Search
- Page Path
- HOME > Search
- Effectiveness of Autologous Platelet-Rich Plasma for the Healing of Ulcers after Endoscopic Submucosal Dissection
- Eunju Jeong, In kyung Yoo, Ozlem Ozer Cakir, Hee Kyung Kim, Won Hee Kim, Sung Pyo Hong, Joo Young Cho
- Clin Endosc 2019;52(5):472-478. Published online May 17, 2019
- DOI: https://doi.org/10.5946/ce.2018.152
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
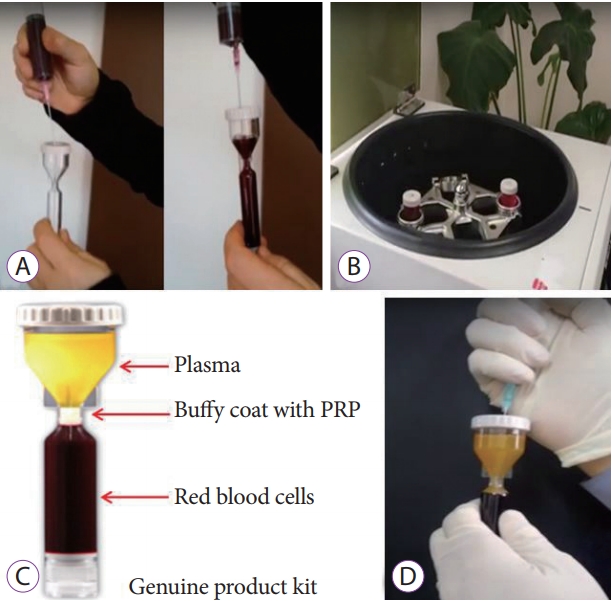
/Aims: Platelet-rich plasma (PRP) has been used for wound healing in various medical fields. The aim of this study was to evaluate the clinical efficacy and safety of local PRP injections after endoscopic submucosal dissection (ESD).
Methods
Patients were non-randomly divided into the following two groups: (1) control group in which patients were administered only an intravenous proton pump inhibitor (PPI), and (2) a study group in which patients were administered an intravenous PPI and a topical PRP injection. We assessed the reduction in the ulcer area and stage of the ulcer after the procedure (24 hours, 48 hours, and 28 days after endoscopic surgery).
Results
We enrolled 7 study and 7 control patients. In the study group, the rate of ulcer reduction was 59% compared to 52% in the control group (p=0.372), 28 days after ESD. There were 5 patients in the S stage and 2 patients in the H stage in the study group compared to no patient in the S stage and 7 patients in the H stage in the control group (p=0.05), 28 days after ESD. There were no serious complications in either group.
Conclusions
The local injection of PRP is a safe and effective procedure for ulcer healing after ESD. -
Citations
Citations to this article as recorded by- Clinical efficacy of blood derivatives on wound healing: A systematic review and network meta‐analysis
Yanhong Wu, Guang Peng, Yuzhi Wang, Jianwu Chen, Bin Zhang, Jianbing Tang, Biao Cheng
International Wound Journal.2024;[Epub] CrossRef - Endoscopic Shielding With Platelet-rich Plasma After Resection Of Large Colorectal Lesions
Vicente Lorenzo-Zúñiga, Vicente Moreno de Vega, Ramón Bartolí
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2021; 31(3): 376. CrossRef - The Additive Effect of Platelet-Rich Plasma in the Treatment of Actively Bleeding Peptic Ulcer
Waseem M. Seleem, Amr Shaaban Hanafy
Clinical Endoscopy.2021; 54(6): 864. CrossRef - Endless Challenges in Overcoming Complications Associated with Endoscopic Submucosal Dissection
Satoshi Ono, Shun Ito, Kenji Ogata
Clinical Endoscopy.2019; 52(5): 395. CrossRef
- Clinical efficacy of blood derivatives on wound healing: A systematic review and network meta‐analysis
- 6,541 View
- 139 Download
- 4 Web of Science
- 4 Crossref

- Korean Society of Gastrointestinal Endoscopy Guidelines for Endoscope Reprocessing
- Byoung Kwan Son, Byung-Wook Kim, Won Hee Kim, Dae-Sung Myung, Young-Seok Cho, Byung Ik Jang, The Disinfection Management and Conscious Sedation Committee of Korean Society of Gastrointestinal Endoscopy
- Clin Endosc 2017;50(2):143-147. Published online March 17, 2017
- DOI: https://doi.org/10.5946/ce.2017.029
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The Korean Society of Gastrointestinal Endoscopy (KSGE) issued guidelines for endoscope reprocessing for the first time in 1995, and the version of the guidelines was updated in August 2009, August 2012, and March 2015. Guidelines for endoscope reprocessing should be revised continuously, because new disinfectants and devices are developed and introduced. The current official version of the KSGE guidelines for endoscope reprocessing is explained herein to assist the reader in understanding the KSGE requirements for cleaning and disinfecting endoscopes.
