INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is a well-established procedure that has been in use for a long time. The success rate of ERCP-related procedures in patients with normal anatomy is 95%.1 In contrast, ERCP in patients with surgically altered anatomy (SAA) is difficult to complete. Patients with SAA includes those who have had a Roux-en-Y gastrectomy (including Roux-en-Y gastric bypass), hepaticojejunostomy with Roux-en-Y (in which all of the stomach is preserved), pancreaticoduodenectomy, and Billroth II gastrectomy. In these patients, various challenges have to be resolved to complete the intended procedure. First, the path to the target site (e.g., papilla or hepaticojejunal anastomosis) is longer compared to normal anatomy, especially for Roux-en-Y anastomosis. Second, selective biliary cannulation in patients with an intact papilla is difficult as the papilla is observed as an inverse image and often located in a tangential direction. Moreover, the completion of selected procedures, such as stone extraction (including endoscopic sphincterotomy [EST]) and self-expandable metallic stent (SEMS) placement, can be exceptionally challenging. In the last two decades, the success rate of selected procedures in patients with SAA, especially those involving the papilla or a hepaticojejunal anastomosis, using conventional endoscopes, such as duodenoscope and pediatric colonoscope, have not been satisfactory.2-4 In failed cases, surgery or percutaneous transhepatic biliary drainage (PTBD) has been necessary.
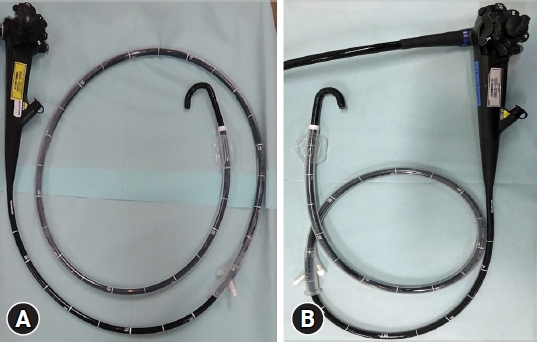
Double-balloon enteroscopy (DBE) was first introduced clinically in 2001.5 Since then, DBE and single-balloon enteroscopy (SBE)-assisted ERCPs have become the preferable approaches for patients with SAA (Fig. 1A).6-9 Importantly, balloon enteroscopy facilitates scope insertion towards the target site. The latest systematic review and meta-analysis regarding SBE-assisted ERCP reported a pooled total procedure success rate of 75.8%.10 However, the scopes used in SBE-assisted ERCP usually have a working length of 200 cm and a channel of 2.8 mm in diameter and only a few ERCP-accessories have been available. To overcome these limitations, a short-type DBE and SBE (short SBE) with a working length of 152 cm and a channel of 3.2 mm in diameter has been introduced (Fig. 1B). Short SBE can be used with many of accessories needed in procedures, such as stone extraction or SEMS placement.11-13 The reported total procedural success rate of short SBE-assisted ERCP ranged between 70.4% to 85.9% (Table 1).14-17 A recent multi-center study of short SBE-assisted ERCP in patients with SAA reported a total procedural success and adverse event rate of 74.9% and 7.7%, respectively.18 The same study identified several factors associated with procedural failure, including Roux-en-Y anastomosis and malignant cases.18
ERCP in patients with Billroth II gastrectomy is considered possible using the side-viewing and conventional forward-viewing endoscopes. However, there is a reported 10% of scope insertion failure cases using these scopes due to the long and angulated afferent loop. Hence, the use of SBE in difficult cases can provide unique advantages, even in patients with Billroth II gastrectomy.19,20
As more and more endoscopists perform balloon endoscopy (BE)-assisted ERCP, it is important to elucidate technical tips to ensure better outcomes and prevent serious adverse events, such as intestinal perforation. This review discussed the technical tips for performing SBE-assisted ERCP in patients with SAA.
