Search
- Page Path
- HOME > Search
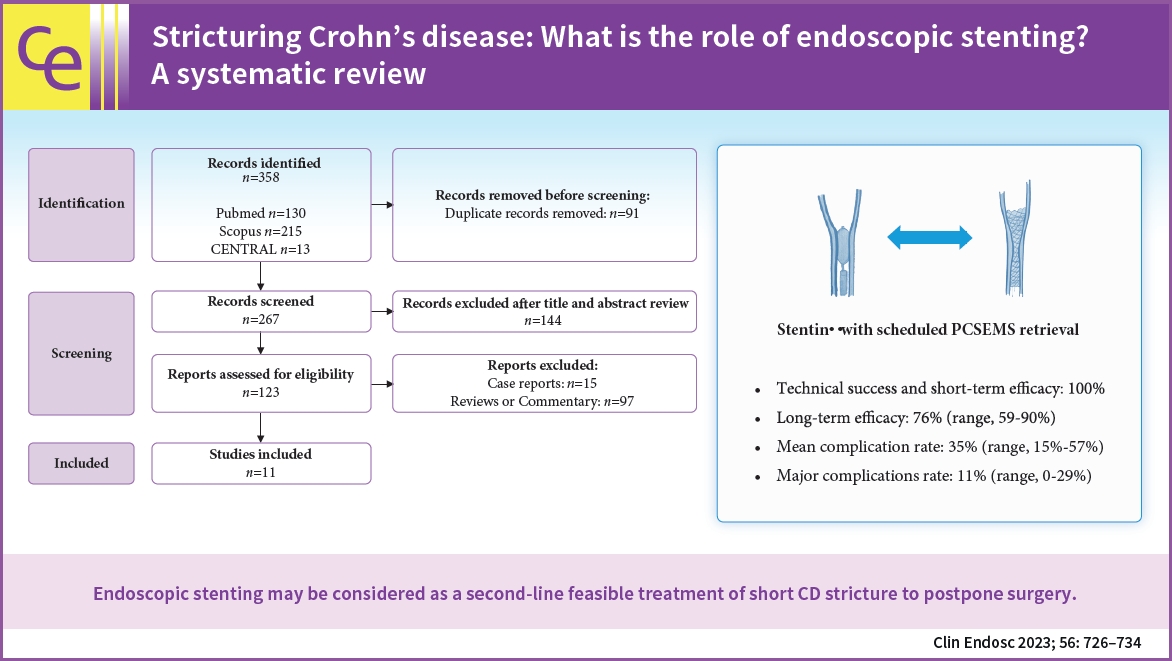
- Stricturing Crohn's disease: what is the role of endoscopic stenting? A systematic review
- Giorgia Burrelli Scotti, Roberto Lorenzetti, Annalisa Aratari, Antonietta Lamazza, Enrico Fiori, Claudio Papi, Stefano Festa
- Clin Endosc 2023;56(6):726-734. Published online October 24, 2023
- DOI: https://doi.org/10.5946/ce.2023.059
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 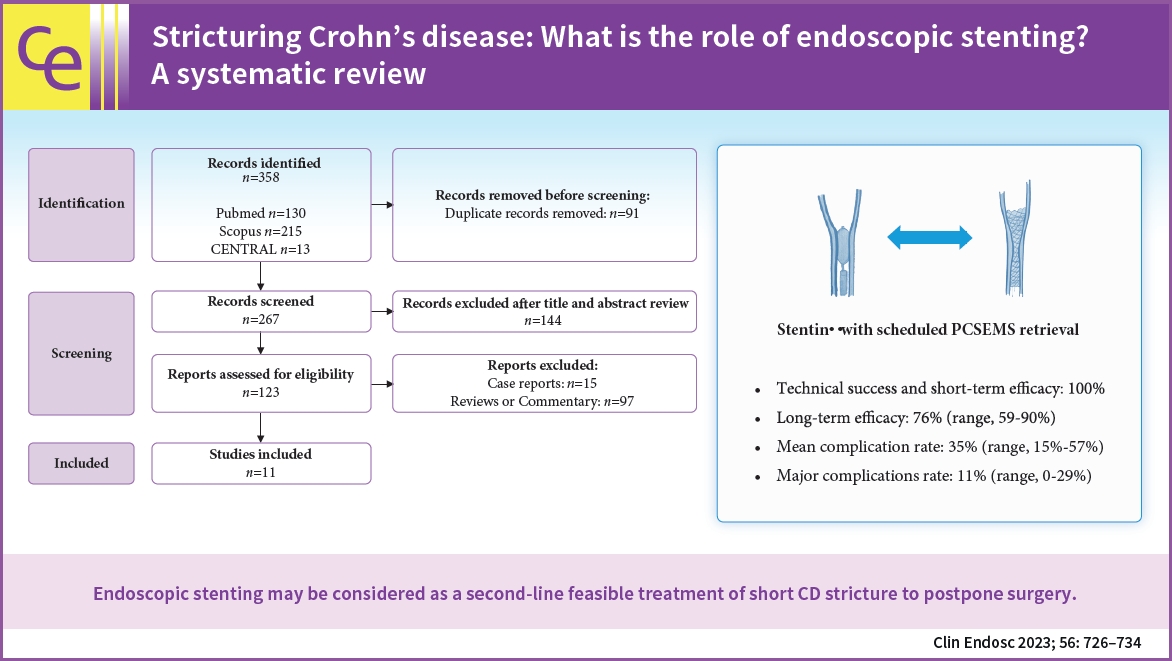
- Background
/Aims: Endoscopic stenting for stricturing Crohn's disease (CD) is an emerging treatment that achieves more persistent dilatation of the stricture over time than endoscopic balloon dilatation (EBD). We aimed to explore the efficacy and safety of stenting for the treatment of CD strictures.
Methods
A systematic electronic literature search was performed (PROSPERO; no. CRD42022308033). The primary outcomes were technical success, efficacy, complication rate, and the need for further interventions due to reobstruction. The outcomes of partially covered self-expanding metal stents (PCSEMS) with scheduled retrieval after seven days were also analyzed.
Results
Eleven eligible studies were included in the review. Overall, 173 patients with CD were included in this study. Mean percentage of technical success was 95% (range, 80%–100%), short-term efficacy was 100% in all studies, and long-term efficacy was 56% (range, 25%–90%). In patients with a scheduled PCSEMS retrieval, the long-term efficacy was 76% (range, 59%–90%), the mean complication rate was 35% (range, 15%–57%), and the major complication rate was 11% (range, 0%–29%).
Conclusions
Endoscopic stenting with scheduled PCSEMS retrieval may be considered a feasible second-line treatment for short CD strictures to postpone surgery. However, larger head-to-head prospective studies are needed to understand the role of stenting as an alternative or additional treatment to EBD in CD. -
Citations
Citations to this article as recorded by- Perioperative Considerations for the Surgical Treatment of Crohn’s Disease with Discussion on Surgical Antibiotics Practices and Impact on the Gut Microbiome
Shelbi Olson, Lindsay Welton, Cyrus Jahansouz
Antibiotics.2024; 13(4): 317. CrossRef
- Perioperative Considerations for the Surgical Treatment of Crohn’s Disease with Discussion on Surgical Antibiotics Practices and Impact on the Gut Microbiome
- 2,722 View
- 181 Download
- 1 Web of Science
- 1 Crossref

- Recent advances in surveillance colonoscopy for dysplasia in inflammatory bowel disease
- Soo-Young Na, Won Moon
- Clin Endosc 2022;55(6):726-735. Published online November 18, 2022
- DOI: https://doi.org/10.5946/ce.2022.132

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Inflammatory bowel disease (IBD) has a global presence with rapidly increasing incidence and prevalence. Patients with IBD including those with ulcerative colitis and Crohn’s disease have a higher risk of developing colorectal cancer (CRC) compared to the general population. Risk factors for CRC in patients with IBD include long disease duration, extensive colitis, primary sclerosing cholangitis, family history of CRC, stricture, and prior dysplasia. Surveillance colonoscopy for CRC in patients with IBD should be tailored to individualized risk factors and requires careful monitoring every year to every five years. The current surveillance techniques are based on several guidelines. Chromoendoscopy with targeted biopsy is being recommended increasingly, and high-definition colonoscopy is gradually replacing standard-definition colonoscopy. However, it remains unclear whether chromoendoscopy, virtual chromoendoscopy, or white-light endoscopy has better efficiency when a high-definition scope is used. With the development of new endoscopic instruments and techniques, the paradigm of surveillance strategy has gradually changed. In this review, we discuss cutting-edge surveillance colonoscopy in patients with IBD including a review of literature.
-
Citations
Citations to this article as recorded by- Inflammatory bowel disease and primary sclerosing cholangitis: One disease or two?
Kim N. van Munster, Annika Bergquist, Cyriel Y. Ponsioen
Journal of Hepatology.2024; 80(1): 155. CrossRef - Extrachromosomal Circular DNA: An Emerging Potential Biomarker for Inflammatory Bowel Diseases?
Valentina Petito, Federica Di Vincenzo, Lorenza Putignani, Maria T. Abreu, Birgitte Regenberg, Antonio Gasbarrini, Franco Scaldaferri
Genes.2024; 15(4): 414. CrossRef - A Review of Colonoscopy in Intestinal Diseases
Seung Hong, Dong Baek
Diagnostics.2023; 13(7): 1262. CrossRef - Potential Oral Microbial Markers for Differential Diagnosis of Crohn’s Disease and Ulcerative Colitis Using Machine Learning Models
Sang-Bum Kang, Hyeonwoo Kim, Sangsoo Kim, Jiwon Kim, Soo-Kyung Park, Chil-Woo Lee, Kyeong Ok Kim, Geom-Seog Seo, Min Suk Kim, Jae Myung Cha, Ja Seol Koo, Dong-Il Park
Microorganisms.2023; 11(7): 1665. CrossRef - Update on Endoscopic Dysplasia Surveillance in Inflammatory Bowel Disease
Nayantara Coelho-Prabhu, James D. Lewis
American Journal of Gastroenterology.2023; 118(10): 1748. CrossRef
- Inflammatory bowel disease and primary sclerosing cholangitis: One disease or two?
- 2,919 View
- 206 Download
- 5 Web of Science
- 5 Crossref

- Chronological Review of Endoscopic Indices in Inflammatory Bowel Disease
- Joon Seop Lee, Eun Soo Kim, Won Moon
- Clin Endosc 2019;52(2):129-136. Published online August 21, 2018
- DOI: https://doi.org/10.5946/ce.2018.042

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Inflammatory bowel disease (IBD) is considered a chronic condition characterized by mucosal or transmural inflammation in the gastrointestinal tract. Endoscopic diagnosis and surveillance in patients with IBD have become crucial. In addition, endoscopy is a useful modality in estimation and evaluation of the disease, treatment results, and efficacy of treatment delivery and surveillance. In relation to these aspects, endoscopic disease activity has been commonly estimated in clinical practices and trials.
At present, many endoscopic indices of ulcerative colitis have been introduced, including the Truelove and Witts Endoscopy Index, Baron Index, Powell-Tuck Index, Sutherland Index, Mayo Clinic Endoscopic Sub-Score, Rachmilewitz Index, Modified Baron Index, Endoscopic Activity Index, Ulcerative Colitis Endoscopic Index of Severity, Ulcerative Colitis Colonoscopic Index of Severity, and Modified Mayo Endoscopic Score. Endoscopic indices have been also suggested for Crohn’s disease, such as the Crohn’s Disease Endoscopic Index of Severity, Simple Endoscopic Score for Crohn’s Disease, and Rutgeerts Postoperative Endoscopic Index. However, most endoscopic indices have not been validated owing to the complexity of their parameters and inter-observer variations. Therefore, a chronological approach for understanding the various endoscopic indices relating to IBD is needed to improve the management. -
Citations
Citations to this article as recorded by- The assessment of segmental healing by the Modified Mayo Endoscopic Score (MMES) complements the prediction of long‐term clinical outcomes in patients with ulcerative colitis
Matthias Lenfant, Bram Verstockt, João Sabino, Séverine Vermeire, Marc Ferrante
Alimentary Pharmacology & Therapeutics.2024; 59(1): 64. CrossRef - Recent Trends in Non-Invasive Methods of Diagnosis and Evaluation of Inflammatory Bowel Disease: A Short Review
Dan Vălean, Roxana Zaharie, Roman Țaulean, Lia Usatiuc, Florin Zaharie
International Journal of Molecular Sciences.2024; 25(4): 2077. CrossRef - Accuracy of the Pancolonic Modified Mayo Score in predicting the long-term outcomes of ulcerative colitis: a promising scoring system
Péter Bacsur, Panu Wetwittayakhlang, Tamás Resál, Emese Földi, Béla Vasas, Bernadett Farkas, Mariann Rutka, Talat Bessissow, Waqqas Afif, Anita Bálint, Anna Fábián, Renáta Bor, Zoltán Szepes, Klaudia Farkas, Peter L Lakatos, Tamás Molnár
Therapeutic Advances in Gastroenterology.2024;[Epub] CrossRef - Disease clearance in ulcerative colitis: Setting the therapeutic goals for future in the treatment of ulcerative colitis
Laura Ramos, Jeny Teo-Loy, Manuel Barreiro-de Acosta
Frontiers in Medicine.2023;[Epub] CrossRef - Use of Standardized Inflammatory Bowel Disease Endoscopy Scores in Clinical Practice
Jill K J Gaidos, Badr Al Bawardy, Francis A Farraye, Miguel Regueiro
Crohn's & Colitis 360.2023;[Epub] CrossRef - Systematic Literature Review and Meta-analysis: Real-World Mucosal Healing in Vedolizumab-Treated Patients with Crohn’s Disease
Silvio Danese, Pravin Kamble, Jin Yang, Jean-Gabriel Le Moine, Shahnaz Khan, Emma Hawe, Christian Agboton, Song Wang, Peter M. Irving, Than Than Aye
GastroHep.2022; 2022: 1. CrossRef - Assessment of Endoscopic Disease Activity in Ulcerative Colitis: Is Simplicity the Ultimate Sophistication?
Ala I. Sharara, Maher Malaeb, Matthias Lenfant, Marc Ferrante
Inflammatory Intestinal Diseases.2022; 7(1): 7. CrossRef - Endoscopic activity in inflammatory bowel disease: clinical significance and application in practice
Kyeong Ok Kim
Clinical Endoscopy.2022; 55(4): 480. CrossRef - Predicting Mucosal Healing in Crohn’s Disease: A Nomogram Model Developed from a Retrospective Cohort
Nana Tang, Han Chen, Ruidong Chen, Wen Tang, Hongjie Zhang
Journal of Inflammation Research.2022; Volume 15: 5515. CrossRef - Micronutrient deficiency among patients with ulcerative colitis
Amany Hussien, Sawsan Abd El-Moniem, Ziyad Tawhid, Ahmed Altonbary
The Egyptian Journal of Internal Medicine.2022;[Epub] CrossRef - State-of-the-art surgery for ulcerative colitis
Shanglei Liu, Samuel Eisenstein
Langenbeck's Archives of Surgery.2021; 406(6): 1751. CrossRef - Magnetic beads in gastrointestinal tract
Eva Karásková, Miloš Geryk, Radek Vrba, Tomáš Malý FEBPS, Jakub Čivrný, Dagmar Pospíšilová
Pediatrie pro praxi.2021; 22(5): 346. CrossRef - Can red blood cell distribution width (RDW) predict clinical and endoscopic activity in ulcerative colitis patients?
Hüseyin PÜLAT, Serkan YALAKİ
Journal of Surgery and Medicine.2020;[Epub] CrossRef - Case Report on Ulcerative Colitis in 16 year girl
MD.Salma MD.Salma, Y.Siva Y.Siva , , J.Bhargava Narendra , J.Bhargava Narendra
World Journal of Current Medical and Pharmaceutical Research.2020; : 287. CrossRef - Characterization of γδ T Cells in Intestinal Mucosa From Patients With Early-Onset or Long-Standing Inflammatory Bowel Disease and Their Correlation With Clinical Status
Elena Lo Presti, Roberto Di Mitri, Filippo Mocciaro, Anna Barbara Di Stefano, Nunzia Scibetta, Elettra Unti, Giuseppe Cicero, Giulia Pecoraro, Elisabetta Conte, Francesco Dieli, Serena Meraviglia
Journal of Crohn's and Colitis.2019; 13(7): 873. CrossRef - Endoscopic scoring systems for the evaluation and monitoring of disease activity in Crohn's disease
Lara Hart, Talat Bessissow
Best Practice & Research Clinical Gastroenterology.2019; 38-39: 101616. CrossRef - British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults
Christopher Andrew Lamb, Nicholas A Kennedy, Tim Raine, Philip Anthony Hendy, Philip J Smith, Jimmy K Limdi, Bu’Hussain Hayee, Miranda C E Lomer, Gareth C Parkes, Christian Selinger, Kevin J Barrett, R Justin Davies, Cathy Bennett, Stuart Gittens, Malcolm
Gut.2019; 68(Suppl 3): s1. CrossRef - Novel oral-targeted therapies for mucosal healing in ulcerative colitis
Elisabetta Antonelli, Vincenzo Villanacci, Gabrio Bassotti
World Journal of Gastroenterology.2018; 24(47): 5322. CrossRef
- The assessment of segmental healing by the Modified Mayo Endoscopic Score (MMES) complements the prediction of long‐term clinical outcomes in patients with ulcerative colitis
- 11,738 View
- 475 Download
- 15 Web of Science
- 18 Crossref

