B Hashem, Hedy A Badary, Ahmed Bahaa, Nader Bakheet
International Journal of General Medicine.2022; Volume 15: 2861. CrossRef - Colonic Intramural Hematoma in a Cat: A Case Report
Ti-Chiu Hsu, Lee-Shuan Lin, Cheng-Shu Chung, Chuan Chiang, Hsien-Chieh Chiu, Ping-Hsun Huang
Frontiers in Veterinary Science.2022;[Epub] CrossRef - Traumatic Acute Colonic Intramural Hematoma: A Rare Entity and Successful Expectant Approach
Devarajan Jebin Aaron, Sandeep Bhattarai, Oseen Shaikh, Sarath Chandra Sistla
Cureus.2020;[Epub] CrossRef
- Systemic AL amyloidosis with multiple submucosal hematomas of the colon: a case report and literature review
- 5,900 View
- 101 Download
- 4 Web of Science
- 4 Crossref

- Guide-Wire Assisted Endobiliary Forceps Biopsy Sampling
- Chang-Il Kwon, Tae Hoen Kim, Kyoung Ah Kim
- Clin Endosc 2017;50(4):404-405. Published online February 13, 2017
- DOI: https://doi.org/10.5946/ce.2016.149
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Endobiliary biopsy
Riccardo Inchingolo, Fabrizio Acquafredda, Alessandro Posa, Thiago Franchi Nunes, Stavros Spiliopoulos, Francesco Panzera, Carlos Alberto Praticò
World Journal of Gastrointestinal Endoscopy.2022; 14(5): 291. CrossRef - How Can We Differentiate Malignant Biliary Strictures from Clinically Indeterminate Biliary Strictures?
Eui Joo Kim, Jae Hee Cho
Clinical Endoscopy.2019; 52(2): 95. CrossRef
- Endobiliary biopsy
- 5,245 View
- 142 Download
- 3 Web of Science
- 2 Crossref

- Mechanisms of Biliary Plastic Stent Occlusion and Efforts at Prevention
- Chang-Il Kwon, Glen A. Lehman
- Clin Endosc 2016;49(2):139-146. Published online March 22, 2016
- DOI: https://doi.org/10.5946/ce.2016.024
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Biliary stenting via endoscopic retrograde cholangiopancreatography has greatly improved the quality of patient care over the last 30 years. Plastic stent occlusion limits the life span of such stents. Attempts to improve plastic stent patency duration have mostly failed. Metal stents (self-expandable metal stents [SEMSs]) have therefore replaced plastic stents, especially for malignant biliary strictures. SEMS are at least 10 times more expensive than plastic stents. In this focused review, we will discuss basic mechanisms of plastic stent occlusion, along with a systematic summary of previous efforts and related studies to improve stent patency and potential new techniques to overcome existing limitations.
-
Citations
Citations to this article as recorded by- Clinical use of uncovered balloon‐expandable metallic biliary stents for treatment of extrahepatic biliary tract obstructions in cats and dogs: 11 cases (2012–2022)
Julia L. Bergen, Blake M. Travis, Fred S. Pike
Veterinary Surgery.2024; 53(2): 320. CrossRef - Therapeutic biliary stents: applications and opportunities
Matthew Ledenko, Beau Toskich, Christine Mehner, Hakan Ceylan, Tushar Patel
Expert Review of Medical Devices.2024; 21(5): 399. CrossRef - Fabrication of a Universal Composite Coating for Biliary Stents with Protein Antifouling and Antibacterial Synergies
Sipei Zhao, Changlu Zhou, Rui Zan, Tao Suo, Zhong Xin
Industrial & Engineering Chemistry Research.2024; 63(22): 9833. CrossRef - Development of novel biliary metal stent with coil-spring structure and its application in vivo swine biliary stricture model
In Rae Cho, Sang Hyub Lee, Jin Ho Choi, Namyoung Park, Min Woo Lee, Joo Seong Kim, Seok Jeong, Don Haeng Lee, Tae-Won Jeong, Byoung-Yun Ki, Woo Hyun Paik, Ji Kon Ryu, Yong-Tae Kim
Frontiers in Oncology.2023;[Epub] CrossRef - Biliary and pancreatic stents
Samuel Han, Jorge V. Obando, Amit Bhatt, Juan Carlos Bucobo, Dennis Chen, Andrew P. Copland, Koushik K. Das, Mohit Girotra, Allon Kahn, Kumar Krishnan, Sonali S. Sakaria, Monica Saumoy, Guru Trikudanathan, Arvind J. Trindade, Julie Yang, Ryan J. Law, Davi
iGIE.2023; 2(2): 240. CrossRef - Diagnostik und Therapie von Gallenwegserkrankungen
David Albers, Brigitte Schumacher
Gastroenterologie up2date.2023; 19(02): 133. CrossRef - CT imaging features of bile duct stent complications
Nga T. Nguyen, Hasan A. Khan, Kian Abdul-Baki, Woongsoon Choi, Neel K. Shroff, Zahra Akhtar, Peeyush Bhargava
Clinical Imaging.2023; 103: 109986. CrossRef - Assessment of postoperative common bile duct stones after endoscopic extraction and subsequent cholecystectomy
Ryo Sugiura, Hideaki Nakamura, Shoichi Horita, Takashi Meguro, Kiyotaka Sasaki, Hidetoshi Kagaya, Tatsuya Yoshida, Hironori Aoki, Takayuki Morita, Miyoshi Fujita, Eiji Tamoto, Masayuki Fukushima, Yoshitomo Ashitate, Takashi Ueno, Akio Tsutaho, Masaki Kuwa
Surgical Endoscopy.2022; 36(9): 6535. CrossRef - Characterization and preliminaryin vivoevaluation of a self-expandable hydrogel stent with anisotropic swelling behavior and endoscopic deliverability for use in biliary drainage
Yoshiyasu Nagakawa, Satoshi Fujita, Shunji Yunoki, Takayoshi Tsuchiya, Shin-ichiro Suye, Kenji Kinoshita, Motoki Sasaki, Takao Itoi
Journal of Materials Chemistry B.2022; 10(23): 4375. CrossRef - Impact of a shorter replacement interval of plastic stents on premature stent exchange rate in benign and malignant biliary strictures
Alica Kubesch, Fabian Görnert, Natalie Filmann, Jörg Bojunga, Stefan Zeuzem, Michael Jung, Mireen Friedrich‐Rust, Dirk Walter
Journal of Gastroenterology and Hepatology.2022; 37(6): 1076. CrossRef - Palliation in Gallbladder Cancer: The Role of Gastrointestinal Endoscopy
Tommaso Schepis, Ivo Boškoski, Andrea Tringali, Vincenzo Bove, Guido Costamagna
Cancers.2022; 14(7): 1686. CrossRef - Role of ERCP in Benign Biliary Strictures
Tommaso Schepis, Ivo Boškoski, Andrea Tringali, Guido Costamagna
Gastrointestinal Endoscopy Clinics of North America.2022; 32(3): 455. CrossRef - Enteral extended biliary stents versus conventional plastic biliary stents for the treatment of extrahepatic malignant biliary obstruction: a single-center prospective randomized controlled study
Xiaofen Xu, Yaopeng Zhang, Wei Zheng, Yingchun Wang, Wei Yao, Ke Li, Xiue Yan, Hong Chang, Yonghui Huang
Surgical Endoscopy.2022; 36(11): 8202. CrossRef - Risk factors for post-endoscopic retrograde cholangiopancreatography cholangitis in patients with hepatic alveolar echinococcosis—an observational study
Fei Du, Wenhao Yu, Zhixin Wang, Zhi Xie, Li Ren
Annals of Medicine.2022; 54(1): 1809. CrossRef - A RARE CASE OF BILIARY PLASTIC STENT OBSTRUCTION BY PANCREATIC PLASTIC STENT MIGRATION: A CASE REPORT
Andrea Minciullo, Serena Stigliano, Benedetto Neri, Benedetta Colombo, Francesco Maria Di Matteo
Gastroenterology Nursing.2022; 45(5): 367. CrossRef - Impact of endobiliary radiofrequency ablation on biliary drainage in patients with malignant biliary strictures treated with uncovered self-expandable metal stents: a randomized controlled multicenter trial
David Albers, Arthur Schmidt, Moritz Schiemer, Karel Caca, Andreas Wannhoff, Peter Sauer, Marcel Wiesweg, Brigitte Schumacher, Alexander Dechene
Gastrointestinal Endoscopy.2022; 96(6): 970. CrossRef - Mechanical properties and degradation process of biliary self‐expandable biodegradable stents
Chang‐Il Kwon, Jun Sik Son, Kyu Seok Kim, Jong Pil Moon, Sehwan Park, Jinkyung Jeon, Gwangil Kim, Sung Hoon Choi, Kwang Hyun Ko, Seok Jeong, Don Haeng Lee
Digestive Endoscopy.2021; 33(7): 1158. CrossRef - Personalized Endoscopy in Complex Malignant Hilar Biliary Strictures
Ivo Boškoski, Tommaso Schepis, Andrea Tringali, Pietro Familiari, Vincenzo Bove, Fabia Attili, Rosario Landi, Vincenzo Perri, Guido Costamagna
Journal of Personalized Medicine.2021; 11(2): 78. CrossRef - Palliative endoscopic retrograde biliary drainage for malignant biliary obstruction in Korea: A nationwide assessment
DongKee Jang, Jungmee Kim, SeungBae Yoon, WonJae Yoon, Jung-Wook Kim, TaeHee Lee, Jae-Young Jang, ChangNyol Paik, JunKyu Lee
Saudi Journal of Gastroenterology.2021; 27(3): 173. CrossRef - Predictors of stent dysfunction in patients with bilateral metal stents for malignant hilar obstruction
Hoonsub So, Chi Hyuk Oh, Tae Jun Song, Sung Woo Ko, Jun Seong Hwang, Dongwook Oh, Do Hyun Park, Sang Soo Lee, Dong-Wan Seo, Seok Ho Dong, Sung Koo Lee, Myung-Hwan Kim, Gianfranco D. Alpini
PLOS ONE.2021; 16(3): e0249096. CrossRef - Survival, stent patency, and cost‐effectiveness of plastic biliary stent versus metal biliary stent for palliation in malignant biliary obstruction in a developing country tertiary hospital
Muthia Farani, Siti R F Saldi, Hasan Maulahela, Murdani Abdullah, Ari F Syam, Dadang Makmum
JGH Open.2021; 5(8): 959. CrossRef - New anti-reflux plastic stent to reduce the risk of stent-related cholangitis in the treatment of biliary strictures
Xiang-Lei Yuan, Lian-Song Ye, Xian-Hui Zeng, Qing-Hua Tan, Yi Mou, Wei Liu, Chun-Cheng Wu, Hang Yang, Bing Hu
World Journal of Gastroenterology.2021; 27(28): 4697. CrossRef - Duodenoscope-Acquired Infections: Risk Factors to Consider
Grace Thornhill, Brian Dunkin
Journal of Digestive Endoscopy.2021; 12(03): 151. CrossRef - Self‐expandable hydrogel biliary stent design utilizing the swelling property of poly(vinyl alcohol) hydrogel
Yoshiyasu Nagakawa, Satoshi Fujita, Shunji Yunoki, Takayoshi Tsuchiya, Shin‐ichiro Suye, Takao Itoi
Journal of Applied Polymer Science.2020;[Epub] CrossRef - Biodegradable Stent/Tube for Pancreatic and Biliary Disease
Chang-Il Kwon
The Korean Journal of Pancreas and Biliary Tract.2020; 25(1): 18. CrossRef - Endoscopic transpapillary gallbladder drainage for the management of acute calculus cholecystitis patients unfit for urgent cholecystectomy
Tae Hyeon Kim, Dong Eun Park, Hyung Ku Chon, Ezio Lanza
PLOS ONE.2020; 15(10): e0240219. CrossRef - Reducing deposition of encrustation in ureteric stents by changing the stent architecture: A microfluidic-based investigation
A. Mosayyebi, D. Lange, Q. Yann Yue, B. K. Somani, X. Zhang, C. Manes, D. Carugo
Biomicrofluidics.2019;[Epub] CrossRef - Risk Factors for the Development of Stent-Associated Cholangitis Following Endoscopic Biliary Stent Placement
Brendan T. Everett, Shelly Naud, Richard S. Zubarik
Digestive Diseases and Sciences.2019; 64(8): 2300. CrossRef - Relief of Obstruction in the Management of Pancreatic Cancer
Chang-Il Kwon
The Korean Journal of Gastroenterology.2019; 74(2): 69. CrossRef - Predictive risk factors associated with cholangitis following ERCP
Joshua Tierney, Neal Bhutiani, Bryce Stamp, John S. Richey, Michael H. Bahr, Gary C. Vitale
Surgical Endoscopy.2018; 32(2): 799. CrossRef - Characterization of biofilms in biliary stents and potential factors involved in occlusion
Chetana Vaishnavi, Jayanta Samanta, Rakesh Kochhar
World Journal of Gastroenterology.2018; 24(1): 112. CrossRef - Quantification of major constituents of biofilms in occluded pancreatic stents
Chetana Vaishnavi, Pramod K. Gupta, Megha Sharma, Rakesh Kochhar
Journal of Medical Microbiology.2018; 67(9): 1225. CrossRef - Evaluation of valve function in antireflux biliary metal stents
Chang-Il Kwon, Jong Pil Moon, Ho Yun, Seok Jeong, Dong Hee Koh, Woo Jung Lee, Kwang Hyun Ko, Dae Hwan Kang
BMC Gastroenterology.2018;[Epub] CrossRef - Ursodeoxycholic acid attenuates 5‑fluorouracil‑induced mucositis in a rat model
Seung Kim, Hoon Chun, Hyuk Choi, Eun Kim, Bora Keum, Yeon Seo, Yoon Jeen, Hong Lee, Soon Um, Chang Kim
Oncology Letters.2018;[Epub] CrossRef - The Stent Patency and Migration Rate of Different Shaped Plastic Stents in Bile Flow Phantom Model and In Vivo Animal Bile Duct Dilation Model
Chang-Il Kwon, Gwangil Kim, Seok Jeong, Don Haeng Lee, Kyoung Ah Kim, Kwang Hyun Ko, Joo Young Cho, Sung Pyo Hong
Digestive Diseases and Sciences.2017; 62(5): 1246. CrossRef - Peripheral hepatojejunostomy: a last resort palliative solution in Greece during the economic crisis
Georgios C Sotiropoulos, Eleftherios Spartalis, Nikolaos Machairas, Gregory Kouraklis
BMJ Case Reports.2017; : bcr-2016-217368. CrossRef - Is There Room for Improvement in Increasing the Stent Patency of Biliary Plastic Stents?
Jung Wan Choe, Jong Jin Hyun
Gut and Liver.2016; 10(4): 499. CrossRef
- Clinical use of uncovered balloon‐expandable metallic biliary stents for treatment of extrahepatic biliary tract obstructions in cats and dogs: 11 cases (2012–2022)
- 16,348 View
- 272 Download
- 37 Web of Science
- 37 Crossref

