Search
- Page Path
- HOME > Search
- Endoscopic management of giant colonic polyps: a retrospective Italian study
- Paolo Quitadamo, Sara Isoldi, Germana De Nucci, Giulia Muzi, Flora Caruso
- Received September 12, 2023 Accepted January 14, 2024 Published online June 5, 2024
- DOI: https://doi.org/10.5946/ce.2023.229 [Epub ahead of print]

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Polyps greater than 30 mm are classified as “giants”. Their endoscopic removal represents a technical challenge. The choice of the endoscopic removal technique is important because it provides a resection sample for precise histopathological staging. This is pivotal for diagnostic, prognostic, and management purposes.
Methods
From a retrospective analysis, we obtained a sample of 38 giant polyps. Eighteen polypectomies were performed using the epinephrine volume reduction (EVR) method, nine polypectomies utilized endo-looping or clipping methods, and 11 patients underwent surgery.
Results
We obtained en bloc resection with the EVR method in all cases; histology confirmed the correct indication for endoscopic resection in all cases. Moreover, no early or delayed complications were observed, and no patient required hospitalization. Using endo-looping or clipping methods, we observed advanced histology in 1/9 (11.1%) cases, while another patient (1/9, 11.1%) had delayed bleeding. Among patients who underwent surgery, 5/11 (45.5%) were deemed overtreated and three had post-surgical complications.
Conclusions
We propose EVR as an alternative technique for giant polyp resection due to its safety, effectiveness, cost-efficiency, and the advantage of avoiding the need to postpone polypectomy to a later time. Further prospective studies might help improve this experience and enhance the technique.
- 1,006 View
- 20 Download

- Outcomes of thin versus thick-wire snares for cold snare polypectomy: a systematic review and meta-analysis
- Suprabhat Giri, Vaneet Jearth, Harish Darak, Sridhar Sundaram
- Clin Endosc 2022;55(6):742-750. Published online November 9, 2022
- DOI: https://doi.org/10.5946/ce.2022.141
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: Cold snare polypectomy (CSP) is commonly used for the resection of colorectal polyps ≤10 mm. Data regarding the influence of snare type on CSP effectiveness are conflicting. Hence, this meta-analysis aimed to compare the outcomes and safety of thin- and thick-wire snares for CSP.
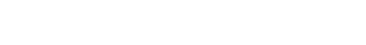
Methods
A comprehensive search of the literature published between 2000 and 2021 was performed of various databases for comparative studies evaluating the outcomes of thin- versus thick-wire snares for CSP.
Results
Five studies with data on 1,425 polyps were included in the analysis. The thick-wire snare was comparable to the thin-wire snare with respect to complete histological resection (risk ratio [RR], 1.03; 95% confidence interval [CI], 0.97–1.09), overall bleeding (RR, 0.98; 95% CI, 0.40–2.40), polyp retrieval (RR, 1.01; 95% CI, 0.97–1.04), and involvement of submucosa in the resection specimen (RR, 1.28; 95% CI, 0.72–2.28). There was no publication bias and a small study effect, and the relative effects remained the same in the sensitivity analysis.
Conclusions
CSP using a thin-wire snare has no additional benefit over thick-wire snares in small colorectal polyps. Factors other than snare design may play a role in improving CSP outcomes. -
Citations
Citations to this article as recorded by- Factors determining the resection ability of snares in cold snare polypectomy: Construction of an ex vivo model for accurately evaluating resection ability
Ryohei Hirose, Takuma Yoshida, Naohisa Yoshida, Katsuma Yamauchi, Hajime Miyazaki, Naoto Watanabe, Risa Bandou, Ken Inoue, Hiroshi Ikegaya, Takaaki Nakaya, Yoshito Itoh
Digestive Endoscopy.2024; 36(5): 573. CrossRef - Effectiveness and safety of thin vs. thick cold snare polypectomy of small colorectal polyps: Systematic review and meta-analysis
Rishad Khan, Sunil Samnani, Marcus Vaska, Samir C Grover, Catharine M Walsh, Jeffrey Mosko, Michael J Bourke, Steven J Heitman, Nauzer Forbes
Endoscopy International Open.2024; 12(01): E99. CrossRef - International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
Seung Joo Kang, Chung Hyun Tae, Chang Seok Bang, Cheol Min Shin, Young-Hoon Jeong, Miyoung Choi, Joo Ha Hwang, Yutaka Saito, Philip Wai Yan Chiu, Rungsun Rerknimitr, Christopher Khor, Vu Van Khien, Kee Don Choi, Ki-Nam Shim, Geun Am Song, Oh Young Lee
Clinical Endoscopy.2024; 57(2): 141. CrossRef - Does the wire diameter really determine the outcomes in cold snare polypectomy?
S Giri, S Sundaram
Journal of Gastroenterology and Hepatology.2023; 38(4): 665. CrossRef - Cold resection for colorectal polyps: where we are and where we are going?
Antonio Capogreco, Ludovico Alfarone, Davide Massimi, Alessandro Repici
Expert Review of Gastroenterology & Hepatology.2023; 17(7): 719. CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef
- Factors determining the resection ability of snares in cold snare polypectomy: Construction of an ex vivo model for accurately evaluating resection ability
- 2,608 View
- 158 Download
- 6 Web of Science
- 6 Crossref