-
Citations
Citations to this article as recorded by- Comparison of channel sampling methods and brush heads in surveillance culture of endoscope reprocessing: A propensity score matching and paired study
Xue-Yue Ji, Pei-Yong Ning, Chun-Nan Fei, Jia Song, Xue-Mei Dou, Nan-Nan Zhang, Jun Liu, He Liu
Saudi Journal of Gastroenterology.2022; 28(1): 46. CrossRef - Altered Gastric Microbiota and Inflammatory Cytokine Responses in Patients with Helicobacter pylori-Negative Gastric Cancer
Han-Na Kim, Min-Jeong Kim, Jonathan P. Jacobs, Hyo-Joon Yang
Nutrients.2022; 14(23): 4981. CrossRef - Efficacy of a novel channel-cleaning ball brush for endoscope reprocessing: a randomized controlled trial
Kwang Hyun Chung, Jeong Don Chae, Wonho Choe, Hyo Young Lee, Il Hwan Oh, Byoung Kwan Son
Clinical Endoscopy.2022; 55(5): 674. CrossRef - Guidelines for accreditation of endoscopy units: quality measures from the Korean Society of Coloproctology
Rumi Shin, Seongdae Lee, Kyung-Su Han, Dae Kyung Sohn, Sang Hui Moon, Dong Hyun Choi, Bong-Hyeon Kye, Hae-Jung Son, Sun Il Lee, Sumin Si, Won-Kyung Kang
Annals of Surgical Treatment and Research.2021; 100(3): 154. CrossRef - Guidelines for Cancer Care during the COVID-19 Pandemic in South Korea
Jii Bum Lee, Minkyu Jung, June Hyuk Kim, Bo Hyun Kim, Yeol Kim, Young Seok Kim, Byung Chang Kim, Jin Kim, Sung Ho Moon, Keon-Uk Park, Meerim Park, Hyeon Jin Park, Sung Hoon Sim, Hong Man Yoon, Soo Jung Lee, Eunyoung Lee, June Young Chun, Youn Kyung Chung,
Cancer Research and Treatment.2021; 53(2): 323. CrossRef - The Effectiveness of Drying on Residual Droplets, Microorganisms, and Biofilms in Gastrointestinal Endoscope Reprocessing: A Systematic Review
Hefeng Tian, Jiao Sun, Shaoning Guo, Xuanrui Zhu, Han Feng, Yijin Zhuang, Xiu Wang, Konstantinos Triantafyllou
Gastroenterology Research and Practice.2021; 2021: 1. CrossRef - Does the Reprocessing of Endoscopes Have to Take Place Immediately after Pre-Cleaning? A First Evaluation
Vanessa M Eichel, Jonas M Jabs, Samy Unser, Nico T Mutters, Martin Scherrer
Clinical Endoscopy.2021; 54(4): 526. CrossRef - Ambient air pollution in gastrointestinal endoscopy unit
Chang Seok Bang, Keunwook Lee, Young Joo Yang, Gwang Ho Baik
Surgical Endoscopy.2020; 34(9): 3795. CrossRef - Updates on the Disinfection and Infection Control Process of the Accredited Endoscopy Unit
Jeong Eun Shin, Yunho Jung, Jeong Hoon Lee, Byoung Kwan Son, Jae-Young Jang, Hyung-Keun Kim, Byung Ik Jang
Clinical Endoscopy.2019; 52(5): 443. CrossRef - Ambient air pollution in gastrointestinal endoscopy unit; rationale and design of a prospective study
Chang Seok Bang, Keunwook Lee, Jae Ho Choi, Jae Seung Soh, Ji Young Hong, Gwang Ho Baik, Dong Joon Kim
Medicine.2018; 97(49): e13600. CrossRef
- Comparison of channel sampling methods and brush heads in surveillance culture of endoscope reprocessing: A propensity score matching and paired study
- 9,249 View
- 310 Download
- 10 Web of Science
- 10 Crossref

- Double-Scope Peroral Endoscopic Myotomy (POEM) for Esophageal Achalasia: The First Trial of a New Double-Scope POEM
- Hee Jin Hong, Ga Won Song, Weon Jin Ko, Won Hee Kim, Ki Baik Hahm, Sung Pyo Hong, Joo Young Cho
- Clin Endosc 2016;49(4):383-386. Published online March 15, 2016
- DOI: https://doi.org/10.5946/ce.2015.108
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - With the accumulation of clinical trials demonstrating its efficacy and safety, peroral endoscopic myotomy (POEM) has emerged as a less invasive treatment option for esophageal achalasia compared with laparoscopic Heller myotomy. However, the difficulty in determining the exact extent of myotomy, a critical factor associated with the success and safety of the procedure, remains a limitation. Although the various endoscopic landmarks and ancillary techniques have been applied, none of these has been proven sufficient. As a solution for this limitation, the double-scope POEM technique with a second endoscope to assure the exact length of the submucosal tunnel has been applied since 2014. Before double-scope POEM was introduced, the second endoscope was applied only to confirm the accuracy of the procedure. In the present study, we performed double-scope POEM in the treatment of esophageal achalasia through a novel procedure of simultaneous application of the second endoscope to assist in the conventional POEM procedure.
