Search
- Page Path
- HOME > Search
- Management of complications related to colorectal endoscopic submucosal dissection
- Tae-Geun Gweon, Dong-Hoon Yang
- Clin Endosc 2023;56(4):423-432. Published online July 27, 2023
- DOI: https://doi.org/10.5946/ce.2023.104

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Compared to endoscopic mucosal resection (EMR), colonoscopic endoscopic submucosal dissection (C-ESD) has the advantages of higher en bloc resection rates and lower recurrence rates of colorectal neoplasms. Therefore, C-ESD is considered an effective treatment method for laterally spread tumors and early colorectal cancer. However, C-ESD is technically more difficult and requires a longer procedure time than EMR. In addition to therapeutic efficacy and procedural difficulty, safety concerns should always be considered when performing C-ESD in clinical practice. Bleeding and perforation are the main adverse events associated with C-ESD and can occur during C-ESD or after the completion of the procedure. Most bleeding associated with C-ESD can be managed endoscopically, even if it occurs during or after the procedure. More recently, most perforations identified during C-ESD can also be managed endoscopically, unless the mural defect is too large to be sutured with endoscopic devices or the patient is hemodynamically unstable. Delayed perforations are quite rare, but they require surgical treatment more frequently than endoscopically identified intraprocedural perforations or radiologically identified immediate postprocedural perforations. Post-ESD coagulation syndrome is a relatively underestimated adverse event, which can mimic localized peritonitis from perforation. Here, we classify and characterize the complications associated with C-ESD and recommend management options for them.
-
Citations
Citations to this article as recorded by- International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
Seung Joo Kang, Chung Hyun Tae, Chang Seok Bang, Cheol Min Shin, Young-Hoon Jeong, Miyoung Choi, Joo Ha Hwang, Yutaka Saito, Philip Wai Yan Chiu, Rungsun Rerknimitr, Christopher Khor, Vu Van Khien, Kee Don Choi, Ki-Nam Shim, Geun Am Song, Oh Young Lee
Clinical Endoscopy.2024; 57(2): 141. CrossRef - Is there a best choice of equipment for colorectal endoscopic submucosal dissection?
Francesco Cocomazzi, Sonia Carparelli, Nunzia Labarile, Antonio Capogreco, Marco Gentile, Roberta Maselli, Jahnvi Dhar, Jayanta Samanta, Alessandro Repici, Cesare Hassan, Francesco Perri, Antonio Facciorusso
Expert Review of Medical Devices.2024; : 1. CrossRef
- International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
- 1,724 View
- 130 Download
- 4 Web of Science
- 2 Crossref

-
Significance of rescue hybrid endoscopic submucosal dissection in difficult colorectal cases

- Hayato Yamaguchi, Masakatsu Fukuzawa, Takashi Kawai, Takahiro Muramatsu, Taisuke Matsumoto, Kumiko Uchida, Yohei Koyama, Akira Madarame, Takashi Morise, Shin Kono, Sakiko Naito, Naoyoshi Nagata, Mitsushige Sugimoto, Takao Itoi
- Clin Endosc 2023;56(6):778-789. Published online July 26, 2023
- DOI: https://doi.org/10.5946/ce.2022.268

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub 
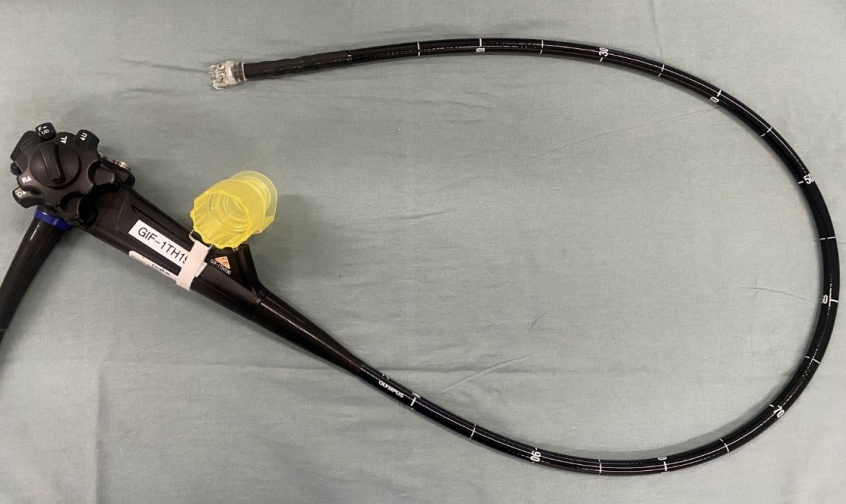
- Background
/Aims: Hybrid endoscopic submucosal dissection (ESD), in which an incision is made around a lesion and snaring is performed after submucosal dissection, has some advantages in colorectal surgery, including shorter procedure time and preventing perforation. However, its value for rescue resection in difficult colorectal ESD cases remains unclear. This study evaluated the utility of rescue hybrid ESD (RH-ESD).
Methods
We divided 364 colorectal ESD procedures into the conventional ESD group (C-ESD, n=260), scheduled hybrid ESD group (SH-ESD, n=69), and RH-ESD group (n=35) and compared their clinical outcomes.
Results
Resection time was significantly shorter in the following order: RH-ESD (149 [90–197] minutes) >C-ESD (90 [60–140] minutes) >SH-ESD (52 [29–80] minutes). The en bloc resection rate increased significantly in the following order: RH-ESD (48.6%), SH-ESD (78.3%), and C-ESD (97.7%). An analysis of factors related to piecemeal resection of RH-ESD revealed that the submucosal dissection rate was significantly lower in the piecemeal resection group (25% [20%–30%]) than in the en bloc resection group (40% [20%–60%]).
Conclusions
RH-ESD was ineffective in terms of curative resection because of the low en bloc resection rate, but was useful for avoiding surgery. -
Citations
Citations to this article as recorded by- Planned Hybrid Endoscopic Submucosal Dissection as Alternative for Colorectal Neoplasms: A Propensity Score-Matched Study
Yu-xin Zhang, Xun Liu, Fang Gu, Shi-gang Ding
Digestive Diseases and Sciences.2024; 69(3): 949. CrossRef - Understanding hybrid endoscopic submucosal dissection subtleties
João Paulo de Souza Pontual, Alexandre Moraes Bestetti, Diogo Turiani Hourneaux de Moura
Clinical Endoscopy.2023; 56(6): 738. CrossRef
- Planned Hybrid Endoscopic Submucosal Dissection as Alternative for Colorectal Neoplasms: A Propensity Score-Matched Study
- 2,217 View
- 121 Download
- 2 Web of Science
- 2 Crossref

-
Endoscopic retrograde cholangiopancreatography-related complications: risk stratification, prevention, and management

- Clement Chun Ho Wu, Samuel Jun Ming Lim, Christopher Jen Lock Khor
- Clin Endosc 2023;56(4):433-445. Published online July 17, 2023
- DOI: https://doi.org/10.5946/ce.2023.013
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) plays a crucial role in the management of pancreaticobiliary disorders. Although the ERCP technique has been refined over the past five decades, it remains one of the endoscopic procedures with the highest rate of complications. Risk factors for ERCP-related complications are broadly classified into patient-, procedure-, and operator-related risk factors. Although non-modifiable, patient-related risk factors allow for the closer monitoring and instatement of preventive measures. Post-ERCP pancreatitis is the most common complication of ERCP. Risk reduction strategies include intravenous hydration, rectal nonsteroidal anti-inflammatory drugs, and pancreatic stent placement in selected patients. Perforation is associated with significant morbidity and mortality, and prompt recognition and treatment of ERCP-related perforations are key to ensuring good clinical outcomes. Endoscopy plays an expanding role in the treatment of perforations. Specific management strategies depend on the location of the perforation and the patient’s clinical status. The risk of post-ERCP bleeding can be attenuated by preprocedural optimization and adoption of intra-procedural techniques. Endoscopic measures are the mainstay of management for post-ERCP bleeding. Escalation to angioembolization or surgery may be required for refractory bleeding. Post-ERCP cholangitis can be reduced with antibiotic prophylaxis in high risk patients. Bile culture-directed therapy plays an important role in antimicrobial treatment.
-
Citations
Citations to this article as recorded by- Prevention of post-ERCP complications
Lotfi Triki, Andrea Tringali, Marianna Arvanitakis, Tommaso Schepis
Best Practice & Research Clinical Gastroenterology.2024; 69: 101906. CrossRef - International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
Seung Joo Kang, Chung Hyun Tae, Chang Seok Bang, Cheol Min Shin, Young-Hoon Jeong, Miyoung Choi, Joo Ha Hwang, Yutaka Saito, Philip Wai Yan Chiu, Rungsun Rerknimitr, Christopher Khor, Vu Van Khien, Kee Don Choi, Ki-Nam Shim, Geun Am Song, Oh Young Lee
Clinical Endoscopy.2024; 57(2): 141. CrossRef - Double-guidewire technique for selective biliary cannulation does not increase the rate of post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with naïve papilla
Han Taek Jeong, June Hwa Bae, Ho Gak Kim, Jimin Han
Clinical Endoscopy.2024; 57(2): 226. CrossRef - Could assessment of genetic susceptibility be an effective solution to prevent pancreatitis from occurring after endoscopic retrograde cholangiopancreatography?
Jae Min Lee
The Korean Journal of Internal Medicine.2023; 38(6): 783. CrossRef
- Prevention of post-ERCP complications
- 3,236 View
- 311 Download
- 3 Web of Science
- 4 Crossref

- Over-the-Scope Clip in the Treatment of Gastrointestinal Leaks and Perforations
- Mike T. Wei, Ji Yong Ahn, Shai Friedland
- Clin Endosc 2021;54(6):798-804. Published online November 30, 2021
- DOI: https://doi.org/10.5946/ce.2021.250
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - While perforations, postoperative fistulas, and leaks have traditionally led to surgical or interventional radiology consultation for management, the introduction of the over-the-scope clip has allowed increased therapeutic possibilities for endoscopists. While primarily limited to case reports and series, the over-the-scope clip successfully manages gastrointestinal bleeding, perforations, as well as postoperative leaks and fistulas. Retrospective studies have demonstrated a relatively high success rate and a low complication rate. Given the similarity to variceal banding equipment, the learning curve with the over-the-scope clip is rapid. However, given the higher risk of procedures involving the use of the over-the-scope clip, it is essential to obtain the scope in a stable position and grasp sufficient tissue with the cap using a grasping tool and/or suction. From our experience, while closure may be successful in lesions sized up to 3 cm, successful outcomes are obtained for lesions sized <1 cm. Ultimately, given the limited available data, prospective randomized trials are needed to better evaluate the utility of the over-the-scope clip in various clinical scenarios, including fistula and perforation management.
-
Citations
Citations to this article as recorded by- A Multicenter Survey of Percutaneous Endoscopic Gastrostomy in 2019 at Korean Medical Institutions
Jun Woo Park, Tae Gyun Kim, Kwang Bum Cho, Jeong Seok Kim, Jin Woong Cho, Jung Won Jeon, Sun Gyo Lim, Chan Gyoo Kim, Hong Jun Park, Tae Jun Kim, Eun Sun Kim, Su Jin Jeong, Yong Hwan Kwon
Gut and Liver.2024; 18(1): 77. CrossRef - Clinical Practice Guideline for Percutaneous Endoscopic Gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
Gut and Liver.2024; 18(1): 10. CrossRef - Use of anchor pronged clips to close complex polyp resection defects
Mike Tzuhen Wei, Shai Friedland
VideoGIE.2023; 8(6): 245. CrossRef - Novel endoscopic management of gastroenterological anastomosis leakage by injecting gel-forming solutions: an experimental animal study
Yusuke Watanabe, Keiko Yamamoto, Zijian Yang, Haruna Tsuchibora, Masakazu Fujii, Masayoshi Ono, Shoko Ono, Takayuki Kurokawa, Naoya Sakamoto
Surgical Endoscopy.2023; 37(10): 8029. CrossRef - Clinical practice guidelines for percutaneous endoscopic gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
Clinical Endoscopy.2023; 56(4): 391. CrossRef - Management of complications related to colorectal endoscopic submucosal dissection
Tae-Geun Gweon, Dong-Hoon Yang
Clinical Endoscopy.2023; 56(4): 423. CrossRef - Gastroesophageal Reflux Disease in Obesity: Bariatric Surgery as Both the Cause and the Cure in the Morbidly Obese Population
Muaaz Masood, Donald Low, Shanley B. Deal, Richard A. Kozarek
Journal of Clinical Medicine.2023; 12(17): 5543. CrossRef - Clinical Practice Guideline for Percutaneous Endoscopic Gastrostomy
Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim, Chul-Hyun Lim, Jeong-Sik Byeon, Ki-Nam Shim, Geun Am Song, Moon Sung Lee, Jong-Jae Park, Oh Young Lee
The Korean Journal of Gastroenterology.2023; 82(3): 107. CrossRef - Endoscopic Management of Esophageal Cancer
Christopher Paiji, Alireza Sedarat
Cancers.2022; 14(15): 3583. CrossRef - Use of a novel dual-action clip for closure of complex endoscopic resection defects
Mike Tzuhen Wei, Shai Friedland
VideoGIE.2022; 7(11): 389. CrossRef
- A Multicenter Survey of Percutaneous Endoscopic Gastrostomy in 2019 at Korean Medical Institutions
- 3,632 View
- 120 Download
- 8 Web of Science
- 10 Crossref

