Search
- Page Path
- HOME > Search
- Drainage for fluid collections post pancreatic surgery and acute pancreatitis: similar but different?
- Yousuke Nakai, Saburo Matsubara, Tsuyoshi Mukai, Tsuyoshi Hamada, Takashi Sasaki, Hirotoshi Ishiwatari, Susumu Hijioka, Hideyuki Shiomi, Mamoru Takenaka, Takuji Iwashita, Atsuhiro Masuda, Tomotaka Saito, Hiroyuki Isayama, Ichiro Yasuda, for the WONDERFUL study group in Japan
- Received October 3, 2023 Accepted November 1, 2023 Published online May 17, 2024
- DOI: https://doi.org/10.5946/ce.2023.254 [Epub ahead of print]
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
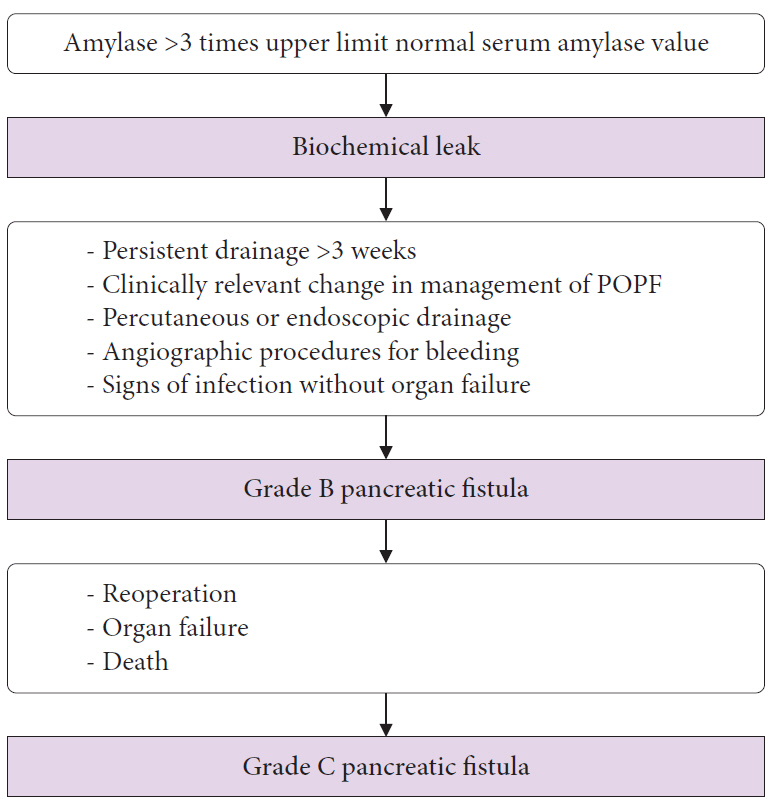
ePub - Postoperative pancreatic fistulas (POPFs) are common adverse events that occur after pancreatic surgery. Endoscopic ultrasonography (EUS)-guided drainage (EUS-D) is a first-line treatment, similar to that for pancreatic fluid collection (PFCs) after acute pancreatitis. However, some POPFs do not develop fluid collections depending on the presence or location of the surgical drain, whereas others develop fluid collections, such as postoperative fluid collections (POPFCs). Although POPFCs are similar to PFCs, the strategy and modality for POPF management need to be modified according to the presence of fluid collections, surgical drains, and surgical type. As discussed for PFCs, the indications, timing, and selection of interventions or stents for EUS-D have not been fully elucidated for POPFs. In this review, we discuss the management of POPFs and POPFCs in comparison with PFCs due to acute pancreatitis and summarize the topics that should be addressed in future studies.
- 1,934 View
- 72 Download

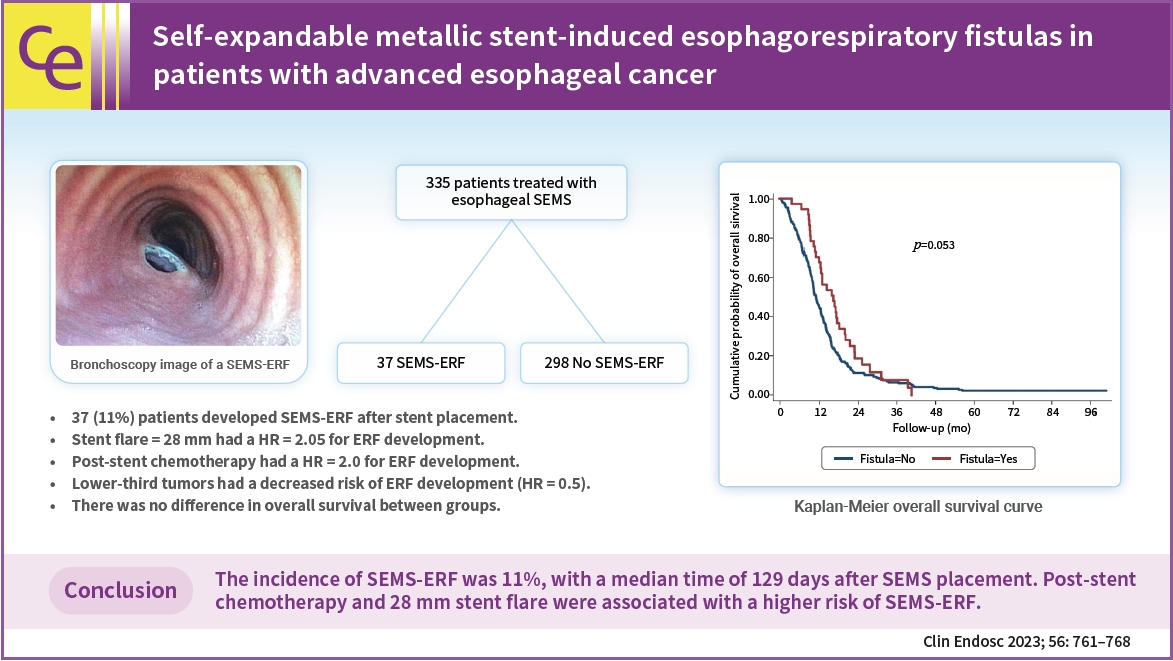
- Self-expandable metallic stent-induced esophagorespiratory fistulas in patients with advanced esophageal cancer
- Iatagan R. Josino, Bruno C. Martins, Andressa A. Machado, Gustavo R. de A. Lima, Martin A. C. Cordero, Amanda A. M. Pombo, Rubens A. A. Sallum, Ulysses Ribeiro Jr, Todd H. Baron, Fauze Maluf-Filho
- Clin Endosc 2023;56(6):761-768. Published online July 25, 2023
- DOI: https://doi.org/10.5946/ce.2022.297
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 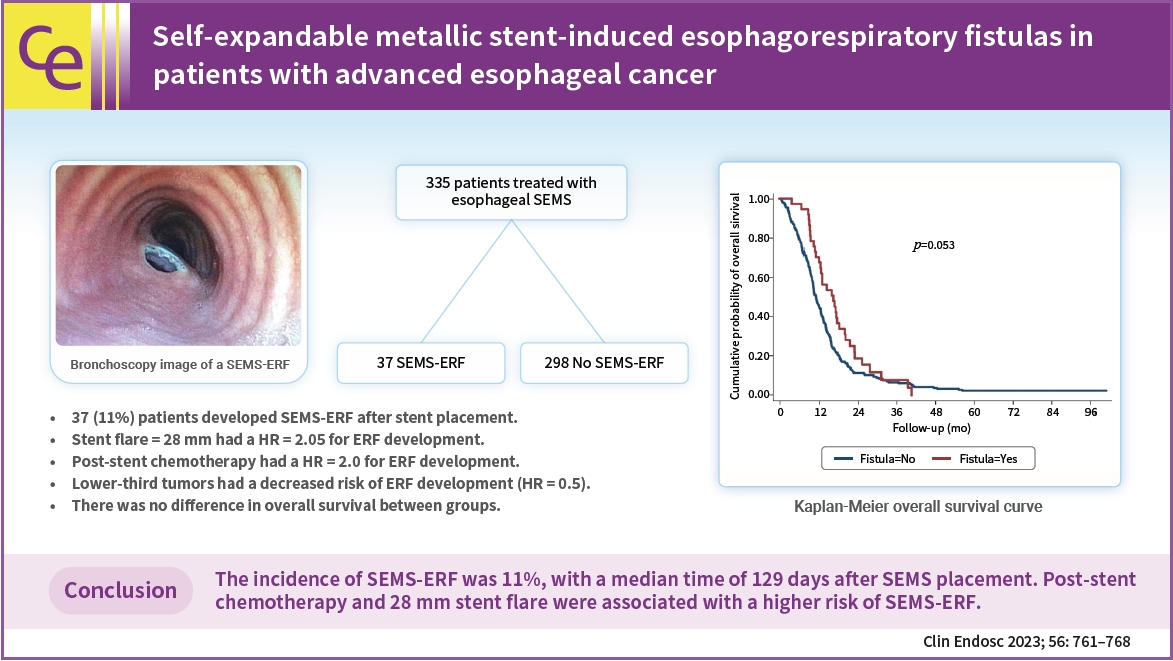
- Background
/Aims: Self-expandable metallic stents (SEMSs) are widely adopted for the palliation of dysphagia in patients with malignant esophageal strictures. An important adverse event is the development of SEMS-induced esophagorespiratory fistulas (SEMS-ERFs). This study aimed to assess the risk factors related to the development of SEMS-ERF after SEMS placement in patients with esophageal cancer.
Methods
This retrospective study was performed at the Instituto do Cancer do Estado de São Paulo. All patients with malignant esophageal strictures who underwent esophageal SEMS placement between 2009 and 2019 were included in the study.
Results
Of the 335 patients, 37 (11.0%) developed SEMS-ERF, with a median time of 129 days after SEMS placement. Stent flare of 28 mm (hazard ratio [HR], 2.05; 95% confidence interval [CI], 1.15–5.51; p=0.02) and post-stent chemotherapy (HR, 2.0; 95% CI, 1.01–4.00; p=0.05) were associated with an increased risk of developing SEMS-ERF, while lower-third tumors were a protective factor (HR, 0.5; 95% CI, 0.26–0.85; p=0.01). No difference was observed in overall survival.
Conclusions
The incidence of SEMS-ERFs was 11%, with a median time of 129 days after SEMS placement. Post-stent chemotherapy and a 28 mm stent flare were associated with a higher risk of SEMS-ERF. -
Citations
Citations to this article as recorded by- How to reduce fistula formation after self-expandable metallic stent insertion for treating malignant esophageal stricture?
Kwang Bum Cho
Clinical Endoscopy.2023; 56(6): 735. CrossRef
- How to reduce fistula formation after self-expandable metallic stent insertion for treating malignant esophageal stricture?
- 2,006 View
- 107 Download
- 1 Web of Science
- 1 Crossref

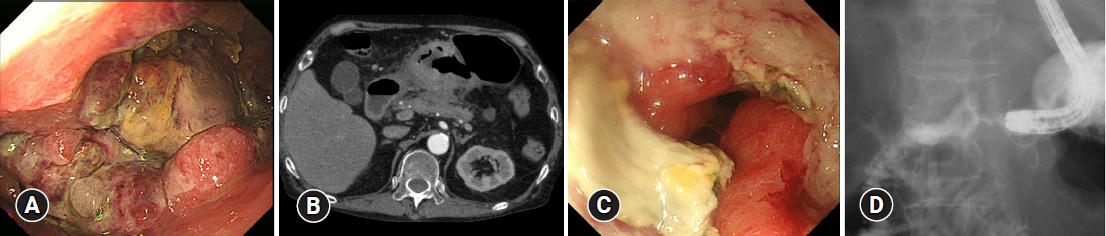
- Gastric cancer presenting with ramucirumab-related gastrocolic fistula successfully managed by colonic stenting: a case report
- Hiroki Fukuya, Yoichiro Iboshi, Masafumi Wada, Yorinobu Sumida, Naohiko Harada, Makoto Nakamuta, Hiroyuki Fujii, Eikichi Ihara
- Clin Endosc 2023;56(6):812-816. Published online May 11, 2023
- DOI: https://doi.org/10.5946/ce.2022.117
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - We report a rare case of gastric cancer presenting with a gastrocolic fistula during ramucirumab and paclitaxel combination therapy that was successfully managed with colonic stenting. A 75-year-old man was admitted to our hospital with the chief complaint of melena. Esophagogastroduodenoscopy revealed a large ulcerated tumor in the lower stomach, judged by laparoscopy as unresectable (sT4bN1M0). After four cycles of first-line chemotherapy with S-1 plus oxaliplatin, the patient showed disease progression, and second-line therapy with ramucirumab and paclitaxel was started. At the end of the third cycle, the patient had gastric antral stenosis, which necessitated the placement of a gastroduodenal stent. When the patient complained of diarrhea 10 days later, esophagogastroduodenoscopy revealed a fistula between the greater curvature of the stomach and the transverse colon. The fistula was covered by double colonic stenting, with a covered metal stent placed within an uncovered metal stent, after which leakage from the stomach to the colon stopped.
-
Citations
Citations to this article as recorded by- Ramucirumab
Reactions Weekly.2024; 1989(1): 189. CrossRef - Metastatic bladder cancer forming a sigmoidorectal fistula after enfortumab vedotin therapy: a case report
Shinji Tamada, Daiki Ikarashi, Naoki Yanagawa, Moe Toyoshima, Kenta Takahashi, Tomohiko Matsuura, Shigekatsu Maekawa, Renpei Kato, Mitsugu Kanehira, Ryo Takata, Wataru Obara
Frontiers in Oncology.2023;[Epub] CrossRef
- Ramucirumab
- 1,804 View
- 140 Download
- 1 Web of Science
- 2 Crossref