TECHNICAL TIPS FOR SCOPE INSERTION
Before inserting the scope, it is important to examine the patientŌĆÖs past operation record to determine the reconstruction method and access of the afferent limb. In our facility, an attachment cap is placed at the tip of the scope in all cases. This cap facilitates not only scope insertion but also selective biliary cannulation. Importantly, not using the attachment cap is one of the factors attributed to total procedural failure.16 It is also useful to insert the scope under carbon dioxide; otherwise, the room air that accumulates in the small intestine can render insertion difficult. The patients are usually in the prone position to prevent pulmonary aspiration and allow confirmation of the scope position using fluoroscopy.
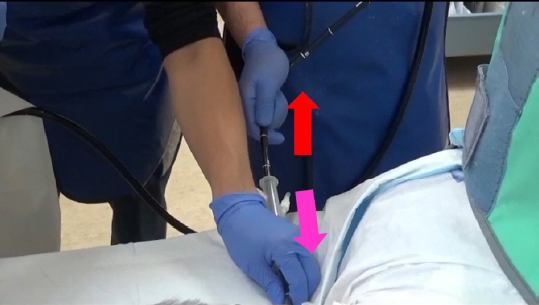
The principle of deep insertion using SBE is referred to as the ŌĆ£push and pullŌĆØ method. After pushing the scope pass the corner in the small intestine, the scope is pulled to create pleats that shorten the small intestine. At the time of shortening, the balloon that is attached to the tip of the overtube is advanced. Before performing the shortening, it is better to advance the overtube as deep as possible toward the tip of scope. When advancing the overtube, the balloon should be deflated. While advancing the overtube, the scope tends to also advance, but this is not effective. To overcome this, the scope itself should be pulled while advancing the overtube (Fig. 2 and Supplementary Video 1). When performing the shortening, the balloon is inflated to fix the small intestine and the scope is pulled while the scope angle is used to hook the small intestine. Of note, this is performed without withdrawing the scope. Particularly, the pathway to the target site in patients with hepaticojejunostomy and Roux-en-Y with preserved stomach is long. Therefore, it is important to maximize the scope shortening step. Importantly, scope shortening should be performed right after a loop is made as scope shortening is more difficult if the scope keeps advancing while the loop remained. Immediately after passing through a sharp flexure is an ideal time for scope shortening. It is sometimes difficult to advance the scope when passing through a sharp flexure. Short SBE has a passive bending function which facilitates the smooth passage of the scope through the bend and advance forward.11 Changing the patient to the left lateral position or abdominal compression can effectively facilitate this procedure.
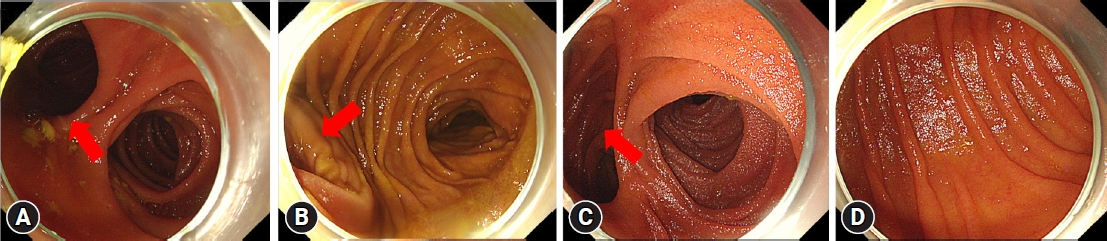
Identifying the afferent limb is one of the next challenges following scope insertion. The way to identify the afferent limb is different depending on the reconstruction method. Distinguishing the junction between the afferent and efferent limbs in patients with Billroth II gastrectomy and pancreaticoduodenectomy (Whipple or Child procedure) is easier than in patients with a Roux-en-Y anastomosis. In the majority of cases, the steep bending part is the afferent limb (Fig. 3A, B). On the other hand, in patients with a Roux-en-Y anastomosis, the anatomy is difficult because the steep bending part is not always the afferent limb. Previous studies have suggested several methods for differentiating the afferent limb, such as confirmation using intraluminal indigo carmine injection or carbon dioxide insufflation at the Roux-en-Y anastomosis.21,22 However, identification can sometimes be difficult even with these methods. To overcome this challenge, we try to confirm the disruption of the transverse folds in patients with Roux-en-Y gastrectomy. As the afferent limb is anastomosed to the side of the slit in Roux-en-Y anastomosis, the site of the disruption can be considered the afferent limb (Fig. 3C).23 In contrast, in patients with hepaticojejunostomy with Roux-en-Y, the transverse folds are symmetric and there is no disruption, thus it is most difficult to identify the afferent limb (Fig. 3D). In such cases, confirming the shape of the scope using fluoroscopy to determine whether the tip of the scope is advancing towards the afferent or efferent limb is necessary.