- Endoscopic Diagnosis and Differentiation of Inflammatory Bowel Disease
- Ji Min Lee, Kang-Moon Lee
- Clin Endosc 2016;49(4):370-375. Published online July 29, 2016
- DOI: https://doi.org/10.5946/ce.2016.090
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Patients with inflammatory bowel disease have significantly increased in recent decades in Korea. Intestinal tuberculosis (ITB) and intestinal Behcet’s disease (BD), which should be differentiated from Crohn’s disease (CD), are more frequent in Korea than in the West. Thus, the accurate diagnosis of these inflammatory diseases is problematic in Korea and clinicians should fully understand their clinical and endoscopic characteristics. Ulcerative colitis mostly presents with rectal inflammation and continuous lesions, while CD presents with discontinuous inflammatory lesions and frequently involves the ileocecal area. Involvement of fewer than four segments, a patulous ileocecal valve, transverse ulcers, and scars or pseudopolyps are more frequently seen in ITB than in CD. A few ulcers with discrete margins are a typical endoscopic finding of intestinal BD. However, the differential diagnosis is difficult in many clinical situations because typical endoscopic findings are not always observed. Therefore, clinicians should also consider symptoms and laboratory, pathological, and radiological findings, in addition to endoscopic findings.
-
Citations
Citations to this article as recorded by- Recent Trends in Non-Invasive Methods of Diagnosis and Evaluation of Inflammatory Bowel Disease: A Short Review
Dan Vălean, Roxana Zaharie, Roman Țaulean, Lia Usatiuc, Florin Zaharie
International Journal of Molecular Sciences.2024; 25(4): 2077. CrossRef - Differential diagnosis of Crohn’s disease and intestinal tuberculosis based on ATR-FTIR spectroscopy combined with machine learning
Yuan-Peng Li, Tian-Yu Lu, Fu-Rong Huang, Wei-Min Zhang, Zhen-Qiang Chen, Pei-Wen Guang, Liang-Yu Deng, Xin-Hao Yang
World Journal of Gastroenterology.2024; 30(10): 1377. CrossRef - The quality of life of patients with inflammatory bowel diseases and the multidisciplinary team
Roxana-Ioana Ghenade, Ilie-Marius Ciorbă
Medic.ro.2024; 3(159): 24. CrossRef - A Case Report and Literature Review of Rectosigmoid Crohn’s Disease: A Diagnostic Pitfall Ultimately Leading to Spontaneous Colonic Perforation
Muhammad Z Ali, Muhammad Usman Tariq, Muhammad Hasan Abid, Hamma Abdulaziz, Mohmmad AlAdwani, Arif Khurshid, Muhammad Rashid, Fawaz Al Thobaiti , Amjad Althagafi
Cureus.2023;[Epub] CrossRef - Identification of cuproptosis-associated subtypes and signature genes for diagnosis and risk prediction of Ulcerative colitis based on machine learning
Dadong Tang, Baoping Pu, Shiru Liu, Hongyan Li
Frontiers in Immunology.2023;[Epub] CrossRef - Endoscopic features of the intestinal mucosa in patients with ulcerative colitis depending on the level of IgG4
Yu.M. Stepanov, M.V. Stoykevich, Yu.A. Gaidar, T.S. Tarasova, O.V. Simonova, O.M. Tatarchuk, O.P. Petishko
GASTROENTEROLOGY.2023; 57(1): 30. CrossRef - Standardizing Scoring Conventions for Crohn’s Disease Endoscopy: An International RAND/UCLA Appropriateness Study
Reena Khanna, Christopher Ma, Malcolm Hogan, Guangyong Zou, Talat Bessissow, Brian Bressler, Jean-Frédéric Colombel, Silvio Danese, Marco Daperno, James E. East, Lawrence Hookey, Edward V. Loftus, John W.D. McDonald, Remo Panaccione, Laurent Peyrin-Biroul
Clinical Gastroenterology and Hepatology.2023; 21(11): 2938. CrossRef - Creeping fat exhibits distinct Inflammation-specific adipogenic preadipocytes in Crohn’s disease
Nahee Hwang, Dongwoo Kang, Su-Jin Shin, Bo Kyung Yoon, Jaeyoung Chun, Jae-woo Kim, Sungsoon Fang
Frontiers in Immunology.2023;[Epub] CrossRef - PD-1-positive cells contribute to the diagnosis of inflammatory bowel disease and can aid in predicting response to vedolizumab
Min Kyu Kim, Su In Jo, Sang-Yeob Kim, Hyun Lim, Ho Suk Kang, Sung‑Hoon Moon, Byong Duk Ye, Jae Seung Soh, Sung Wook Hwang
Scientific Reports.2023;[Epub] CrossRef - Inflammatory bowel disease in adults
Umang Qazi
InnovAiT: Education and inspiration for general practice.2022; 15(2): 97. CrossRef - Integrative computational approach identifies immune‐relevant biomarkers in ulcerative colitis
Tianzhen He, Kai Wang, Peng Zhao, Guanqun Zhu, Xinbao Yin, Yulian Zhang, Zongliang Zhang, Kai Zhao, Zhenlin Wang, Ke Wang
FEBS Open Bio.2022; 12(2): 500. CrossRef - Absent X‐linked inhibitor of apoptosis protein expression in T cell blasts and causal mutations including non‐coding deletion
Shimaa Said Mohamed Ali Abdrabou, Nariaki Toita, Shin Ichihara, Yusuke Tozawa, Michiko Takahashi, Shin‐ichi Fujiwara, Toshifumi Ashida, Osamu Ohara, Tadashi Ariga, Atsushi Manabe, Mutsuko Konno, Masafumi Yamada
Pediatrics International.2022;[Epub] CrossRef - Mechanisms of mucosal healing: treating inflammatory bowel disease without immunosuppression?
Eduardo J. Villablanca, Katja Selin, Charlotte R. H. Hedin
Nature Reviews Gastroenterology & Hepatology.2022; 19(8): 493. CrossRef - Role of multidetector computed tomography in patients with acute infectious colitis
Seung Jung Yu, Jae Hyuk Heo, Eun Jeong Choi, Jong Hyuk Kim, Hong Sub Lee, Sun Young Kim, Jae Hoon Lim
World Journal of Clinical Cases.2022; 10(12): 3686. CrossRef - Differential Diagnosis of Crohn’s Disease and Ulcerative Primary Intestinal Lymphoma: A Scoring Model Based on a Multicenter Study
Hong Yang, Huimin Zhang, Wei Liu, Bei Tan, Tao Guo, Xiang Gao, Rui Feng, Kaichun Wu, Qian Cao, Zhihua Ran, Zhanju Liu, Naizhong Hu, Liangru Zhu, Yamin Lai, Congling Wang, Wei Han, Jiaming Qian
Frontiers in Oncology.2022;[Epub] CrossRef - Gut inflammation induced by drugs: Can pathology help to differentiate from inflammatory bowel disease?
Naoimh Herlihy, Roger Feakins
United European Gastroenterology Journal.2022; 10(5): 451. CrossRef - A Rare Case of New-Onset Ulcerative Colitis in a Nonagenarian
Emmanuel U Emeasoba, Cece E Ibeson, Sanchit Kundal, Stefanie Biondi, Ifeanyi Nwosu, Shmuel Golfeyz, Michael Kantrowitz, Dimitry Khodorskiy
Cureus.2022;[Epub] CrossRef - Application value of tissue tuberculosis antigen combined with Xpert MTB/RIF detection in differential diagnoses of intestinal tuberculosis and Crohn’s disease
Baoying Fei, Lin Zhou, Yu Zhang, Linhe Luo, Yuanyuan Chen
BMC Infectious Diseases.2021;[Epub] CrossRef - De Novo Inflammatory Bowel Disease Rarely Occurs During Posttransplant Immunosuppression
Jiayun M Fang, Laura Lamps, Amoah Yeboah-Korang, Jerome Cheng, Maria Westerhoff
American Journal of Clinical Pathology.2021; 156(6): 1113. CrossRef - Diterpenoids Isolated from Podocarpus macrophyllus Inhibited the Inflammatory Mediators in LPS-Induced HT-29 and RAW 264.7 Cells
ChoEen Kim, DucDat Le, Mina Lee
Molecules.2021; 26(14): 4326. CrossRef - Retrospective study of the differential diagnosis between cryptogenic multifocal ulcerous stenosing enteritis and small bowel Crohn’s disease
Dan Chen, Wei Liu, Weixun Zhou, Weiyang Zheng, Dong Wu, Jiaming Qian
BMC Gastroenterology.2020;[Epub] CrossRef - PREVALENCE AND FACTORS ASSOCIATED WITH SMALL INTESTINAL BACTERIAL OVERGROWTH IN PATIENTS WITH CROHN’S DISEASE: A RETROSPECTIVE STUDY AT A REFERRAL CENTER
Erika Ruback BERTGES, Júlio Maria Fonseca CHEBLI
Arquivos de Gastroenterologia.2020; 57(3): 283. CrossRef - Can natural language processing help differentiate inflammatory intestinal diseases in China? Models applying random forest and convolutional neural network approaches
Yuanren Tong, Keming Lu, Yingyun Yang, Ji Li, Yucong Lin, Dong Wu, Aiming Yang, Yue Li, Sheng Yu, Jiaming Qian
BMC Medical Informatics and Decision Making.2020;[Epub] CrossRef - Chronological Review of Endoscopic Indices in Inflammatory Bowel Disease
Joon Seop Lee, Eun Soo Kim, Won Moon
Clinical Endoscopy.2019; 52(2): 129. CrossRef - Illuminating an Invisible Epidemic: A Systemic Review of the Clinical and Economic Benefits of Early Diagnosis and Treatment in Inflammatory Disease and Related Syndromes
Wylezinski, Gray, Polk, Harmata, Spurlock
Journal of Clinical Medicine.2019; 8(4): 493. CrossRef - Anti-IL-13Rα2 therapy promotes recovery in a murine model of inflammatory bowel disease
Erik P. Karmele, Trisha S. Pasricha, Thirumalai R. Ramalingam, Robert W. Thompson, Richard L. Gieseck, Kayla J. Knilans, Martin Hegen, Mark Farmer, Fang Jin, Aaron Kleinman, David A. Hinds, Thiago Almeida Pereira, Rafael de Queiroz Prado, Nan Bing, Lioudm
Mucosal Immunology.2019; 12(5): 1174. CrossRef - A challenge in diagnosis and management of ulcerative colitis in elderly patient with atypical presentation: A reported case
Panutchaya Kongon, Vorapatu Tangsirapat, Vittawat Ohmpornuwat, Kannakrit Sumtong, Vichack Chakrapan Na Ayudhya, Kobkool Chakrapan Na Ayudhya, Paiboon Sookpotarom, Paisarn Vejchapipat
International Journal of Surgery Case Reports.2019; 61: 234. CrossRef - Primary hypertrophic osteoarthropathy related gastrointestinal complication has distinctive clinical and pathological characteristics: two cases report and review of the literature
Qiang Wang, Ying-he Li, Guo-le Lin, Yue Li, Wei-xun Zhou, Jia-ming Qian, Wei-bo Xia, Dong Wu
Orphanet Journal of Rare Diseases.2019;[Epub] CrossRef - Intestinal granulomatous disease: what is the first call
Alex Guri, Michal Kori, Pearl Herskovitz, Oren Zimhony
BMJ Case Reports.2018; : bcr-2017-223094. CrossRef - Aspecific ileitis: Crohn’s disease or not Crohn’s disease? A prospective study
Cristina Bezzio, Ilaria Arena, Massimo Devani, Barbara Omazzi, Gianpiero Manes, Simone Saibeni
International Journal of Colorectal Disease.2017; 32(7): 1025. CrossRef - Endoscopic Bamboo Joint-like Appearance of the Stomach in Crohn's Disease
Kwang Il Seo, Won Moon
The Korean Journal of Gastroenterology.2017; 69(2): 151. CrossRef - Management of Crohn's disease in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease
Shu-Chen Wei, Ting-An Chang, Te-Hsin Chao, Jinn-Shiun Chen, Jen-Wei Chou, Yenn-Hwei Chou, Chiao-Hsiung Chuang, Wen-Hung Hsu, Tien-Yu Huang, Tzu-Chi Hsu, Chun-Chi Lin, Hung-Hsin Lin, Jen-Kou Lin, Wei-Chen Lin, Yen-Hsuan Ni, Ming-Jium Shieh, I-Lun Shih, Chi
Intestinal Research.2017; 15(3): 285. CrossRef
- Recent Trends in Non-Invasive Methods of Diagnosis and Evaluation of Inflammatory Bowel Disease: A Short Review
- 26,400 View
- 773 Download
- 30 Web of Science
- 32 Crossref