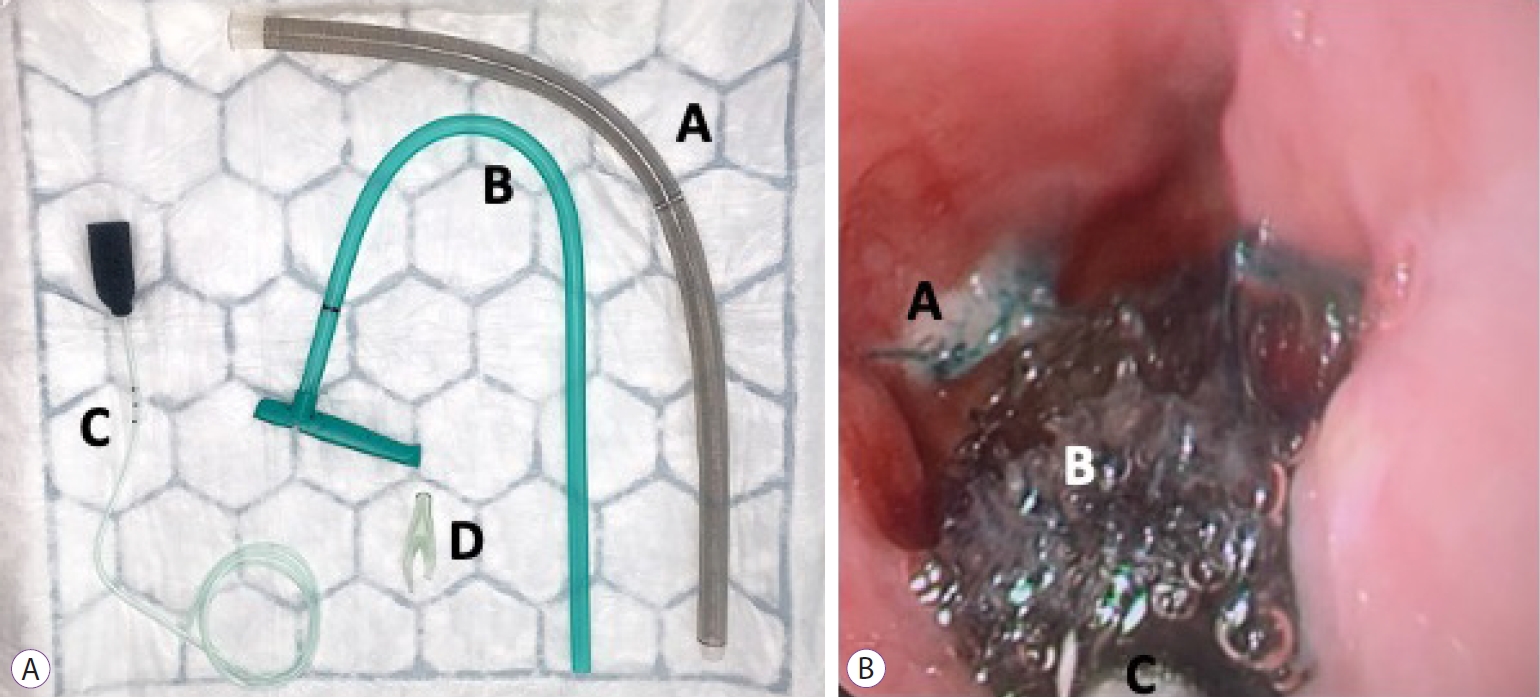
- Current Status of Endoscopic Vacuum Therapy in the Management of Esophageal Perforations and Post-Operative Leaks
- Imogen Livingstone, Lily Pollock, Bruno Sgromo, Sotiris Mastoridis
- Clin Endosc 2021;54(6):787-797. Published online November 16, 2021
- DOI: https://doi.org/10.5946/ce.2021.240
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Esophageal wall defects, including perforations and postoperative leaks, are associated with high morbidity and mortality and pose a significant management challenge. In light of the high morbidity of surgical management or revision, in recent years, endoscopic vacuum therapy (EVT) has emerged as a novel alternative treatment strategy. EVT involves transoral endoscopic placement of a polyurethane sponge connected to an externalized nasogastric tube to provide continuous negative pressure with the intention of promoting defect healing, facilitating cavity drainage, and ameliorating sepsis. In the last decade, EVT has become increasingly adopted in the management of a diverse spectrum of esophageal defects. Its popularity has been attributed in part to the growing body of evidence suggesting superior outcomes and defect closure rates in excess of 80%. This growing body of evidence, coupled with the ongoing evolution of the technology and techniques of deployment, suggests that the utilization of EVT has become increasingly widespread. Here, we aimed to review the current status of the field, addressing the mechanism of action, indications, technique methodology, efficacy, safety, and practical considerations of EVT implementation. We also sought to highlight future directions for the use of EVT in esophageal wall defects.
-
Citations
Citations to this article as recorded by- Multi-modality management of defects in the gastrointestinal tract: Where the endoscope meets the scalpel: Endoscopic vacuum therapy in the upper gastrointestinal tract
Lisanne M.D. Pattynama, Wietse J. Eshuis, Stefan Seewald, Roos E. Pouw
Best Practice & Research Clinical Gastroenterology.2024; : 101901. CrossRef - Management of esophageal anastomotic leaks, a systematic review and network meta-analysis
William Murray, Mathew G Davey, William Robb, Noel E Donlon
Diseases of the Esophagus.2024;[Epub] CrossRef - Management of an Aortoesophageal Fistula With Esophageal Endoluminal Wound Vacuum Therapy
Antoine Nehme, Samuel Brown, Salman Zaheer, Alexander Leung
Annals of Thoracic Surgery Short Reports.2024;[Epub] CrossRef - Treatment of Esophageal-Pleural Fistula After Diverticulectomy Using Transluminal Vacuum Therapy in a Patient with HIV Infection
M. A. Panasyuk, G. Yu. Aldaranov, V. N. Makhutov, E. G. Grigoriev
Russian Sklifosovsky Journal "Emergency Medical Care".2024; 13(1): 156. CrossRef - Homemade endoscopic vacuum therapy device for the management of transmural gastrointestinal defects
Diogo Turiani Hourneaux de Moura, Bruno Salomão Hirsch, Thomas R. McCarty, Marcos Eduardo Lera dos Santos, Hugo Gonçalo Guedes, Guilherme Francisco Gomes, Flaubert Sena de Medeiros, Eduardo Guimarães Hourneaux de Moura
Digestive Endoscopy.2023; 35(6): 745. CrossRef - Choosing the best endoscopic approach for post-bariatric surgical leaks and fistulas: Basic principles and recommendations
Victor Lira de Oliveira, Alexandre Moraes Bestetti, Roberto Paolo Trasolini, Eduardo Guimarães Hourneaux de Moura, Diogo Turiani Hourneaux de Moura
World Journal of Gastroenterology.2023; 29(7): 1173. CrossRef - Vacuum-Assisted Closure Treats Refractory Esophageal Leak in a Pediatric Patient
Evan K Lin, Felicia Lee, Jasmin Cao, Christian Saliba, Vivian Lu, Raymond I Okeke, Justin Sobrino, Christopher Blewett
Cureus.2023;[Epub] CrossRef - Esophageal Perforation
Kelly Fairbairn, Stephanie G. Worrell
Thoracic Surgery Clinics.2023; 33(2): 117. CrossRef - Endoscopic Treatment of Non-malignant Esophageal Perforation: Time to Go Vacuum?
Diogo Turiani Hourneaux de Moura, Bruno Salomão Hirsch, Heli Clóvis de Medeiros Neto, Victor Lira de Oliveira, Alexandre Moraes Bestetti, Bruna Furia Buzetti Hourneaux de Moura, Mouen A. Khashab, Eduardo Guimarães Hourneaux de Moura
Current Treatment Options in Gastroenterology.2023; 21(2): 95. CrossRef - Prophylactic endoluminal vacuum therapy after major gastrointestinal surgery: a systematic review
Olga Adamenko, Carlo Ferrari, Stefan Seewald, Jan Schmidt
Updates in Surgery.2022; 74(4): 1177. CrossRef - Endoscopic Management of Esophageal Cancer
Christopher Paiji, Alireza Sedarat
Cancers.2022; 14(15): 3583. CrossRef
- Multi-modality management of defects in the gastrointestinal tract: Where the endoscope meets the scalpel: Endoscopic vacuum therapy in the upper gastrointestinal tract
- 4,571 View
- 239 Download
- 7 Web of Science
- 11 Crossref

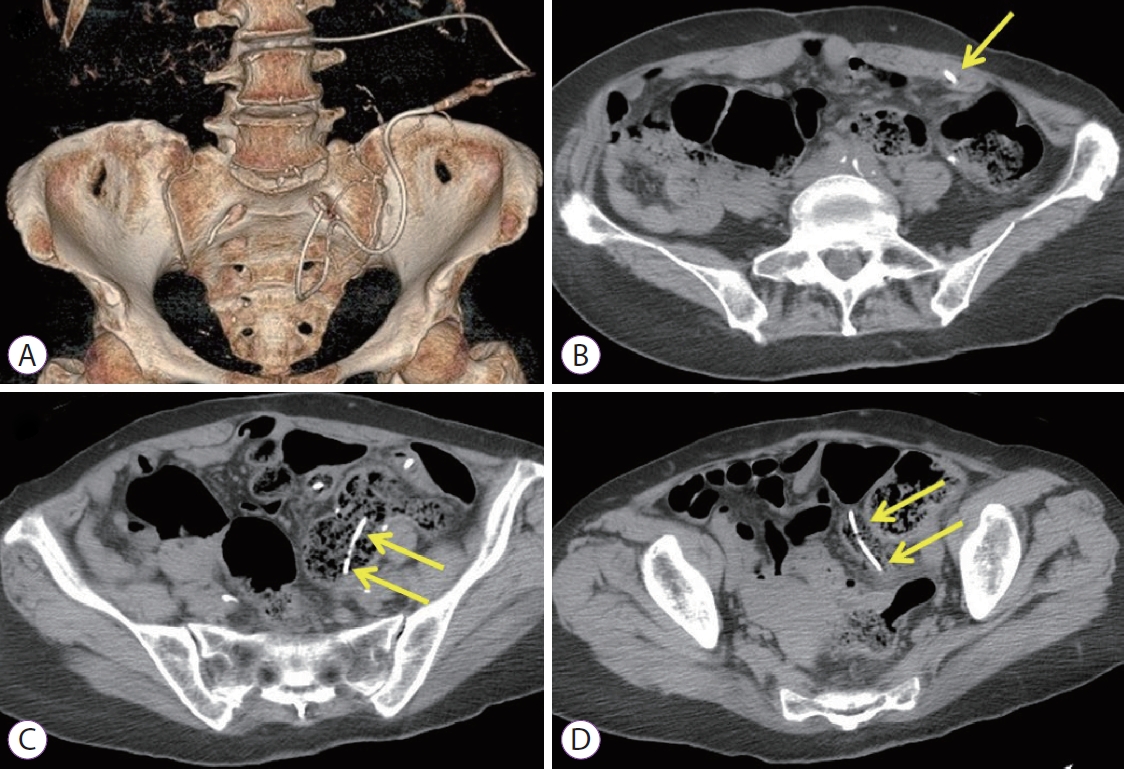
- Endoscopic Treatment of Iatrogenic Perforation of Sigmoid Diverticulum: A Case Report of Multidisciplinary Management
- Giacomo Emanuele Maria Rizzo, Giuseppina Ferro, Giovanna Rizzo, Giovanni Di Carlo, Alessandro Cantone, Gaetano Giuseppe Di Vita, Carmelo Sciumè
- Clin Endosc 2022;55(2):292-296. Published online June 7, 2021
- DOI: https://doi.org/10.5946/ce.2021.005
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
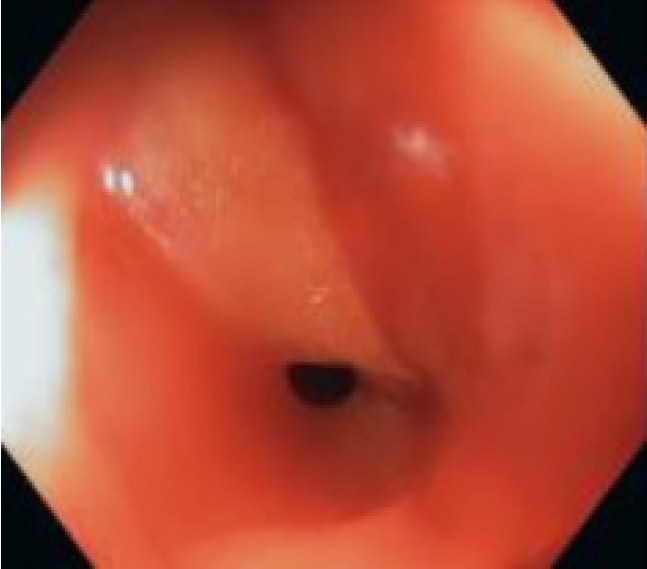
ePub - Iatrogenic perforations are severe complications of gastrointestinal endoscopy; therefore, their management should be adequately planned. A 77-year-old man with a history of diverticulosis underwent a colonoscopy for anemia. During the procedure, an iatrogenic perforation occurred suddenly in the sigmoid colon, near a severe angle among the numerous diverticula. Through-the-scope clips were immediately applied to treat it and close mucosal edges. Laboratory tests showed increased levels of inflammation and infection, and although there were no complaints of abdominal pain, the patient had an extremely distended abdomen. A multidisciplinary board began management based on a conservative approach. Pneumoperitoneum was treated with computed tomography-assisted drainage. After 72 hours, his intestinal canalization and laboratory tests were normal. Though this adverse event is rare, a multidisciplinary board should be promptly gathered upon occurrence, even if the patient appears clinically stable, to consider a conservative approach and avoid surgical treatment.
- 3,550 View
- 161 Download

- Intestinal Perforation Caused by Lumboperitoneal Shunt Insertion Repaired with an Over-the-Scope Clip
- Naoki Ishizuka, Eiji Komatsu
- Clin Endosc 2022;55(1):146-149. Published online March 3, 2021
- DOI: https://doi.org/10.5946/ce.2020.293
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Lumboperitoneal or ventriculoperitoneal shunt insertion is a standard therapy for hydrocephalus that diverts cerebrospinal fluid from the subarachnoid space into the peritoneal cavity. Gastrointestinal perforations due to this procedure occur rarely; however, accepted treatment strategies have not yet been established. Hence, the most common treatment approaches are open surgery or spontaneous closure without endoscopy. We report the case of a small intestinal perforation in a 73-year-old-woman that occurred after the insertion of a lumboperitoneal shunt. A positive cerebrospinal fluid culture and high cerebrospinal fluid white blood cell count indicated a retrograde bacterial infection, and computed tomography revealed that the peritoneal tip of the shunt catheter was located in the lumen of the gastrointestinal tract. We repaired the perforation endoscopically using an over-the-scope clip, and the patient’s recovery was uneventful. Use of an over-the-scope clip could be an effective and minimally invasive treatment for intestinal perforations caused by lumboperitoneal or ventriculoperitoneal shunt insertion.
-
Citations
Citations to this article as recorded by- Progress in Surgical Treatment of Traffic Hydrocephalus
飞 张
Advances in Clinical Medicine.2021; 11(09): 3942. CrossRef
- Progress in Surgical Treatment of Traffic Hydrocephalus
- 2,979 View
- 136 Download
- 1 Crossref

-
Diode Laser—Can It Replace the Electrical Current Used in Endoscopic Submucosal Dissection?

- Yunho Jung, Gwang Ho Baik, Weon Jin Ko, Bong Min Ko, Seong Hwan Kim, Jin Seok Jang, Jae-Young Jang, Wan-Sik Lee, Young Kwan Cho, Sun Gyo Lim, Hee Seok Moon, In Kyung Yoo, Joo Young Cho
- Clin Endosc 2021;54(4):555-562. Published online January 13, 2021
- DOI: https://doi.org/10.5946/ce.2020.229
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
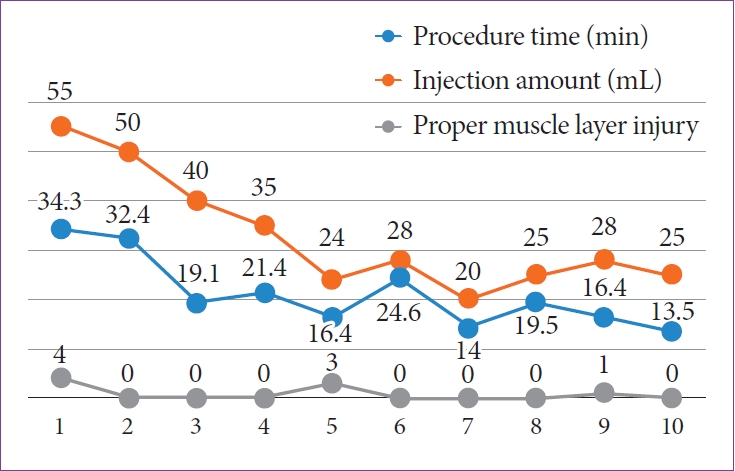
ePub - Background
/Aims: A new medical fiber-guided diode laser system (FDLS) is expected to offer high-precision cutting with simultaneous hemostasis. Thus, this study aimed to evaluate the feasibility of using the 1,940-nm FDLS to perform endoscopic submucosal dissection (ESD) in the gastrointestinal tract of an animal model.
Methods
In this prospective animal pilot study, gastric and colorectal ESD using the FDLS was performed in ex vivo and in vivo porcine models. The completeness of en bloc resection, the procedure time, intraprocedural bleeding, histological injuries to the muscularis propria (MP) layer, and perforation were assessed.
Results
The en bloc resection and perforation rates in the ex vivo study were 100% (10/10) and 10% (1/10), respectively; those in the in vivo study were 100% (4/4) and 0% for gastric ESD and 100% (4/4) and 25% (1/4) for rectal ESD, respectively. Deep MP layer injuries tended to occur more frequently in the rectal than in the gastric ESD cases, and no intraprocedural bleeding occurred in either group.
Conclusions
The 1,940-nm FDLS was capable of yielding high en bloc resection rates without intraprocedural bleeding during gastric and colorectal ESD in animal models. -
Citations
Citations to this article as recorded by- Use of Diode Laser in Hysteroscopy for the Management of Intrauterine Pathology: A Systematic Review
Andrea Etrusco, Giovanni Buzzaccarini, Antonio Simone Laganà, Vito Chiantera, Salvatore Giovanni Vitale, Stefano Angioni, Maurizio Nicola D’Alterio, Luigi Nappi, Felice Sorrentino, Amerigo Vitagliano, Tommaso Difonzo, Gaetano Riemma, Liliana Mereu, Alessa
Diagnostics.2024; 14(3): 327. CrossRef - Recent advances in endoscopic management of gastric neoplasms
Hira Imad Cheema, Benjamin Tharian, Sumant Inamdar, Mauricio Garcia-Saenz-de-Sicilia, Cem Cengiz
World Journal of Gastrointestinal Endoscopy.2023; 15(5): 319. CrossRef - Safety and efficacy of dual emission endoscopic laser treatment in patients with upper or lower gastrointestinal vascular lesions causing chronic anemia: results from the first multicenter cohort study
Gian Eugenio Tontini, Lorenzo Dioscoridi, Alessandro Rimondi, Paolo Cantù, Flaminia Cavallaro, Aurora Giannetti, Luca Elli, Luca Pastorelli, Francesco Pugliese, Massimiliano Mutignani, Maurizio Vecchi
Endoscopy International Open.2022; 10(04): E386. CrossRef
- Use of Diode Laser in Hysteroscopy for the Management of Intrauterine Pathology: A Systematic Review
- 3,882 View
- 110 Download
- 3 Web of Science
- 3 Crossref