-
Citations
Citations to this article as recorded by- Peroral Endoscopic Myotomy (POEM) in Children: A State of the Art Review
Ali A. Mencin, Amrita Sethi, Monique T. Barakat, Diana G. Lerner
Journal of Pediatric Gastroenterology & Nutrition.2022; 75(3): 231. CrossRef - Per-oral endoscopic myotomy (POEM) for a sigmoid type of achalasia: short-term outcomes and changes in the esophageal angle
Shota Maruyama, Yusuke Taniyama, Tadashi Sakurai, Makoto Hikage, Chiaki Sato, Kai Takaya, Takuro Konno, Takeshi Naitoh, Michiaki Unno, Takashi Kamei
Surgical Endoscopy.2020; 34(9): 4124. CrossRef - Characteristics of a Subset of Achalasia With Normal Integrated Relaxation Pressure
Eunju Kim, In Kyung Yoo, Dong Keon Yon, Joo Young Cho, Sung Pyo Hong
Journal of Neurogastroenterology and Motility.2020; 26(2): 274. CrossRef - Feasibility of using an led-probe in third-space endoscopy: a clinical study
Oscar Víctor Hernández Mondragón, Raúl Zamarripa Mottú, Omar Solórzano Pineda, Raúl Alberto Gutierrez Aguilar, Luís Fernando García Contreras
BMC Gastroenterology.2020;[Epub] CrossRef - 2007–2019: a “Third”-Space Odyssey in the Endoscopic Management of Gastrointestinal Tract Diseases
Anastassios C. Manolakis, Haruhiro Inoue, Akiko Ueno, Yuto Shimamura
Current Treatment Options in Gastroenterology.2019; 17(2): 202. CrossRef - Treatment of Achalasia with Per-Oral Endoscopic Myotomy: Analysis of 50 Consecutive Patients
Erica D. Kane, David J. Desilets, Donna Wilson, Marc Leduc, Vikram Budhraja, John R. Romanelli
Journal of Laparoendoscopic & Advanced Surgical Techniques.2018; 28(5): 514. CrossRef - Two penetrating vessels as a novel indicator of the appropriate distal end of peroral endoscopic myotomy
Shinwa Tanaka, Fumiaki Kawara, Takashi Toyonaga, Haruhiro Inoue, Robert Bechara, Namiko Hoshi, Hirohumi Abe, Yoshiko Ohara, Tsukasa Ishida, Yoshinori Morita, Eiji Umegaki
Digestive Endoscopy.2018; 30(2): 206. CrossRef
- Peroral Endoscopic Myotomy (POEM) in Children: A State of the Art Review
- 7,733 View
- 109 Download
- 9 Web of Science
- 7 Crossref

- Optimal Methods for the Management of Iatrogenic Colonoscopic Perforation
- Dae Kyu Shin, Sun Young Shin, Chi Young Park, Sun Mi Jin, Yang Hyun Cho, Won Hee Kim, Chang-Il Kwon, Kwang Hyun Ko, Ki Baik Hahm, Pil Won Park, Jong Woo Kim, Sung Pyo Hong
- Clin Endosc 2016;49(3):282-288. Published online February 18, 2016
- DOI: https://doi.org/10.5946/ce.2015.046
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Colonoscopic perforations have been managed with exploratory laparotomy, and have resulted in some morbidity and mortality. Recently, laparoscopic surgery is commonly performed for this purpose. The aim of this study was to compare the outcomes of several management strategies for iatrogenic colonoscopic perforations.
Methods
We retrospectively reviewed the medical records of patients who had been treated for colonoscopic perforation between January 2004 and April 2013 at CHA Bundang Medical Center in Korea.
Results
A total of 41 patients with colonoscopic perforation were enrolled. Twenty patients underwent conservative management with a success rate of 90%. Surgical management was performed in 23 patients including two patients who were converted to surgical management after the failure of the initial conservative management. Among 14 patients who underwent surgery at 8 hours after the perforation, there was no considerable difference in adverse outcomes between the laparotomy group and the laparoscopic surgery group. The medical costs and claim rate were 1.45 and 1.87 times greater in the exploratory laparotomy group, respectively.