- Fecal Microbiota Transplantation: Current Applications, Effectiveness, and Future Perspectives
- Hyun Ho Choi, Young-Seok Cho
- Clin Endosc 2016;49(3):257-265. Published online March 9, 2016
- DOI: https://doi.org/10.5946/ce.2015.117
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Fecal microbiota transplantation (FMT) is the infusion of liquid filtrate feces from a healthy donor into the gut of a recipient to cure a specific disease. A fecal suspension can be administered by nasogastric or nasoduodenal tube, colonoscope, enema, or capsule. The high success rate and safety in the short term reported for recurrent Clostridium difficile infection has elevated FMT as an emerging treatment for a wide range of disorders, including Parkinson’s disease, fibromyalgia, chronic fatigue syndrome, myoclonus dystopia, multiple sclerosis, obesity, insulin resistance, metabolic syndrome, and autism. There are many unanswered questions regarding FMT, including donor selection and screening, standardized protocols, long-term safety, and regulatory issues. This article reviews the efficacy and safety of FMT used in treating a variety of diseases, methodology, criteria for donor selection and screening, and various concerns regarding FMT.
-
Citations
Citations to this article as recorded by- Antiaging Strategies and Remedies: A Landscape of Research Progress and Promise
Rumiana Tenchov, Janet M. Sasso, Xinmei Wang, Qiongqiong Angela Zhou
ACS Chemical Neuroscience.2024;[Epub] CrossRef - Corticosteroid-resistant immune-related adverse events: a systematic review
Eveline Daetwyler, Till Wallrabenstein, David König, Laura C Cappelli, Jarushka Naidoo, Alfred Zippelius, Heinz Läubli
Journal for ImmunoTherapy of Cancer.2024; 12(1): e007409. CrossRef - Lurking Danger: Emerging Evidence
Palepu B Gopal
Indian Journal of Critical Care Medicine.2024; 28(2): 93. CrossRef - Evaluation of the safety and efficacy of fecal microbiota transplantations in bottlenose dolphins (Tursiops truncatus) using metagenomic sequencing
Barbara K Linnehan, Sho M Kodera, Sarah M Allard, Erin C Brodie, Celeste Allaband, Rob Knight, Holly L Lutz, Maureen C Carroll, Jennifer M Meegan, Eric D Jensen, Jack A Gilbert
Journal of Applied Microbiology.2024;[Epub] CrossRef - Impact of the diet in the gut microbiota after an inter-species microbial transplantation in fish
Alberto Ruiz, Enric Gisbert, Karl B. Andree
Scientific Reports.2024;[Epub] CrossRef - Protective effects of fecal microbiota transplantation against ischemic stroke and other neurological disorders: an update
Tousif Ahmed Hediyal, C. Vichitra, Nikhilesh Anand, Mahendran Bhaskaran, Saeefh M. Essa, Pravir Kumar, M. Walid Qoronfleh, Mohammed Akbar, Ruchika Kaul-Ghanekar, Arehally M. Mahalakshmi, Jian Yang, Byoung-Joon Song, Tanya M. Monaghan, Meena Kishore Sakhar
Frontiers in Immunology.2024;[Epub] CrossRef - Crosstalk between COVID-19 and the gut-brain axis: a gut feeling
Nida Kalam, Vinod R M T Balasubramaniam
Postgraduate Medical Journal.2024;[Epub] CrossRef - Complementary Therapeutic Effect of Fecal Microbiota Transplantation in Ulcerative Colitis after the Response to Anti-Tumor Necrosis Factor Alpha Agent Was Lost: A Case Report
Jongbeom Shin, Ga Hyeon Baek, Boram Cha, Soo-Hyun Park, Jung-Hwan Lee, Jun-Seob Kim, Kye Sook Kwon
Biomedicines.2024; 12(4): 800. CrossRef - Changes in the Progression of Chronic Kidney Disease in Patients Undergoing Fecal Microbiota Transplantation
Giovanna Yazmín Arteaga-Muller, Samantha Flores-Treviño, Paola Bocanegra-Ibarias, Diana Robles-Espino, Elvira Garza-González, Graciela Catalina Fabela-Valdez, Adrián Camacho-Ortiz
Nutrients.2024; 16(8): 1109. CrossRef - Enterotype-Dependent Probiotic-Mediated Changes in the Male Rat Intestinal Microbiome In Vivo and In Vitro
Nikolay Kolzhetsov, Natalia Markelova, Maria Frolova, Olga Alikina, Olga Glazunova, Lubov Safonova, Irina Kalashnikova, Vladimir Yudin, Valentin Makarov, Anton Keskinov, Sergey Yudin, Daria Troshina, Viktoria Rechkina, Viktoria Shcherbakova, Konstantin Sh
International Journal of Molecular Sciences.2024; 25(8): 4558. CrossRef - Unveiling the gut-eye axis: how microbial metabolites influence ocular health and disease
Yvonne Nguyen, Josephine Rudd Zhong Manis, Nicole Marie Ronczkowski, Tommy Bui, Allston Oxenrider, Ravirajsinh N. Jadeja, Menaka C. Thounaojam
Frontiers in Medicine.2024;[Epub] CrossRef - Modify gut microbiome in autism: a promising strategy?
Jean Demarquoy, Haifa Othman, Caroline Demarquoy
Exploration of Neuroscience.2023; : 140. CrossRef - Targeting Gut Microbiota in Cancer Cachexia: Towards New Treatment Options
Concetta Panebianco, Annacandida Villani, Adele Potenza, Enrica Favaro, Concetta Finocchiaro, Francesco Perri, Valerio Pazienza
International Journal of Molecular Sciences.2023; 24(3): 1849. CrossRef - Gut Microbiota and Alzheimer’s Disease: How to Study and Apply Their Relationship
Ngoc Minh Nguyen, Jungsook Cho, Choongho Lee
International Journal of Molecular Sciences.2023; 24(4): 4047. CrossRef - Impact of Intensive Care Unit Nutrition on the Microbiome and Patient Outcomes
Mara A. Serbanescu, Monica Da Silva, Ahmed Zaky
Anesthesiology Clinics.2023; 41(1): 263. CrossRef - Connecting the Dots: The Interplay Between Stroke and the Gut-Brain Axis
Pooja M Murthy, Jayashankar CA, Venkataramana Kandi, Mithun K Reddy, Ganaraja V Harikrishna, Kavitha Reddy, Ramya JP, Ankush N Reddy, Jigya Narang
Cureus.2023;[Epub] CrossRef - The role of faecal microbiota transplantation in chronic noncommunicable disorders
Benjamin H. Mullish, Ege Tohumcu, Serena Porcari, Marcello Fiorani, Natalia Di Tommaso, Antonio Gasbarrini, Giovanni Cammarota, Francesca Romana Ponziani, Gianluca Ianiro
Journal of Autoimmunity.2023; 141: 103034. CrossRef - Role of gut microbiota and bacterial metabolites in mucins of colorectal cancer
Ming Gu, Weixiang Yin, Jiaming Zhang, Junfeng Yin, Xiaofei Tang, Jie Ling, Zhijie Tang, Weijuan Yin, Xiangjun Wang, Qing Ni, Yunxiang Zhu, Tuo Chen
Frontiers in Cellular and Infection Microbiology.2023;[Epub] CrossRef - Fecal microbiota transplantation for the treatment of irritable bowel syndrome: A systematic review and meta-analysis
Sofie Ingdam Halkjær, Bobby Lo, Frederik Cold, Alice Højer Christensen, Savanne Holster, Julia König, Robert Jan Brummer, Olga C Aroniadis, Perttu Lahtinen, Tom Holvoet, Lise Lotte Gluud, Andreas Munk Petersen
World Journal of Gastroenterology.2023; 29(20): 3185. CrossRef - Systems biology approaches to identify potential targets and inhibitors of the intestinal microbiota to treat depression
Fei Teng, Zhongwen Lu, Fei Gao, Jing Liang, Jiawen Li, Xuanhe Tian, Xianshuai Wang, Haowei Guan, Jin Wang
Scientific Reports.2023;[Epub] CrossRef - The Diversity of Gut Microbiota at Weaning Is Altered in Prolactin Receptor-Null Mice
Ivan Luzardo-Ocampo, Ana Luisa Ocampo-Ruiz, José Luis Dena-Beltrán, Gonzalo Martínez de la Escalera, Carmen Clapp, Yazmín Macotela
Nutrients.2023; 15(15): 3447. CrossRef - Recipient-independent, high-accuracy FMT-response prediction and optimization in mice and humans
Oshrit Shtossel, Sondra Turjeman, Alona Riumin, Michael R. Goldberg, Arnon Elizur, Yarin Bekor, Hadar Mor, Omry Koren, Yoram Louzoun
Microbiome.2023;[Epub] CrossRef - The role of Fecal Microbiota Transplantation (FMT) in treating patients with multiple sclerosis
George G. Zhanel, Rotem Keynan, Yoav Keynan, James A. Karlowsky
Expert Review of Neurotherapeutics.2023; 23(10): 921. CrossRef - The Next Generation Fecal Microbiota Transplantation: To Transplant Bacteria or Virome
You Yu, Weihong Wang, Faming Zhang
Advanced Science.2023;[Epub] CrossRef - Fecal microbiota transplantation: History, procedure and regulatory considerations
Thanush D, M.P. Venkatesh
La Presse Médicale.2023; 52(4): 104204. CrossRef - Gut microbiota of Suncus murinus, a naturally obesity-resistant animal, improves the ecological diversity of the gut microbiota in high-fat-diet-induced obese mice
Mingshou Zhang, Ting Yang, Rujia Li, Ke Ren, Jun Li, Maozhang He, Juefei Chen, Shuang-Qin Yi, Farah Al-Marzooq
PLOS ONE.2023; 18(11): e0293213. CrossRef - Role of Fecal Microbiota Transplantation in Managing Clostridium Difficile Infection and Inflammatory Bowel Disease: A Narrative Review
Haider Ghazanfar, Sameer Kandhi, Trishna Acherjee, Zaheer A Qureshi, Mohammed Shaban, Diaz Saez Yordanka, Dessiree Cordero, Siddarth Chinta, Abhilasha Jyala, Harish Patel
Cureus.2023;[Epub] CrossRef - Co-Housing and Fecal Microbiota Transplantation: Technical Support for TCM Herbal Treatment of Extra-Intestinal Diseases Based on Gut Microbial Ecosystem Remodeling
Xian Sun, Xi Zhou, Weiming He, Wei Sun, Zheng Xu
Drug Design, Development and Therapy.2023; Volume 17: 3803. CrossRef - Microbe-based therapies for colorectal cancer: Advantages and limitations
Mohd Saeed, Ambreen Shoaib, Raghuram Kandimalla, Shamama Javed, Ahmad Almatroudi, Ramesh Gupta, Farrukh Aqil
Seminars in Cancer Biology.2022; 86: 652. CrossRef - Fecal Microbiota Transplantation to Prevent and Treat Chronic Disease: Implications for Dietetics Practice
Irene Opoku-Acheampong, Taylor McLaud, Olivia S. Anderson
Journal of the Academy of Nutrition and Dietetics.2022; 122(1): 33. CrossRef - Targeting the Gut in Obesity: Signals from the Inner Surface
Natalia Petersen, Thomas U. Greiner, Lola Torz, Angie Bookout, Marina Kjærgaard Gerstenberg, Carlos M. Castorena, Rune Ehrenreich Kuhre
Metabolites.2022; 12(1): 39. CrossRef - Observational Study of Small Animal Practitioners’ Awareness, Clinical Practice and Experience With Fecal Microbiota Transplantation in Dogs
Silke Salavati Schmitz
Topics in Companion Animal Medicine.2022; 47: 100630. CrossRef - Interventions on Microbiota: Where Do We Stand on a Gut–Brain Link in Autism? A Systematic Review
Margherita Prosperi, Elisa Santocchi, Letizia Guiducci, Jacopo Frinzi, Maria Aurora Morales, Raffaella Tancredi, Filippo Muratori, Sara Calderoni
Nutrients.2022; 14(3): 462. CrossRef - The Potential Role of Gut Microbiota in Alzheimer’s Disease: From Diagnosis to Treatment
Angelica Varesi, Elisa Pierella, Marcello Romeo, Gaia Bavestrello Piccini, Claudia Alfano, Geir Bjørklund, Abigail Oppong, Giovanni Ricevuti, Ciro Esposito, Salvatore Chirumbolo, Alessia Pascale
Nutrients.2022; 14(3): 668. CrossRef - Stochastic microbiome assembly depends on context
Eric W. Jones, Jean M. Carlson, David A. Sivak, William B. Ludington
Proceedings of the National Academy of Sciences.2022;[Epub] CrossRef - Efficacy of Fecal Microbiota Transplantation in Irritable Bowel Syndrome Patients
Amal Mohamed Elhusein, Hammad Ali Fadlalmola
Gastroenterology Nursing.2022; 45(1): 11. CrossRef - Effects of Probiotics, Prebiotics and Synbiotic Supplementation on Cognitive Impairment: A Review
Murugan Mukilan
Journal of Experimental Biology and Agricultural Sciences.2022; 10(1): 1. CrossRef - Multi-Donor Fecal Microbial Transplantation for Critically Ill Patients: Rationale and Standard Operating Procedure
Veronika Řehořová, Ivana Cibulková, Hana Soukupová, František Duška
Future Pharmacology.2022; 2(1): 55. CrossRef - The first report on effect of fecal microbiota transplantation as a complementary treatment in a patient with steroid-refractory Cronkhite-Canada syndrome
Sun Young Kim, Jongbeom Shin, Jin-Seok Park, Boram Cha, Youjeong Seo, Soo-Hyun Park, Jung Hwan Lee, Jun-Seob Kim, Gyesook Kwon
Medicine.2022; 101(12): e29135. CrossRef - Gut Microbiome: Profound Implications for Diet and Disease
Ronald D. Hills Jr., Benjamin A. Pontefract, Hillary R. Mishcon, Cody A. Black, Steven C. Sutton, Cory R. Theberge
Kompass Nutrition & Dietetics.2022; : 1. CrossRef - Bacteria and Bellicosity: Photoperiodic Shifts in Gut Microbiota Drive Seasonal Aggressive Behavior in Male Siberian Hamsters
Elyan K. Shor, Shawn P. Brown, David A. Freeman
Journal of Biological Rhythms.2022; 37(3): 296. CrossRef - Fecal Microbiota and Human Intestinal Fluid Transplantation: Methodologies and Outlook
Ye Chen, Lin Zhiliang, Cui Jiaqu, Lv Xiaoqiong, Zhang Shaoyi, Ma Chunlian, Yan Yinmei, Yang Bo, Zhao Di, Tian Hongliang, Li Ning, Chen Qiyi, Qin Huanlong
Frontiers in Medicine.2022;[Epub] CrossRef - Adverse events of intestinal microbiota transplantation in randomized controlled trials: a systematic review and meta-analysis
Chong Chen, Liyu Chen, Dayong Sun, Cailan Li, Shiheng Xi, Shihua Ding, Rongrong Luo, Yan Geng, Yang Bai
Gut Pathogens.2022;[Epub] CrossRef - Gut microbiota dysbiosis induced by polychlorinated biphenyl 126 contributes to increased brain proinflammatory cytokines: Landscapes from the gut-brain axis and fecal microbiota transplantation
Tongtong Li, Dongcan Tian, Mengtian Lu, Bijiao Wang, Jun Li, Baohua Xu, Hao Chen, Shijin Wu
Ecotoxicology and Environmental Safety.2022; 241: 113726. CrossRef - Induction of mastitis by cow-to-mouse fecal and milk microbiota transplantation causes microbiome dysbiosis and genomic functional perturbation in mice
M. Nazmul Hoque, M. Shaminur Rahman, Tofazzal Islam, Munawar Sultana, Keith A. Crandall, M. Anwar Hossain
Animal Microbiome.2022;[Epub] CrossRef - Alteration of intestinal microecology by oral antibiotics promotes oral squamous cell carcinoma development
Wei Wei, Jia Li, Fan Liu, Miaomiao Wu, Kaixin Xiong, Qing He, Bo Zhang, Ye Deng, Yan Li
Molecular Immunology.2022; 149: 94. CrossRef - Impacts of Gut Microbiota on the Immune System and Fecal Microbiota Transplantation as a Re-Emerging Therapy for Autoimmune Diseases
Ashenafi Feyisa Beyi, Michael Wannemuehler, Paul J. Plummer
Antibiotics.2022; 11(8): 1093. CrossRef - Lung and gut microbiomes in pulmonary aspergillosis: Exploring adjunctive therapies to combat the disease
Liuyang Cai, Peigen Gao, Zeyu Wang, Chenyang Dai, Ye Ning, Macit Ilkit, Xiaochun Xue, Jinzhou Xiao, Chang Chen
Frontiers in Immunology.2022;[Epub] CrossRef - Role of Intestinal Dysbiosis and Nutrition in Rheumatoid Arthritis
Malavikalakshmi Attur, Jose U Scher, Steven B. Abramson, Mukundan Attur
Cells.2022; 11(15): 2436. CrossRef - The effects of functional microbial agents on the soil microbial communities of high-frigid grassland under desertification in Northwest Sichuan
Xia Yuan, Cuiyu Li, Yi Tang, Zhiyu Chen, Chunping Huang
Botanica Serbica.2022; 46(2): 259. CrossRef - Orchestrating the fecal microbiota transplantation: Current technological advancements and potential biomedical application
Manisha Nigam, Abhaya Shikhar Panwar, Rahul Kunwar Singh
Frontiers in Medical Technology.2022;[Epub] CrossRef - Gut microbiota, pathogenic proteins and neurodegenerative diseases
Wei Wei, Shixu Wang, Chongchong Xu, Xuemei Zhou, Xinqing Lian, Lin He, Kuan Li
Frontiers in Microbiology.2022;[Epub] CrossRef - The Interplay between Gut Microbiota and Parkinson’s Disease: Implications on Diagnosis and Treatment
Angelica Varesi, Lucrezia Irene Maria Campagnoli, Foroogh Fahmideh, Elisa Pierella, Marcello Romeo, Giovanni Ricevuti, Marchesi Nicoletta, Salvatore Chirumbolo, Alessia Pascale
International Journal of Molecular Sciences.2022; 23(20): 12289. CrossRef - Early life microbiota transplantation from highly feed-efficient broiler improved weight gain by reshaping the gut microbiota in laying chicken
Abdelmotaleb A. Elokil, Wei Chen, Khalid Mahrose, Mahmoud M. Elattrouny, Khaled F. M. Abouelezz, Hafiz Ishfaq Ahmad, Hua-Zhen Liu, Ahmed A. Elolimy, Mahmoud I. Mandouh, Alzahraa M. Abdelatty, Shijun Li
Frontiers in Microbiology.2022;[Epub] CrossRef - Alternatives Therapeutic Approaches to Conventional Antibiotics: Advantages, Limitations and Potential Application in Medicine
Hiba Alaoui Mdarhri, Rachid Benmessaoud, Houda Yacoubi, Lina Seffar, Houda Guennouni Assimi, Mouhsine Hamam, Rihabe Boussettine, Najoie Filali-Ansari, Fatima Azzahra Lahlou, Idrissa Diawara, Moulay Mustapha Ennaji, Mohamed Kettani-Halabi
Antibiotics.2022; 11(12): 1826. CrossRef - La microbiota intestinal en la salud y en la enfermedad
M.Á. Ortega, C. García-Montero, O. Fraile-Martínez, J. Monserrat, M.A. Álvarez-Mon
Medicine - Programa de Formación Médica Continuada Acreditado.2022; 13(69): 4054. CrossRef - Semi-automated socio-anthropologic analysis of the medical discourse on rheumatoid arthritis: Potential impact on public health
Christine Nardini, Lucia Candelise, Mauro Turrini, Olga Addimanda, Dario Ummarino
PLOS ONE.2022; 17(12): e0279632. CrossRef - First evidence of altered microbiota and intestinal damage and their link to absence epilepsy in a genetic animal model, the WAG/Rij rat
Rita Citraro, Francesca Lembo, Carmen De Caro, Martina Tallarico, Lorena Coretti, Luigi Francesco Iannone, Antonio Leo, Domenico Palumbo, Mariella Cuomo, Elisabetta Buommino, Valentina Nesci, Nadia Marascio, Michelangelo Iannone, Angela Quirino, Roberto R
Epilepsia.2021; 62(2): 529. CrossRef - Fecal microbiota transplantation for COVID-19; a potential emerging treatment strategy
Seyed Aria Nejadghaderi, Ehsan Nazemalhosseini-Mojarad, Hamid Asadzadeh Aghdaei
Medical Hypotheses.2021; 147: 110476. CrossRef - Predictors of failure after fecal microbiota transplantation for recurrent Clostridioides difficile infection: a systematic review and meta-analysis
Raseen Tariq, Maham Hayat, Darrell Pardi, Sahil Khanna
European Journal of Clinical Microbiology & Infectious Diseases.2021; 40(7): 1383. CrossRef - Single Donor FMT Reverses Microbial/Immune Dysbiosis and Induces Clinical Remission in a Rat Model of Acute Colitis
Petra Adamkova, Petra Hradicka, Sona Gancarcikova, Monika Kassayova, Lubos Ambro, Izabela Bertkova, Martin Maronek, Silvia Farkasova Iannaccone, Vlasta Demeckova
Pathogens.2021; 10(2): 152. CrossRef - MALDI-TOF MS: An alternative approach for ribotyping Clostridioides difficile isolates in Brazil
Leandro Gouveia Carneiro, Tatiana Castro Abreu Pinto, Hercules Moura, John Barr, Regina Maria Cavalcanti Pilotto Domingues, Eliane de Oliveira Ferreira
Anaerobe.2021; 69: 102351. CrossRef - Knowledge, attitudes, ethical and social perspectives towards fecal microbiota transplantation (FMT) among Jordanian healthcare providers
Amal G. Al-Bakri, Amal A. Akour, Wael K. Al-Delaimy
BMC Medical Ethics.2021;[Epub] CrossRef - A method for detection of SARS-CoV-2 RNA in healthy human stool: a validation study
Michael P Coryell, Mikhail Iakiviak, Nicole Pereira, Pallavi P Murugkar, Jason Rippe, David B Williams, Taylor Heald-Sargent, L Nelson Sanchez-Pinto, Jairo Chavez, Jessica L Hastie, Rosa L Sava, Christopher Z Lien, Tony T Wang, William J Muller, Michael A
The Lancet Microbe.2021; 2(6): e259. CrossRef - Could the Gut Microbiota Serve as a Therapeutic Target in Ischemic Stroke?
Jiyao Zhang, Qiang Tang, Luwen Zhu, San Jun Shi
Evidence-Based Complementary and Alternative Medicine.2021; 2021: 1. CrossRef - Inflammatory neuropsychiatric disorders and COVID-19 neuroinflammation
Siu Wa Tang, Daiga Helmeste, Brian Leonard
Acta Neuropsychiatrica.2021; 33(4): 165. CrossRef - Gut microbiome colonization and development in neonatal ruminants: Strategies, prospects, and opportunities
Muhammad A. Arshad, Faiz-ul Hassan, Muhammad S. Rehman, Sharon A. Huws, Yanfen Cheng, Ahmad U. Din
Animal Nutrition.2021; 7(3): 883. CrossRef - An Immunologic Compatibility Testing Was Not Useful for Donor Selection in Fecal Microbiota Transplantation for Ulcerative Colitis
Manuel Ponce-Alonso, Carlota García-Hoz, Ana Halperin, Javier Nuño, Pilar Nicolás, Adolfo Martínez-Pérez, Juan Ocaña, Juan Carlos García-Pérez, Antonio Guerrero, Antonio López-Sanromán, Rafael Cantón, Garbiñe Roy, Rosa del Campo
Frontiers in Immunology.2021;[Epub] CrossRef - Micro- and Nanotechnological Delivery Platforms for Treatment of Dysbiosis-Related Inflammatory Bowel Disease
Dingpei Long, Didier Merlin
Nanomedicine.2021; 16(20): 1741. CrossRef - Molecular Communication Between Neuronal Networks and Intestinal Epithelial Cells in Gut Inflammation and Parkinson's Disease
Alice Drobny, Phuong A. Ngo, Markus F. Neurath, Friederike Zunke, Rocío López-Posadas
Frontiers in Medicine.2021;[Epub] CrossRef - Microbiota and epigenetics: promising therapeutic approaches?
Amr El-Sayed, Lotfi Aleya, Mohamed Kamel
Environmental Science and Pollution Research.2021; 28(36): 49343. CrossRef - Effect of probiotics supplementation on disease progression, depression, general health, and anthropometric measurements in relapsing‐remitting multiple sclerosis patients: A systematic review and meta‐analysis of clinical trials
Shahrzad Mirashrafi, Seyedeh Zahra Hejazi Taghanaki, Faezeh Sarlak, Amir Reza Moravejolahkami, Mohammad Ali Hojjati Kermani, Mohsen Haratian
International Journal of Clinical Practice.2021;[Epub] CrossRef - Metabolic Influences of Gut Microbiota Dysbiosis on Inflammatory Bowel Disease
Salma Sultan, Mohammed El-Mowafy, Abdelaziz Elgaml, Tamer A. E. Ahmed, Hebatoallah Hassan, Walid Mottawea
Frontiers in Physiology.2021;[Epub] CrossRef - Mucins, gut microbiota, and postbiotics role in colorectal cancer
Ramesh Pothuraju, Sanjib Chaudhary, Satyanarayana Rachagani, Sukhwinder Kaur, Hemant K. Roy, Michael Bouvet, Surinder K. Batra
Gut Microbes.2021;[Epub] CrossRef - Faecal transplantation and Clostridioides difficile infection
Darija Knežević, Miroslav Petković
Scripta Medica.2021; 52(3): 215. CrossRef - Gut Microbiome as Potential Therapeutics in Multiple Sclerosis
Wen Zhu, Kiersten Dykstra, Lili Zhang, Zongqi Xia
Current Treatment Options in Neurology.2021;[Epub] CrossRef - The Emerging Role of Gut Microbiota in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Current Evidence and Potential Therapeutic Applications
Angelica Varesi, Undine-Sophie Deumer, Sanjana Ananth, Giovanni Ricevuti
Journal of Clinical Medicine.2021; 10(21): 5077. CrossRef - Microbiota, Bacterial Carbonic Anhydrases, and Modulators of Their Activity: Links to Human Diseases?
Amedeo Amedei, Clemente Capasso, Giulia Nannini, Claudiu T. Supuran, Giuseppe Valacchi
Mediators of Inflammation.2021; 2021: 1. CrossRef - Efficacy and Safety of Washed Microbiota Transplantation to Treat Patients with Mild-to-Severe COVID-19 and Suspected of Having Gut Microbiota Dysbiosis: Study Protocol for a Randomized Controlled Trial
Li-hao Wu, Zhi-ning Ye, Ping Peng, Wen-rui Xie, Jia-ting Xu, Xue-yuan Zhang, Harry Hua-xiang Xia, Xing-xiang He
Current Medical Science.2021; 41(6): 1087. CrossRef - Gut Microbiota Implications for Health and Welfare in Farm Animals: A Review
Siyu Chen, Shuyan Luo, Chao Yan
Animals.2021; 12(1): 93. CrossRef - Is the Internet Different from Traditional Mass Media in Promoting Patient Compliance with Mature Treatments?
Xinyi Lu, Runtong Zhang, Wen Wu, Xiaopu Shang, Lily Sun, Xiaomin Zhu
Telemedicine and e-Health.2020; 26(1): 69. CrossRef - Acceptability, tolerability, and safety of fecal microbiota transplantation in patients with active ulcerative colitis (AT&S Study)
Ajit Sood, Arshdeep Singh, Ramit Mahajan, Vandana Midha, Varun Mehta, Yogesh Kumar Gupta, Vikram Narang, Kirandeep Kaur
Journal of Gastroenterology and Hepatology.2020; 35(3): 418. CrossRef - Interplay of Human Gut Microbiome in Health and Wellness
Nirjara Singhvi, Vipin Gupta, Mohita Gaur, Vishal Sharma, Akshita Puri, Yogendra Singh, Gyanendra P. Dubey, Rup Lal
Indian Journal of Microbiology.2020; 60(1): 26. CrossRef - Ethical implications of recruiting universal stool donors for faecal microbiota transplantation
Moiz Mikail, Kieran C O'Doherty, Susan M Poutanen, Susy S Hota
The Lancet Infectious Diseases.2020; 20(3): e44. CrossRef - The greater inflammatory pathway—high clinical potential by innovative predictive, preventive, and personalized medical approach
Maria Giovanna Maturo, Marzia Soligo, Greg Gibson, Luigi Manni, Christine Nardini
EPMA Journal.2020; 11(1): 1. CrossRef - Efficacy and safety of microbiota transfer therapy for the management of autism spectrum disorder in children: a systematic review
Pablo Daniel Estrella Porter, Luis Eduardo Guzmán Freire, Joseth Paulina Adatty Molina, María Verónica Burneo Raza, Henry Alejandro Carrión Celi, Isabel María Espinosa Borja, Andrea Carolina Falconí Páez, Andrés Sebastián Gudiño Vega, María José Jaramillo
F1000Research.2020; 9: 48. CrossRef - Exploring the Effects of Patient Activation in Online Health Communities on Patient Compliance
Xijing Zhang, Runtong Zhang, Xinyi Lu
Telemedicine and e-Health.2020; 26(11): 1373. CrossRef - Therapies to modulate gut microbiota: Past, present and future
Akshita Gupta, Srishti Saha, Sahil Khanna
World Journal of Gastroenterology.2020; 26(8): 777. CrossRef - Faecal microbiota transplantation: Application in treatment of some digestive diseases and safety concerns
Cheng-Yue Jin, Ying Hu, Bo Jin
World Chinese Journal of Digestology.2020; 28(4): 135. CrossRef - The Gut Microbiota and Its Implication in the Development of Atherosclerosis and Related Cardiovascular Diseases
Estefania Sanchez-Rodriguez, Alejandro Egea-Zorrilla, Julio Plaza-Díaz, Jerónimo Aragón-Vela, Sergio Muñoz-Quezada, Luis Tercedor-Sánchez, Francisco Abadia-Molina
Nutrients.2020; 12(3): 605. CrossRef - Clinical care is evolving: The microbiome for advanced practice nurses
Mark B. Lockwood, Stefan J. Green
Journal of the American Association of Nurse Practitioners.2020; 32(4): 290. CrossRef - Microbiome in Multiple Sclerosis: Where Are We, What We Know and Do Not Know
Marina Kleopatra Boziki, Evangelia Kesidou, Paschalis Theotokis, Alexios-Fotios A. Mentis, Eleni Karafoulidou, Mikhail Melnikov, Anastasia Sviridova, Vladimir Rogovski, Alexey Boyko, Nikolaos Grigoriadis
Brain Sciences.2020; 10(4): 234. CrossRef - Role of gut microbiota in cardiovascular diseases
Marko Novakovic, Amit Rout, Thomas Kingsley, Robert Kirchoff, Amteshwar Singh, Vipin Verma, Ravi Kant, Rahul Chaudhary
World Journal of Cardiology.2020; 12(4): 110. CrossRef - Therapeutic advances in non-alcoholic fatty liver disease: A microbiota-centered view
Hui-Ting Chen, Hong-Li Huang, Yong-Qiang Li, Hao-Ming Xu, Yong-Jian Zhou
World Journal of Gastroenterology.2020; 26(16): 1901. CrossRef - Fecal microbiota transplantation for treatment of irritable bowel syndrome
Sofie I Halkjaer, Bobby Lo, Frederik Cold, Alice Hoejer H Christensen, Lise Lotte Gluud, Andreas M Petersen
Cochrane Database of Systematic Reviews.2020;[Epub] CrossRef - Bi-Directional interactions between microbiota and ionizing radiation in head and neck and pelvic radiotherapy – clinical relevance
Nidhya Teresa Joseph, Saligrama R. Shankar, Rekha K. Narasimhamurthy, Satish Bola Sadashiva Rao, Kamalesh Dattaram Mumbrekar
International Journal of Radiation Biology.2020; 96(8): 961. CrossRef - Computational Approaches for Unraveling the Effects of Variation in the Human Genome and Microbiome
Chengsheng Zhu, Maximilian Miller, Zishuo Zeng, Yanran Wang, Yannick Mahlich, Ariel Aptekmann, Yana Bromberg
Annual Review of Biomedical Data Science.2020; 3(1): 411. CrossRef - Engineering the gut microbiota to treat chronic diseases
Noura S. Dosoky, Linda S. May-Zhang, Sean S. Davies
Applied Microbiology and Biotechnology.2020; 104(18): 7657. CrossRef - Gut Microbiota and Response to Immunotherapeutic Drugs in Oncology: More Questions Than Answers
Dhiraj Abhyankar, Kelly T McKee, Pavle Vukojevic
Clinical Medicine Insights: Oncology.2020; 14: 117955492093386. CrossRef - Transplanting fecal material from wild‐type mice fed black raspberries alters the immune system of recipient mice
Yi‐Wen Huang, Pan Pan, Carla Elena Echeveste, Hsin‐Tzu Wang, Kiyoko Oshima, Chien‐Wei Lin, Martha Yearsley, Jianbo Xiao, Jiebiao Chen, Chongde Sun, Jianhua Yu, Li‐Shu Wang
Food Frontiers.2020; 1(3): 253. CrossRef - “Microbiota, symbiosis and individuality summer school” meeting report
Isobel Ronai, Gregor P. Greslehner, Federico Boem, Judith Carlisle, Adrian Stencel, Javier Suárez, Saliha Bayir, Wiebke Bretting, Joana Formosinho, Anna C. Guerrero, William H. Morgan, Cybèle Prigot-Maurice, Salome Rodeck, Marie Vasse, Jacqueline M. Walli
Microbiome.2020;[Epub] CrossRef - Single-Arm, Non-randomized, Time Series, Single-Subject Study of Fecal Microbiota Transplantation in Multiple Sclerosis
Phillip A. Engen, Antonia Zaferiou, Heather Rasmussen, Ankur Naqib, Stefan J. Green, Louis F. Fogg, Christopher B. Forsyth, Shohreh Raeisi, Bruce Hamaker, Ali Keshavarzian
Frontiers in Neurology.2020;[Epub] CrossRef - The Efficacy of Washed Microbiota Transplantation on Helicobacter pylori Eradication: A Pilot Study
Zhi-Ning Ye, Harry Hua-Xiang Xia, Ran Zhang, Lan Li, Li-Hao Wu, Xu-Juan Liu, Wen-Rui Xie, Xing-Xiang He, Fa-Ming Zhang
Gastroenterology Research and Practice.2020; 2020: 1. CrossRef - Regulating Gut Microbiome: Therapeutic Strategy for Rheumatoid Arthritis During Pregnancy and Lactation
Yao Yao, Xiaoyu Cai, Weidong Fei, Fujia Ren, Fengmei Wang, Xiaofei Luan, Fengying Chen, Caihong Zheng
Frontiers in Pharmacology.2020;[Epub] CrossRef - Endobariatrics and Metabolic Endoscopy: Can We Solve the Obesity Epidemic with Our Scope?
Jad Farha, Shahem Abbarh, Zadid Haq, Mohamad I. Itani, Andreas Oberbach, Vivek Kumbhari, Dilhana Badurdeen
Current Gastroenterology Reports.2020;[Epub] CrossRef - The influence of the gut microbiome on obesity
Christy Blanco
Journal of the American Association of Nurse Practitioners.2020; 32(7): 504. CrossRef - Gastrointestinal Microbiome – What We Need to Know in Clinical Practice
Raquel Ortigão, Pedro Pimentel-Nunes, Mário Dinis-Ribeiro, Diogo Libânio
GE - Portuguese Journal of Gastroenterology.2020; 27(5): 336. CrossRef - Gut microbiota, hypertension and chronic kidney disease: Recent advances
Antonio Sircana, Franco De Michieli, Renato Parente, Luciana Framarin, Nicola Leone, Mara Berrutti, Elena Paschetta, Daria Bongiovanni, Giovanni Musso
Pharmacological Research.2019; 144: 390. CrossRef - Fecal microbiota transplantation: Review and update
Jiunn-Wei Wang, Chao-Hung Kuo, Fu-Chen Kuo, Yao-Kuang Wang, Wen-Hung Hsu, Fang-Jung Yu, Huang-Ming Hu, Ping-I. Hsu, Jaw-Yuan Wang, Deng-Chyang Wu
Journal of the Formosan Medical Association.2019; 118: S23. CrossRef - Reverse phenotype transfer via fecal microbial transplantation in inflammatory bowel disease
Robert Liptak, Barbora Gromova, Martin Maronek, Roman Gardlik
Medical Hypotheses.2019; 122: 41. CrossRef - Gut microbiota and obesity: An opportunity to alter obesity through faecal microbiota transplant (FMT)
Patrick Lee, Bruce R. Yacyshyn, Mary B. Yacyshyn
Diabetes, Obesity and Metabolism.2019; 21(3): 479. CrossRef - Patient perception and approval of faecal microbiota transplantation (FMT) as an alternative treatment option for obesity
F. Gundling, S. Roggenbrod, S. Schleifer, M. Sohn, W. Schepp
Obesity Science & Practice.2019; 5(1): 68. CrossRef - Cream Cheese-Derived Lactococcus chungangensis CAU 28 Modulates the Gut Microbiota and Alleviates Atopic Dermatitis in BALB/c Mice
Jong-Hwa Kim, Kiyoung Kim, Wonyong Kim
Scientific Reports.2019;[Epub] CrossRef - Role of gut microbial metabolites in nonalcoholic fatty liver disease
Ze Hua Zhao, Jonathan King‐Lam Lai, Liang Qiao, Jian Gao Fan
Journal of Digestive Diseases.2019; 20(4): 181. CrossRef - Fecal Microbiota Transplantation: An Update on Clinical Practice
Kyeong Ok Kim, Michael Gluck
Clinical Endoscopy.2019; 52(2): 137. CrossRef - Cutting Edge: Probiotics and Fecal Microbiota Transplantation in Immunomodulation
Wenjie Zeng, Jie Shen, Tao Bo, Liangxin Peng, Hongbo Xu, Moussa Ide Nasser, Quan Zhuang, Mingyi Zhao
Journal of Immunology Research.2019; 2019: 1. CrossRef - RecurrentClostridium difficileInfection: Risk Factors, Treatment, and Prevention
Jung Hoon Song, You Sun Kim
Gut and Liver.2019; 13(1): 16. CrossRef - Gut Microbiota Regulation of T Cells During Inflammation and Autoimmunity
Eric M. Brown, Douglas J. Kenny, Ramnik J. Xavier
Annual Review of Immunology.2019; 37(1): 599. CrossRef - Impact of Gut Microbiota Composition on Onset and Progression of Chronic Non-Communicable Diseases
Annalisa Noce, Giulia Marrone, Francesca Di Daniele, Eleonora Ottaviani, Georgia Wilson Jones, Roberta Bernini, Annalisa Romani, Valentina Rovella
Nutrients.2019; 11(5): 1073. CrossRef - Fecal microbiota transplantation for refractory diarrhea in immunocompromised diseases: a pediatric case report
Shuwen Zhong, Jingqing Zeng, Zhaohui Deng, Lirong Jiang, Bin Zhang, Kaihua Yang, Wenyu Wang, Tianao Zhang
Italian Journal of Pediatrics.2019;[Epub] CrossRef - Potential relevance of pig gut content transplantation for production and research
Nuria Canibe, Mark O’Dea, Sam Abraham
Journal of Animal Science and Biotechnology.2019;[Epub] CrossRef - Gut Microbiome: Profound Implications for Diet and Disease
Ronald Hills, Benjamin Pontefract, Hillary Mishcon, Cody Black, Steven Sutton, Cory Theberge
Nutrients.2019; 11(7): 1613. CrossRef - Parkinson’s Disease: The Emerging Role of Gut Dysbiosis, Antibiotics, Probiotics, and Fecal Microbiota Transplantation
Sudhir K Dutta, Sandeep Verma, Vardhmaan Jain, Balarama K Surapaneni, Rakesh Vinayek, Laila Phillips, Padmanabhan P Nair
Journal of Neurogastroenterology and Motility.2019; 25(3): 363. CrossRef - A Novel Animal Model for Regional Microbial Dysbiosis of the Pioneer Microbial Community
Nilusha Malmuthuge, Philip J. Griebel
Frontiers in Microbiology.2019;[Epub] CrossRef - Successional Dynamics in the Gut Microbiome Determine the Success of Clostridium difficile Infection in Adult Pig Models
Stephanie D. Jurburg, Jan J. B. W. J. Cornelissen, Paulo de Boer, Mari A. Smits, Johanna M. J. Rebel
Frontiers in Cellular and Infection Microbiology.2019;[Epub] CrossRef - Pain regulation by gut microbiota: molecular mechanisms and therapeutic potential
Ran Guo, Li-Hua Chen, Chungen Xing, Tong Liu
British Journal of Anaesthesia.2019; 123(5): 637. CrossRef - The Gut Microbiota in Multiple Sclerosis: An Overview of Clinical Trials
Giovanni Schepici, Serena Silvestro, Placido Bramanti, Emanuela Mazzon
Cell Transplantation.2019; 28(12): 1507. CrossRef - Recent Advances in Anti-Aging Medicine
Da-Hye Son, Woo-Jin Park, Yong-Jae Lee
Korean Journal of Family Medicine.2019; 40(5): 289. CrossRef - Electroactive Smart Materials: Novel Tools for Tailoring Bacteria Behavior and Fight Antimicrobial Resistance
Margarida M. Fernandes, Estela O. Carvalho, Senentxu Lanceros-Mendez
Frontiers in Bioengineering and Biotechnology.2019;[Epub] CrossRef - Microbiota transplant therapy and autism: lessons for the clinic
James B. Adams, Thomas J. Borody, Dae-Wook Kang, Alexander Khoruts, Rosa Krajmalnik-Brown, Michael J. Sadowsky
Expert Review of Gastroenterology & Hepatology.2019; 13(11): 1033. CrossRef - The Microbiota and Cancer Cachexia
Kelly M. Herremans, Andrea N. Riner, Miles E. Cameron, Jose G. Trevino
International Journal of Molecular Sciences.2019; 20(24): 6267. CrossRef - THE ROLE OF GUT MICROBIOTA IN THE DEVELOPMENT OF OBESITY
V.A. Volovnikova, A.D. Kotrova, K.A. Ivanova, E.I. Ermolenko, A.N. Shishkin
Juvenis Scientia.2019; (6): 4. CrossRef - Gastrointestinal inflammation by gut microbiota disturbance induces memory impairment in mice
S-E Jang, S-M Lim, J-J Jeong, H-M Jang, H-J Lee, M J Han, D-H Kim
Mucosal Immunology.2018; 11(2): 369. CrossRef - Gut microbiota changes in the extreme decades of human life: a focus on centenarians
Aurelia Santoro, Rita Ostan, Marco Candela, Elena Biagi, Patrizia Brigidi, Miriam Capri, Claudio Franceschi
Cellular and Molecular Life Sciences.2018; 75(1): 129. CrossRef - Interspecies comparison of probiotics isolated from different animals
Amr M. Abdou, Riham H. Hedia, Shimaa T. Omara, Mohamed Abd El-Fatah Mahmoud, Mai M. Kandil, M. A. Bakry
Veterinary World.2018; 11(2): 227. CrossRef - Bacteroidetes Neurotoxins and Inflammatory Neurodegeneration
Yuhai Zhao, Walter J. Lukiw
Molecular Neurobiology.2018; 55(12): 9100. CrossRef - Fecal microbiota transplantation in refractory or recurrent Clostridium difficile infection: a real-life experience in a non-academic center
Ana Ponte, Rolando Pinho, Margarida Mota, Joana Silva, Nuno Vieira, Rosa Oliveira, Jaime Rodrigues, Mafalda Sousa, Isabel Sousa, João Carvalho
Revista Española de Enfermedades Digestivas.2018;[Epub] CrossRef - Fecal Transplantation for Treatment of Clostridium Difficile Infection in Elderly and Debilitated Patients
Tali Friedman-Korn, Dan Meir Livovsky, Nitsan Maharshak, Nathaniel Aviv Cohen, Kalman Paz, Ariella Bar-Gil Shitrit, Eran Goldin, Benjamin Koslowsky
Digestive Diseases and Sciences.2018; 63(1): 198. CrossRef - Gut Microbiota in Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis: Current Applications and Future Perspectives
Fengna Chu, Mingchao Shi, Yue Lang, Donghui Shen, Tao Jin, Jie Zhu, Li Cui
Mediators of Inflammation.2018; 2018: 1. CrossRef - The Gastrointestinal Microbiome: A Review
P.C. Barko, M.A. McMichael, K.S. Swanson, D.A. Williams
Journal of Veterinary Internal Medicine.2018; 32(1): 9. CrossRef - Healthy hosts rule within: ecological forces shaping the gut microbiota
Mariana X. Byndloss, Sandy R. Pernitzsch, Andreas J. Bäumler
Mucosal Immunology.2018; 11(5): 1299. CrossRef - Mature or Emerging? The Impact of Treatment-Related Internet Health Information Seeking on Patients’ Trust in Physicians
Runtong Zhang, Xinyi Lu, Wen Wu, Xiaopu Shang, Manlu Liu
International Journal of Environmental Research and Public Health.2018; 15(9): 1855. CrossRef - Current Evidence in Delivery and Therapeutic Uses of Fecal Microbiota Transplantation in Human Diseases—Clostridium difficile Disease and Beyond
Joshua Stripling, Martin Rodriguez
The American Journal of the Medical Sciences.2018; 356(5): 424. CrossRef - Gut microbes as future therapeutics in treating inflammatory and infectious diseases: Lessons from recent findings
Suprabhat Mukherjee, Nikhilesh Joardar, Subhasree Sengupta, Santi P. Sinha Babu
The Journal of Nutritional Biochemistry.2018; 61: 111. CrossRef - Takotsubo syndrome
Jason Han, Hao Xiang, William E Ridley, Lloyd J Ridley
Journal of Medical Imaging and Radiation Oncology.2018; 62(S1): 50. CrossRef - Fecal microbiota transplantation as a tool to treat and reduce susceptibility to disease in animals
Megan C. Niederwerder
Veterinary Immunology and Immunopathology.2018; 206: 65. CrossRef - Safety of fecal microbiota transplantation in chinese children: A single-center retrospective study
Xin-Yue Zhang, Yi-Zhong Wang, Xiao-Lu Li, Hui Hu, Hai-Feng Liu, Dan Li, Yong-Mei Xiao, Ting Zhang
World Journal of Clinical Cases.2018; 6(16): 1121. CrossRef - THE SCIENTIFIC BACKGROUNDS FOR THE CREATION OF A MICROECOLOGICAL CRYOPRESERVATION OF HUMAN RESOURCES
Boris A. Shenderov, S. M. Yudin, M. P. Shevyreva, E. A. Boyko
Hygiene and sanitation.2018; 97(5): 396. CrossRef - Fecal microbiota transplantation for gastrointestinal disorders
Thomas Malikowski, Sahil Khanna, Darrell S. Pardi
Current Opinion in Gastroenterology.2017; 33(1): 8. CrossRef - Gut microbiota: A player in aging and a target for anti-aging intervention
Alexander M. Vaiserman, Alexander K. Koliada, Francesco Marotta
Ageing Research Reviews.2017; 35: 36. CrossRef - Fecal Microbiota Transplantation
Stephen M. Vindigni, Christina M. Surawicz
Gastroenterology Clinics of North America.2017; 46(1): 171. CrossRef - Gut Microbiota in Health and Probiotics in Functional Bowel Disease
Jai Hyun Rhyou
The Ewha Medical Journal.2017; 40(1): 22. CrossRef - Fecal Microbiota Transplantation for Fibromyalgia: A Case Report and Review of the Literature
T. Thurm, J. N. Ablin, D. Buskila, N. Maharshak
Open Journal of Gastroenterology.2017; 07(04): 131. CrossRef - The Microbiome and Blood Pressure: Can Microbes Regulate Our Blood Pressure?
Souhaila Al Khodor, Bernd Reichert, Ibrahim F. Shatat
Frontiers in Pediatrics.2017;[Epub] CrossRef - Secretory Products of the Human GI Tract Microbiome and Their Potential Impact on Alzheimer's Disease (AD): Detection of Lipopolysaccharide (LPS) in AD Hippocampus
Yuhai Zhao, Vivian Jaber, Walter J. Lukiw
Frontiers in Cellular and Infection Microbiology.2017;[Epub] CrossRef - Effect of gut microbiota on host whole metabolome
Takeo Moriya, Yoshinori Satomi, Shumpei Murata, Hiroshi Sawada, Hiroyuki Kobayashi
Metabolomics.2017;[Epub] CrossRef - The Present Status of Fecal Microbiota Transplantation and Its Value in the Elderly
Yao-Wen Cheng, Monika Fischer
Current Treatment Options in Gastroenterology.2017; 15(3): 349. CrossRef - Modulation of Multiple Sclerosis and Its Animal Model Experimental Autoimmune Encephalomyelitis by Food and Gut Microbiota
Ward J. van den Hoogen, Jon D. Laman, Bert A. ’t Hart
Frontiers in Immunology.2017;[Epub] CrossRef - Can fecal microbiota transplantation cure irritable bowel syndrome?
Sofie Ingdam Halkjær, Anders Watt Boolsen, Stig Günther, Alice Højer Christensen, Andreas Munk Petersen
World Journal of Gastroenterology.2017; 23(22): 4112. CrossRef - Innovation in microbiome-based strategies for promoting metabolic health
Marina Romaní-Pérez, Ana Agusti, Yolanda Sanz
Current Opinion in Clinical Nutrition & Metabolic Care.2017; 20(6): 484. CrossRef - Faecal microbiota transplantation: establishment of a clinical application framework
Simon M.D. Jørgensen, Mette M. Hansen, Christian Erikstrup, Jens F. Dahlerup, Christian L. Hvas
European Journal of Gastroenterology & Hepatology.2017; 29(11): e36. CrossRef - Faecal microbiota transplantation in patients with Clostridium difficile and significant comorbidities as well as in patients with new indications: A case series
Perttu Lahtinen, Eero Mattila, Veli-Jukka Anttila, Jyrki Tillonen, Matti Teittinen, Pasi Nevalainen, Seppo Salminen, Reetta Satokari, Perttu Arkkila
World Journal of Gastroenterology.2017; 23(39): 7174. CrossRef - Is Expansion of Fecal Microbiota Transplantation Available?
Wan Soo Kim, Hyun Jin Kim
Korean Journal of Gastroenterology.2017; 70(4): 211. CrossRef - Enteric Microbiome Markers as Early Predictors of Clinical Outcome in Allogeneic Hematopoietic Stem Cell Transplant: Results of a Prospective Study in Adult Patients
Nicasio Mancini, Raffaella Greco, Renée Pasciuta, Maria Chiara Barbanti, Giacomo Pini, Olivia Beatrice Morrow, Mara Morelli, Luca Vago, Nicola Clementi, Fabio Giglio, Maria Teresa Lupo Stanghellini, Alessandra Forcina, Laura Infurnari, Sarah Marktel, Andr
Open Forum Infectious Diseases.2017;[Epub] CrossRef - Gleaning Insights from Fecal Microbiota Transplantation and Probiotic Studies for the Rational Design of Combination Microbial Therapies
Lauren E. Hudson, Sarah E. Anderson, Anita H. Corbett, Tracey J. Lamb
Clinical Microbiology Reviews.2017; 30(1): 191. CrossRef - Engineering Diagnostic and Therapeutic Gut Bacteria
Brian P. Landry, Jeffrey J. Tabor, Robert Allen Britton, Patrice D. Cani
Microbiology Spectrum.2017;[Epub] CrossRef - Farmen i tarmen
Siv Kjølsrud Bøhn
Norsk tidsskrift for ernæring.2017; 15(2): 24. CrossRef - Microbiota and pathogen ‘pas de deux’: setting up and breaking down barriers to intestinal infection
Elizabeth S. McKenney, Melissa M. Kendall, Brooke Napier
Pathogens and Disease.2016; 74(5): ftw051. CrossRef - Système immunitaire muqueux et microbiote intestinal : Histoire d’une symbiose
Marie-Nathalie Kolopp-Sarda
Revue Francophone des Laboratoires.2016; 2016(484): 39. CrossRef - The gut microbiome and HIV-1 pathogenesis
Stephanie M. Dillon, Daniel N. Frank, Cara C. Wilson
AIDS.2016; 30(18): 2737. CrossRef - Fecal Microbiota Transplantation and the Brain Microbiota in Neurological Diseases
Marco Ruggiero
Clinical Endoscopy.2016; 49(6): 579. CrossRef - Modulation of microbiota as treatment for intestinal inflammatory disorders: An uptodate
Antonella Gallo, Giovanna Passaro, Antonio Gasbarrini, Raffaele Landolfi, Massimo Montalto
World Journal of Gastroenterology.2016; 22(32): 7186. CrossRef
- Antiaging Strategies and Remedies: A Landscape of Research Progress and Promise
- 28,795 View
- 796 Download
- 181 Web of Science
- 172 Crossref