- Korean guidelines for postpolypectomy colonoscopic surveillance: 2022 revised edition
- Su Young Kim, Min Seob Kwak, Soon Man Yoon, Yunho Jung, Jong Wook Kim, Sun-Jin Boo, Eun Hye Oh, Seong Ran Jeon, Seung-Joo Nam, Seon-Young Park, Soo-Kyung Park, Jaeyoung Chun, Dong Hoon Baek, Mi-Young Choi, Suyeon Park, Jeong-Sik Byeon, Hyung Kil Kim, Joo Young Cho, Moon Sung Lee, Oh Young Lee, Korean Society of Gastrointestinal Endoscopy, Korean Society of Gastroenterology, Korean Association for the Study of Intestinal Diseases
- Clin Endosc 2022;55(6):703-725. Published online October 13, 2022
- DOI: https://doi.org/10.5946/ce.2022.136
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
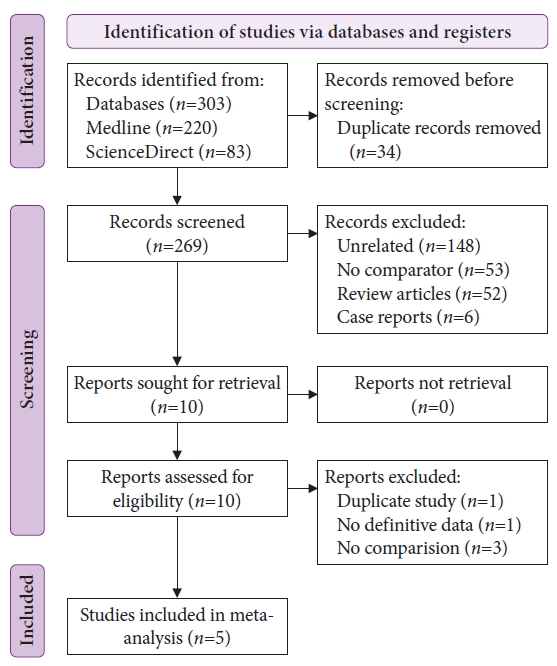
ePub - Colonoscopic polypectomy is effective in decreasing the incidence and mortality of colorectal cancer (CRC). Premalignant polyps discovered during colonoscopy are associated with the risk of metachronous advanced neoplasia. Postpolypectomy surveillance is the most important method for the management of advanced metachronous neoplasia. A more efficient and evidence-based guideline for postpolypectomy surveillance is required because of limited medical resources and concerns regarding colonoscopy complications. In these consensus guidelines, an analytic approach was used to address all reliable evidence to interpret the predictors of CRC or advanced neoplasia during surveillance colonoscopy. The key recommendations state that the high-risk findings for metachronous CRC following polypectomy are as follows: (1) adenoma ≥10 mm in size; (2) 3 to 5 (or more) adenomas; (3) tubulovillous or villous adenoma; (4) adenoma containing high-grade dysplasia; (5) traditional serrated adenoma; (6) sessile serrated lesion (SSL) containing any grade of dysplasia; (7) serrated polyp of at least 10 mm in size; and (8) 3 to 5 (or more) SSLs. More studies are needed to fully comprehend the patients most likely to benefit from surveillance colonoscopy and the ideal surveillance interval to prevent metachronous CRC.
-
Citations
Citations to this article as recorded by- Association between Atherosclerosis and High-Risk Colorectal Adenomas based on Cardio-Ankle Vascular Index and Ankle-Brachial Index
Jung Ho Lee, Hyunseok Cho, Sang Hoon Lee, Sung Joon Lee, Chang Don Kang, Dae Hee Choi, Jin Myung Park, Seung-Joo Nam, Tae Suk Kim, Ji Hyun Kim, Sung Chul Park
The Korean Journal of Gastroenterology.2024; 83(4): 143. CrossRef - A survey of current practices in post-polypectomy surveillance in Korea
Jeongseok Kim, Tae-Geun Gweon, Min Seob Kwak, Su Young Kim, Seong Jung Kim, Hyun Gun Kim, Eun Ran Kim, Sung Noh Hong, Eun Sun Kim, Chang Mo Moon, Dae Seong Myung, Dong Hoon Baek, Shin Ju Oh, Hyun Jung Lee, Ji Young Lee, Yunho Jung, Jaeyoung Chun, Dong-Hoo
Intestinal Research.2024; 22(2): 186. CrossRef - Korean Guidelines for Postpolypectomy Colonoscopic Surveillance: 2022 Revision
Su Young Kim
The Korean Journal of Medicine.2023; 98(3): 102. CrossRef - Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Mizuki Nagai, Sho Suzuki, Yohei Minato, Fumiaki Ishibashi, Kentaro Mochida, Ken Ohata, Tetsuo Morishita
Clinical Endoscopy.2023; 56(5): 553. CrossRef - Understanding colorectal polyps to prevent colorectal cancer
Dong-Hoon Yang
Journal of the Korean Medical Association.2023; 66(11): 626. CrossRef - Classification and endoscopic diagnosis of colorectal polyps
Ji Hyun Kim, Sung Chul Park
Journal of the Korean Medical Association.2023; 66(11): 633. CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef - Strategy for post-polypectomy colonoscopy surveillance: focus on the revised Korean guidelines
Yong Soo Kwon, Su Young Kim
Journal of the Korean Medical Association.2023; 66(11): 652. CrossRef
- Association between Atherosclerosis and High-Risk Colorectal Adenomas based on Cardio-Ankle Vascular Index and Ankle-Brachial Index
- 5,241 View
- 515 Download
- 8 Web of Science
- 8 Crossref

