Search
- Page Path
- HOME > Search
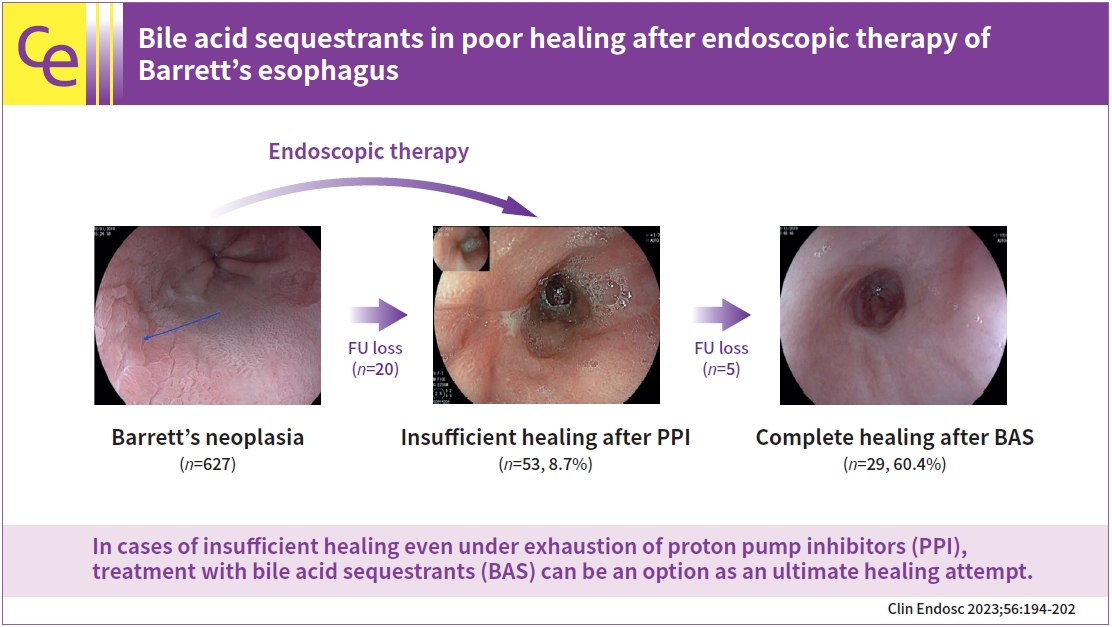
- Bile acid sequestrants in poor healing after endoscopic therapy of Barrett’s esophagus
- Lukas Welsch, Andrea May, Tobias Blasberg, Jens Wetzka, Elisa Müller, Myriam Heilani, Mireen Friedrich-Rust, Mate Knabe
- Clin Endosc 2023;56(2):194-202. Published online March 9, 2023
- DOI: https://doi.org/10.5946/ce.2022.121
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 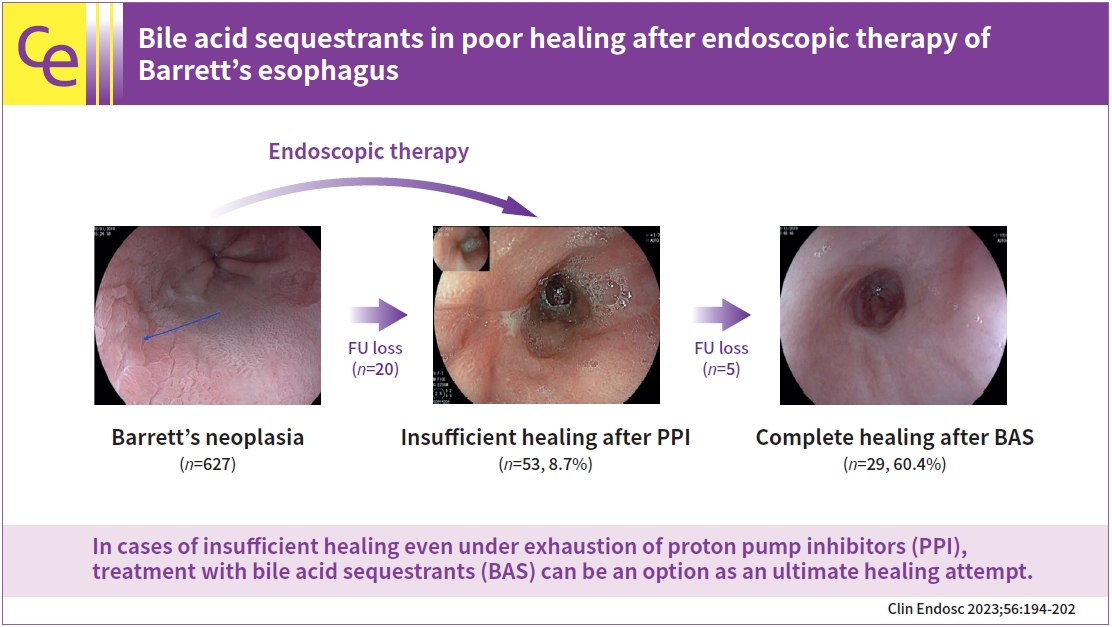
- Background
/Aims: Endoscopic therapy for neoplastic Barrett’s esophagus (BE) has become the standard of care over the past two decades. In clinical practice, we regularly encounter patients who fail to achieve complete squamous epithelialization of the esophagus. Although the therapeutic strategies in the individual stages of BE, dysplasia, and esophageal adenocarcinoma are well studied and largely standardized, the problem of inadequate healing after endoscopic therapy is only marginally considered. This study aimed to shed light on the variables influencing inadequate wound healing after endoscopic therapy and the effect of bile acid sequestrants (BAS) on healing.