Conclusions
Conservative management of colonoscopic perforation could be an option for patients without overt symptoms of peritonitis or with a small defect size. If surgical management is required, laparoscopic surgery may be considered as the initial procedure even with a delayed diagnosis. -
Citations
Citations to this article as recorded by- Surgical repair of endoscopy-induced colonic perforations: a case-matched study of short-term morbidity and mortality
Fady DANIEL, Suha JABAK, Mohammad HOSNI, Hani TAMIM, Aurelie MAILHAC, Ayman ALRAZIM, Noura AL-ALI, Robert CHURCH, Mohammad KHALIFE, Shafik SIDANI, Faek JAMALI
Minerva Surgery.2024;[Epub] CrossRef - Laparoscopic versus open surgery for colonoscopic perforation: A systematic review and meta-analysis
Wu Zhong, Chuanyuan Liu, Chuanfa Fang, Lei Zhang, Xianping He, Weiquan Zhu, Xueyun Guan
Medicine.2023; 102(24): e34057. CrossRef - Elastography for Pediatric Chronic Liver Disease
Giovanna Ferraioli, Richard G. Barr, Jonathan R. Dillman
Journal of Ultrasound in Medicine.2021; 40(5): 909. CrossRef - Clinical outcomes of laparoscopic versus open surgery for repairing colonoscopic perforation: a multicenter study
Jae Seok Lee, Jeong Yeon Kim, Byung Mo Kang, Sang Nam Yoon, Jun Ho Park, Bo Young Oh, Jong Wan Kim
Surgery Today.2021; 51(2): 285. CrossRef - The analysis of outcomes of surgical management for colonoscopic perforations: A 16-years experiences at a single institution
Dae Ro Lim, Jung Kul Kuk, Taehyung Kim, Eung Jin Shin
Asian Journal of Surgery.2020; 43(5): 577. CrossRef - Multicenter retrospective evaluation of ileocecocolic perforations associated with diagnostic lower gastrointestinal endoscopy in dogs and cats
Vanessa L. Woolhead, Jacqueline C. Whittemore, Sarah A. Stewart
Journal of Veterinary Internal Medicine.2020; 34(2): 684. CrossRef - Endoscopic Management of the Ascending Colon Perforation Secondary to a Rare-Earth Magnets Ingestion in a Pediatric Patient
Sandra Mabel Camacho-Gomez, James Meredith Noel, Robert Adam Noel
ACG Case Reports Journal.2020; 7(8): e00436. CrossRef - Pseudo‐obstruction But a Real Perforation
AORN Journal.2019; 109(1): 142. CrossRef - Treatment of colonoscopic perforation: outcomes from a major single tertiary institution
Carolyn R. Chew, Justin M. C. Yeung, Ian G. Faragher
ANZ Journal of Surgery.2019; 89(5): 546. CrossRef - Management of colonoscopic perforations: A systematic review
Alexander T. Hawkins, Kenneth W. Sharp, Molly M. Ford, Roberta L. Muldoon, M. Benjamin Hopkins, Timothy M. Geiger
The American Journal of Surgery.2018; 215(4): 712. CrossRef - 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation
Nicola de’Angelis, Salomone Di Saverio, Osvaldo Chiara, Massimo Sartelli, Aleix Martínez-Pérez, Franca Patrizi, Dieter G. Weber, Luca Ansaloni, Walter Biffl, Offir Ben-Ishay, Miklosh Bala, Francesco Brunetti, Federica Gaiani, Solafah Abdalla, Aurelien Ami
World Journal of Emergency Surgery.2018;[Epub] CrossRef - Management Outcomes of Colonoscopic Perforations Are Affected by the General Condition of the Patients
Jae Ho Park, Kyung Jong Kim
Annals of Coloproctology.2018; 34(1): 16. CrossRef - Abdominal Sepsis: An Update
Mircea Gabriel Mureșan, Ioan Alexandru Balmoș, Iudita Badea, Ario Santini
The Journal of Critical Care Medicine.2018; 4(4): 120. CrossRef - Laparoscopic vs. open surgery for the treatment of iatrogenic colonoscopic perforations: a systematic review and meta-analysis
Aleix Martínez-Pérez, Nicola de’Angelis, Francesco Brunetti, Yann Le Baleur, Carmen Payá-Llorente, Riccardo Memeo, Federica Gaiani, Marco Manfredi, Paschalis Gavriilidis, Giorgio Nervi, Federico Coccolini, Aurelien Amiot, Iradj Sobhani, Fausto Catena, Gia
World Journal of Emergency Surgery.2017;[Epub] CrossRef - Urinary Bladder Injury During Colonoscopy Without Colon Perforation
Jung Wook Suh, Jun Won Min, Hwan Namgung, Dong-Guk Park
Annals of Coloproctology.2017; 33(3): 112. CrossRef - The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections
Massimo Sartelli, Alain Chichom-Mefire, Francesco M. Labricciosa, Timothy Hardcastle, Fikri M. Abu-Zidan, Abdulrashid K. Adesunkanmi, Luca Ansaloni, Miklosh Bala, Zsolt J. Balogh, Marcelo A. Beltrán, Offir Ben-Ishay, Walter L. Biffl, Arianna Birindelli, M
World Journal of Emergency Surgery.2017;[Epub] CrossRef - How Should We Manage Iatrogenic Perforation Caused by Colonoscopy?
Eun Sun Kim
Clinical Endoscopy.2016; 49(3): 214. CrossRef
- Surgical repair of endoscopy-induced colonic perforations: a case-matched study of short-term morbidity and mortality
- 8,247 View
- 151 Download
- 20 Web of Science
- 17 Crossref

- Recent Update on Microbiological Monitoring of Gastrointestinal Endoscopes after High-Level Disinfection
- Suk Pyo Shin, Won Hee Kim
- Clin Endosc 2015;48(5):369-373. Published online September 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.5.369
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Endoscopy-related infections are important contributors to nosocomial infections. Endoscope reprocessing according to standard guidelines ensures high-level disinfection and prevents endoscopy-related infections. Microbiological surveillance may help in monitoring the effectiveness of gastrointestinal endoscope disinfection. The process involves microbial cultures and non-culture methods such as bioburden assays, adenosine triphosphate (ATP) bioluminescence, and quantitative polymerase chain reactions (PCRs). Surveillance culturing to monitor endoscopes after reprocessing has been recommended by a majority of organizations. Bioburden assays, ATP bioluminescence, and quantitative PCRs provide rapid and reliable measures. Each institution will have to try to establish its own surveillance guidelines.