- Optimal Methods for the Management of Iatrogenic Colonoscopic Perforation
- Dae Kyu Shin, Sun Young Shin, Chi Young Park, Sun Mi Jin, Yang Hyun Cho, Won Hee Kim, Chang-Il Kwon, Kwang Hyun Ko, Ki Baik Hahm, Pil Won Park, Jong Woo Kim, Sung Pyo Hong
- Clin Endosc 2016;49(3):282-288. Published online February 18, 2016
- DOI: https://doi.org/10.5946/ce.2015.046
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Colonoscopic perforations have been managed with exploratory laparotomy, and have resulted in some morbidity and mortality. Recently, laparoscopic surgery is commonly performed for this purpose. The aim of this study was to compare the outcomes of several management strategies for iatrogenic colonoscopic perforations.
Methods
We retrospectively reviewed the medical records of patients who had been treated for colonoscopic perforation between January 2004 and April 2013 at CHA Bundang Medical Center in Korea.
Results
A total of 41 patients with colonoscopic perforation were enrolled. Twenty patients underwent conservative management with a success rate of 90%. Surgical management was performed in 23 patients including two patients who were converted to surgical management after the failure of the initial conservative management. Among 14 patients who underwent surgery at 8 hours after the perforation, there was no considerable difference in adverse outcomes between the laparotomy group and the laparoscopic surgery group. The medical costs and claim rate were 1.45 and 1.87 times greater in the exploratory laparotomy group, respectively.
Conclusions
Conservative management of colonoscopic perforation could be an option for patients without overt symptoms of peritonitis or with a small defect size. If surgical management is required, laparoscopic surgery may be considered as the initial procedure even with a delayed diagnosis. -
Citations
Citations to this article as recorded by- Surgical repair of endoscopy-induced colonic perforations: a case-matched study of short-term morbidity and mortality
Fady DANIEL, Suha JABAK, Mohammad HOSNI, Hani TAMIM, Aurelie MAILHAC, Ayman ALRAZIM, Noura AL-ALI, Robert CHURCH, Mohammad KHALIFE, Shafik SIDANI, Faek JAMALI
Minerva Surgery.2024;[Epub] CrossRef - Laparoscopic versus open surgery for colonoscopic perforation: A systematic review and meta-analysis
Wu Zhong, Chuanyuan Liu, Chuanfa Fang, Lei Zhang, Xianping He, Weiquan Zhu, Xueyun Guan
Medicine.2023; 102(24): e34057. CrossRef - Elastography for Pediatric Chronic Liver Disease
Giovanna Ferraioli, Richard G. Barr, Jonathan R. Dillman
Journal of Ultrasound in Medicine.2021; 40(5): 909. CrossRef - Clinical outcomes of laparoscopic versus open surgery for repairing colonoscopic perforation: a multicenter study
Jae Seok Lee, Jeong Yeon Kim, Byung Mo Kang, Sang Nam Yoon, Jun Ho Park, Bo Young Oh, Jong Wan Kim
Surgery Today.2021; 51(2): 285. CrossRef - The analysis of outcomes of surgical management for colonoscopic perforations: A 16-years experiences at a single institution
Dae Ro Lim, Jung Kul Kuk, Taehyung Kim, Eung Jin Shin
Asian Journal of Surgery.2020; 43(5): 577. CrossRef - Multicenter retrospective evaluation of ileocecocolic perforations associated with diagnostic lower gastrointestinal endoscopy in dogs and cats
Vanessa L. Woolhead, Jacqueline C. Whittemore, Sarah A. Stewart
Journal of Veterinary Internal Medicine.2020; 34(2): 684. CrossRef - Endoscopic Management of the Ascending Colon Perforation Secondary to a Rare-Earth Magnets Ingestion in a Pediatric Patient
Sandra Mabel Camacho-Gomez, James Meredith Noel, Robert Adam Noel
ACG Case Reports Journal.2020; 7(8): e00436. CrossRef - Pseudo‐obstruction But a Real Perforation
AORN Journal.2019; 109(1): 142. CrossRef - Treatment of colonoscopic perforation: outcomes from a major single tertiary institution
Carolyn R. Chew, Justin M. C. Yeung, Ian G. Faragher
ANZ Journal of Surgery.2019; 89(5): 546. CrossRef - Management of colonoscopic perforations: A systematic review
Alexander T. Hawkins, Kenneth W. Sharp, Molly M. Ford, Roberta L. Muldoon, M. Benjamin Hopkins, Timothy M. Geiger
The American Journal of Surgery.2018; 215(4): 712. CrossRef - 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation
Nicola de’Angelis, Salomone Di Saverio, Osvaldo Chiara, Massimo Sartelli, Aleix Martínez-Pérez, Franca Patrizi, Dieter G. Weber, Luca Ansaloni, Walter Biffl, Offir Ben-Ishay, Miklosh Bala, Francesco Brunetti, Federica Gaiani, Solafah Abdalla, Aurelien Ami
World Journal of Emergency Surgery.2018;[Epub] CrossRef - Management Outcomes of Colonoscopic Perforations Are Affected by the General Condition of the Patients
Jae Ho Park, Kyung Jong Kim
Annals of Coloproctology.2018; 34(1): 16. CrossRef - Abdominal Sepsis: An Update
Mircea Gabriel Mureșan, Ioan Alexandru Balmoș, Iudita Badea, Ario Santini
The Journal of Critical Care Medicine.2018; 4(4): 120. CrossRef - Laparoscopic vs. open surgery for the treatment of iatrogenic colonoscopic perforations: a systematic review and meta-analysis
Aleix Martínez-Pérez, Nicola de’Angelis, Francesco Brunetti, Yann Le Baleur, Carmen Payá-Llorente, Riccardo Memeo, Federica Gaiani, Marco Manfredi, Paschalis Gavriilidis, Giorgio Nervi, Federico Coccolini, Aurelien Amiot, Iradj Sobhani, Fausto Catena, Gia
World Journal of Emergency Surgery.2017;[Epub] CrossRef - Urinary Bladder Injury During Colonoscopy Without Colon Perforation
Jung Wook Suh, Jun Won Min, Hwan Namgung, Dong-Guk Park
Annals of Coloproctology.2017; 33(3): 112. CrossRef - The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections
Massimo Sartelli, Alain Chichom-Mefire, Francesco M. Labricciosa, Timothy Hardcastle, Fikri M. Abu-Zidan, Abdulrashid K. Adesunkanmi, Luca Ansaloni, Miklosh Bala, Zsolt J. Balogh, Marcelo A. Beltrán, Offir Ben-Ishay, Walter L. Biffl, Arianna Birindelli, M
World Journal of Emergency Surgery.2017;[Epub] CrossRef - How Should We Manage Iatrogenic Perforation Caused by Colonoscopy?
Eun Sun Kim
Clinical Endoscopy.2016; 49(3): 214. CrossRef
- Surgical repair of endoscopy-induced colonic perforations: a case-matched study of short-term morbidity and mortality
- 8,246 View
- 151 Download
- 20 Web of Science
- 17 Crossref