- Tracheal Involvement in Crohn Disease: the First Case in Korea
- Seunghyun Park, Jongha Park, Hyun-Kuk Kim, Ji Yeon Kim, So Chong Hur, Ju Hyung Lee, Jae Won Jung, Juwon Lee
- Clin Endosc 2016;49(2):202-206. Published online February 16, 2016
- DOI: https://doi.org/10.5946/ce.2015.059
- Correction in: Clin Endosc 2016;49(3):310
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Respiratory involvement in Crohn disease (CD) is rare condition with only about a dozen reported cases. We report the first case of CD with tracheal involvement in Korea. An 18-year-old woman with CD was hospitalized because of coughing, dyspnea, and fever sustained for 3 weeks. Because she had stridor in her neck, we performed computed tomography of the neck, which showed circumferential wall thickening of the larynx and hypopharynx. Bronchoscopy revealed mucosal irregularity, ulceration, and exudates debris in the proximal trachea, and bronchial biopsy revealed chronic inflammation with granulation tissue. Based on these findings, we suspected CD with tracheal involvement and began administering intravenous methylprednisolone at 1 mg/kg per day, after which her symptoms and bronchoscopic findings improved.
-
Citations
Citations to this article as recorded by- Tracheobronchitis and laryngitis associated with Crohn's disease
Shogo Nakai, Moeko Morikawa, Toshiya Hiramatsu, Yurina Murakami, Koji Nishimoto, Sayomi Matsushima, Masanori Harada, Tomohiro Uto, Jun Sato, Shiro Imokawa, Takafumi Suda
Respiratory Medicine Case Reports.2023; 46: 101918. CrossRef - Tracheobronchial Crohn’s Disease: Case Report and Systematic Review of the Literature
Rao G Raghava, Vishal Sharma, Srikant Kashinath Malegaonkar, Sahajal Dhooria, Inderpaul Singh Sehgal, Kuruswamy Thurai Prasad, Amanjit Bal, Ritesh Agarwal, Valliappan Muthu
Inflammatory Bowel Diseases.2022; 28(3): e33. CrossRef - Granulomatous tracheo‐bronchitis from Crohn's disease
Amr J. Alwakeel, Stéphane Beaudoin
Respirology Case Reports.2022;[Epub] CrossRef - Nonasthmatic eosinophilic bronchitis in an ulcerative colitis patient – a putative adverse reaction to mesalazine: A case report and review of literature
Andrei Tudor Cernomaz, Gabriela Bordeianu, Cristina Terinte, Cristina Maria Gavrilescu
World Journal of Clinical Cases.2020; 8(18): 4162. CrossRef - Obstrucción de la vía aérea central por enfermedad inflamatoria intestinal y rescate terapéutico con membrana de oxigenación extracorpórea
M. Ramírez-Romero, B. Hernández-Alonso, C. García-Polo, A.J. Abraldes-Bechiarelli, A. Garrino-Fernández, A. Gordillo-Brenes
Medicina Intensiva.2018; 42(5): 317. CrossRef - Central airway obstruction due to inflammatory bowel disease and rescue with extracorporeal membrane oxygenation
M. Ramírez-Romero, B. Hernández-Alonso, C. García-Polo, A.J. Abraldes-Bechiarelli, A. Garrino-Fernández, A. Gordillo-Brenes
Medicina Intensiva (English Edition).2018; 42(5): 317. CrossRef - MORPHOMETRIC DIFFERENTIAL DIAGNOSIS OF INTESTINAL TUBERCULOSIS AND CROHN’S DISEASE
TA A Fedorina, GV V Nedugov
Science and Innovations in Medicine.2018; 3(3): 57. CrossRef - Managing Head and Neck Malignancy Arising in a Field of Crohn Disease Inflammation: Report of a Case
Christina Yver, Darshana Jhala, Amanda Muir, Devraj Basu
Ear, Nose & Throat Journal.2017; 96(10-11): E1. CrossRef
- Tracheobronchitis and laryngitis associated with Crohn's disease
- 8,596 View
- 83 Download
- 9 Web of Science
- 8 Crossref