- Post-polypectomy surveillance: the present and the future
- Masau Sekiguchi, Takahisa Matsuda, Kinichi Hotta, Yutaka Saito
- Clin Endosc 2022;55(4):489-495. Published online July 11, 2022
- DOI: https://doi.org/10.5946/ce.2022.097
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
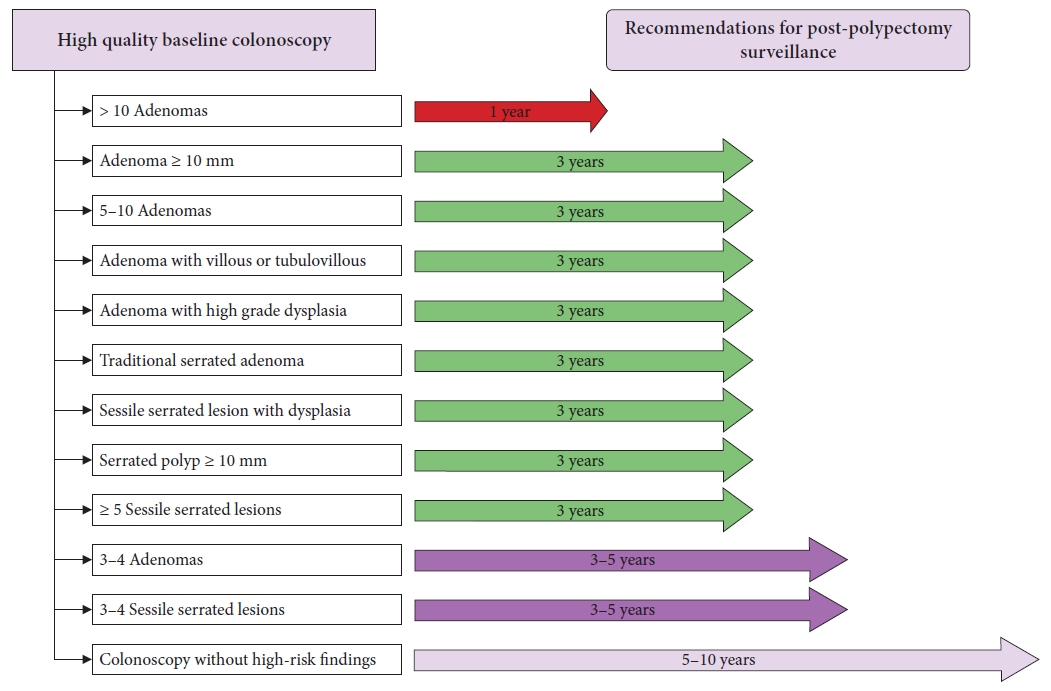
ePub - An appropriate post-polypectomy surveillance program requires the effectiveness of reducing colorectal cancer and safety. In addition, the post-polypectomy surveillance program should consider the burden of limited medical resource capacity, cost-effectiveness, and patient adherence. In this sense, a risk-stratified surveillance program based on baseline colonoscopy results is ideal. Major international guidelines for post-polypectomy surveillance, such as those from the European Union and the United States, have recommended risk-stratified surveillance programs. Both guidelines have recently been updated to better differentiate between high- and low-risk individuals. In both updated guidelines, more individuals have been downgraded to lower-risk groups that require less frequent or no surveillance. Furthermore, increased attention has been paid to the surveillance of patients who undergo serrated polyp removal. Previous guidelines in Japan did not clearly outline the risk stratification in post-polypectomy surveillance. However, the new colonoscopy screening and surveillance guidelines presented by the Japan Gastroenterological Endoscopy Society include a risk-stratified post-polypectomy surveillance program. Further discussion and analysis of unresolved issues in this field, such as the optimal follow-up after the first surveillance, the upper age limit for surveillance, and the ideal method for improving adherence to surveillance guidelines, are warranted.
-
Citations
Citations to this article as recorded by- Protocolo diagnóstico del seguimiento de pólipos colónicos
S. Redondo Evangelista, M. Sierra Morales, I. Bartolomé Oterino, P. García Centeno, A. Santos Rodríguez
Medicine - Programa de Formación Médica Continuada Acreditado.2024; 14(4): 219. CrossRef - Metabolic‐associated fatty liver disease is associated with colorectal adenomas in young and older Korean adults
Jiwon Chang, Yoosoo Chang, Yoosun Cho, Hyun‐Suk Jung, Dong‐Il Park, Soo‐Kyung Park, Soo‐Youn Ham, Sarah H. Wild, Christopher D. Byrne, Seungho Ryu
Liver International.2023; 43(11): 2548. CrossRef - Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Mizuki Nagai, Sho Suzuki, Yohei Minato, Fumiaki Ishibashi, Kentaro Mochida, Ken Ohata, Tetsuo Morishita
Clinical Endoscopy.2023; 56(5): 553. CrossRef - Strategy for post-polypectomy colonoscopy surveillance: focus on the revised Korean guidelines
Yong Soo Kwon, Su Young Kim
Journal of the Korean Medical Association.2023; 66(11): 652. CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef - Understanding colorectal polyps to prevent colorectal cancer
Dong-Hoon Yang
Journal of the Korean Medical Association.2023; 66(11): 626. CrossRef
- Protocolo diagnóstico del seguimiento de pólipos colónicos
- 3,556 View
- 249 Download
- 5 Web of Science
- 6 Crossref

