Search
- Page Path
- HOME > Search
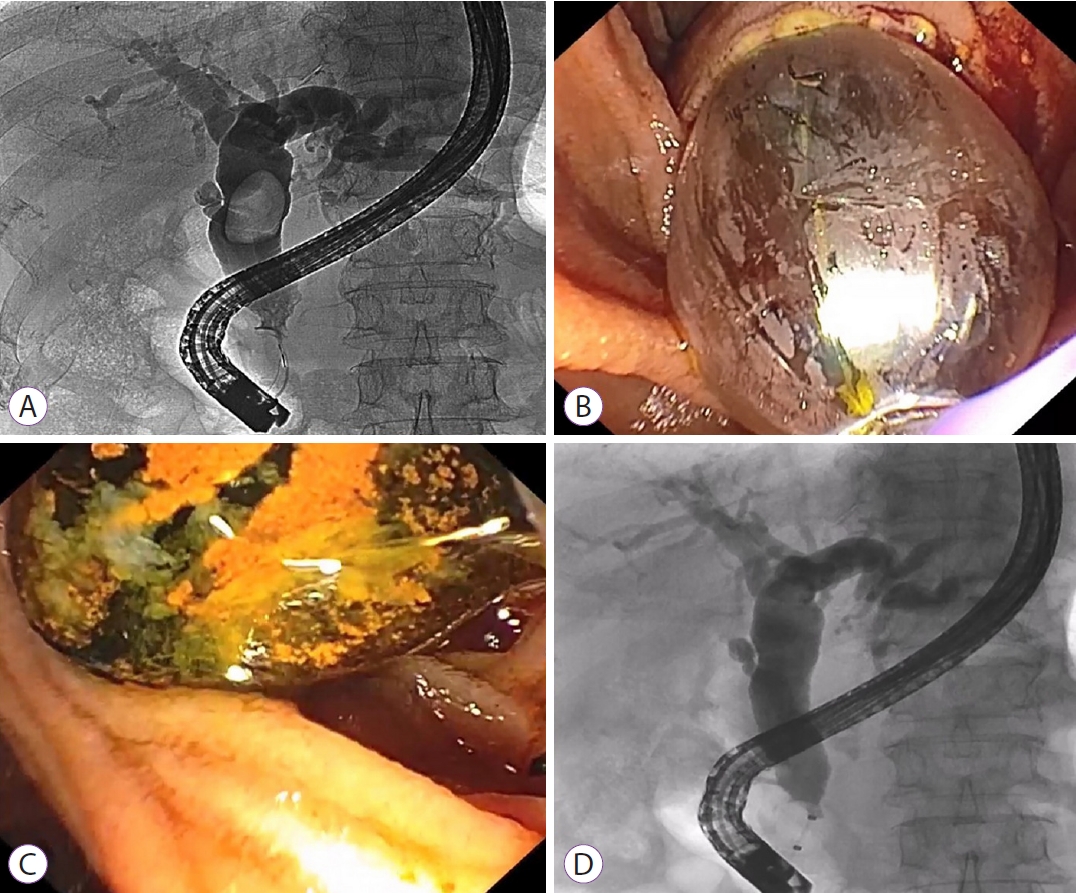
- Successful removal of remnant cystic duct stump stone using single-operator cholangioscopy-guided electrohydraulic lithotripsy: two case reports
- Sung Hyeok Ryou, Hong Ja Kim
- Clin Endosc 2023;56(3):375-380. Published online January 5, 2023
- DOI: https://doi.org/10.5946/ce.2021.273

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Cholecystectomy is the best method for treating gallstone diseases. However, 10%–30% of patients who undergo a cholecystectomy continue to complain of upper abdominal pain, dyspepsia, or jaundice—this is referred to as postcholecystectomy syndrome. Cystic duct stump stones are a troublesome cause of postcholecystectomy syndrome. Conventionally, surgery is mainly performed to remove cystic duct stump stones. However, repeated surgery can cause complications, such as postoperative bleeding, biliary injury, and wound infection. As an alternative method of surgery, endoscopic retrograde cholangiopancreatography is sometimes used to remove cystic duct stump stones, although the success rate is not high due to technical difficulties. Recently, peroral cholangioscopy, which can directly observe the bile duct, has been suggested as an alternative method. We report two cases in which a cystic duct stump stone was successfully removed via a single-operator cholangioscopy, after failure with an endoscopic retrograde cholangiopancreatography.
-
Citations
Citations to this article as recorded by- Holmium Laser Lithotripsy in the Management of Difficult Biliary and Cystic Ductal Stones – A Case Series
Amit Kumar, Harindra Kumar Goje, Nimesh Kumar Tarway, Vivek Hande
Journal of Marine Medical Society.2024;[Epub] CrossRef - Laparoscopic management of remnant gall bladder with stones: Lessons from a tertiary care centre's experience
Gilbert Samuel Jebakumar, Jeevanandham Muthiah, Loganathan Jayapal, R. Santhosh Kumar, Siddhesh Tasgaonkar, K.S. Santhosh Anand, J.K.A. Jameel, Sudeepta Kumar Swain, K.J. Raghunath, Prasanna Kumar Reddy, Tirupporur Govindaswamy Balachandar
Laparoscopic, Endoscopic and Robotic Surgery.2024; 7(1): 27. CrossRef - A remnant cystic duct presenting as a duodenal subepithelial tumor
Gwang Ha Kim, Dong Chan Joo
Clinical Endoscopy.2024; 57(2): 268. CrossRef
- Holmium Laser Lithotripsy in the Management of Difficult Biliary and Cystic Ductal Stones – A Case Series
- 3,762 View
- 186 Download
- 2 Web of Science
- 3 Crossref