- Communicating Tubular Esophageal Duplication Combined with Bronchoesophageal Fistula
- Ju Hwan Kim, Chang-Il Kwon, Ji Young Rho, Sang Woo Han, Ji Su Kim, Suk Pyo Shin, Ga Won Song, Ki Baik Hahm
- Clin Endosc 2016;49(1):81-85. Published online January 28, 2016
- DOI: https://doi.org/10.5946/ce.2016.49.1.81
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Esophageal duplication (ED) is rarely diagnosed in adults and is usually asymptomatic. Especially, ED that is connected to the esophagus through a tubular communication and combined with bronchoesophageal fistula (BEF) is extremely rare and has never been reported in the English literature. This condition is very difficult to diagnose. Although some combinations of several modalities, such as upper gastrointestinal endoscopy, esophagography, computed tomography, magnetic resonance imaging, and endoscopic ultrasonography, can be used for the diagnosis, the results might be inconclusive. Here, we report on a patient with communicating tubular ED that was incidentally diagnosed on the basis of endoscopy and esophagography during the postoperational evaluation of BEF.
-
Citations
Citations to this article as recorded by- Reconstruction of Adult Tubular Esophageal Duplication with Supraclavicular Artery Island Flap: A Rare Case Presentation
Xin Yang, Zheng Jiang, Jun Liu, Fei Chen
Ear, Nose & Throat Journal.2023; : 014556132311734. CrossRef - Tubular Duplication of the Esophagus in a Newborn, Treated by Thoracoscopy
Igor Khvorostov, Alexey Gusev, Abdumanap Alkhasov, Sergey Yatsyk, Elena D'yakonova
European Journal of Pediatric Surgery Reports.2022; 10(01): e49. CrossRef - Endoscopic septum division of tubular esophageal duplication in two children and systematic review
Rahşan Özcan, Ali Ekber Hakalmaz, Şenol Emre, Ayşe Karagöz, Çiğdem Tütüncü, Sebuh Kuruğoğlu, Gonca Topuzlu Tekant
Pediatric Surgery International.2022; 38(11): 1525. CrossRef - Endoscopic management of a tubular esophageal duplication in a young adult
Pietro Familiari, Rosario Landi, Francesca Mangiola, Camilla Vittoria Vita, Guido Costamagna
VideoGIE.2020; 5(10): 455. CrossRef - Esophageal duplication and congenital esophageal stenosis
A. Francois Trappey, Shinjiro Hirose
Seminars in Pediatric Surgery.2017; 26(2): 78. CrossRef
- Reconstruction of Adult Tubular Esophageal Duplication with Supraclavicular Artery Island Flap: A Rare Case Presentation
- 10,123 View
- 91 Download
- 4 Web of Science
- 5 Crossref

- Twenty-Second versus Sixty-Second Dilation Duration in Endoscopic Papillary Balloon Dilation for the Treatment of Small Common Bile Duct Stones: A Prospective Randomized Controlled Multicenter Trial
- Byoung Wook Bang, Tae Hoon Lee, Tae Jun Song, Joung-Ho Han, Hyun Jong Choi, Jong Ho Moon, Chang-Il Kwon, Seok Jeong
- Clin Endosc 2015;48(1):59-65. Published online January 31, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.1.59
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Endoscopic papillary balloon dilation (EPBD) has been advocated as an alternative therapy to endoscopic sphincterotomy for the treatment of common bile duct (CBD) stones. However, there is no established consensus on the optimal balloon dilation duration (BDD). We prospectively evaluated the efficacy and post-endoscopic retrograde cholangiopancreatography (ERCP) complications between the 20- and 60-second EPBD groups.
Methods A total of 228 patients with small CBD stones (≤12 mm) were randomly assigned to undergo EPBD with a 20- or 60-second duration at six institutions. We evaluated baseline patient characteristics, endoscopic data, clinical outcomes, and procedure-related complications. In addition, we analyzed risk factors for postprocedural pancreatitis.
Results CBD stones were removed successfully in 107 of 109 patients (98.1%) in the 20-second group and in 112 of 119 patients (94.1%) in the 60-second group (
p =0.146). Post-ERCP pancreatitis developed in seven patients (6.4%) in the 20-second group and nine patients (7.5%) in the 60-second group (p =0.408). In multivariate analysis, contrast dye injection into the pancreatic duct is a significant risk factor for post-EPBD pancreatitis.Conclusions Based on the data showing that there were no significant differences in safety and efficacy between the two BDD groups, 20 seconds of BDD may be adequate for treatment of small CBD stones with EPBD.
-
Citations
Citations to this article as recorded by- The therapeutic effect of balloon dilatation with different duration for biliary duct calculi: A network meta-analysis
ZhiYuan Yu, Chen Liang, ShiYu Yang, Xu Zhang, Yan Sun
Journal of Minimal Access Surgery.2022; 18(3): 327. CrossRef - The ballooning time in endoscopic papillary balloon dilation for removal of bile duct stones
Qiang Wang, Luyao Fu, Tao Wu, Xiong Ding
Medicine.2021; 100(11): e24735. CrossRef - Nouveautés dans la prise en charge des calculs biliaires à l’UEGW 2015
E. Bories, C. Lefort
Acta Endoscopica.2016; 46(1-2): 20. CrossRef - Is endoscopic papillary balloon dilatation really a risk factor for post-ERCP pancreatitis?
Toshio Fujisawa, Koichi Kagawa, Kantaro Hisatomi, Kensuke Kubota, Atsushi Nakajima, Nobuyuki Matsuhashi
World Journal of Gastroenterology.2016; 22(26): 5909. CrossRef - Is the Balloon Dilation Duration in Endoscopic Papillary Balloon Dilation (EPBD) Related to the Occurrence of Post-EPBD Pancreatitis?
Dong Uk Kim
Clinical Endoscopy.2015; 48(1): 6. CrossRef
- The therapeutic effect of balloon dilatation with different duration for biliary duct calculi: A network meta-analysis
- 7,315 View
- 83 Download
- 4 Web of Science
- 5 Crossref

