Search
- Page Path
- HOME > Search
- Clinical Outcomes and Adverse Events of Gastric Endoscopic Submucosal Dissection of the Mid to Upper Stomach under General Anesthesia and Monitored Anesthetic Care
- Jong-In Chang, Tae Jun Kim, Na Young Hwang, Insuk Sohn, Yang Won Min, Hyuk Lee, Byung-Hoon Min, Jun Haeng Lee, Poong-Lyul Rhee, Jae J Kim
- Clin Endosc 2022;55(1):77-85. Published online July 5, 2021
- DOI: https://doi.org/10.5946/ce.2021.002
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
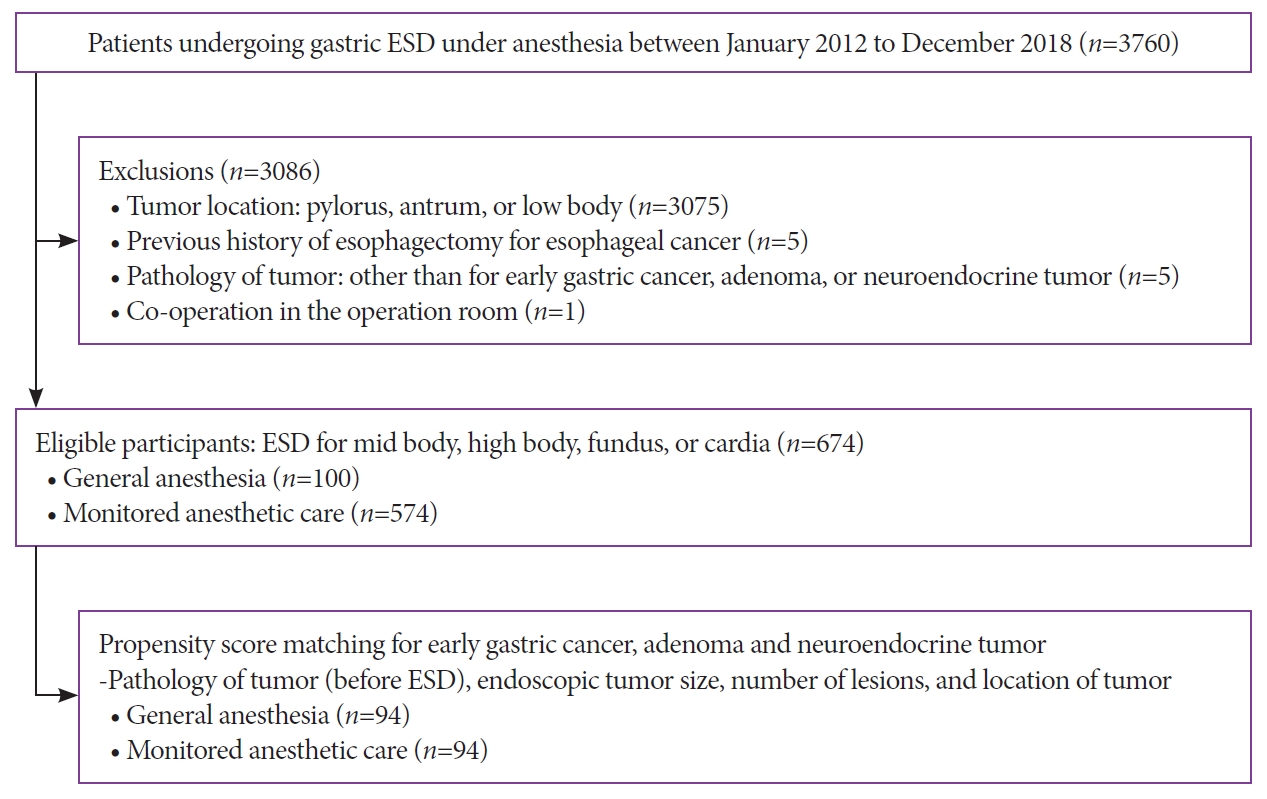
/Aims: Endoscopic submucosal dissection (ESD) of gastric tumors in the mid-to-upper stomach is a technically challenging procedure. This study compared the therapeutic outcomes and adverse events of ESD of tumors in the mid-to-upper stomach performed under general anesthesia (GA) or monitored anesthesia care (MAC).