- Cracking Difficult Biliary Stones
- Phonthep Angsuwatcharakon, Rungsun Rerknimitr
- Clin Endosc 2021;54(5):660-668. Published online March 16, 2021
- DOI: https://doi.org/10.5946/ce.2020.256-IDEN
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Apart from difficult biliary cannulation, biliary stone removal is considered one of the hurdles in endoscopic retrograde cholangiopancreatography. Generally, simple common bile duct (CBD) stones can be removed either with an extraction balloon or a basket. However, there are difficult stones that cannot be removed using these standard methods. The most difficult stones are large CBD stones and impacted stones in a tapering CBD. A few decades ago, mechanical lithotripsy was usually required to manage these stones. At present, endoscopic papillary large balloon dilation (EPLBD) of the biliary orifice has become the gold standard for large CBD stones up to 1.5 cm. EPLBD can reduce the procedural time by shortening the stone removal process. It can also save the cost of the devices, especially multiple baskets, used in mechanical lithotripsy. Unfortunately, very large CBD stones, stones impacted in a tapering CBD, and some intrahepatic duct stones still require lithotripsy. Peroral cholangioscopy provides direct visualization of the stone, which helps the endoscopist perform a probe-based lithotripsy either with an electrohydraulic probe or a laser probe. This technique can facilitate the management of difficult CBD stones with a high success rate and save procedural time without significant technical complications.
-
Citations
Citations to this article as recorded by- Cholangioscopy as a rescue for a post-cholecystectomy adherent stone formed around a migrated surgical clip in the common bile duct
Chukwunonso Ezeani, Samuel O. Igbinedion, Kwabena Asafo-Agyei, Erik A. Holzwanger, Sultan Mahmood, Mandeep S. Sawhney, Tyler M. Berzin, Moamen Gabr, Douglas K. Pleskow
VideoGIE.2024; 9(5): 241. CrossRef - Endoscopic Treatment of Large Bile Duct Stones: A Systematic Review and Network Meta-Analysis
Antonio Facciorusso, Paraskevas Gkolfakis, Daryl Ramai, Georgios Tziatzios, Janice Lester, Stefano Francesco Crinò, Leonardo Frazzoni, Ioannis S. Papanikolaou, Marianna Arvanitakis, Daniel Blero, Arnaud Lemmers, Pierre Eisendrath, Lorenzo Fuccio, Konstant
Clinical Gastroenterology and Hepatology.2023; 21(1): 33. CrossRef - First experience of endoscopic treatment of large biliary stones by contact lithotripsy
L.L. Generdukayev, D.A. Blagovestnov, Yu.S. Teterin, P.A. Yartsev
Endoskopicheskaya khirurgiya.2023; 29(2): 51. CrossRef - Percutaneous transhepatic cholangioscopy for benign and malignant biliary disease using a novel short single-operator cholangioscope
A. K. Uribe Rivera, B. Seeliger, C. A. Saldivar, E. Houghton, F. Rodríguez, P. Acquafresca, M. Palermo, M. E. Giménez
Surgical Endoscopy.2023; 37(10): 7774. CrossRef - Outcomes of balloon vs basket catheter for clearance of choledocholithiasis: a systematic review and meta-analysis
Ruchi Sharma, Vikram Sharma, Umang Singhal, Madhusudhan Sanaka
Endoscopy International Open.2022; 10(11): E1447. CrossRef
- Cholangioscopy as a rescue for a post-cholecystectomy adherent stone formed around a migrated surgical clip in the common bile duct
- 4,651 View
- 212 Download
- 3 Web of Science
- 5 Crossref

- Minimally Invasive Approach Using Digital Single-Operator Peroral Cholangioscopy-Guided Electrohydraulic Lithotripsy and Endoscopic Nasogallbladder Drainage for the Management of High-Grade Mirizzi Syndrome
- Hyung Ku Chon, Chan Park, Tae Hyeon Kim
- Clin Endosc 2021;54(6):930-934. Published online February 18, 2021
- DOI: https://doi.org/10.5946/ce.2021.015

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Mirizzi syndrome is a rare complication of gallbladder disease that can be difficult to treat. In particular, endoscopic treatment often fails because of the inability to access or to capture the impacted cystic duct stone. We report a case of Mirizzi syndrome grade III that was successfully managed by digital single-operator peroral cholangioscopy-guided electrohydraulic lithotripsy with endoscopic nasogallbladder drainage and interval laparoscopic cholecystectomy. Based on our experience, digital single-operator peroral cholangioscopy-guided electrohydraulic lithotripsy with endoscopic nasogallbladder drainage is a feasible minimally invasive approach for the management of high-grade Mirizzi syndrome.
-
Citations
Citations to this article as recorded by- Difficult Biliary Stones: A Comprehensive Review of New and Old Lithotripsy Techniques
Edoardo Troncone, Michelangela Mossa, Pasquale De Vico, Giovanni Monteleone, Giovanna Del Vecchio Blanco
Medicina.2022; 58(1): 120. CrossRef - Endoscopic management of cystic duct stones and Mirizzi’s syndrome: experience at an academic medical center
Rishi Pawa, Robert Dorrell, Swati Pawa
Endoscopy International Open.2022; 10(01): E135. CrossRef - Mirizzi Syndrome Type IV Successfully Treated with Peroral Single-operator Cholangioscopy-guided Electrohydraulic Lithotripsy: A Case Report with Literature Review
Hirokazu Kawai, Toshifumi Sato, Masaaki Natsui, Kotaro Watanabe, Ryosuke Inoue, Mayuki Kimura, Kazumi Yoko, Syun-ya Sasaki, Masashi Watanabe, Taku Ohashi, Akihiro Tsukahara, Norio Tanaka, Yoshihisa Tsukada
Internal Medicine.2022; 61(23): 3513. CrossRef - Quality of life of treated patients with Mirizi syndrome
F. M. Pavuk
Klinicheskaia khirurgiia.2021; 88(1-2): 69. CrossRef - A Stone in Remnant Cystic Duct Causing Mirizzi Syndrome Following Laparoscopic Cholecystectomy
Min Jae Yang, Do Hyun Park
Clinical Endoscopy.2021; 54(5): 777. CrossRef
- Difficult Biliary Stones: A Comprehensive Review of New and Old Lithotripsy Techniques
- 3,207 View
- 91 Download
- 4 Web of Science
- 5 Crossref