- Current Treatment Strategy for Superficial Nonampullary Duodenal Epithelial Tumors
- Tetsuya Suwa, Kohei Takizawa, Noboru Kawata, Masao Yoshida, Yohei Yabuuchi, Yoichi Yamamoto, Hiroyuki Ono
- Clin Endosc 2022;55(1):15-21. Published online September 29, 2021
- DOI: https://doi.org/10.5946/ce.2021.141

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic submucosal dissection (ESD) is the standard treatment method for esophageal, gastric, and colorectal cancers. However, it has not been standardized for duodenal lesions because of its high complication rates. Recently, minimally invasive and simple methods such as cold snare polypectomy and underwater endoscopic mucosal resection have been utilized more for superficial nonampullary duodenal epithelial tumors (SNADETs). Although the rate of complications associated with duodenal ESD has been gradually decreasing because of technical advancements, performing ESD for all SNADETs is unnecessary. As such, the appropriate treatment plan for SNADETs should be chosen according to the lesion type, patient condition, and endoscopist’s skill.
-
Citations
Citations to this article as recorded by- International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
Seung Joo Kang, Chung Hyun Tae, Chang Seok Bang, Cheol Min Shin, Young-Hoon Jeong, Miyoung Choi, Joo Ha Hwang, Yutaka Saito, Philip Wai Yan Chiu, Rungsun Rerknimitr, Christopher Khor, Vu Van Khien, Kee Don Choi, Ki-Nam Shim, Geun Am Song, Oh Young Lee
Clinical Endoscopy.2024; 57(2): 141. CrossRef - Underwater Endoscopic Mucosal Resection Versus Conventional Endoscopic Mucosal Resection for Superficial Non-ampullary Duodenal Epithelial Tumors ≤20 mm
Zhikun Yin, Ji Li, Weilin Yang, Weifeng Huang, Dong Xu, Xiaoyi Lei, Jinyan Zhang
Journal of Clinical Gastroenterology.2023; 57(9): 928. CrossRef - Long-term outcomes of endoscopic resection for duodenal neuroendocrine tumors
Kiyoun Yi, Gwang Ha Kim, Su Jin Kim, Cheol Woong Choi, Moon Won Lee, Bong Eun Lee, Geun Am Song
Scientific Reports.2023;[Epub] CrossRef - Endoscopic management of NADTs
Enrique Pérez-Cuadrado-Robles, Pierre H. Deprez
Endoscopy International Open.2022; 10(06): E733. CrossRef - Duodenaladenome und -karzinome: chirurgische Therapiekonzepte
Michael Ghadimi, Jochen Gaedcke
Allgemein- und Viszeralchirurgie up2date.2022; 16(03): 257. CrossRef - Issues and Prospects of Current Endoscopic Treatment Strategy for Superficial Non-Ampullary Duodenal Epithelial Tumors
Tetsuya Suwa, Masao Yoshida, Hiroyuki Ono
Current Oncology.2022; 29(10): 6816. CrossRef - Duodenaladenome und -karzinome: chirurgische Therapiekonzepte
Michael Ghadimi, Jochen Gaedcke
Onkologie up2date.2022; 4(04): 325. CrossRef
- International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
- 5,012 View
- 352 Download
- 4 Web of Science
- 7 Crossref

- Extracutaneous mastocytoma of colon: a case report and literature review
- Min Su Chu, Eui Joong Kim
- Clin Endosc 2022;55(6):810-814. Published online July 7, 2021
- DOI: https://doi.org/10.5946/ce.2021.003
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Extracutaneous mastocytoma is a rare benign tumor composed of mature mast cells and is located in tissues other than the skin. We report the case of a 61-year-old male who was diagnosed with extracutaneous mastocytoma via colonoscopic polypectomy and biopsy. To our knowledge, this was the first case of a solitary extracutaneous mastocytoma of the colon. We reported this case and reviewed the literature.
-
Citations
Citations to this article as recorded by- Incidental discovery of KIT‐mutated mastocytoma in a colon polyp
Naseema Gangat, Ellen McPhail, Kaaren Reichard, Attilio Orazi, Animesh Pardanani, Ayalew Tefferi
American Journal of Hematology.2024; 99(5): 973. CrossRef
- Incidental discovery of KIT‐mutated mastocytoma in a colon polyp
- 3,361 View
- 161 Download
- 1 Web of Science
- 1 Crossref