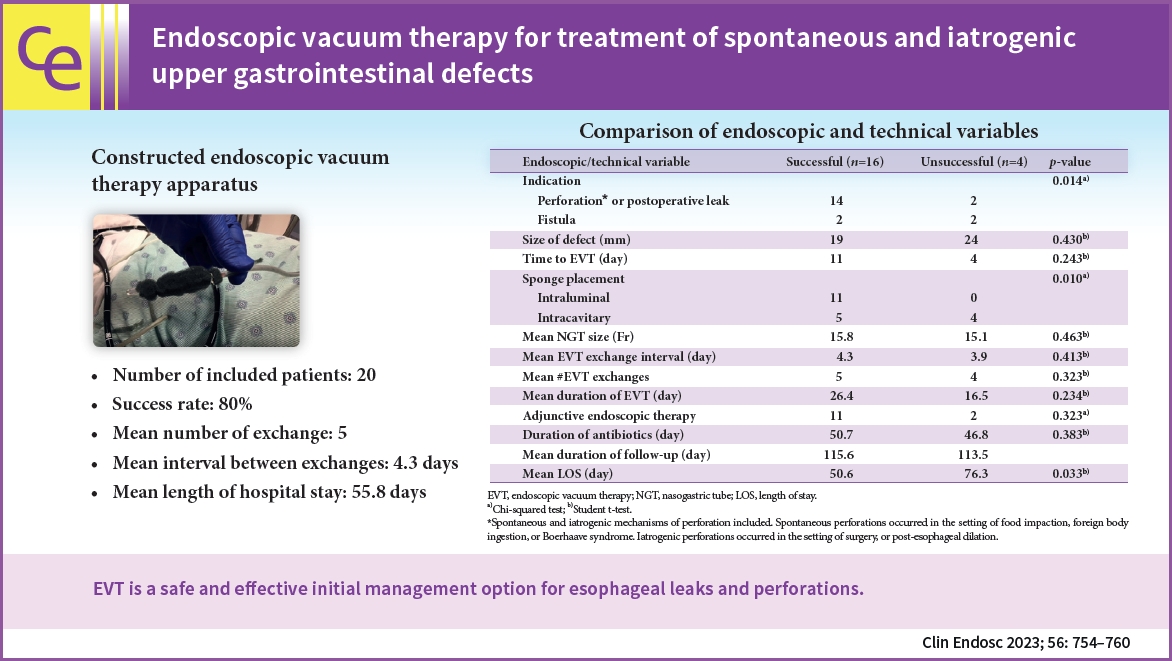
- Endoscopic vacuum therapy for treatment of spontaneous and iatrogenic upper gastrointestinal defects
- Kavea Panneerselvam, Jake S. Jacob, Ronald E. Samuel, Andy Tau, Gyanprakash A. Ketwaroo, Wasif M. Abidi, Robert J. Sealock
- Clin Endosc 2023;56(6):754-760. Published online May 9, 2023
- DOI: https://doi.org/10.5946/ce.2022.177
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 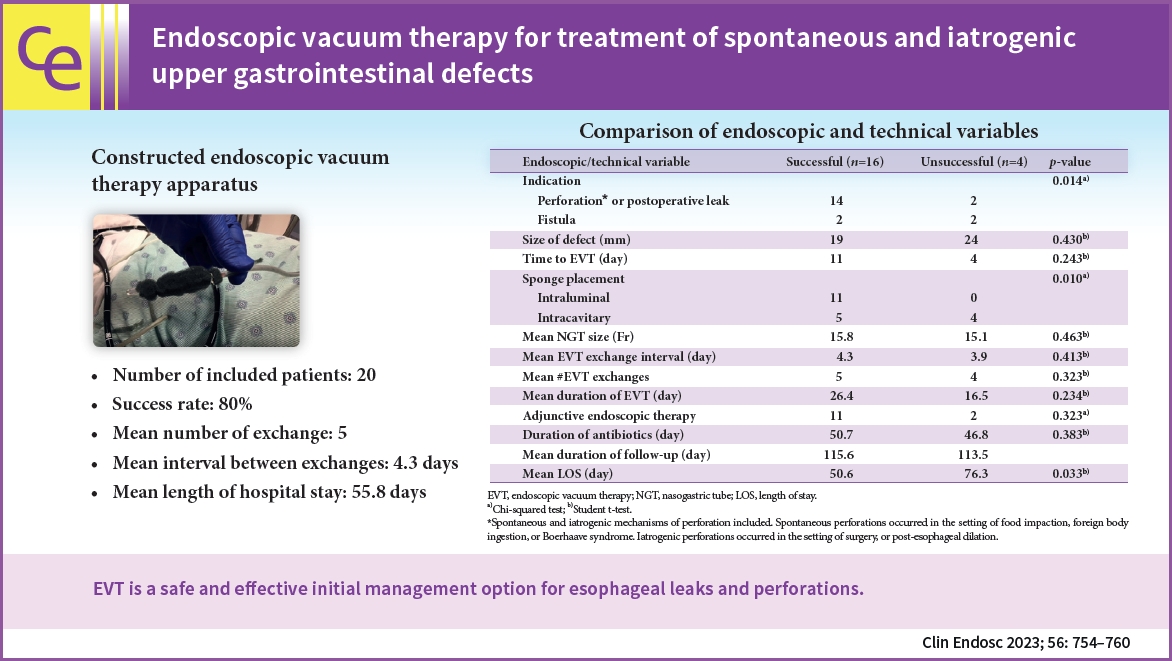
- Background
/Aims: Endoscopic vacuum therapy (EVT) can heal a variety of defects within the gastrointestinal (GI) tract via applying negative pressure, which reduces the defect size, aspirates the infected fluid, and promotes granulation tissue. Here we present our experience with EVT as it relates to both spontaneous and iatrogenic upper GI tract perforations, leaks, and fistulas.
Methods
This retrospective study was conducted at four large hospital centers. All patients who underwent EVT between June 2018 and March 2021 were included. Data on multiple variables were collected, including demographics, defect size and location, number and intervals of EVT exchanges, technical success, and hospital length of stay. Student t-test and the chi-squared test were used to analyze the data.
Results
Twenty patients underwent EVT. The most common defect cause was spontaneous esophageal perforation (50%). The most common defect location was the distal esophagus (55%). The success rate was 80%. Seven patients were treated with EVT as the primary closure method. The mean number of exchanges was five with a mean interval of 4.3 days between exchanges. The mean length of hospital stay was 55.8 days.
Conclusions
EVT is a safe and effective initial management option for esophageal leaks and perforations. -
Citations
Citations to this article as recorded by- Endoscopic vacuum therapy: management of upper gastrointestinal anastomotic leaks and esophageal perforations
María de Armas Conde, Carmen Díaz-López , Vanessa Concepción-Martín, María Del Pilar Borque-Barrera
Revista Española de Enfermedades Digestivas.2024;[Epub] CrossRef - Management of fistulas in the upper gastrointestinal tract
Maria Valeria Matteo, Maria Mihaela Birligea, Vincenzo Bove, Valerio Pontecorvi, Martina De Siena, Loredana Gualtieri, Federico Barbaro, Cristiano Spada, Ivo Boškoski
Best Practice & Research Clinical Gastroenterology.2024; : 101929. CrossRef - Endoscopic Vacuum Therapy of Upper Gastrointestinal Anastomotic Leaks: How to Deal with the Challenges (with Video)
Laurent Monino, Tom G. Moreels
Life.2023; 13(6): 1412. CrossRef
- Endoscopic vacuum therapy: management of upper gastrointestinal anastomotic leaks and esophageal perforations
- 2,061 View
- 132 Download
- 1 Web of Science
- 3 Crossref

- Portal cavernography during endoscopic retrograde cholangiopancreatography: from bilhemia to hemobilia
- Rawad A. Yared, Paraskevas Gkolfakis, Arnaud Lemmers, Vincent Huberty, Thierry Degrez, Jacques Devière, Daniel Blero
- Clin Endosc 2023;56(4):521-526. Published online January 5, 2023
- DOI: https://doi.org/10.5946/ce.2021.276
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Portobiliary fistulas are rare but may lead to life-threatening complications. Biliary plastic stent-induced portobiliary fistulas during endoscopic retrograde cholangiopancreatography have been described. Herein, we present a case of portal cavernography and recurrent hemobilia after endoscopic retrograde cholangiopancreatography in which a portobiliary fistula was detected in a patient with portal biliopathy. This likely indicates a change in clinical presentation (from bilhemia to hemobilia) after biliary drainage that was successfully treated by placement of a fully covered, self-expandable metallic stent.
- 1,456 View
- 119 Download

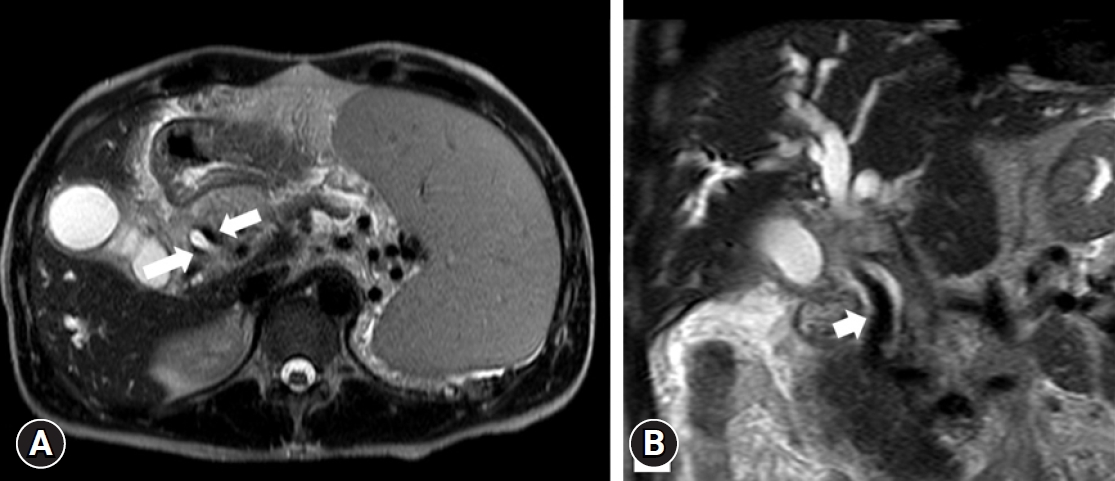
- Bronchoesophageal fistula in a patient with Crohn’s disease receiving anti-tumor necrosis factor therapy
- Kyunghwan Oh, Kee Don Choi, Hyeong Ryul Kim, Tae Sun Shim, Byong Duk Ye, Suk-Kyun Yang, Sang Hyoung Park
- Clin Endosc 2023;56(2):239-244. Published online December 21, 2021
- DOI: https://doi.org/10.5946/ce.2021.215
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Tuberculosis is an adverse event in patients with Crohn’s disease receiving anti-tumor necrosis factor (TNF) therapy. However, tuberculosis presenting as a bronchoesophageal fistula (BEF) is rare. We report a case of tuberculosis and BEF in a patient with Crohn’s disease who received anti-TNF therapy. A 33-year-old Korean woman developed fever and cough 2 months after initiation of anti-TNF therapy. And the symptoms persisted for 1 months, so she visited the emergency room. Chest computed tomography was performed upon visiting the emergency room, which showed BEF with aspiration pneumonia. Esophagogastroduodenoscopy with biopsy and endobronchial ultrasound with transbronchial needle aspiration confirmed that the cause of BEF was tuberculosis. Anti-tuberculosis medications were administered, and esophageal stent insertion through endoscopy was performed to manage the BEF. However, the patient’s condition did not improve; therefore, fistulectomy with primary closure was performed. After fistulectomy, the anastomosis site healing was delayed due to severe inflammation, a second esophageal stent and gastrostomy tube were inserted. Nine months after the diagnosis, the fistula disappeared without recurrence, and the esophageal stent and gastrostomy tube were removed.
-
Citations
Citations to this article as recorded by- (Re-)introduction of TNF antagonists and JAK inhibitors in patients with previous tuberculosis: a systematic review
Thomas Theo Brehm, Maja Reimann, Niklas Köhler, Christoph Lange
Clinical Microbiology and Infection.2024;[Epub] CrossRef - Azathioprine/infliximab/methylprednisolone
Reactions Weekly.2023; 1963(1): 114. CrossRef
- (Re-)introduction of TNF antagonists and JAK inhibitors in patients with previous tuberculosis: a systematic review
- 3,740 View
- 272 Download
- 2 Crossref

- Over-the-Scope Clip in the Treatment of Gastrointestinal Leaks and Perforations
- Mike T. Wei, Ji Yong Ahn, Shai Friedland
- Clin Endosc 2021;54(6):798-804. Published online November 30, 2021
- DOI: https://doi.org/10.5946/ce.2021.250
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - While perforations, postoperative fistulas, and leaks have traditionally led to surgical or interventional radiology consultation for management, the introduction of the over-the-scope clip has allowed increased therapeutic possibilities for endoscopists. While primarily limited to case reports and series, the over-the-scope clip successfully manages gastrointestinal bleeding, perforations, as well as postoperative leaks and fistulas. Retrospective studies have demonstrated a relatively high success rate and a low complication rate. Given the similarity to variceal banding equipment, the learning curve with the over-the-scope clip is rapid. However, given the higher risk of procedures involving the use of the over-the-scope clip, it is essential to obtain the scope in a stable position and grasp sufficient tissue with the cap using a grasping tool and/or suction. From our experience, while closure may be successful in lesions sized up to 3 cm, successful outcomes are obtained for lesions sized <1 cm. Ultimately, given the limited available data, prospective randomized trials are needed to better evaluate the utility of the over-the-scope clip in various clinical scenarios, including fistula and perforation management.
-
Citations
Citations to this article as recorded by- A Multicenter Survey of Percutaneous Endoscopic Gastrostomy in 2019 at Korean Medical Institutions
Jun Woo Park, Tae Gyun Kim, Kwang Bum Cho, Jeong Seok Kim, Jin Woong Cho, Jung Won Jeon, Sun Gyo Lim, Chan Gyoo Kim, Hong Jun Park, Tae Jun Kim, Eun Sun Kim, Su Jin Jeong, Yong Hwan Kwon
Gut and Liver.2024; 18(1): 77. CrossRef - Clinical Practice Guideline for Percutaneous Endoscopic Gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
Gut and Liver.2024; 18(1): 10. CrossRef - Use of anchor pronged clips to close complex polyp resection defects
Mike Tzuhen Wei, Shai Friedland
VideoGIE.2023; 8(6): 245. CrossRef - Novel endoscopic management of gastroenterological anastomosis leakage by injecting gel-forming solutions: an experimental animal study
Yusuke Watanabe, Keiko Yamamoto, Zijian Yang, Haruna Tsuchibora, Masakazu Fujii, Masayoshi Ono, Shoko Ono, Takayuki Kurokawa, Naoya Sakamoto
Surgical Endoscopy.2023; 37(10): 8029. CrossRef - Clinical practice guidelines for percutaneous endoscopic gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
Clinical Endoscopy.2023; 56(4): 391. CrossRef - Management of complications related to colorectal endoscopic submucosal dissection
Tae-Geun Gweon, Dong-Hoon Yang
Clinical Endoscopy.2023; 56(4): 423. CrossRef - Gastroesophageal Reflux Disease in Obesity: Bariatric Surgery as Both the Cause and the Cure in the Morbidly Obese Population
Muaaz Masood, Donald Low, Shanley B. Deal, Richard A. Kozarek
Journal of Clinical Medicine.2023; 12(17): 5543. CrossRef - Clinical Practice Guideline for Percutaneous Endoscopic Gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
The Korean Journal of Gastroenterology.2023; 82(3): 107. CrossRef - Endoscopic Management of Esophageal Cancer
Christopher Paiji, Alireza Sedarat
Cancers.2022; 14(15): 3583. CrossRef - Use of a novel dual-action clip for closure of complex endoscopic resection defects
Mike Tzuhen Wei, Shai Friedland
VideoGIE.2022; 7(11): 389. CrossRef
- A Multicenter Survey of Percutaneous Endoscopic Gastrostomy in 2019 at Korean Medical Institutions
- 3,632 View
- 120 Download
- 8 Web of Science
- 10 Crossref