- Electrohydraulic Lithotripsy of an Impacted Enterolith Causing Acute Afferent Loop Syndrome
- Young Sin Cho, Tae Hoon Lee, Soon Oh Hwang, Sunhyo Lee, Yunho Jung, Il-Kwun Chung, Sang-Heum Park, Sun-Joo Kim
- Clin Endosc 2014;47(4):367-370. Published online July 28, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.4.367
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Afferent loop syndrome caused by an impacted enterolith is very rare, and endoscopic removal of the enterolith may be difficult if a stricture is present or the normal anatomy has been altered. Electrohydraulic lithotripsy is commonly used for endoscopic fragmentation of biliary and pancreatic duct stones. A 64-year-old man who had undergone subtotal gastrectomy and gastrojejunostomy presented with acute, severe abdominal pain for a duration of 2 hours. Initially, he was diagnosed with acute pancreatitis because of an elevated amylase level and pain, but was finally diagnosed with acute afferent loop syndrome when an impacted enterolith was identified by computed tomography. We successfully removed the enterolith using direct electrohydraulic lithotripsy conducted using a transparent cap-fitted endoscope without complications. We found that this procedure was therapeutically beneficial.
-
Citations
Citations to this article as recorded by- Migrated Pancreaticojejunal Stent Forming a Stent–Stone Complex in the Jejunum with Resultant Small Bowel Obstruction: A Case Report
Jiwon Kim, Young Han Kim, Byung-Hee Lee
Journal of the Korean Society of Radiology.2023; 84(2): 512. CrossRef - Use of a pneumatic device for intraluminal enterolith fragmentation in horses
Bruna Machado Amaral Rosa, Peterson Triches Dornbusch, Juan Carlos Duque Moreno, Jackson Schade
Equine Veterinary Education.2023;[Epub] CrossRef - Clinical characteristics and indications for surgery for bezoar-induced small bowel obstruction
Shuai Wang, Xiaohui Yang, Yixiong Zheng, Yulian Wu
Journal of International Medical Research.2021; 49(1): 030006052097937. CrossRef - Diagnosis and treatment of the afferent loop syndrome
Panotpol Termsinsuk, Tanyaporn Chantarojanasiri, Nonthalee Pausawasdi
Clinical Journal of Gastroenterology.2020; 13(5): 660. CrossRef - Cola Dissolution Therapy via Ileus Tube Was Effective for Ileus Secondary to Small Bowel Obstruction Induced by an Enterolith
Yuga Komaki, Shuji Kanmura, Akihito Tanaka, Mari Nakashima, Fukiko Komaki, Hiromichi Iwaya, Shiho Arima, Fumisato Sasaki, Yuichiro Nasu, Shiroh Tanoue, Shinichi Hashimoto, Akio Ido
Internal Medicine.2019; 58(17): 2473. CrossRef - Intestinal stones: A rare cause of bowel obstruction
Emilio de León Castorena, Miriam Daniela de León Castorena
SAGE Open Medical Case Reports.2019; 7: 2050313X1984983. CrossRef - Afferent loop obstruction with obstructive jaundice and ileus due to an enterolith after distal gastrectomy: A case report
Koki Sato, Masataka Banshodani, Masahiro Nishihara, Junko Nambu, Yasuo Kawaguchi, Fumio Shimamoto, Keizo Sugino, Hideki Ohdan
International Journal of Surgery Case Reports.2018; 50: 9. CrossRef - Afferent Loop Syndrome after Roux-en-Y Total Gastrectomy Caused by Volvulus of the Roux-Limb
Hideki Katagiri, Kana Tahara, Kentaro Yoshikawa, Alan Kawarai Lefor, Tadao Kubota, Ken Mizokami
Case Reports in Surgery.2016; 2016: 1. CrossRef
- Migrated Pancreaticojejunal Stent Forming a Stent–Stone Complex in the Jejunum with Resultant Small Bowel Obstruction: A Case Report
- 6,140 View
- 66 Download
- 10 Web of Science
- 8 Crossref