-
Citations
Citations to this article as recorded by- Monthly endoscopy surveillance culture facilitates detection of breaches in the scope reprocessing procedure: 5‐year experience in an endoscopy center
Shu‐Hui Chen, Theophile Liu, Huei‐Wen Lai, Hui‐Lan Chang, Hsu‐Heng Yen
Advances in Digestive Medicine.2022; 9(2): 103. CrossRef - Gastrointestinal Endoscopy-Associated Infections: Update on an Emerging Issue
Anasua Deb, Abhilash Perisetti, Hemant Goyal, Mark M. Aloysius, Sonali Sachdeva, Dushyant Dahiya, Neil Sharma, Nirav Thosani
Digestive Diseases and Sciences.2022; 67(5): 1718. CrossRef - Microbiological Surveillance of Endoscopes in a Southern Italian Transplantation Hospital: A Retrospective Study from 2016 to 2019
Valentina Marchese, Daniele Di Carlo, Gaetano Fazio, Santi Mauro Gioè, Angelo Luca, Rossella Alduino, Monica Rizzo, Fabio Tuzzolino, Francesco Monaco, Pier Giulio Conaldi, Bruno Douradinha, Giuseppina Di Martino
International Journal of Environmental Research and Public Health.2021; 18(6): 3057. CrossRef - The application of plan, do, check, act (PDCA) quality management in reducing nosocomial infections in endoscopy rooms: It does work
Xiaoming Kong, Xiaolu Zhu, Yidan Zhang, Jie Wu
International Journal of Clinical Practice.2021;[Epub] CrossRef - Does the Reprocessing of Endoscopes Have to Take Place Immediately after Pre-Cleaning? A First Evaluation
Vanessa M Eichel, Jonas M Jabs, Samy Unser, Nico T Mutters, Martin Scherrer
Clinical Endoscopy.2021; 54(4): 526. CrossRef - Turbulent fluid flow is a novel closed-system sample extraction method for flexible endoscope channels of various inner diameters
Seo Yean Sohn, Michelle J. Alfa, Richard Lai, Yacoob Tabani, Mohamed E. Labib
Journal of Microbiological Methods.2020; 168: 105782. CrossRef - Duodenoscope as a Vector for Transmission
Jennifer T. Higa, Andrew S. Ross
Gastrointestinal Endoscopy Clinics of North America.2020; 30(4): 653. CrossRef - A Prospective, Randomized Comparison of Duodenoscope Reprocessing Surveillance Methods
Travis J. De Wolfe, Nasia Safdar, Megan Meller, John Marx, Patrick R. Pfau, Eric M. Nelsen, Mark E. Benson, Anurag Soni, Mark Reichelderfer, Megan Duster, Deepak V. Gopal
Canadian Journal of Gastroenterology and Hepatology.2019; 2019: 1. CrossRef - Comparative Study of Microbiological Monitoring Results from Three Types of Sampling Methods after Gastrointestinal Endoscope Reprocessing
Su Ma, Lili Feng, Ziyi Jiang, Xian Gao, Xisha Long, Shaonan Zhuang, Wenxia Ding, Taiyao Chen, Zhaoshen Li, Lingjuan Zhang, Huijun Xi, Hongzhi Zhang
BioMed Research International.2019; 2019: 1. CrossRef - Métodos microbiológicos para la monitorización de la limpieza, desinfección y esterilización de dispositivos médicos
Rosa María Blázquez-Garrido, Eva Cuchí-Burgos, Carmen Martín-Salas, Patricia Ruiz-Garbajosa
Enfermedades Infecciosas y Microbiología Clínica.2018; 36(10): 657. CrossRef - The validity of adenosine triphosphate measurement in detecting endoscope contamination
C.E. McCafferty, D. Abi-Hanna, M.J. Aghajani, G.T. Micali, I. Lockart, K. Vickery, I.B. Gosbell, S.O. Jensen
Journal of Hospital Infection.2018; 100(3): e142. CrossRef - Microbiological monitoring of medical devices after cleaning, disinfection and sterilisation
Rosa María Blázquez-Garrido, Eva Cuchí-Burgos, Carmen Martín-Salas, Patricia Ruiz-Garbajosa
Enfermedades infecciosas y microbiologia clinica (English ed.).2018; 36(10): 657. CrossRef - Association Between Storage Interval and Contamination of Reprocessed Flexible Endoscopes in a Pediatric Gastrointestinal Procedural Unit
Patricia Scanlon, Kathleen Flaherty, Erik A. Reilly, Ellen G. Barth, Gail Potter-Bynoe, Jeff Cardini, Ann Marie Riley, Alexander J. McAdam, Thomas J. Sandora
Infection Control & Hospital Epidemiology.2017; 38(2): 131. CrossRef - Surveillance of Endoscopes: Comparison of Different Sampling Techniques
Lien Cattoir, Thomas Vanzieleghem, Lisa Florin, Tania Helleputte, Martine De Vos, Bruno Verhasselt, Jerina Boelens, Isabel Leroux-Roels
Infection Control & Hospital Epidemiology.2017; 38(9): 1062. CrossRef - Education and Training Guidelines for the Board of the Korean Society of Gastrointestinal Endoscopy
Hee Seok Moon, Eun Kwang Choi, Ji Hyun Seo, Jeong Seop Moon, Ho June Song, Kyoung Oh Kim, Jong Jin Hyun, Sung Kwan Shin, Beom Jae Lee, Sang Heon Lee
Clinical Endoscopy.2017; 50(4): 345. CrossRef - Sterile Reverse Osmosis Water Combined with Friction Are Optimal for Channel and Lever Cavity Sample Collection of Flexible Duodenoscopes
Michelle J. Alfa, Harminder Singh, Zoann Nugent, Donald Duerksen, Gale Schultz, Carol Reidy, Patricia DeGagne, Nancy Olson
Frontiers in Medicine.2017;[Epub] CrossRef - The Assessment and Improvement of the Steps in the Endoscope-Reprocessing: A Hospital Report
