Search
- Page Path
- HOME > Search
-
Dedicated Cold Snare vs. Traditional Snare for Polypectomy of Diminutive and Small Lesions in a Porcine Model: A Research Group for Endoscopic Instruments and Stents (REIS) Study

- Han Hee Lee, Bo-In Lee, Jung-Wook Kim, Hyun Lim, Si Hyung Lee, Jun-Hyung Cho, Yunho Jung, Kyoung Oh Kim, Chan Gyoo Kim, Kee Myung Lee, Jong-Jae Park, Myung-Gyu Choi, Hoon Jai Chun, Ho Gak Kim
- Clin Endosc 2021;54(3):390-396. Published online September 10, 2020
- DOI: https://doi.org/10.5946/ce.2020.096
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: The aim of this in vivo animal study was to evaluate the effectiveness and safety of dedicated cold snare (DCS) compared with those of traditional snare (TS) for cold snare polypectomy (CSP).
Methods
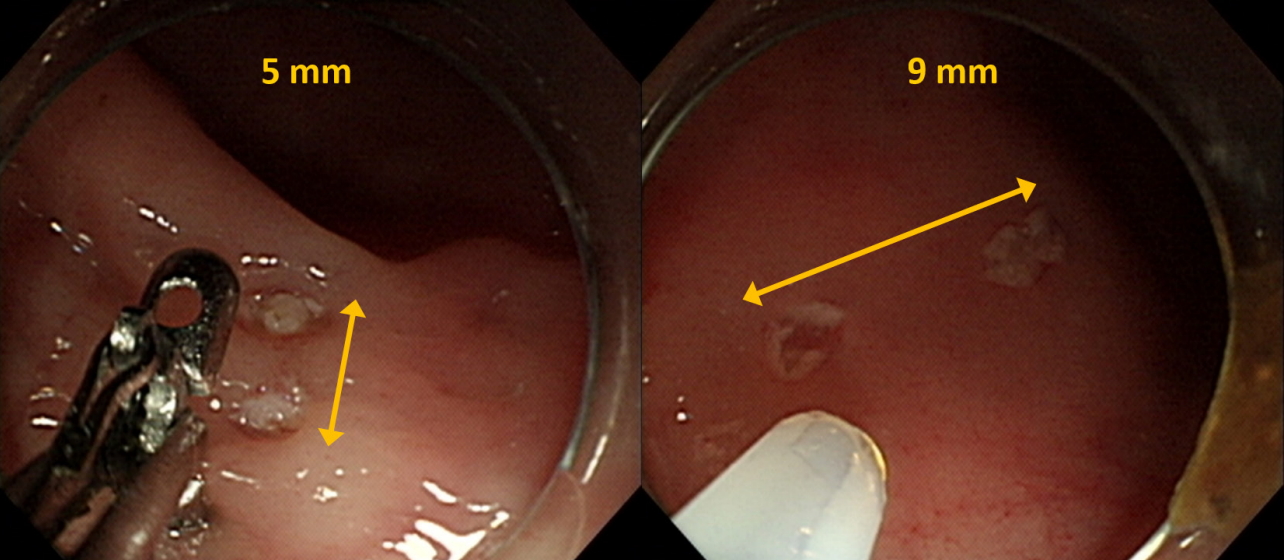
A total of 36 diminutive (5 mm) and 36 small (9 mm) pseudolesions were made by electrocoagulation in the colons of mini-pigs.
Results
For the diminutive lesions, there were no significant differences in technical success rate, procedure time, or complete resection rate between the DCS and TS groups; the rate of uneven resection margin in the DCS group was significantly lower than that of the TS group. For small lesions, technical success rate and complete resection rate were significantly higher in the DCS group than in the TS group (100% [18/18] vs. 55.6% [10/18], p=0.003; 94.4% [17/18] vs. 40% [4/10], p=0.006). In addition, the procedure duration was significantly shorter, and the rate of uneven resection margin was significantly lower in the DCS group (28.5 sec vs. 66.0 sec, p=0.006; 11.1% [2/18] vs. 100% [10/10], p<0.001). Two cases of perforation occurred in the DCS group. Multivariate analysis revealed that DCS use was independently associated with complete resection.
Conclusions
DCS is superior to TS in terms of technical success, complete resection, and reducing the duration of the procedure for CSP of small polyps. -
Citations
Citations to this article as recorded by- Comparison of complete resection rates in cold snare polypectomy using two different wire diameter snares: A randomized controlled study
Toshiki Horii, Sho Suzuki, Akihiro Sugita, Misa Yamauchi, Hisatomo Ikehara, Chika Kusano, Takuji Gotoda
Journal of Gastroenterology and Hepatology.2023; 38(5): 752. CrossRef - Comparison of the clinical efficacy of cold snare polypectomy using a thin-wire snare and thick-wire snare for small colorectal polyps
Hong Jin Yoon, Yunho Jung, Young Sin Cho, Il-Kwun Chung
International Journal of Gastrointestinal Intervention.2023; 12(4): 183. CrossRef - Big Issues on Small Polyps: An Ideal Device, But Is It for an Ideal Indication?