-
Endoscopic Submucosal Dissection Using a Novel Versatile Knife: An Animal Feasibility Study (with Video)

- Chang-Il Kwon, Gwangil Kim, Il-Kwun Chung, Won Hee Kim, Kwang Hyun Ko, Sung Pyo Hong, Seok Jeong, Don Haeng Lee
- Clin Endosc 2014;47(6):544-554. Published online November 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.6.544
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub Background/Aims In order to reduce the procedure time and the number of accessory changes during endoscopic submucosal dissection (ESD), we developed a novel versatile knife, which has the combined advantages of several conventional knives. The aim of this study was to compare the efficacy, safety, and histological quality of ESD performed using this novel versatile knife and a combination of several conventional knives.
Methods This was an
in vivo animal study comparing two different modalities of ESD in mini-pigs. Completion time of each resection was documented, and the resected specimens were retrieved and evaluated for completeness. To assess the quality control of the procedures and adverse events, detailed histopathological examinations were performed.Results A total of 18 specimens were dissected by ESD safely and easily (nine specimens using the new versatile knife; nine specimens by mixing conventional knives). All resections were completed as
en bloc resections. There was no significant difference in procedure time between the 2 modalities (456 seconds vs. 355 seconds,p =0.258) and cutting speed (1.983 mm2/sec vs. 1.57 mm2/sec,p =1.000). The rate of adverse events and histological quality did not statistically differ between the modalities.Conclusions ESD with a versatile knife appeared to be an easy, safe, and technically efficient method.
-
Citations
Citations to this article as recorded by- Comparison of synchronous dual wavelength diode laser versus conventional endo-knives for esophageal endoscopic submucosal dissection: an animal study
Jian Tang, Shufang Ye, Xueliang Ji, Jun Li, Feng Liu
Surgical Endoscopy.2018; 32(12): 5037. CrossRef - Technological review on endoscopic submucosal dissection: available equipment, recent developments and emerging techniques
Georgios Mavrogenis, Juergen Hochberger, Pierre Deprez, Morteza Shafazand, Dimitri Coumaros, Katsumi Yamamoto
Scandinavian Journal of Gastroenterology.2017; 52(4): 486. CrossRef
- Comparison of synchronous dual wavelength diode laser versus conventional endo-knives for esophageal endoscopic submucosal dissection: an animal study
- 7,188 View
- 60 Download
- 3 Web of Science
- 2 Crossref

- Long-Term Outcome of Endoscopic Papillary Large Balloon Dilatation
- Chang-Il Kwon
- Clin Endosc 2013;46(6):601-602. Published online November 19, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.6.601
- 4,723 View
- 28 Download

- Endoscopic Resection of Giant Colonic Lipoma: Case Series with Partial Resection
- Gun Woo Kim, Chang-Il Kwon, Sang Hee Song, Sun Mi Jin, Kyung Ho Kim, Jie Hye Moon, Sung Pyo Hong, Pil Won Park
- Clin Endosc 2013;46(5):586-590. Published online September 30, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.5.586
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Colonic lipoma, a very rare form of benign tumor, is typically detected incidentally in asymptomatic patients. The size of lipoma is reported variously from 2 mm to 30 cm, with higher likelihood of symptoms as the size is bigger. Cases with symptom or bigger lesion are surgically resected in principle; endoscopic resection, which has developed recently with groundbreaking advance of endoscopic excision technology, is being used more often but with rare report of success due to high chance of complications such as bowel perforation or bleeding. The authors report here, together with a literature review, our experiences of three cases of giant colonic lipomas showing complete remission after aggressive unroofing technique, at certain intervals, using snare catheter at the origin of the lipoma so that the remaining lipoma could be drained out of the exposed surface spontaneously, in order to reduce complications.
-
Citations
Citations to this article as recorded by- Colonic intussusception from pedunculated colonic lipoma at hepatic flexure: A case report and review of current literature
Richard Edmund Hogan, Ben Michael Murray, Michael Flanagan, Shane Brennan, Conor Shortt, Dara Kavanagh
Surgery Case Reports.2024; 1: 100008. CrossRef - A giant colonic lipoma
Tara M. Connelly, Cillian Clancy, Shaomin Hu, Joshua Sommovilla
ANZ Journal of Surgery.2023; 93(1-2): 428. CrossRef - Obscure gastrointestinal bleeding from a large jejunal lipoma treated using an endoscopic unroofing technique with double balloon enteroscopy: a case study
Reo Kobayashi, Ken Inoue, Ryohei Hirose, Toshifumi Doi, Akihito Harusato, Osamu Dohi, Naohisa Yoshida, Kazuhiko Uchiyama, Takeshi Ishikawa, Tomohisa Takagi, Hiroaki Yasuda, Hideyuki Konishi, Yukiko Morinaga, Yoshito Itoh
Clinical Journal of Gastroenterology.2023; 16(1): 32. CrossRef - Endoscopic debulking of a large colonic lipoma causing recurrent intussusception using endoscopic mucosotomy technique
Jenson Phung, Morgan Freeman, Mohammad Bilal
Endoscopy.2023; 55(S 01): E817. CrossRef - Large colonic lipoma with a laterally spreading tumor treated by endoscopic submucosal dissection: A case report
Jun Yong Bae, Hun Kyu Kim, Yee Jin Kim, Se Woong Kim, Youngeun Lee, Chang Beom Ryu, Moon Sung Lee
World Journal of Clinical Cases.2023; 11(26): 6194. CrossRef - Observation of the drainage process of the residual lipoma after endoscopic unroofing technique during colonoscopic evaluation of post-procedural hematochezia
Yi-Ling Ko, Hiroki Matsuoka, Ryohei Nomaru, So Imakiire, Hideto Sakisaka, Satoshi Matsuoka, Nobuaki Kuno, Koichi Abe, Sadahiro Funakoshi, Yusuke Ishida, Hideki Ishibashi, Kaori Koga, Tetsuhiro Saito, Morishige Takeshita, Fumihito Hirai
Clinical Journal of Gastroenterology.2022; 15(2): 407. CrossRef - Spontaneous expulsion of a duodenal lipoma after endoscopic biopsy: A case report
Zhi-Hao Chen, Li-Hong Lv, Wen-Sheng Pan, Yi-Miao Zhu
World Journal of Gastroenterology.2022; 28(34): 5086. CrossRef - Pedunculated sigmoid lipoma causing colo-colonic intussusception
Kenneth Ford, Samantha Lopez, Gaurav Synghal, Yomi Fayiga, Brittany Carter, Anuj Kandel, Kenneth Ford
Baylor University Medical Center Proceedings.2021; 34(3): 371. CrossRef - Colonoscopic resection of giant colonic lipoma causing subacute large bowel obstruction
Amy Donovan, Sandun Abeyasundara, Hajir Nabi
ANZ Journal of Surgery.2020;[Epub] CrossRef - COLON LIPOMA COMPLICATED BY COLON INVAGINATION
U. B. Urmonov, S. G. Afanasyev, A. Yu. Dobrodeev, A. V. Avgustinovich, M. Yu. Volkov, N. V. Vasiliev, E. N. Samtsov
Grekov's Bulletin of Surgery.2020; 178(6): 63. CrossRef - Endoscopic treatment of large symptomatic colon lipomas: A systematic review of efficacy and safety
Michiel Bronswijk, Anne‐Marie Vandenbroucke, Peter Bossuyt
United European Gastroenterology Journal.2020; 8(10): 1147. CrossRef - Endoscopic resection of giant colon lipomas: get rid of the roof!
Michiel Bronswijk
VideoGIE.2019; 4(7): 341. CrossRef - Submucosal lipoma of the sigmoid colon as a rare cause of mucoid diarrhea: a case report
S. U. B. Dassanayake, N. P. Dinamithra, N. M. M. Nawarathne
Journal of Medical Case Reports.2016;[Epub] CrossRef - Endoscopic resection of giant GI lipoma: a case series
Diane Lorenzo, Jean Michel Gonzalez, Alban Benezech, Marc Barthet
VideoGIE.2016; 1(2): 43. CrossRef - Two Patients with Large Colonic Lipomas for which Endoscopic Unroofing was Ineffective
Yuichi Tomiki, Koichiro Niwa, Kiichi Nagayasu, Yu Okazawa, Shingo Ito, Ryosuke Ichikawa, Hisashi Ro, Shun Ishiyama, Kiichi Sugimoto, Kazuhiro Sakamoto
Case Reports in Gastroenterology.2016; 10(3): 538. CrossRef - Colonoscopy‐assisted laparoscopic resection of an obstructing ‘giant’ lipoma of the transverse colon
B. Asantha De Silva, Raeed Deen, Wasantha K. Wijenayake
ANZ Journal of Surgery.2015; 85(10): 785. CrossRef - Unroofing Technique as an Option for the Endoscopic Treatment of Giant Gastrointestinal Lipomas
Marcela Kopáčová, Stanislav Rejchrt, Jan Bureš
Acta Medica (Hradec Kralove, Czech Republic).2015; 58(4): 115. CrossRef - Large “pedunculated” colonic lipoma: A word of caution while cutting into fat!
Syed Adnan Mohiuddin, Saad Al Kaabi, Ragesh Babu Thandassery, Khalid Mohsin Al Ejji, Nazeeh Al Dweik, Emran Amir, Manik Sharma
Indian Journal of Gastroenterology.2014; 33(6): 571. CrossRef
- Colonic intussusception from pedunculated colonic lipoma at hepatic flexure: A case report and review of current literature
- 7,514 View
- 95 Download
- 18 Crossref