- Endoscopic Treatment of Pancreatic Calculi
- Yong Hoon Kim, Sung Ill Jang, Kwangwon Rhee, Dong Ki Lee
- Clin Endosc 2014;47(3):227-235. Published online May 31, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.3.227
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Chronic pancreatitis is a progressive inflammatory disease that destroys pancreatic parenchyma and alters ductal stricture, leading to ductal destruction and abdominal pain. Pancreatic duct stones (PDSs) are a common complication of chronic pancreatitis that requires treatment to relieve abdominal pain and improve pancreas function. Endoscopic therapy, extracorporeal shock wave lithotripsy (ESWL), and surgery are treatment modalities of PDSs, although lingering controversies have hindered a consensus recommendation. Many comparative studies have reported that surgery is the superior treatment because of reduced duration and frequency of hospitalization, cost, pain relief, and reintervention, while endoscopic therapy is effective and less invasive but cannot be used in all patients. Surgery is the treatment of choice when endoscopic therapy has failed, malignancy is suspected, or duodenal stricture is present. However, in patients with the appropriate indications or at high-risk for surgery, endoscopic therapy in combination with ESWL can be considered a first-line treatment. We expect that the development of advanced endoscopic techniques and equipment will expand the role of endoscopic treatment in PDS removal.
-
Citations
Citations to this article as recorded by- Pancreatic duct stones treated by Whipple as a last resort: A case report
Usra I. Ghanem, Peter R. Bael, Izzeddin Bakri, Bashar Jaber, Omar Abu-Zaydeh, Khaled N. Al-Shawa
International Journal of Surgery Case Reports.2024; 115: 109286. CrossRef - Endoscopic Retrograde Cholangiopancreatography for Management of Chronic Pancreatitis
Aliana Bofill-Garcia, Camille Lupianez-Merly
Gastrointestinal Endoscopy Clinics of North America.2024; 34(3): 449. CrossRef - Management of Pancreatic Duct Stones
Christian Gerges, Torsten Beyna, Horst Neuhaus
Gastrointestinal Endoscopy Clinics of North America.2023; 33(4): 821. CrossRef - Transpapillary Pancreatoscopy in an Emergency Hospital
L. L. Generdukayev, Yu. S. Teterin, D. A. Blagovestnov, E. S. Yeletskaya, K. A. Nugumanova, P. A. Yartsev
Russian Sklifosovsky Journal "Emergency Medical Care".2023; 12(2): 316. CrossRef - Rectal indometacin to prevent pancreatitis after extracorporeal shock wave lithotripsy (RIPEP): a single-centre, double-blind, randomised, placebo-controlled trial
Yang-Yang Qian, Nan Ru, Hui Chen, Wen-Bin Zou, Hao Wu, Jun Pan, Bo Li, Lei Xin, Ji-Yao Guo, Xin-Ying Tang, Liang-Hao Hu, Zhen-Dong Jin, Dong Wang, Yi-Qi Du, Luo-Wei Wang, Zhao-Shen Li, Zhuan Liao
The Lancet Gastroenterology & Hepatology.2022; 7(3): 238. CrossRef - ESWL pancreatitis: yet another post-procedural pancreatitis to worry about?
Lars Aabakken, Vemund Paulsen
The Lancet Gastroenterology & Hepatology.2022; 7(3): 199. CrossRef - Per-oral pancreatoscopy with intraductal lithotripsy for difficult pancreatic duct stones: a systematic review and meta-analysis
Thomas R. McCarty, Zain Sobani, Tarun Rustagi
Endoscopy International Open.2020; 08(10): E1460. CrossRef - Pancreatoscopy in endoscopic treatment of pancreatic duct stones: a systematic review
Christian Gerges, David Pullmann, Markus Schneider, Peter Siersema, Erwin van Geenen, Horst Neuhaus, Torsten Beyna
Minerva Chirurgica.2019;[Epub] CrossRef - Management Algorithm of Pancreatic Calculi
Dong Kee Jang, Jun Kyu Lee
The Korean Journal of Pancreas and Biliary Tract.2019; 24(3): 89. CrossRef - Basket impaction during the extraction of a pancreatic ductal stone
Ankit Dalal, Gaurav K. Patil, Amit P. Maydeo, Arun Iyer, Nikhil Patil
Indian Journal of Gastroenterology.2019; 38(6): 550. CrossRef - Laparoscopic pancreatic duct incision and stone removal and T-type tube drainage for pancreatic duct stone: A case report and review of literature
Yang Bai, Shi-An Yu, Li-Yuan Wang, Dao-Jun Gong
World Journal of Clinical Cases.2018; 6(13): 679. CrossRef - Endoscopic Therapies for Chronic Pancreatitis
Jeffrey M. Adler, Timothy B. Gardner
Digestive Diseases and Sciences.2017; 62(7): 1729. CrossRef - Rectally administered indomethacin to prevent post-ESWL-pancreatitis (RIPEP): study protocol for a randomized controlled trial
Yang-Yang Qian, Hui Chen, Xin-Ying Tang, Xi Jiang, Wei Qian, Wen-Bin Zou, Lei Xin, Bo Li, Yan-Fen Qi, Liang-Hao Hu, Duo-Wu Zou, Zhen-Dong Jin, Dong Wang, Yi-Qi Du, Luo-Wei Wang, Feng Liu, Zhao-Shen Li, Zhuan Liao
Trials.2017;[Epub] CrossRef - Recent Advances in Management of Chronic Pancreatitis
Seon Mee Park
The Korean Journal of Gastroenterology.2015; 66(3): 144. CrossRef
- Pancreatic duct stones treated by Whipple as a last resort: A case report
- 9,628 View
- 119 Download
- 10 Web of Science
- 14 Crossref