Yoji Takeuchi
Clinical Endoscopy.2021; 54(3): 297. CrossRef - Cold versus hot polypectomy/endoscopic mucosal resection–A review of current evidence
Raquel Ortigão, Jochen Weigt, Ahmed Afifi, Diogo Libânio
United European Gastroenterology Journal.2021; 9(8): 938. CrossRef
- Comparison of complete resection rates in cold snare polypectomy using two different wire diameter snares: A randomized controlled study
- 8,391 View
- 221 Download
- 4 Web of Science
- 4 Crossref

- Efficacy of the Over-the-Scope Clip System for Treatment of Gastrointestinal Fistulas, Leaks, and Perforations: A Korean Multi-Center Study
- Hang Lak Lee, Joo Young Cho, Jun-Hyung Cho, Jong Jae Park, Chan Gyoo Kim, Seong Hwan Kim, Joung-Ho Han
- Clin Endosc 2018;51(1):61-65. Published online August 29, 2017
- DOI: https://doi.org/10.5946/ce.2017.027
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Currently, a new over-the-scope clip (OTSC) system has been introduced. This system has been used for gastrointestinal perforations and fistulas in other countries. The aim of our study is to examine the therapeutic success rate of endoscopic treatment using the OTSC system in Korea.
Methods
This was a multicenter prospective study. A total of seven endoscopists at seven centers performed this procedure.
Results
A total of 19 patients were included, with gastrointestinal leakages from anastomosis sites, fistulas, or esophageal perforations due to Boerhaave’s syndrome. Among these, there were three gastrojejunostomy sites, three esophagojejunostomy sites, four esophagogastrostomy sites, one esophagocolonostomy site, one jejuno-jejunal site, two endoscopic full thickness resection site closures, one Boerhaave’s syndrome, two esophago-bronchial fistulas, one gastrocolonic fistula, and one colonopseudocyst fistula. The size of the leakage ranged from 5 to 30 mm. The median procedure time was 16 min. All cases were technically successful. Complete closure of the leak was achieved in 14 of 19 patients using OTSC alone.
Conclusions
The OTSC system is a safe and effective method for the management of gastrointestinal leakage, especially in cases of anastomotic leakage after surgery. -
Citations
Citations to this article as recorded by- Bariatric surgery and reproduction-implications for gynecology and obstetrics
Isaac A. Babarinsa, Mohammed Bashir, Husham AbdelRahman Ahmed, Badreldeen Ahmed, Justin C. Konje
Best Practice & Research Clinical Obstetrics & Gynaecology.2023; 90: 102382. CrossRef - Current status in endoscopic management of upper gastrointestinal perforations, leaks and fistulas
Shannon Melissa Chan, Kitty Kit Ying Auyeung, Siu Fung Lam, Philip Wai Yan Chiu, Anthony Yuen Bun Teoh
Digestive Endoscopy.2022; 34(1): 43. CrossRef - Endoscopic vacuum therapy (EVT) for acute esophageal perforation: Could it replace surgery?
Petros Stathopoulos, Malte Zumblick, Sabine Wächter, Leif Schiffmann, Thomas M. Gress, Detlef Bartsch, Guido Seitz, Ulrike W. Denzer
Endoscopy International Open.2022; 10(05): E686. CrossRef - Acquired Benign Tracheoesophageal Fistula
Hasnain S. Bawaadam, Matthew Russell, Yaron B. Gesthalter
Journal of Bronchology & Interventional Pulmonology.2022; 29(3): e38. CrossRef - Exclusión pilórica con dispositivo Ovesco (over-thescope) en caso de fístula yeyunal en obstrucción duodenal de etiología maligna
Raul Eduardo Pinilla Morales, Helena Facundo Navia, Elio Fabio Sánchez Cortés, Ivette C. Jiménez Lafourie, Álvaro Eduardo Sánchez Hernández, Luis Carlos Llorente Portillo
Revista colombiana de Gastroenterología.2022; 37(3): 320. CrossRef - Endoscopic management of leaks and fistulas after bariatric surgery: a systematic review and meta-analysis
Pawel Rogalski, Agnieszka Swidnicka-Siergiejko, Justyna Wasielica-Berger, Damian Zienkiewicz, Barbara Wieckowska, Eugeniusz Wroblewski, Andrzej Baniukiewicz, Magdalena Rogalska-Plonska, Grzegorz Siergiejko, Andrzej Dabrowski, Jaroslaw Daniluk
Surgical Endoscopy.2021; 35(3): 1067. CrossRef - Endoscopic management of gastro‐bronchial fistula following two‐stage esophagectomy using over‐the‐scope‐clip (OTSC): Case series
Chih Y. Tan, Htet A. Kyaw, Neda Farhangmehr, Cheuk‐Bong Tang, Naga V. Jayanthi
Advances in Digestive Medicine.2021; 8(2): 84. CrossRef - Over-the-Scope Clip Closure of Persistent Gastrocutaneous Fistula After Percutaneous Endoscopic Gastrostomy Tube Removal: A Report of Two Cases
Shigenori Masaki, Keishi Yamada
Cureus.2021;[Epub] CrossRef - Over‐the‐scope clip: a novel approach to the management of a colorectal anastomotic leak
Stephanie G. Jordan, Gregory J. Nolan
ANZ Journal of Surgery.2021; 91(11): 2534. CrossRef - Conservative treatment of patients with small bowel fistula
A.V. Vodyasov, D.M. Kopaliani, P.A. Yartsev, O.Kh. Kaloeva
Khirurgiya. Zhurnal im. N.I. Pirogova.2021; (4): 78. CrossRef - An Approach to Accelerate Healing and Shorten the Hospital Stay of Patients With Anastomotic Leakage After Esophagectomy: An Explorative Study of Systematic Endoscopic Intervention