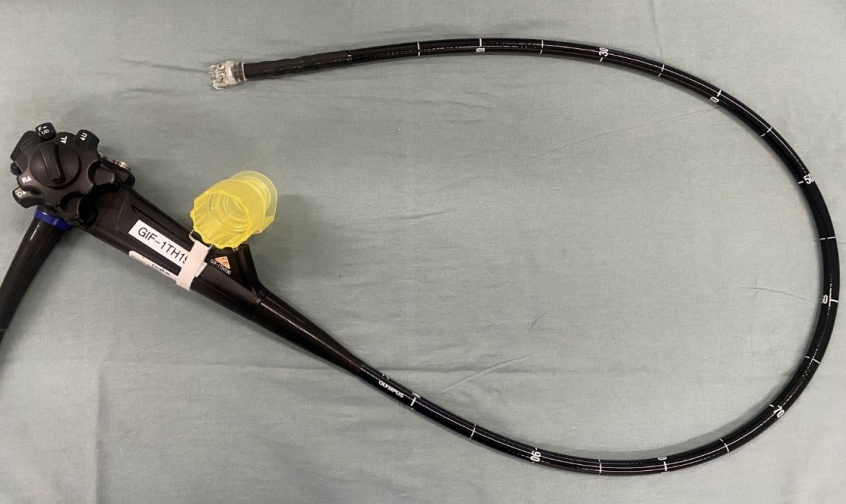
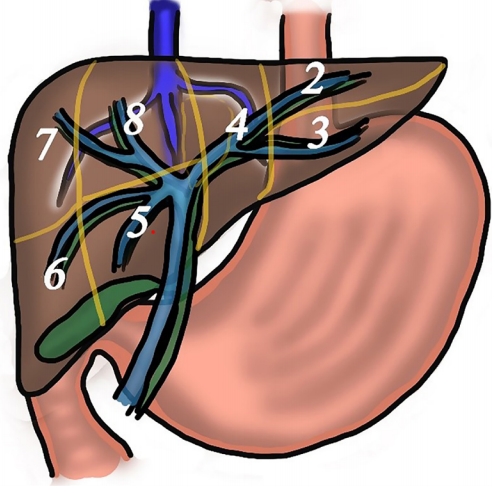
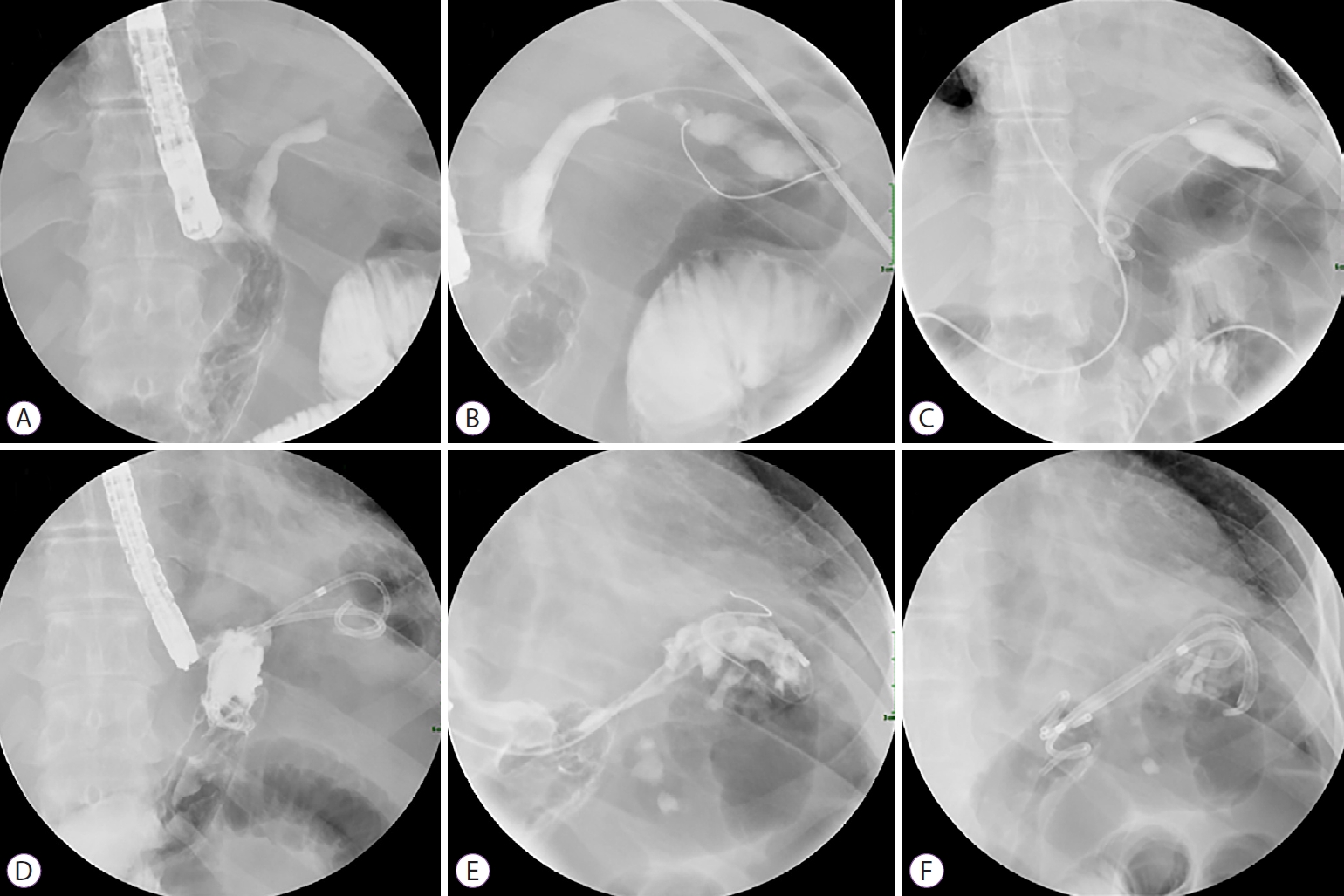
- What You Need to Know Before Performing Endoscopic Ultrasound-guided Hepaticogastrostomy
- Tanyaporn Chantarojanasiri, Thawee Ratanachu-Ek, Nonthalee Pausawasdi
- Clin Endosc 2021;54(3):301-308. Published online May 28, 2021
- DOI: https://doi.org/10.5946/ce.2021.103
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) is the primary treatment modality for bile duct obstruction. When ERCP is unsuccessful, percutaneous transhepatic biliary drainage can be an alternative method. Endoscopic ultrasound-guided biliary drainage (EUS-BD) has emerged as a treatment option for biliary obstruction, especially after ERCP failure. EUS-BD offers transluminal intrahepatic and extrahepatic drainage through a transgastric and transduodenal approach. EUS-guided hepaticogastrostomy (EUS-HGS) is an excellent choice for patients with hilar strictures or those with a surgically altered anatomy. The optimal steps in EUS-HGS are case selection, bile duct visualization, puncture-site selection, wire insertion and manipulation, tract dilation, and stent placement. Caution should be taken at each step to prevent complications. Dedicated devices for EUS-HGS have been developed to improve the technical success rate and reduce complications. This technical review focuses on the essential practical points at each step of EUS-HGS.
-
Citations
Citations to this article as recorded by- Use of a novel screw-type dilator for endoscopic ultrasonography-guided hepaticogastrostomy via 22-gauge needle and 0.018-inch guidewire.
Shin Kato, Mariko Tsukamoto, Taichi Murai, Yuta Koike
Revista Española de Enfermedades Digestivas.2024;[Epub] CrossRef - Transbulbäre und transgastrale Gallengangsdrainage
Philipp Thies, Markus Dollhopf
Gastroenterologie up2date.2024; 20(01): 69. CrossRef - Safety of endoscopic ultrasound-guided hepaticogastrostomy in patients with malignant biliary obstruction and ascites
Tsukasa Yasuda, Kazuo Hara, Nobumasa Mizuno, Shin Haba, Takamichi Kuwahara, Nozomi Okuno, Yasuhiro Kuraishi, Takafumi Yanaidani, Sho Ishikawa, Masanori Yamada, Toshitaka Fukui
Clinical Endoscopy.2024; 57(2): 246. CrossRef - Risk factors for recurrent stenosis after balloon dilation for benign hepaticojejunostomy anastomotic stricture
Takafumi Mie, Takashi Sasaki, Takeshi Okamoto, Tsuyoshi Takeda, Chinatsu Mori, Yuto Yamada, Takaaki Furukawa, Akiyoshi Kasuga, Masato Matsuyama, Masato Ozaka, Naoki Sasahira
Clinical Endoscopy.2024; 57(2): 253. CrossRef - Endoscopic ultrasound-guided intervention for inaccessible papilla in advanced malignant hilar biliary obstruction
Partha Pal, Sundeep Lakhtakia
Clinical Endoscopy.2023; 56(2): 143. CrossRef - Liver impaction technique improves technical success rate of guidewire insertion during EUS-guided hepaticogastrostomy (with video)
Junichi Nakamura, Takeshi Ogura, Saori Ueno, Atsushi Okuda, Nobu Nishioka, Yuki Uba, Mitsuki Tomita, Kimi Bessho, Nobuhiro Hattori, Hiroki Nishikawa
Therapeutic Advances in Gastroenterology.2023;[Epub] CrossRef - Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review
Roy L. J. van Wanrooij, Michiel Bronswijk, Rastislav Kunda, Simon M. Everett, Sundeep Lakhtakia, Mihai Rimbas, Tomas Hucl, Abdenor Badaoui, Ryan Law, Paolo Giorgio Arcidiacono, Alberto Larghi, Marc Giovannini, Mouen A. Khashab, Kenneth F. Binmoeller, Marc
Endoscopy.2022; 54(03): 310. CrossRef - Practical Tips for Safe and Successful Endoscopic Ultrasound-Guided Hepaticogastrostomy: A State-of-the-Art Technical Review
Saburo Matsubara, Keito Nakagawa, Kentaro Suda, Takeshi Otsuka, Masashi Oka, Sumiko Nagoshi
Journal of Clinical Medicine.2022; 11(6): 1591. CrossRef - Prevention of Serious Complications during Endoscopic Ultrasound-Guided Biliary Drainage: A Case-Based Technical Review
Surinder Singh Rana, Jimil Shah, Harish Bhujade, Ujjwal Gorsi, Mandeep Kang, Rajesh Gupta
Journal of Digestive Endoscopy.2022; 13(02): 082. CrossRef
- Use of a novel screw-type dilator for endoscopic ultrasonography-guided hepaticogastrostomy via 22-gauge needle and 0.018-inch guidewire.
- 5,157 View
- 214 Download
- 7 Web of Science
- 9 Crossref

- Endoscopic hemostasis using an over-the-scope clip for massive bleeding after percutaneous endoscopic gastrostomy removal: a case report
- Sun Young Moon, Min Kyu Jung, Jun Heo
- Clin Endosc 2022;55(3):443-446. Published online May 25, 2021
- DOI: https://doi.org/10.5946/ce.2020.294

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Percutaneous endoscopic gastrostomy (PEG) is a common method for providing long-term enteral nutrition to patients. PEG tube placement and removal are relatively safe; generally, a PEG tube can be removed using gentle traction, and excessive bleeding is rare. The over-the-scope clip system is a new device that can be used for gastrointestinal hemostasis and for closing gastrointestinal fistulae. In the present case, a 68-year-old male patient had to remove the PEG tube because of persistent leakage around the PEG tube. Although it was gently removed using traction, incessant bleeding continued, with a Rockall score of 5 points, even after hemocoagulation was attempted. An over-the-scope clip device was used to achieve hemostasis and fistula closure.
-
Citations
Citations to this article as recorded by- Clinical Practice Guideline for Percutaneous Endoscopic Gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
Gut and Liver.2024; 18(1): 10. CrossRef - Clinical practice guidelines for percutaneous endoscopic gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
Clinical Endoscopy.2023; 56(4): 391. CrossRef - Clinical Practice Guideline for Percutaneous Endoscopic Gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
The Korean Journal of Gastroenterology.2023; 82(3): 107. CrossRef
- Clinical Practice Guideline for Percutaneous Endoscopic Gastrostomy
- 3,060 View
- 149 Download
- 3 Web of Science
- 3 Crossref

- A Gastrobronchial Fistula Secondary to Endoscopic Internal Drainage of a Post-Sleeve Gastrectomy Fluid Collection
- Paraskevas Gkolfakis, Marc-André Bureau, Marianna Arvanitakis, Jacques Devière, Daniel Blero
- Clin Endosc 2022;55(1):141-145. Published online April 16, 2021
- DOI: https://doi.org/10.5946/ce.2021.033
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - A 44-year-old woman underwent sleeve gastrectomy, which was complicated by a leak. She was treated with two sessions of endoscopic internal drainage using plastic double-pigtail stents. Her clinical evolution was favorable, but four months after the initial stent placement, she became symptomatic, and a gastrobronchial fistula with the proximal end of the stents invading the diaphragm was diagnosed. She was treated with antibiotics, plastic stents were removed, and a partially covered metallic esophageal stent was placed. Eleven weeks later, the esophageal stent was removed with no evidence of fistula. Inappropriate stent size, position, stenting duration, and persistence of low-grade inflammation could explain the patient’s symptoms and provide a mechanism for gradual muscle rupture and fistula formation. Although endoscopic internal drainage is usually safe and effective for the management of post-laparoscopic sleeve gastrectomy leaks, close clinical and radiological follow-up is mandatory.
-
Citations
Citations to this article as recorded by- Management of Leakage and Fistulas after Bariatric Surgery
Stephen A. Firkins, Roberto Simons-Linares
Best Practice & Research Clinical Gastroenterology.2024; : 101926. CrossRef - Role of Endoscopic Internal Drainage in Treating Gastro-Bronchial and Gastro-Colic Fistula After Sleeve Gastrectomy
Alessandra D’Alessandro, Giovanni Galasso, Francesco Paolo Zito, Cristiano Giardiello, Fabrizio Cereatti, Roberto Arienzo, Filippo Pacini, Jean-Marc Chevallier, Gianfranco Donatelli
Obesity Surgery.2022; 32(2): 342. CrossRef
- Management of Leakage and Fistulas after Bariatric Surgery
- 3,664 View
- 144 Download
- 2 Crossref

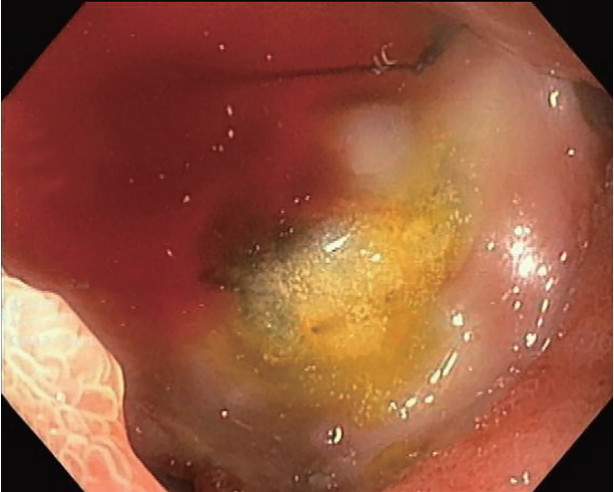
- Endoscopic Ultrasound-Guided Vascular Therapy for Portoduodenal Fistula
- Tanyaporn Chantarojanasiri, Apichet Sirinawasatien, Chalermrat Bunchorntavakul, Aroon Siripun, Sa-ard Treepongkaruna, Thawee Ratanachu-ek
- Clin Endosc 2020;53(6):750-753. Published online February 13, 2020
- DOI: https://doi.org/10.5946/ce.2019.167
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Portoenteric fistula is a rare cause of massive upper gastrointestinal bleeding. Most cases can be treated with radiointervention or surgery, but portoenteric fistula is associated with a high mortality. We reported a case of intermittent massive upper gastrointestinal bleeding in a 33-year-old man with cholangiocarcinoma who underwent surgical resection followed by chemoradiation. A portoduodenal fistula due to chronic duodenal ulceration was identified. The bleeding was successfully controlled by endoscopic ultrasound-guided coil placement through the duodenal bulb using the anchoring technique. Follow-up endoscopy and computed tomography scan showed multiple coil placements between a part of the portal vein and the duodenal bulb without any evidence of portal vein thrombosis. There were no complications, and bleeding did not recur during the 8-month follow-up period.
-
Citations
Citations to this article as recorded by- Management of non-variceal upper gastrointestinal bleeding: role of endoscopic ultrasound-guided treatments
Chaoqun Han, Xin Ling, Jun Liu, Rong Lin, Zhen Ding
Therapeutic Advances in Gastroenterology.2022; 15: 175628482110561. CrossRef - A Case of an Internal Pancreatic Stent Penetrating the Portal Vein after Pancreaticoduodenectomy for Ampullary Carcinoma
Masanobu Taniguchi, Atsushi Mitsunaka, Yumi Zen, Takayuki Higashiguchi, Masaru Nagato, Yasuhisa Tango, Ichiro Nakamura, Tomoaki Nakamura, Hisanori Shiomi
The Japanese Journal of Gastroenterological Surgery.2022; 55(2): 99. CrossRef - Endoscopic ultrasound-guided portal vein coiling: troubleshooting interventional endoscopic ultrasonography
Shin Haba, Kazuo Hara, Nobumasa Mizuno, Takamichi Kuwahara, Nozomi Okuno, Akira Miyano, Daiki Fumihara, Moaz Elshair
Clinical Endoscopy.2022; 55(3): 458. CrossRef
- Management of non-variceal upper gastrointestinal bleeding: role of endoscopic ultrasound-guided treatments
- 4,098 View
- 85 Download
- 2 Web of Science
- 3 Crossref