Methods
Retrospective analysis of endoscopically treated neoplastic BE in a single referral center.
Results
In 12.1% out of 627 patients, insufficient healing was present 8 to 12 weeks after previous endoscopic therapy. The average follow-up duration was 38.8±18.4 months. Complete healing was achieved in 13 patients already after intensifying proton pump inhibitor therapy. Out of 48 patients under BAS, 29 patients (60.4%) showed complete healing. An additional eight patients (16.7%) improved, but only partial healing was achieved. Eleven (22.9%) patients showed no response to BAS augmented therapy.
Conclusions
In cases of insufficient healing even under exhaustion of proton pump inhibitors, treatment with BAS can be an option as an ultimate healing attempt. -
Citations
Citations to this article as recorded by
- 2,516 View
- 160 Download
- 1 Web of Science
- 2 Crossref

- Endoscopic Approach for Major Complications of Bariatric Surgery
- Moon Kyung Joo
- Clin Endosc 2017;50(1):31-41. Published online December 23, 2016
- DOI: https://doi.org/10.5946/ce.2016.140
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - As lifestyle and diet patterns have become westernized in East Asia, the prevalence of obesity has rapidly increased. Bariatric surgeries, such as Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (SG), and laparoscopic adjustable gastric banding (LAGB), are considered the first-line treatment option in patients with severe obesity. However, postoperative complications have increased and the proper management of these complications, including the use of endoscopic procedures, has become important. The most serious complications, such as leaks and fistulas, can be treated with endoscopic stent placement and injection of fibrin glue, and a novel full-thickness closure over-the-scope clip (OTSC) has been used for treatment of postoperative leaks. Stricture at the gastrojejunal (GJ) anastomosis site after RYGB or incisura angularis in SG can be managed using stents or endoscopic balloon dilation. Dilation of the GJ anastomosis or gastric pouch may lead to failure of weight loss, and the use of endoscopic sclerotherapy, novel endoscopic suturing devices, and OTSCs have been attempted. Intragastric migration of the gastric band can be successfully treated using various endoscopic tools. Endoscopy plays a pivotal role in the management of post-bariatric complications, and close cooperation between endoscopists and bariatric surgeons may further increase the success rate of endoscopic procedures.
-
Citations
Citations to this article as recorded by- Advanced endolumenal management of acute and chronic leaks after bariatric surgery
Andrew R. Harner, Francisco Jr Guerra, Shinil K. Shah, Kulvinder S. Bajwa, Peter A. Walker, Erik B. Wilson, Melissa M. Felinski
Mini-invasive Surgery.2024;[Epub] CrossRef - Current Management and Treatment Paradigms of Gastroesophageal Reflux Disease following Sleeve Gastrectomy
Muaaz Masood, Donald E. Low, Shanley B. Deal, Richard A. Kozarek
Journal of Clinical Medicine.2024; 13(5): 1246. CrossRef - Endoscopic Management of Post-Sleeve Gastrectomy Complications
Muaaz Masood, Donald E. Low, Shanley B. Deal, Richard A. Kozarek
Journal of Clinical Medicine.2024; 13(7): 2011. CrossRef - A Systemic Review on Photodynamic Therapy: Emerging Technology with
Healing Process
Prachi Varshney, Yogesh Kumar, Devdhar Yadav, Amit Singh, Naga Rani Kagithala, Pramod Kumar Sharma, Omji Porwal, Neeraj Kumar Fuloria, Pradeep Kumar Sharma, Ashok Kumar Gupta, G.S.N. Koteswara Rao
Current Cancer Therapy Reviews.2024; 20(3): 283. CrossRef - Endoscopic closure techniques of bariatric surgery complications: a meta-analysis
William N. Doyle, Alexander Netzley, Rahul Mhaskar, Abdul-Rahman F. Diab, Samer Ganam, Joseph Sujka, Christopher DuCoin, Salvatore Docimo
Surgical Endoscopy.2024; 38(5): 2894. CrossRef - Digestive neo-epithelialization after endoscopic stenting for upper digestive tract complete disunion
Sohaib Ouazzani, Arnaud Lemmers, Jean-Michel Gonzalez, Jean Closset, Imad El Moussaoui, Jacques Devière, Marc Barthet
Endoscopy.2024;[Epub] CrossRef - The Efficacy and Safety of Endoscopic Balloon Dilatation in the Treatment of Functional Post-Sleeve-Gastrectomy Stenosis