- Perforation of a Gastric Tear during Esophageal Endoscopic Submucosal Dissection under General Anesthesia
- Tomoaki Yamasaki, Yuhei Sakata, Takehisa Suekane, Hiroko Nebiki
- Clin Endosc 2021;54(6):916-919. Published online November 12, 2020
- DOI: https://doi.org/10.5946/ce.2020.220
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Mallory-Weiss tears (MWT) are occasionally encountered during endoscopic procedures. Esophageal endoscopic submucosal dissection (ESD) is widely performed under general anesthesia to avoid unexpected body movements. We present the case of a 68-year-old woman with squamous cell carcinoma. Although ESD was performed under general anesthesia, a gastric perforation at the MWT caused by gastric inflation was observed after the procedure. The perforation was closed endoscopically, and she was discharged without any sequelae. Although general anesthesia is useful for esophageal ESD, it should be noted that it can cause MWT, and in rare cases, gastric perforation, due to gastric inflation during the procedure.
-
Citations
Citations to this article as recorded by- Gastric Perforation Encountered during Duodenal Stent Insertion
Sung Woo Ko, Hoonsub So, Sung Jo Bang
The Korean Journal of Gastroenterology.2022; 80(5): 221. CrossRef
- Gastric Perforation Encountered during Duodenal Stent Insertion
- 3,796 View
- 77 Download
- 1 Web of Science
- 1 Crossref

-
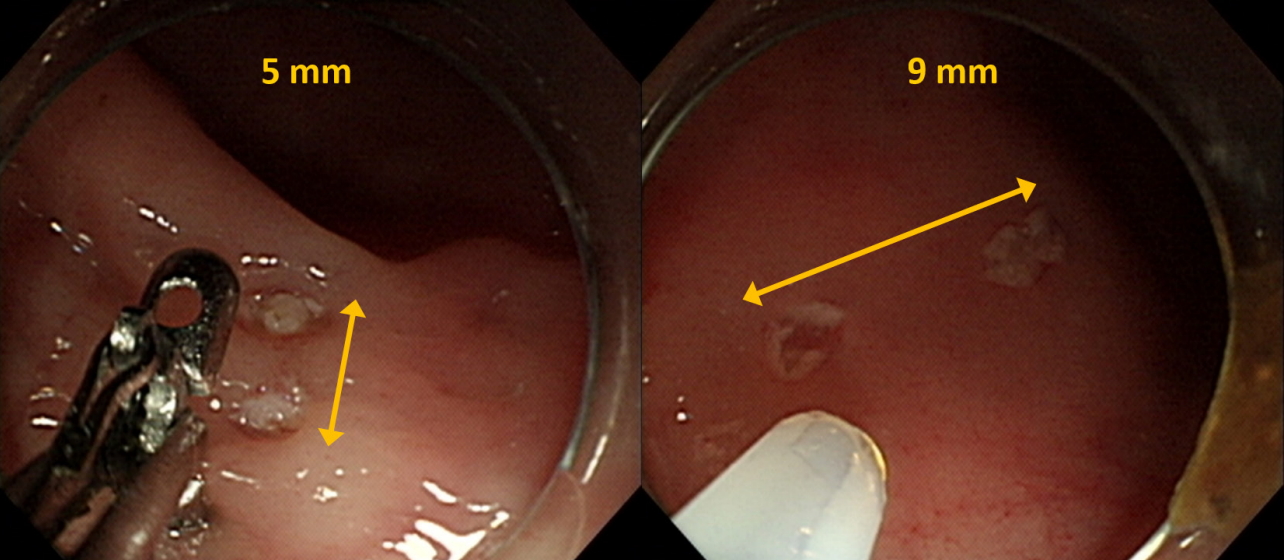
Dedicated Cold Snare vs. Traditional Snare for Polypectomy of Diminutive and Small Lesions in a Porcine Model: A Research Group for Endoscopic Instruments and Stents (REIS) Study

- Han Hee Lee, Bo-In Lee, Jung-Wook Kim, Hyun Lim, Si Hyung Lee, Jun-Hyung Cho, Yunho Jung, Kyoung Oh Kim, Chan Gyoo Kim, Kee Myung Lee, Jong-Jae Park, Myung-Gyu Choi, Hoon Jai Chun, Ho Gak Kim
- Clin Endosc 2021;54(3):390-396. Published online September 10, 2020
- DOI: https://doi.org/10.5946/ce.2020.096
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: The aim of this in vivo animal study was to evaluate the effectiveness and safety of dedicated cold snare (DCS) compared with those of traditional snare (TS) for cold snare polypectomy (CSP).
Methods
A total of 36 diminutive (5 mm) and 36 small (9 mm) pseudolesions were made by electrocoagulation in the colons of mini-pigs.
Results
For the diminutive lesions, there were no significant differences in technical success rate, procedure time, or complete resection rate between the DCS and TS groups; the rate of uneven resection margin in the DCS group was significantly lower than that of the TS group. For small lesions, technical success rate and complete resection rate were significantly higher in the DCS group than in the TS group (100% [18/18] vs. 55.6% [10/18], p=0.003; 94.4% [17/18] vs. 40% [4/10], p=0.006). In addition, the procedure duration was significantly shorter, and the rate of uneven resection margin was significantly lower in the DCS group (28.5 sec vs. 66.0 sec, p=0.006; 11.1% [2/18] vs. 100% [10/10], p<0.001). Two cases of perforation occurred in the DCS group. Multivariate analysis revealed that DCS use was independently associated with complete resection.
Conclusions
DCS is superior to TS in terms of technical success, complete resection, and reducing the duration of the procedure for CSP of small polyps. -
Citations
Citations to this article as recorded by- Comparison of complete resection rates in cold snare polypectomy using two different wire diameter snares: A randomized controlled study
Toshiki Horii, Sho Suzuki, Akihiro Sugita, Misa Yamauchi, Hisatomo Ikehara, Chika Kusano, Takuji Gotoda
Journal of Gastroenterology and Hepatology.2023; 38(5): 752. CrossRef - Comparison of the clinical efficacy of cold snare polypectomy using a thin-wire snare and thick-wire snare for small colorectal polyps
Hong Jin Yoon, Yunho Jung, Young Sin Cho, Il-Kwun Chung
International Journal of Gastrointestinal Intervention.2023; 12(4): 183. CrossRef - Big Issues on Small Polyps: An Ideal Device, But Is It for an Ideal Indication?
Yoji Takeuchi
Clinical Endoscopy.2021; 54(3): 297. CrossRef - Cold versus hot polypectomy/endoscopic mucosal resection–A review of current evidence
Raquel Ortigão, Jochen Weigt, Ahmed Afifi, Diogo Libânio
United European Gastroenterology Journal.2021; 9(8): 938. CrossRef
- Comparison of complete resection rates in cold snare polypectomy using two different wire diameter snares: A randomized controlled study
- 8,391 View
- 221 Download
- 4 Web of Science
- 4 Crossref

- Endoscopic Management of Iatrogenic Colon Perforation
- Yunho Jung
- Clin Endosc 2020;53(1):29-36. Published online July 3, 2019
- DOI: https://doi.org/10.5946/ce.2019.061

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Colon perforations are difficult to resolve because they occur unexpectedly and infrequently. If the clinician is unprepared or lacks training in dealing with perforations, the clinical prognosis will be affected, which can lead to legal issues. We describe here the proper approach to the management of perforations, including deciding on endoscopic or surgical treatment, selection of endoscopic devices, endoscopic closure procedures, and general management of perforations that occur during diagnostic or therapeutic colonoscopy.
-
Citations
Citations to this article as recorded by- Closure of gastrointestinal perforations using an endoloop system and a single-channel endoscope: description of a simple, reproducible, and standardized method
Flavius-Stefan Marin, Antoine Assaf, Paul Doumbe-Mandengue, Einas Abou Ali, Arthur Belle, Romain Coriat, Stanislas Chaussade
Surgical Endoscopy.2024;[Epub] CrossRef - Endoclip combined with colonic transendoscopic enteral tubing: a new approach for managing iatrogenic colonoscopy perforation
Xiaomeng Jiang, Chunhua Ni, Fatema Tabak, Yi Li, Faming Zhang
Surgical Endoscopy.2024; 38(3): 1647. CrossRef - Management of complications related to colorectal endoscopic submucosal dissection
Tae-Geun Gweon, Dong-Hoon Yang
Clinical Endoscopy.2023; 56(4): 423. CrossRef - GCA-Net: global context attention network for intestinal wall vascular segmentation
Sheng Li, Xueting Kong, Cheng Lu, Jinhui Zhu, Xiongxiong He, Ruibiao Fu
International Journal of Computer Assisted Radiology and Surgery.2022; 17(3): 569. CrossRef - Safety of Gastrointestinal Endoscopy in Korea: A Nationwide Survey and Population-Based Study
Yunho Jung, Jung-Wook Kim, Jong Pil Im, Yu Kyung Cho, Tae Hee Lee, Jae-Young Jang
Journal of Korean Medical Science.2022;[Epub] CrossRef - Clinical characteristics and outcome of iatrogenic colonic perforation related to diagnostic vs. therapeutic colonoscopy
Ra Ri Cha, Hee Jin Kim, Chang Min Lee, Jae Min Lee, Sang Soo Lee, Hyun Jin Cho, Chang Yoon Ha, Hyun Jin Kim, Ok-Jae Lee
Surgical Endoscopy.2022; 36(8): 5938. CrossRef - A Soft Sensor for Bleeding Detection in Colonoscopies
Arincheyan Gerald, Max McCandless, Avani Sheth, Hiroyuki Aihara, Sheila Russo
Advanced Intelligent Systems.2022;[Epub] CrossRef - Endoscopic Treatment of Iatrogenic Perforation of Sigmoid Diverticulum: A Case Report of Multidisciplinary Management
Giacomo Emanuele Maria Rizzo, Giuseppina Ferro, Giovanna Rizzo, Giovanni Di Carlo, Alessandro Cantone, Gaetano Giuseppe Di Vita, Carmelo Sciumè
Clinical Endoscopy.2022; 55(2): 292. CrossRef - Factors for conversion risk of colorectal endoscopic submucosal dissection: a multicenter study
Yuki Kamigaichi, Shiro Oka, Shinji Tanaka, Shinji Nagata, Masaki Kunihiro, Toshio Kuwai, Yuko Hiraga, Akira Furudoi, Seiji Onogawa, Hideharu Okanobu, Takeshi Mizumoto, Tomohiro Miwata, Shiro Okamoto, Kenichi Yoshimura, Kazuaki Chayama
Surgical Endoscopy.2022; 36(8): 5698. CrossRef - Iatrogenic colon perforation during colonoscopy, diagnosis/treatment, and follow-up processes: A single-center experience
Nihat Gülaydın, Raim İliaz, Atakan Özkan, A Hande Gökçe, Hanifi Önalan, Berrin Önalan, Aziz Arı
Turkish Journal of Surgery.2022; 38(3): 221. CrossRef - Endoscopic Closure of Iatrogenic Rectal Perforation Using the Tulip Bundle Technique
Francisco Pires, Ana Catarina Carvalho, Ricardo Araújo
ACG Case Reports Journal.2022; 9(12): e00898. CrossRef
- Closure of gastrointestinal perforations using an endoloop system and a single-channel endoscope: description of a simple, reproducible, and standardized method
- 9,585 View
- 489 Download
- 11 Web of Science
- 11 Crossref

- Management of Complications of Colorectal Submucosal Dissection
- Eun Ran Kim, Dong Kyung Chang
- Clin Endosc 2019;52(2):114-119. Published online March 29, 2019
- DOI: https://doi.org/10.5946/ce.2019.063
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic submucosal dissection (ESD) is a useful procedure for the treatment of superficial gastrointestinal neoplasm. Compared with endoscopic mucosal resection (EMR), ESD has several benefits, which include resectability of various difficult lesion, accurate histologic assessment of specimen, and lower recurrence rate. However, the risk of procedure- related complications is higher with ESD than with EMR. Moreover, because the colon has a thin wall and limited endoscopic maneuverability, ESD is considered a more challenging and risky procedure when performed in the colon than in the stomach. ESD-related complications are more likely to occur. The significant complications associated with ESD are bleeding, perforation, coagulation syndrome and stenosis, most of which can be treated and prevented by endoscopic intervention and preparation. Therefore, it is important to know how to occur and manage the ESD related complication.
-
Citations
Citations to this article as recorded by- Feasibility and safety of 0.6% sodium alginate in endoscopic submucosal dissection for colorectal neoplastic lesion: A pilot study
Hajime Nakamura, Rie Morita, Ryo Ito, Akira Sakurada, Natsumi Tomita, Yuya Hirata, Yusuke Kanari, Yuya Komatsu, Kunihiro Takanashi, Tomonori Anbo, Shinichi Katsuki
DEN Open.2024;[Epub] CrossRef - Endoscopic Submucosal Dissection for Resections Larger than 10 cm: Outcomes from a Portuguese Center
Raquel R. Mendes, Pedro Barreiro, André Mascarenhas, Ana Rita Franco, Liliana Carvalho, Cristina Chagas
GE - Portuguese Journal of Gastroenterology.2024; 31(1): 33. CrossRef - A Phase II Clinical Trial to Study the Safety of Triamcinolone after Endoscopic Radial Incision and Cutting Dilatation for Benign Stenosis of the Lower Gastrointestinal Tract: A Study Protocol
RINTARO MOROI, HISASHI SHIGA, KOTARO NOCHIOKA, HIROFUMI CHIBA, YUSUKE SHIMOYAMA, MOTOYUKI ONODERA, TAKEO NAITO, MASAKI TOSA, YOICHI KAKUTA, YUICHIRO SATO, SHOICHI KAYABA, SEICHI TAKAHASHI, SATOSHI MIYATA, YOSHITAKA KINOUCHI, ATSUSHI MASAMUNE
The Kurume Medical Journal.2024;[Epub] CrossRef - Meta-Analysis of Endoscopic Full-Thickness Resection Versus Endoscopic Submucosal Dissection for Complex Colorectal Lesions
Sahib Singh, Babu P. Mohan, Rakesh Vinayek, Sudhir Dutta, Dushyant S. Dahiya, Manesh K. Gangwani, Vishnu C. Suresh Kumar, Ganesh Aswath, Ishfaq Bhat, Sumant Inamdar, Neil Sharma, Douglas G. Adler
Journal of Clinical Gastroenterology.2024;[Epub] CrossRef - Management of giant colorectal polyps (≥3 cm) by endoscopic submucosal dissection (ESD) versus surgery: a propensity score–based analysis
Lo Hau Ching Michelle, Poon Chi Ming Michael
Surgical Practice.2024;[Epub] CrossRef - The role of endoluminal surgery in a colorectal surgical practice. A global view
Ilker Ozgur, Fevzi Cengiz
Seminars in Colon and Rectal Surgery.2024; 35(2): 101023. CrossRef - Endoscopic submucosal dissection for colorectal polyps: outcome determining factors
Chi Woo Samuel Chow, Tak Lit Derek Fung, Pak Tat Chan, Kam Hung Kwok
Surgical Endoscopy.2023; 37(2): 1293. CrossRef - A novel strategy to perform endoscopic full-thickness resection at the ileocecal valve and securing the orifice with a double-pigtail catheter
Moritz Meiborg, Nicolae-Catalin Mechie, Tobias Blasberg, Marie Weber, Edris Wedi
Endoscopy.2023; 55(S 01): E375. CrossRef - A novel strategy to perform endoscopic full-thickness resection at the ileocecal valve and securing the orifice with a double-pigtail catheter
Moritz Meiborg, Nicolae-Catalin Mechie, Tobias Blasberg, Marie Weber, Edris Wedi
Endoscopy.2023; 55(06): 583. CrossRef - Experience of surgical treatment in a granular cell tumor in the qscending colon: a case report
In-Kyeong Kim, Young-Tae Ju, Han-Gil Kim, Jin-Kwon Lee, Dong-Chul Kim, Jae-Myung Kim, Jin Kyu Cho, Ji-Ho Park, Ju-Yeon Kim, Chi-Young Jeong, Soon-Chan Hong, Seung-Jin Kwag
Annals of Coloproctology.2023; 39(3): 275. CrossRef - Management of complications related to colorectal endoscopic submucosal dissection
Tae-Geun Gweon, Dong-Hoon Yang
Clinical Endoscopy.2023; 56(4): 423. CrossRef - Endoscopic Mucosal Resection and Endoscopic Submucosal Dissection
Sumeyye Yilmaz, Emre Gorgun
Clinics in Colon and Rectal Surgery.2023;[Epub] CrossRef - Colorectal Endoscopic Submucosal Dissection: Performance of a Novel Hybrid-Technology Knife in an Animal Trial
Jérémie Jacques, Horst Neuhaus, Markus D. Enderle, Ulrich Biber, Walter Linzenbold, Martin Schenk, Kareem Khalaf, Alessandro Repici
Diagnostics.2023; 13(21): 3347. CrossRef - Delayed Perforation of Colorectal Endoscopic Submucosal Dissection Treated by Endoscopic Ultrasound-Guided Drainage
Koichi Hamada, Yoshiki Shiwa, Akira Kurita, Yukitoshi Todate, Yoshinori Horikawa, Kae Techigawara, Masafumi Ishikawa, Takayuki Nagahashi, Yuki Takeda, Daizo Fukushima, Noriyuki Nishino, Hideo Sakuma, Michitaka Honda
Case Reports in Gastroenterology.2023; 17(1): 155. CrossRef - Colonoscopic‐assisted laparoscopic wedge resection versus segmental colon resection for benign colonic polyps: a comparative cost analysis
Julia Hanevelt, Laura W. Leicher, Leon M. G. Moons, Frank P. Vleggaar, Jelle F. Huisman, Henderik L. van Westreenen, Wouter H. de Vos tot Nederveen Cappel
Colorectal Disease.2023; 25(11): 2147. CrossRef - Temperature profile and residual heat of monopolar laparoscopic and endoscopic dissection instruments
Franz Brinkmann, Ronny Hüttner, Philipp J. Mehner, Konrad Henkel, Georgi Paschew, Moritz Herzog, Nora Martens, Andreas Richter, Sebastian Hinz, Justus Groß, Clemens Schafmayer, Jochen Hampe, Alexander Hendricks, Frank Schwandner
Surgical Endoscopy.2022; 36(6): 4507. CrossRef - A pilot study investigating the safety and feasibility of endoscopic dilation using a radial incision and cutting technique for benign strictures of the small intestine: a study protocol
Rintaro Moroi, Hisashi Shiga, Kotaro Nochioka, Yusuke Shimoyama, Masatake Kuroha, Yoichi Kakuta, Yoshitaka Kinouchi, Atsushi Masamune
Pilot and Feasibility Studies.2022;[Epub] CrossRef - Applicability of endoscopic submucosal dissection after unsuccessful endoscopic mucosal resection in colorectal laterally spreading tumors: a single center experience
Abdullah Murat BUYRUK, Ayten LİVAOĞLU, Aydın AKTAŞ
Ege Tıp Dergisi.2022; 61(2): 151. CrossRef - One thousand endoscopic submucosal dissections. Experience of the national center
S.I. Achkasov, Yu.A. Shelygin, A.A. Likutov, D.A. Mtvralashvili, V.V. Veselov, O.A. Mainovskaya, M.A. Nagudov, S.V. Chernyshov
Khirurgiya. Zhurnal im. N.I. Pirogova.2022; (8): 5. CrossRef - Post-polypectomy syndrome—a rare complication in colonoscopy procedures: a case report
Julián A Romo, Jorge David Peña, Laura A López, Carlos Figueroa, Horacio Garzon, Andrea Recamán
Journal of Surgical Case Reports.2022;[Epub] CrossRef - Clinical outcomes of endoscopic submucosal dissection for colorectal neoplasms: A single-center experience in Southern Taiwan
Chen-Yu Ko, Chih-Chien Yao, Yu-Chi Li, Lung-Sheng Lu, Yeh-Pin Chou, Ming-Luen Hu, Yi-Chun Chiu, Seng-Kee Chuah, Wei-Chen Tai, Hsu-Heng Yen
PLOS ONE.2022; 17(10): e0275723. CrossRef - Safety and feasibility of same-day discharge after esophageal endoscopic submucosal dissection
Yuri Hanada, Kenneth K. Wang
Gastrointestinal Endoscopy.2021; 93(4): 853. CrossRef - Evaluations on laser ablation of ex vivo porcine stomach tissue for development of Ho:YAG-assisted endoscopic submucosal dissection (ESD)
Hanjae Pyo, Hyeonsoo Kim, Hyun Wook Kang
Lasers in Medical Science.2021; 36(7): 1437. CrossRef - Evaluation of improved bi-manual endoscopic resection using a customizable 3D-printed manipulator system designed for use with standard endoscopes: a feasibility study using a porcine ex-vivo model
Benjamin Walter, Yannick S. Krieger, Dirk Wilhelm, Hubertus Feussner, Tim C. Lueth, Alexander Meining
Endoscopy International Open.2021; 09(06): E881. CrossRef - A patient-like swine model of gastrointestinal fibrotic strictures for advancing therapeutics
Ling Li, Mohamad I. Itani, Kevan J. Salimian, Yue Li, Olaya Brewer Gutierrez, Haijie Hu, George Fayad, Jean A. Donet, Min Kyung Joo, Laura M. Ensign, Vivek Kumbhari, Florin M. Selaru
Scientific Reports.2021;[Epub] CrossRef - Review on colorectal endoscopic submucosal dissection focusing on the technical aspect
Tak Lit Derek Fung, Chi Woo Samuel Chow, Pak Tat Chan, Kam Hung Kwok
Surgical Endoscopy.2020; 34(9): 3766. CrossRef - Endovascular hemostasis for endoscopic procedure-related gastrointestinal bleeding
Minho Park, Jong Woo Kim, Ji Hoon Shin
International Journal of Gastrointestinal Intervention.2019; 8(3): 134. CrossRef
- Feasibility and safety of 0.6% sodium alginate in endoscopic submucosal dissection for colorectal neoplastic lesion: A pilot study
- 8,803 View
- 339 Download
- 27 Web of Science
- 27 Crossref