- Percutaneous Cholangioscopic Lithotripsy for Afferent Loop Syndrome Caused by Enterolith Development after Roux-en-Y Hepaticojejunostomy: A Case Report
- Seong Hyun Kim, Seok Jeong, Don Haeng Lee, Sung Soo Yoo, Keon-Young Lee
- Clin Endosc 2013;46(6):679-682. Published online November 19, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.6.679
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Afferent loop obstruction caused by enterolith formation is rare and cannot be easily treated with endoscopy because of the difficulty associated with the nonsurgical removal of enteroliths. A 74-year-old woman was admitted with fever and acute abdominal pain. Clinical features and imaging studies suggested afferent loop obstruction caused by an enterolith after Roux-en-Y hepaticojejunostomy. Percutaneous transhepatic biliary drainage was initially performed because of severe cholangitis with septic shock. The enterolith was located in the jejunal limb adjacent to the hepaticojejunostomy site. Cholangioscopic lithotripsy was performed through the percutaneous transhepatic route to the enterolith, and the fragments were moved into the efferent loop using scope push and saline flush methods. Here, we describe a case of afferent loop syndrome caused by an enterolith that developed after Roux-en-Y hepaticojejunostomy and was treated with percutaneous transhepatic cholangio-enteroscopic lithotripsy.
-
Citations
Citations to this article as recorded by- Migrated Pancreaticojejunal Stent Forming a Stent–Stone Complex in the Jejunum with Resultant Small Bowel Obstruction: A Case Report
Jiwon Kim, Young Han Kim, Byung-Hee Lee
Journal of the Korean Society of Radiology.2023; 84(2): 512. CrossRef - Enterolith Causing Afferent Loop Perforation After Distal Gastrectomy
Naoya Ozawa, Masaki Kanzaki
Cureus.2023;[Epub] CrossRef - Successful treatment of postoperative nonobstructive recurrent cholangitis by tract conversion surgery after total pancreatectomy: a case report
Masanori Odaira, Fumiki Toriumi, Shota Hoshino, Nozomi Iwama, Yasuhiro Ito, Takashi Endo, Hirohisa Harada
Surgical Case Reports.2023;[Epub] CrossRef - Enterolith in Roux limb causing extrahepatic biliary obstruction in a patient with a hepaticojejunostomy: case report and relevant literature review
Vipan Kumar, Venu Bhargava Mulpuri, Pankaj Gupta, Vikas Gupta
BMJ Case Reports.2022; 15(3): e246935. CrossRef - Choledochoscopy: An update
Tsinrong Lee, Thomas Zheng Jie Teng, Vishal G Shelat
World Journal of Gastrointestinal Endoscopy.2021; 13(12): 571. CrossRef - Roux‐en‐Y enterolith leading to obstruction and ischemic necrosis after pediatric orthotopic liver transplantation
Ralph C. Quillin, Advaith Bongu, Vania Kasper, Jennifer M. Vittorio, Mercedes Martinez, Steven J. Lobritto, Adam D. Griesemer, James V. Guarrera
Pediatric Transplantation.2018;[Epub] CrossRef - Recurrent Cholangitis by Biliary Stasis Due to Non-Obstructive Afferent Loop Syndrome After Pylorus-Preserving Pancreatoduodenectomy: Report of a Case
Yukihiro Sanada, Naoya Yamada, Masanobu Taguchi, Kazue Morishima, Naoya Kasahara, Yuji Kaneda, Atsushi Miki, Yasunao Ishiguro, Akira Kurogochi, Kazuhiro Endo, Masaru Koizumi, Hideki Sasanuma, Takehito Fujiwara, Yasunaru Sakuma, Atsushi Shimizu, Masanobu H
International Surgery.2014; 99(4): 426. CrossRef
- Migrated Pancreaticojejunal Stent Forming a Stent–Stone Complex in the Jejunum with Resultant Small Bowel Obstruction: A Case Report
- 5,999 View
- 46 Download
- 7 Crossref