LeQi Zhong, JiuDi Zhong, ZiHui Tan, YiTong Wei, XiaoDong Su, ZheSheng Wen, TieHua Rong, Yi Hu, KongJia Luo
Frontiers in Oncology.2021;[Epub] CrossRef - AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review
Jeffrey H. Lee, Prashant Kedia, Stavros N. Stavropoulos, David Carr-Locke
Clinical Gastroenterology and Hepatology.2021; 19(11): 2252. CrossRef - Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clinical Endoscopy.2021; 54(5): 633. CrossRef - Diagnostic challenge and surgical management of Boerhaave’s syndrome: a case series
Jiayue Wang, Degang Wang, Jianjiao Chen
Journal of Medical Case Reports.2021;[Epub] CrossRef - Over-the-scope clip management of non-acute, full-thickness gastrointestinal defects
David J. Morrell, Joshua S. Winder, Ansh Johri, Salvatore Docimo, Ryan M. Juza, Samantha R. Witte, Vamsi V. Alli, Eric M. Pauli
Surgical Endoscopy.2020; 34(6): 2690. CrossRef - Use of the Over the Scope Clip to Close Perforations and Fistulas
Panida Piyachaturawat, Parit Mekaroonkamol, Rungsun Rerknimitr
Gastrointestinal Endoscopy Clinics of North America.2020; 30(1): 25. CrossRef - Therapie der Ösophagusleckagen
Jutta Weber-Eibel
Journal für Gastroenterologische und Hepatologische Erkrankungen.2020; 18(1): 8. CrossRef - Successful Closure of a Benign Refractory Tracheoesophageal Fistula Using an Over-the-Scope Clip after Failed Esophageal Stent Placement and Surgical Management
Nonthalee Pausawasdi, Chotirot Angkurawaranon, Tanyaporn Chantarojanasiri, Arunchai Chang, Wanchai Wongkornrat, Somchai Leelakusolvong, Asada Methasate
Clinical Endoscopy.2020; 53(3): 361. CrossRef - Clinical efficacy of the over-the-scope clip device: A systematic review
Nicholas Bartell, Krystle Bittner, Vivek Kaul, Truptesh H Kothari, Shivangi Kothari
World Journal of Gastroenterology.2020; 26(24): 3495. CrossRef - Endoscopic devices and techniques for the management of bariatric surgical adverse events (with videos)
Allison R. Schulman, Rabindra R. Watson, Barham K. Abu Dayyeh, Manoop S. Bhutani, Vinay Chandrasekhara, Pichamol Jirapinyo, Kumar Krishnan, Nikhil A. Kumta, Joshua Melson, Rahul Pannala, Mansour A. Parsi, Guru Trikudanathan, Arvind J. Trindade, John T. Ma
Gastrointestinal Endoscopy.2020; 92(3): 492. CrossRef - Gastrointestinal tract injuries after thermal ablative therapies for hepatocellular carcinoma: A case report and review of the literature
Teresa Marzia Rogger, Andrea Michielan, Sandro Sferrazza, Cecilia Pravadelli, Luisa Moser, Flora Agugiaro, Giovanni Vettori, Sonia Seligmann, Elettra Merola, Marcello Maida, Francesco Antonio Ciarleglio, Alberto Brolese, Giovanni de Pretis
World Journal of Gastroenterology.2020; 26(35): 5375. CrossRef - Over‐the‐scope clip system: A review of 1517 cases over 9 years
Hideki Kobara, Hirohito Mori, Noriko Nishiyama, Shintaro Fujihara, Keiichi Okano, Yasuyuki Suzuki, Tsutomu Masaki
Journal of Gastroenterology and Hepatology.2019; 34(1): 22. CrossRef - Recent advancements in the minimally invasive management of esophageal perforation, leaks, and fistulae
Shirin Siddiqi, Dean P. Schraufnagel, Hafiz Umair Siddiqui, Michael J. Javorski, Adam Mace, Abdulrhman S. Elnaggar, Haytham Elgharably, Patrick R. Vargo, Robert Steffen, Saad M. Hasan, Siva Raja
Expert Review of Medical Devices.2019; 16(3): 197. CrossRef - Diagnosis and endoscopic treatment of esophageal leakage: a systematic review
Bram D. Vermeulen, Peter D. Siersema
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 58. CrossRef - Management of esophagojejunal anastomosis leakage after total gastrectomy
Pablo Priego, Pietro Giordano, Marta Cuadrado, Araceli Ballestero, Julio Galindo, Eduardo Lobo
European Surgery.2018; 50(6): 262. CrossRef - Endoluminal Therapies for Esophageal Perforations and Leaks
Jeffrey R. Watkins, Alexander S. Farivar
Thoracic Surgery Clinics.2018; 28(4): 541. CrossRef - Esophageal leaks: I thought that glue was not effective
Ignacio Fernández-Urién, Juan Vila
Endoscopy International Open.2018; 06(09): E1100. CrossRef
- Bariatric surgery and reproduction-implications for gynecology and obstetrics
- 7,580 View
- 324 Download
- 26 Web of Science
- 27 Crossref

- Advanced Imaging Technology Other than Narrow Band Imaging
- Jun-Hyung Cho
- Clin Endosc 2015;48(6):503-510. Published online November 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.6.503
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - To improve the detection rate of gastrointestinal tumors, image-enhanced endoscopy has been widely used during screening and surveillance endoscopy in Korea. In addition to narrow band imaging (NBI) with/without magnification, various types of electronic chromoendoscopies have been used, including autofluorescence imaging, I-scan, and flexible spectral imaging color enhancement. These technologies enable the accurate characterization of tumors because they enable visualization of microvascular and microsurface patterns. The present review focuses on understanding the principle and clinical applications of advanced imaging technologies other than NBI.