- Stomach Perforation Caused by Ingesting Liquid Nitrogen: A Case Report on the Effect of a Dangerous Snack
- Dong-Wook Kim
- Clin Endosc 2018;51(4):381-383. Published online March 5, 2018
- DOI: https://doi.org/10.5946/ce.2017.178
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - We report our experience with a case of stomach perforation after accidental ingestion of liquid nitrogen. A 13-year-old boy ate a snack at an amusement park and began to complain of sudden onset of severe abdominal pain with shortness of breath. It was determined that the snack he had ingested had been cooled with liquid nitrogen. A computed tomography scan of the abdomen and a chest X-ray showed a large volume of pneumoperitoneum. During surgery, a 4-cm perforation of the angularis incisura of the stomach was identified. Primary repair and omentopexy was performed. The patient was discharged without postoperative complications.
-
Citations
Citations to this article as recorded by- Gastric Perforation by Smoking Biscuits: Report of a Case
Abhishek Mishra, Ashirbad Panda, Laxminarayan Mohanty, Mohammad Ibrarullah
Indian Journal of Surgery.2023; 85(3): 630. CrossRef - Liquid Nitrogen Applied at Point of Sale
Victoria A. Pinilla Escobar, Caroline J. Granger, Anthony R. Hogan, Chad M. Thorson, Eduardo A. Perez, Juan E. Sola, Ann-Christina Brady
Pediatric Emergency Care.2022; 38(1): e85. CrossRef
- Gastric Perforation by Smoking Biscuits: Report of a Case
- 8,368 View
- 152 Download
- 2 Web of Science
- 2 Crossref

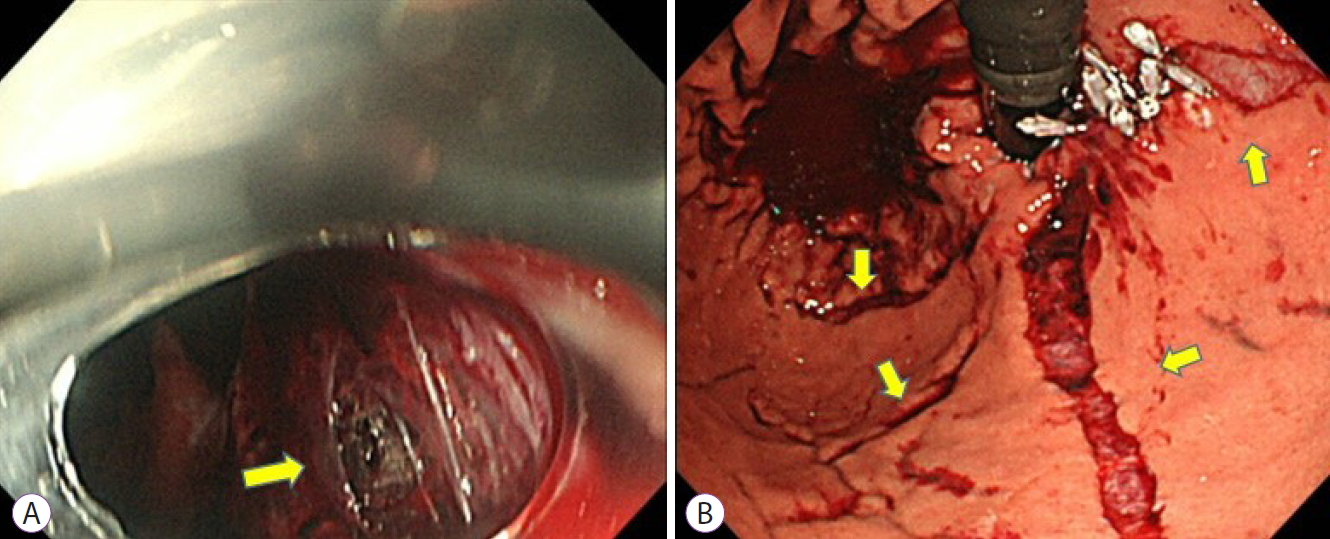
- An Unusual Case of Ovarian Carcinomatosis with Microscopic Tumor Embolism Leading to Rectal Ischemia and Perforation
- Man Hon Tang, Jason Lim, Inny Bushmani, Chee Yung Ng
- Clin Endosc 2018;51(3):294-298. Published online February 22, 2018
- DOI: https://doi.org/10.5946/ce.2017.152
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
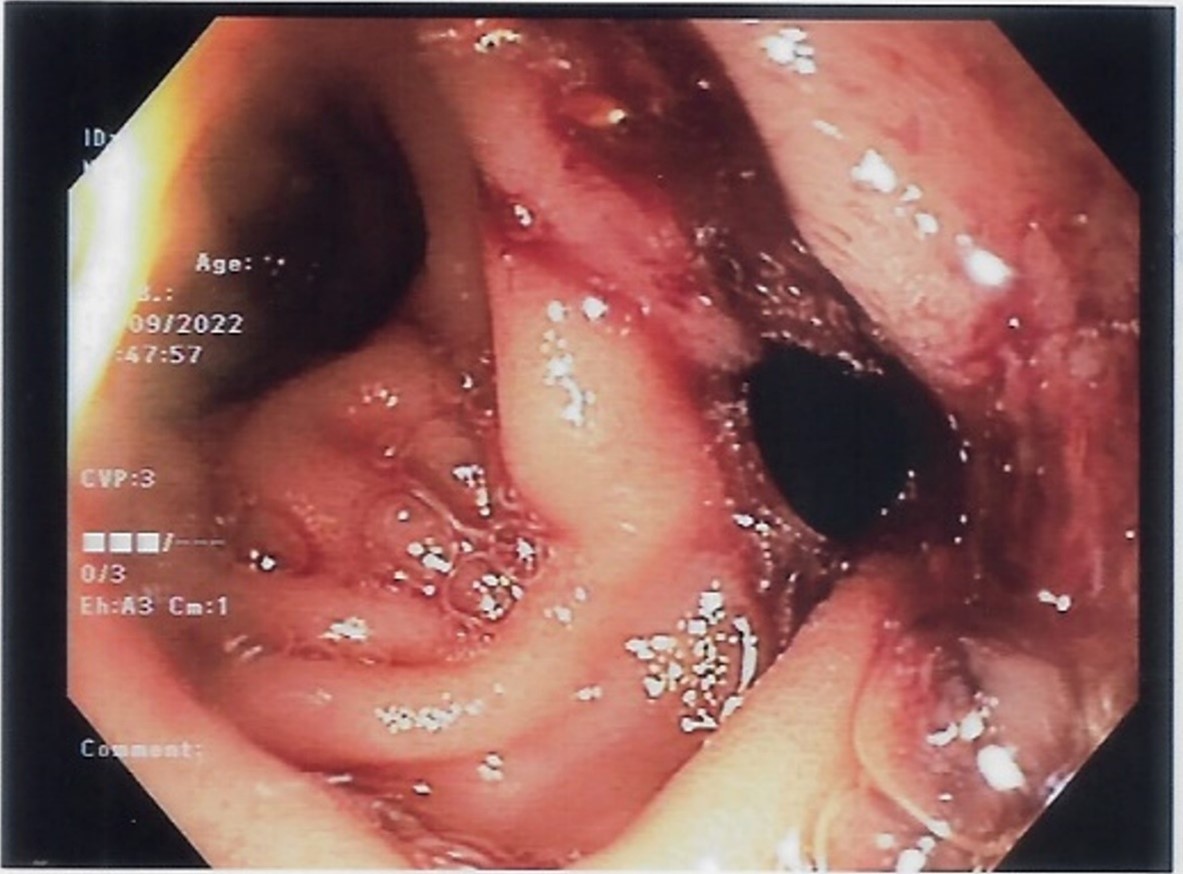
ePub - We present an unusual case of advanced ovarian carcinoma with postoperative complications of ischemia and perforation of the rectum as a result of tumor embolism. The interval progression from ischemia to infarction of the rectum was captured in repeated sigmoidoscopies. A brief discussion on tumor embolism and management of this case is also included.
-
Citations
Citations to this article as recorded by- Arterial Embolism in Malignancy: The Role of Surgery
Patrick Harnarayan, Shariful Islam, Vijay Naraynsingh
Therapeutics and Clinical Risk Management.2021; Volume 17: 635. CrossRef
- Arterial Embolism in Malignancy: The Role of Surgery
- 5,479 View
- 87 Download
- 1 Web of Science
- 1 Crossref

- Role of Endoscopy in the Management of Boerhaave Syndrome
- Juan Ignacio Tellechea, Jean-Michel Gonzalez, Pablo Miranda-García, Adrian Culetto, Xavier Benoit D’Journo, Pascal Alexandre Thomas, Marc Barthet
- Clin Endosc 2018;51(2):186-191. Published online September 20, 2017
- DOI: https://doi.org/10.5946/ce.2017.043
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Boerhaave syndrome (BS) is a spontaneous esophageal perforation which carries high mortality. Surgical treatment is well established, but the development of interventional endoscopy has proposed new therapies. We expose our experience in a Gastrointestinal and Endoscopy Unit. With a retrospective, observational, open-label, single center, consecutive case series. All patients diagnosed with BS who were managed in our center were included. Treated conservatively, endoscopically or surgically, according to their clinical condition and lesion presentation. Fourteen patients were included. Ten were treated with primary surgery. One conservatively. In total, 7/14 patients required an endoscopic treatment. All required metallic stents deployment, 3 cases over-the-scope-clips concomitantly and one case a novel technique an internal drain. 6/7 cases endoscopically treated achieved complete esophageal healing. In conclusion, endoscopy is an useful tool at all stages BS management: difficult diagnosis, primary treatment in selected patients and as salvage when surgery fails. With mortality rates and outcomes comparables to surgery.
-
Citations
Citations to this article as recorded by- The perilous consequences of bowel preparation: a case study with literature review of Boerhaave syndrome
Ruo-yu Gao, Xiao-lan Wei, Jin-feng Wu, Zhi-wei Zhou, Xi-qiu Yu
Frontiers in Medicine.2024;[Epub] CrossRef - A Conservative and Multidisciplinary Approach to Boerhaave Syndrome: A Case Report
Ricardo Ribeiro, Paulo Cardoso, Florissandra Santos
Cureus.2024;[Epub] CrossRef - Boerhaave's syndrome in a patient with achalasia: A rare case report
Pirouz Samidoust, Mohammad Taghi Ashoobi, Manouchehr Aghajanzadeh, Mohammad Sadegh Esmaeili Delshad, Mohammad Haghighi
International Journal of Surgery Case Reports.2023; 106: 108183. CrossRef - Boerhaave's syndrome: Better late than never – Delayed management using endoscopic over-the-scope clip
Arulprakash Sarangapani, TarunJ George, S Malathi
Gastroenterology, Hepatology and Endoscopy Practice.2023; 3(4): 167. CrossRef - Case of successful treatment of long spontaneous rupture of the esophagus
Ye. B. Topolnitskiy, N. A. Shefer, G. Ts. Dambayev
Issues of Reconstructive and Plastic Surgery.2022; 24(3-4): 82. CrossRef - Atypical chest pain: A case report of Boerhaave syndrome
Christelle Margot, Jérémy Desmercieres
International Journal of Case Reports and Images.2022; 13: 1. CrossRef - Boerhaave Syndrome: An Unexpected Complication of Diabetic Ketoacidosis
Brandon Wiggins, Fady Banno, Kyle T Knight, Ian Fladie, Justin Miller
Cureus.2022;[Epub] CrossRef - Conservative Management in a Patient with Recurrent Boerhaave Syndrome
Alexander J Kaye, Daniel Rim, Sushil Ahlawat
EMJ Gastroenterology.2022;[Epub] CrossRef - Minimally Invasive Approach in Boerhaave's Syndrome: Case Series and Systematic Review
Oliver Pickering, Philip H. Pucher, Henry De'Ath, Mahmoud Abuawwad, Jamie Kelly, Timothy J. Underwood, Fergus Noble, James P. Byrne
Journal of Laparoendoscopic & Advanced Surgical Techniques.2021; 31(11): 1254. CrossRef - Endoscopic negative pressure therapy (ENPT) of a spontaneous oesophageal rupture (Boerhaave’s syndrome) with peritonitis – a new treatment option
Gunnar Loske, Katrin Albers, Christian T. Mueller
Innovative Surgical Sciences.2021; 6(2): 81. CrossRef - Laparoscopic transhiatal suture and gastric valve as a safe and feasible treatment for Boerhaave’s syndrome: an Italian single center case series study
A. Veltri, J. Weindelmayer, L. Alberti, C. A. De Pasqual, M. Bencivenga, S. Giacopuzzi
World Journal of Emergency Surgery.2020;[Epub] CrossRef - Endoscopic management of Boerhaave�s syndrome
Eduardo Valdivielso Cortázar, Ignacio Couto W�rner, Pedro Alonso Aguirre
Revista Española de Enfermedades Digestivas.2019;[Epub] CrossRef - Esophageal emergencies: WSES guidelines
Mircea Chirica, Michael D. Kelly, Stefano Siboni, Alberto Aiolfi, Carlo Galdino Riva, Emanuele Asti, Davide Ferrari, Ari Leppäniemi, Richard P. G. ten Broek, Pierre Yves Brichon, Yoram Kluger, Gustavo Pereira Fraga, Gil Frey, Nelson Adami Andreollo, Feder
World Journal of Emergency Surgery.2019;[Epub] CrossRef - Over-the-scope-clip: Endoscopic treatment of Boerhaave syndrome
Mª Henar Núñez Rodríguez, Fátima Sánchez Martin, Rodrigo Nájera, Pilar Diez Redondo
Gastroenterología y Hepatología.2019; 42(9): 564. CrossRef - Boerhaave Syndrome Causing Bilateral Empyemas
Divya Chalikonda, Joseph Yoo, Drew Johnson, Christina Tofani
ACG Case Reports Journal.2019; 6(9): e00203. CrossRef - WITHDRAWN: Over-the-scope clip: Endoscopic treatment of Boerhaave syndrome
Mª Henar Núñez Rodríguez, Fátima Sánchez Martin, Rodrigo Nájera, Pilar Diez Redondo
Gastroenterología y Hepatología (English Edition).2019;[Epub] CrossRef - Over-the-scope-clip: Endoscopic treatment of Boerhaave syndrome
Mª Henar Núñez Rodríguez, Fátima Sánchez Martin, Rodrigo Nájera, Pilar Diez Redondo
Gastroenterología y Hepatología (English Edition).2019; 42(9): 564. CrossRef
- The perilous consequences of bowel preparation: a case study with literature review of Boerhaave syndrome
- 6,341 View
- 267 Download
- 15 Web of Science
- 17 Crossref