When inserting the scope to the target site, intestinal perforation from the tight adhesion may arise, especially near the target site. A multi-center study reported intestinal perforation in 1.9% of patients.18 Patients with Billroth II tend to have a short afferent loop between the gastro-jejunal anastomosis and Treitz ligament, which leads to the highest risk of perforation as a strong force is applied to this segment when advancing the scope.24 Careful scope manipulation is required in such cases.
TECHNICAL TIPS FOR SELECTIVE BILIARY CANNULATION
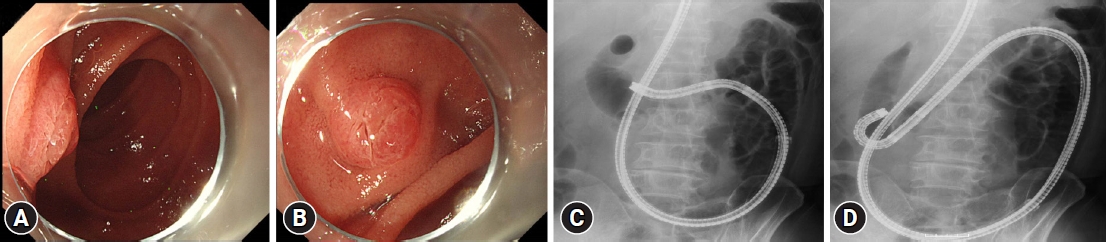
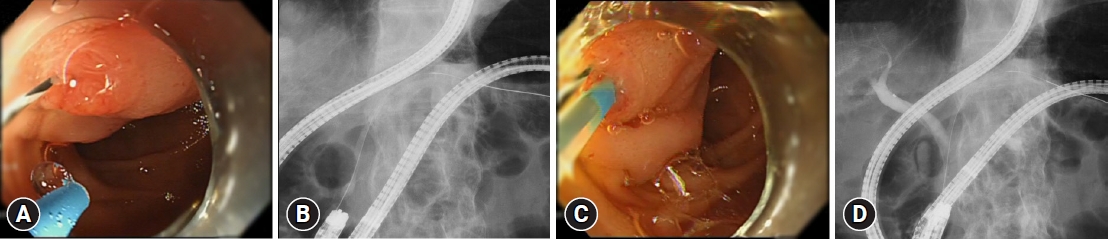
The bile duct is located at 11 to 12 oŌĆÖclock of the papilla in normal anatomy. On the contrary, it is located at 5 to 6 oŌĆÖclock in patients with SAA, such as Roux-en-Y gastrectomy or Billroth II gastrectomy, because the papilla is located as an inversed image. Moreover, the method of cannulation is significantly different between DBE and SBE due to the direction of the working channel where the catheter passes through. As the catheter appears from the half past five (05:30) direction in DBE, the positioning and fixing of the papilla at a six oŌĆÖclock direction on the endoscopic view is considered appropriate. In contrast, as the catheter appears from the eight oŌĆÖclock direction in SBE, the positioning and fixing of the papilla at eleven oŌĆÖclock direction is indicated (Fig. 4B).25 Therefore, it is important to control the view of the papilla depending on what type of scope is used for the BE-assisted ERCP. Moreover, as the SBE (also the DBE) has no elevator function, the brand-new straight catheter (without pre-grooming) should be used when performing selective biliary cannulation. The bendable catheter is also useful as it allows the direction of the bile duct to be adjusted.