- Functional Self-Expandable Metal Stents in Biliary Obstruction
- Chang-Il Kwon, Kwang Hyun Ko, Ki Baik Hahm, Dae Hwan Kang
- Clin Endosc 2013;46(5):515-521. Published online September 30, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.5.515
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Biliary stents are widely used not only for palliative treatment of malignant biliary obstruction but also for benign biliary diseases. Each plastic stent or self-expandable metal stent (SEMS) has its own advantages, and a proper stent should be selected carefully for individual condition. To compensate and overcome several drawbacks of SEMS, functional self-expandable metal stent (FSEMS) has been developed with much progress so far. This article looks into the outcomes and defects of each stent type for benign biliary stricture and describes newly introduced FSEMSs according to their functional categories.
-
Citations
Citations to this article as recorded by- Anti-fibrotic and anti-stricture effects of biodegradable biliary stents braided with dexamethasone-impregnated sheath/core structured monofilaments
Ju-Ro Lee, Seung Won Yang, Chang-Il Kwon, Kyu Seok Kim, Se Hwan Park, Myeong Jin Jang, Ga Hee Kim, Min Je Sung, Gwangil Kim, Jun Sik Son, Yoon Ki Joung
Acta Biomaterialia.2024; 178: 137. CrossRef - CT imaging features of bile duct stent complications
Nga T. Nguyen, Hasan A. Khan, Kian Abdul-Baki, Woongsoon Choi, Neel K. Shroff, Zahra Akhtar, Peeyush Bhargava
Clinical Imaging.2023; 103: 109986. CrossRef - Research progress on biliary stents
Progress in Medical Devices.2023;[Epub] CrossRef - A poly(l‐lactic acid) braided stent with high mechanical properties during in vitro degradation in bile
Gutian Zhao, Yuan Tian, Rixin Hua, Qingwei Liu, Jie Cheng, Gensheng Wu, Yi Zhang, Zhonghua Ni
Journal of Applied Polymer Science.2022;[Epub] CrossRef - Preliminary application of brachytherapy with double-strand 125I seeds and biliary drainage for malignant obstructive jaundice
Zong-Ming Li, De-Chao Jiao, Xin-Wei Han, Qin-Yu Lei, Xue-Liang Zhou, Miao Xu
Surgical Endoscopy.2022; 36(7): 4932. CrossRef - A viewpoint on material and design considerations for oesophageal stents with extended lifetime
Caitlin E. Jackson, Liam S. J. Johnson, Dominic A. Williams, Hans-Ulrich Laasch, Derek W. Edwards, Alison G. Harvey
Journal of Materials Science.2022; 57(1): 3. CrossRef - Emerging trends in biliary stents: a materials and manufacturing perspective
Saswat Choudhury, Sonal Asthana, Shervanthi Homer-Vanniasinkam, Kaushik Chatterjee
Biomaterials Science.2022; 10(14): 3716. CrossRef - Antireflux metal stent for biliary obstruction: Any benefits?
Tsuyoshi Hamada, Yousuke Nakai, Hiroyuki Isayama, Kazuhiko Koike
Digestive Endoscopy.2021; 33(3): 310. CrossRef - A poly(L‐lactic acid) monofilament with high mechanical properties for application in biodegradable biliary stents
Yuan Tian, Jing Zhang, Jie Cheng, Gensheng Wu, Yi Zhang, Zhonghua Ni, Gutian Zhao
Journal of Applied Polymer Science.2021;[Epub] CrossRef - Mechanical properties and degradation process of biliary self‐expandable biodegradable stents
Chang‐Il Kwon, Jun Sik Son, Kyu Seok Kim, Jong Pil Moon, Sehwan Park, Jinkyung Jeon, Gwangil Kim, Sung Hoon Choi, Kwang Hyun Ko, Seok Jeong, Don Haeng Lee
Digestive Endoscopy.2021; 33(7): 1158. CrossRef - Biodegradable Stent/Tube for Pancreatic and Biliary Disease
Chang-Il Kwon
The Korean Journal of Pancreas and Biliary Tract.2020; 25(1): 18. CrossRef - Drug-eluting Biliary Stent
Sung Ill Jang, Dong Ki Lee
The Korean Journal of Pancreas and Biliary Tract.2020; 25(1): 11. CrossRef - Mechanisms and prevention of biliary stent occlusion
A.V. Shabunin, M.M. Tavobilov, S.S. Lebedev, A.A. Karpov
Khirurgiya. Zhurnal im. N.I. Pirogova.2020; (5): 70. CrossRef - Endoscopic management of anastomotic stricture after living-donor liver transplantation
Dong Wook Lee, Jimin Han
The Korean Journal of Internal Medicine.2019; 34(2): 261. CrossRef - Relief of Obstruction in the Management of Pancreatic Cancer
Chang-Il Kwon
The Korean Journal of Gastroenterology.2019; 74(2): 69. CrossRef - The Stent Patency and Migration Rate of Different Shaped Plastic Stents in Bile Flow Phantom Model and In Vivo Animal Bile Duct Dilation Model
Chang-Il Kwon, Gwangil Kim, Seok Jeong, Don Haeng Lee, Kyoung Ah Kim, Kwang Hyun Ko, Joo Young Cho, Sung Pyo Hong
Digestive Diseases and Sciences.2017; 62(5): 1246. CrossRef - Current Status of Biliary Metal Stents
Hyeong Seok Nam, Dae Hwan Kang
Clinical Endoscopy.2016; 49(2): 124. CrossRef - Mechanisms of Biliary Plastic Stent Occlusion and Efforts at Prevention
Chang-Il Kwon, Glen A. Lehman
Clinical Endoscopy.2016; 49(2): 139. CrossRef - Time Sequence Evaluation of Biliary Stent Occlusion by Dissection Analysis of Retrieved Stents
Chang-Il Kwon, Mark A. Gromski, Stuart Sherman, Jeffrey J. Easler, Ihab I. El Hajj, James Watkins, Evan L. Fogel, Lee McHenry, Glen A. Lehman
Digestive Diseases and Sciences.2016; 61(8): 2426. CrossRef - Bile Flow Phantom Model and Animal Bile Duct Dilation Model for Evaluating Biliary Plastic Stents with Advanced Hydrophilic Coating
Chang-Il Kwon, Gwangil Kim, Seok Jeong, Won Seop Lee, Don Haeng Lee, Kwang Hyun Ko, Sung Pyo Hong, Ki Baik Hahm
Gut and Liver.2016; 10(4): 632. CrossRef - Spontaneous Common Bile Duct Perforation Treated with Placement of Metal Stent
Dong Hoon Yang, Sang Wook Park, Hyeung Chul Moon, Kyoung Wan You, Seo Joon Eun, Seung Ki Moon, Choel Min Bak, Shin Hyoung Jo
Korean Journal of Pancreas and Biliary Tract.2016; 21(4): 222. CrossRef - Reintervention for occluded metal stent in malignant bile duct obstruction: A prospective randomized trial comparing covered and uncovered metal stent
Ban Seok Lee, Ji Kon Ryu, Dong Kee Jang, Kwang Hyun Chung, Won Jae Yoon, Jaihwan Kim, Sang Myung Woo, Sang Hyub Lee, Woo Jin Lee, Yong‐Tae Kim
Journal of Gastroenterology and Hepatology.2016; 31(11): 1901. CrossRef - Resolution of pneumobilia as a predictor of biliary stent occlusion
Stephen Thomas, Rina P. Patel, Aytekin Oto
Clinical Imaging.2015; 39(4): 650. CrossRef - Initial experience with endoscopic retrograde cholangiography and endoscopic retrograde biliary stenting for treatment of extrahepatic bile duct obstruction in dogs
Allyson Berent, Chick Weisse, Mark Schattner, Hans Gerdes, Peter Chapman, Michael Kochman
Journal of the American Veterinary Medical Association.2015; 246(4): 436. CrossRef - Recent Advances in Gastrointestinal Stent Development
Jin-Seok Park, Seok Jeong, Don Haeng Lee
Clinical Endoscopy.2015; 48(3): 209. CrossRef - Stents with specialized functions: drug-eluting stents and stents with antireflux devices
Sung Ill Jang, Dong Ki Lee
Gastrointestinal Intervention.2015; 4(1): 50. CrossRef - Prótesis metálica autoexpandible en el tratamiento de la estenosis del colédoco postrasplante de hígado en un niño. A propósito de un caso
Gerardo Blanco Rodríguez, Juan Manuel Blancas Valencia, Gustavo Varela Fascinetto, José Alejandro Hernández Plata, Juan Manuel Alcantar Fierros, Gustavo Teyssier Morales, Jaime Penchyna Grub
Endoscopia.2014; 26(4): 128. CrossRef - Polyurethane membrane with porous surface for controlled drug release in drug eluting stent
Eun Ha Seo, Kun Na
Biomaterials Research.2014;[Epub] CrossRef
- Anti-fibrotic and anti-stricture effects of biodegradable biliary stents braided with dexamethasone-impregnated sheath/core structured monofilaments
- 9,453 View
- 75 Download
- 28 Crossref