Habip Gedik
Journal of Bacteriology & Mycology: Open Access.2017;[Epub] CrossRef - Duodenoscope-Associated Bacterial Infections: A Review and Update
Jennifer T. Higa, Michael Gluck, Andrew S. Ross
Current Treatment Options in Gastroenterology.2016; 14(2): 185. CrossRef
- Monthly endoscopy surveillance culture facilitates detection of breaches in the scope reprocessing procedure: 5‐year experience in an endoscopy center
- 10,120 View
- 214 Download
- 17 Web of Science
- 18 Crossref

- Extragastroesophageal Malignancy-Associated Secondary Achalasia: A Rare Association of Pancreatic Cancer Rendering Alarm Manifestation
- Hong Min Kim, Ji Min Chu, Won Hee Kim, Sung Pyo Hong, Ki Baik Hahm, Kwang Hyun Ko
- Clin Endosc 2015;48(4):328-331. Published online July 24, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.4.328
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Secondary achalasia or pseudoachalasia is a rare esophageal motor abnormality, which mimics primary achalasia; it is not easily distinguishable from idiopathic achalasia by manometry, radiological examination, or endoscopy. Although the majority of reported pseudoachalasia cases are associated with neoplasms at or near the esophagogastric (EG) junction, other neoplastic processes or even chronic illnesses such as rheumatoid arthritis can lead to the development of pseudoachalasia, for example, mediastinal masses, gastrointestinal (GI) tumors of the liver and biliary tract, and non-GI malignancies. Therefore, even if a patient presents with the typical findings of achalasia, we should be alert to the possibility of other GI malignancies besides EG tumors. For instance, pancreatic cancer was found in the case reported here; only four such cases have been reported in the literature. A 47-year-old man was admitted to our center with a 3-month history of dysphagia. His endoscopic and esophageal manometric findings were compatible with primary achalasia. However, unresponsiveness to diverse conventional achalasia treatments led us to suspect secondary achalasia. An active search led to a diagnosis of pancreatic mucinous cystadenocarcinoma invading the gastric fundus and EG junction. This rare case of pseudoachalasia caused by pancreatic carcinoma emphasizes the need for suspecting GI malignancies other than EG tumors in patients refractory to conventional achalasia treatment.
-
Citations
Citations to this article as recorded by- Delayed Presentation of Malignancy-Associated Pseudoachalasia of the Gastric Cardia
Clive J Miranda, Farhan Azad, Ross R Moyer, Sasikanth N Ravi, Gina M Sparacino
Cureus.2024;[Epub] CrossRef - Is it necessary to perform a morphological assessment for an esophageal motility disorder? A retrospective descriptive study
Sofya Latrache, Chloe Melchior, Charlotte Desprez, Sabrina Sidali, Julien Recton, Olivier Touchais, Elise van der Eecken, Fabien Wuestenberghs, Cloe Charpentier, Anne Marie Leroi, Guillaume Gourcerol
Clinics and Research in Hepatology and Gastroenterology.2021; 45(6): 101633. CrossRef - When a Late Metastasis Is Hard to Swallow
Catarina Negrão, Rita Sismeiro, Margarida Monteiro, Filipa G Pereira, Marta Jonet
Cureus.2021;[Epub] CrossRef - Development of pseudoachalasia following magnetic sphincter augmentation (MSA) with restoration of peristalsis after endoscopic dilation
Katrin Schwameis, Shahin Ayazi, Ali H. Zaidi, Toshitaka Hoppo, Blair A. Jobe
Clinical Journal of Gastroenterology.2020; 13(5): 697. CrossRef - Burkitt’s Lymphoma of the Gastrohepatic Omentum: A Malignant Presentation of Pseudoachalasia
Eric Omar Then, Andrew Ofosu, Prashanth Rawla, Tagore Sunkara, Sriharsha Dadana, Andrea Culliford, Vinaya Gaduputi
Case Reports in Gastrointestinal Medicine.2019; 2019: 1. CrossRef
- Delayed Presentation of Malignancy-Associated Pseudoachalasia of the Gastric Cardia
- 7,129 View
- 57 Download
- 6 Web of Science
- 5 Crossref

-
Endoscopic Submucosal Dissection Using a Novel Versatile Knife: An Animal Feasibility Study (with Video)

- Chang-Il Kwon, Gwangil Kim, Il-Kwun Chung, Won Hee Kim, Kwang Hyun Ko, Sung Pyo Hong, Seok Jeong, Don Haeng Lee
- Clin Endosc 2014;47(6):544-554. Published online November 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.6.544
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub Background/Aims In order to reduce the procedure time and the number of accessory changes during endoscopic submucosal dissection (ESD), we developed a novel versatile knife, which has the combined advantages of several conventional knives. The aim of this study was to compare the efficacy, safety, and histological quality of ESD performed using this novel versatile knife and a combination of several conventional knives.