- Is Submucosal Injection Helpful in Cold Snare Polypectomy for Small Colorectal Polyps?
- Ji Hyun Song, Shai Friedland
- Clin Endosc 2021;54(3):397-403. Published online February 9, 2021
- DOI: https://doi.org/10.5946/ce.2020.226
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
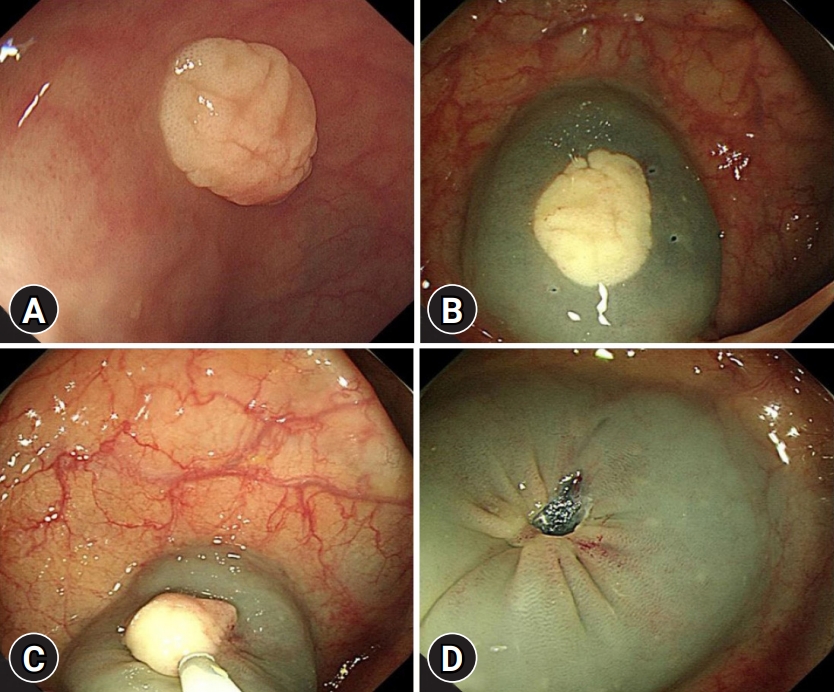
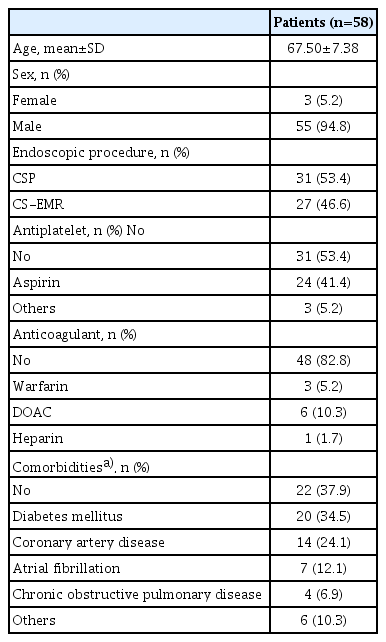
ePub - Background
/Aims: Cold snare polypectomy (CSP) is an effective method of polyp removal for small colorectal polyps. However, the effect of submucosal injection in cold snare endoscopic mucosal resection (CS-EMR) for small polyps is unclear. Therefore, this study aimed to evaluate the effect of submucosal injection in CS-EMR for small polyps.
Methods
Between 2018 and 2019, 100 consecutive small colorectal polyps (5–10 mm) were identified in 58 patients. The first 50 consecutive polyps were removed by CS-EMR, and the remaining 50 were removed by CSP. Demographic data, clinical data, endoscopic findings, procedure times, complication rates, and pathology data were collected.
Results
No difference in the complete resection rate was observed between the CS-EMR and CSP groups. A total of 9 polyps showed post-polypectomy bleeding (7 had immediate bleeding, 1 had delayed bleeding, and 1 had both immediate and delayed bleeding). No difference in the bleeding rate was observed between the two groups. In multivariate analysis, warfarin (odds ratio [OR], 42.334; 95% confidence interval [CI], 1.006–1,781.758) and direct-acting oral anticoagulants (OR, 35.244; 95% CI, 3.853–322.397) showed a significantly increased risk of bleeding.
Conclusions
The effect of submucosal injection in CSP was not significant for small colorectal polyps. -
Citations
Citations to this article as recorded by- Colorectal cold snare polypectomy: Current standard technique and future perspectives
Fumiaki Ishibashi, Sho Suzuki, Mizuki Nagai, Kentaro Mochida, Tetsuo Morishita
Digestive Endoscopy.2023; 35(3): 278. CrossRef - The efficacy and safety of cold snare polypectomy with submucosal injection for the removal of polyps less than 20 mm in size: a systematic review and meta‐analysis
Zheng Liang, Yongqiu Wei, Shutian Zhang, Peng Li
Journal of Gastroenterology and Hepatology.2023; 38(11): 1892. CrossRef - Impact of Submucosal Saline Injection During Cold Snare Polypectomy for Colorectal Polyps Sized 3–9 mm: A Multicenter Randomized Controlled Trial
Yi Mou, Liansong Ye, Xiaobo Qin, Rui Feng, Lifan Zhang, Qin Hu, Tingting Cao, Xinyue Zhou, Wu Wen, Chuanming Zhang, Zonghua Chen, Yi Liu, Zhimin Yang, Tao Huo, Fang Pan, Xuelian Li, Bing Hu
American Journal of Gastroenterology.2023; 118(10): 1848. CrossRef - Cold resection for colorectal polyps: where we are and where we are going?
Antonio Capogreco, Ludovico Alfarone, Davide Massimi, Alessandro Repici
Expert Review of Gastroenterology & Hepatology.2023; 17(7): 719. CrossRef - Cold snare endoscopic mucosal resection for colon polyps: a systematic review and meta-analysis
Mohamed Abdallah, Khalid Ahmed, Daniyal Abbas, Mouhand F. H. Mohamed, Gaurav Suryawanshi, Nicholas McDonald, Natalie Wilson, Shifa Umar, Aasma Shaukat, Mohammad Bilal
Endoscopy.2023; 55(12): 1083. CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef
- Colorectal cold snare polypectomy: Current standard technique and future perspectives
- 4,347 View
- 167 Download
- 7 Web of Science
- 6 Crossref

-
Dedicated Cold Snare vs. Traditional Snare for Polypectomy of Diminutive and Small Lesions in a Porcine Model: A Research Group for Endoscopic Instruments and Stents (REIS) Study