Mohamed A. Elsebaey, Mohamed Elsayed Enaba, Heba Elashry, Waleed Elrefaey, Rasha Youssef Hagag, Neveen A. Shalaby, Mohamed Sabry Aboelnasr, Mohamed Elsayed Sarhan, Omneya Mohamed Darrag, Assem Mohamed Elsokkary, Mohamed Abd Allah Alabd, Ahmed Mohamed El N
Medicina.2024; 60(5): 833. CrossRef - Bariatric Surgery Emergencies in Acute Care Surgery
Kalyana C. Nandipati, Kristin C. Bremer
Surgical Clinics of North America.2023; 103(6): 1113. CrossRef - Massive enlargement of gastric pouch as a complication of gastrojejunal anastomotic stenosis following one anastomosis laparoscopic gastric bypass: A case report
A. Martel-Vilchis, V. Gallardo-Chavez, P. León-Cabral, A. Paz-Fernández, E. Luna-Martinez, M. Sierra-Salazar
International Journal of Surgery Case Reports.2023; 110: 108557. CrossRef - Unexplained recurrent left lower lobe pneumonia, haematemesis and splenomegaly in a 32‐year‐old gentleman
Cynthuja Thilakanathan, Matthew Hall, Wassim Rahman, Mark Magdy, John Jorgensen
ANZ Journal of Surgery.2022; 92(1-2): 258. CrossRef - An innovative endoscopic management strategy for postoperative fistula after laparoscopic sleeve gastrectomy
Haiming Fang, Tingting Yao, Yating Chen, Yan Lu, Kangwei Xiong, Yuan Su, Yujue Zhang, Yong Wang, Lijiu Zhang
Surgical Endoscopy.2022; 36(9): 6439. CrossRef - Stent Management of Leaks After Bariatric Surgery: a Systematic Review and Meta-analysis
Andreu Martínez Hernández, Homero Beltrán Herrera, Vicente Martínez García, Miguel Ibáñez Belenguer, Raquel Queralt Martín, Ana Karina Maiocchi Segredo, Elena Aliaga Hilario, José Manuel Laguna Sastre
Obesity Surgery.2022; 32(4): 1034. CrossRef - Status of bariatric endoscopy–what does the surgeon need to know? A review
Diogo Turiani Hourneaux de Moura, Anna Carolina Batista Dantas, Igor Braga Ribeiro, Thomas R McCarty, Flávio Roberto Takeda, Marco Aurelio Santo, Sergio Carlos Nahas, Eduardo Guimarães Hourneaux de Moura
World Journal of Gastrointestinal Surgery.2022; 14(2): 185. CrossRef - Personalized Health Care Technology in Managing Postoperative Gastrointestinal Surgery Complications: Proof of Concept Study
Yaqeen Qudah, Mohammed Abdallah, Juan S. Barajas-Gamboa, Gabriel Diaz Del Gobbo, Juan Pablo Pantoja, Ricard Corcelles, John Rodriguez, Numan Balci, Matthew Kroh
Journal of Laparoendoscopic & Advanced Surgical Techniques.2022; 32(11): 1170. CrossRef - Role of Primary Use of Mega Stents Alone and Combined with Other Endoscopic Procedures for Early Leak and Stenosis After Bariatric Surgery, Single-Institution Experience
Mohamed Hany, Mohamed Ibrahim, Ahmed Zidan, Mohamed Samir, Amr Elsherif, Mohamed Selema, Mohamed Sharaan, Mohamed Elhashash
Obesity Surgery.2021; 31(5): 2050. CrossRef - A Comprehensive Review of Endoscopic Management of Sleeve Gastrectomy Leaks
Mihajlo Gjeorgjievski, Zaid Imam, Mitchell S. Cappell, Laith H. Jamil, Michel Kahaleh
Journal of Clinical Gastroenterology.2021; 55(7): 551. CrossRef - Foregut Issues After Bariatric Surgery
Fareed Cheema, Aurora D. Pryor
Foregut: The Journal of the American Foregut Society.2021; 1(4): 386. CrossRef - Endoscopic Stents in the Management of Bariatric Complications: Our Algorithm and Outcomes
Shyam Vedantam, Jay Roberts
Obesity Surgery.2020; 30(3): 1150. CrossRef - Mini gastric bypass for the management of gastrobronchial fistula: A case report
Abdulhamid Alharbi, Mohammed Alnaami, Abdulrahman Alsayyari, Mana Almuhaideb
International Journal of Surgery Case Reports.2020; 66: 192. CrossRef - Incidence and Efficacy of Stent Placement in Leak Management After Bariatric Surgery
Arielle E. Kanters, Sarah P. Shubeck, Oliver A. Varban, Justin B. Dimick, Dana A. Telem
Annals of Surgery.2020; 271(1): 134. CrossRef - Evolving procedural options for the treatment of obesity
Talar Tatarian, Kais A. Rona, Daniel H. Shin, Daniel G. Chen, Christopher G. Ducoin, Rachel L. Moore, Vitor O. Brunaldi, Manoel Galvão-Neto, Jessica Ardila-Gatas, Salvatore Docimo, Diogo T. Hourneax de Moura, Pichamol Jirapinyo, Christopher C. Thompson, H
Current Problems in Surgery.2020; 57(4): 100742. CrossRef - Endoscopic treatment of early leaks and strictures after laparoscopic one anastomosis gastric bypass
Fadi Younis, Mati Shnell, Nathan Gluck, Subhi Abu-Abeid, Shai Eldar, Sigal Fishman
BMC Surgery.2020;[Epub] CrossRef - Endoscopic balloon dilation for treatment of sleeve gastrectomy stenosis: a systematic review and meta-analysis