- Efficacy of the Over-the-Scope Clip System for Treatment of Gastrointestinal Fistulas, Leaks, and Perforations: A Korean Multi-Center Study
- Hang Lak Lee, Joo Young Cho, Jun-Hyung Cho, Jong Jae Park, Chan Gyoo Kim, Seong Hwan Kim, Joung-Ho Han
- Clin Endosc 2018;51(1):61-65. Published online August 29, 2017
- DOI: https://doi.org/10.5946/ce.2017.027
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Currently, a new over-the-scope clip (OTSC) system has been introduced. This system has been used for gastrointestinal perforations and fistulas in other countries. The aim of our study is to examine the therapeutic success rate of endoscopic treatment using the OTSC system in Korea.
Methods
This was a multicenter prospective study. A total of seven endoscopists at seven centers performed this procedure.
Results
A total of 19 patients were included, with gastrointestinal leakages from anastomosis sites, fistulas, or esophageal perforations due to Boerhaave’s syndrome. Among these, there were three gastrojejunostomy sites, three esophagojejunostomy sites, four esophagogastrostomy sites, one esophagocolonostomy site, one jejuno-jejunal site, two endoscopic full thickness resection site closures, one Boerhaave’s syndrome, two esophago-bronchial fistulas, one gastrocolonic fistula, and one colonopseudocyst fistula. The size of the leakage ranged from 5 to 30 mm. The median procedure time was 16 min. All cases were technically successful. Complete closure of the leak was achieved in 14 of 19 patients using OTSC alone.
Conclusions
The OTSC system is a safe and effective method for the management of gastrointestinal leakage, especially in cases of anastomotic leakage after surgery. -
Citations
Citations to this article as recorded by- Bariatric surgery and reproduction-implications for gynecology and obstetrics
Isaac A. Babarinsa, Mohammed Bashir, Husham AbdelRahman Ahmed, Badreldeen Ahmed, Justin C. Konje
Best Practice & Research Clinical Obstetrics & Gynaecology.2023; 90: 102382. CrossRef - Current status in endoscopic management of upper gastrointestinal perforations, leaks and fistulas
Shannon Melissa Chan, Kitty Kit Ying Auyeung, Siu Fung Lam, Philip Wai Yan Chiu, Anthony Yuen Bun Teoh
Digestive Endoscopy.2022; 34(1): 43. CrossRef - Endoscopic vacuum therapy (EVT) for acute esophageal perforation: Could it replace surgery?
Petros Stathopoulos, Malte Zumblick, Sabine Wächter, Leif Schiffmann, Thomas M. Gress, Detlef Bartsch, Guido Seitz, Ulrike W. Denzer
Endoscopy International Open.2022; 10(05): E686. CrossRef - Acquired Benign Tracheoesophageal Fistula
Hasnain S. Bawaadam, Matthew Russell, Yaron B. Gesthalter
Journal of Bronchology & Interventional Pulmonology.2022; 29(3): e38. CrossRef - Exclusión pilórica con dispositivo Ovesco (over-thescope) en caso de fístula yeyunal en obstrucción duodenal de etiología maligna
Raul Eduardo Pinilla Morales, Helena Facundo Navia, Elio Fabio Sánchez Cortés, Ivette C. Jiménez Lafourie, Álvaro Eduardo Sánchez Hernández, Luis Carlos Llorente Portillo
Revista colombiana de Gastroenterología.2022; 37(3): 320. CrossRef - Endoscopic management of leaks and fistulas after bariatric surgery: a systematic review and meta-analysis
Pawel Rogalski, Agnieszka Swidnicka-Siergiejko, Justyna Wasielica-Berger, Damian Zienkiewicz, Barbara Wieckowska, Eugeniusz Wroblewski, Andrzej Baniukiewicz, Magdalena Rogalska-Plonska, Grzegorz Siergiejko, Andrzej Dabrowski, Jaroslaw Daniluk
Surgical Endoscopy.2021; 35(3): 1067. CrossRef - Endoscopic management of gastro‐bronchial fistula following two‐stage esophagectomy using over‐the‐scope‐clip (OTSC): Case series
Chih Y. Tan, Htet A. Kyaw, Neda Farhangmehr, Cheuk‐Bong Tang, Naga V. Jayanthi
Advances in Digestive Medicine.2021; 8(2): 84. CrossRef - Over-the-Scope Clip Closure of Persistent Gastrocutaneous Fistula After Percutaneous Endoscopic Gastrostomy Tube Removal: A Report of Two Cases
Shigenori Masaki, Keishi Yamada
Cureus.2021;[Epub] CrossRef - Over‐the‐scope clip: a novel approach to the management of a colorectal anastomotic leak
Stephanie G. Jordan, Gregory J. Nolan
ANZ Journal of Surgery.2021; 91(11): 2534. CrossRef - Conservative treatment of patients with small bowel fistula
A.V. Vodyasov, D.M. Kopaliani, P.A. Yartsev, O.Kh. Kaloeva
Khirurgiya. Zhurnal im. N.I. Pirogova.2021; (4): 78. CrossRef - An Approach to Accelerate Healing and Shorten the Hospital Stay of Patients With Anastomotic Leakage After Esophagectomy: An Explorative Study of Systematic Endoscopic Intervention
LeQi Zhong, JiuDi Zhong, ZiHui Tan, YiTong Wei, XiaoDong Su, ZheSheng Wen, TieHua Rong, Yi Hu, KongJia Luo
Frontiers in Oncology.2021;[Epub] CrossRef - AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review
Jeffrey H. Lee, Prashant Kedia, Stavros N. Stavropoulos, David Carr-Locke
Clinical Gastroenterology and Hepatology.2021; 19(11): 2252. CrossRef - Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clinical Endoscopy.2021; 54(5): 633. CrossRef - Diagnostic challenge and surgical management of Boerhaave’s syndrome: a case series
Jiayue Wang, Degang Wang, Jianjiao Chen
Journal of Medical Case Reports.2021;[Epub] CrossRef - Over-the-scope clip management of non-acute, full-thickness gastrointestinal defects
David J. Morrell, Joshua S. Winder, Ansh Johri, Salvatore Docimo, Ryan M. Juza, Samantha R. Witte, Vamsi V. Alli, Eric M. Pauli
Surgical Endoscopy.2020; 34(6): 2690. CrossRef - Use of the Over the Scope Clip to Close Perforations and Fistulas
Panida Piyachaturawat, Parit Mekaroonkamol, Rungsun Rerknimitr
Gastrointestinal Endoscopy Clinics of North America.2020; 30(1): 25. CrossRef - Therapie der Ösophagusleckagen
Jutta Weber-Eibel
Journal für Gastroenterologische und Hepatologische Erkrankungen.2020; 18(1): 8. CrossRef - Successful Closure of a Benign Refractory Tracheoesophageal Fistula Using an Over-the-Scope Clip after Failed Esophageal Stent Placement and Surgical Management
Nonthalee Pausawasdi, Chotirot Angkurawaranon, Tanyaporn Chantarojanasiri, Arunchai Chang, Wanchai Wongkornrat, Somchai Leelakusolvong, Asada Methasate
Clinical Endoscopy.2020; 53(3): 361. CrossRef - Clinical efficacy of the over-the-scope clip device: A systematic review
Nicholas Bartell, Krystle Bittner, Vivek Kaul, Truptesh H Kothari, Shivangi Kothari
World Journal of Gastroenterology.2020; 26(24): 3495. CrossRef - Endoscopic devices and techniques for the management of bariatric surgical adverse events (with videos)
Allison R. Schulman, Rabindra R. Watson, Barham K. Abu Dayyeh, Manoop S. Bhutani, Vinay Chandrasekhara, Pichamol Jirapinyo, Kumar Krishnan, Nikhil A. Kumta, Joshua Melson, Rahul Pannala, Mansour A. Parsi, Guru Trikudanathan, Arvind J. Trindade, John T. Ma
Gastrointestinal Endoscopy.2020; 92(3): 492. CrossRef - Gastrointestinal tract injuries after thermal ablative therapies for hepatocellular carcinoma: A case report and review of the literature
Teresa Marzia Rogger, Andrea Michielan, Sandro Sferrazza, Cecilia Pravadelli, Luisa Moser, Flora Agugiaro, Giovanni Vettori, Sonia Seligmann, Elettra Merola, Marcello Maida, Francesco Antonio Ciarleglio, Alberto Brolese, Giovanni de Pretis
World Journal of Gastroenterology.2020; 26(35): 5375. CrossRef - Over‐the‐scope clip system: A review of 1517 cases over 9 years
Hideki Kobara, Hirohito Mori, Noriko Nishiyama, Shintaro Fujihara, Keiichi Okano, Yasuyuki Suzuki, Tsutomu Masaki
Journal of Gastroenterology and Hepatology.2019; 34(1): 22. CrossRef - Recent advancements in the minimally invasive management of esophageal perforation, leaks, and fistulae
Shirin Siddiqi, Dean P. Schraufnagel, Hafiz Umair Siddiqui, Michael J. Javorski, Adam Mace, Abdulrhman S. Elnaggar, Haytham Elgharably, Patrick R. Vargo, Robert Steffen, Saad M. Hasan, Siva Raja
Expert Review of Medical Devices.2019; 16(3): 197. CrossRef - Diagnosis and endoscopic treatment of esophageal leakage: a systematic review
Bram D. Vermeulen, Peter D. Siersema
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 58. CrossRef - Management of esophagojejunal anastomosis leakage after total gastrectomy
Pablo Priego, Pietro Giordano, Marta Cuadrado, Araceli Ballestero, Julio Galindo, Eduardo Lobo
European Surgery.2018; 50(6): 262. CrossRef - Endoluminal Therapies for Esophageal Perforations and Leaks
Jeffrey R. Watkins, Alexander S. Farivar
Thoracic Surgery Clinics.2018; 28(4): 541. CrossRef - Esophageal leaks: I thought that glue was not effective
Ignacio Fernández-Urién, Juan Vila
Endoscopy International Open.2018; 06(09): E1100. CrossRef
- Bariatric surgery and reproduction-implications for gynecology and obstetrics
- 7,581 View
- 324 Download
- 26 Web of Science
- 27 Crossref

-
Gastric Perforation Caused by an Intragastric Balloon: Endoscopic Findings

- In Kyung Yoo, Hoon Jai Chun, Yoon Tae Jeen
- Clin Endosc 2017;50(6):602-604. Published online May 18, 2017
- DOI: https://doi.org/10.5946/ce.2017.015
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Intragastric balloon (IGB) insertion has been most frequently used in the West as an effective endoscopic treatment for morbid obesity, in practice. Recently, there is a growing number of cases requiring IGB deployment for obesity treatment in Korea. One of the reported complications of IGB use is gastric perforation. A 47-year-old woman was admitted to the hospital with mild symptoms, 7 weeks after having an IGB placed. Esophagogastroduodenoscopy was performed and gastric ulcer perforation was observed in the ulcer base, where food particles were impacted. Laparoscopic primary repair was done successfully. This was a case of gastric perforation, secondary to poor compliance with a proton-pump inhibitor (PPI). PPI and Helicobacter pylori eradication are important for ulcer prevention following IGB deployment.
-
Citations
Citations to this article as recorded by- Common, Less Common, and Unexpected Complications after Bariatric Surgery: A Pictorial Essay
Francesca Iacobellis, Giuseppina Dell’Aversano Orabona, Antonio Brillantino, Marco Di Serafino, Alessandro Rengo, Paola Crivelli, Luigia Romano, Mariano Scaglione
Diagnostics.2022; 12(11): 2637. CrossRef - Endoscopic bariatric therapies for obesity: a review
Dominic A Staudenmann, Zhixian Sui, Payal Saxena, Arthur J Kaffes, George Marinos, Vivek Kumbhari, Patrick Aepli, Adrian Sartoretto
Medical Journal of Australia.2021; 215(4): 183. CrossRef - Stomach Volume Assessment Using Three-dimensional Computed Tomography Gastrography for Bariatric Treatment
Seung Han Kim, Bora Keum, Hyuk Soon Choi, Eun Sun Kim, Yeon Seok Seo, Yoon Tae Jeen, Hong Sik Lee, Hoon Jai Chun, Soon Ho Um, Chang Duck Kim
Obesity Surgery.2020; 30(2): 401. CrossRef - COMBINED ENDOSCOPY AND LAPAROSCOPIC APPROACH OF A GASTRIC PERFORATION DUE TO INTRAGASTRIC BALLOON INSERTION
Guillermo Perez Aguado, José Carlos Cabrera Marrero, Lucía Jiménez-Ruano
Revista Española de Enfermedades Digestivas.2020;[Epub] CrossRef - The role of silent helicobacter pylori infection in intragastric ulcers induced by balloon insertion used for management of obesity
Tamer Haydara, Ahmed M. Kabel, Ayman M. Elsaka
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 116. CrossRef - Review article: Postoperative bariatric patients in the emergency department: Review of surgical complications for the emergency physician
Ryan Windish, Jason Wong
Emergency Medicine Australasia.2019; 31(3): 309. CrossRef - Currently Available Non-Balloon Devices
Hang Lak Lee
Clinical Endoscopy.2018; 51(5): 416. CrossRef - Gastric Ulceration and Bleeding with Hemodynamic Instability Caused by an Intragastric Balloon for Weight Loss
Larrite Reed, Hawa Edriss, Kenneth Nugent
Clinical Endoscopy.2018; 51(6): 584. CrossRef - Exclusively endoscopic approach to treating gastric perforation caused by an intragastric balloon: case series and literature review
Sérgio Alexandre Barrichello Junior, Igor Braga Ribeiro, Ricardo José Fittipaldi-Fernandez, Ana Carolina Hoff, Diogo Turiani Hourneaux de Moura, Mauricio Kazuyoshi Minata, Thiago Ferreira de Souza, Manoel dos Passos Galvão Neto, Eduardo Guimarães Hourneau
Endoscopy International Open.2018; 06(11): E1322. CrossRef
- Common, Less Common, and Unexpected Complications after Bariatric Surgery: A Pictorial Essay
- 6,334 View
- 171 Download
- 10 Web of Science
- 9 Crossref