-
Citations
Citations to this article as recorded by- Comparison of narrow-band imaging with autofluorescence imaging for endoscopic detection of squamous cell carcinoma of the tonsil
J. Syba, K. Trnkova, L. Dostalova, M. Votava, E. Lukesova, S. Novak, M. Kana, M. Tesarova, M. Zabrodsky, J. Plzak, P. Lukes
European Archives of Oto-Rhino-Laryngology.2023; 280(11): 5073. CrossRef - A prospective study for evaluating the effect of gastric targeted biopsy sampling with I‐scan optical enhancement on the diagnostic yield of CLOtest for Helicobacter pylori infection
Hosam Mohamed Dawod
Health Science Reports.2022;[Epub] CrossRef - Diagnostic Value of Endoscopic Narrow-Band Imaging Technique in Early Gastric Cancer and Precancerous Lesions
Xianxin Huang, Rong Chen, Liang Zhao, Danilo Pelusi
Scanning.2022; 2022: 1. CrossRef - Endoscopy Lifetime Systems Architecture: Scoping Out the Past to Diagnose the Future Technology
Craig M. Browning, Robert Cloutier, Thomas C. Rich, Silas J. Leavesley
Systems.2022; 10(5): 189. CrossRef - Biomedical Photonics for Intraoperative Diagnostics: Review of Capabilities and Clinical Applications
E. A. Shirshin, B. P. Yakimov, G. S. Budylin, N. V. Zlobina, D. A. Davydov, A. G. Armaganov, V. V. Fadeev, N. N Sysoev, A. A. Kamalov
Moscow University Physics Bulletin.2022; 77(6): 777. CrossRef - Optimized diagnosis of Helicobacter pylori and tailored eradication therapy for preventing gastric cancer: a proposal for SHAKE strategy
Jun-Hyung Cho, So-Young Jin
Expert Review of Gastroenterology & Hepatology.2020; 14(7): 553. CrossRef - Clinical applicability of gastroscopy with narrow-band imaging for the diagnosis of Helicobacter pylori gastritis, precancerous gastric lesion, and neoplasia
Jun-Hyung Cho, Seong Ran Jeon, So-Young Jin
World Journal of Clinical Cases.2020; 8(14): 2902. CrossRef - Colonoscopy technologies for diagnostics and drug delivery
Rajib Ahmed, Krieshshanthan Santhirakumar, Haider Butt, Ali K. Yetisen
MEDICAL DEVICES & SENSORS.2019;[Epub] CrossRef - A guide to multimodal endoscopy imaging for gastrointestinal malignancy — an early indicator
Arthur Hoffman, Henrik Manner, Johannes W. Rey, Ralf Kiesslich
Nature Reviews Gastroenterology & Hepatology.2017; 14(7): 421. CrossRef - Linked color imaging application for improving the endoscopic diagnosis accuracy: a pilot study
Xiaotian Sun, Tenghui Dong, Yiliang Bi, Min Min, Wei Shen, Yang Xu, Yan Liu
Scientific Reports.2016;[Epub] CrossRef - Narrow band imaging versus autofluorescence imaging for head and neck squamous cell carcinoma detection: a prospective study
X-G Ni, Q-Q Zhang, G-Q Wang
The Journal of Laryngology & Otology.2016; 130(11): 1001. CrossRef
- Comparison of narrow-band imaging with autofluorescence imaging for endoscopic detection of squamous cell carcinoma of the tonsil
- 12,988 View
- 187 Download
- 12 Web of Science
- 11 Crossref

- Endoscopic Treatment of Various Gastrointestinal Tract Defects with an Over-the-Scope Clip: Case Series from a Tertiary Referral Hospital
- Woong Cheul Lee, Weon Jin Ko, Jun-Hyung Cho, Tae Hee Lee, Seong Ran Jeon, Hyun Gun Kim, Joo Young Cho
- Clin Endosc 2014;47(2):178-182. Published online March 31, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.2.178
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Recently, increasingly invasive therapeutic endoscopic procedures and more complex gastrointestinal surgeries such as endoscopic mucosal resection, endoscopic submucosal dissection, and novel laparoscopic approaches have resulted in endoscopists being confronted more frequently with perforations, fistulas, and anastomotic leakages, for which nonsurgical closure is desired. In this article, we present our experiences with the use of over-the-scope clip (OTSC) for natural orifice transluminal endoscopic surgery (NOTES) closure, prevention of perforation, anastomotic leakages, and fistula closures. The OTSC is a valuable device for closing intestinal perforations and fistulas, for NOTES closure, and for the prevention of perforation after the excision of a tumor from the proper muscle layer. Furthermore, it seems to be quite safe to perform, even by endoscopists with little experience of the technique.