Steven H. Chang, Violeta B. Popov, Christopher C. Thompson
Gastrointestinal Endoscopy.2020; 91(5): 989. CrossRef - Long-term outcomes following endoscopic stenting in the management of leaks after foregut and bariatric surgery
Varun Krishnan, Kevin Hutchings, Andrew Godwin, Jonathan T. Wong, Julio Teixeira
Surgical Endoscopy.2019; 33(8): 2691. CrossRef - A Spanish Society joint SECO and SEEDO approach to the Post-operative management of the patients undergoing surgery for obesity
R Vilallonga, JL Pereira-Cunill, S Morales-Conde, I Alarcón, I Breton, E Domínguez-Adame, JV Ferrer, A Garcia Ruiz-de-Gordejuela, A Goday, A Lecube, E Martín García-Almenta, MÁ Rubio, FJ Tinahones, PP García-Luna
Obesity Surgery.2019; 29(12): 3842. CrossRef - Endoscopic Abscess Septotomy: A Less Invasive Approach for the Treatment of Sleeve Gastrectomy Leaks
Camila B. Ortega, Alfredo D. Guerron, Dana Portenier
Journal of Laparoendoscopic & Advanced Surgical Techniques.2018; 28(7): 859. CrossRef - Management of gastric fistula complicating laparoscopic sleeve gastrectomy with biological glue in a combined percutaneous and endoscopic approach
Ahmad Assalia, Anat Ilivitzki, Amos Ofer, Alain Suissa, Elias Manassa, Iyad Khamaysi, Ahmad Mahajna
Surgery for Obesity and Related Diseases.2018; 14(8): 1093. CrossRef - A Retrospective 2-Year Follow-up of Late Complications Treated Surgically and Endoscopically After Laparoscopic Roux-en-Y Gastric Bypass (LRYGB) and Laparoscopic Sleeve Gastrectomy (LSG) for Morbid Obesity
Mervi Javanainen, Anne Penttilä, Harri Mustonen, Anne Juuti, Tom Scheinin, Marja Leivonen
Obesity Surgery.2018; 28(4): 1055. CrossRef - Acute bleeding obstruction pancreatitis after Roux-en-Y anastomosis in total gastrectomy: a single center experience
J. Weindelmayer, S. Laiti, R. La Mendola, M. Bencivenga, L. Scorsone, V. Mengardo, S. Giacopuzzi
Updates in Surgery.2018; 70(2): 301. CrossRef - Management of Bariatric Complications Using Endoscopic Stents: a Multi-Center Study
Rena C. Moon, Andre F. Teixeira, Lyz Bezerra, Helga Cristina Almeida Wahnon Alhinho, Josemberg Campos, Luiz Gustavo de Quadros, Artagnan Menezes Barbosa de Amorim, Manoel Galvao Neto, Muhammad A. Jawad
Obesity Surgery.2018; 28(12): 4034. CrossRef - Endoscopic management of surgical complications
Robert J. Bowles-Cintron, Armando Perez-Ginnari, Jose M. Martinez
Techniques in Gastrointestinal Endoscopy.2018; 20(4): 182. CrossRef - A nutrition problem solved by a two-step endoscopic removal of a non-adjustable gastric band
Christer D Johansen, Jan Norum, Bernt E Engebretsen, Uwe Agledahl
Journal of Surgical Case Reports.2018;[Epub] CrossRef - Organization of future training in bariatric gastroenterology
Timothy R Koch, Timothy R Shope, Christopher J Gostout
World Journal of Gastroenterology.2017; 23(35): 6371. CrossRef
- Advanced endolumenal management of acute and chronic leaks after bariatric surgery
- 10,365 View
- 329 Download
- 31 Web of Science
- 33 Crossref

- Endoscopic Management of Tumor Bleeding from Inoperable Gastric Cancer
- Young-Il Kim, Il Ju Choi
- Clin Endosc 2015;48(2):121-127. Published online March 27, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.2.121
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Tumor bleeding is not a rare complication in patients with inoperable gastric cancer. Endoscopy has important roles in the diagnosis and primary treatment of tumor bleeding, similar to its roles in other non-variceal upper gastrointestinal bleeding cases. Although limited studies have been performed, endoscopic therapy has been highly successful in achieving initial hemostasis. One or a combination of endoscopic therapy modalities, such as injection therapy, mechanical therapy, or ablative therapy, can be used for hemostasis in patients with endoscopic stigmata of recent hemorrhage. However, rebleeding after successful hemostasis with endoscopic therapy frequently occurs. Endoscopic therapy may be a treatment option for successfully controlling this rebleeding. Transarterial embolization or palliative surgery should be considered when endoscopic therapy fails. For primary and secondary prevention of tumor bleeding, proton pump inhibitors can be prescribed, although their effectiveness to prevent bleeding remains to be investigated.