- Pneumothorax after Colonoscopy – A Review of Literature
- Ajay Gupta, Hammad Zaidi, Khalid Habib
- Clin Endosc 2017;50(5):446-450. Published online April 10, 2017
- DOI: https://doi.org/10.5946/ce.2016.118
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The purpose of this study was to determine the anatomical aspects, mechanisms, risk factors and appropriate management of development of pneumothorax during a routine colonoscopy. A systematic search of the literature (MEDLINE, Embase and Google Scholar) revealed 21 individually documented patients of pneumothorax following a colonoscopy, published till December 2015. One additional patient treated at our center was added. A pooled analysis of these 22 patients was performed including patient characteristics, indication of colonoscopy, any added procedure, presenting symptoms,risk factors and treatment given. The review suggested that various risk factors may be female gender, therapeutic interventions, difficult colonoscopy and underlying bowel pathology. Diagnosis of this condition requires a high index of suspicion and treatment should be tailored to individual needs.
-
Citations
Citations to this article as recorded by- A CASE OF PNEUMOTHORAX AFTER COLONOSCOPIC POLYPECTOMY: A CASE REPORT AND REVIEW OF THE LITERATURE
Mehmet Ası Oktan, Cenk Emre Meral, Atakan Arslan, Yasemin Kaya, Batuhan Hazer, Bahattin Tuncalı
Gastroenterology Nursing.2024; 47(3): 217. CrossRef - Bilateral pneumothorax and pneumomediastinum during colonoscopy in a patient with intestinal Behcet’s disease: A case report
Tong Mu, Hua Feng
World Journal of Clinical Cases.2022; 10(6): 2030. CrossRef - Pneumothorax
Nai-Chien Huan, Calvin Sidhu, Rajesh Thomas
Clinics in Chest Medicine.2021; 42(4): 711. CrossRef - A rare phenomenon creating dilemma for the surgeon: Pneumoperitoneum after colonoscopy
Ferhat Ferhatoglu, Ilker Filiz
Sanamed.2018; 13(2): 171. CrossRef
- A CASE OF PNEUMOTHORAX AFTER COLONOSCOPIC POLYPECTOMY: A CASE REPORT AND REVIEW OF THE LITERATURE
- 6,999 View
- 136 Download
- 5 Web of Science
- 4 Crossref

- Endoscopic Management of Gastrointestinal Leaks and Perforation with Polyglycolic Acid Sheets
- Sojung Han, Hyunsoo Chung, Jun Chul Park, Sung Kwan Shin, Sang Kil Lee, Yong Chan Lee
- Clin Endosc 2017;50(3):293-296. Published online March 8, 2017
- DOI: https://doi.org/10.5946/ce.2016.121
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Gastrointestinal (GI) leakage, fistulae, and perforations can be serious and life threatening. There has been a paradigm shift in the management approach of these conditions, from surgical to conservative, including endoscopic management. Here, we report two cases of endoscopic closure of a GI fistula and perforation using polyglycolic acid (PGA) sheets with fibrin glue. The first case is of an anastomotic leak detected after subtotal gastrectomy with gastroduodenostomy. After failed application of endoclips, a PGA sheet was applied, and the fistula was successfully closed. The second case was of a 15-mm large perforated gastric ulcer, which was also successfully closed with a PGA sheet. This is the first case report that PGA sheet was used for the treatment of overt perforation. The outcome of these cases suggest that endoscopic closure using PGA sheets can be considered as a useful alternative for the management of GI leakage, fistulae, and perforations.
-
Citations
Citations to this article as recorded by- A Randomized Controlled Trial of Fibrin Glue to Prevent Bleeding After Gastric Endoscopic Submucosal Dissection
Hyun Deok Lee, Eunwoo Lee, Sang Gyun Kim, Cheol Min Shin, Jun Chul Park, Kee Don Choi, Seokyung Hahn, Soo-Jeong Cho
American Journal of Gastroenterology.2023; 118(5): 892. CrossRef - Large anastomotic leak: endoscopic treatment using combined fibrin glue and polyglycolic acid (PGA) sheets
Soo In Choi, Ji Young Park
BMJ Case Reports.2021; 14(8): e240188. CrossRef - The treatment for refractory rectovaginal fistula after low anterior resection with estriol, polyglycolic acid sheets and primary closure: A case report
Masatsugu Hiraki, Toshiya Tanaka, Tadayuki Kanai, Takuya Shimamura, Osamu Ikeda, Makio Yasunaga, Shinichi Ogata, Kenji Kitahara
International Journal of Surgery Case Reports.2020; 75: 483. CrossRef - Endoscopic management of esophagorespiratory fistulas
Brian Larson, Douglas G. Adler
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 65. CrossRef - Endoscopic closure of an anastomo-cutaneous fistula: Filling and shielding using polyglycolic acid sheets and fibrin glue with easily deliverable technique
Hideaki Kawabata, Yuji Okazaki, Naonori Inoue, Yukino Kawakatsu, Misuzu Hitomi, Masatoshi Miyata, Shigehiro Motoi
Endoscopy International Open.2018; 06(08): E994. CrossRef - Successful Endoscopic Closure Using Polyglycolic Acid Sheets with Fibrin Glue for Nonhealing Duodenal Ulcer with Perforation after Proton Beam Therapy of Liver Tumor
Ko Watanabe, Takuto Hikichi, Jun Nakamura, Minami Hashimoto, Tadayuki Takagi, Rei Suzuki, Mitsuru Sugimoto, Naoki Konno, Mika Takasumi, Yuki Sato, Hiroki Irie, Takashi Kimura, Akira Kenjo, Shigeru Marubashi, Katsutoshi Obara, Hiromasa Ohira
Case Reports in Gastroenterology.2018; 12(3): 679. CrossRef
- A Randomized Controlled Trial of Fibrin Glue to Prevent Bleeding After Gastric Endoscopic Submucosal Dissection
- 7,809 View
- 222 Download
- 7 Web of Science
- 6 Crossref

- Repair of an Endoscopic Retrograde Cholangiopancreatography-Related Large Duodenal Perforation Using Double Endoscopic Band Ligation and Endoclipping
- Keunmo Kim, Eun Bee Kim, Yong Hyeok Choi, Youngmin Oh, Joung-Ho Han, Seon Mee Park
- Clin Endosc 2017;50(2):202-205. Published online September 13, 2016
- DOI: https://doi.org/10.5946/ce.2016.112
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic closure techniques have been introduced for the repair of duodenal wall perforations that occur during endoscopic retrograde cholangiopancreatography (ERCP). We report a case of successful repair of a large duodenal wall perforation by using double endoscopic band ligation (EBL) and an endoclip. Lateral duodenal wall perforation occurred during ERCP in a 93-year-old woman with acute calculous cholangitis. We switched to a forward endoscope that had a transparent band apparatus. A 2.0-cm ovalshaped perforation was found at the lateral duodenal wall. We repaired the perforation by sequentially performing double EBL and endoclipping. The first EBL was performed at the proximal edge of the perforation orifice, and two-thirds of the perforation were repaired. The second EBL, which also included the contents covered under the first EBL, repaired the defect almost completely. Finally, to account for the possible presence of a residual perforation, an endoclip was applied at the distal end of the perforation. The detection and closure of the perforation were completed within 10 minutes. We suggest that double EBL is an effective method for closure.
-
Citations
Citations to this article as recorded by- Endoscopic treatment of ERCP-related duodenal perforation
Nicole Evans, James L. Buxbaum
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 83. CrossRef
- Endoscopic treatment of ERCP-related duodenal perforation
- 8,832 View
- 183 Download
- 2 Web of Science
- 1 Crossref

- Endoscopic Closure for Full-Thickness Gastrointestinal Defects: Available Applications and Emerging Innovations
- Nobuyoshi Takeshita, Khek Yu Ho
- Clin Endosc 2016;49(5):438-443. Published online August 30, 2016
- DOI: https://doi.org/10.5946/ce.2016.104
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Full-thickness gastrointestinal defects such as perforation, anastomotic leak, and fistula are severe conditions caused by various types of pathologies. They are more likely to require intensive care and a long hospital stay and have high rates of morbidity and mortality. After intentional full-thickness opening of hollow organs for natural orifice transluminal endoscopic surgery, safe and secure closure is urgently required. The currently available advanced endoscopic closing techniques have a major role in the treatment of full-thickness gastrointestinal defects. Appropriate usage of these techniques requires taking into account their advantages and limitations during practical application. We reviewed the available endoscopic modalities, including endoscopic clips, stents, vacuum-assisted closure, gap filling, and suturing devices, discussed their advantages and limitations when treating full-thickness gastrointestinal defects, and explored emerging innovations, including a novel endoluminal surgical platform for versatile suturing and a cell-laden scaffold for effective gap filling. Although these emerging technologies still require further pre-clinical and clinical trials to assess their feasibility and efficacy, the available modalities may be replaced and refined by these new techniques in the near future.
-
Citations
Citations to this article as recorded by- Injectable nanoengineered adhesive hydrogel for treating enterocutaneous fistulas
Natan Roberto de Barros, Ankit Gangrade, Ahmad Rashad, RunRun Chen, Fatemeh Zehtabi, Menekse Ermis, Natashya Falcone, Reihaneh Haghniaz, Safoora Khosravi, Alejandro Gomez, Shuyi Huang, Marvin Mecwan, Danial Khorsandi, Junmin Lee, Yangzhi Zhu, Bingbing Li,
Acta Biomaterialia.2024; 173: 231. CrossRef - Novel external reinforcement device for gastrointestinal anastomosis in an experimental study
Hiro Hasegawa, Nobuyoshi Takeshita, Woogi Hyon, Suong-Hyu Hyon, Masaaki Ito
BMC Surgery.2023;[Epub] CrossRef - Colon Sparing Endoscopic Full-Thickness Resection for Advanced Colorectal Lesions: Is It Time for Global Adoption?
Zhong-Wei Wu, Chao-Hui Ding, Yao-Dong Song, Zong-Chao Cui, Xiu-Qian Bi, Bo Cheng
Frontiers in Oncology.2022;[Epub] CrossRef - The Etiology, Diagnosis, and Management of Esophageal Perforation
Puja Gaur Khaitan, Amber Famiglietti, Thomas J. Watson
Journal of Gastrointestinal Surgery.2022; 26(12): 2606. CrossRef - Advanced Endoscopic Tools
Eleanor C. Fung
Digestive Disease Interventions.2021; 05(02): 194. CrossRef - Repair of upper-GI fistulas and anastomotic leakage by the use of endoluminal vacuum-assisted closure
Andrew Watson, Tobias Zuchelli
VideoGIE.2019; 4(1): 40. CrossRef - Effect of poly(3-hydroxyalkanoates) as natural polymers on mesenchymal stem cells
Vera Voinova, Garina Bonartseva, Anton Bonartsev
World J Stem Cells.2019; 11(10): 764. CrossRef - Endoscopic Closure of Gastrointestinal Fistulae and Leaks
Jaehoon Cho, Ara B. Sahakian
Gastrointestinal Endoscopy Clinics of North America.2018; 28(2): 233. CrossRef - Non-visible colovesical fistula located by cystoscopy and successfully managed with the novel Padlock® device for endoscopic closure
Benito Velayos, L. Del Olmo, L. Merino, M. Valsero, J. M. González
International Journal of Colorectal Disease.2018; 33(6): 827. CrossRef - Poly(3-hydroxybutyrate) and Human Microbiota (Review)
A. P. Bonartsev, V. V. Voinova, G. A. Bonartseva
Applied Biochemistry and Microbiology.2018; 54(6): 547. CrossRef - Hepatocolic fistula managed with a novel Padlock® device for endoscopic closure
Benito Velayos Jiménez, Lourdes Del Olmo Martínez, Carmen Alonso Martín, Javier Trueba Arguiñarena, José Manuel González Hernández
Revista Española de Enfermedades Digestivas.2017;[Epub] CrossRef - Anastomotic leaks in gastrointestinal surgery and their prevention
Tomasz Banasiewicz, Adam Dziki, Paweł Lampe, Zbigniew Lorenc, Marek Szczepkowski, Jacek Zieliński, Grzegorz Wallner
Polish Journal of Surgery.2017; 89(2): 49. CrossRef
- Injectable nanoengineered adhesive hydrogel for treating enterocutaneous fistulas
- 9,454 View
- 189 Download
- 11 Web of Science
- 12 Crossref

- Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations
- Seon Mee Park
- Clin Endosc 2016;49(4):376-382. Published online July 29, 2016
- DOI: https://doi.org/10.5946/ce.2016.088
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The management strategy for endoscopic retrograde cholangiopancreatography-related duodenal perforation can be determined based on the site and extent of injury, the patient’s condition, and time to diagnosis. Most cases of perivaterian or bile duct perforation can be managed with a biliary stent or nasobiliary drainage. Duodenal wall perforations had been treated with immediate surgical repair. However, with the development of endoscopic devices and techniques, endoscopic closure has been reported to be a safe and effective treatment that uses through-the-scope clips, ligation band, fibrin glue, endoclips and endoloops, an over-the-scope clipping device, suturing devices, covering luminal stents, and open-pore film drainage. Endoscopic therapy could be instituted in selected patients in whom perforation was identified early or during the procedure. Early diagnosis, proper conservative management, and effective endoscopic closure are required for favorable outcomes of non-surgical management. If endoscopic treatment fails, or in the cases of clinical deterioration, prompt surgical management should be considered.
-
Citations
Citations to this article as recorded by- ERCP-induced perforation: review and revisit after half a century
Abdel Rahman A. A. Al Manasra, Zaid Mesmar, Tarek Manasreh, Hanan M . Hammouri, Anas Husein, Khaled Jadallah, Mohammed Bani hani, Niazy Abu Farsakh, Shatha K. Shahwan, Doaa Al-qaoud, Jehad Fataftah
F1000Research.2024; 12: 612. CrossRef - ERCP-induced perforation: review and revisit after half a century
Abdel Rahman A. A. Al Manasra, Zaid Mesmar, Tarek Manasreh, Hanan M . Hammouri, Anas Husein, Khaled Jadallah, Mohammed Bani hani, Niazy Abu Farsakh, Shatha K. Shahwan, Doaa Al-qaoud, Jehad Fataftah
F1000Research.2023; 12: 612. CrossRef - Fully covered self-expandable metal stent for intraprocedural or late-diagnosed Type-II endoscopic retrograde cholangiopancreatography-related perforations
Osman Bozbiyik, Bartu Cetin, Tufan Gumus, Fatih Tekin, Alper Uguz
BMC Gastroenterology.2022;[Epub] CrossRef - Clinical analysis of 45 cases of perforation were identified during endoscopic retrograde cholangiopancreatography procedure
Yin-Shui Miao, Yuan-Yuan Li, Bo-Wen Cheng, Yan-Fang Zhan, Sheng Zeng, Xiao-Jiang Zhou, You-Xiang Chen, Nong-Hua Lv, Guo-Hua Li
Frontiers in Medicine.2022;[Epub] CrossRef - AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review
Jeffrey H. Lee, Prashant Kedia, Stavros N. Stavropoulos, David Carr-Locke
Clinical Gastroenterology and Hepatology.2021; 19(11): 2252. CrossRef - Evaluation of complications after endoscopic retrograde cholangiopancreatography using a short type double balloon endoscope in patients with altered gastrointestinal anatomy: a single‐center retrospective study of 1,576 procedures
Mitsuo Tokuhara, Masaaki Shimatani, Toshiyuki Mitsuyama, Masataka Masuda, Takashi Ito, Sachi Miyamoto, Norimasa Fukata, Hideaki Miyoshi, Tsukasa Ikeura, Makoto Takaoka, Katsuyasu Kouda, Kazuichi Okazaki
Journal of Gastroenterology and Hepatology.2020; 35(8): 1387. CrossRef - Retracted: Endoscopic Treatment of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
Ding Shi, Jian feng Yang, Yong pan Liu
Journal of Laparoendoscopic & Advanced Surgical Techniques.2019; 29(3): 385. CrossRef - Duodenal perforation after the cutting an ENPD tube in a patient with pancreatic cancer and acute suppurative pancreatic ductitis
Akihisa OHNO, Nao FUJIMORI, Kazuhide MATSUMOTO, Katsuhito TERAMATSU, Yu TAKAMATSU, Masami MIKI, Takehiro TAKAOKA, Takamasa OONO
Suizo.2019; 34(1): 30. CrossRef - Endoscopic treatment of ERCP-related duodenal perforation
Nicole Evans, James L. Buxbaum
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 83. CrossRef - Endoscopic management of iatrogenic gastrointestinal perforations
Kan Wang, Jihao Shi, Linna Ye
Laparoscopic, Endoscopic and Robotic Surgery.2019; 2(2): 41. CrossRef - The Management of Duodenal Perforation: Change Over Time. A Case Series and Literature Review
Amit Nehra, Rajesh Godara
Hellenic Journal of Surgery.2019; 91(5-6): 159. CrossRef - A Case of Unresolved and Worsening Retroperitoneal Abscess
Raghav Bansal, Mohamed Barakat, Soohwan Chun, Sonam Rosberger, Joel Baum, Melik Tiba
Case Reports in Gastrointestinal Medicine.2018; 2018: 1. CrossRef - On the feasibility of the computational modelling of the endoluminal vacuum-assisted closure of an oesophageal anastomotic leakage
Ester Comellas, Facundo J. Bellomo, Iván Rosales, Luis F. del Castillo, Ricardo Sánchez, Pau Turon, Sergio Oller
Royal Society Open Science.2018; 5(2): 171289. CrossRef - Endoscopic retrograde cholangiopancreatography complications: Techniques to reduce risk and management strategies
Paul R. Tarnasky, Prashant Kedia
International Journal of Gastrointestinal Intervention.2017; 6(1): 37. CrossRef - A systematic review of the management and outcome of ERCP related duodenal perforations using a standardized classification system
Roberto Cirocchi, Michael Denis Kelly, Ewen A. Griffiths, Renata Tabola, Massimo Sartelli, Luigi Carlini, Stefania Ghersi, Salomone Di Saverio
The Surgeon.2017; 15(6): 379. CrossRef
- ERCP-induced perforation: review and revisit after half a century
- 11,730 View
- 295 Download
- 14 Web of Science
- 15 Crossref