-
Citations
Citations to this article as recorded by- Experimental Evaluation of the Optimal Suture Pattern With a Flexible Endoscopic Suturing System
Peter Halvax, Michele Diana, Yoshihiro Nagao, Jacques Marescaux, Lee Swanström
Surgical Innovation.2017; 24(3): 201. CrossRef - Management of non-acute gastrointestinal defects using the over-the-scope clips (OTSCs): a retrospective single-institution experience
Joshua S. Winder, Afif N. Kulaylat, Jane R. Schubart, Hassan M. Hal, Eric M. Pauli
Surgical Endoscopy.2016; 30(6): 2251. CrossRef - Early endoscopic closure of colocutaneous fistula adjacent to unmatured low colorectal anastomosis with the Over-The-Scope Clip (OTSC)
Constantinos Avgoustou, K. Paraskeva
Hellenic Journal of Surgery.2016; 88(3): 193. CrossRef - Endoscopic Closure for Full-Thickness Gastrointestinal Defects: Available Applications and Emerging Innovations
Nobuyoshi Takeshita, Khek Yu Ho
Clinical Endoscopy.2016; 49(5): 438. CrossRef
- Experimental Evaluation of the Optimal Suture Pattern With a Flexible Endoscopic Suturing System
- 6,115 View
- 58 Download
- 3 Web of Science
- 4 Crossref

- White Esophageal Mucosa and Black Gastric Mucosa: Upper Gastrointestinal Injury Due to Hydrochloric Acid Ingestion
- Woong Cheul Lee, Tae Hee Lee, Jun-Hyung Cho
- Clin Endosc 2014;47(1):119-120. Published online January 24, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.1.119
-
 PDF
PDF PubReader
PubReader ePub
ePub -
Citations
Citations to this article as recorded by- Severe Intentional Corrosive (Nitric Acid) Acute Poisoning: A Case Report and Literature Review
Alexandra Stoica, Cătălina Lionte, Mădălina Palaghia, Irina Gîrleanu, Victoriţa Şorodoc, Alexandr Ceasovschih, Oana Sîrbu, Raluca Haliga, Cristina Bologa, Ovidiu Petriş, Vlad Nuţu, Ana Trofin, Gheorghe Bălan, Andreea Catana, Adorata Coman, Mihai Constanti
Journal of Personalized Medicine.2023; 13(6): 987. CrossRef
- Severe Intentional Corrosive (Nitric Acid) Acute Poisoning: A Case Report and Literature Review
- 5,140 View
- 54 Download
- 2 Web of Science
- 1 Crossref

- Evidence-Based Recommendations on Upper Gastrointestinal Tract Stenting: A Report from the Stent Study Group of the Korean Society of Gastrointestinal Endoscopy
- Sam Ryong Jee, Joo Young Cho, Kyung Ho Kim, Sang Gyun Kim, Jun-Hyung Cho, The Stent Study Group of the Korean Society of Gastrointestinal Endoscopy
- Clin Endosc 2013;46(4):342-354. Published online July 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.4.342
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Endoscopic stents have evolved dramatically over the past 20 years. With the introduction of uncovered self-expanding metal stents in the early 1990s, they are primarily used to palliate symptoms of malignant obstruction in patients with inoperable gastrointestinal (GI) cancer. At present, stents have emerged as an effective, safe, and less invasive alternative for the treatment of malignant GI obstruction. Clinical decisions about stent placement should be made based on the exact understanding of the patient's condition. These recommendations based on a critical review of the available data and expert consensus are made for the purpose of providing endoscopists with information about stent placement. These can be helpful for management of patients with inoperable cancer or various nonmalignant conditions in the upper GI tract.
-
Citations
Citations to this article as recorded by- Endoscopic Procedures for Upper Gastrointestinal Tract Lesions and a Brief Review of Literature
Selim Doğan, Ekrem Çakar, Bünyamin Gürbulak, Şükrü Çolak, Hasan Bektaş, Cihad Tatar
Istanbul Medical Journal.2022; 23(2): 154. CrossRef - Endoscopic Treatment of a Twisted Small Bowel Obstruction after Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction
Ki Bum Park, Seong Woo Jeon
The Korean Journal of Gastroenterology.2020; 75(5): 296. CrossRef - Temporary self-expandable metallic stent placement in post-gastrectomy complications
Hyun Jin Oh, Chul-Hyun Lim, Seung Bae Yoon, Han Hee Lee, Jin Su Kim, Yu Kyung Cho, Jae Myung Park, Myung-Gyu Choi
Gastric Cancer.2019; 22(1): 231. CrossRef - Peptic Ulcer-related Stenosis
Cheol Woong Choi
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2019; 19(1): 10. CrossRef - Clinical Feasibility and Safety of Endoscopic Self-Expandable Metal Stent Placement for Upper Gastrointestinal Pathologies
Bünyamin Gürbulak, Esin Kabul Gürbulak, Hasan Bektaş, İsmail Ethem Akgün, Hızır Yakup Akyildiz, Özgür Segmen, Fevzi Celayir, Muharrem Battal, Kenan Büyükaşık
International Surgery.2018; 103(11-12): 605. CrossRef - Endoscopic management of complications of self-expandable metal stents for treatment of malignant esophageal stenosis and tracheoesophageal fistulas
Renáta Bor, Anna Fábián, Anita Bálint, Klaudia Farkas, Mónika Szűcs, Ágnes Milassin, László Czakó, Mariann Rutka, Tamás Molnár, Zoltán Szepes
Therapeutic Advances in Gastroenterology.2017; 10(8): 599. CrossRef - Gastroduodenal Outlet Obstruction and Palliative Self-Expandable Metal Stenting: A Dual-Centre Experience
Nik S. Ding, Sina Alexander, Michael P. Swan, Christopher Hair, Patrick Wilson, Emma Clarebrough, David Devonshire
Journal of Oncology.2013; 2013: 1. CrossRef
- Endoscopic Procedures for Upper Gastrointestinal Tract Lesions and a Brief Review of Literature
- 7,902 View
- 52 Download
- 7 Crossref

- Peroral Endoscopic Myotomy for Treatment of Achalasia: Initial Results of a Korean Study
- Byung Hoo Lee, Kwang Yeun Shim, Su Jin Hong, Gene Hyun Bok, Jun-Hyung Cho, Tae Hee Lee, Joo Young Cho
- Clin Endosc 2013;46(2):161-167. Published online March 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.2.161
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Achalasia is a rare esophageal motility disorder. Recently, a novel endoscopic technique, peroral endoscopic myotomy (POEM), was introduced as an alternative treatment for achalasia. We report the results and short term outcomes of POEM for patients with achalasia.