- Angular Positioning of Stent Increases Bowel Perforation after Self-Expandable Metal Stent Placement for Malignant Colorectal Obstruction
- Jeong Guil Lee, Kwang Ho Yoo, Chang-Il Kwon, Kwang Hyun Ko, Sung Pyo Hong
- Clin Endosc 2013;46(4):384-389. Published online July 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.4.384
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Some factors like stent wires, balloon dilatation and use of guide wires seems to increase perforation after self-expandable metal stent (SEMS) placement, but few studies mentioned about the relationship between angulation of malignant stricture and perforation. The present study aimed to confirm that more angular positioning of stents increases perforation.
Methods This study was conducted with retrospectively evaluation at Digestive Disease Center, CHA Bundang Medical Center, CHA University. Between January 2002 and August 2011, SEMS was inserted in 130 patients with malignant colorectal obstruction. We studied the difference in the angle of stenosis between perforation and non-perforation groups using fluorography images.
Results SEMS insertion was performed in 130 cases of obstruction due to colon cancer. Perforation occurred in eight patients (6.2%) of them. Thirteen cases were excluded from the analysis due to poor fluoroscopic images. Among the eight patients with perforation, the mean stenosis angle was 109.9° compared to 153.1° in the nonperforation group, indicating that the angle was more acute in the perforation group (
p =0.016).Conclusions This study shows that more angular positioning of stent increases bowel perforation after SEMS placement for malignant colorectal obstruction.
-
Citations
Citations to this article as recorded by- Analysis of Reported Adverse Events With Colonic Stents: An FDA MAUDE Database Study
Chong-Chi Chiu, Kuo-Chuan Hung, Li-Ren Yeh
Journal of Clinical Gastroenterology.2023; 57(6): 640. CrossRef - Clinical outcomes of colorectal stenting
S.V. Davydova, A.G. Fedorov, O.A. Yun, A.E. Klimov
Endoskopicheskaya khirurgiya.2023; 29(6): 12. CrossRef - Colonic stenting for malignant obstructions-A review of current indications and outcomes
Amelie Lueders, Gabie Ong, Peter Davis, Jonathan Weyerbacher, Jonathan Saxe
The American Journal of Surgery.2022; 224(1): 217. CrossRef - Comparison of different types of covered self-expandable metal stents for malignant colorectal obstruction
Joon Seop Lee, Hyun Seok Lee, Eun Soo Kim, Min Kyu Jung, Jin Tae Jung, Ho Gak Kim, Dong Wook Lee, Dae Jin Kim, Yoo Jin Lee, Chang Heon Yang
Surgical Endoscopy.2021; 35(8): 4124. CrossRef - Self‐expanding metallic stent improves histopathological edema compared with transanal drainage tube for malignant colorectal obstruction
Hiroshi Takeyama, Kotaro Kitani, Tomoko Wakasa, Masanori Tsujie, Yoshinori Fujiwara, Shigeto Mizuno, Masao Yukawa, Yoshio Ohta, Masatoshi Inoue
Digestive Endoscopy.2016; 28(4): 456. CrossRef - Oncologic safety of self-expanded metal stent insertion as a bridge to elective surgery in malignant colorectal obstruction
Se Hui Oh, Nak Jun Choi, Sang Hyuk Seo, Min Sung An, Kwang Hee Kim, Ki Beom Bae, Jin Won Hwang, Sang Heon Lee, Ji Hyun Kim, Sam Ryong Jee, Mi Seon Kang, Kwan Hee Hong
Korean Journal of Clinical Oncology.2016; 12(1): 48. CrossRef - Enteral stent construction: Current principles
Hans-Ulrich Laasch, Derek W. Edwards, Ho-Young Song
International Journal of Gastrointestinal Intervention.2016; 5(2): 85. CrossRef - Comparison of through-the-scope stent insertion with standard stent insertion for the management of malignant colorectal obstruction: a prospective study
Y. Wan, Y.-Q. Zhu, N.-W. Chen, Z.-G. Wang, Y.-S. Cheng, J. Shi
Techniques in Coloproctology.2016; 20(10): 707. CrossRef - Intestinal Stricture in Crohn's Disease
Chen-Wang Chang, Jau-Min Wong, Chien-Chih Tung, I-Lun Shih, Horng-Yuan Wang, Shu-Chen Wei
Intestinal Research.2015; 13(1): 19. CrossRef - Predictive Factors for Successful Colonic Stenting in Acute Large-Bowel Obstruction
Derek J. Boyle, Christopher Thorn, Ashish Saini, Colin Elton, Gary K. Atkin, Ian C. Mitchell, Kevin Lotzof, Adrian Marcus, Pawan Mathur
Diseases of the Colon & Rectum.2015; 58(3): 358. CrossRef - Stents for colonic strictures: Materials, designs, and more
Nandakumar Srinivasan, Richard A. Kozarek
Techniques in Gastrointestinal Endoscopy.2014; 16(3): 100. CrossRef - Patients who failed endoscopic stenting for left-sided malignant colorectal obstruction suffered the worst outcomes
Tian-Zhi Lim, Dedrick Chan, Ker-Kan Tan
International Journal of Colorectal Disease.2014; 29(10): 1267. CrossRef
- Analysis of Reported Adverse Events With Colonic Stents: An FDA MAUDE Database Study
- 7,008 View
- 59 Download
- 12 Crossref