- Delayed Severe Hemobilia after Endoscopic Biliary Plastic Stent Insertion
- Sung Hak Lee, Seung Goun Hong, Kyoung yong Lee, Pyung Kang Park, Sung Du Kim, Mahn Lee, Dong Wook Yu, Man Yong Hong
- Clin Endosc 2016;49(3):303-307. Published online March 25, 2016
- DOI: https://doi.org/10.5946/ce.2015.081
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Hemobilia is a rare gastrointestinal bleeding, usually caused by injury to the bile duct. Hemobilia after endoscopic retrograde cholangiopancreatography (ERCP) is generally self-limiting and patients will spontaneously recover, but some severe and fatal hemorrhages have been reported. ERCP-related bowel or bile duct perforation should be managed promptly, according to the type of injury and the status of the patient. We recently experienced a case of late-onset severe hemobilia in which the patient recovered after endoscopic biliary stent insertion. The problem was attributable to ERCP-related bile duct perforation during stone removal, approximately 5 weeks prior to the hemorrhagic episode. The removal of the stent was performed 10 days before the onset of hemobilia. The bleeding was successfully treated by two sessions of transarterial coil embolization.
-
Citations
Citations to this article as recorded by- A rare incidence of a hepatic artery pseudoaneurysm following plastic biliary stent insertion
Toshihiko Motohara, Kensuke Yamamura, Shigenori Ueno, Hiroshi Takeno, Yasunori Nagayama, Eri Oda, Ryuichi Karashima, Nobuyuki Ozaki, Toshiro Masuda, Toru Beppu
Clinical Journal of Gastroenterology.2024; 17(2): 352. CrossRef - A Study on the Spectrum of Imaging Findings of Post-ERCP-Specific Complications: A Retrospective Descriptive Study
Ruchira Mukherji, Manoj Gopinath
Indian Journal of Radiology and Imaging.2024;[Epub] CrossRef - Delayed Hemobilia Caused by Penetration of Biliary Plastic Stent into Portal Vein
Jinhyong Kang, Yang Tae Park, Hyo Jung Kim, Jae Seon Kim
The Korean Journal of Pancreas and Biliary Tract.2022; 27(3): 135. CrossRef - Complications of endoscopic retrograde cholangiopancreatography: an imaging review
Dinesh Manoharan, Deep Narayan Srivastava, Arun Kumar Gupta, Kumble Seetharama Madhusudhan
Abdominal Radiology.2019; 44(6): 2205. CrossRef - Recurrent Bleeding from a Hepatic Artery Pseudoaneurysm after Biliary Stent Placement
Kenji Yamauchi, Daisuke Uchida, Hironari Kato, Hiroyuki Okada
Internal Medicine.2018; 57(1): 49. CrossRef - Transcatheter arterial embolization for iatrogenic bleeding after endoscopic ultrasound-guided pancreaticobiliary drainage
N.J. Lee, J.H. Shin, S.S. Lee, D.H. Park, S.K. Lee, H.-K. Yoon
Diagnostic and Interventional Imaging.2018; 99(11): 717. CrossRef - Hemobilia due to arteriobiliary fistula complicating ERCP for residual bile duct stone in a case of Mirizzi syndrome
Surendrakumar Mathur, Vinaykumar Thapar, Vasudev Chowda
Annals of Hepato-Biliary-Pancreatic Surgery.2017; 21(2): 88. CrossRef
- A rare incidence of a hepatic artery pseudoaneurysm following plastic biliary stent insertion
- 9,338 View
- 76 Download
- 8 Web of Science
- 7 Crossref

- Optimal Methods for the Management of Iatrogenic Colonoscopic Perforation
- Dae Kyu Shin, Sun Young Shin, Chi Young Park, Sun Mi Jin, Yang Hyun Cho, Won Hee Kim, Chang-Il Kwon, Kwang Hyun Ko, Ki Baik Hahm, Pil Won Park, Jong Woo Kim, Sung Pyo Hong
- Clin Endosc 2016;49(3):282-288. Published online February 18, 2016
- DOI: https://doi.org/10.5946/ce.2015.046
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Colonoscopic perforations have been managed with exploratory laparotomy, and have resulted in some morbidity and mortality. Recently, laparoscopic surgery is commonly performed for this purpose. The aim of this study was to compare the outcomes of several management strategies for iatrogenic colonoscopic perforations.
Methods
We retrospectively reviewed the medical records of patients who had been treated for colonoscopic perforation between January 2004 and April 2013 at CHA Bundang Medical Center in Korea.
Results
A total of 41 patients with colonoscopic perforation were enrolled. Twenty patients underwent conservative management with a success rate of 90%. Surgical management was performed in 23 patients including two patients who were converted to surgical management after the failure of the initial conservative management. Among 14 patients who underwent surgery at 8 hours after the perforation, there was no considerable difference in adverse outcomes between the laparotomy group and the laparoscopic surgery group. The medical costs and claim rate were 1.45 and 1.87 times greater in the exploratory laparotomy group, respectively.
Conclusions
Conservative management of colonoscopic perforation could be an option for patients without overt symptoms of peritonitis or with a small defect size. If surgical management is required, laparoscopic surgery may be considered as the initial procedure even with a delayed diagnosis. -
Citations
Citations to this article as recorded by- Surgical repair of endoscopy-induced colonic perforations: a case-matched study of short-term morbidity and mortality
Fady DANIEL, Suha JABAK, Mohammad HOSNI, Hani TAMIM, Aurelie MAILHAC, Ayman ALRAZIM, Noura AL-ALI, Robert CHURCH, Mohammad KHALIFE, Shafik SIDANI, Faek JAMALI
Minerva Surgery.2024;[Epub] CrossRef - Laparoscopic versus open surgery for colonoscopic perforation: A systematic review and meta-analysis
Wu Zhong, Chuanyuan Liu, Chuanfa Fang, Lei Zhang, Xianping He, Weiquan Zhu, Xueyun Guan
Medicine.2023; 102(24): e34057. CrossRef - Elastography for Pediatric Chronic Liver Disease
Giovanna Ferraioli, Richard G. Barr, Jonathan R. Dillman
Journal of Ultrasound in Medicine.2021; 40(5): 909. CrossRef - Clinical outcomes of laparoscopic versus open surgery for repairing colonoscopic perforation: a multicenter study
Jae Seok Lee, Jeong Yeon Kim, Byung Mo Kang, Sang Nam Yoon, Jun Ho Park, Bo Young Oh, Jong Wan Kim
Surgery Today.2021; 51(2): 285. CrossRef - The analysis of outcomes of surgical management for colonoscopic perforations: A 16-years experiences at a single institution
Dae Ro Lim, Jung Kul Kuk, Taehyung Kim, Eung Jin Shin
Asian Journal of Surgery.2020; 43(5): 577. CrossRef - Multicenter retrospective evaluation of ileocecocolic perforations associated with diagnostic lower gastrointestinal endoscopy in dogs and cats
Vanessa L. Woolhead, Jacqueline C. Whittemore, Sarah A. Stewart
Journal of Veterinary Internal Medicine.2020; 34(2): 684. CrossRef - Endoscopic Management of the Ascending Colon Perforation Secondary to a Rare-Earth Magnets Ingestion in a Pediatric Patient
Sandra Mabel Camacho-Gomez, James Meredith Noel, Robert Adam Noel
ACG Case Reports Journal.2020; 7(8): e00436. CrossRef - Pseudo‐obstruction But a Real Perforation
AORN Journal.2019; 109(1): 142. CrossRef - Treatment of colonoscopic perforation: outcomes from a major single tertiary institution
Carolyn R. Chew, Justin M. C. Yeung, Ian G. Faragher
ANZ Journal of Surgery.2019; 89(5): 546. CrossRef - Management of colonoscopic perforations: A systematic review
Alexander T. Hawkins, Kenneth W. Sharp, Molly M. Ford, Roberta L. Muldoon, M. Benjamin Hopkins, Timothy M. Geiger
The American Journal of Surgery.2018; 215(4): 712. CrossRef - 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation
Nicola de’Angelis, Salomone Di Saverio, Osvaldo Chiara, Massimo Sartelli, Aleix Martínez-Pérez, Franca Patrizi, Dieter G. Weber, Luca Ansaloni, Walter Biffl, Offir Ben-Ishay, Miklosh Bala, Francesco Brunetti, Federica Gaiani, Solafah Abdalla, Aurelien Ami
World Journal of Emergency Surgery.2018;[Epub] CrossRef - Management Outcomes of Colonoscopic Perforations Are Affected by the General Condition of the Patients
Jae Ho Park, Kyung Jong Kim
Annals of Coloproctology.2018; 34(1): 16. CrossRef - Abdominal Sepsis: An Update
Mircea Gabriel Mureșan, Ioan Alexandru Balmoș, Iudita Badea, Ario Santini
The Journal of Critical Care Medicine.2018; 4(4): 120. CrossRef - Laparoscopic vs. open surgery for the treatment of iatrogenic colonoscopic perforations: a systematic review and meta-analysis
Aleix Martínez-Pérez, Nicola de’Angelis, Francesco Brunetti, Yann Le Baleur, Carmen Payá-Llorente, Riccardo Memeo, Federica Gaiani, Marco Manfredi, Paschalis Gavriilidis, Giorgio Nervi, Federico Coccolini, Aurelien Amiot, Iradj Sobhani, Fausto Catena, Gia
World Journal of Emergency Surgery.2017;[Epub] CrossRef - Urinary Bladder Injury During Colonoscopy Without Colon Perforation
Jung Wook Suh, Jun Won Min, Hwan Namgung, Dong-Guk Park
Annals of Coloproctology.2017; 33(3): 112. CrossRef - The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections
Massimo Sartelli, Alain Chichom-Mefire, Francesco M. Labricciosa, Timothy Hardcastle, Fikri M. Abu-Zidan, Abdulrashid K. Adesunkanmi, Luca Ansaloni, Miklosh Bala, Zsolt J. Balogh, Marcelo A. Beltrán, Offir Ben-Ishay, Walter L. Biffl, Arianna Birindelli, M
World Journal of Emergency Surgery.2017;[Epub] CrossRef - How Should We Manage Iatrogenic Perforation Caused by Colonoscopy?
Eun Sun Kim
Clinical Endoscopy.2016; 49(3): 214. CrossRef
- Surgical repair of endoscopy-induced colonic perforations: a case-matched study of short-term morbidity and mortality
- 8,245 View
- 151 Download
- 20 Web of Science
- 17 Crossref

- Unexpected Delayed Colon Perforation after the Endoscopic Submucosal Dissection with Snaring of a Laterally Spreading Tumor
- Young Bo Ko, Jeong-Mi Lee, Wan Soo Kim, Min Seob Kwak, Ji Wan Lee, Dong Yeol Shin, Dong-Hoon Yang, Jeong-Sik Byeon
- Clin Endosc 2015;48(6):570-575. Published online November 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.6.570
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Colonic perforation may occur as a complication of diagnostic and therapeutic colonoscopy. The risk factors for perforation after colorectal endoscopic submucosal dissection (ESD) include an inexperienced endoscopist, a large tumor size, and submucosal fibrosis. The mechanisms of perforation include unintended endoscopic resection/dissection and severe thermal injury. Here, we report a case of colon perforation that occurred after ESD with snaring of a laterally spreading tumor. The perforation was completely unexpected because there were no colorectal ESD-associated risk factors for perforation, deep dissection, or severe coagulation injury in our patient.
-
Citations
Citations to this article as recorded by- Tri-Axial Force Sensor in a Soft Catheter Using Fiber Bragg Gratings for Endoscopic Submucosal Dissection
Ramzi Ben Hassen, Arnaud Lemmers, Alain Delchambre
IEEE Sensors Journal.2023; 23(20): 24626. CrossRef - Factors for conversion risk of colorectal endoscopic submucosal dissection: a multicenter study
Yuki Kamigaichi, Shiro Oka, Shinji Tanaka, Shinji Nagata, Masaki Kunihiro, Toshio Kuwai, Yuko Hiraga, Akira Furudoi, Seiji Onogawa, Hideharu Okanobu, Takeshi Mizumoto, Tomohiro Miwata, Shiro Okamoto, Kenichi Yoshimura, Kazuaki Chayama
Surgical Endoscopy.2022; 36(8): 5698. CrossRef - Life on a knife edge: the optimal approach to the management of perforations during endoscopic submucosal dissection (ESD)
Shria Kumar, Young Hoon Youn, Jeffrey H. Lee
Expert Review of Gastroenterology & Hepatology.2020; 14(10): 965. CrossRef - Delayed perforation after endoscopic resection of a colonic laterally spreading tumor: A case report and literature review
Ge-Yu-Jia Zhou, Jin-Long Hu, Sheng Wang, Nan Ge, Xiang Liu, Guo-Xin Wang, Si-Yu Sun, Jin-Tao Guo
World Journal of Clinical Cases.2020; 8(16): 3608. CrossRef - Predicting and managing complications following colonoscopy: risk factors and management of advanced interventional endoscopy with a focus on colorectal ESD
Hiroyuki Takamaru, Rina Goto, Masayoshi Yamada, Taku Sakamoto, Takahisa Matsuda, Yutaka Saito
Expert Review of Medical Devices.2020; 17(9): 929. CrossRef - Cost Analysis of Endoscopic Submucosal Dissection for the Treatment of Colorectal Lesions in China
Ning Cui, Yu Zhao, Honggang Yu
BioMed Research International.2019; 2019: 1. CrossRef - Delayed perforation after endoscopic submucosal dissection for mucosal colon cancer: A conservatively treated case
Kazumasa Kawashima, Takuto Hikichi, Tatsuo Fujiwara, Naohiko Gunji, Jun Nakamura, Ko Watanabe, Kyoko Katakura, Hiromasa Ohira
FUKUSHIMA JOURNAL OF MEDICAL SCIENCE.2018; 64(3): 157. CrossRef
- Tri-Axial Force Sensor in a Soft Catheter Using Fiber Bragg Gratings for Endoscopic Submucosal Dissection
- 11,051 View
- 97 Download
- 7 Web of Science
- 7 Crossref