-
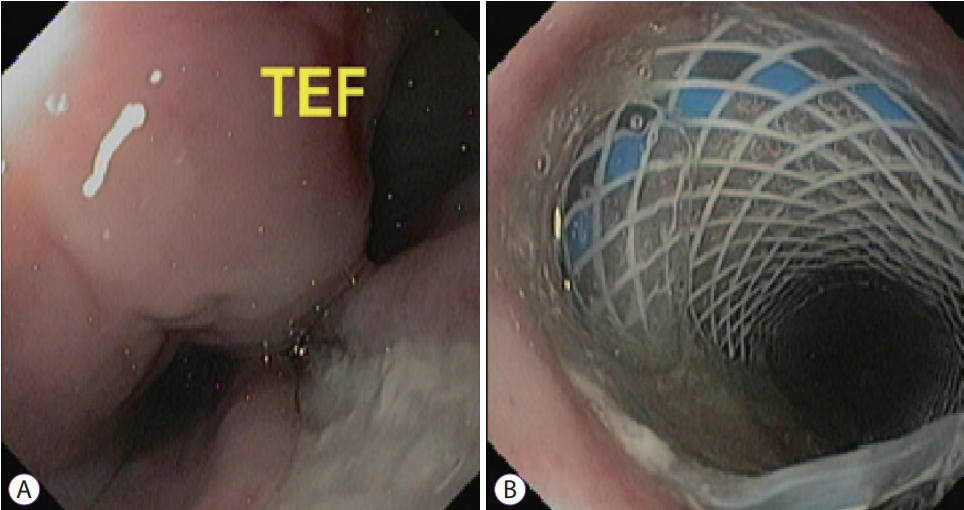
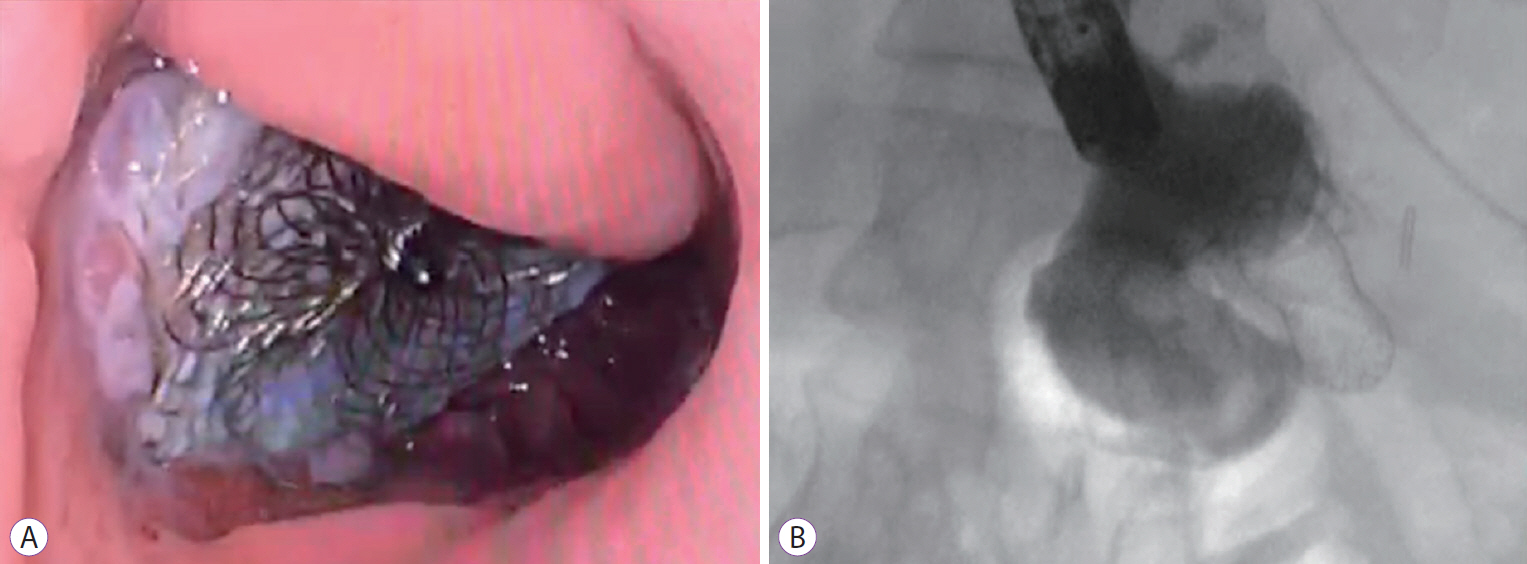
Successful Closure of a Benign Refractory Tracheoesophageal Fistula Using an Over-the-Scope Clip after Failed Esophageal Stent Placement and Surgical Management

- Nonthalee Pausawasdi, Chotirot Angkurawaranon, Tanyaporn Chantarojanasiri, Arunchai Chang, Wanchai Wongkornrat, Somchai Leelakusolvong, Asada Methasate
- Clin Endosc 2020;53(3):361-365. Published online October 28, 2019
- DOI: https://doi.org/10.5946/ce.2019.106
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Tracheoesophageal fistulas (TEFs) have traditionally been managed surgically, but the endoscopic approach is widely performed as a less invasive alternative. Different closure techniques have been proposed with inconsistent results. An over-the-scope clip (OTSC) appears to be a reasonable option, but long-term results have not been well defined. We report the long-term outcomes of a complex case of successful closure of a benign refractory TEF using an OTSC after failed surgical management and esophageal stent placement.
-
Citations
Citations to this article as recorded by- Successful Closure of a Tracheoesophageal Fistula Using an Over-The-Scope Clip
Osman Ali, Gurbani Singh, Sindhura Kolachana, Mohammed a Khan, Varun Kesar
Cureus.2023;[Epub] CrossRef - Over-the-Scope Clip Closure of Persistent Gastrocutaneous Fistula After Percutaneous Endoscopic Gastrostomy Tube Removal: A Report of Two Cases
Shigenori Masaki, Keishi Yamada
Cureus.2021;[Epub] CrossRef - Over-the-Scope Clip-Associated Endoscopic Muscular Dissection for Seven Cases of Small Gastric Submucosal Tumor: A Video-Based Case Series
Xin Li, Rongfen Wei, Jianfu Qin, Fei Qin, Peng Peng, Mengbin Qin, Shiquan Liu, Jiean Huang, Piero Chirletti
Gastroenterology Research and Practice.2021; 2021: 1. CrossRef
- Successful Closure of a Tracheoesophageal Fistula Using an Over-The-Scope Clip
- 5,043 View
- 154 Download
- 3 Web of Science
- 3 Crossref

- Role of Cardiac Septal Occluders in the Treatment of Gastrointestinal Fistulas: A Systematic Review
- Diogo Turiani Hourneaux De Moura, Alberto Baptista, Pichamol Jirapinyo, Eduardo Guimarães Hourneaux De Moura, Christopher Thompson
- Clin Endosc 2020;53(1):37-48. Published online July 9, 2019
- DOI: https://doi.org/10.5946/ce.2019.030
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Treating gastrointestinal (GI) fistulas endoscopically is challenging owing to an established epithelial tract. The variety of endoscopic approaches is transforming endoscopy into a first-line therapy. However, many sessions are often required, with variable success rates. Owing to these limitations, the off-label use of cardiac septal occluders (CSOs) has been reported. We searched for articles related to CSOs in the MEDLINE, EMBASE, Cochrane Library, and LILACS databases and gray literature. The primary outcomes included technical success, clinical success, and safety of CSOs in GI fistula management. A total of 25,574 records were identified, and 19 studies ultimately satisfied the inclusion criteria. Technical success was achieved in all cases. Of the 22 fistulas, 77.27% had successful closure, with a mean follow-up period of 32.02 weeks. The adverse event rate was 22.72%, with no associated mortality. Univariable and multivariable regression analyses showed no significant difference in the success of closure and adverse events in relation to several variables among the subgroups. The use of CSOs appeared to be technically feasible, effective, and safe in the treatment of GI fistulas. The satisfactory results derived from this sparse literature suggest that it can be an option in the management of GI fistulas.
-
Citations
Citations to this article as recorded by- Endoscopic closure of a recto-pelvic fistula with a cardiac septal occluder device
Ayowumi A. Adekolu, Ethan M. Cohen, Sardar Momin Shah-Khan, Soban Maan, Joyce Foryoung, Ademola Ajibade, Shyam Thakkar, Shailendra Singh
VideoGIE.2024; 9(1): 31. CrossRef - Cardiac Septal Occluder for Refractory Anastamotic Leak
Marcel Tomaszewski, Cameron McAlister, Janarthanan Sathananthan, Fergal Donnellan
Journal of the Canadian Association of Gastroenterology.2023; 6(5): 153. CrossRef - Use of atrial septal occluder in the treatment of chronic fistula following post-esophagectomy anastomotic leak
Manisha Daminda Kariyawasam, Jonathan Liang Yap, Zehao Tan, Tiffany Lye, Weng Hoong Chan, Jeremy Tian Hui Tan, Chin Hong Lim
Endoscopy.2023; 55(S 01): E1005. CrossRef - Closure of a Bronchoesophageal Fistula After Lung Transplantation With an Amplatzer Occluder Device
Erik J. Orozco-Hernandez, David McGiffin, Gregory Von Mering, Mustafa Ahmed, Joseph Thachuthara-George, Kondal R. Kyanam-Kabir-Baig, Charles W. Hoopes
Annals of Thoracic Surgery Short Reports.2023; 1(2): 332. CrossRef - Choosing the best endoscopic approach for post-bariatric surgical leaks and fistulas: Basic principles and recommendations
Victor Lira de Oliveira, Alexandre Moraes Bestetti, Roberto Paolo Trasolini, Eduardo Guimarães Hourneaux de Moura, Diogo Turiani Hourneaux de Moura
World Journal of Gastroenterology.2023; 29(7): 1173. CrossRef - Endoscopic closure of refractory upper GI–tracheobronchial fistulas with a novel occluder: a prospective, single-arm, single-center study (with video)
Lurong Li, Yun Wang, Chang Zhu, Jianyu Wei, Weifeng Zhang, Huaiming Sang, Han Chen, Haisheng Qian, Miao Xu, Jiahao Liu, Shuxian Jin, Yu Jin, Wangjian Zha, Wei Song, Yi Zhu, Jiwang Wang, Simon K. Lo, Guoxin Zhang
Gastrointestinal Endoscopy.2023; 97(5): 859. CrossRef - Endoscopic Treatment of Non-malignant Esophageal Perforation: Time to Go Vacuum?
Diogo Turiani Hourneaux de Moura, Bruno Salomão Hirsch, Heli Clóvis de Medeiros Neto, Victor Lira de Oliveira, Alexandre Moraes Bestetti, Bruna Furia Buzetti Hourneaux de Moura, Mouen A. Khashab, Eduardo Guimarães Hourneaux de Moura
Current Treatment Options in Gastroenterology.2023; 21(2): 95. CrossRef - Technical Review on Endoscopic Treatment Devices for Management of Upper Gastrointestinal Postsurgical Leaks
Renato Medas, Eduardo Rodrigues-Pinto, Eiji Sakai
Gastroenterology Research and Practice.2023; 2023: 1. CrossRef - Endoscopic Management of a Chronic Gastrocutaneous Fistula after Bariatric Revisional Surgery Using a Novel Cardiac Septal Occluder
Mariana Kumaira Fonseca, Nelson Heitor Vieira Coelho, João Luiz Langer Manica, Rafael Ramos Ramblo, Ingrid Elisa Spier, Artur Pacheco Seabra
GE - Portuguese Journal of Gastroenterology.2023; 30(Suppl. 1): 52. CrossRef - Catheter-based deployment of vascular plugs for the management of challenging gastric fistulae
Prashanth Rau, Philip McNamara, Ikechukwu Achebe, Dimitri Belkin, Odel Zadeh, Neil B. Marya
VideoGIE.2023; 8(12): 497. CrossRef - Long-term endoscopic follow-up after closure of a post-bariatric surgery fistula with a cardiac septal defect occluder
Diogo Turiani Hourneaux de Moura, Mateus Bond Boghossian, Bruno Salomão Hirsch, Thomas R. McCarty, Alberto Jose Baptista, Eduardo Guimarães Hourneaux de Moura
Endoscopy.2022; 54(03): E127. CrossRef - Status of bariatric endoscopy–what does the surgeon need to know? A review
Diogo Turiani Hourneaux de Moura, Anna Carolina Batista Dantas, Igor Braga Ribeiro, Thomas R McCarty, Flávio Roberto Takeda, Marco Aurelio Santo, Sergio Carlos Nahas, Eduardo Guimarães Hourneaux de Moura
World Journal of Gastrointestinal Surgery.2022; 14(2): 185. CrossRef - Tailored endoscopic treatment of tracheo-oesophageal fistula using preoperative holographic assessment and a cardiac septal occluder
Stefano Siboni, Angelo Fabio D'Aiello, Massimo Chessa, Luigi Bonavina
BMJ Case Reports.2022; 15(3): e248981. CrossRef - Closure of recurrent colovaginal fistulas using AMPLATZER occluder device
Joseph Simmons, Ahmed Sherif, Jason Mader, Saba Altarawneh, Mehiar El-Hamdani, Wesam Frandah
BMJ Open Gastroenterology.2022; 9(1): e000921. CrossRef - Acquired Benign Tracheoesophageal Fistula
Hasnain S. Bawaadam, Matthew Russell, Yaron B. Gesthalter
Journal of Bronchology & Interventional Pulmonology.2022; 29(3): e38. CrossRef - Adequate Management of Postoperative Complications after Esophagectomy: A Cornerstone for a Positive Outcome
Imad Kamaleddine, Alexander Hendricks, Magdalena Popova, Clemens Schafmayer
Cancers.2022; 14(22): 5556. CrossRef - Colovaginal fistula closure using a cardiac septal defect occluder
Omar Sadiq, Stephen Simmer, Andrew Watson, Marvin Eng, Tiberio Frisoli, Tobias Zuchelli
VideoGIE.2021; 6(1): 41. CrossRef - Cardiac septal occluder for closure of persistent gastrogastric fistula
Ki-Yoon Kim, Matthew J. Skinner
VideoGIE.2021; 6(7): 294. CrossRef - Role and possibilities of endoscopic Vacuum Therapy in the treatment of transmural defects of upper gastrointestinal tract
Vladimir Alekseevich Porkhanov, Stanislav Nikolayevich Pyatakov, Alexander Gennadievich Baryshev, Denis Mikhailovich Melnik, Maxim Sergeevich Shevchenko, Mikhail Ilyich Bykov, Svetlana Nikolaevna Pyatakova
Hirurg (Surgeon).2021; (1): 5. CrossRef - A Comprehensive Review of Endoscopic Management of Sleeve Gastrectomy Leaks
Mihajlo Gjeorgjievski, Zaid Imam, Mitchell S. Cappell, Laith H. Jamil, Michel Kahaleh
Journal of Clinical Gastroenterology.2021; 55(7): 551. CrossRef
- Endoscopic closure of a recto-pelvic fistula with a cardiac septal occluder device
- 7,606 View
- 272 Download
- 14 Web of Science
- 20 Crossref