Methods This was an
in vivo animal study comparing two different modalities of ESD in mini-pigs. Completion time of each resection was documented, and the resected specimens were retrieved and evaluated for completeness. To assess the quality control of the procedures and adverse events, detailed histopathological examinations were performed.Results A total of 18 specimens were dissected by ESD safely and easily (nine specimens using the new versatile knife; nine specimens by mixing conventional knives). All resections were completed as
en bloc resections. There was no significant difference in procedure time between the 2 modalities (456 seconds vs. 355 seconds,p =0.258) and cutting speed (1.983 mm2/sec vs. 1.57 mm2/sec,p =1.000). The rate of adverse events and histological quality did not statistically differ between the modalities.Conclusions ESD with a versatile knife appeared to be an easy, safe, and technically efficient method.
-
Citations
Citations to this article as recorded by- Comparison of synchronous dual wavelength diode laser versus conventional endo-knives for esophageal endoscopic submucosal dissection: an animal study
Jian Tang, Shufang Ye, Xueliang Ji, Jun Li, Feng Liu
Surgical Endoscopy.2018; 32(12): 5037. CrossRef - Technological review on endoscopic submucosal dissection: available equipment, recent developments and emerging techniques
Georgios Mavrogenis, Juergen Hochberger, Pierre Deprez, Morteza Shafazand, Dimitri Coumaros, Katsumi Yamamoto
Scandinavian Journal of Gastroenterology.2017; 52(4): 486. CrossRef
- Comparison of synchronous dual wavelength diode laser versus conventional endo-knives for esophageal endoscopic submucosal dissection: an animal study
- 7,189 View
- 60 Download
- 3 Web of Science
- 2 Crossref

- Gastrointestinal Cancers in a Peutz-Jeghers Syndrome Family: A Case Report
- Sang Hee Song, Kun Woo Kim, Won Hee Kim, Chang Il Kwon, Kwang Hyun Ko, Ki Baik Hahm, Pil Won Park, Sung Pyo Hong
- Clin Endosc 2013;46(5):572-575. Published online September 30, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.5.572
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub A 17-year-old man was diagnosed as Peutz-Jeghers syndrome (PJS) because of pigmented lip and multiple gastrointestinal polyps. He had anemia and underwent polypectomy on the duodenum and colon. His maternal family members were patients with PJS. His mother used to be screened with endoscopy to remove large polyps. One and half years later, he underwent jejunal segmental resection due to intussusceptions. He underwent endoscopic polypectomy every 2 to 3 years. When he was 23 years old, high-grade dysplasia was found in colonic polyp and his mother underwent partial pancreatectomy due to intraductal papillary mucinous carcinoma. When he was 27 years old, diffuse gastric polyps on the greater curvature of corpus expanded and grew. Therefore, wide endoscopic polypectomy was done. Histological examination revealed focal intramucosal carcinoma and low-grade dysplasia in hamartomatous polyps. We report cases of cancers occurred in first-degree relatives with PJS.
-
Citations
Citations to this article as recorded by- Familial and hereditary gastric cancer, an overview
Fátima Carneiro
Best Practice & Research Clinical Gastroenterology.2022; 58-59: 101800. CrossRef - Small bowel intussusception and concurrent sigmoid polyp with malignant transformation in Peutz–Jeghers syndrome
Maidah Algarni, Enas Raml, Nora Trabulsi, Mohammed Nassif
Journal of Surgical Case Reports.2019;[Epub] CrossRef - The first European family with gastric adenocarcinoma and proximal polyposis of the stomach: case report and review of the literature
Rudolf Repak, Darina Kohoutova, Miroslav Podhola, Stanislav Rejchrt, Marek Minarik, Lucie Benesova, Michal Lesko, Jan Bures
Gastrointestinal Endoscopy.2016; 84(4): 718. CrossRef - Gastric Hamartomatous Polyps—Review and Update
Monika Vyas, Xiu Yang, Xuchen Zhang
Clinical Medicine Insights: Gastroenterology.2016; 9: CGast.S38452. CrossRef - Giant rectal polyp prolapse in an adult patient with the Peutz-Jeghers syndrome
Ana Delfina Cano-Contreras, Arturo Meixueiro-Daza, Peter Grube-Pagola, Jose Maria Remes-Troche
BMJ Case Reports.2016; : bcr2016215629. CrossRef - Prevention Strategies for Gastric Cancer: A Global Perspective
Jin Young Park, Lawrence von Karsa, Rolando Herrero
Clinical Endoscopy.2014; 47(6): 478. CrossRef
- Familial and hereditary gastric cancer, an overview
- 6,559 View
- 58 Download
- 6 Crossref

- Endoscopic Treatment of Refractory Gastroesohageal Reflux Disease
- Won Hee Kim, Pil Won Park, Ki Baik Hahm, Sung Pyo Hong
- Clin Endosc 2013;46(3):230-234. Published online May 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.3.230
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Though efficient acid suppression with proton pump inhibitors (PPIs) remains the mainstay of treatment of gastroesophageal reflux disease (GERD), some of the patients showed refractory response to PPIs, necessitating further intervention. After increasing dose of PPIs and other kinds of pharmacological intervention adopting prokinetics or others, variable endoscopic treatments are introduced for the treatment of these refractory cases. The detailed introduction regarding endoscopic treatment for GERD is forwarded in this review article. Implantation of reabsorbable or synthetic materials in the distal esophagus was tried in vain and is expelled from the market due to limited efficacy and serious complication. Radiofrequency energy delivery (Stretta) and transoral incisionless fundoplication (EsophyX) are actively tried currently.