- Endoluminal Closure of Colon Perforation with Endoscopic Band Ligation: Technical Feasibility and Safety in an In Vivo Canine Model
- Joung-Ho Han, Myounghwan Kim, Tae Hoon Lee, Hyun Kim, Yunho Jung, Seon Mee Park, Heebok Chae, Seijin Youn, Ji Yun Shin, In-Kwang Lee, Tae Soo Lee, Seok Hwa Choi
- Clin Endosc 2015;48(6):534-541. Published online November 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.6.534
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic band ligation (EBL) is an accepted method in the management of variceal bleeding; however, there is little evidence on the safety and feasibility of EBL for the closure of bowel perforation. In this study, we aimed to evaluate the technical feasibility and efficacy of EBL in iatrogenic colon perforation by using a canine model.
Methods
We established an iatrogenic colon perforation model by using seven beagle dogs. Longitudinal 1.5- to 1.7-cm colon perforations were created with a needle knife and an insulated-tip knife, and the perforation was subsequently closed with EBL. During a 2-week follow-up period, the animals were carefully monitored and then euthanized for pathologic examination.
Results
The EBL of iatrogenic colon perforations was successful in all dogs. The mean procedure time for EBL closure with one to three bands was 191.7 seconds, and there were no immediate complications. One animal was euthanized after 3 days because of peritonitis. There were no clinical and laboratory features of sepsis or peritonitis in the remaining six animals. On necropsy, we did not find any fecal peritonitis, pericolonic abscess formation, or transmural dehiscence at the perforation site. Histopathology demonstrated inflamed granulation tissue and scar lesions replaced by fibrosis.
Conclusions
EBL might be a feasible and safe method for the management of iatrogenic colon perforations in an in vivo model. -
Citations
Citations to this article as recorded by- Endoscopic Management of Iatrogenic Colon Perforation
Yunho Jung
Clinical Endoscopy.2020; 53(1): 29. CrossRef - Endoluminal closure of an unrecognized penetrating stab wound of the duodenum with endoscopic band ligation: A case report
Dae Hoon Kim, Hanlim Choi, Ki Bae Kim, Hyo Yung Yun, Joung-Ho Han
World Journal of Clinical Cases.2019; 7(20): 3271. CrossRef - Endoscopic management of iatrogenic gastrointestinal perforations
Kan Wang, Jihao Shi, Linna Ye
Laparoscopic, Endoscopic and Robotic Surgery.2019; 2(2): 41. CrossRef - Endoscopic Band Ligation Is Able to Close Perforations Caused by Colonoscopy: A Porcine Model Study
Yidong Yang, Xianyi Lin, Siwei Tan, Xiaoli Huang, Zijun Xie, Xuan Xu, Yiming Lei, Bin Wu
Gastroenterology Research and Practice.2018; 2018: 1. CrossRef
- Endoscopic Management of Iatrogenic Colon Perforation
- 10,369 View
- 79 Download
- 3 Web of Science
- 4 Crossref

- Efficacy and Safety of Endoscopic Papillary Balloon Dilation Using Cap-Fitted Forward-Viewing Endoscope in Patients Who Underwent Billroth II Gastrectomy
- Jong Soon Jang, Seungho Lee, Hee Seung Lee, Myeong Ho Yeon, Joung-Ho Han, Soon Man Yoon, Hee Bok Chae, Sei Jin Youn, Seon Mee Park
- Clin Endosc 2015;48(5):421-427. Published online September 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.5.421
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Endoscopic exploration of the common bile duct (CBD) is difficult and dangerous in patients with Billroth II gastrectomy (B-II). Endoscopic papillary balloon dilation (EPBD) via a cap-fitted forward-viewing endoscope has been reported to be an effective and safe procedure. We analyzed the technical success and complications of EPBD in patients who underwent B-II.
Methods Thirty-six consecutive patients with B-II were enrolled from among 2,378 patients who had undergone endoscopic retrograde cholangiopancreatography in a single institute in the last 4 years. The EPBD procedure was carried out using a cap-fitted forward-viewing endoscope with 8-mm balloon catheters for 60 seconds. We analyzed the rates of CBD exploration, technical success, and complications.
Results Afferent loop intubation was performed in all patients and selective cannulation of the bile duct was performed in 32 patients (88.9%). Complications such as transient hypoxia were observed in two patients (5.6%) and perforation, in three patients (9.7%). The perforation sites were ductal injury in two patients and one patient showed retroperitoneal air alone without symptoms. Three patients manifested different clinical courses of severe acute pancreatitis and peritonitis, transient abdominal pain, and retroperitoneal air alone. The condition of one patient improved with surgery and that of the other two patients, with conservative management.
Conclusions Patients with perforation during EPBD in B-II showed different clinical courses. Tailored treatment strategies are necessary for improving the clinical outcomes.
-
Citations
Citations to this article as recorded by- A “One Accessory and One Guidewire-in-One Channel” Technique in a Patient with Billroth II Anastomosis
Kook Hyun Kim, Sung Bum Kim, Tae Nyeun Kim
Clinical Endoscopy.2021; 54(1): 139. CrossRef - Which scope is appropriate for endoscopic retrograde cholangiopancreatography after Billroth II reconstruction: An esophagogastroduodenoscope or a colonoscope?
Mitsuru Sugimoto, Tadayuki Takagi, Rei Suzuki, Naoki Konno, Hiroyuki Asama, Yuki Sato, Hiroki Irie, Ko Watanabe, Jun Nakamura, Hitomi Kikuchi, Mika Takasumi, Minami Hashimoto, Tsunetaka Kato, Takuto Hikichi, Hiromasa Ohira
World Journal of Gastrointestinal Endoscopy.2020; 12(8): 220. CrossRef - Recent advances in endoscopic retrograde cholangiopancreatography in Billroth II gastrectomy patients: A systematic review
Tae Young Park, Tae Jun Song
World Journal of Gastroenterology.2019; 25(24): 3091. CrossRef - Challenges of endoscopic retrograde cholangiopancreatography in patients with Billroth II gastrointestinal anatomy: A review article
Rabbinu Rangga Pribadi, Abdul Aziz Rani, Murdani Abdullah
Journal of Digestive Diseases.2019; 20(12): 631. CrossRef - Endoscopic retrograde cholangiopancreatography in Billroth II gastrectomy patients: Outcomes and potential factors affecting technical failure
Jia-Su Li, Duo-Wu Zou, Zhen-Dong Jin, Jie Chen, Xin-Gang Shi, Zhao-Shen Li, Feng Liu
Saudi Journal of Gastroenterology.2019; 25(6): 355. CrossRef - Endoscopic Management of Difficult Bile Duct Stones
Murad Aburajab, Kulwinder Dua
Current Gastroenterology Reports.2018;[Epub] CrossRef - Forward-viewing endoscope for ERCP in patients with Billroth II gastrectomy: a systematic review and meta-analysis
Tae Young Park, Chang Seok Bang, Sang Hyeon Choi, Young Joo Yang, Suk Pyo Shin, Ki Tae Suk, Gwang Ho Baik, Dong Joon Kim, Jai Hoon Yoon
Surgical Endoscopy.2018; 32(11): 4598. CrossRef - Self-expandable metal stents for choledocholithiasis in Billroth II gastrectomy patients
Min-Gui Han, Eunae Cho, Chang-Hwan Park, Chung-Hwan Jun, Seon-Young Park
Hepatobiliary & Pancreatic Diseases International.2018; 17(6): 546. CrossRef - Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations
Seon Mee Park
Clinical Endoscopy.2016; 49(4): 376. CrossRef
- A “One Accessory and One Guidewire-in-One Channel” Technique in a Patient with Billroth II Anastomosis
- 8,954 View
- 77 Download
- 10 Web of Science
- 9 Crossref

- Delayed Perforation Occurring after Endoscopic Submucosal Dissection for Early Gastric Cancer
- Soo Hoon Kang, Kyungho Lee, Hyun Woo Lee, Ga Eun Park, Yun Soo Hong, Byung-Hoon Min
- Clin Endosc 2015;48(3):251-255. Published online May 29, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.3.251
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Delayed perforation is a very rare complication of endoscopic submucosal dissection (ESD), with a reported incidence of 0.1% to 0.45%. Few reports exist on the clinical features and outcomes of delayed perforation after ESD, and it is unclear whether the optimal management strategy is emergency surgery or endoscopic closure with conservative treatment. Here, we report two cases of delayed perforation occurring after ESD for early gastric cancer. In both cases, lesions were located in the antrum, and tumor depths were confined to the mucosal layer. Total procedure times for ESD were 25 and 45 minutes, respectively. Because delayed perforation may be associated with excessive thermal damage and necrosis of the muscle layer, treatment with emergency surgery should be used instead of conservative management in cases of delayed perforation after ESD.
-
Citations
Citations to this article as recorded by- Delayed Perforation Occurring after Gastric Endoscopic Submucosal Dissection: Clinical Features and Management Strategy
Tae-Se Kim, Byung-Hoon Min, Yang Won Min, Hyuk Lee, Poong-Lyul Rhee, Jae J. Kim, Jun Haeng Lee
Gut and Liver.2024; 18(1): 40. CrossRef - Complications of endoscopic resection in the upper gastrointestinal tract
Takeshi Uozumi, Seiichiro Abe, Mai Ego Makiguchi, Satoru Nonaka, Haruhisa Suzuki, Shigetaka Yoshinaga, Yutaka Saito
Clinical Endoscopy.2023; 56(4): 409. CrossRef - Novel image enhancement technology that helps find bleeding points during endoscopic submucosal dissection of gastric neoplasms
Kohei Funasaka, Ryoji Miyahara, Noriyuki Horiguchi, Takafumi Omori, Hayato Osaki, Dai Yoshida, Hyuga Yamada, Keishi Koyama, Mitsuo Nagasaka, Yoshiyuki Nakagawa, Senju Hashimoto, Tomoyuki Shibata, Yoshiki Hirooka
Journal of Gastroenterology and Hepatology.2022; 37(10): 1955. CrossRef - Clinical practice guideline for endoscopic resection of early gastrointestinal cancer
Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong
Intestinal Research.2021; 19(2): 127. CrossRef - Endoscopic Resection of Gastric Cancer
Ga Hee Kim, Hwoon-Yong Jung
Gastrointestinal Endoscopy Clinics of North America.2021; 31(3): 563. CrossRef - Clinical Practice Guideline for Endoscopic Resection of Early Gastrointestinal Cancer
Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong
Clinical Endoscopy.2020; 53(2): 142. CrossRef - Clinical Practice Guideline for Endoscopic Resection of Early Gastrointestinal Cancer
Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong
The Korean Journal of Gastroenterology.2020; 75(5): 264. CrossRef - Clinical Practice Guideline for Endoscopic Resection of Early Gastrointestinal Cancer
Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2020; 20(2): 117. CrossRef - Delayed perforation occurring on the 24th day after endoscopic submucosal dissection for early gastric cancer
Satoru Homma, Kazuaki Tokodai, Minami Watanabe, Kai Takaya, Eiji Hashizume
Clinical Journal of Gastroenterology.2017; 10(2): 124. CrossRef - Clinical Factors of Delayed Perforation after Endoscopic Submucosal Dissection for Gastric Neoplasms
Yoshinobu Yamamoto, Hogara Nishisaki, Hideki Sakai, Nagahiro Tokuyama, Hiroaki Sawai, Aya Sakai, Takuya Mimura, Saeko Kushida, Hidetaka Tsumura, Takeshi Sakamoto, Ikuya Miki, Masahiro Tsuda, Hideto Inokuchi
Gastroenterology Research and Practice.2017; 2017: 1. CrossRef - Management and associated factors of delayed perforation after gastric endoscopic submucosal dissection
Haruhisa Suzuki
World Journal of Gastroenterology.2015; 21(44): 12635. CrossRef
- Delayed Perforation Occurring after Gastric Endoscopic Submucosal Dissection: Clinical Features and Management Strategy
- 8,732 View
- 103 Download
- 9 Web of Science
- 11 Crossref

- Esophgeal Perforation and Bilateral Empyema Following Endoscopic EsophyX Transoral Incisionless Fundoplication
- Hawa Edriss, Amal El-Bakush, Kenneth Nugent
- Clin Endosc 2014;47(6):560-563. Published online November 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.6.560
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Transoral incisionless fundoplication (TIF) has been used for endoscopic treatment of gastroesophageal reflux disease (GERD). TIF using the EsophyX device system (EndoGastric Solutions) was designed to create a full-thickness valve at the gastroesophageal junction through the insertion of multiple fasteners; it improves GERD, reduces proton pump inhibitor use, and improves quality of life. Although TIF is effective in select patients, a significant subset of patients undergoing TIF develop persistent or recurrent GERD symptoms and may need antireflux surgery to control the GERD symptoms. We now report a 48-year-old man with chronic GERD unresponsive to medical management. He underwent TIF complicated by esophageal perforation and developed mediastinitis, left pneumothorax, bilateral pleural effusions, and acute respiratory failure. He required chest tube placement and bilateral decortication for treatment of nonresolving empyemas. Additional postmarketing studies are required to assess the safety, efficacy, and clinical outcomes of this novel procedure, and patients undergoing this procedure need close postprocedural follow-up.
-
Citations
Citations to this article as recorded by- Efficacy and patient satisfaction of single-session transoral incisionless fundoplication and laparoscopic hernia repair
Catherine Gisi, Kelly Wang, Farhaad Khan, Sonya Reicher, Linda Hou, Clark Fuller, James Sattler, Viktor Eysselein
Surgical Endoscopy.2021; 35(2): 921. CrossRef - Endoscopic Management of Gastroesophageal Reflux Disease
Colin G. DeLong, Joshua S. Winder
Digestive Disease Interventions.2021; 05(02): 199. CrossRef - Long-term Outcomes of Patients Receiving a Magnetic Sphincter Augmentation Device for Gastroesophageal Reflux
Robert A. Ganz, Steven A. Edmundowicz, Paul A. Taiganides, John C. Lipham, C. Daniel Smith, Kenneth R. DeVault, Santiago Horgan, Garth Jacobsen, James D. Luketich, Christopher C. Smith, Steven C. Schlack-Haerer, Shanu N. Kothari, Christy M. Dunst, Thomas
Clinical Gastroenterology and Hepatology.2016; 14(5): 671. CrossRef
- Efficacy and patient satisfaction of single-session transoral incisionless fundoplication and laparoscopic hernia repair
- 6,969 View
- 57 Download
- 3 Web of Science
- 3 Crossref

- Gastric Endoscopic Submucosal Dissection Is Safe for Day Patients
- Sun Young Ahn, Sun Ik Jang, Dong Wook Lee, Seong Woo Jeon
- Clin Endosc 2014;47(6):538-543. Published online November 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.6.538
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Although the advantages of endoscopic submucosal dissection (ESD) are well established, there are important limitations that relate to its higher cost and higher rate of complications compared with endoscopic mucosal resection. This study assessed the therapeutic safety and efficacy of ESD in the treatment of small gastric dysplasia and early gastric cancer (EGC) located within the antrum in an outpatient setting, and it compared the results with those from patients admitted to hospital for ESD treatment.
Methods This study was a retrospective analysis of a prospectively maintained database. We reviewed consecutive patients with EGC or gastric dysplasia who underwent ESD between October 2007 and May 2008. The lesions were smaller than 2 cm and were located in the antrum. We analyzed 105 lesions in 105 patients. The patients were assigned to two groups according to each patient's preference.
Results The overall rates of complete resection were 98.1% in the inpatients group and 94.3% in the outpatients group. Immediate bleeding occurred in four inpatients, which included one patient in the outpatient group. Delayed bleeding occurred in one inpatient within 24 hours of the procedure. Macroperforations did not occur in either group. A microperforation was found in one outpatient.
Conclusions The safety and efficacy of ESD used to treat small gastric tumors in the antrum in an outpatient setting appeared to be similar to the safety and efficacy of ESD used to treat patients who were admitted to the hospital.
-
Citations
Citations to this article as recorded by- Pathology and Clinical Relevance of Gastric Epithelial Dysplasia
Tetsuo Ushiku, Gregory Y. Lauwers
Gastroenterology Clinics of North America.2024; 53(1): 39. CrossRef - Outpatient hybrid endoscopic submucosal dissection with SOUTEN for early gastric cancer, followed by endoscopic suturing of the mucosal defect: A case report
Renma Ito, Kazuhiro Miwa, Yutaka Matano
World Journal of Gastrointestinal Surgery.2023; 15(8): 1831. CrossRef - Endoscopic submucosal dissection of gastrointestinal lesions on an outpatient basis
Francisco Baldaque-Silva, Margarida Marques, Ana Patrícia Andrade, Nuno Sousa, Joanne Lopes, Fatima Carneiro, Guilherme Macedo
United European Gastroenterology Journal.2019; 7(2): 326. CrossRef - Risk factors for bleeding after gastric endoscopic submucosal dissection: a systematic review and meta-analysis
Diogo Libânio, Mariana Nuno Costa, Pedro Pimentel-Nunes, Mário Dinis-Ribeiro
Gastrointestinal Endoscopy.2016; 84(4): 572. CrossRef - Gastric dysplasia: update and practical approach
Namrata Setia, Gregory Y. Lauwers
Diagnostic Histopathology.2015; 21(8): 312. CrossRef - Endoscopic Submucosal Dissection for Gastric Neoplasm at an Outpatient Clinic: Efficacy and Safety
Hwoon-Yong Jung, Ji Yong Ahn
Clinical Endoscopy.2014; 47(6): 473. CrossRef
- Pathology and Clinical Relevance of Gastric Epithelial Dysplasia
- 5,978 View
- 54 Download
- 6 Web of Science
- 6 Crossref


 KSGE
KSGE


 First
First Prev
Prev