- Unusual Complications Related to Endoscopic Retrograde Cholangiopancreatography and Its Endoscopic Treatment
- Chang-Il Kwon, Sang Hee Song, Ki Baik Hahm, Kwang Hyun Ko
- Clin Endosc 2013;46(3):251-259. Published online May 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.3.251
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Endoscopic retrograde cholangiopancreatography (ERCP)-induced complications, once occurred, can lead to significant morbidity. Commonly 5% to 10% of patients experience procedure related complications such as post-ERCP pancreatitis, biliary hemorrhage, and cholangitis, in descending order. However, complications such as perforation, pneumothorax, air embolism, splenic injury, and basket impaction are rare but are associated with high mortality if occurred. Such unexpected unusual complications might extend the length of hospitalization, require urgent surgical intervention, and put the patient in miserable condition leading to permanent disability or mortality. Although these ERCP-induced complications can be minimized by a skilled operator using advanced techniques and devices, the occurrence of unusual complications are hard to expect and induce very difficult management condition. In this review, we will focus on the uncommon complications related to ERCP. This review is also aimed at suggesting optimal endoscopic treatment strategies for several complications based on our institutional experiences.
-
Citations
Citations to this article as recorded by- Cystic duct disimpaction for acute cholecystitis in the high-risk cholecystectomy patient: Case report
Humzah Iqbal, Aalam Sohal, Kanana Aburayyan, Bandhul Hans, Juliana Yang
SAGE Open Medical Case Reports.2024;[Epub] CrossRef - Emergency digital cholangioscopy-assisted electrohydraulic lithotripsy for basket impaction with an entrapped bile duct stone
Akane Hara, Kosuke Minaga, Yasuo Otsuka, Hidekazu Tanaka, Mamoru Takenaka, Masatoshi Kudo
Endoscopy International Open.2024; 12(02): E271. CrossRef - A Study on the Spectrum of Imaging Findings of Post-ERCP-Specific Complications: A Retrospective Descriptive Study
Ruchira Mukherji, Manoj Gopinath
Indian Journal of Radiology and Imaging.2024;[Epub] CrossRef - Management of ERCP complications
Partha Pal, Mohan Ramchandani
Best Practice & Research Clinical Gastroenterology.2024; 69: 101897. CrossRef - Outcomes of ERCP in Patients With Cystic Fibrosis
Salman Haider, Daryl Ramai, Saira Shah, Nayna D. Riyat, Marco Spadaccini, Saurabh Chandan, Marcello Maida, Asad Ur Rehman, Monique T. Barakat
Journal of Clinical Gastroenterology.2024;[Epub] CrossRef - Prophylactic cholecystectomy offers best outcomes following ERCP clearance of common bile duct stones: a meta-analysis
Gearóid Mc Geehan, Conor Melly, Niall O’ Connor, Gary Bass, Shahin Mohseni, Magda Bucholc, Alison Johnston, Michael Sugrue
European Journal of Trauma and Emergency Surgery.2023; 49(5): 2257. CrossRef - Subcapsular Biloma following Endoscopic Retrograde Cholangiopancreatography and Endoscopic Biliary Sphincterotomy: A Case Report with a Mini Review of Literature
Natalia Valeria Pentara, Aristidis Ioannidis, Georgios Tzikos, Leonidas Kougias, Eleni Karlafti, Angeliki Chorti, Despoina Tsalkatidou, Antonios Michalopoulos, Daniel Paramythiotis
Diagnostics.2023; 13(5): 831. CrossRef - HEMATOMA POST-ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY. AN ANALYSIS OF THREE CASES
Sandra Díez Ruiz, Irene Latras Cortés, Sandra Borrego Rivas, Víctor Blázquez Ávila, Marcos Jiménez Palacios, Rubén Díez Rodríguez, Jesús Espinel Díez, Francisco Jorquera Plaza
Revista Española de Enfermedades Digestivas.2023;[Epub] CrossRef - Gas spread following endoscopic sphincterotomy: Challenging diagnosis and management: A case reports
Asma Sghaier, Khalil Fradi, Amine El Ghali, Khaireddine Dhouioui, Fehmi Hamila, Sabri Youssef
International Journal of Surgery Case Reports.2023; 108: 108487. CrossRef - Gas Embolism After a Patient's Ninth ERCP Procedure
Helal Said Ahmad, Sari Anne Cohen, Tawfik Khoury, Riad Tome, Haitam Zeibak, Wisam Abboud, Amir Mari
ACG Case Reports Journal.2023; 10(8): e01124. CrossRef - ERCP in patients over 90 years old: Safety and efficacy comparison with a younger cohort
Ana E Colmenero Gargari, Fernando E Melgar Somoza, Jorge Vera, Carlos G Micames
Endoscopy International Open.2023; 11(09): E893. CrossRef - Endoscopic management of upper gastrointestinal perforations, leakage and fistula
Hee Seok Moon
Journal of Innovative Medical Technology.2023; 1(1): 15. CrossRef - Rare post-endoscopic retrograde cholangiopancreatography complications: Can we avoid them?
Marta Aleksandra Przybysz, Rafał Stankiewicz
World Journal of Meta-Analysis.2022; 10(3): 122. CrossRef - Fatal Venous Gas Embolism During Endoscopic Retrograde Cholangiopancreatography After Simultaneous Deployment of 2 Self-Expandable Metallic Stents
Justin Chuang, Rebecca Kuang, Ajit Ramadugu, Dipen Patel, Sachit Sharma, Kishan Shrestha, Jordan Burlen, Ali Nawras
ACG Case Reports Journal.2022; 9(10): e00873. CrossRef - Best practices for prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis
Simcha Weissman, Mohamed Ahmed, Matthew R Baniqued, Dean Ehrlich, James H Tabibian
World Journal of Gastrointestinal Endoscopy.2021; 13(6): 161. CrossRef - Nonsurgical rescue after basket-stone impaction by endoscopic cutting of a metallic lithotripter and laser lithotripsy
Toshiaki Terauchi, Satoshi Shinozaki, Masazumi Inoue, Alan Kawarai Lefor, Hiroharu Shinozaki
VideoGIE.2021; 6(9): 416. CrossRef - Splenic laceration following endoscopic retrograde cholangiopancreatography: A literature review and our experience
Kan Wang, Yanfei Fang, Aihua Huang, Min Gao
Laparoscopic, Endoscopic and Robotic Surgery.2020; 3(3): 80. CrossRef - Gallstone Dislodgement in the Airway during ERCP: A Case Report and Review of the Literature
Hisham Hurreiz, Amira Babikir, Edward Black
Case Reports in Gastrointestinal Medicine.2020; 2020: 1. CrossRef - Experiencia de cinco años en el manejo de pacientes con alto riesgo de coledocolitiasis
Josué Israel Olivares del Moral, José Augusto Rodríguez Osuna, Danyel Chávez Fernández, José Cruz De la Torre Gonzáles, Ramiro Gómez-Arámbulo, Efrén Flores-Álvarez, José de Jesús Marín-López
Revista Mexicana de Cirugía Endoscópica.2020; 21(1): 26. CrossRef - Retracted: Endoscopic Treatment of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
Ding Shi, Jian feng Yang, Yong pan Liu
Journal of Laparoendoscopic & Advanced Surgical Techniques.2019; 29(3): 385. CrossRef - Complications of endoscopic retrograde cholangiopancreatography: an imaging review
Dinesh Manoharan, Deep Narayan Srivastava, Arun Kumar Gupta, Kumble Seetharama Madhusudhan
Abdominal Radiology.2019; 44(6): 2205. CrossRef -
COMPARATIVE EVALUATION OF RADIcitation_listOGICAL IMAGING RESULTS OF CHcitation_listEDOCHcitation_listITHIASIS IN PATIENTS WITH ACUTE CALCULOUS CHcitation_listECYSTITIS
V. I. Kolomiytsev, O. M. Terletskiy, M. M. Bufan
Bulletin of Problems Biology and Medicine.2019; 2.1(150): 236. CrossRef - Intrahepatic subcapsular biloma after endoscopic retrograde cholangiopancreatography treated by endoscopic biliary drainage
Hiroaki Igarashi, Hiroko Yamashita, Kiyoshi Tsuchiya, Dai Sugimoto, Itsuro Ogata
Clinical Journal of Gastroenterology.2018; 11(2): 167. CrossRef - Embolía pulmonar aérea secundaria a colangiopancreatografía retrógrada endoscópica en una paciente con trasplante hepático. Reporte de caso.
Gustavo Adolfo Reyes, Renzo Pinto Carta, Fernando Sierra Arango, Luis Felipe Cabrera Vargas
Revista Colombiana de Gastroenterología.2018; 33(4): 464. CrossRef - Cerebral air embolism after ERCP
Sonia Trabanco, Sara Pardo, Mónica Williams, Javier Diaz, Cristina Ruiz
Journal of Clinical Anesthesia.2017; 36: 133. CrossRef - Bilateral Pneumothoraces as a Complication of Endoscopic Retrograde Cholangiopancreatography
Douglas E. Rappaport, Joshua J. Solano, Jonathan A. Edlow
The Journal of Emergency Medicine.2017; 52(4): 573. CrossRef - Cholangitis after endoscopic retrograde cholangiopancreatography: a rare complication?
Armando Peixoto, Marco Silva, Guilherme Macedo
Revista Española de Enfermedades Digestivas.2017;[Epub] CrossRef - Training in Endoscopy: Endoscopic Retrograde Cholangiopancreatography
Jaihwan Kim
Clinical Endoscopy.2017; 50(4): 334. CrossRef - The role of endoscopic ultrasound in children with Pancreatobiliary and gastrointestinal disorders: a single center series and review of the literature
Alessandro Fugazza, Barbara Bizzarri, Federica Gaiani, Marco Manfredi, Alessia Ghiselli, Pellegrino Crafa, Maria Clotilde Carra, Nicola de’Angelis, Gian Luigi de’Angelis
BMC Pediatrics.2017;[Epub] CrossRef - ERCP–Related Duodenal Perforation; The Prevention and Management
Hong Ja Kim, Seon Mee Park
Korean Journal of Pancreas and Biliary Tract.2016; 21(2): 61. CrossRef - Upper gastrointestinal endoscopy: expected post-procedural findings and adverse events
Tarek N. Hanna, Saurabh Rohatgi, Haris N. Shekhani, Fatima Shahid, Vijayanadh Ojili, Faisal Khosa
Emergency Radiology.2016; 23(5): 503. CrossRef - Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations
Seon Mee Park
Clinical Endoscopy.2016; 49(4): 376. CrossRef - Complications of ERCP
Rupjyoti Talukdar
Best Practice & Research Clinical Gastroenterology.2016; 30(5): 793. CrossRef - Parenchymal Guidewire Perforation during ERCP: An Unappreciated Injury
M. Ezzedien Rabie, Saad Al Faris, Ali Nasser, Abdul Aziz Shahir, Yasser Al Mahdi, Mansour Youssef Al Asmari
Case Reports in Surgery.2015; 2015: 1. CrossRef - Retroperitoneales Emphysem nach endoskopischer retrograder Cholangiopankreatikographie
T. Vowinkel, N. Senninger
Der Chirurg.2015; 86(5): 462. CrossRef - Duodenal Perforations After Endoscopic Retrograde Cholangiopancreatography
María Desirée Armas Ojeda, Vanesa Ojeda Marrero, Cristina Roque Castellano, José Carlos Cabrera Marrero, María del Pino Mathías Gutierrez, Daniel Ceballos Santos, Joaquín Marchena Gómez
Cirugía Española (English Edition).2015; 93(6): 403. CrossRef - Perforaciones duodenales tras colangiopancreatografía retrógrada endoscópica
María Desirée Armas Ojeda, Vanesa Ojeda Marrero, Cristina Roque Castellano, José Carlos Cabrera Marrero, María del Pino Mathías Gutierrez, Daniel Ceballos Santos, Joaquín Marchena Gómez
Cirugía Española.2015; 93(6): 403. CrossRef - Huge biloma after endoscopic retrograde cholangiopancreatography and endoscopic biliary sphincterotomy
Harith M. Alkhateeb, Thaer J. Aljanabi, Khairallh H. Al-azzawi, Taha A. Alkarboly
International Journal of Surgery Case Reports.2015; 16: 7. CrossRef - Cross-sectional imaging of common and unusual complications after endoscopic retrograde cholangiopancreatography
Massimo Tonolini, Alessandra Pagani, Roberto Bianco
Insights into Imaging.2015; 6(3): 323. CrossRef - Acute Air Embolism during Retrograde Cholangiography for Postoperative Recurrent Cholangitis Due to Intraductal Residual Meals after Choledochoduodenostomy
Osamu Miyoshi, Shu Nakano
The Japanese Journal of Gastroenterological Surger.2015; 48(5): 463. CrossRef - Early endoscopic ultrasonography in acute biliary pancreatitis: A prospective pilot study
Andrea Anderloni
World Journal of Gastroenterology.2015; 21(36): 10427. CrossRef - ERCP-induced duodenal perforation successfully treated with endoscopic purse-string suture: a case report
Quanpeng Li, Jie Ji, Fei Wang, Xianxiu Ge, Junjie Nie, Boming Xu, Xiuhua Zhang, Guobing Jiang, Lin Miao
Oncotarget.2015; 6(19): 17847. CrossRef - Development of a swine bile duct dilation model using endoclips or a detachable snare under cap-assisted endoscopy
Jin-Seok Park, Chang-Il Kwon, Seok Jeong, Kwangil Kim, Jong Ho Moon, Don Haeng Lee
Gastrointestinal Endoscopy.2014; 80(2): 325. CrossRef - Rare and underappreciated complications of endoscopic retrograde cholangiopancreatography
Ji Young Bang, Gregory A. Coté
Techniques in Gastrointestinal Endoscopy.2014; 16(4): 195. CrossRef - Air Embolism after Endoscopic Retrograde Cholangiopancreatography in a Patient with Budd Chiari Syndrome
Beatriz Wills-Sanin, Yenny R. Cárdenas, Lucas Polanco, Oscar Rivero, Sebastian Suarez, Andrés F. Buitrago
Case Reports in Critical Care.2014; 2014: 1. CrossRef - Endoscopic retrograde cholangiopancreatography-related perforation: Management and prevention
Varayu Prachayakul
World Journal of Clinical Cases.2014; 2(10): 522. CrossRef - Emergencies after endoscopic procedures
Carla Rolanda, Ana C. Caetano, Mário Dinis-Ribeiro
Best Practice & Research Clinical Gastroenterology.2013; 27(5): 783. CrossRef - Endoscopic Treatments of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
Tae Hoon Lee, Joung-Ho Han, Sang-Heum Park
Clinical Endoscopy.2013; 46(5): 522. CrossRef
- Cystic duct disimpaction for acute cholecystitis in the high-risk cholecystectomy patient: Case report
- 9,646 View
- 167 Download
- 48 Crossref