Methods
Between 2012 and 2018, 674 patients underwent ESD for gastric tumors in the midbody, high body, fundus, or cardia (100 patients received GA; 574 received MAC). The outcomes of the propensity score (PS)-matched (1:1) patients receiving either GA or MAC were analyzed.
Results
The PS matching identified 94 patients who received GA and 94 patients who received MAC. Both groups showed high rates of en bloc resection (GA, 95.7%; MAC, 97.9%; p=0.68) and complete resection (GA, 81.9%; MAC, 84.0%; p=0.14). There were no significant differences between the rates of adverse events (GA, 16.0%; MAC, 8.5%; p=0.18) in the anesthetic groups. Logistic regression analysis indicated that the method of anesthesia did not affect the rates of complete resection or adverse events.
Conclusions
ESD of tumors in the mid-to-upper stomach at our high-volume center had good outcomes, regardless of the method of anesthesia. Our results demonstrate no differences between the efficacies and safety of ESD performed under MAC and GA. -
Citations
Citations to this article as recorded by- General Anesthesia and Endoscopic Upper Gastrointestinal Tumor Resection
Seung Hyun Kim
Journal of Digestive Cancer Research.2023; 11(3): 125. CrossRef - Is General Anesthesia Needed in Endoscopic Submucosal Dissection for Lesions Located in the Mid to Upper Stomach?
Prasit Mahawongkajit, Jirawat Swangsri
Clinical Endoscopy.2022; 55(1): 43. CrossRef - Therapeutic approach to non-curative resection after endoscopic treatment in early gastric cancer
Eun Jeong Gong, Chang Seok Bang
Journal of the Korean Medical Association.2022; 65(5): 284. CrossRef - Paneth Cell Carcinoma of the Stomach
Jun Wan Kim, Gwang Ha Kim, Kyung Bin Kim
The Korean Journal of Gastroenterology.2022; 80(1): 34. CrossRef - Comparing Different Anesthesia Methods on Anesthetic Effect and Postoperative Pain in Patients with Early Gastric Cancer during Endoscopic Submucosal Dissection
Jie Zhang, Yanlei Chen, Zhiwu Liu, Zhihao Pan, Jinghua Pan
Journal of Oncology.2022; 2022: 1. CrossRef
- General Anesthesia and Endoscopic Upper Gastrointestinal Tumor Resection
- 3,708 View
- 173 Download
- 5 Web of Science
- 5 Crossref

- Endoscopic Submucosal Dissection for Early Gastric Neoplasia Occurring in the Remnant Stomach after Distal Gastrectomy
- Ji Young Lee, Byung-Hoon Min, Jung Gyu Lee, Donghyo Noh, Jun Haeng Lee, Poong-Lyul Rhee, Jae J. Kim
- Clin Endosc 2016;49(2):182-186. Published online February 11, 2016
- DOI: https://doi.org/10.5946/ce.2015.049
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic submucosal dissection (ESD) for tumors occurring in the remnant stomach is technically difficult to perform because of limited working space and severe fibrosis and staples present around the suture line. We aimed to elucidate the feasibility and clinical outcomes of performing ESD for tumors in the remnant stomach.
Methods
Between December 2007 and January 2013, 18 patients underwent ESD for tumors (six adenomas and 12 differentiated-type early gastric cancers [EGCs]) occurring in the remnant stomach after distal gastrectomy. Clinicopathologic features and clinical outcomes after ESD were retrospectively analyzed.
Results
Two-thirds of the lesions were located on the body, and half were located on the suture line. En bloc resection, R0 resection, and en bloc with R0 resection rates were 88.9%, 100%, and 88.9%, respectively. Curative resection rate for EGC was 91.7%. Perforation occurred in one patient (5.6%) and was successfully managed by endoscopic closure with metallic clips and conservative management. There was no significant bleeding after ESD. During a median follow-up of 47.5 months, no local, metachronous, or extragastric recurrence was seen for either EGC or adenoma lesions.