- Endoscopic Papillary Large Balloon Dilation: Guidelines for Pursuing Zero Mortality
- Dong Ki Lee, Jung Woo Han
- Clin Endosc 2012;45(3):299-304. Published online August 22, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.3.299
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Since endoscopic papillary large balloon dilation (EPLBD) is used to treat benign disease and as a substitute for conventional methods, such as endoscopic sphincterotomy plus endoscopic mechanical lithotripsy, we should aim for zero mortality. This review defines EPLBD and suggests guidelines for its use based on a review of published articles and our large-scale multicenter retrospective review.
-
Citations
Citations to this article as recorded by- Endoscopic Papillary Large Balloon Dilatation (EPLBD) for the Extraction of Common Bile Duct Stones (CBDS).
Mohamed Alsenbesy, Khaled Shahat, Abdallah Nawara, Mohammad Sallam, Mohamed Fakhry, Mohamed Shazly, Mohamed Moussa, Mohammed Tag-Adeen, Hussein El-Amin, Mohammed Sobh
Revista Española de Enfermedades Digestivas.2019;[Epub] CrossRef - Endoscopic Papillary Balloon Dilation/Endoscopic Papillary Large Balloon Dilation
Seok Jeong
The Korean Journal of Pancreas and Biliary Tract.2019; 24(4): 175. CrossRef - Does preserved sphincter of Oddi function prevent common bile duct stones recurrence in patients after endoscopic papillary balloon dilation?
Tzung-Jiun Tsai, Chiun-Ku Lin, Kwok-Hung Lai, Hoi-Hung Chan, E-Ming Wang, Wei-Lun Tsai, Jin-Shiung Cheng, Hsien-Chung Yu, Wen-Chi Chen, Ping-I Hsu
Journal of the Chinese Medical Association.2018; 81(4): 311. CrossRef - Japan Gastroenterological Endoscopy Society guidelines for endoscopic papillary large balloon dilation
Takao Itoi, Shomei Ryozawa, Akio Katanuma, Yoshinobu Okabe, Hironori Kato, Jun Horaguchi, Takayoshi Tsuchiya, Takuji Gotoda, Naotaka Fujita, Kenjiro Yasuda, Yoshinori Igarashi, Kazuma Fujimoto
Digestive Endoscopy.2018; 30(3): 293. CrossRef - International consensus guidelines for endoscopic papillary large-balloon dilation
Tae Hyeon Kim, Jin Hong Kim, Dong Wan Seo, Dong Ki Lee, Nageshwar D. Reddy, Rungsun Rerknimitr, Thawee Ratanachu-Ek, Christopher J.L. Khor, Takao Itoi, Ichiro Yasuda, Hiroyuki Isayama, James Y.W. Lau, Hsiu-Po Wang, Hoi-Hung Chan, Bing Hu, Richard A. Kozar
Gastrointestinal Endoscopy.2016; 83(1): 37. CrossRef - Efficacy and Safety of Endoscopic Papillary Large Balloon Dilation for Removal of Large Bile Duct Stones in Advanced Age
Kook Hyun Kim, Tae Nyeun Kim
Canadian Journal of Gastroenterology and Hepatology.2016; 2016: 1. CrossRef - Tips in biliary stone removal using endoscopic papillary large balloon dilation
Anthony Yuen Bun Teoh, James Yun Wong Lau
Journal of Hepato-Biliary-Pancreatic Sciences.2015;[Epub] CrossRef - Mid‐term outcome of endoscopic sphincterotomy combined with large balloon dilation
Fumihide Itokawa, Takao Itoi, Atsushi Sofuni, Toshio Kurihara, Takayoshi Tsuchiya, Kentaro Ishii, Shujiro Tsuji, Nobuhito Ikeuchi, Junko Umeda, Reina Tanaka, Ryosuke Tonozuka, Mitsuyoshi Honjyo, Fuminori Moriyasu, Kazuhiko Kasuya, Akihiko Tsuchida
Journal of Gastroenterology and Hepatology.2015; 30(1): 223. CrossRef - The Efficacy of Endoscopic Papillary Balloon Dilation for Patients with Acute Biliary Pancreatitis
Wei-Chih Sun, Hoi-Hung Chan, Kwok-Hung Lai, Tzung-Jiun Tsai, Huey-Shyan Lin, Kung-Hung Lin, Kai-Ming Wang, Sung-Shuo Kao, Po-Hung Chiang, Jin-Shiung Cheng, Ping-I Hsu, Wei-Lun Tsai, Wen-Chi Chen, Yun-Da Li, E-Ming Wang
Gastroenterology Research and Practice.2015; 2015: 1. CrossRef - Which Is the Better Treatment for the Removal of Large Biliary Stones? Endoscopic Papillary Large Balloon Dilation versus Endoscopic Sphincterotomy
Woo Hyun Paik, Ji Kon Ryu, Jin Myung Park, Byeong Jun Song, Jaihwan Kim, Joo Kyung Park, Yong-Tae Kim
Gut and Liver.2014; 8(4): 438. CrossRef - A Case of Metabolic Encephalopathy Due to Bleeding after EPBD
June Young Lee, Jee Hyun Kim, Seung Hyeon Jang, Bong Kyun Kang, In Kyeom Hwang, Yoon Suk Lee, Jin-Hyeok Hwang, Jaihwan Kim
Korean Journal of Pancreas and Biliary Tract.2014; 19(2): 94. CrossRef - Efficacy and Safety of Endoscopic Papillary Large Balloon Dilation for Large Bile Duct Stones in Elderly Patients
Ryosuke Tonozuka, Takao Itoi, Atsushi Sofuni, Fumihide Itokawa, Toshio Kurihara, Takayoshi Tsuchiya, Kentaro Ishii, Shujiro Tsuji, Nobuhito Ikeuchi, Junko Umeda, Reina Tanaka, Mitsuyoshi Honjyo, Shuntaro Mukai, Mitsuru Fujita, Fuminori Moriyasu
Digestive Diseases and Sciences.2014; 59(9): 2299. CrossRef - Balloon dilation itself may not be a major determinant of post-endoscopic retrograde cholangiopancreatography pancreatitis
Sung Ill Jang
World Journal of Gastroenterology.2014; 20(45): 16913. CrossRef - Immediate balloon deflation method in endoscopic papillary large balloon dilation for extraction of difficult bile duct stones
Duk Joo Choi, Yeon Suk Kim, Jung Ho Kim, Yang Suh Ku, Min Su Ha, Ju Hyeon Kim
Open Journal of Gastroenterology.2013; 03(02): 142. CrossRef - Long-Term Outcome of Endoscopic Papillary Large Balloon Dilatation
Chang-Il Kwon
Clinical Endoscopy.2013; 46(6): 601. CrossRef - Highlights of Pancreatobiliary Endoscopy in International Digestive Endoscopy Network 2012: How Much Has It Advanced?
Seok Ho Dong
Clinical Endoscopy.2012; 45(3): 297. CrossRef
- Endoscopic Papillary Large Balloon Dilatation (EPLBD) for the Extraction of Common Bile Duct Stones (CBDS).
- 5,538 View
- 80 Download
- 16 Crossref

- Endoscopic Removal of a Severed, Impacted Lithotomy Basket in the Pancreatic Duct in a Patient with Pancreas Divisum -Endoscopic Removal of Severed, Impacted Basket-
- Soo Jung Park, M.D., Sung Koo Lee, M.D., Jeung Hye Han, M.D., Kyung Uk Jo, M.D., Sang Soo Lee, M.D., Dong Wan Seo, M.D. and Myung-Hwan Kim, M.D.
- Korean J Gastrointest Endosc 2007;34(5):286-290. Published online May 30, 2007
-
 Abstract
Abstract
 PDF
PDF - Therapeutic endoscopy in patients with pancreas divisum has continued to evolve with the availability of minor papilla endoscopic sphincterotomy, stenting, or sphinteroplasty. A combination of a sphincterotomy followed by balloon/basket deployment and emergency mechanical lithotripsy had facilitated the removal of impacted or large stones in the pancreatic and biliary ducts. The impaction of the basket with captured stones or rupture of the basket traction-wire during mechanical lithotripsy are rare complications. We report the successful retrieval of a center-severed and impacted lithotomy basket in the duct of Santorini in a 47-year-old patient with pancreas divisum. Endobiliary biopsy forceps were introduced into minor papilla, the basket was drawn and the stone was removed successfully after 2 months. To the best of our knowledge, this is a first report of the removal of a center-severed and impacted lithotomy basket in the pancreatic duct. (Korean J Gastrointest Endosc 2007;34:286290)
- 1,999 View
- 8 Download