- Han Hee Lee, Bo-In Lee, Jung-Wook Kim, Hyun Lim, Si Hyung Lee, Jun-Hyung Cho, Yunho Jung, Kyoung Oh Kim, Chan Gyoo Kim, Kee Myung Lee, Jong-Jae Park, Myung-Gyu Choi, Hoon Jai Chun, Ho Gak Kim
- Clin Endosc 2021;54(3):390-396. Published online September 10, 2020
- DOI: https://doi.org/10.5946/ce.2020.096
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
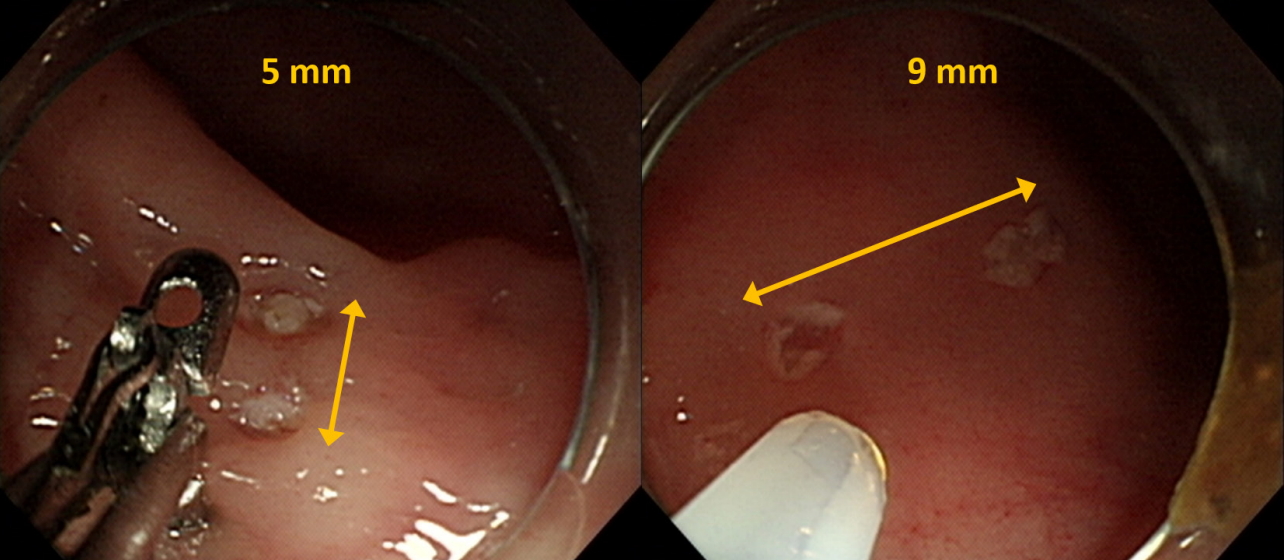
/Aims: The aim of this in vivo animal study was to evaluate the effectiveness and safety of dedicated cold snare (DCS) compared with those of traditional snare (TS) for cold snare polypectomy (CSP).
Methods
A total of 36 diminutive (5 mm) and 36 small (9 mm) pseudolesions were made by electrocoagulation in the colons of mini-pigs.
Results
For the diminutive lesions, there were no significant differences in technical success rate, procedure time, or complete resection rate between the DCS and TS groups; the rate of uneven resection margin in the DCS group was significantly lower than that of the TS group. For small lesions, technical success rate and complete resection rate were significantly higher in the DCS group than in the TS group (100% [18/18] vs. 55.6% [10/18], p=0.003; 94.4% [17/18] vs. 40% [4/10], p=0.006). In addition, the procedure duration was significantly shorter, and the rate of uneven resection margin was significantly lower in the DCS group (28.5 sec vs. 66.0 sec, p=0.006; 11.1% [2/18] vs. 100% [10/10], p<0.001). Two cases of perforation occurred in the DCS group. Multivariate analysis revealed that DCS use was independently associated with complete resection.
Conclusions
DCS is superior to TS in terms of technical success, complete resection, and reducing the duration of the procedure for CSP of small polyps. -
Citations
Citations to this article as recorded by- Comparison of complete resection rates in cold snare polypectomy using two different wire diameter snares: A randomized controlled study
Toshiki Horii, Sho Suzuki, Akihiro Sugita, Misa Yamauchi, Hisatomo Ikehara, Chika Kusano, Takuji Gotoda
Journal of Gastroenterology and Hepatology.2023; 38(5): 752. CrossRef - Comparison of the clinical efficacy of cold snare polypectomy using a thin-wire snare and thick-wire snare for small colorectal polyps
Hong Jin Yoon, Yunho Jung, Young Sin Cho, Il-Kwun Chung
International Journal of Gastrointestinal Intervention.2023; 12(4): 183. CrossRef - Big Issues on Small Polyps: An Ideal Device, But Is It for an Ideal Indication?
Yoji Takeuchi
Clinical Endoscopy.2021; 54(3): 297. CrossRef - Cold versus hot polypectomy/endoscopic mucosal resection–A review of current evidence
Raquel Ortigão, Jochen Weigt, Ahmed Afifi, Diogo Libânio
United European Gastroenterology Journal.2021; 9(8): 938. CrossRef
- Comparison of complete resection rates in cold snare polypectomy using two different wire diameter snares: A randomized controlled study
- 8,391 View
- 221 Download
- 4 Web of Science
- 4 Crossref

- Endoscopic Management of Post-Polypectomy Bleeding
- Aditya Gutta, Mark A. Gromski
- Clin Endosc 2020;53(3):302-310. Published online September 17, 2019
- DOI: https://doi.org/10.5946/ce.2019.062