The papilla is useful for locating the tangential direction of the scope, especially in patients with a Roux-en-Y gastrectomy. In such situations, the retroflex position is useful.26 As the endoscope is advanced, the retroflex position is formed by the up angle of the inferior part of the duodenal angle. As such, the scope makes a J-turn form to provide a better view of the papilla. A good view of the papilla facilitates better success in selective biliary cannulation (Fig. 4). Using multivariate analysis, a previous study determined that the retroflex position increases the likelihood of success in selective biliary cannulation among patients with Roux-en-Y gastrectomy.27 The success rate using the retroflex position is reportedly approximately 60%.24 The success rate depends on the duodenal space and the extent of intestinal adhesion. If forming the retroflex position seems too difficult, it should be omitted, otherwise intestinal perforation may occur.
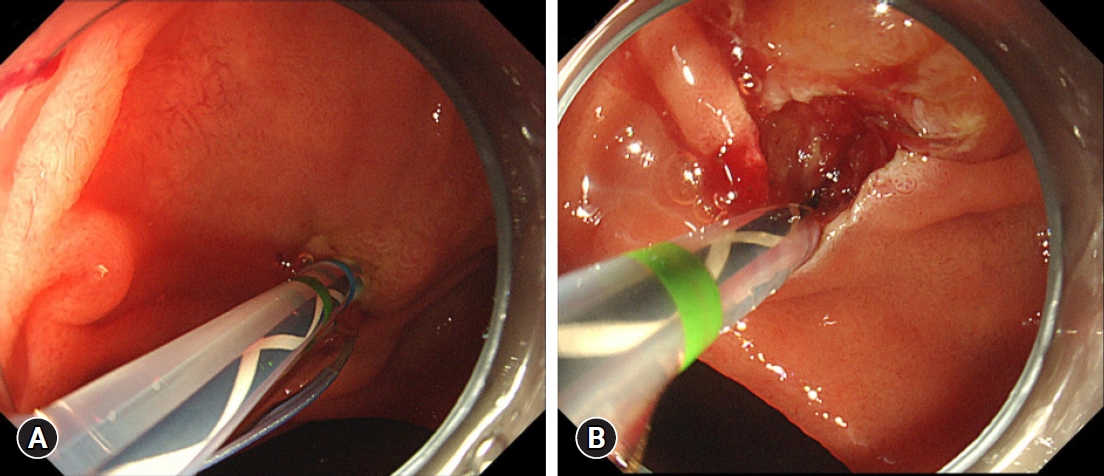
In cases where selective biliary cannulation is difficult, cannulation using the pancreatic duct, such as the ŌĆ£double-guidewire methodŌĆØ28 may be useful, as this is similar to ERCP in normal anatomy (Fig. 5). Besides the double-guidewire method, pancreatic duct stent-assisted biliary cannulation,29 or cannulation using the double-lumen cannula30 can also be helpful. As selective biliary cannulation in patients with SAA (especially, those with a native papilla) tends to be difficult, many attempts may be required and the longer time involved could cause post-ERCP pancreatitis. Hence, for safety, it is important to abort the procedure after a certain time has lapsed. Rather than prolonging the time, reattempting the cannulation on another day is preferred. Alternatively, the rendezvous technique or direct drainage using an alternative method, such as PTBD or endoscopic ultrasound-guided biliary drainage (EUS-BD), should be considered, depending on the patientŌĆÖs condition and the procedural details.