-
Citations
Citations to this article as recorded by- Endoscopic Management of Tumor Bleeding
Frances Dang, Marc Monachese
Gastrointestinal Endoscopy Clinics of North America.2024; 34(1): 155. CrossRef - State of the scientific evidence and recommendations for the management of older patients with gastric cancer
Irene Paredero-Pérez, Paula Jimenez-Fonseca, Juana María Cano, Virginia Arrazubi, Alberto Carmona-Bayonas, Marta Covela-Rúa, Ana Fernández-Montes, Marta Martín-Richard, Regina Gironés-Sarrió
Journal of Geriatric Oncology.2024; 15(3): 101657. CrossRef - The Chinese Society of Clinical Oncology (CSCO): Clinical guidelines for the diagnosis and treatment of gastric cancer, 2023
Feng‐Hua Wang, Xiao‐Tian Zhang, Lei Tang, Qi Wu, Mu‐Yan Cai, Yuan‐Fang Li, Xiu‐Juan Qu, Hong Qiu, Yu‐Jing Zhang, Jie‐Er Ying, Jun Zhang, Ling‐Yu Sun, Rong‐Bo Lin, Chang Wang, Hao Liu, Miao‐Zhen Qiu, Wen‐Long Guan, Sheng‐Xiang Rao, Jia‐Fu Ji, Yan Xin, Wei‐
Cancer Communications.2024; 44(1): 127. CrossRef - Meaning of Better Scoring System for the Patients with Cancer Bleeding in the Upper Gastrointestinal Tract
Ji Yong Ahn
Gut and Liver.2024; 18(2): 195. CrossRef - Complicated gastric cancer and modern treatment approaches
S.A. Tarasov, P.A. Yartsev, M.M. Rogal, S.O. Aksenova
Pirogov Russian Journal of Surgery.2024; (4): 125. CrossRef - Upper gastrointestinal bleeding as a warning sign of gastrointestinal cancer
Haozhe Cui, Qinglun Gao, Zhiming Zhao, Xiangming Ma
Preventive Medicine Reports.2024; 43: 102773. CrossRef - Hemostatic Powders in Non-Variceal Upper Gastrointestinal Bleeding: The Open Questions
Omero Alessandro Paoluzi, Edoardo Troncone, Elena De Cristofaro, Mezia Sibilia, Giovanni Monteleone, Giovanna Del Vecchio Blanco
Medicina.2023; 59(1): 143. CrossRef - A rare clinical case of primary multiple metachronous cancer: primary gastric melanoma and prostate cancer
Z.A. Bagateliya, D.N. Grekov, K.S. Titov, V.N. Yakomaskin, K.S. Kurdyukov, Z.A. Ibragimli
Onkologiya. Zhurnal imeni P.A.Gertsena.2023; 12(1): 28. CrossRef - New strategy in hemorrhagic gastric cancer: A case report of complete pathological remission after neoadjuvant chemotherapy
Yuhang Zhou, Yuchen Zhou, Xiaojun Lin, Shengtao Lin, Weihua Li
Medicine.2023; 102(6): e32789. CrossRef - Cross-phenotype association analysis of gastric cancer: in-silico functional annotation based on the disease–gene network
Sangjun Lee, Han-Kwang Yang, Hyuk-Joon Lee, Do Joong Park, Seong-Ho Kong, Sue K. Park
Gastric Cancer.2023; 26(4): 517. CrossRef - Mortality in patients with unresectable gastric cancer complicated with tumor bleeding
Edgardo Amaya, Angélica Hernández-Guerrero , José Guillermo de la Mora Levy, Mauro Eduardo Ramírez-Solís, J. Octavio Alonso-Lárraga, Luis Guillermo Beltrán-Galindo
Revista Española de Enfermedades Digestivas.2023;[Epub] CrossRef - Use of Endoscopic Suturing for the Treatment of Malignant Gastric Ulcer-Related Hemorrhage
Michael Andreone, Bryant Megna, Nicholas McDonald, Dharma Sunjaya, Brian Hanson, Mohammad Bilal
ACG Case Reports Journal.2023; 10(5): e01047. CrossRef - Knowledge and Awareness About Gastric Cancer Among the General Population in Al-Baha City, Saudi Arabia
Ali G Alghamdi, Alshareef M Alshareef, Aghnar T Alzahrani, Ziyad S Alharthi, Sarah S Alghamdi, Ahmed M Alghamdi, Faisal A Alzahrani, Reem A Alzahrani
Cureus.2023;[Epub] CrossRef - Efficacy and safety of gastroscopic hemostasis in the treatment of acute gastric hemorrhage: A meta-analysis
Hai-Yan Pan, Xiao-Wei Wang, Qiong-Xiao He, Yi-Dan Lu, Wan-Yi Zhang, Jian-Wei Jin, Bin Lin
World Journal of Gastrointestinal Oncology.2023; 15(11): 1988. CrossRef - Гостро кровоточивий рак шлунка, ускладнений перфорацією