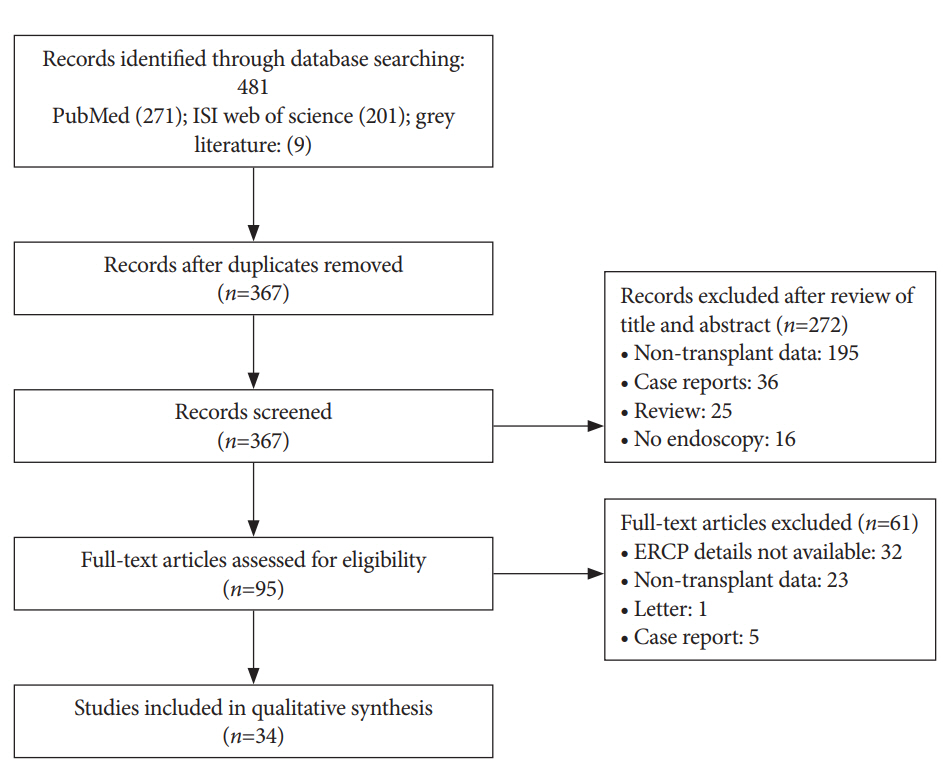
- Efficacy of Nasobiliary Tubes and Biliary Stents in Management of Patients with Bile Leak after Liver Transplantation: A Systematic Review
- Ali Raza, Anam Omer, Sara Iqbal, Vineet Gudsoorkar, Pramoda Koduru, Kumar Krishnan
- Clin Endosc 2019;52(2):159-167. Published online March 29, 2019
- DOI: https://doi.org/10.5946/ce.2018.118
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Bile leak is one of the most common complications of liver transplantation. The treatment options for bile leaks include conservative management, surgical re-intervention, percutaneous drainage and endoscopic drainage. We aimed to perform a systematic review to identify the efficacy of endoscopic treatment in the resolution of post-transplant bile leaks. Methods: Two independent reviewers performed systematic literature search in PubMed, ISI Web of Science, grey literature and relevant references in May 2017. Human studies in English with documented post-liver transplant bile leaks were included. Results: Thirty-four studies were included in the final analysis. The pooled efficacy of biliary stents for the resolution of post-transplant bile leaks was 82.43% compared with 87.15% efficacy of nasobiliary tubes. The efficacy of biliary stents was lower for anastomotic leaks (69.23%) compared to T-tube (90.9%) or cut-surface/ cystic duct stump related leaks (92.8%). Similarly, the efficacy of nasobiliary tube was also lower for anastomotic leaks (58.33%) compared to T-tube or cut-surface related leaks (100%). Conclusions: In this systematic review, the overall efficacy was 82.43% in biliary stent group, and 87.15% in nasobiliary tube group. Both biliary stent and nasobiliary tube were more effective in managing non-anastomotic leaks compared to anastomotic leaks. -
Citations
Citations to this article as recorded by- Application of percutaneous biliary drainage in the treatment of post-operative bile leakage after liver rupture: A case report
Jinlong Chen, Zhikuan Wang, Lixin Zhang, Xi Chen, Yuanyuan Liu, Hong Chen, Xiaoqiang Tong, Yanchao Dong
Journal of Minimal Access Surgery.2024;[Epub] CrossRef - A nomogram for prediction of ERCP success in patients with bile duct leaks: a multicenter study
De-xin Chen, Sheng-xin Chen, Sen-lin Hou, Gui-hai Wen, Hai-kun Yang, Da-peng Shi, Qing-xin Lu, Ya-qi Zhai, Ming-yang Li
Surgical Endoscopy.2024; 38(5): 2465. CrossRef - Complications in Post-Liver Transplant Patients
Carlotta Agostini, Simone Buccianti, Matteo Risaliti, Laura Fortuna, Luca Tirloni, Rosaria Tucci, Ilenia Bartolini, Gian Luca Grazi
Journal of Clinical Medicine.2023; 12(19): 6173. CrossRef - Nasobiliary drainage: an effective treatment for pruritus in cholestatic liver disease
Wafaa Ahmed, Rebecca Jeyaraj, David Reffitt, John Devlin, Abid Suddle, John Hunt, Michael A Heneghan, Phillip Harrison, Deepak Joshi
Frontline Gastroenterology.2022; 13(5): 416. CrossRef - A case of combined use of endoscopic drainage and percutaneous drainage for traumatic liver injury type III b
Shigekuni Okumura, Jun Oda, Yousuke Minami, Masaru Hirayama, Kennta Aida
Journal of the Japanese Society of Intensive Care Medicine.2021; 28(3): 210. CrossRef - Biliary Complications Following Adult Deceased Donor Liver Transplantation: Risk Factors and Implications at a High-volume US Center
Abraham J. Matar, Katie Ross-Driscoll, Lisa Kenney, Hannah K. Wichmann, Joseph F. Magliocca, William H. Kitchens
Transplantation Direct.2021; 7(10): e754. CrossRef - The Need for a Better-Designed Study of the Outcomes of Endoscopic Management of Bile Leak
Hyung Ku Chon, Eun Ji Shin, Seong-Hun Kim
Clinical Endoscopy.2020; 53(6): 633. CrossRef
- Application of percutaneous biliary drainage in the treatment of post-operative bile leakage after liver rupture: A case report
- 6,043 View
- 99 Download
- 5 Web of Science
- 7 Crossref

- Gastrocolocutaneous Fistula: An Unusual Case of Gastrostomy Tube Malfunction with Diarrhea
- Junghwan Lee, Jinyoung Kim, Ha il Kim, Chung Ryul Oh, Sungim Choi, Soomin Noh, Hee Kyong Na, Hwoon-Yong Jung
- Clin Endosc 2018;51(2):196-200. Published online August 31, 2017
- DOI: https://doi.org/10.5946/ce.2017.062
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - A gastrocolocutaneous fistula is a rare complication of percutaneous endoscopic gastrostomy (PEG). We report a case of a gastrocolocutaneous fistula presenting with intractable diarrhea and gastrostomy tube malfunction. A 62-year-old woman with a history of multiple system atrophy was referred to us because of PEG tube malfunction. Twenty days prior to presentation, the patient started developing sudden diarrhea within minutes after starting PEG feeding. Fluoroscopy revealed that the balloon of the PEG tube was located in the lumen of the transverse colon with the contrast material filling the colon. Subsequently, the PEG tube was removed and the opening of the gastric site was endoscopically closed using hemoclips. Clinicians should be aware of gastrocolocutaneous fistula as one of the complications of PEG insertion. Sudden onset of diarrhea, immediately after PEG feedings, might suggest this complication, which can be effectively treated with endoscopic closure.
-
Citations
Citations to this article as recorded by- A Rare Case of Severe Diarrhea: Gastrocolic Fistula Caused by Migration of Percutaneous Endoscopic Gastrostomy Tube
Maria Elena Pugliese, Riccardo Battaglia, Antonio Cerasa, Lucia Francesca Lucca
Healthcare.2023; 11(9): 1263. CrossRef - An unusual complication of percutaneous endoscopic gastrostomy and its endoscopic treatment
Noble Thomas, Cherukara Philip Thomas, C. Ganesh Pai
Indian Journal of Gastroenterology.2023; 42(4): 580. CrossRef - How far is the endoscopist to blame for a percutaneous endoscopic gastrostomy complication?
George Stavrou, Persefoni Gionga, George Chatziantoniou, Georgios Tzikos, Alexandra Menni, Stavros Panidis, Anne Shrewsbury, Katerina Kotzampassi
World Journal of Gastrointestinal Surgery.2023; 15(5): 940. CrossRef - Misplacement of the PEG tube through the transverse colon, an uncommon but possible complication
David Viso Vidal, Francisco Jorquera Plaza
Revista Española de Enfermedades Digestivas.2022;[Epub] CrossRef - Endoscopic management of enteral tubes in adult patients – Part 2: Peri- and post-procedural management. European Society of Gastrointestinal Endoscopy (ESGE) Guideline
Paraskevas Gkolfakis, Marianna Arvanitakis, Edward J. Despott, Asuncion Ballarin, Torsten Beyna, Kurt Boeykens, Peter Elbe, Ingrid Gisbertz, Alice Hoyois, Ofelia Mosteanu, David S. Sanders, Peter T. Schmidt, Stéphane M. Schneider, Jeanin E. van Hooft
Endoscopy.2021; 53(02): 178. CrossRef - Een laattijdige complicatie na het plaatsen van een PEG-sonde
H. DEDECKER, T. STEINHAUSER, S. BOUHADAN, O. PETERS, A. BEUNIS
Tijdschrift voor Geneeskunde.2021;[Epub] CrossRef - Complex gastro-colo-cutaneous fistula secondary to a gunshot injury, management and literature review
Maha Al Shaibi, Mohamed Al Abri, Ghaitha Al Mahruqi, Alok Mittal
Trauma Case Reports.2020; 28: 100313. CrossRef - Colocutaneous Fistula after Percutaneous Endoscopic Gastrostomy (PEG) Tube Insertion
Matthew Warner, Muhammad Durrani
Clinical Practice and Cases in Emergency Medicine.2020; 4(4): 632. CrossRef - Rectal Bleeding after Insertion of a Percutaneous Endoscopic Gastrostomy Tube
Ghadeer Alhazmi, Mroj Alsabri, Shahad Alsuwat, Adnan Al-Zangabi, Abdulaziz Al-Zahrani, Mohammed Kareemulla Shariff
Case Reports in Gastroenterology.2020; 14(3): 637. CrossRef - Long-Term Gastrocolocutaneous Fistula after Endoscopic Gastrostomy: How Concerned Should We Be?
Gonçalo Nunes, Gabriel Paiva de Oliveira, João Cruz, Carla Adriana Santos, Jorge Fonseca
GE - Portuguese Journal of Gastroenterology.2019; 26(6): 441. CrossRef - Update on endoscopic enteral access
Kamthorn Yolsuriyanwong, Bipan Chand
Techniques in Gastrointestinal Endoscopy.2018; 20(4): 172. CrossRef
- A Rare Case of Severe Diarrhea: Gastrocolic Fistula Caused by Migration of Percutaneous Endoscopic Gastrostomy Tube
- 9,385 View
- 151 Download
- 10 Web of Science
- 11 Crossref

- Efficacy of the Over-the-Scope Clip System for Treatment of Gastrointestinal Fistulas, Leaks, and Perforations: A Korean Multi-Center Study
- Hang Lak Lee, Joo Young Cho, Jun-Hyung Cho, Jong Jae Park, Chan Gyoo Kim, Seong Hwan Kim, Joung-Ho Han
- Clin Endosc 2018;51(1):61-65. Published online August 29, 2017
- DOI: https://doi.org/10.5946/ce.2017.027
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Currently, a new over-the-scope clip (OTSC) system has been introduced. This system has been used for gastrointestinal perforations and fistulas in other countries. The aim of our study is to examine the therapeutic success rate of endoscopic treatment using the OTSC system in Korea.
Methods
This was a multicenter prospective study. A total of seven endoscopists at seven centers performed this procedure.
Results
A total of 19 patients were included, with gastrointestinal leakages from anastomosis sites, fistulas, or esophageal perforations due to Boerhaave’s syndrome. Among these, there were three gastrojejunostomy sites, three esophagojejunostomy sites, four esophagogastrostomy sites, one esophagocolonostomy site, one jejuno-jejunal site, two endoscopic full thickness resection site closures, one Boerhaave’s syndrome, two esophago-bronchial fistulas, one gastrocolonic fistula, and one colonopseudocyst fistula. The size of the leakage ranged from 5 to 30 mm. The median procedure time was 16 min. All cases were technically successful. Complete closure of the leak was achieved in 14 of 19 patients using OTSC alone.
Conclusions
The OTSC system is a safe and effective method for the management of gastrointestinal leakage, especially in cases of anastomotic leakage after surgery. -
Citations
Citations to this article as recorded by- Bariatric surgery and reproduction-implications for gynecology and obstetrics
Isaac A. Babarinsa, Mohammed Bashir, Husham AbdelRahman Ahmed, Badreldeen Ahmed, Justin C. Konje
Best Practice & Research Clinical Obstetrics & Gynaecology.2023; 90: 102382. CrossRef - Current status in endoscopic management of upper gastrointestinal perforations, leaks and fistulas
Shannon Melissa Chan, Kitty Kit Ying Auyeung, Siu Fung Lam, Philip Wai Yan Chiu, Anthony Yuen Bun Teoh
Digestive Endoscopy.2022; 34(1): 43. CrossRef - Endoscopic vacuum therapy (EVT) for acute esophageal perforation: Could it replace surgery?
Petros Stathopoulos, Malte Zumblick, Sabine Wächter, Leif Schiffmann, Thomas M. Gress, Detlef Bartsch, Guido Seitz, Ulrike W. Denzer
Endoscopy International Open.2022; 10(05): E686. CrossRef - Acquired Benign Tracheoesophageal Fistula
Hasnain S. Bawaadam, Matthew Russell, Yaron B. Gesthalter
Journal of Bronchology & Interventional Pulmonology.2022; 29(3): e38. CrossRef - Exclusión pilórica con dispositivo Ovesco (over-thescope) en caso de fístula yeyunal en obstrucción duodenal de etiología maligna
Raul Eduardo Pinilla Morales, Helena Facundo Navia, Elio Fabio Sánchez Cortés, Ivette C. Jiménez Lafourie, Álvaro Eduardo Sánchez Hernández, Luis Carlos Llorente Portillo
Revista colombiana de Gastroenterología.2022; 37(3): 320. CrossRef - Endoscopic management of leaks and fistulas after bariatric surgery: a systematic review and meta-analysis
Pawel Rogalski, Agnieszka Swidnicka-Siergiejko, Justyna Wasielica-Berger, Damian Zienkiewicz, Barbara Wieckowska, Eugeniusz Wroblewski, Andrzej Baniukiewicz, Magdalena Rogalska-Plonska, Grzegorz Siergiejko, Andrzej Dabrowski, Jaroslaw Daniluk
Surgical Endoscopy.2021; 35(3): 1067. CrossRef - Endoscopic management of gastro‐bronchial fistula following two‐stage esophagectomy using over‐the‐scope‐clip (OTSC): Case series
Chih Y. Tan, Htet A. Kyaw, Neda Farhangmehr, Cheuk‐Bong Tang, Naga V. Jayanthi
Advances in Digestive Medicine.2021; 8(2): 84. CrossRef - Over-the-Scope Clip Closure of Persistent Gastrocutaneous Fistula After Percutaneous Endoscopic Gastrostomy Tube Removal: A Report of Two Cases
Shigenori Masaki, Keishi Yamada
Cureus.2021;[Epub] CrossRef - Over‐the‐scope clip: a novel approach to the management of a colorectal anastomotic leak
Stephanie G. Jordan, Gregory J. Nolan
ANZ Journal of Surgery.2021; 91(11): 2534. CrossRef - Conservative treatment of patients with small bowel fistula
A.V. Vodyasov, D.M. Kopaliani, P.A. Yartsev, O.Kh. Kaloeva
Khirurgiya. Zhurnal im. N.I. Pirogova.2021; (4): 78. CrossRef - An Approach to Accelerate Healing and Shorten the Hospital Stay of Patients With Anastomotic Leakage After Esophagectomy: An Explorative Study of Systematic Endoscopic Intervention
LeQi Zhong, JiuDi Zhong, ZiHui Tan, YiTong Wei, XiaoDong Su, ZheSheng Wen, TieHua Rong, Yi Hu, KongJia Luo
Frontiers in Oncology.2021;[Epub] CrossRef - AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review
Jeffrey H. Lee, Prashant Kedia, Stavros N. Stavropoulos, David Carr-Locke
Clinical Gastroenterology and Hepatology.2021; 19(11): 2252. CrossRef - Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clinical Endoscopy.2021; 54(5): 633. CrossRef - Diagnostic challenge and surgical management of Boerhaave’s syndrome: a case series
Jiayue Wang, Degang Wang, Jianjiao Chen
Journal of Medical Case Reports.2021;[Epub] CrossRef - Over-the-scope clip management of non-acute, full-thickness gastrointestinal defects
David J. Morrell, Joshua S. Winder, Ansh Johri, Salvatore Docimo, Ryan M. Juza, Samantha R. Witte, Vamsi V. Alli, Eric M. Pauli
Surgical Endoscopy.2020; 34(6): 2690. CrossRef - Use of the Over the Scope Clip to Close Perforations and Fistulas
Panida Piyachaturawat, Parit Mekaroonkamol, Rungsun Rerknimitr
Gastrointestinal Endoscopy Clinics of North America.2020; 30(1): 25. CrossRef - Therapie der Ösophagusleckagen
Jutta Weber-Eibel
Journal für Gastroenterologische und Hepatologische Erkrankungen.2020; 18(1): 8. CrossRef - Successful Closure of a Benign Refractory Tracheoesophageal Fistula Using an Over-the-Scope Clip after Failed Esophageal Stent Placement and Surgical Management
Nonthalee Pausawasdi, Chotirot Angkurawaranon, Tanyaporn Chantarojanasiri, Arunchai Chang, Wanchai Wongkornrat, Somchai Leelakusolvong, Asada Methasate
Clinical Endoscopy.2020; 53(3): 361. CrossRef - Clinical efficacy of the over-the-scope clip device: A systematic review
Nicholas Bartell, Krystle Bittner, Vivek Kaul, Truptesh H Kothari, Shivangi Kothari
World Journal of Gastroenterology.2020; 26(24): 3495. CrossRef - Endoscopic devices and techniques for the management of bariatric surgical adverse events (with videos)
Allison R. Schulman, Rabindra R. Watson, Barham K. Abu Dayyeh, Manoop S. Bhutani, Vinay Chandrasekhara, Pichamol Jirapinyo, Kumar Krishnan, Nikhil A. Kumta, Joshua Melson, Rahul Pannala, Mansour A. Parsi, Guru Trikudanathan, Arvind J. Trindade, John T. Ma
Gastrointestinal Endoscopy.2020; 92(3): 492. CrossRef - Gastrointestinal tract injuries after thermal ablative therapies for hepatocellular carcinoma: A case report and review of the literature
Teresa Marzia Rogger, Andrea Michielan, Sandro Sferrazza, Cecilia Pravadelli, Luisa Moser, Flora Agugiaro, Giovanni Vettori, Sonia Seligmann, Elettra Merola, Marcello Maida, Francesco Antonio Ciarleglio, Alberto Brolese, Giovanni de Pretis
World Journal of Gastroenterology.2020; 26(35): 5375. CrossRef - Over‐the‐scope clip system: A review of 1517 cases over 9 years
Hideki Kobara, Hirohito Mori, Noriko Nishiyama, Shintaro Fujihara, Keiichi Okano, Yasuyuki Suzuki, Tsutomu Masaki
Journal of Gastroenterology and Hepatology.2019; 34(1): 22. CrossRef - Recent advancements in the minimally invasive management of esophageal perforation, leaks, and fistulae
Shirin Siddiqi, Dean P. Schraufnagel, Hafiz Umair Siddiqui, Michael J. Javorski, Adam Mace, Abdulrhman S. Elnaggar, Haytham Elgharably, Patrick R. Vargo, Robert Steffen, Saad M. Hasan, Siva Raja
Expert Review of Medical Devices.2019; 16(3): 197. CrossRef - Diagnosis and endoscopic treatment of esophageal leakage: a systematic review
Bram D. Vermeulen, Peter D. Siersema
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 58. CrossRef - Management of esophagojejunal anastomosis leakage after total gastrectomy
Pablo Priego, Pietro Giordano, Marta Cuadrado, Araceli Ballestero, Julio Galindo, Eduardo Lobo
European Surgery.2018; 50(6): 262. CrossRef - Endoluminal Therapies for Esophageal Perforations and Leaks
Jeffrey R. Watkins, Alexander S. Farivar
Thoracic Surgery Clinics.2018; 28(4): 541. CrossRef - Esophageal leaks: I thought that glue was not effective
Ignacio Fernández-Urién, Juan Vila
Endoscopy International Open.2018; 06(09): E1100. CrossRef
- Bariatric surgery and reproduction-implications for gynecology and obstetrics
- 7,581 View
- 324 Download
- 26 Web of Science
- 27 Crossref