-
Citations
Citations to this article as recorded by- Refractory gastroesophageal reflux disease
C. R. Subramanian, G. Triadafilopoulos
Gastroenterology Report.2015; 3(1): 41. CrossRef - Long-term outcomes of patients with refractory gastroesophageal reflux disease following a minimally invasive endoscopic procedure: a prospective observational study
Wei-Tao Liang, Zhong-Gao Wang, Feng Wang, Yue Yang, Zhi-Wei Hu, Jian-Jun Liu, Guang-Chang Zhu, Chao Zhang, Ji-Min Wu
BMC Gastroenterology.2014;[Epub] CrossRef
- Refractory gastroesophageal reflux disease
- 7,730 View
- 73 Download
- 2 Crossref

- Endoscopically Diagnosed Gastric Cancers: Looking Alike, but Behave Differently
- Won Hee Kim, Ki Baik Hahm
- Clin Endosc 2013;46(2):111-112. Published online March 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.2.111
- 4,448 View
- 35 Download

- An Impacted Pancreatic Stone in the Papilla Induced Acute Obstructive Cholangitis in a Patient with Chronic Pancreatitis
- Kwang-Ho Yoo, Chang-Il Kwon, Sang-Wook Yoon, Won Hee Kim, Jung Min Lee, Kwang Hyun Ko, Sung Pyo Hong, Pil Won Park
- Clin Endosc 2012;45(1):99-102. Published online March 31, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.1.99
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Obstructive jaundice is very rarely caused by impaction of a pancreatic stone in the papilla. We report here on a case of obstructive jaundice with acute cholangitis that was caused by an impacted pancreatic stone in the papilla in a patient with chronic pancreatitis. A 48-year-old man presented with acute obstructive cholangitis. Abdominal computed tomography with the reconstructed image revealed distal biliary obstruction that was caused by a pancreatic stone in the pancreatic head, and there was also pancreatic ductal dilatation and parenchymal atrophy of the pancreatic body and tail with multiple calcifications. Emergency duodenoscopy revealed an impacted pancreatic stone in the papilla. Precut papillotomy using a needle knife was performed, followed by removal of the pancreatic stone using grasping forceps. After additional sphincterotomy, a large amount of dark-greenish bile juice gushed out. The patient rapidly improved and he has remained well.
-
Citations
Citations to this article as recorded by- Pancreatic stones causing secondary biliary obstruction: An uncommon presentation of chronic pancreatitis
Wesley C. Judy, Tom K. Lin
JPGN Reports.2024;[Epub] CrossRef - The “squeezing with forceps” method for emergency endoscopic removal of an impacted pancreatic stone in the papilla of a patient on antithrombotic therapy
Sho Kitagawa, Shori Ishikawa, Keiya Okamura
Endoscopy.2023; 55(S 01): E454. CrossRef - Biliary Outlet Obstruction Due to Pancreatic Calculi in a Post-cholecystectomy Patient
Joey Almaguer, Dylan Murray, Matthew Murray, Richard Murray
Cureus.2023;[Epub] CrossRef - Ampullary stone in chronic pancreatitis causing obstructive jaundice and cholangitis
Sandheep Janardhanan, Allwin James, Alagammai Palaniappan, Ramesh Ardhanari
Gastroenterology, Hepatology and Endoscopy Practice.2021; 1(2): 69. CrossRef - Ursodeoxycholic acid attenuates 5‑fluorouracil‑induced mucositis in a rat model
Seung Kim, Hoon Chun, Hyuk Choi, Eun Kim, Bora Keum, Yeon Seo, Yoon Jeen, Hong Lee, Soon Um, Chang Kim
Oncology Letters.2018;[Epub] CrossRef - Pancreatic Calculus Causing Biliary Obstruction: Endoscopic Therapy for a Rare Initial Presentation of Chronic Pancreatitis
Anurag J. Shetty, C. Ganesh Pai, Shiran Shetty, Girisha Balaraju
Digestive Diseases and Sciences.2015; 60(9): 2840. CrossRef
- Pancreatic stones causing secondary biliary obstruction: An uncommon presentation of chronic pancreatitis
- 5,953 View
- 50 Download
- 6 Crossref


 KSGE
KSGE


 First
First Prev
Prev