- Computed Tomography Enterography for Evaluation of Inflammatory Bowel Disease
- Min Jung Park, Joon Seok Lim
- Clin Endosc 2013;46(4):327-366. Published online July 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.4.327
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Computed tomography enterography (CTE) has become a main modality for the evaluation of inflammatory bowel disease (IBD). It simultaneously offers visualization of the small bowel and extraintestinal status, which is helpful for diagnosing IBD. Crohn disease has long segmental enhancing wall thickening related with the eccentric longitudinal distribution. In addition, mural stratification, fibrofatty proliferation, positive comb sign by increased mesenteric vascularity and internal/perianal fistula are characteristics of Crohn disease and can be identified on CTE. Short segmental inflammatory wall thickening and the central low attenuated lymph nodes are favorable CT finding of intestinal tuberculosis. A geographic, relatively large, and deep penetrating ulcer with bowel wall thickening and mural hyperenhancement in ileocecal area are characteristics of intestinal Behcet disease. Each of CTE findings for the IBDs is helpful for differential diagnosis. The main disadvantage of this technique is the requisite radiation exposure of patients, particularly in young patients. However, recent development of advanced CT techniques is promising for radiation dose reduction without compromising diagnostic image quality.
-
Citations
Citations to this article as recorded by- Differential diagnosis of Crohn’s disease and intestinal tuberculosis based on ATR-FTIR spectroscopy combined with machine learning
Yuan-Peng Li, Tian-Yu Lu, Fu-Rong Huang, Wei-Min Zhang, Zhen-Qiang Chen, Pei-Wen Guang, Liang-Yu Deng, Xin-Hao Yang
World Journal of Gastroenterology.2024; 30(10): 1377. CrossRef - Imaging of Gastrointestinal Tract Ailments
Boyang Sun, Jingang Liu, Silu Li, Jonathan F. Lovell, Yumiao Zhang
Journal of Imaging.2023; 9(6): 115. CrossRef - Computed tomography enterography-based multiregional radiomics model for differential diagnosis of Crohn’s disease from intestinal tuberculosis
Tong Gong, Mou Li, Hong Pu, Long-lin Yin, Sheng-kun Peng, Zhou Zhou, Mi Zhou, Hang Li
Abdominal Radiology.2023; 48(6): 1900. CrossRef - The treatment principles and targets for intestinal Behcet’s disease
Kun He, Dong Wu
Therapeutic Advances in Gastroenterology.2023; 16: 175628482311672. CrossRef - Differentiating gastrointestinal tuberculosis and Crohn's disease- a comprehensive review
Arup Choudhury, Jasdeep Dhillon, Aravind Sekar, Pankaj Gupta, Harjeet Singh, Vishal Sharma
BMC Gastroenterology.2023;[Epub] CrossRef - New score models for assessing disease activity in Crohn's disease based on bowel ultrasound and biomarkers: Ideal surrogates for endoscopy or imaging
Qingyang Zhou, Qingli Zhu, Wei Liu, Wenbo Li, Li Ma, Mengsu Xiao, Jingjuan Liu, Hong Yang, Jiaming Qian
Clinical and Translational Science.2023; 16(9): 1639. CrossRef - Appearance of the Bowel and Mesentery During Surgery Is Not Predictive of Postoperative Recurrence After Ileocecal Resection for Crohn’s Disease: A Prospective Monocentric Study
Gabriele Bislenghi, Julie Van Den Bossch, Steffen Fieuws, Albert Wolthuis, Marc Ferrante, Gert de Hertogh, Severine Vermeire, André D’Hoore
Inflammatory Bowel Diseases.2023;[Epub] CrossRef - Results of the Eighth Scientific Workshop of ECCO: Pathophysiology and Risk Factors of Postoperative Crohn’s Disease Recurrence after an Ileocolonic Resection
Pauline Rivière, Gabriele Bislenghi, Nassim Hammoudi, Bram Verstockt, Steven Brown, Melissa Oliveira-Cunha, Willem Bemelman, Gianluca Pellino, Paulo Gustavo Kotze, Gabriele Dragoni, Mariangela Allocca, Nurulamin M Noor, Lieven Pouillon, Míriam Mañosa, Edo
Journal of Crohn's and Colitis.2023; 17(10): 1557. CrossRef - How can the surgeon reduce recurrence after surgery for ileocolic Crohn's disease?
Steven R. Brown
Seminars in Colon and Rectal Surgery.2023; 34(4): 100985. CrossRef - Machine Learning and Radiomics: Changing the Horizon of Crohn’s Disease Assessment
Raseen Tariq, Saam Dilmaghani
Inflammatory Bowel Diseases.2023;[Epub] CrossRef - Magnetic resonance colonography with intestine-absorbable nanoparticle contrast agents in evaluation of colorectal inflammation
Xue Dong, Jingfeng Luo, Pengxun Lan, Xiuyu Guo, Xin Zhao, Xiaoyan Wang, Fei Zhou, Qiangfeng Wang, Hong Yuan, Jihong Sun
European Radiology.2021; 31(7): 4615. CrossRef - Intestinal tuberculosis or Crohn’s disease: a review of the diagnostic models designed to differentiate between these two gastrointestinal diseases
Julajak Limsrivilai, Nonthalee Pausawasdi
Intestinal Research.2021; 19(1): 21. CrossRef - Diagnostic role of computed tomography enterography (CTE) in assessment of intra-mural and extra-intestinal CT findings in active Crohn’s disease (CD)
Rasha Mostafa Mohamed Ali, Mai Bahgat Ibrahim Ghonimy
Egyptian Journal of Radiology and Nuclear Medicine.2021;[Epub] CrossRef - Computed tomography enterography for crohn’s disease: correlation between the imaging findings and histopathologic scoring system
Liang Ma, Xing Shen, Yi-Jing Chen, Qi Zhang, Bo Li, Wei Zhang
Abdominal Radiology.2021; 46(9): 4121. CrossRef - Wireless Capsule Endoscopy for Diagnosis and Management of Post-Operative Recurrence of Crohn’s Disease
Adil Mir, Vu Q. Nguyen, Youssef Soliman, Dario Sorrentino
Life.2021; 11(7): 602. CrossRef - COMPARATIVE ANALYSIS OF TWO ORAL CONTRAST AGENT VOLUMES FOR COMPUTED TOMOGRAPHY ENTEROGRAPHY IN CROHN’S DISEASE PATIENTS
Fernanda Lofiego RENOSTO, Jaqueline Ribeiro de BARROS, Guilherme A BERTOLDI, Sergio Ribeiro MARRONE, Ligia Yukie SASSAKI, Rogerio SAAD-HOSSNE
Arquivos de Gastroenterologia.2021; 58(3): 322. CrossRef - Crohn’s disease at radiological imaging: focus on techniques and intestinal tract
Giuseppe Cicero, Silvio Mazziotti
Intestinal Research.2021; 19(4): 365. CrossRef - Computed Tomography Enterography Demonstrates Association to Histopathological Grading of Small Bowel Crohn’s Activity
Husam H Mansour, Yasser S Alajerami, Ahmed A Najim, Khaled M Abushab
Electronic Journal of General Medicine.2021; 18(6): em330. CrossRef - Autoinflammatory diseases in childhood, part 2: polygenic syndromes
María Navallas, Emilio J. Inarejos Clemente, Estíbaliz Iglesias, Mónica Rebollo-Polo, Joan Calzada Hernández, Oscar M. Navarro
Pediatric Radiology.2020; 50(3): 431. CrossRef - Diagnostic efficacy of double-balloon enteroscopy in patients with suspected isolated small bowel Crohn’s disease
Zihan Huang, Xiang Liu, Fei Yang, Guoxin Wang, Nan Ge, Sheng Wang, Jintao Guo, Siyu Sun
BMC Gastroenterology.2020;[Epub] CrossRef - Evidence-based diagnosis and clinical practice guidelines for intestinal Behçet’s disease 2020 edited by Intractable Diseases, the Health and Labour Sciences Research Grants
Kenji Watanabe, Satoshi Tanida, Nagamu Inoue, Reiko Kunisaki, Kiyonori Kobayashi, Masakazu Nagahori, Katsuhiro Arai, Motoi Uchino, Kazutaka Koganei, Taku Kobayashi, Mitsuhiro Takeno, Fumiaki Ueno, Takayuki Matsumoto, Nobuhisa Mizuki, Yasuo Suzuki, Tadakaz
Journal of Gastroenterology.2020; 55(7): 679. CrossRef - Retrospective study of the differential diagnosis between cryptogenic multifocal ulcerous stenosing enteritis and small bowel Crohn’s disease
Dan Chen, Wei Liu, Weixun Zhou, Weiyang Zheng, Dong Wu, Jiaming Qian
BMC Gastroenterology.2020;[Epub] CrossRef - The Role of Active Inflammation and Surgical Therapy in Crohn’s Disease Recurrence
S. Ingallinella, M. Campanelli, A. Antonelli, C. Arcudi, V. Bellato, A. Divizia, M. Franceschilli, L. Petagna, B. Sensi, S. Sibio, L. Siragusa, G. S. Sica, Lukas J.A.C. Hawinkels
Gastroenterology Research and Practice.2020; 2020: 1. CrossRef - The Mesentery, Systemic Inflammation, and Crohn’s Disease
Edgardo D Rivera, John Calvin Coffey, Dara Walsh, Eli D Ehrenpreis
Inflammatory Bowel Diseases.2019; 25(2): 226. CrossRef - Intestinal fibrosis
Marco Vincenzo Lenti, Antonio Di Sabatino
Molecular Aspects of Medicine.2019; 65: 100. CrossRef - Evaluation of CT enterography findings for endoscopic complete remission after anti-TNF-α therapy in patients with Crohn’s disease
Jieun Kim, Seung Ho Kim, Tae Oh Kim
Acta Radiologica.2019; 60(10): 1200. CrossRef - Crohn's disease: A retrospective analysis between computed tomography enterography, colonoscopy, and histopathology
C. Saade, L. Nasr, A. Sharara, K. Barada, A. Soweid, F. Murad, A. Tawil, D. Ghieh, K. Asmar, H. Tamim, N.J. Khoury
Radiography.2019; 25(4): 349. CrossRef - Cinematic rendering: a new imaging approach for ulcerative colitis
Jun Yang, Xu Liu, Chengde Liao, Qinqing Li, Dan Han
Japanese Journal of Radiology.2019; 37(8): 590. CrossRef - CT ENTEROCLYSIS VERSUS CT ENTEROGRAPHY IN THE EVALUATION OF SUSPECTED SMALL BOWEL PATHOLOGIES - A CASE SERIES
Monisha Jacob, Jeffrey Ralph, Praveen Kumar Vasanthraj, Prithiviraj P. V, Sushmitha M. S
Journal of Evidence Based Medicine and Healthcare.2019; 6(7): 458. CrossRef - The effect of without using anisodamine during CT enterography on image quality, diagnostic performance and latent side effects
Didi Wen, Jian Xu, Ying Liu, Rui An, Jian Li, Hongliang Zhao, Minwen Zheng
Clinical Imaging.2018; 48: 106. CrossRef - Comparison of diagnostic performance between 1 millisievert CT enterography and half-standard dose CT enterography for evaluating active inflammation in patients with Crohn’s disease
Jung Hee Son, Seung Ho Kim, Een Young Cho, Kyeong Hwa Ryu
Abdominal Radiology.2018; 43(7): 1558. CrossRef - Management of Crohn’s Disease and Complications in Patients With Ostomies
Xinying Wang, Bo Shen
Inflammatory Bowel Diseases.2018; 24(6): 1167. CrossRef - Value of dual-energy CT enterography in the analysis of pathological bowel segments in patients with Crohn's disease
A.M. Villanueva Campos, G. Tardáguila de la Fuente, E. Utrera Pérez, C. Jurado Basildo, D. Mera Fernández, C. Martínez Rodríguez
Radiología (English Edition).2018; 60(3): 223. CrossRef - Valor de la enterografía por tomografía computarizada con doble energía en el análisis de segmentos intestinales patológicos en pacientes con enfermedad de Crohn
A.M. Villanueva Campos, G. Tardáguila de la Fuente, E. Utrera Pérez, C. Jurado Basildo, D. Mera Fernández, C. Martínez Rodríguez
Radiología.2018; 60(3): 223. CrossRef - Role of surgery in the management of Crohn's disease
Alessandro Fichera, Francisco Schlottmann, Mukta Krane, Greta Bernier, Erin Lange
Current Problems in Surgery.2018; 55(5): 162. CrossRef - Intestinal Behçet Disease: Evaluation With MR Enterography—A Case-Control Study
Elif Peker, Ayşe Erden, İlhan Erden, Nurşen Düzgün
American Journal of Roentgenology.2018; 211(4): 767. CrossRef - 18 F-FDG PET/CT in Extensive Graft-Versus-Host Disease of the Gastrointestinal Tract Following Autologous Stem Cell Transplantation
Danijela Dejanovic, Annemarie Amtoft, Annika Loft
Diagnostics.2018; 8(4): 72. CrossRef - The Association of Coloproctology of Great Britain and Ireland consensus guidelines in surgery for inflammatory bowel disease
S. R. Brown, N. S. Fearnhead, O. D. Faiz, J. F. Abercrombie, A. G. Acheson, R. G. Arnott, S. K. Clark, S. Clifford, R. J. Davies, M. M. Davies, W. J. P. Douie, M. G. Dunlop, J. C. Epstein, M. D. Evans, B. D. George, R. J. Guy, R. Hargest, A. B. Hawthorne,
Colorectal Disease.2018; 20(S8): 3. CrossRef - Meta-Analytic Bayesian Model For Differentiating Intestinal Tuberculosis from Crohn's Disease
Julajak Limsrivilai, Andrew B Shreiner, Ananya Pongpaibul, Charlie Laohapand, Rewat Boonanuwat, Nonthalee Pausawasdi, Supot Pongprasobchai, Sathaporn Manatsathit, Peter D R Higgins
American Journal of Gastroenterology.2017; 112(3): 415. CrossRef - Structured reporting of CT enterography for inflammatory bowel disease: effect on key feature reporting, accuracy across training levels, and subjective assessment of disease by referring physicians
Benjamin Wildman-Tobriner, Brian C. Allen, Mustafa R. Bashir, Morgan Camp, Chad Miller, Lauren E. Fiorillo, Alan Cubre, Sanaz Javadi, Alex D. Bibbey, Wendy L. Ehieli, Nancy McGreal, Reinaldo Quevedo, Julie K. Thacker, Maciej Mazurowski, Tracy A. Jaffe
Abdominal Radiology.2017; 42(9): 2243. CrossRef - Magnetic Resonance Enterography Findings of Intestinal Behçet Disease in a Child
Tommaso D’Angelo, Romina Gallizzi, Claudio Romano, Giuseppe Cicero, Silvio Mazziotti
Case Reports in Radiology.2017; 2017: 1. CrossRef - Nanoparticle‐based imaging of inflammatory bowel disease
Yingwei Wu, Karen Briley, Xiaofeng Tao
WIREs Nanomedicine and Nanobiotechnology.2016; 8(2): 300. CrossRef - Misdiagnosis and Mistherapy of Crohn's Disease as Intestinal Tuberculosis
Jiang-Peng Wei, Xiao-Yan Wu, Sen-Yang Gao, Qiu-Yu Chen, Tong Liu, Gang Liu
Medicine.2016; 95(1): e2436. CrossRef - Role of Computed Tomography in Pediatric Abdominal Conditions
Anu Eapen, Sridhar Gibikote
The Indian Journal of Pediatrics.2016; 83(7): 691. CrossRef - The Role of the Mesentery in Crohnʼs Disease
Yi Li, Weiming Zhu, Lugen Zuo, Bo Shen
Inflammatory Bowel Diseases.2016; 22(6): 1483. CrossRef - Diagnostic imaging and radiation exposure in inflammatory bowel disease
Nekisa Zakeri, Richard CG Pollok
World Journal of Gastroenterology.2016; 22(7): 2165. CrossRef
- Differential diagnosis of Crohn’s disease and intestinal tuberculosis based on ATR-FTIR spectroscopy combined with machine learning
- 12,333 View
- 155 Download
- 46 Crossref