- Endoscopic Management of Gastrointestinal Leaks and Perforation with Polyglycolic Acid Sheets
- Sojung Han, Hyunsoo Chung, Jun Chul Park, Sung Kwan Shin, Sang Kil Lee, Yong Chan Lee
- Clin Endosc 2017;50(3):293-296. Published online March 8, 2017
- DOI: https://doi.org/10.5946/ce.2016.121
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Gastrointestinal (GI) leakage, fistulae, and perforations can be serious and life threatening. There has been a paradigm shift in the management approach of these conditions, from surgical to conservative, including endoscopic management. Here, we report two cases of endoscopic closure of a GI fistula and perforation using polyglycolic acid (PGA) sheets with fibrin glue. The first case is of an anastomotic leak detected after subtotal gastrectomy with gastroduodenostomy. After failed application of endoclips, a PGA sheet was applied, and the fistula was successfully closed. The second case was of a 15-mm large perforated gastric ulcer, which was also successfully closed with a PGA sheet. This is the first case report that PGA sheet was used for the treatment of overt perforation. The outcome of these cases suggest that endoscopic closure using PGA sheets can be considered as a useful alternative for the management of GI leakage, fistulae, and perforations.
-
Citations
Citations to this article as recorded by- A Randomized Controlled Trial of Fibrin Glue to Prevent Bleeding After Gastric Endoscopic Submucosal Dissection
Hyun Deok Lee, Eunwoo Lee, Sang Gyun Kim, Cheol Min Shin, Jun Chul Park, Kee Don Choi, Seokyung Hahn, Soo-Jeong Cho
American Journal of Gastroenterology.2023; 118(5): 892. CrossRef - Large anastomotic leak: endoscopic treatment using combined fibrin glue and polyglycolic acid (PGA) sheets
Soo In Choi, Ji Young Park
BMJ Case Reports.2021; 14(8): e240188. CrossRef - The treatment for refractory rectovaginal fistula after low anterior resection with estriol, polyglycolic acid sheets and primary closure: A case report
Masatsugu Hiraki, Toshiya Tanaka, Tadayuki Kanai, Takuya Shimamura, Osamu Ikeda, Makio Yasunaga, Shinichi Ogata, Kenji Kitahara
International Journal of Surgery Case Reports.2020; 75: 483. CrossRef - Endoscopic management of esophagorespiratory fistulas
Brian Larson, Douglas G. Adler
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 65. CrossRef - Endoscopic closure of an anastomo-cutaneous fistula: Filling and shielding using polyglycolic acid sheets and fibrin glue with easily deliverable technique
Hideaki Kawabata, Yuji Okazaki, Naonori Inoue, Yukino Kawakatsu, Misuzu Hitomi, Masatoshi Miyata, Shigehiro Motoi
Endoscopy International Open.2018; 06(08): E994. CrossRef - Successful Endoscopic Closure Using Polyglycolic Acid Sheets with Fibrin Glue for Nonhealing Duodenal Ulcer with Perforation after Proton Beam Therapy of Liver Tumor
Ko Watanabe, Takuto Hikichi, Jun Nakamura, Minami Hashimoto, Tadayuki Takagi, Rei Suzuki, Mitsuru Sugimoto, Naoki Konno, Mika Takasumi, Yuki Sato, Hiroki Irie, Takashi Kimura, Akira Kenjo, Shigeru Marubashi, Katsutoshi Obara, Hiromasa Ohira
Case Reports in Gastroenterology.2018; 12(3): 679. CrossRef
- A Randomized Controlled Trial of Fibrin Glue to Prevent Bleeding After Gastric Endoscopic Submucosal Dissection
- 7,809 View
- 222 Download
- 7 Web of Science
- 6 Crossref

- Endoscopic Management of Gastrointestinal Leaks and Bleeding with the Over-the-Scope Clip: A Prospective Study
- Mahesh Kumar Goenka, Vijay Kumar Rai, Usha Goenka, Indrajit Kumar Tiwary
- Clin Endosc 2017;50(1):58-63. Published online October 31, 2016
- DOI: https://doi.org/10.5946/ce.2016.028
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: The over-the-scope clip (OTSC) is a device used for endoscopic closure of perforations, leaks and fistulas, and for endoscopic hemostasis. To evaluate the clinical effectiveness and safety of OTSC.
Methods
Between October 2013 and November 2015, 12 patients underwent OTSC placement by an experienced endoscopist. OTSC was used for the closure of gastrointestinal (GI) leaks and fistula in six patients, three of which were iatrogenic (esophageal, gastric, and duodenal) and three of which were inflammatory. In six patients, OTSC was used for hemostasis of non-variceal upper GI bleeding. Endoscopic tattooing using India ink was used to assist the accurate placement of the clip.
Results
All subjects except one with a colonic defect experienced immediate technical success as well as long-term clinical success, during a mean follow-up of 6 weeks. Only one clip was required to close each of the GI defects and to achieve hemostasis in all patients. There were no misfirings or complications of clips. The procedure was well tolerated, and patients were hospitalized for an average of 8 days (range, 3 to 10). Antiplatelet therapy was continued in patients with GI bleeding.
Conclusions
In our experience, OTSC was safe and effective for the closure of GI defect and to achieve hemostasis of non-variceal GI bleeding. -
Citations
Citations to this article as recorded by- Endoscopic self-expandable metal stent versus endoscopy vacuum therapy for traumatic esophageal perforations: a retrospective cohort study
Alessandrino Terceiro de Oliveira, Márcio Alencar Barreira, José Wilson da Cunha Parente Júnior, José Ruver Lima Herculano Junior, Jeany Borges e Silva Ribeiro, Orleancio Gomes Ripardo de Azevedo, Paulo Roberto Cavalcante de Vasconcelos
Surgical Endoscopy.2024; 38(4): 2142. CrossRef - Meta‐analysis: Over‐the‐scope clips in patients at high risk of re‐bleeding following upper gastrointestinal tract bleeding
Kun He, Ke Pang, Lujing Ying, Daiyu Yang, Kai Song, Yangjin Ciren, Xiaxiao Yan, Ziqi Guo, Chengzhen Lyu, Qiang Wang, Dong Wu
Alimentary Pharmacology & Therapeutics.2024;[Epub] CrossRef - Use of over-the-scope clip (OTSC) versus standard therapy for the prevention of rebleeding in large peptic ulcers (size ≥1.5 cm): an open-labelled, multicentre international randomised controlled trial
Shannon Chan, Rapat Pittayanon, Hsiu-Po Wang, Jiann-Hwa Chen, Anthony YB Teoh, Yu Ting Kuo, Raymond SY Tang, Hon Chi Yip, Stephen Ka Kei Ng, Sunny Wong, Joyce Wing Yan Mak, Heyson Chan, Louis Lau, Rashid N Lui, Marc Wong, Rungsun Rerknimitr, Enders K Ng,
Gut.2023; 72(4): 638. CrossRef - Current status in endoscopic management of upper gastrointestinal perforations, leaks and fistulas
Shannon Melissa Chan, Kitty Kit Ying Auyeung, Siu Fung Lam, Philip Wai Yan Chiu, Anthony Yuen Bun Teoh
Digestive Endoscopy.2022; 34(1): 43. CrossRef - The application of endoscopic loop ligation in defect repair following endoscopic full-thickness resection of gastric submucosal tumors originating from the muscularis propria layer
Guoxiang Wang, Yanli Xiang, Yangde Miao, Honggang Wang, Meidong Xu, Guang Yu
Scandinavian Journal of Gastroenterology.2022; 57(1): 119. CrossRef - Gastrointestinal Emergencies and the Role of Endoscopy
Vinod Kumar Dixit, Manoj Kumar Sahu, Vybhav Venkatesh, Varanasi Yugandhar Bhargav, Vinod Kumar, Mayank Bhushan Pateriya, Jayanthi Venkataraman
Journal of Digestive Endoscopy.2022; 13(03): 179. CrossRef - Closure of Gastrointestinal Fistulas and Leaks with the Over-the-Scope Clip: Case-Series Analysis
Abdullah Senlikci, Tahsin Dalgic, Ahmet Alyanak, Erdal Birol Bostanci
Indian Journal of Surgery.2021; 83(6): 1413. CrossRef - Combination Endoscopic Therapy is Effective for Treatment of Nonbariatric Postoperative Gastroenteric Leaks
Nikhil R. Thiruvengadam, Christopher Hamerski, Andrew Nett, Yasser Bhat, Janak Shah, Jona Bernabe, Steven Kane, Kenneth Binmoeller, Rabindra R. Watson
Techniques and Innovations in Gastrointestinal Endoscopy.2021; 23(2): 122. CrossRef - Efficacy of the OTSC System in the treatment of GI bleeding and wall defects: a PMCF meta-analysis
Timo Weiland, Sabrina Rohrer, Arthur Schmidt, Edris Wedi, Peter Bauerfeind, Karel Caca, Mouen A. Khashab, Juergen Hochberger, Franziska Baur, Thomas Gottwald, Marc O. Schurr
Minimally Invasive Therapy & Allied Technologies.2020; 29(3): 121. CrossRef - Long-term assessment of over-the-scope clip (OTSC) behavior after gastric application
Jinlong Hu, Yang Yang, Nan Ge, Sheng Wang, Jintao Guo, Xiang Liu, Guoxin Wang, Siyu Sun
Minimally Invasive Therapy & Allied Technologies.2020; 29(2): 86. CrossRef - Use of the Over the Scope Clip to Close Perforations and Fistulas
Panida Piyachaturawat, Parit Mekaroonkamol, Rungsun Rerknimitr
Gastrointestinal Endoscopy Clinics of North America.2020; 30(1): 25. CrossRef - Clinical efficacy of the over-the-scope clip device: A systematic review
Nicholas Bartell, Krystle Bittner, Vivek Kaul, Truptesh H Kothari, Shivangi Kothari
World Journal of Gastroenterology.2020; 26(24): 3495. CrossRef - Life on a knife edge: the optimal approach to the management of perforations during endoscopic submucosal dissection (ESD)
Shria Kumar, Young Hoon Youn, Jeffrey H. Lee
Expert Review of Gastroenterology & Hepatology.2020; 14(10): 965. CrossRef - Gastrointestinal tract injuries after thermal ablative therapies for hepatocellular carcinoma: A case report and review of the literature
Teresa Marzia Rogger, Andrea Michielan, Sandro Sferrazza, Cecilia Pravadelli, Luisa Moser, Flora Agugiaro, Giovanni Vettori, Sonia Seligmann, Elettra Merola, Marcello Maida, Francesco Antonio Ciarleglio, Alberto Brolese, Giovanni de Pretis
World Journal of Gastroenterology.2020; 26(35): 5375. CrossRef - Fístula broncoesofágica secundaria a aspergilosis pulmonar
Antonio María Caballero-Mateos, Mercedes López de Hierro Ruíz, Eduardo Redondo Cerezo
Revista Colombiana de Gastroenterología.2020; 35(4): 558. CrossRef - Over-the-Scope Clip to the Rescue! A Novel Tool for Refractory Acute Nonvariceal Upper Gastrointestinal Hemorrhage
Shivantha Amarnath, Jobin Philipose, Jeffrey Abergel, Hafiz Khan
Case Reports in Gastroenterology.2020; 14(2): 261. CrossRef - Over‐the‐scope clip system: A review of 1517 cases over 9 years
Hideki Kobara, Hirohito Mori, Noriko Nishiyama, Shintaro Fujihara, Keiichi Okano, Yasuyuki Suzuki, Tsutomu Masaki
Journal of Gastroenterology and Hepatology.2019; 34(1): 22. CrossRef - Over-the-scope-clips as primary and rescue therapy for non-variceal gastrointestinal bleeding: a systematic review and meta-analysis
Andrew Ofosu, Daryl Ramai, Febin John, Mohammed Barakat, Tagore Sunkara, Santosh Sharma, Vinaya Gaduputi, Douglas G. Adler, Madhavi Reddy
Minerva Gastroenterologica e Dietologica.2019;[Epub] CrossRef - Cierre endoscópico de perforaciones y fístulas del tracto digestivo mediante el sistema «Over-the scope clip» (Ovesco), en un centro terciario
G. Mosquera-Klinger, R. Torres-Rincón, J. Jaime-Carvajal
Revista de Gastroenterología de México.2019; 84(2): 263. CrossRef - Endoscopic closure of gastrointestinal perforations and fistulas using the Ovesco Over-The-Scope Clip system at a tertiary care hospital center
G. Mosquera-Klinger, R. Torres-Rincón, J. Jaime-Carvajal
Revista de Gastroenterología de México (English Edition).2019; 84(2): 263. CrossRef - Management of Bleeding from Unresectable Gastric Cancer
Hideaki Kawabata, Misuzu Hitomi, Shigehiro Motoi
Biomedicines.2019; 7(3): 54. CrossRef - Over‐the‐scope clip for acute esophageal variceal bleeding
Carolina Mangas‐Sanjuan, Belén Martínez-Moreno, Maryana Bozhychko, Luis Compañy, Juan Martinez, Francisco Ruiz, Juan Antonio Casellas, José Ramón Aparicio
Digestive Endoscopy.2019; 31(6): 712. CrossRef - Clinical outcomes of over-the-scope-clip system for the treatment of acute upper non-variceal gastrointestinal bleeding: a systematic review and meta-analysis
Chunyu Zhong, Shali Tan, Yutang Ren, Muhan Lü, Yan Peng, Xiangsheng Fu, Xiaowei Tang
BMC Gastroenterology.2019;[Epub] CrossRef - Endoscopic Management with a Novel Over-The-Scope Padlock Clip System
Mahesh Kumar Goenka, Gajanan Ashokrao Rodge, Indrajeet Kumar Tiwary
Clinical Endoscopy.2019; 52(6): 574. CrossRef - Over the Scope Clips for Treatment of Acute Nonvariceal Gastrointestinal Bleeding in Children Are Safe and Effective
Paul Tran, Joshua Carroll, Bradley A. Barth, Nandini Channabasappa, David M. Troendle
Journal of Pediatric Gastroenterology and Nutrition.2018; 67(4): 458. CrossRef - Endoscopic titanium clip closure of gastric fistula after splenectomy: A case report
Jing Yu, Cheng-Ji Zhou, Pan Wang, Shou-Jiang Wei, Jin-Song He, Jin Tang
World Journal of Clinical Cases.2018; 6(15): 1047. CrossRef - New endoscopic techniques in treating gastrointestinal bleeding
Young Sin Cho
International Journal of Gastrointestinal Intervention.2018; 7(3): 131. CrossRef - Over-the-Scope Clip in the Management of Gastrointestinal Defect and Intractable Non-Variceal Bleeding
Hyungkil Kim
Clinical Endoscopy.2017; 50(1): 3. CrossRef - Hémorragies digestives : qui ? quand ? place des nouveaux traitements ?
D. Heresbach, A. Laquière
Acta Endoscopica.2017; 47(5): 281. CrossRef - Over-the-scope clip
Bhanwar Singh Dhandhu, Kumar Shwetanshu Narayan, Surinder Sultania, Sandeep Nijhawan
Journal of Digestive Endoscopy.2016; 07(02): 047. CrossRef
- Endoscopic self-expandable metal stent versus endoscopy vacuum therapy for traumatic esophageal perforations: a retrospective cohort study
- 9,600 View
- 307 Download
- 31 Web of Science
- 30 Crossref