Selective biliary cannulation in patients with papilla diversion, such as hepaticojejunal anastomosis (e.g., in patients with hepaticojejunostomy, Roux-en-Y, or pancreaticoduodenectomy) is generally easy as long as the orifice of the hepaticojejunal anastomosis is found. Cannulation failure mostly occurs when the anastomotic site is not reached or found. In cases where the scope has reached the intended location, but the site is difficult to identify, the scar around the orifice can help identify the anastomotic site. Recently, a texture and color enhancement imaging (TXI)-equipped new-generation endoscopy system (EVIS X1; Olympus Marketing)31 has been developed, which facilitates the identification of such orifices.32
TECHNICAL TIPS FOR SUBSEQUENT PROCEDURES
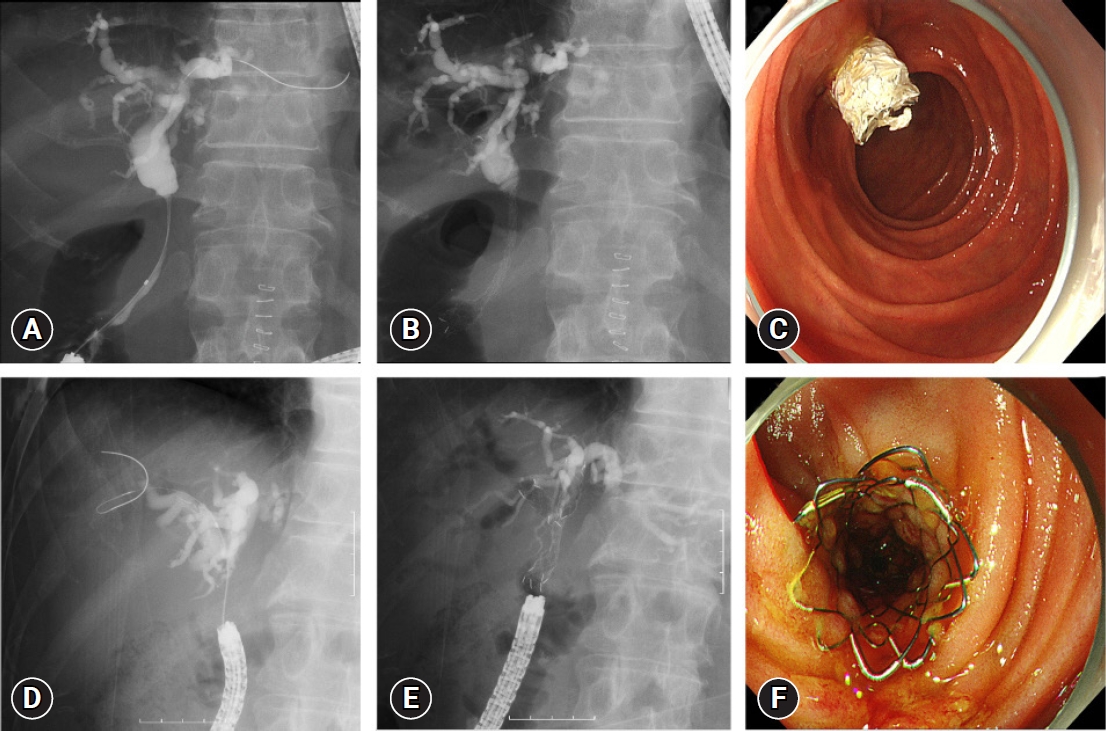
After reaching the target site and successful cannulation, the subsequent procedures, such as stone extraction and SEMS placement, can also be challenging. Before performing these procedures, EST, endoscopic papillary balloon dilation, or endoscopic papillary large balloon dilation (EPLBD) is required. Particularly, EST is especially difficult because the cutting direction is usually either opposite to that of standard sphincterotomy or more tangential to that direction. Moreover, there are not many dedicated devices for making a correct incision to the direction of the bile duct safely. Previously, we performed EST using a needle knife after placing a plastic stent in the bile duct to facilitate a safe cutting-direction. The incision is made while exposing the stent and checking that the incision is in the correct direction. Since 2022, we have been performing EST in patients with SAA using a new dedicated sphincterotome (CleverCut3V; KD-V410V-0720; Olympus Marketing).33 The blade of this sphincterotome can be easily adjusted towards the 5 oŌĆÖclock direction, which indicates the bile duct direction in patients with SAA (Fig. 6).