- Balloon Catheter Assisted Biliary Stent Insertion
- Chang-Il Kwon, Kwang Hyun Ko
- Clin Endosc 2013;46(2):201-202. Published online March 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.2.201
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Differentiated approach of using extraction balloon catheters in endoscopic biliary surgery
A. E. Kotovskiy, B. M. Magomedova, K. G. Glebov, A. A. Martyntsov, A. K. Mahmudova, A. S. Prividentseva
Annaly khirurgicheskoy gepatologii = Annals of HPB Surgery.2021; 26(3): 123. CrossRef
- Differentiated approach of using extraction balloon catheters in endoscopic biliary surgery
- 4,200 View
- 35 Download
- 1 Crossref

- Endoscopic Submucosal Dissection (ESD) Training and Performing ESD with Accurate and Safe Techniques
- Chang-Il Kwon
- Clin Endosc 2012;45(4):347-349. Published online November 30, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.4.347
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Introduction of endoscopic submucosal dissection (ESD) has brought about a renaissance in therapeutic endoscopy. For the globalization and universalization of ESD, the number of physicians who can perform ESD has rapidly increased with general
ex vivo andin vivo training using animal models and hand-on courses. In this focused review series, world-renowned ESD experts described the published studies or their own precious experiences about ESD training and performing ESD with accurate and safe techniques. First, Dr. Adolfo Parra-Blanco reviewed onex vivo andin vivo models for ESD training. Next, Dr. Joo Young Cho described detailed practical settings and current status of hands-on courses usingex vivo andin vivo models in Korea. Dr. Takashi Toyonaga described quality controlled ESD and basic techniques to prevent complications. Dr. Tsuneo Oyama reviewed recently published methods to facilitate ESD. Dr. Jae-Young Jang reviewed the usefulness of magnifying and narrow band imaging to measure the depth of invasion before ESD.-
Citations
Citations to this article as recorded by- Endoscopic submucosal dissection training: evaluation of an ex vivo training model with continuous perfusion (ETM-CP) for hands-on teaching and training in China
Jun Huang, Bing-ran Du, Wei-guang Qiao, Si-lin Huang, Lan-feng Xue, Liang Deng, Jun-ming Liang, Jun Wang, Jian-yi Li, Yu Chen
Surgical Endoscopy.2023; 37(6): 4774. CrossRef - Disección endoscópica submucosa: curva de aprendizaje en modelos porcinos
Victor Efrén Gallardo Cabrera, Oscar Hernández Mondragón, Dulce María Rascón Martínez, Gerardo Blanco Velasco, Roberto Ramos González, Amina Evelyn Tun Abraham, Juan Manuel Blancas Valencia
Endoscopia.2015; 27(3): 109. CrossRef - Training in endoscopic submucosal dissection
Roxana M Coman
World Journal of Gastrointestinal Endoscopy.2013; 5(8): 369. CrossRef
- Endoscopic submucosal dissection training: evaluation of an ex vivo training model with continuous perfusion (ETM-CP) for hands-on teaching and training in China
- 5,109 View
- 66 Download
- 3 Crossref

- An Impacted Pancreatic Stone in the Papilla Induced Acute Obstructive Cholangitis in a Patient with Chronic Pancreatitis
- Kwang-Ho Yoo, Chang-Il Kwon, Sang-Wook Yoon, Won Hee Kim, Jung Min Lee, Kwang Hyun Ko, Sung Pyo Hong, Pil Won Park
- Clin Endosc 2012;45(1):99-102. Published online March 31, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.1.99
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Obstructive jaundice is very rarely caused by impaction of a pancreatic stone in the papilla. We report here on a case of obstructive jaundice with acute cholangitis that was caused by an impacted pancreatic stone in the papilla in a patient with chronic pancreatitis. A 48-year-old man presented with acute obstructive cholangitis. Abdominal computed tomography with the reconstructed image revealed distal biliary obstruction that was caused by a pancreatic stone in the pancreatic head, and there was also pancreatic ductal dilatation and parenchymal atrophy of the pancreatic body and tail with multiple calcifications. Emergency duodenoscopy revealed an impacted pancreatic stone in the papilla. Precut papillotomy using a needle knife was performed, followed by removal of the pancreatic stone using grasping forceps. After additional sphincterotomy, a large amount of dark-greenish bile juice gushed out. The patient rapidly improved and he has remained well.
-
Citations
Citations to this article as recorded by- Pancreatic stones causing secondary biliary obstruction: An uncommon presentation of chronic pancreatitis
Wesley C. Judy, Tom K. Lin
JPGN Reports.2024;[Epub] CrossRef - The “squeezing with forceps” method for emergency endoscopic removal of an impacted pancreatic stone in the papilla of a patient on antithrombotic therapy
Sho Kitagawa, Shori Ishikawa, Keiya Okamura
Endoscopy.2023; 55(S 01): E454. CrossRef - Biliary Outlet Obstruction Due to Pancreatic Calculi in a Post-cholecystectomy Patient
Joey Almaguer, Dylan Murray, Matthew Murray, Richard Murray
Cureus.2023;[Epub] CrossRef - Ampullary stone in chronic pancreatitis causing obstructive jaundice and cholangitis
Sandheep Janardhanan, Allwin James, Alagammai Palaniappan, Ramesh Ardhanari
Gastroenterology, Hepatology and Endoscopy Practice.2021; 1(2): 69. CrossRef - Ursodeoxycholic acid attenuates 5‑fluorouracil‑induced mucositis in a rat model
Seung Kim, Hoon Chun, Hyuk Choi, Eun Kim, Bora Keum, Yeon Seo, Yoon Jeen, Hong Lee, Soon Um, Chang Kim
Oncology Letters.2018;[Epub] CrossRef - Pancreatic Calculus Causing Biliary Obstruction: Endoscopic Therapy for a Rare Initial Presentation of Chronic Pancreatitis
Anurag J. Shetty, C. Ganesh Pai, Shiran Shetty, Girisha Balaraju
Digestive Diseases and Sciences.2015; 60(9): 2840. CrossRef
- Pancreatic stones causing secondary biliary obstruction: An uncommon presentation of chronic pancreatitis
- 5,951 View
- 50 Download
- 6 Crossref


 KSGE
KSGE

 First
First Prev
Prev