- Endoscopic Closure for Full-Thickness Gastrointestinal Defects: Available Applications and Emerging Innovations
- Nobuyoshi Takeshita, Khek Yu Ho
- Clin Endosc 2016;49(5):438-443. Published online August 30, 2016
- DOI: https://doi.org/10.5946/ce.2016.104
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Full-thickness gastrointestinal defects such as perforation, anastomotic leak, and fistula are severe conditions caused by various types of pathologies. They are more likely to require intensive care and a long hospital stay and have high rates of morbidity and mortality. After intentional full-thickness opening of hollow organs for natural orifice transluminal endoscopic surgery, safe and secure closure is urgently required. The currently available advanced endoscopic closing techniques have a major role in the treatment of full-thickness gastrointestinal defects. Appropriate usage of these techniques requires taking into account their advantages and limitations during practical application. We reviewed the available endoscopic modalities, including endoscopic clips, stents, vacuum-assisted closure, gap filling, and suturing devices, discussed their advantages and limitations when treating full-thickness gastrointestinal defects, and explored emerging innovations, including a novel endoluminal surgical platform for versatile suturing and a cell-laden scaffold for effective gap filling. Although these emerging technologies still require further pre-clinical and clinical trials to assess their feasibility and efficacy, the available modalities may be replaced and refined by these new techniques in the near future.
-
Citations
Citations to this article as recorded by- Injectable nanoengineered adhesive hydrogel for treating enterocutaneous fistulas
Natan Roberto de Barros, Ankit Gangrade, Ahmad Rashad, RunRun Chen, Fatemeh Zehtabi, Menekse Ermis, Natashya Falcone, Reihaneh Haghniaz, Safoora Khosravi, Alejandro Gomez, Shuyi Huang, Marvin Mecwan, Danial Khorsandi, Junmin Lee, Yangzhi Zhu, Bingbing Li,
Acta Biomaterialia.2024; 173: 231. CrossRef - Novel external reinforcement device for gastrointestinal anastomosis in an experimental study
Hiro Hasegawa, Nobuyoshi Takeshita, Woogi Hyon, Suong-Hyu Hyon, Masaaki Ito
BMC Surgery.2023;[Epub] CrossRef - Colon Sparing Endoscopic Full-Thickness Resection for Advanced Colorectal Lesions: Is It Time for Global Adoption?
Zhong-Wei Wu, Chao-Hui Ding, Yao-Dong Song, Zong-Chao Cui, Xiu-Qian Bi, Bo Cheng
Frontiers in Oncology.2022;[Epub] CrossRef - The Etiology, Diagnosis, and Management of Esophageal Perforation
Puja Gaur Khaitan, Amber Famiglietti, Thomas J. Watson
Journal of Gastrointestinal Surgery.2022; 26(12): 2606. CrossRef - Advanced Endoscopic Tools
Eleanor C. Fung
Digestive Disease Interventions.2021; 05(02): 194. CrossRef - Repair of upper-GI fistulas and anastomotic leakage by the use of endoluminal vacuum-assisted closure
Andrew Watson, Tobias Zuchelli
VideoGIE.2019; 4(1): 40. CrossRef - Effect of poly(3-hydroxyalkanoates) as natural polymers on mesenchymal stem cells
Vera Voinova, Garina Bonartseva, Anton Bonartsev
World J Stem Cells.2019; 11(10): 764. CrossRef - Endoscopic Closure of Gastrointestinal Fistulae and Leaks
Jaehoon Cho, Ara B. Sahakian
Gastrointestinal Endoscopy Clinics of North America.2018; 28(2): 233. CrossRef - Non-visible colovesical fistula located by cystoscopy and successfully managed with the novel Padlock® device for endoscopic closure
Benito Velayos, L. Del Olmo, L. Merino, M. Valsero, J. M. González
International Journal of Colorectal Disease.2018; 33(6): 827. CrossRef - Poly(3-hydroxybutyrate) and Human Microbiota (Review)
A. P. Bonartsev, V. V. Voinova, G. A. Bonartseva
Applied Biochemistry and Microbiology.2018; 54(6): 547. CrossRef - Hepatocolic fistula managed with a novel Padlock® device for endoscopic closure
Benito Velayos Jiménez, Lourdes Del Olmo Martínez, Carmen Alonso Martín, Javier Trueba Arguiñarena, José Manuel González Hernández
Revista Española de Enfermedades Digestivas.2017;[Epub] CrossRef - Anastomotic leaks in gastrointestinal surgery and their prevention
Tomasz Banasiewicz, Adam Dziki, Paweł Lampe, Zbigniew Lorenc, Marek Szczepkowski, Jacek Zieliński, Grzegorz Wallner
Polish Journal of Surgery.2017; 89(2): 49. CrossRef
- Injectable nanoengineered adhesive hydrogel for treating enterocutaneous fistulas
- 9,454 View
- 189 Download
- 11 Web of Science
- 12 Crossref

- Multidrug-Resistant Tuberculous Mediastinal Lymphadenitis, with an Esophagomediastinal Fistula, Mimicking an Esophageal Submucosal Tumor
- Dongwuk Kim, Juwon Kim, Daegeun Lee, Ha Sung Chang, Hyunsung Joh, Won-Jung Koh, Jun Haeng Lee
- Clin Endosc 2016;49(6):564-569. Published online April 18, 2016
- DOI: https://doi.org/10.5946/ce.2016.020
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Mediastinal tuberculous lymphadenitis rarely mimics esophageal submucosal tumor, particularly in the case of multidrug-resistant tuberculosis (MDR-TB). Herein, we report the case of a 61-year-old woman who visited a local hospital complaining of odynophagia. An initial esophagogastroduodenoscopy revealed an esophageal submucosal tumor, and subsequent chest computed tomography showed subcarinal lymphadenopathy with an esophagomediastinal fistula. The patient was then referred to Samsung Medical Center, and a second esophagogastroduodenoscopy showed deep central ulceration, as well as a suspicious fistula in the esophageal submucosal tumor-like lesion. A biopsy examination of the ulcerative lesion confirmed focal inflammation only. Next, an endobronchial, ultrasound-guided lymph node biopsy was performed, and TB was confirmed. The patient initially began a course of isoniazid, rifampicin, ethambutol, and pyrazinamide. However, after a drug sensitivity test, she was diagnosed with MDR-TB, and second-line anti-TB medications were prescribed. She recovered well subsequently.
-
Citations
Citations to this article as recorded by- Detection of Esophageal Tuberculosis, a Rare Cause of Abdominal Pain, on18F-FDG PET/CT
Tarun Kumar Jain, Hemant Malhotra, Subhash Nepalia, Ganesh Narayan Saxena
Journal of Nuclear Medicine Technology.2024; 52(2): 179. CrossRef - Esophagomediastinal fistula secondary to tuberculous mediastinal lymphadenopathy
Ming-Dong Zhou, Dong-Ge Han, Wei Liu
Clinics and Research in Hepatology and Gastroenterology.2023; 47(10): 102243. CrossRef - “Esophagomediastinal fistula presenting as drug resistant tuberculosis”
Chinnu Sasikumar, Ketaki Utpat, Unnati Desai, Jyotsna M. Joshi
Indian Journal of Tuberculosis.2020; 67(3): 363. CrossRef - Tuberculous esophagomediastinal fistula with concomitant mediastinal bronchial artery aneurysm-acute upper gastrointestinal bleeding: A case report
Sultan R Alharbi
World Journal of Gastroenterology.2019; 25(17): 2144. CrossRef - Combined transbronchoscopic needle aspiration (TBNA) and rapid on-site cytological evaluation (ROSE) for diagnosis of tuberculous mediastinal lymphadenitis
Xi Dai, Bin Niu, Xiao-Qiong Yang, Guo-Ping Li
Medicine.2018; 97(37): e11724. CrossRef - Mediastinal Tuberculous Lymphadenitis Diagnosed by Endosonographic Fine Needle Aspiration
Joonhwan Kim, Youngwoo Jang, Kyung Oh Kim, Yoon Jae Kim, Dong Kyun Park, Dong Hae Chung, Eun Young Kim, Jun-Won Chung
The Korean Journal of Gastroenterology.2016; 68(6): 312. CrossRef
- Detection of Esophageal Tuberculosis, a Rare Cause of Abdominal Pain, on18F-FDG PET/CT
- 10,597 View
- 123 Download
- 4 Web of Science
- 6 Crossref

- Tuberculous Prostatic Abscess with Prostatorectal Fistula after Intravesical Bacillus Calmette-Guérin Immunotherapy
- Jeong Ho Eom, Jai Hoon Yoon, Seok Won Lee, Hyo Sun Kim, Tae Young Park, Chang Seok Bang, Gwang Ho Baik, Dong Joon Kim
- Clin Endosc 2016;49(5):488-491. Published online March 15, 2016
- DOI: https://doi.org/10.5946/ce.2015.145
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Intravesical bacillus Calmette-Guérin (BCG) immunotherapy is a common treatment modality for bladder cancer after transurethral resection of a bladder tumor. This therapy is generally safe, and development of a prostatic abscess with a prostatorectal fistula after intravesical BCG immunotherapy is a very rare complication. This finding was incidentally obtained by the authors, who examined a patient with colonoscopy for evaluation of abdominal pain. The patient was successfully treated with antitubercular drugs. To the authors’ knowledge, this is the first report of a patient with a tuberculous prostatic abscess with prostatorectal fistula after BCG immunotherapy in South Korea.
-
Citations
Citations to this article as recorded by- A case of perforation of the prostatic abscess into the rectum resulting in a rectoprostatic fistula
Yuichi Sugiyama, Atsushi Fujikawa, Shuhei Yokokawa
IJU Case Reports.2023; 6(6): 433. CrossRef - Incidental findings in and around the prostate on prostate MRI: a pictorial review
Janki Trivedi, Tom Sutherland, Mark Page
Insights into Imaging.2021;[Epub] CrossRef - Prostate abscess: A comprehensive review of the literature
Alexander J Ridgway, Angus Chin-On Luk, Ian Pearce
Journal of Clinical Urology.2019; 12(6): 441. CrossRef - Tuberculous prostatic abscess following intravesical bacillus Calmette-Guérin immunotherapy
Bin Wang, Ji-Wen Song, Hui-Qing Chen
Chinese Medical Journal.2019; 132(18): 2263. CrossRef - Diagnosis and treatment of patients with prostatic abscess in the post‐antibiotic era
Anne Lenore Ackerman, Pooja S Parameshwar, Jennifer T Anger
International Journal of Urology.2018; 25(2): 103. CrossRef - An Unusual Cause of a Prostatic Abscess
Rohit Majumdar, Nancy F. Crum-Cianflone
Infectious Diseases in Clinical Practice.2018; 26(3): 175. CrossRef - THE SIGNIFICANCE OF PATHOMORPHOLOGICAL INVESTIGATION IN THE DIAGNOSIS OF PROSTATE TUBERCULOSIS
V. V. Potapov, E. V. Brizhatuk
Herald Urology.2018; 6(2): 21. CrossRef
- A case of perforation of the prostatic abscess into the rectum resulting in a rectoprostatic fistula
- 8,515 View
- 114 Download
- 5 Web of Science
- 7 Crossref

- Communicating Tubular Esophageal Duplication Combined with Bronchoesophageal Fistula
- Ju Hwan Kim, Chang-Il Kwon, Ji Young Rho, Sang Woo Han, Ji Su Kim, Suk Pyo Shin, Ga Won Song, Ki Baik Hahm
- Clin Endosc 2016;49(1):81-85. Published online January 28, 2016
- DOI: https://doi.org/10.5946/ce.2016.49.1.81
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Esophageal duplication (ED) is rarely diagnosed in adults and is usually asymptomatic. Especially, ED that is connected to the esophagus through a tubular communication and combined with bronchoesophageal fistula (BEF) is extremely rare and has never been reported in the English literature. This condition is very difficult to diagnose. Although some combinations of several modalities, such as upper gastrointestinal endoscopy, esophagography, computed tomography, magnetic resonance imaging, and endoscopic ultrasonography, can be used for the diagnosis, the results might be inconclusive. Here, we report on a patient with communicating tubular ED that was incidentally diagnosed on the basis of endoscopy and esophagography during the postoperational evaluation of BEF.
-
Citations
Citations to this article as recorded by- Reconstruction of Adult Tubular Esophageal Duplication with Supraclavicular Artery Island Flap: A Rare Case Presentation
Xin Yang, Zheng Jiang, Jun Liu, Fei Chen
Ear, Nose & Throat Journal.2023; : 014556132311734. CrossRef - Tubular Duplication of the Esophagus in a Newborn, Treated by Thoracoscopy
Igor Khvorostov, Alexey Gusev, Abdumanap Alkhasov, Sergey Yatsyk, Elena D'yakonova
European Journal of Pediatric Surgery Reports.2022; 10(01): e49. CrossRef - Endoscopic septum division of tubular esophageal duplication in two children and systematic review
Rahşan Özcan, Ali Ekber Hakalmaz, Şenol Emre, Ayşe Karagöz, Çiğdem Tütüncü, Sebuh Kuruğoğlu, Gonca Topuzlu Tekant
Pediatric Surgery International.2022; 38(11): 1525. CrossRef - Endoscopic management of a tubular esophageal duplication in a young adult
Pietro Familiari, Rosario Landi, Francesca Mangiola, Camilla Vittoria Vita, Guido Costamagna
VideoGIE.2020; 5(10): 455. CrossRef - Esophageal duplication and congenital esophageal stenosis
A. Francois Trappey, Shinjiro Hirose
Seminars in Pediatric Surgery.2017; 26(2): 78. CrossRef
- Reconstruction of Adult Tubular Esophageal Duplication with Supraclavicular Artery Island Flap: A Rare Case Presentation
- 10,122 View
- 91 Download
- 4 Web of Science
- 5 Crossref