Iryna Pliuta , Volodymyr Skuba, Mykola Stets, Sergey Trepet , Oleksandr Ivanko
The Ukrainian Scientific Medical Youth Journal.2023; 142(4): 94. CrossRef - Clinical outcomes of palliative 3-dimensional conformal external beam gastric radiotherapy: single center experience
Hüseyin Furkan ÖZTÜRK, Gonca ALTINIŞIK İNAN, İpek Pınar ARAL, Suheyla AYTAÇ ARSLAN, Sedef GÖKHAN AÇIKGÖZ, Havva BEYAZ, Yılmaz TEZCAN
Journal of Medicine and Palliative Care.2023; 4(1): 46. CrossRef - Review of surgical strategies in gastric cancer
Soumil Vyas, Avinash Supe
Oncology and Translational Medicine.2023; 9(5): 199. CrossRef - Хірургічна тактика лікування ускладнень раку шлунка в умовах війни
М. М. СТЕЦЬ, С. О. ТРЕПЕТ, О. В. ІВАНЬКО, Н. В. ВОЙТЮК, І. І. ПЛЮТА
Шпитальна хірургія. Журнал імені Л. Я. Ковальчука.2023; (4): 69. CrossRef - Gastric Cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology
Jaffer A. Ajani, Thomas A. D’Amico, David J. Bentrem, Joseph Chao, David Cooke, Carlos Corvera, Prajnan Das, Peter C. Enzinger, Thomas Enzler, Paul Fanta, Farhood Farjah, Hans Gerdes, Michael K. Gibson, Steven Hochwald, Wayne L. Hofstetter, David H. Ilson
Journal of the National Comprehensive Cancer Network.2022; 20(2): 167. CrossRef - Gastric cancer complicated by bleeding: a systematic review
I.S. Stilidi, B.V. Sigua, V.P. Zemlyanoy, A.A. Kurkov, I.I. Gubkov
Khirurgiya. Zhurnal im. N.I. Pirogova.2022; (3): 101. CrossRef - A Case of Upper Gastrointestinal Bleeding Due to Metastatic High-Grade B-Cell Lymphoma Successfully Treated With Chemotherapy
Samuel Tanner, Elie Al Kazzi, Rabail Aslam, Gerard Isenberg, Gregory Cooper
Cureus.2022;[Epub] CrossRef - Gastric cancer complicated by bleeding. (A systematic review)
I.S. Stilidi, B.V. Sigua, V.P. Zemlyanoy, A.A. Kurkov, I.I. Gubkov
Khirurgiya. Zhurnal im. N.I. Pirogova.2022; (6): 102. CrossRef - Endoscopy for the diagnosis and treatment of gastrointestinal bleeding caused by malignancy
Hamzah Abu‐Sbeih, David Szafron, Ahmed A. Elkafrawy, Victor Garcia‐Rodriguez, Weijie Ma, Ann Xu, Shruti Khurana, Laith Numan, Ellie Chen, Ryan Goldstein, Adrianne Tsen, Yuanzun Peng, Mariela Blum, Edmund S Kopetz, Naruhiko Ikoma, Malek Shatila, Wei Qiao,
Journal of Gastroenterology and Hepatology.2022; 37(10): 1983. CrossRef - Surgery for Gastric Cancer: State of the Art
Manish S. Bhandare, Vikram Chaudhari, Shailesh V. Shrikhande
Indian Journal of Surgery.2021; 83(S3): 719. CrossRef - Efficacy of a novel hemostatic adhesive powder in patients with upper gastrointestinal tumor bleeding
Jongbeom Shin, Boram Cha, Jin-Seok Park, Weonjin Ko, Kye Sook Kwon, Jin-Woo Lee, Hyung Kil Kim, Yong Woon Shin
BMC Gastroenterology.2021;[Epub] CrossRef - The Chinese Society of Clinical Oncology (CSCO): Clinical guidelines for the diagnosis and treatment of gastric cancer, 2021
Feng‐Hua Wang, Xiao‐Tian Zhang, Yuan‐Fang Li, Lei Tang, Xiu‐Juan Qu, Jie‐Er Ying, Jun Zhang, Ling‐Yu Sun, Rong‐Bo Lin, Hong Qiu, Chang Wang, Miao‐Zhen Qiu, Mu‐Yan Cai, Qi Wu, Hao Liu, Wen‐Long Guan, Ai‐Ping Zhou, Yu‐Jing Zhang, Tian‐Shu Liu, Feng Bi, Xian
Cancer Communications.2021; 41(8): 747. CrossRef - Gastrointestinal hemorrhage in the setting of gastrointestinal cancer: Anatomical prevalence, predictors, and interventions
Mohamad A Minhem, Ahmad Nakshabandi, Rabia Mirza, Mohd Amer Alsamman, Mark C Mattar
World Journal of Gastrointestinal Endoscopy.2021; 13(9): 391. CrossRef - Gastric cancer: Russian clinical guidelines
Nataliia S. Besova, Aleksei E. Kalinin, Sergei N. Nered, Aleksei A. Triakin, Sergei V. Gamaiunov, Nikolai A. Kozlov, Ivan S. Stilidi, Aleksei M. Karachun, Pavel V. Kononets, Olga A. Malikhova, Andrei B. Riabov, Vladimir M. Khomiakov, Aleksandr A. Fedenko,