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Post-polypectomy bleeding (PPB) is one of the most common complications of endoscopic polypectomy. There are multiple risk factors related to patient and polyp characteristics that should be considered. In most cases, immediate PPB can be effectively managed endoscopically when recognized and managed promptly. Delayed PPB can manifest in a myriad of ways. In severe delayed PPB, resuscitation for hemodynamic stabilization should be prioritized, followed by endoscopic evaluation and therapy once the patient is stabilized. Future areas of research in PPB include the risks of direct oral anticoagulants and of specific electrosurgical settings for hot-snare polypectomy vs. cold-snare polypectomy, benefits of closure of post-polypectomy mucosal defects using through-the-scope clips, and prospective comparative evaluation of newer hemostasis agents such as hemostatic spray powder and over-the-scope clips.
-
Citations
Citations to this article as recorded by- Updates on the Prevention and Management of Post-Polypectomy Bleeding in the Colon
Hisham Wehbe, Aditya Gutta, Mark A. Gromski
Gastrointestinal Endoscopy Clinics of North America.2024; 34(2): 363. CrossRef - Colonoscopic polypectomy of juvenile polyps in children: Experience from a tertiary centre of Bangladesh
Salahuddin Mahmud, Mashud Parvez, Madhabi Baidya, Farhana Tasneem, Ahmed Rashidul Hasan, Tanzila Farhana, Md Jahangir Alam, Syed Shafi Ahmed
Gastroenterology & Endoscopy.2024; 2(1): 1. CrossRef - Review article: Advances in the management of lower gastrointestinal bleeding
Ali A. Alali, Majid A. Almadi, Alan N. Barkun
Alimentary Pharmacology & Therapeutics.2024; 59(5): 632. CrossRef - Endoscopic management of intraprocedural bleeding during endoscopic interventions
Ali A. Alali, Asma A. Alkandari
Best Practice & Research Clinical Gastroenterology.2024; 69: 101912. CrossRef - Effect of Cold Versus Hot Snare Polypectomy on Colon Postpolypectomy Bleeding in Patients with End-Stage Renal Disease: A Retrospective Cohort Study
Hsueh-Chien Chiang, Chien-Ming Chiang, Xi-Zhang Lin, Po-Jun Chen
Digestive Diseases and Sciences.2024;[Epub] CrossRef - Isolated ischaemic appendicitis as a rare complication of selective angioembolization for lower gastrointestinal bleed
Luke S. Crawford, Nadim S. Jafri, Dingle Foote, Melissa M. Felinski, Peter A. Walker, Kulvinder S. Bajwa, Shinil K. Shah
ANZ Journal of Surgery.2023; 93(1-2): 404. CrossRef - JAG consensus statements for training and certification in colonoscopy
Keith Siau, Stavroula Pelitari, Susi Green, Brian McKaig, Arun Rajendran, Mark Feeney, Mo Thoufeeq, John Anderson, Vathsan Ravindran, Paul Hagan, Neil Cripps, Ian L P Beales, Karen Church, Nicholas I Church, Elizabeth Ratcliffe, Said Din, Rupert D Pullan,
Frontline Gastroenterology.2023; 14(3): 201. CrossRef - JAG consensus statements for training and certification in flexible sigmoidoscopy
Keith Siau, Stavroula Pelitari, Susi Green, Brian McKaig, Arun Rajendran, Mark Feeney, Mo Thoufeeq, John Anderson, Vathsan Ravindran, Paul Hagan, Neil Cripps, Ian L P Beales, Karen Church, Nicholas I Church, Elizabeth Ratcliffe, Said Din, Rupert D Pullan,
Frontline Gastroenterology.2023; 14(3): 181. CrossRef - Management of Patients With Acute Lower Gastrointestinal Bleeding: An Updated ACG Guideline
Neil Sengupta, Joseph D. Feuerstein, Vipul Jairath, Amandeep K. Shergill, Lisa L. Strate, Robert J. Wong, David Wan
American Journal of Gastroenterology.2023; 118(2): 208. CrossRef - Korean Guidelines for Postpolypectomy Colonoscopic Surveillance: 2022 revised edition
Su Young Kim, Min Seob Kwak, Soon Man Yoon, Yunho Jung, Jong Wook Kim, Sun-Jin Boo, Eun Hye Oh, Seong Ran Jeon, Seung-Joo Nam, Seon-Young Park, Soo-Kyung Park, Jaeyoung Chun, Dong Hoon Baek, Mi-Young Choi, Suyeon Park, Jeong-Sik Byeon, Hyung Kil Kim, Joo
Intestinal Research.2023; 21(1): 20. CrossRef - A Review of Colonoscopy in Intestinal Diseases
Seung Min Hong, Dong Hoon Baek
Diagnostics.2023; 13(7): 1262. CrossRef - Bleeding After Endoscopic Resection of Colonic Adenomatous Polyps Sized 4-10 mm
Violeta Hristova Janik
PRILOZI.2023; 44(2): 157. CrossRef - Endoscopic management of delayed bleeding after polypectomy of small colorectal polyps: two or more clips may be safe
Xue-Feng Guo, Xiang-An Yu, Jian-Cong Hu, De-Zheng Lin, Jia-Xin Deng, Ming-Li Su, Juan Li, Wei Liu, Jia-Wei Zhang, Qing-Hua Zhong
Gastroenterology Report.2022;[Epub] CrossRef - Clinical progress note: Diagnostic approach to lower gastrointestinal bleeding
Daniel J. Stein, Hyder Said, Joseph D. Feuerstein
Journal of Hospital Medicine.2022; 17(7): 547. CrossRef - Safety of Cold Snare Polypectomy for Small Colorectal Polyps in Patients Receiving Antithrombotic Therapy
Dai Nakamatsu, Tsutomu Nishida, Yoshifumi Fujii, Sho Yamaoka, Naoto Osugi, Aya Sugimoto, Kaori Mukai, Kengo Matsumoto, Masashi Yamamoto, Shiro Hayashi, Sachiko Nakajima
Techniques and Innovations in Gastrointestinal Endoscopy.2022; 24(3): 246. CrossRef - Postcolonoscopy Complications
Jetsen A. Rodriguez-Silva, Justin A. Maykel
Diseases of the Colon & Rectum.2022; 65(5): 622. CrossRef - Expanding rather than closing the wound can rescue the endoscopic procedure when massive bleeding occurs during endoscopic submucosal dissection
Ming-Ching Yuan, Ching-Tai Lee, Kun-Feng Tsai, Chao-Wen Hsu, Chu-Kuang Chou
Endoscopy.2022; 54(S 02): E1036. CrossRef - Korean Guidelines for Postpolypectomy Colonoscopic Surveillance: 2022 Revised Edition
Su Young Kim, Min Seob Kwak, Soon Man Yoon, Yunho Jung, Jong Wook Kim, Sun-Jin Boo, Eun Hye Oh, Seong Ran Jeon, Seung-Joo Nam, Seon-Young Park, Soo-Kyung Park, Jaeyoung Chun, Dong Hoon Baek, Mi-Young Choi, Suyeon Park, Jeong-Sik Byeon, Hyung Kil Kim, Joo
The Korean Journal of Gastroenterology.2022; 80(3): 115. CrossRef - Korean guidelines for postpolypectomy colonoscopic surveillance: 2022 revised edition
Su Young Kim, Min Seob Kwak, Soon Man Yoon, Yunho Jung, Jong Wook Kim, Sun-Jin Boo, Eun Hye Oh, Seong Ran Jeon, Seung-Joo Nam, Seon-Young Park, Soo-Kyung Park, Jaeyoung Chun, Dong Hoon Baek, Mi-Young Choi, Suyeon Park, Jeong-Sik Byeon, Hyung Kil Kim, Joo
Clinical Endoscopy.2022; 55(6): 703. CrossRef - Can prophylactic argon plasma coagulation reduce delayed post‐papillectomy bleeding? A prospective multicenter trial
Jae Kook Yang, Jong Jin Hyun, Tae Hoon Lee, Jun‐Ho Choi, Yun Nah Lee, Jung Wan Choe, Jin‐Seok Park, Chang‐Il Kwon, Seok Jeong, Hong Ja Kim, Jong Ho Moon, Sang‐Heum Park
Journal of Gastroenterology and Hepatology.2021; 36(2): 467. CrossRef - Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) Guideline
Konstantinos Triantafyllou, Paraskevas Gkolfakis, Ian M. Gralnek, Kathryn Oakland, Gianpiero Manes, Franco Radaelli, Halim Awadie, Marine Camus Duboc, Dimitrios Christodoulou, Evgeny Fedorov, Richard J. Guy, Marcus Hollenbach, Mostafa Ibrahim, Ziv Neeman,
Endoscopy.2021; 53(08): 850. CrossRef - Estimation and influence of blood loss under endoscope for percutaneous endoscopic lumbar discectomy (PELD): a clinical observational study combined with in vitro experiment
Dong Dong Sun, Dan Lv, Wei Zhou Wu, He Fei Ren, Bu He Bao, Qun Liu, Ming Lin Sun
Journal of Orthopaedic Surgery and Research.2020;[Epub] CrossRef
- Updates on the Prevention and Management of Post-Polypectomy Bleeding in the Colon
- 14,676 View
- 589 Download
- 18 Web of Science
- 22 Crossref