When performing stone extraction, it is important to loosen the orifice of the papilla as much as possible by performing EST, and/or EPLBD. The main way to control the force for stone extraction in patients with SAA is by withdrawing the scope. However, it is difficult to control the force and intestinal perforation may occur after the scope passes through the papilla if the papilla is not loosened. Therefore, it is highly recommended that the papilla be loosened. Several studies have evaluated the factors affecting complete stone extraction, including the failure to form the retroflex position and a common bile duct diameter of Ōēź14 mm.34 A larger bile duct diameter (mean, 15.9 mm) has been associated with unsuccessful stone extraction.13 As the SBE has no elevator functions, it is difficult to control the basket catheter in cases with large bile ducts and capturing the stones is also challenging. More dedicated devices for stone extraction in patients with SAA are warranted. When it seems difficult to complete stone extraction via SBE-assisted ERCP, a combination of stone extraction methods, such as adding the EUS-BD route, may be a good alternative.35,36
As the short SBE has a working channel diameter of 3.2 mm, it makes possible to place various SEMS in patients with SAA.34 Almost all SEMSs used in patients with normal anatomy can also be used for patients with SAA. However, some SEMSs have a length of approximately 180 cm, so it is impossible to place them into the hilar part across the stricture, especially in patients with a papilla and a common bile duct. On the other hand, SEMSs with a working length of 180 cm can be placed into the hilar part in patients with hepaticojejunal anastomosis (hepaticojejunostomy with Roux-en-Y or pancreaticoduodenectomy) whose common bile duct has been resected. Therefore, a SEMS with enough length to access the intended area is important. This is dependent on the anatomy when performing ERCP in patients with SAA using a short SBE. We usually place a covered SEMS in patients with distal malignant biliary obstruction across the papilla after performing an EST and an uncovered SEMS in patients with hilar malignant biliary obstruction (Fig. 7). The clinical success and recurrent biliary obstruction rates in patients with SAA were similar to those in normal anatomy using SEMS.37,38 In recurrent biliary obstruction, the papilla or hepaticojejunal anastomosis is located in the deep afferent limb, thus, it is assumed that food impaction rarely occurs in patients with SAA compared to normal anatomy.37 However, afferent limb obstruction may cause recurrent biliary obstruction while the stent is still patent.
FACTORS AFFECTING PROCEDURE RESULTS
It is important to be aware of factors that may lead to incomplete SBE-assisted ERCP procedures. Several reports have evaluated these factors.16-18 In particular, Roux-en-Y reconstruction, malignant biliary obstruction, and pancreatic indications were identified.
Appropriate responses to such difficult situations is paramount. First, in cases of Roux-en-Y, the difficulty associated with scope insertion increases the failure risk. In patients with Roux-en-Y gastric bypass and hepaticojejunostomy with Roux-en-Y, the longer Roux limbs contribute to the difficulty. In such cases, conventional SBE with a working length of 200 cm is useful. We use the 200 cm scope when scope insertion using the short SBE failed. A previous study of 27 patients with scope insertion failure using short SBE reported that 24 (88.9%) succeeded with a conventional SBE.18 Second, malignant biliary obstruction cases tend to cause strong adhesion due to cancer, so scope manipulation is difficult and procedural failure is possible. Moreover, small intestine or papilla invasion due to the cancer may further complicate the procedure. In such cases, it is difficult to complete the intended procedure by SBE-assisted ERCP. PTBD or EUS-BD could be good alternatives. Third, pancreatic indications, especially when approaching the pancreaticojejunal anastomosis, are difficult as a pancreatico-jejunal anastomosis is located deeper than a hepaticojejunal anastomosis in the afferent limb, thus, more difficult to find, especially in instances of complete obstruction. The technical success rate in these cases is approximately 70%.39 As mentioned above, the TXI-equipped new-generation endoscopy system can facilitate the identification of such orifices.32 Furthermore, the EUS-guided pancreatic duct approach should be considered, although this procedure is more difficult and may cause more severe adverse events, compared to EUS-BD procedures.
CONCLUSIONS
In the present review, we discussed the technical tips of SBE-assisted ERCP in terms of scope insertion, selective biliary cannulation, and subsequent procedures and highlighted points for the prevention of adverse events. The study also reported on the factors that affect procedural success and the strategies for solving these difficulties. The review aimed to inform endoscopists who are performing SBE-assisted ERCP. Recently, EUS-BD has been reported as another alternative with a shorter procedure duration. However, due to the limited accessory choices, EUS-BD may cause severe adverse events, such as bile leak or stent migration into the abdominal cavity, even when performed by experienced endoscopists. In contrast, DBE- and SBE-assisted ERCPs are more predictable and safer because ERCP is a well-established procedure and many dedicated accessories are available. Furthermore, when choosing between SBE-assisted ERCP or EUS-BD, the postoperative reconstruction, patient condition, and more importantly, the endoscopistŌĆÖs experience should be considered.