Journal of Modern Oncology.2021; 23(4): 541. CrossRef - Outcomes after venous thromboembolism in patients with gastric cancer: Analysis of the RIETE Registry
Kaushal Majmudar, Iva Golemi, Alfonso J Tafur, Jorge Del Toro, Adriana Visonà, Conxita Falgá, Joan Carles Sahuquillo, Manuel Alejandro Lorente, Antonella Tufano, Ido Weinberg, Pierpaolo Di Micco, Manuel Monreal
Vascular Medicine.2020; 25(3): 210. CrossRef - Hemostatic radiotherapy for inoperable gastric cancer: a pilot study
Osamu Tanaka, Akihiko Sugiyama, Tatsushi Omatsu, Masahiro Tawada, Chiyoko Makita, Masayuki Matsuo
The British Journal of Radiology.2020;[Epub] CrossRef - Palliative care for advanced gastric cancer
Kazuto Harada, Meina Zhao, Namita Shanbhag, Hideo Baba, Jaffer a Ajani
Expert Review of Anticancer Therapy.2020; 20(7): 575. CrossRef - Acute Gastric Hemorrhage due to Gastric Cancer Eroding Into a Splenic Artery Pseudoaneurysm: Two Dangerously Rare Etiologies of Upper Gastrointestinal Bleeding
Anabel Liyen Cartelle, Pearl Princess Uy, John Erikson L Yap
Cureus.2020;[Epub] CrossRef - Radiotherapy for Gastric Bleeding from Tumor Invasion of Recurrent Colon Cancer with Liver Metastasis After Resection
Osamu Tanaka, Ryoma Yokoi, Tsuyoshi Mukai, Makoto Yamada, Tomohiro Kato, Takuya Taniguchi, Kousei Ono, Masayuki Matsuo
Journal of Gastrointestinal Cancer.2019; 50(2): 349. CrossRef - Long-Term Effectiveness, Safety and Mortality Associated with the Use of TC-325 for Malignancy-Related Upper Gastrointestinal Bleeds: A Multicentre Retrospective Study
Zhao Wu Meng, Kaleb J Marr, Rachid Mohamed, Paul D James
Journal of the Canadian Association of Gastroenterology.2019; 2(2): 91. CrossRef - Two Sessions of Radiotherapy Were Successful in Treating Gastric Cancer with Bleeding
Osamu Tanaka, Makoto Yamada, Tomohiro Kato, Takuya Taniguchi, Kousei Ono, Masayuki Matsuo
Journal of Gastrointestinal Cancer.2019; 50(4): 955. CrossRef - Management of Bleeding from Unresectable Gastric Cancer
Hideaki Kawabata, Misuzu Hitomi, Shigehiro Motoi
Biomedicines.2019; 7(3): 54. CrossRef - Hemostatic spray powder TC-325 for GI bleeding in a nationwide study: survival and predictors of failure via competing risks analysis
Enrique Rodríguez de Santiago, Diego Burgos-Santamaría, Leticia Pérez-Carazo, Enric Brullet, Lucía Ciriano, Faust Riu Pons, Miguel Ángel de Jorge Turrión, Susana Prados, Daniel Pérez-Corte, Irene Becerro-Gonzalez, Emma Martinez-Moneo, Angel Barturen, Igna
Gastrointestinal Endoscopy.2019; 90(4): 581. CrossRef - Efficacy of interventional therapy and effect on inflammatory factors in patients with gastric cancer after chemotherapy
Puzhao Wu, Jing Wang
Oncology Letters.2019;[Epub] CrossRef - Experience of Low-Dose, Short-Course Palliative Radiotherapy for Bleeding from Unresectable Gastric Cancer
Hideaki Kawabata, Koji Uno, Kenjiro Yasuda, Masato Yamashita
Journal of Palliative Medicine.2017; 20(2): 177. CrossRef - Gastrointestinal Bleeding Due to Gastrointestinal Tract Malignancy: Natural History, Management, and Outcomes
Richard A. Schatz, Don C. Rockey
Digestive Diseases and Sciences.2017; 62(2): 491. CrossRef - Effect of a Proton Pump Inhibitor on Tumor Bleeding Prevention in Unresectable Gastric Cancer Patients: a Double-Blind, Randomized, Placebo-Controlled Trial
Young-Il Kim, Mi-Jung Kim, Sook Ryun Park, Hark Kyun Kim, Soo-Jeong Cho, Jong Yeul Lee, Chan Gyoo Kim, Gwang Ha Kim, Moo In Park, Byung-Ho Nam, Young Iee Park, Il Ju Choi
Journal of Gastric Cancer.2017; 17(2): 120. CrossRef - Can Endoscopic Bleeding Control Improve the Prognosis of Advanced Gastric Cancer Patients?