Conclusions
ESD is a feasible and effective treatment modality and can be considered a primary intervention for early gastric neoplasia occurring in the remnant stomach. -
Citations
Citations to this article as recorded by- Long-Term Outcomes of Endoscopic Submucosal Dissection for Early Remnant Gastric Cancer: A Retrospective Multicenter Study
Kazunori Tsuda, Shinwa Tanaka, Tetsuya Yoshizaki, Yoshinobu Yamamoto, Takayuki Ose, Tsukasa Ishida, Yasuaki Kitamura, Daisuke Obata, Mineo Iwatate, Atsushi Ikeda, Ryusuke Ariyoshi, Fumiaki Kawara, Hiroshi Takihara, Hirofumi Abe, Toshitatsu Takao, Yoshinor
Digestion.2023; 104(5): 381. CrossRef - The Incidence and Risk Factors for Metachronous Gastric Cancer in the Remnant Stomach after Gastric Cancer Surgery
Yonghoon Choi, Nayoung Kim, Hyuk Yoon, Cheol Min Shin, Young Soo Park, Dong Ho Lee, Young Suk Park, Sang-Hoon Ahn, Yun-Suhk Suh, Do Joong Park, Hyung Ho Kim
Gut and Liver.2022; 16(3): 366. CrossRef - Comparison of Endoscopic Submucosal Dissection and Radical Surgery for Early Gastric Cancer in Remnant Stomach
Yi Liu, Zhihao Chen, Hong Zhou, Yingtai Chen, Lizhou Dou, Yueming Zhang, Yong Liu, Shun He, Dongbing Zhao, Guiqi Wang
Journal of Clinical Medicine.2022; 11(18): 5403. CrossRef - Endoscopic Submucosal Dissection in Patients with Early Gastric Cancer in the Remnant Stomach
Mai Murakami, Takuto Hikichi, Jun Nakamura, Minami Hashimoto, Tsunetaka Kato, Ryoichiro Kobashi, Takumi Yanagita, Rei Suzuki, Mitsuru Sugimoto, Yuki Sato, Hiroki Irie, Mika Takasumi, Tadayuki Takagi, Yuko Hashimoto, Masao Kobayakawa, Hiromasa Ohira
Diagnostics.2022; 12(10): 2480. CrossRef - Intestinal Mucosal Wound Healing and Barrier Integrity in IBD–Crosstalk and Trafficking of Cellular Players
Katrin Sommer, Maximilian Wiendl, Tanja M. Müller, Karin Heidbreder, Caroline Voskens, Markus F. Neurath, Sebastian Zundler
Frontiers in Medicine.2021;[Epub] CrossRef - Clinical outcomes of endoscopic submucosal dissection for lesions on the proximal location between remnant and entire stomach
Su Jin Kim, Cheol Woong Choi, Dae Hwan Kang, Hyung Wook Kim, Su Bum Park, Hyeong Seok Nam, Dae Gon Ryu
Surgical Endoscopy.2020; 34(2): 880. CrossRef - Endoscopic submucosal dissection for early neoplastic lesions in the surgically altered stomach: a systematic review and meta-analysis
Mohamed Barakat, Mohamed Seif, Mohamed M. Abdelfatah, Andrew Ofosu, David L. Carr-Locke, Mohamed O. Othman
Surgical Endoscopy.2019; 33(8): 2381. CrossRef - Current controversies in treating remnant gastric cancer: Are minimally invasive approaches feasible?
Fu-Hai Ma, Hao Liu, Shuai Ma, Yang Li, Yan-Tao Tian
World Journal of Clinical Cases.2019; 7(21): 3384. CrossRef - Endoscopic Submucosal Dissection of Gastric Epithelial Neoplasms after Partial Gastrectomy: A Single-Center Experience
Byeong Gu Song, Gwang Ha Kim, Bong Eun Lee, Hye Kyung Jeon, Dong Hoon Baek, Geun Am Song
Gastroenterology Research and Practice.2017; 2017: 1. CrossRef
- Long-Term Outcomes of Endoscopic Submucosal Dissection for Early Remnant Gastric Cancer: A Retrospective Multicenter Study
- 9,269 View
- 88 Download
- 13 Web of Science
- 9 Crossref

- Usefulness of Ready-to-Use 0.4% Sodium Hyaluronate (Endo-Ease) in the Endoscopic Resection of Gastrointestinal Neoplasms
- Eun Ran Kim, Yun Gyoung Park, Byung-Hoon Min, Jun Haeng Lee, Poong-Lyul Rhee, Jae J. Kim, Jung Ho Park, Dong Il Park, Dong Kyung Chang
- Clin Endosc 2015;48(5):392-398. Published online September 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.5.392
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Commercially available sodium hyaluronate solutions are usually too thick to inject through catheters and need dilution with normal saline (NS) before use, which increases the risk of contamination. We evaluated the usefulness of ready-to-use 0.4% sodium hyaluronate, Endo-Ease (EE; UNIMED Pharm. Inc., Seoul, Korea).