- Forecasting and Retreatment of Unsuccessful Endoscopic Mechanical Lithotripsy in Patients with Difficult Bile Duct Stones
- Sang Hyub Lee, M.D., Joo Kyung Park, M.D., Won Jae Yoon, M.D., Jun Kyu Lee, M.D., Ji Kon Ryu, M.D., Yong-Tae Kim, M.D. and Yong Bum Yoon, M.D.
- Korean J Gastrointest Endosc 2005;31(6):374-382. Published online December 30, 2005
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: Endoscopic removal of a bile duct stone becomes more difficult with increasing stone size. The endoscopic mechanical lithotripsy is frequently used to overcome this problem. However, it is necessary to predict its outcome and determine the optimal treatment when it does fail. This study examined the predictors and optimal treatment for an unsuccessful endoscopic mechanical lithotripsy. Methods: One hundred and twenty five patients who underwent endoscopic mechanical lithotripsy, were retrospectively evaluated. Various predictive factors and procedure-related complications were analyzed. In addition, the clinical outcome of retreatment for unsuccessful endoscopic mechanical lithotripsy was evaluated. Results: Endoscopic mechanical lithotripsy was successful in 97 patients (77.6%). An impacted stone(s), stone size (≥30 mm) and stone size/bile duct diameter (>1.0) were significant factors forecasting failure, with an estimated odds ratio 26.67, 5.94 and 5.99, respectively. More frequent complications related with the failure were not observed. When the procedure did fail, all were retreated successfully with various modalities including surgery. Despite the short hospitalization period, non-surgical treatment had a similar clinical outcome to that of surgery. Conclusions: An impacted stone, stone size (≥ 30 mm) or stone size/bile duct diameter (>1.0) in difficult choledocholithiasis are indicators of unsuccessful endoscopic mechanical lithotripsy. Alternative non-surgical treatment might be considered to manage difficult choledocholithiasis when endoscopic mechanical lithotripsy fails. (Korean J Gastrointest Endosc 2005;31:374382)
- 1,811 View
- 2 Download

- A Case of Gastric Bezoar Formed by Ingestion of Gypsum, and it was Treated Endoscopically Using Electrohydraulic Lithotripsy
- Jong Kwan Park, M.D., Min Su Kim, M.D., Young Gyun Kim, M.D., Won Na Suh, M.D., Tae Il Kim, M.D. and Hyojin Park, M.D.
- Korean J Gastrointest Endosc 2005;31(5):328-333. Published online November 30, 2005
-
 Abstract
Abstract
 PDF
PDF - Gastric bezoars are collection of indigestible material in the stomach, and these can be classified into five broad categories: phytobezoar, trichobezoar, pharmacobezoar, lactobezoar and miscellaneous materials such as sand, stone and concrete (gypsum). The treatment of gastric bezoars has recently changed from surgical management to such nonsurgical interventions as enzymatic dissolution, nasogastric suctioning and endoscopic removal by polypectomy snare and basket. Up to the present, electrohydraulic lithotripsy has been a well established method for the treatment of urinary and hepatobiliary stones. We report here on a patient who had a huge gastric bezoar that was formed by the ingestion of gypsum, and this was treated with endoscopic electrohydraulic lithotripsy. (Korean J Gastrointest Endosc 2005;31:328333)
- 1,608 View
- 4 Download

- Gastric Intramural Hematoma Simulating Submucosal Tumor Following Extracorporeal Shockwave Lithotripsy in a Patient with Pancreatic Duct Stones
- Kyung-Jo Kim, M.D.*, Sung Koo Lee, M.D., Myung Hwan Kim, M.D., Dong Wan Seo, M.D., Sang Soo Lee, M.D., and Young Il Min, M.D.
- Korean J Gastrointest Endosc 2005;30(3):150-154. Published online March 31, 2005
-
 Abstract
Abstract
 PDF
PDF - Gastric intramural hematoma is a very rare disease entity. There is no reported case of gastric intramural hematoma in Korea following the extracorporeal shockwave lithotripsy (ESWL). Most have been associated with hereditary coagulopathy, but abdominal trauma, peptic ulceration, and inadvertent ingestion of foreign bodies have been listed as etiologic agents. This is the first description of a case of gastric intramural hematoma simulating gastric submucosal tumor, which regressed spontaneously, following ESWL in a patient with pancreatic duct stones. (Korean J Gastrointest Endosc 2005;30:150154)
- 1,794 View
- 11 Download

- 응급 기계적 쇄석술 실패 후 감돈된 바스켓 제거를 위한 새로운 방법 ( Retrieval of an Impacted Dormia Basket during Emergency Mechanical Lithotripsy Using a Novel Method - Retrieval of impacted basket - )
- Korean J Gastrointest Endosc 2001;22(1):57-61. Published online November 30, 2000
-
 Abstract
Abstract
 PDF
PDF - In many cases where failure to remove the stone during mechanical lithotripsy occur, an emergency mechanical lithotriptor enabled the stone to be removed. Stones captured within an impacted basket are either crushed or the wires of the Dormia basket are broken to release the trapped basket. However, occasionally, emergent mechanical lithotripsy may be complicated by the impaction of a basket wire due to fracture of the traction wire during crushing of the stone. We report a novel method for retrieval of an entrapped Dormia basket fractured just outside the oral cavity during an attempt to use the emergent lithotriptor. This was done by introducing a second Dormia basket into the bile duct. After catching the knob of the impacted basket, the basket was then disengaged from the stone. The simplicity of this maneuver makes it a first line salvage technique to be used before subjecting the patient to more invasive techniques. (Korean J Gastrointest Endosc 2001;22:57 - 61)
- 1,555 View
- 6 Download