- Successful Palliation of a Malignant Cologastric Fistula with a Covered Self-Expanding Metal Stent
- Mathilde Therese Winther Breitenbauch, Anders Tøttrup
- Clin Endosc 2015;48(6):576-578. Published online November 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.6.576
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - When patients present with malignant cologastric fistulas, the tumor stage is often advanced and management is only palliative. We report the case of a 75-year-old man with a symptomatic cologastric fistula arising from an advanced tumor in the transverse colon, previously stented owing to malignant obstruction. An 8-cm-long covered self-expanding metal stent (COMVI enteral colonic stent; Taewoong Medical) was placed inside the primary stent, which sealed the fistula and completely alleviated the symptoms. Considering the successful outcome, we propose that insertion of a covered stent be considered in the palliative management of patients with malignant cologastric fistulas.
- 7,138 View
- 47 Download

- Utility of Over-the-Scope Clipping for Closure of a Persistent Post-Percutaneous Endoscopic Gastrostomy Fistula under Long-Term Steroid Therapy
- Yoshihisa Arao, Yuichi Sato, Satoru Hashimoto, Hiroki Honda, Kazumi Yoko, Masaaki Takamura, Ken-ichi Mizuno, Masaaki Kobayashi
- Clin Endosc 2015;48(6):563-565. Published online November 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.6.563
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - A 50-year-old woman had a percutaneous endoscopic gastrostomy (PEG) tube placed after surgery for pharyngeal cancer. After 21 months, the PEG tube was removed due to improvement of per-oral ingestion. She had taken prednisolone for 31 years for systemic lupus erythematosus. The post-PEG fistula did not close spontaneously. The cause of the fistula was slow wound healing and gastrostomy site inflammation due to long-term steroid therapy. We were able to close the fistula with an over-the-scope clipping (OTSC) system. This case suggests that OTSC is useful for closing persistent post-PEG fistulas in patients receiving long-term prednisolone therapy.
-
Citations
Citations to this article as recorded by- UEG Week 2016 Poster Presentations
United European Gastroenterology Journal.2016; 4(5_suppl): A157. CrossRef
- UEG Week 2016 Poster Presentations
- 9,716 View
- 66 Download
- 1 Crossref

- Treatment of Traumatic Esophagopleural Fistula Using the Over-the-Scope-Clip System
- Ji Hyoung Kim, Jong-Jae Park, Il Woo Jung, Sang Hoon Kim, Hee Dong Kim, Jung Wan Choe, Moon Kyung Joo, Hyun Gu Kim
- Clin Endosc 2015;48(5):440-443. Published online September 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.5.440
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Esophagopleural fistula (EPF) is a rare condition that is usually accompanied by severe infection and life-threatening morbidity. Here, we report the successful treatment of an EPF by closing an esophageal orifice using the over-the-scope-clip (OTSC) system without postprocedural complications. A 41-year-old man had serious thoracic and abdominal trauma due to a traffic accident. Computed tomography revealed findings suggestive of esophageal rupture due to Boerhaave syndrome. An emergent explorative operation was performed for primary repair with the insertion of a vacuum-assisted closure device. A postoperative upper gastrointestinal series revealed an EPF tract connecting the left pleural space and distal esophagus. We performed an endoscopic procedure using the "traumatic-type"OTSC to seal the EPF, and the esophageal orifice was completely healed 2 weeks postoperatively. The OTSC system might represent a safe and feasible modality for the treatment of EPF.
-
Citations
Citations to this article as recorded by- A Comprehensive Review of Endoscopic Management of Sleeve Gastrectomy Leaks
Mihajlo Gjeorgjievski, Zaid Imam, Mitchell S. Cappell, Laith H. Jamil, Michel Kahaleh
Journal of Clinical Gastroenterology.2021; 55(7): 551. CrossRef - Bevacizumab-induced esophageal pleural fistula during maintenance therapy without radiation in lung cancer
Ting Wang, Asmitananda Thakur, Baoqing Chen
BMC Pulmonary Medicine.2021;[Epub] CrossRef - Over-the-Scope Clip Closure of an Esophageal-Pleural Fistula Secondary to Esophageal Stent Placement: A Case Report
Justin Chuang, Naveena Luke, Khushbu Patel, Jordan Burlen, Ali Nawras
Cureus.2021;[Epub] CrossRef - Endoluminal vacuum therapy in the management of an esophago-pleural fistula as a complication of Boerhaave syndrome in a patient with eosinophilic esophagitis
Carlos Tuñon, Juan De Lucas, Jan Cubilla, Rafael Andrade, Miguel Aguirre, Julio Zúñiga Cisneros
BMC Gastroenterology.2021;[Epub] CrossRef - Komplikationsbeherrschung bei Körperhöhlentrauma
H. Vogelsang
Trauma und Berufskrankheit.2017; 19(S1): 88. CrossRef - Endoscopic Approach for Major Complications of Bariatric Surgery
Moon Kyung Joo
Clinical Endoscopy.2017; 50(1): 31. CrossRef - Endoscopic clipping of spontaneous esophageal rupture: Case reports of three patients
Koji Otsuka, Masahiko Murakami, Tomotake Ariyoshi, Takeshi Yamashita, Satoru Goto, Makoto Watanabe, Takeshi Aoki
International Journal of Surgery Case Reports.2017;[Epub] CrossRef
- A Comprehensive Review of Endoscopic Management of Sleeve Gastrectomy Leaks
- 7,183 View
- 72 Download
- 6 Web of Science
- 7 Crossref

- Cholangitis Secondary to Food Material Impaction in the Common Bile Duct through a Choledochoduodenal Fistula
- Bong-Koo Kang, Sung Min Park, Byung-Wook Kim, Joon Sung Kim, Ji Hee Kim, Jeong-Seon Ji, Hwang Choi
- Clin Endosc 2015;48(3):265-267. Published online May 29, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.3.265
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Biliary-enteric communications caused by duodenal ulcers are uncommon, and choledochoduodenal fistula (CDF) is by far the most common type. Usually in this situation, food material does not enter the common bile duct because the duodenal lumen is intact. Here, we report a case in which cholangitis occurred due to food materials impacted through a CDF. Duodenal obstruction secondary to duodenal ulcer prevented food passage into the duodenum in this case. Surgical management was recommended; however, the patient refused surgery because of poor general condition. Consequently, the patient expired with sepsis secondary to ascending cholangitis.
-
Citations
Citations to this article as recorded by- Stone-Induced Purulent Choledocoduodenal Fistula Presenting with Ascending Cholangitis
Christienne Shams, Michael Cannon, Jared Bortman, Seifeldin Hakim
ACG Case Reports Journal.2018; 5(1): e60. CrossRef - Successful Conservative Treatment of a Cholecystoduodenal Fistula Caused by a Cytomegalovirus-associated Duodenal Ulcer
Hideki Mori, Moriya Zakimi, Shin Kato, Koki Yamada, Kenji Chinen, Tomiaki Kubota, Masayuki Arashiro, Susumu Shinoura, Kaoru Kikuchi
Internal Medicine.2016; 55(18): 2617. CrossRef
- Stone-Induced Purulent Choledocoduodenal Fistula Presenting with Ascending Cholangitis
- 6,315 View
- 64 Download
- 2 Web of Science
- 2 Crossref

- Percutaneous Endoscopic Gastrostomy Through the Sinus Tract of a Surgical Gastrostomy
- Katerina Kotzampassi, George Stavrou
- Clin Endosc 2015;48(1):78-80. Published online January 31, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.1.78
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub We present the case of a woman on whom a percutaneous endoscopic gastrostomy (PEG) was performed through the sinus tract of a previous surgical gastrostomy for supraglottic obstructing malignancy. Five years after the induction of the surgical gastrostomy, she experienced a peristomal leakage, leading to severe necrotizing fasciitis, with skin irritation and inflammation. Despite extensive treatment to heal the abdominal wall close to the feeding tube, it recurred 3 months later, without any obvious cause. It was thus decided to perform a new gastrostomy in a nearby normal skin area, but, since it was totally impossible for the endoscope to be passed by mouth, due to obstruction, the sinus tract of the gastrostomy was used to facilitate endoscope insertion into the stomach for a new PEG.
-
Citations
Citations to this article as recorded by- Percutaneous endoscopic gastrostomy through a cervical esophageal fistula. An alternative, much improved technique for patient safety
George Stavrou, Vassilios Grosomanidis, Anastasia Sarafidou, Gavriil Tsiropoulos, Stefanos Triaridis, Katerina Kotzampassi
American Journal of Otolaryngology.2020; 41(3): 102408. CrossRef
- Percutaneous endoscopic gastrostomy through a cervical esophageal fistula. An alternative, much improved technique for patient safety
- 5,784 View
- 51 Download
- 1 Web of Science
- 1 Crossref

- Endoscopic Treatment of Various Gastrointestinal Tract Defects with an Over-the-Scope Clip: Case Series from a Tertiary Referral Hospital
- Woong Cheul Lee, Weon Jin Ko, Jun-Hyung Cho, Tae Hee Lee, Seong Ran Jeon, Hyun Gun Kim, Joo Young Cho
- Clin Endosc 2014;47(2):178-182. Published online March 31, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.2.178
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Recently, increasingly invasive therapeutic endoscopic procedures and more complex gastrointestinal surgeries such as endoscopic mucosal resection, endoscopic submucosal dissection, and novel laparoscopic approaches have resulted in endoscopists being confronted more frequently with perforations, fistulas, and anastomotic leakages, for which nonsurgical closure is desired. In this article, we present our experiences with the use of over-the-scope clip (OTSC) for natural orifice transluminal endoscopic surgery (NOTES) closure, prevention of perforation, anastomotic leakages, and fistula closures. The OTSC is a valuable device for closing intestinal perforations and fistulas, for NOTES closure, and for the prevention of perforation after the excision of a tumor from the proper muscle layer. Furthermore, it seems to be quite safe to perform, even by endoscopists with little experience of the technique.
-
Citations
Citations to this article as recorded by- Experimental Evaluation of the Optimal Suture Pattern With a Flexible Endoscopic Suturing System
Peter Halvax, Michele Diana, Yoshihiro Nagao, Jacques Marescaux, Lee Swanström
Surgical Innovation.2017; 24(3): 201. CrossRef - Management of non-acute gastrointestinal defects using the over-the-scope clips (OTSCs): a retrospective single-institution experience
Joshua S. Winder, Afif N. Kulaylat, Jane R. Schubart, Hassan M. Hal, Eric M. Pauli
Surgical Endoscopy.2016; 30(6): 2251. CrossRef - Early endoscopic closure of colocutaneous fistula adjacent to unmatured low colorectal anastomosis with the Over-The-Scope Clip (OTSC)
Constantinos Avgoustou, K. Paraskeva
Hellenic Journal of Surgery.2016; 88(3): 193. CrossRef - Endoscopic Closure for Full-Thickness Gastrointestinal Defects: Available Applications and Emerging Innovations
Nobuyoshi Takeshita, Khek Yu Ho
Clinical Endoscopy.2016; 49(5): 438. CrossRef
- Experimental Evaluation of the Optimal Suture Pattern With a Flexible Endoscopic Suturing System
- 6,116 View
- 58 Download
- 3 Web of Science
- 4 Crossref

- A Case of Spontaneous Esophagopleural Fistula Successfully Treated by Endoscopic Stent Insertion
- Gu Hyum Kang, Beom Yong Yoon, Beom Hee Kim, Hee Seok Moon, Hyun Yong Jeong, Jae Kyu Sung, Eaum Seok Lee
- Clin Endosc 2013;46(1):91-94. Published online January 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.1.91
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The most common cause of esophagorespiratory fistulas (ERFs) is associated with malignancy. The use of self-expandable metal stents is effective for the treatment of malignant ERFs, but benign ERF is rare, which is why its optimal treatment is not defined yet. There have been few reports describing benign esophagopleural fistula and its treatments in South Korea. Here, we report a rare case of spontaneous esophagopleural fistula, which was successfully treated by endoscopic placement of a membrane covered metal stent.
-
Citations
Citations to this article as recorded by- Delayed esophagopleural fistula after endoscopic injection sclerotherapy for esophageal varices
Mingliang Sui, Weibing Tang, Changjiang Wu, Jinhu Yang, Huiping Liu, Chaofa Huang, Xianzhu Hu, Damei Xia, Yadi Yang
Medicine.2020; 99(3): e18806. CrossRef - Unusual Presentation of an Esophagopleural Fistula in a Patient With Severe Esophagitis: Blunt Trauma or Iatrogenic?
Yanting Wang, Oscar A. Rivas Chicas, Anupam Basu
ACG Case Reports Journal.2019; 6(10): e00240. CrossRef - Tubercular esophago-pleural fistula—a rare case report and review of literature
Manoj Kumar Pattnaik, Sameer Kumar Panigrahy, Sarada Prasanna Sahoo, Naba Kumar Pattnaik
Indian Journal of Thoracic and Cardiovascular Surgery.2015; 31(4): 316. CrossRef - Treatment of Esophagopleural Fistulas Using Covered Retrievable Expandable Metallic Stents
Tae-Hyung Kim, Ji Hoon Shin, Kyung Rae Kim, Jung-Hoon Park, Jin Hyoung Kim, Ho-Young Song
Journal of Vascular and Interventional Radiology.2014; 25(4): 623. CrossRef
- Delayed esophagopleural fistula after endoscopic injection sclerotherapy for esophageal varices
- 6,232 View
- 44 Download
- 9 Web of Science
- 4 Crossref

- Aortoenteric Fistula Diagnosed by Double Balloon Enteroscopy: A Case Report
- Hyung Geun Yoon, Bong Min Ko, Jae Woong Tae, Su Jin Hong, Jong Ho Moon, Jin Oh Kim, Joon Seong Lee, Moon Sung Lee
- Clin Endosc 2013;46(1):106-109. Published online January 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.1.106
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub A secondary aortoenteric fistula (AEF) is a direct communication between the gastrointestinal tract and the aorta in a patient who has undergone major surgery on the aorta, often an aorta graft operation. We experienced a patient who had undergone graft interposition for abdominal aortic aneurysm and was admitted due to three episodes of hematemesis and following hamatochezia. Gastroscopy, colonoscopy, and radioactive iodine scan failed to identify the bleeding site in the patient. He was diagnosed with AEF by double balloon enteroscopy and recovered after surgical intervention.
-
Citations
Citations to this article as recorded by- Aortic Bulge: A Possible Predictive Sign of Impending Aortoenteric Fistula
Patrick Kennedy, Sandra Monteiro, Gordon Yip, Fernando Gastaldo
Canadian Association of Radiologists Journal.2019; 70(2): 204. CrossRef - Editor's Choice – Management of Secondary Aorto-enteric and Other Abdominal Arterio-enteric Fistulas: A Review and Pooled Data Analysis
S.K. Kakkos, C.D. Bicknell, I.A. Tsolakis, D. Bergqvist
European Journal of Vascular and Endovascular Surgery.2016; 52(6): 770. CrossRef
- Aortic Bulge: A Possible Predictive Sign of Impending Aortoenteric Fistula
- 5,740 View
- 53 Download
- 2 Crossref


 KSGE
KSGE


 First
First Prev
Prev