- Small Bowel Endoscopy in Inflammatory Bowel Disease
- Hirokazu Yamagami, Kenji Watanabe, Noriko Kamata, Mitsue Sogawa, Tetsuo Arakawa
- Clin Endosc 2013;46(4):321-326. Published online July 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.4.321
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Crohn disease (CD) is a chronic inflammatory bowel disease that affects the entire gastrointestinal tract but is most frequently localized to the large and small bowel. Small bowel endoscopy helps with the differential diagnosis of CD in suspected CD patients. Early diagnosis of CD is preferable for suspected CD conditions to improve chronic inflammatory infiltrates, fibrosis. Small bowel endoscopy can help with the early detection of active disease, thus leading to early therapy before the onset of clinical symptoms of established CD. Some patients with CD have mucosal inflammatory changes not in the terminal ileum but in the proximal small bowel. Conventional ileocolonoscopy cannot detect ileal involvement proximal to the terminal ileum. Small bowel endoscopy, however, can be useful for evaluating these small bowel involvements in patients with CD. Small bowel endoscopy by endoscopic balloon dilation (EBD) enables the treatment of small bowel strictures in patients with CD. However, many practical issues still need to be addressed, such as endoscopic findings for early detection of CD, application compared with other imaging modalities, determination of the appropriate interval for endoscopic surveillance of small bowel lesions in patients with CD, and long-term prognosis after EBD.
-
Citations
Citations to this article as recorded by- Video capsule endoscopy in inflammatory bowel disease
Kenji J.L. Limpias Kamiya, Naoki Hosoe, Yukie Hayashi, Takaaki Kawaguchi, Kaoru Takabayashi, Haruhiko Ogata, Takanori Kanai
DEN Open.2022;[Epub] CrossRef - Usefulness of magnetic resonance enterography in the clinical decision-making process for patients with inflammatory bowel disease
Laura Ramos López, Alejandro Hernández Camba, Iago Rodríguez-Lago, Marta Carrillo Palau, Luis Cejas Dorta, Ainara Elorza, Inmaculada Alonso Abreu, Milagros Vela, Alba Hidalgo, Noemi Hernández Álvarez-Builla, G. Esther Rodríguez, Yolanda Rodríguez, Carlos
Gastroenterología y Hepatología.2020; 43(8): 439. CrossRef - Usefulness of magnetic resonance enterography in the clinical decision-making process for patients with inflammatory bowel disease
Laura Ramos López, Alejandro Hernández Camba, Iago Rodríguez-Lago, Marta Carrillo Palau, Luis Cejas Dorta, Ainara Elorza, Inmaculada Alonso Abreu, Milagros Vela, Alba Hidalgo, Noemi Hernández Álvarez-Builla, G. Esther Rodríguez, Yolanda Rodríguez, Carlos
Gastroenterología y Hepatología (English Edition).2020; 43(8): 439. CrossRef - Different clinical outcomes in Crohn’s disease patients with esophagogastroduodenal, jejunal, and proximal ileal disease involvement: is L4 truly a single phenotype?
Ren Mao, Rui-Han Tang, Yun Qiu, Bai-Li Chen, Jing Guo, Sheng-Hong Zhang, Xue-Hua Li, Rui Feng, Yao He, Zi-Ping Li, Zhi-Rong Zeng, Rami Eliakim, Shomron Ben-Horin, Min-Hu Chen
Therapeutic Advances in Gastroenterology.2018; 11: 175628481877793. CrossRef - Capsule endoscopy: Current status and role in Crohn’s disease
Loredana Goran, Ana Maria Negreanu, Ana Stemate, Lucian Negreanu
World Journal of Gastrointestinal Endoscopy.2018; 10(9): 184. CrossRef - Pilot study of endoscopic retrograde 3-dimensional – computed tomography enteroclysis for the assessment of Crohn’s disease
Hiroki Tanabe, Takahiro Ito, Yuhei Inaba, Katsuyoshi Ando, Yoshiki Nomura, Nobuhiro Ueno, Shin Kashima, Kentaro Moriichi, Mikihiro Fujiya, Toshikatsu Okumura
European Journal of Radiology Open.2017; 4: 58. CrossRef - In-vivo Axial-strain Sonoelastography Helps Distinguish Acutely-inflamed from Fibrotic Terminal Ileum Strictures in Patients with Crohn's Disease: Preliminary Results
Luca Maria Sconfienza, Flaminia Cavallaro, Valentino Colombi, Luca Pastorelli, Gianeugenio Tontini, Lorenzo Pescatori, Anastassia Esseridou, Edoardo Savarino, Carmelo Messina, Roberto Casale, Giovanni Di Leo, Francesco Sardanelli, Maurizio Vecchi
Ultrasound in Medicine & Biology.2016; 42(4): 855. CrossRef - Video Capsule Endoscopy in Patients with Chronic Abdominal Pain with or without Associated Symptoms: A Retrospective Study
Jeremy Egnatios, Khushboo Kaushal, Denise Kalmaz, Amir Zarrinpar, Peyman Björklund
PLOS ONE.2015; 10(4): e0126509. CrossRef
- Video capsule endoscopy in inflammatory bowel disease
- 7,437 View
- 53 Download
- 8 Crossref