Methods POEM was performed in 13 patients with achalasia. The procedure consisted of creating a submucosal tunnel followed by endoscopic myotomy of circular muscle bundles. The mucosal entry was closed by conventional hemostatic clips. A validated clinical symptom score (Eckardt score) and high resolution manometry were used to evaluate the outcomes.
Results Both the clinical score of achalasia, as well as the resting lower esophageal sphincter (LES) pressure, were significantly reduced after POEM. Mean posttreatment Eckardt score was 0.4±0.7, compared to 6.4±1.9 prior to the treatment (
p =0.001). The mean pretreatment and posttreatment LES pressure was 30.3 and 15.3 mm Hg, respectively (p =0.007). Following POEM, symptomatic relief from dysphagia without reflux symptoms was observed in all patients (13/13). No serious complications related to POEM were encountered.Conclusions Based upon our initial experience, the authors believe that POEM is a feasible, safe, and effective treatment and may possibly substitute established treatments of refractory achalasia.
-
Citations
Citations to this article as recorded by- Achalasia: Current therapeutic options
Sebastien Rolland, William Paterson, Robert Bechara
Neurogastroenterology & Motility.2023;[Epub] CrossRef - Long versus short peroral endoscopic myotomy for the treatment of achalasia: results of a non-inferiority randomised controlled trial
Pietro Familiari, Federica Borrelli de Andreis, Rosario Landi, Francesca Mangiola, Ivo Boskoski, Andrea Tringali, Vincenzo Perri, Guido Costamagna
Gut.2023; 72(8): 1442. CrossRef - Efficacy and Safety of Peroral Endoscopic Myotomy (POEM) in Achalasia: An Updated Meta-analysis
Afshin Khaiser, Muhammad Baig, David Forcione, Matthew Bechtold, Srinivas R. Puli
Middle East Journal of Digestive Diseases.2023; 15(4): 235. CrossRef - Type II achalasia is associated with a comparably favorable outcome following per oral endoscopic myotomy
Yutaka Tomizawa, Nadim Mahmud, Kevin Dasher, Joseph R Triggs, Monica Saumoy, Gary W Falk, Gregory G Ginsberg
Diseases of the Esophagus.2021;[Epub] CrossRef - Miotomía endoscópica peroral para el tratamiento de acalasia y otros trastornos motores del esófago. Resultados a corto y mediano plazo en un centro de referencia en México
O.V. Hernández-Mondragón, O.M. Solórzano-Pineda, M.A. González-Martínez, J.M. Blancas-Valencia, C. Caballero-Luengas
Revista de Gastroenterología de México.2019; 84(1): 1. CrossRef - Peroral endoscopic myotomy for the treatment of achalasia and other esophageal motor disorders: Short-term and medium-term results at a Mexican tertiary care center
O.V. Hernández-Mondragón, O.M. Solórzano-Pineda, M.A. González-Martínez, J.M. Blancas-Valencia, C. Caballero-Luengas
Revista de Gastroenterología de México (English Edition).2019; 84(1): 1. CrossRef - Bridging the Gap between Advancements in the Evolution of Diagnosis and Treatment towards Better Outcomes in Achalasia
Seng-Kee Chuah, Chee-Sang Lim, Chih-Ming Liang, Hung-I Lu, Keng-Liang Wu, Chi-Sin Changchien, Wei-Chen Tai
BioMed Research International.2019; 2019: 1. CrossRef - Preliminary study of 1940 nm thulium laser usage in peroral endoscopic myotomy for achalasia
J Liu, Y Jiao, Y Niu, L Yu, M Ji, S Zhang
Diseases of the Esophagus.2018;[Epub] CrossRef - POEM in the Treatment of Esophageal Disorders
Nasim Parsa, Mouen A. Khashab
Current Treatment Options in Gastroenterology.2018; 16(1): 27. CrossRef - Current Status of Peroral Endoscopic Myotomy
Young Kwan Cho, Seong Hwan Kim
Clinical Endoscopy.2018; 51(1): 13. CrossRef - Safety and efficacy of POEM for treatment of achalasia: a systematic review of the literature
Oscar M. Crespin, Louis W. C. Liu, Ambica Parmar, Timothy D. Jackson, Jemila Hamid, Eran Shlomovitz, Allan Okrainec
Surgical Endoscopy.2017; 31(5): 2187. CrossRef - Early adverse events of per-oral endoscopic myotomy
Yuki B. Werner, Daniel von Renteln, Tania Noder, Guido Schachschal, Ulrike W. Denzer, Stefan Groth, Jan F. Nast, Jan F. Kersten, Martin Petzoldt, Gerhard Adam, Oliver Mann, Alessandro Repici, Cesare Hassan, Thomas Rösch
Gastrointestinal Endoscopy.2017; 85(4): 708. CrossRef - A multicenter international registry of redo per-oral endoscopic myotomy (POEM) after failed POEM