- 체외충격파쇄석술을 병행한 담관결석의 내시경적 치료 ( Endoscopic Removal of Difficult Bile Duct Stones Combined with Extracorporeal Shock Wave Lithotripsy )
- Korean J Gastrointest Endosc 1999;19(3):379-385. Published online November 30, 1998
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: Nowadays, common bile duct stones are predominantly extracted endoscopically, after endoscopic papillotomy. Nearly 90% of stones can be removed with a Dormia basket or mechanical lithotripter. In the remaining patients several nonoperative procedures serve as alternatives to surgery. Once extracorporeal lithotripsy had been successfully used for gallbladder stones, this technique was extended to bile duct stones. An experience of endoscopic removal of difficult bile duct stones combined with extracorporeal shock wave lithotripsy (ESWL) is reported. Methods: 82 patients were selected for this treatment because conventional stone extraction had failed. The Biolithos Mark III was used for extracorporeal spark-gap lithotripsy and the shock wave number was 2,000 waves (average) at one session. The stones were detected through a fluoroscopy with dye injection through an endoscopic naso-biliary drainage tube. After the fragmentation of bile duct stones, endoscopic removal of stones was performed for the facilitation of the complete removal of the stones, and to decrease the discomfort of the patients for the duration of their stay. Results: Visualization of the stones using a fluoroscopy with dye injection was possible in all patients. On average, these patients had 3.1 (1∼7) sessions of treatment with ESWL. Fragmentation was achieved in 74 (90.2%) patients and complete stone removal occurred in 71 (86.5%) patients. Complete stone clearance was achieved without further intervention in 8 (11.3%) patients, and in 63 (88.7%) patients after endoscopic extraction of the fragments. Thirty-seven (58.7%) patients underwent one endoscopic intervention to extract the remaining fragments. In 54 (81.8%) patients, a balloon catheter or Dormia basket was sufficient to extract the remaining fragments and an additional mechanical lithotripsy was necessary to break down larger fragments in 12 (18.2%) patients. There were no serious adverse effects from ESWL. Conclusions: Endoscopic removal combined with ESWL is also a useful method for the treatment of difficult bile duct stones to facilitate the complete removal of the stones and to decrease the discomfort of the patients, as well as the duration of their hospitalization. (Korean J Gastrointest Endosc 19: 379∼385, 1999)
- 1,454 View
- 1 Download

- 원저 : 담도 췌장 ; 경피경간적 담도내시경법에 의한 폐쇄성 담도질환의 진단 및 치료 ( Original Articles : Biliary Tract & Pancreas ; The Evaluation and Treatment of the Obstructive Biliary Disease through the Percutaneous Transhepatic Choledocoscopy ( PTCS ) )
- Korean J Gastrointest Endosc 1998;18(1):33-39. Published online November 30, 1997
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: Obstructive jaundice is developed from the cholangiocarcinoma, biiliary tract stone, biliary benign stricture and pancreatic head cancer and is rapidly progress to cholangitis or sepsis. So early decompression, accurate diagnosis and treatment are very important. Percutaneous transhepatic choledocoscopy(PTCS) and endoscopic retrograde choledocoscopy(ERCS) have been used for evaluation of the obstructive jaundice. We performed, through the PTCS, electrohydraulic lithotripsy(EHL) for biliary tract stone rernoval, biopsy for diagnosis of biliary stric and self expandible metalic coil stent(EndocoilTM stent, Instent Co.) insertion on biliary stricture to evaluate the usefullness of PTCS in patients with obstructive jaundice. Methods: Between Auguest 1994 and September 1995, PTCS was performed in 37 patients with obstructive jaundice. First, percutaneous transhepatic biliary drainage(PTBD) with 7Fr. drainage tube was done. Three days later, we exchainged the 7Fr. drainage tube with 16Fr.. Seven days later, through the PTCS, we performed EHL, biopsy and EndocoilTM stent insertion. (Korean J Gastrointest Endosc 18: 33-39, 1998) (continue)
- 1,356 View
- 4 Download

- 증례 : 담도 췌장 ; 담낭 , 담낭관 및 총담관 결석이 동반된 환자에서의 내시경적 담석제거술 ( Case Reports : Biliary Tract & Pancreas ; Endoscopic Biliary Lithotripsy in a Patient with Gallstones of Gallbladder , Cystic Duct , and Common Bile Duct )
- Korean J Gastrointest Endosc 1996;16(2):268-276. Published online November 30, 1995
-
 Abstract
Abstract
 PDF
PDF - Endoseopic sphincterotomy(EST) has been an accepted procedure in patients with current or recurrent common bile duct stones. The success rate of sphineterotomy and of subaequent stone extraction were reported upto 90%. Percutaneous transhepatic cholecystoscopy-lithotripsy(PTCCS-L) could be one of the non-surgical treatment modalities for gallbladder stones, and has been considered as a safe, reliable and technically easy therapeutic procedure through improvement in PTCCS-L manipuiatian and through the development of new devices for this technique. PTCCS-L could be usually performed in the sgrgically high risk groups with gallbladder stones. In this report, we presented successful endoscopic biliary lithotripsy in a 60-year-old male with gallstones of gall bladder, cystic duct, and common bile duct, who was highly risk for surgery, because he has been suffered from advanced liver disease. Endoseopic sphincterotomy and stone removal with basket were done for the removal of common bile duct stones. PTCCS was performed and complete removal of gallbladder stones was achieved. Cystic duict stone was successfully removed after bougie dilation of cystic duct. There has been no recurrence of gallstones until 1 year of follow-up. (Korean J Gastrointest Endosc 16: 268~276, 1996)
- 1,385 View
- 1 Download


 KSGE
KSGE


 First
First Prev
Prev