- The Role of Colonoscopy in Inflammatory Bowel Disease
- Yong Gil Kim, Byung Ik Jang
- Clin Endosc 2013;46(4):317-320. Published online July 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.4.317
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub An endoscopic evaluation, particularly ileocolic mucosal and histological findings, is essential for the diagnosis of inflammatory bowel disease (IBD). The introduction of antitumor necrosis factor agents has changed the therapeutic paradigm of patients with IBD, but an endoscopic evaluation is more important to guide therapeutic decision-making. In the future, endoscopy with a histological evaluation will be increasingly used in patients with IBD. Both Crohn colitis and ulcerative colitis result in an increased incidence of colorectal carcinoma. Thus, surveillance colonoscopy is important to detect early neoplastic lesions. Surveillance ileocolonoscopy has also changed recently from multiple random biopsies to pancolonic dye spraying with targeted biopsies of abnormal areas.
-
Citations
Citations to this article as recorded by- YouTube® en español como fuente de información para pacientes con enfermedad inflamatoria intestinal
C.E. Lombo-Moreno, O.M. Muñoz-Velandia, D.G. Fernández-Ávila, J.E. Barahona-Correa, V. López-Ramírez, A. Rodriguez-Varon
Revista de Gastroenterología de México.2024; 89(2): 176. CrossRef - YouTube® in Spanish as a source of information for patients with inflammatory bowel disease
C.E. Lombo-Moreno, O.M. Muñoz-Velandia, D.G. Fernández-Ávila, J.E. Barahona-Correa, V. López-Ramírez, A. Rodriguez-Varon
Revista de Gastroenterología de México (English Edition).2024; 89(2): 176. CrossRef - Role of MR enterography versus ileo-colonoscopy in the assessment of inflammatory bowel diseases
Rasha Mostafa Mohamed Ali, Aya Fawzy Abd El Salam, Ismail Anwar, Hany Shehab, Maryse Youssef Awadallah
Egyptian Journal of Radiology and Nuclear Medicine.2023;[Epub] CrossRef - HISTOPATHOLOGICAL FEATURES IN RELAPSE OF ULCERATIVE COLITIS.
Saroash Iqbal, Aman Ur Rehman, Nausheen Henna, Zara Madiha, Sahar Moeed, Uzma Aslam
JAIMC: Journal of Allama Iqbal Medical College.2023;[Epub] CrossRef - Prevalence and risk factors of cytomegalovirus colitis in inflammatory bowel disease patients in Riyadh, Saudi Arabia: A tertiary center experience
Yazeed Alotaibi, Abed AlLehibi, Abdullah Almtawa, Nawaf Alotaibi, Adel Alghamdi, Saad Alrajhi, Adel AlQutub, Ahmad AlEid, Abdulrhman Alamr, Bashaar Al Ibrahim, Mohammed Alahmari, Hussam Alhamidi, Shameem Ahmad, Fouad Alshammari, Fahad Almotawa, Youssef Al
Saudi Journal of Medicine and Medical Sciences.2023; 11(4): 305. CrossRef - Mango (Mangifera indica L.) polyphenols reduce IL-8, GRO, and GM-SCF plasma levels and increase Lactobacillus species in a pilot study in patients with inflammatory bowel disease
Hyemee Kim, Vinicius P. Venancio, Chuo Fang, Andrew W. Dupont, Stephen T Talcott, Susanne U Mertens-Talcott
Nutrition Research.2020; 75: 85. CrossRef - Can microscopic ileitis in patients with clinically suspected inflammatory bowel disease predict the future?
Fadi Abu Baker, Jesus Alonso Z’cruz De La Garza, Smadar Nafrin, Amir Mari, Muhammed Suki, Baruch Ovadia, Oren Gal, Yael Kopelamn
BMC Gastroenterology.2020;[Epub] CrossRef - Breath Analysis Using eNose and Ion Mobility Technology to Diagnose Inflammatory Bowel Disease—A Pilot Study
Tiele, Wicaksono, Kansara, Arasaradnam, Covington
Biosensors.2019; 9(2): 55. CrossRef - The value of mRNA expression of S100A8 and S100A9 as blood-based biomarkers of inflammatory bowel disease
Tayebeh Azramezani Kopi, Azade Amini Kadijani, Hadi Parsian, Shabnam Shahrokh, Hamid Asadzadeh Aghdaei, Alireza Mirzaei, Hedieh Balaii, Mohammad Reza Zali
Arab Journal of Gastroenterology.2019; 20(3): 135. CrossRef - MR Enterography of Inflammatory Bowel Disease with Endoscopic Correlation
Pankaj Kaushal, Alexander S. Somwaru, Aline Charabaty, Angela D. Levy
RadioGraphics.2017; 37(1): 116. CrossRef - Diagnosing inflammatory bowel disease and differentiating it from potential mimics
Kindra D. Clark-Snustad, Scott D. Lee
Techniques in Gastrointestinal Endoscopy.2016; 18(3): 108. CrossRef
- YouTube® en español como fuente de información para pacientes con enfermedad inflamatoria intestinal
- 9,126 View
- 83 Download
- 11 Crossref