Amy Tyberg, Stefan Seewald, Reem Z. Sharaiha, Guadalupe Martinez, Amit P. Desai, Nikhil A. Kumta, Arnon Lambroza, Amrita Sethi, Kevin M. Reavis, Ketisha DeRoche, Monica Gaidhane, Michael Talbot, Payal Saxena, Felipe Zamarripa, Maximilien Barret, Nicholas
Gastrointestinal Endoscopy.2017; 85(6): 1208. CrossRef - Long-term outcomes of peroral endoscopic myotomy for patients with achalasia: a retrospective single-center study
H. Guo, H. Yang, X. Zhang, L. Wang, Y. Lv, X. Zou, T. Ling
Diseases of the Esophagus.2017; 30(5): 1. CrossRef - Per-Oral Esophageal Myotomy
Eric S. Hungness, Juaquito M. Jorge
Advances in Surgery.2017; 51(1): 193. CrossRef - Comparison of the Outcomes of Peroral Endoscopic Myotomy for Achalasia According to Manometric Subtype
Won Hee Kim, Joo Young Cho, Weon Jin Ko, Sung Pyo Hong, Ki Baik Hahm, Jun-Hyung Cho, Tae Hee Lee, Su Jin Hong
Gut and Liver.2017; 11(5): 642. CrossRef - Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis
K. Patel, N. Abbassi-Ghadi, S. Markar, S. Kumar, P. Jethwa, G. Zaninotto
Diseases of the Esophagus.2016; 29(7): 807. CrossRef - Gastroesophageal reflux disease after peroral endoscopic myotomy: Analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis
Pietro Familiari, Santi Greco, Giovanni Gigante, Anna Calì, Ivo Boškoski, Graziano Onder, Vincenzo Perri, Guido Costamagna
Digestive Endoscopy.2016; 28(1): 33. CrossRef - Peroral Endoscopic Myotomy for Esophageal Achalasia
Pietro Familiari, Giovanni Gigante, Michele Marchese, Ivo Boskoski, Andrea Tringali, Vincenzo Perri, Guido Costamagna
Annals of Surgery.2016; 263(1): 82. CrossRef - Surgery or Peroral Esophageal Myotomy for Achalasia
Luigi Marano, Giovanni Pallabazzer, Biagio Solito, Stefano Santi, Alessio Pigazzi, Raffaele De Luca, Francesco Giuseppe Biondo, Alessandro Spaziani, Maurizio Longaroni, Natale Di Martino, Virginia Boccardi, Alberto Patriti
Medicine.2016; 95(10): e3001. CrossRef - Prospective evaluation of CT esophagram findings after peroral endoscopic myotomy
Davinderbir Pannu, Dennis Yang, Patricia L. Abbitt, Peter V. Draganov
Gastrointestinal Endoscopy.2016; 84(3): 408. CrossRef - Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years
Yuki B Werner, Guido Costamagna, Lee L Swanström, Daniel von Renteln, Pietro Familiari, Ahmed M Sharata, Tania Noder, Guido Schachschal, Jan F Kersten, Thomas Rösch
Gut.2016; 65(6): 899. CrossRef - Double-Scope Peroral Endoscopic Myotomy (POEM) for Esophageal Achalasia: The First Trial of a New Double-Scope POEM
Hee Jin Hong, Ga Won Song, Weon Jin Ko, Won Hee Kim, Ki Baik Hahm, Sung Pyo Hong, Joo Young Cho
Clinical Endoscopy.2016; 49(4): 383. CrossRef - Achalasia: from diagnosis to management
Michael F. Vaezi, Valter N. Felix, Roberto Penagini, Aurelio Mauro, Eduardo Guimarães Hourneaux de Moura, Leonardo Zorrón Cheng Tao Pu, Jan Martínek, Erwin Rieder
Annals of the New York Academy of Sciences.2016; 1381(1): 34. CrossRef - Complications of submucosal endoscopy
Jean-Michel Gonzalez, Alban Benezech, Marc Barthet
Best Practice & Research Clinical Gastroenterology.2016; 30(5): 783. CrossRef - Update on the endoscopic treatments for achalasia
Dushant S Uppal, Andrew Y Wang
World Journal of Gastroenterology.2016; 22(39): 8670. CrossRef - Gestion des complications de l’endoscopie interventionnelle œsophagienne
C. Lorenceau-Savale, G. Rahmi
Acta Endoscopica.2015; 45(3): 90. CrossRef - Greater curvature myotomy is a safe and effective modified technique in per-oral endoscopic myotomy (with videos)
Manabu Onimaru, Haruhiro Inoue, Haruo Ikeda, Chiaki Sato, Hiroki Sato, Chainarong Phalanusitthepha, Esperanza Grace Santi, Kevin L. Grimes, Hiroaki Ito, Shin-ei Kudo
Gastrointestinal Endoscopy.2015; 81(6): 1370. CrossRef - Peroral Esophageal Myotomy Versus Laparoscopic Heller's Myotomy for Achalasia: A Meta-analysis
Mingtian Wei, Tinghan Yang, Xuyang Yang, Ziqiang Wang, Zongguang Zhou
Journal of Laparoendoscopic & Advanced Surgical Techniques.2015; 25(2): 123. CrossRef - Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: a systematic review and meta-analysis
Rupjyoti Talukdar, Haruhiro Inoue, D. Nageshwar Reddy
Surgical Endoscopy.2015; 29(11): 3030. CrossRef - Is Peroral Endoscopic Myotomy Effective for the Treatment of Spastic Esophageal Disorders Refractory to Medical Therapy?