Methods We performed a prospective multicenter randomized study from May 2011 to September 2012. Patients requiring endoscopic resection (ER) for gastric or colorectal neoplasm at two referral hospitals were enrolled.
Results One hundred fifty-four patients (72 with a gastric neoplasm and 82 with a colorectal neoplasm) were included in intention-to-treat analysis. Thirty-seven gastric neoplasms and 43 colorectal neoplasms were enrolled in the EE group. The usefulness rate was significantly higher in the EE group than in the NS group (89.2% vs. 60.0% for gastric neoplasms and 95.3% vs. 67.7% for colorectal neoplasms,
p <0.001). In the EE group, the ease of mucosal resection was significantly higher than in the NS group (p <0.001). The injected volume was smaller in the EE group than in the NS group (p <0.05).Conclusions The use of EE reduced the need for additional injections and improved the ease of ER. A submucosal injection of EE is useful for the ER of both gastric and colorectal neoplasms.
-
Citations
Citations to this article as recorded by- Efficacy and safety of a submucosal injection solution of sodium alginate for endoscopic resection in a porcine model
Kyung Uk Jung, Yeon Jae Lee, Jae-Young Jang, Joo Young Cho
Scientific Reports.2024;[Epub] CrossRef - Injectable temperature-sensitive hydrogel facilitating endoscopic submucosal dissection
Ruifen Xu, Xiaoyu Yang, Tong Yi, Tao Tan, Zhongqi Li, Xuyang Feng, Jing Rao, Pinghong Zhou, Hao Hu, Yonghua Zhan
Frontiers in Bioengineering and Biotechnology.2024;[Epub] CrossRef - Hypertonic solution as an optimal submucosal injection solution for endoscopic resection of gastrointestinal mucosal lesions: Systematic review and network meta‐analysis
Li Gao, Jiawei Bai, Kai Liu, Lulu Wang, Shaohua Zhu, Xin Zhao, Ying Han, Zhiguo Liu
Digestive Endoscopy.2023;[Epub] CrossRef - Injectable Thermosensitive Chitosan Solution with β-Glycerophosphate as an Optimal Submucosal Fluid Cushion for Endoscopic Submucosal Dissection
Seung Jeong, Han Jo Jeon, Kyoung-Je Jang, Sangbae Park, Hyuk Soon Choi, Jong Hoon Chung
Polymers.2021; 13(11): 1696. CrossRef
- Efficacy and safety of a submucosal injection solution of sodium alginate for endoscopic resection in a porcine model
- 7,209 View
- 71 Download
- 4 Web of Science
- 4 Crossref

- A Polypoid Mucosa-Associated Lymphoid Tissue Lymphoma of the Stomach Treated with Endoscopic Polypectomy
- Shin Young Min, Jun Haeng Lee, Poong-Lyul Rhee
- Clin Endosc 2013;46(6):647-650. Published online November 19, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.6.647
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Mucosa-associated lymphoid tissue (MALT) lymphoma of the stomach is the most common extranodal lymphoma of the gastrointestinal tract. It is usually accompanied by
Helicobacter pylori infection, and eradication ofH. pylori remains the mainstay of treatment for gastric MALT lymphoma. However, there is no consensus on the second-line treatment for patients with gastric MALT lymphoma who do not improve after successfulH. pylori eradication. Here, we report the case of a 34-year-old woman who presented with a polypoid type of gastric MALT lymphoma on the greater curvature side of the upper body. Despite successfulH. pylori eradication, the tumor did not regress after 6 months. Because the tumor had a semipedunculated polypoid morphology, gastric polypectomy was implemented as a second-line treatment. No recurrence occurred during the 3-year follow-up period. We suggest that gastric polypectomy be considered an alternative treatment modality for polypoid gastric MALT lymphoma that is unresponsive toH. pylori eradication.
- 6,216 View
- 42 Download


 KSGE
KSGE


 First
First Prev
Prev