- Colonoscopic Cancer Surveillance in Inflammatory Bowel Disease: What's New Beyond Random Biopsy?
- James E. East
- Clin Endosc 2012;45(3):274-277. Published online August 22, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.3.274
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Colonoscopy based colitis surveillance is widely accepted to try to prevent development of and ensure early detection of colitis-associated colorectal cancer. Traditionally this has been performed with quadrantic random biopsies throughout the colon. Chromoendoscopy "dye-spray" with targeted biopsies only has been shown to increase dysplasia detection 4 to 5 fold on a per lesion basis. It has therefore been suggested that random biopsies should be abandoned as they do not increase dysplasia detection nor change patient clinical course. Recent British guidelines for colitis surveillance have strongly endorsed chromoendoscopy. This short review summarizes current international guidelines and looks at how to optimize white light colonoscopy in colitis considering: bowel preparation, withdrawal time, high definition, and structure enhancement. Data for advanced imaging techniques are reviewed including positive evidence in favor of chromoendoscopy, and limited data suggesting autofluoresence imaging may be promising. Narrow band imaging does not increase dysplasia detection in colitis. Confocal endomicroscopy might potentially reduce biopsies beyond that of chromoendoscopy but does not offer a clear detection advantage. Pan-colonic chromoendoscopy with targeted biopsies increases dysplasia detection and is the standard of care in the United Kingdom. It is likely that the use of chromoendoscopy for colitis surveillance will become widely accepted internationally.
-
Citations
Citations to this article as recorded by- Colon Cancer
Sherief Shawki, Jean Ashburn, Steven A. Signs, Emina Huang
Surgical Oncology Clinics of North America.2018; 27(2): 269. CrossRef - Advanced endoscopic imaging for diagnosis of inflammatory bowel diseases: Present and future perspectives
Visvakanth Sivanathan, Gian Eugenio Tontini, Markus Möhler, Peter R. Galle, Helmut Neumann
Digestive Endoscopy.2018; 30(4): 441. CrossRef - Chromoendoscopy for Dysplasia Surveillance in Inflammatory Bowel Disease
Ann D Flynn, John F Valentine
Inflammatory Bowel Diseases.2018; 24(7): 1440. CrossRef - Early detection of ulcerative colitis-associated colorectal cancer
Yu Zhen, Chengxin Luo, Hu Zhang
Gastroenterology Report.2018; 6(2): 83. CrossRef - Screening and surveillance methods for dysplasia in inflammatory bowel disease patients: Where do we stand?
Michail Galanopoulos, Emmanouela Tsoukali, Filippos Gkeros, Marina Vraka, Georgios Karampekos, Gerassimos J Matzaris
World Journal of Gastrointestinal Endoscopy.2018; 10(10): 250. CrossRef - The rectal remnant after total colectomy for colitis – intra-operative,post-operative and longer-term considerations
Kalle Landerholm, Christopher Wood, Alexander Bloemendaal, Nicolas Buchs, Bruce George, Richard Guy
Scandinavian Journal of Gastroenterology.2018; 53(12): 1443. CrossRef - Crohn's disease: risk factor for colorectal cancer
Sandra Cristina Dias dos Santos, Laura Elisabete Ribeiro Barbosa
Journal of Coloproctology.2017; 37(01): 055. CrossRef - Chromoendoscopy for Surveillance in Ulcerative Colitis and Crohn’s Disease: A Systematic Review of Randomized Trials
Andrea Iannone, Marinella Ruospo, Germaine Wong, Mariabeatrice Principi, Michele Barone, Giovanni F.M. Strippoli, Alfredo Di Leo
Clinical Gastroenterology and Hepatology.2017; 15(11): 1684. CrossRef - Chinese consensus on the prevention of colorectal cancer (2016, Shanghai)
Jing‐Yuan Fang, Yong Quan Shi, Ying Xuan Chen, Jing Nan Li, Jian Qiu Sheng
Journal of Digestive Diseases.2017; 18(2): 63. CrossRef - Advanced imaging and therapeutic endoscopy
Chaitanya Pant, Mojtaba S. Olyaee, Amit Rastogi
Techniques in Gastrointestinal Endoscopy.2017; 19(3): 151. CrossRef - Improving the utility of colonoscopy: Recent advances in practice
Crispin J Corte, Rupert W Leong
Journal of Gastroenterology and Hepatology.2016; 31(1): 32. CrossRef - Colorectal Cancer in Patients With Inflammatory Bowel Disease: The Need for a Real Surveillance Program
Rosario Fornaro, Michela Caratto, Elisa Caratto, Giuseppe Caristo, Francesco Fornaro, Davide Giovinazzo, Camilla Sticchi, Marco Casaccia, Enzo Andorno
Clinical Colorectal Cancer.2016; 15(3): 204. CrossRef - How to Optimize Colon Cancer Surveillance in Inflammatory Bowel Disease Patients
Jill K. J. Gaidos, Stephen J. Bickston
Inflammatory Bowel Diseases.2016; 22(5): 1219. CrossRef - Endoscopy in the Diagnosis and Management of Complications of Inflammatory Bowel Disease
Benjamin Tharian, Nayana George, Udayakumar Navaneethan
Inflammatory Bowel Diseases.2016; 22(5): 1184. CrossRef - Surveillance of patients with inflammatory bowel disease
Jessica X. Yu, James E. East, Tonya Kaltenbach
Best Practice & Research Clinical Gastroenterology.2016; 30(6): 949. CrossRef - The role of endoscopy in inflammatory bowel disease
Amandeep K. Shergill, Jenifer R. Lightdale, David H. Bruining, Ruben D. Acosta, Vinay Chandrasekhara, Krishnavel V. Chathadi, G. Anton Decker, Dayna S. Early, John A. Evans, Robert D. Fanelli, Deborah A. Fisher, Lisa Fonkalsrud, Kimberly Foley, Joo Ha Hwa
Gastrointestinal Endoscopy.2015; 81(5): 1101. CrossRef - Chromoendoscopy for Colorectal Cancer Surveillance in Patients with Inflammatory Bowel Disease
Samir A. Shah, David T. Rubin, Francis A. Farraye
Current Gastroenterology Reports.2014;[Epub] CrossRef - Toward a Consensus on Endoscopic Surveillance of Patients with Colonic Inflammatory Bowel Disease
Amandeep K. Shergill, Francis A. Farraye
Gastrointestinal Endoscopy Clinics of North America.2014; 24(3): 469. CrossRef - Achieving the best bowel preparation for colonoscopy
Adolfo Parra-Blanco, Alex Ruiz, Manuel Alvarez-Lobos, Ana Amorós, Juan Cristóbal Gana, Patricio Ibáñez, Akiko Ono, Takahiro Fujii
World Journal of Gastroenterology.2014; 20(47): 17709. CrossRef - Colorectal cancer in inflammatory bowel disease: The risk, pathogenesis, prevention and diagnosis
Eun Ran Kim
World Journal of Gastroenterology.2014; 20(29): 9872. CrossRef - Highlights of the 48th Seminar of Korean Society of Gastrointestinal Endoscopy
Kwang An Kwon, Il Ju Choi, Eun Young Kim, Seok Ho Dong, Ki Baik Hahm
Clinical Endoscopy.2013; 46(3): 203. CrossRef
- Colon Cancer
- 6,529 View
- 40 Download
- 21 Crossref

- Role of Computed Tomography Enterography/Magnetic Resonance Enterography: Is It in Prime Time?
- Ah Young Kim
- Clin Endosc 2012;45(3):269-273. Published online August 22, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.3.269
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Today, cross-sectional imaging modalities, such as computed tomography enterography (CTE) and magnetic resonance enterography (MRE), are particularly suited to evaluate small bowel diseases, especially Crohn's disease (CD). It is well known that CTE/MRE can provide excellent assessment of disease activity as well as the macroscopic features, extramural abnormalities, and complications of the small intestine in patients with CD. In general, CTE is considered as the first-line modality for the evaluation of suspected inflammatory bowel disease and for long-term assessment or follow-up of these patients. Because of the advantage of lack of radiation, MRE is being used more frequently, especially in children or young patients with CD.
-
Citations
Citations to this article as recorded by- Indian guidelines on imaging of the small intestine in Crohn’s disease: A joint Indian Society of Gastroenterology and Indian Radiology and Imaging Association consensus statement
Saurabh Kedia, Raju Sharma, Govind Makharia, Vineet Ahuja, Devendra Desai, Devasenathipathy Kandasamy, Anu Eapen, Karthik Ganesan, Uday C Ghosha, Naveen Kalra, R Karthikeyan, Kumble Seetharama Madhusudhan, Mathew Philip, Amarender Puri, Sunil Puri, Saroj
Indian Journal of Radiology and Imaging.2019; 29(02): 111. CrossRef - Imaging in discriminating intestinal tuberculosis and Crohn’s disease: past, present and the future
Pradeep Goyal, Jimil Shah, Sonali Gupta, Pankaj Gupta, Vishal Sharma
Expert Review of Gastroenterology & Hepatology.2019; 13(10): 995. CrossRef - The effect of without using anisodamine during CT enterography on image quality, diagnostic performance and latent side effects
Didi Wen, Jian Xu, Ying Liu, Rui An, Jian Li, Hongliang Zhao, Minwen Zheng
Clinical Imaging.2018; 48: 106. CrossRef - Ileal Crohn's disease activity predicted by ruler: CT enterography histopathology correlation
Tamer W. Kassem
The Egyptian Journal of Radiology and Nuclear Medicine.2017; 48(1): 7. CrossRef - Faecal biomarkers for screening small bowel inflammation in patients with Crohn’s disease: a prospective study
Takahiro Shimoyama, Takayuki Yamamoto, Satoru Umegae, Koichi Matsumoto
Therapeutic Advances in Gastroenterology.2017; 10(8): 577. CrossRef - Imaging of the small intestine in Crohn’s disease: Joint position statement of the Indian Society of Gastroenterology and Indian Radiological and Imaging Association
Saurabh Kedia, Raju Sharma, Govind K. Makharia, Vineet Ahuja, Devendra Desai, Devasenathipathy Kandasamy, Anu Eapen, Karthik Ganesan, Uday C. Ghoshal, Naveen Kalra, D. Karthikeyan, Kumble Seetharama Madhusudhan, Mathew Philip, Amarender Singh Puri, Sunil
Indian Journal of Gastroenterology.2017; 36(6): 487. CrossRef - Diagnosis of Small-Bowel Diseases: Prospective Comparison of Multi–Detector Row CT Enterography with MR Enterography
Gabriele Masselli, Marco Di Tola, Emanuele Casciani, Elisabetta Polettini, Francesca Laghi, Riccardo Monti, Maria Giulia Bernieri, Gianfranco Gualdi
Radiology.2016; 279(2): 420. CrossRef - Value of Computerized Tomography Enterography in Predicting Crohn’s Disease Activity: Correlation with Crohn’s Disease Activity Index and C-Reactive Protein
Eun Kyung Park, Na Yeon Han, Beom Jin Park, Deuk Jae Sung, Sung Beom Cho, Yoon Tae Jeen, Bora Keum, Min Ju Kim
Iranian Journal of Radiology.2016;[Epub] CrossRef - Identifying the inflammatory and fibrotic bowel stricture: MRI diffusion-weighted imaging in Crohn's disease
Jianguo Zhu, Faming Zhang, Fei Liu, Wenwen He, Jun Tian, Huiyun Han, Peng Cao
Radiology of Infectious Diseases.2015; 2(3): 128. CrossRef - Imaging Inflammatory Bowel Disease with CT and MR Enterography
Piotr Starakiewicz, David J. Grand
Current Radiology Reports.2013; 1(4): 277. CrossRef
- Indian guidelines on imaging of the small intestine in Crohn’s disease: A joint Indian Society of Gastroenterology and Indian Radiology and Imaging Association consensus statement
- 6,293 View
- 68 Download
- 10 Crossref

- A Look into the Small Bowel in Crohn's Disease
- Soo Jung Park, Won Ho Kim
- Clin Endosc 2012;45(3):263-268. Published online August 22, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.3.263
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Crohn's disease (CD) is an inflammatory bowel disease that can affect the entire gastrointestinal tract, with the small bowel (SB) being the most commonly affected site. In some patients, refractory inflammation or chronic strictures of the SB are responsible for a debilitating course of the disease that might lead to severely reduced quality of life. Therefore, SB imaging is a crucial element in diagnosing and/or managing SB CD, and continues to evolve because of technologic advances. SB endoscopy (capsule endoscopy and device-assisted enteroscopy) and cross-sectional radiologic imaging (computed tomography enterography and magnetic resonance enterography) have become key players to diagnose and/or manage CD. In everyday practice, the choice of the imaging modalities is based on the presence and availability of the techniques and of experienced operators in each institute, clinical usefulness, safety, and cost. Here, SB endoscopy and radiologic imaging in suspected or known CD patients will be addressed and discussed.
-
Citations
Citations to this article as recorded by- ECHOGRAPHY IN THE DIAGNOSTICS OF INFLAMMATORY BOWEL DISEASES IN CHILDREN
M. I. Pykov, A. M. Vrublevskaya
Russian Journal of Pediatric Surgery.2020; 24(2): 101. CrossRef - Endoscopy in the Diagnosis and Management of Complications of Inflammatory Bowel Disease
Benjamin Tharian, Nayana George, Udayakumar Navaneethan
Inflammatory Bowel Diseases.2016; 22(5): 1184. CrossRef - The role of capsule endoscopy in evaluating both suspected and known Crohnʼs disease
Erika S. Boroff, Jonathan A. Leighton
Techniques in Gastrointestinal Endoscopy.2015; 17(1): 5. CrossRef
- ECHOGRAPHY IN THE DIAGNOSTICS OF INFLAMMATORY BOWEL DISEASES IN CHILDREN
- 6,910 View
- 57 Download
- 3 Crossref

- Retrieval of a Retained Capsule due to Isolated Crohn's Enteritis by Means of Double Balloon Enteroscopy
- Kon-Ho Shim, M.D., Soo-Yeon Jung, M.D., Jun-Ho Song, M.D., Hyeug Lee, M.D., Eui-Hyung Kim, M.D., Eun-Jung Jeon, M.D., Jung-Hwan Oh, M.D., Jeong-Jo Jeong, M.D., Hwang Choi, M.D. and Sang-Wook Choi, M.D.
- Korean J Gastrointest Endosc 2007;35(6):399-403. Published online December 30, 2007
-
 Abstract
Abstract
 PDF
PDF - Capsule endoscopy is being increasingly used for investigating GI bleeding of an obscure origin and also the bleeding that's due to Crohn's disease. Capsule endoscopy is a safe procedure with few complications. Complications of capsule endoscopy are capsule retention, incomplete small bowel examination, swallowing disorders and technical complications. However, capsule retention still remains a major concern. Crohn's disease may rarely show its first manifestation as GI bleeding. We present here a case of obscure GI bleeding in which the diagnosis of isolated Crohn's enteritis was made by using wireless CE. The retained capsule at the jejunal stricture of Crohn's disease was successfully retrieved by performing double balloon enteroscopy. (Korean J Gastrointest Endosc 2007;35:399-403)
- 2,219 View
- 5 Download

- Clinical Features and Course of Crohn Disease in Children
- Na Young Lee, M.D. and Jae Hong Park, M.D.*
- Korean J Gastrointest Endosc 2007;34(4):193-199. Published online April 30, 2007
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: The aim of this study was to evaluate the clinical features and course of Crohn disease (CD) in children. Methods: The medical records of 30 patients diagnosed with CD between January 1996 and December 2005 were reviewed retrospectively. Results: The actual number of newly diagnosed patients with CD has increased during the 8-year period. The male/female ratio was 2:1 and the mean age at diagnosis was 10.6⁑4.3 years. The major symptoms of CD at diagnosis were abdominal pain (79.2%), weight loss (54.2%), perianal lesion (54.2%), diarrhea (45.8%), hematochezia (41.7%), anemia (29.2%), and fever (23.3%). The disease location of CD was the small bowel in 33.3%, the large bowel in 12.5% and both the small and large bowel in 54.2%. Granuloma was found in 54.2% of patients. The relapse rate of CD in the group with a higher pediatric Crohn disease activity index (PCDAI) at diagnosis (≥30) was higher than in the group with a lower PCDAI (<30). The cumulative relapse rates of the patients with granuloma were 30.2% within 1 year and 53.8% within 5 years after the diagnosis. Conclusions: The incidence of CD in children appears to be increasing. Granuloma formation and a higher score of the PCDAI are associated with a more severe disease course. Pediatric CD may have a somewhat different clinical presentation from older-onset CD. (Korean J Gastrointest Endosc 2007;34:193199)
- 2,222 View
- 26 Download


 KSGE
KSGE

 First
First Prev
Prev