Jae Pil Han
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2015; 15(2): 143. CrossRef - The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on peroral endoscopic myotomy
Vinay Chandrasekhara, David Desilets, Gary W. Falk, Haruhiro Inoue, John R. Romanelli, Thomas J. Savides, Stavros N. Stavropoulos, Lee L. Swanstrom
Gastrointestinal Endoscopy.2015; 81(5): 1087. CrossRef - Peroral Endoscopic Myotomy for Treating Achalasia and Esophageal Motility Disorders
Young Hoon Youn, Hitomi Minami, Philip Wai Yan Chiu, Hyojin Park
Journal of Neurogastroenterology and Motility.2015; 22(1): 14. CrossRef - Effect of Peroral Endoscopic Myotomy on Esoph ageal Motor Function
Su Jin Hong
Journal of Neurogastroenterology and Motility.2015; 22(1): 1. CrossRef - Achalasia: current treatment options
Pietro Familiari, Santi Greco, Ance Volkanovska, Giovanni Gigante, Anna Cali, Ivo Boškoski, Guido Costamagna
Expert Review of Gastroenterology & Hepatology.2015; 9(8): 1101. CrossRef - Systematic review and meta‐analysis: Efficacy and safety of POEM for achalasia
Lavinia A Barbieri, Cesare Hassan, Riccardo Rosati, Uberto Fumagalli Romario, Loredana Correale, Alessandro Repici
United European Gastroenterology Journal.2015; 3(4): 325. CrossRef - Per-oral endoscopic myotomy white paper summary
Stavros N. Stavropoulos, David J. Desilets, Karl-Hermann Fuchs, Christopher J. Gostout, Gregory Haber, Haruhiro Inoue, Michael L. Kochman, Rani Modayil, Thomas Savides, Daniel J. Scott, Lee L. Swanstrom, Melina C. Vassiliou
Surgical Endoscopy.2014; 28(7): 2005. CrossRef - Peroral endoscopic myotomy for achalasia
A. J. Bredenoord, T. Rösch, P. Fockens
Neurogastroenterology & Motility.2014; 26(1): 3. CrossRef - Peroral Endoscopic Myotomy: Establishing a New Program
Nikhil A. Kumta, Shivani Mehta, Prashant Kedia, Kristen Weaver, Reem Z. Sharaiha, Norio Fukami, Hitomi Minami, Fernando Casas, Monica Gaidhane, Arnon Lambroza, Michel Kahaleh
Clinical Endoscopy.2014; 47(5): 389. CrossRef - Introduction of the per-oral endoscopic myotomy technique to pediatric surgical practice
Stephanie Chao, Michael Russo, Robert Wright, Homero Rivas, James Wall
Journal of Pediatric Surgery Case Reports.2014; 2(6): 313. CrossRef - International Digestive Endoscopy Network 2014: Turnpike to the Future
Eun Young Kim, Kwang An Kwon, Il Ju Choi, Ji Kon Ryu, Ki Baik Hahm
Clinical Endoscopy.2014; 47(5): 371. CrossRef - Per-oral endoscopic myotomy white paper summary
Stavros N. Stavropoulos, David J. Desilets, Karl-Hermann Fuchs, Christopher J. Gostout, Gregory Haber, Haruhiro Inoue, Michael L. Kochman, Rani Modayil, Thomas Savides, Daniel J. Scott, Lee L. Swanstrom, Melina C. Vassiliou
Gastrointestinal Endoscopy.2014; 80(1): 1. CrossRef - Effectiveness of peroral endoscopic myotomy in the treatment of achalasia: A pilot trial in Chinese Han population with a minimum of one‐year follow‐up
Ting Sheng Ling, Hui Min Guo, Tian Yang, Chun Yan Peng, Xiao Ping Zou, Rui Hua Shi
Journal of Digestive Diseases.2014; 15(7): 352. CrossRef - Jackhammer Esophagus Treated by a Peroral Endoscopic Myotomy
Weon Jin Ko, Byoung Moo Lee, Won Young Park, Jin Nyoung Kim, Jun-Hyung Cho, Tae Hee Lee, Su Jin Hong, Joo Young Cho
The Korean Journal of Gastroenterology.2014; 64(6): 370. CrossRef - Effect of peroral endoscopic myotomy in achalasia patients with failure of prior pneumatic dilation: A prospective case–control study
Tingsheng Ling, Huimin Guo, Xiaoping Zou
Journal of Gastroenterology and Hepatology.2014; 29(8): 1609. CrossRef - Medical and Endoscopic Management of Achalasia
Jae Pil Han, Su Jin Hong
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2014; 14(2): 82. CrossRef - EndoFLIP system for the intraoperative evaluation of peroral endoscopic myotomy
Pietro Familiari, Giovanni Gigante, Michele Marchese, Ivo Boskoski, Vincenzo Bove, Andrea Tringali, Vincenzo Perri, Graziano Onder, Guido Costamagna
United European Gastroenterology Journal.2014; 2(2): 77. CrossRef - Per Oral Endoscopic Myotomy (POEM): Review of Current Techniques and Outcomes (Including Postoperative Reflux)
David Friedel, Rani Modayil, Stavros N. Stavropoulos
Current Surgery Reports.2013; 1(4): 203. CrossRef - Peroral Endoscopic Myotomy for the Treatment of Achalasia: An Analysis
Dennis Yang, Mihir S. Wagh
Diagnostic and Therapeutic Endoscopy.2013; 2013: 1. CrossRef - Therapeutic flexible endoscopy replacing surgery: Part 3—Peroral esophageal myotomy
Ezra N. Teitelbaum, Eric S. Hungness
Techniques in Gastrointestinal Endoscopy.2013; 15(4): 211. CrossRef - Highlights of International Digestive Endoscopy Network 2013
Kwang An Kwon, Il Ju Choi, Eun Young Kim, Seok Ho Dong, Ki Baik Hahm
Clinical Endoscopy.2013; 46(5): 425. CrossRef - Perorale endoskopische Myotomie zur Therapie der Achalasie
B.H.A. von Rahden, J. Filser, S. Reimer, H. Inoue, C.-T. Germer
Der Chirurg.2013;[Epub] CrossRef
- Achalasia: Current therapeutic options
- 10,830 View
- 75 Download
- 52 Crossref


 KSGE
KSGE


 First
First Prev
Prev