Hyungchul Park, Ji Yong Ahn, Hwoon-Yong Jung, Joo Hyun Chun, Kwangwoo Nam, Jeong Hoon Lee, Kee Wook Jung, Do Hoon Kim, Kee Don Choi, Ho June Song, Gin Hyug Lee, Jin-Ho Kim
Journal of Clinical Gastroenterology.2017; 51(7): 599. CrossRef - Value in palliative cancer surgery: A critical assessment
Ian W. Folkert, Robert E. Roses
Journal of Surgical Oncology.2016; 114(3): 311. CrossRef - Neoadjuvante Therapie bei Tumoren des oberen Gastrointestinaltrakts
I. Gockel, A. Hoffmeister, F. Lordick
Der Chirurg.2015; 86(11): 1014. CrossRef - Tumoren des oberen Gastrointestinaltraktes
I. Gockel, A. Hoffmeister, F. Lordick
best practice onkologie.2015; 10(6): 19. CrossRef
- Endoscopic Management of Tumor Bleeding
- 12,804 View
- 176 Download
- 36 Web of Science
- 45 Crossref

- Clinical Findings of Upper Gastrointestinal Bleeding and Risk Factors for Early Rebleeding in Patients with Bleeding Peptic Ulcers
- Hyeon Yong Park, M.D., Jin Wook Hur, M.D., Paul Choi, M.D., Nam Young Park, M.D., Jee Yeon Kim, M.D., Dong Wan Kim, M.D., Jee Young Lee, M.D., Ki Hwan Kim, M.D., Moo In Park, M.D., Seun Ja Park, M.D. and Ja Young Koo, M.D.
- Korean J Gastrointest Endosc 2003;27(2):57-63. Published online August 30, 2003
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: Upper gastrointestinal (UGI) bleeding may have serious complications. Endoscopic therapy is effective in the hemostasis of active bleeding. We analysed the causes of UGI bleeding and evaluated risk factors and rate of rebleeding in patients with bleeding peptic ulcer. Methods: Records from 326 patients admitted with upper gastrointestinal bleeding between January 1998 and December 2002 were reviewed. We retrospectively analyzed clinical findings and rebleeding risk factors of peptic ulcers. Results: Common causes of UGI bleeding were esophageal varix (38.0%), peptic ulcer (36.9%), Mallory-Weiss tear (13.8%), stomach cancer (6.4%). Early rebleeding of bleeding peptic ulcer after hemostasis occurred in 23 cases (19.2%). On the basis of univariate analysis, significant predictive factors for early rebleeding were old age (>65) (p=0.034), size of ulcer (>2 cm) (p=0.002), number of ulcer (>1) (p=0.059). In multivariate analysis, old age (odds ratio, OR=2.3), size of ulcer (OR=3.3), number of ulcer (OR=2.6) were independent risk factors of rebleeding. Conclusions: Common causes of UGI bleeding are esophageal varix, peptic ulcer, Mallory-Weiss tear. Predictive risk factors for early rebleeding in bleeding peptic ulcer may be old age, size of ulcer and number of ulcer. (Korean J Gastrointest Endosc 2003;27:5763)
- 1,801 View
- 4 Download

- 대량의 상부 위장관 출혈을 유발한 십이지장게실 1 예 ( A Case of Massive Upper Gastrointestinal Bleeding from a Duodenal Diverticulum )
- Korean J Gastrointest Endosc 2000;21(3):746-749. Published online November 30, 1999
-
 Abstract
Abstract
 PDF
PDF - Duodenal diverticulum is well-known pathologic entity. The incidence of duodenal diverticulum varies from 5% to 23% in the general population. Most of diverticula are asymptomatic and have been incidentally observed in upper gastrointestinal series or upper gastrointestinal endoscopy. It usually occurs in the second portion and the medial side of duodenum. The complications of duodenal diverticulum are rare but often result in significant morbidity. They include obstruction, cholelithiasis, ascending cholangitis, ulcers, hemorrhage and perforation. Major gastrointestinal hemorrhage resulting from an inflamed or ulcerated duodenal diverticulum is an uncommon event and it can be treated endoscopically. We report a case of massive upper gastrointestinal bleeding from a duodenal diverticulum which was treated endoscopically.
- 1,531 View
- 2 Download


 KSGE
KSGE


 First
First Prev
Prev