-
First Characterization with Ultrasound Contrast Agent of a Fibrovascular Polyp Before Its Endoscopic Resection: A Case Report (with Videos)

- Nicolas Williet, Radwan Kassir, Francois Casteillo, Violaine Yvorel, Cyril Habougit, Xavier Roblin, Jean-Marc Phelip
- Clin Endosc 2019;52(2):186-190. Published online October 5, 2018
- DOI: https://doi.org/10.5946/ce.2018.083

-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - We described for the first time the contrast enhancement of a giant fibrovascular esophageal polyp using ultrasound contrast agent, Sonovue® (Bracco, Milan, Italy) during echoendoscopy. Fine Doppler was unsuccessful in showing vascularization due to the mobile characteristic of the tumor. In contrast, via Sonovue® , tissue microcirculation was highlighted inside the entire head of the polyp, leading to better appreciate the risk of bleeding related to its resection. In a second part, we showed the feasibility of classic polypectomy for this giant polyp (5×5 cm) without complication and results of control endoscopy at 3 months. The present case is summarized in a video.
-
Citations
Citations to this article as recorded by- Hybrid laparo-endoscopic access: New approach to surgical treatment for giant fibrovascular polyp of esophagus: A case report and review of literature
Seda Dzhantukhanova, Lyudmila Grigori Avetisyan, Amina Badakhova, Yury Starkov, Andrey Glotov
World Journal of Gastrointestinal Endoscopy.2023; 15(11): 666. CrossRef - Hybrid laparo-endoscopic access for giant fibrovascular esophageal polyp: a case report
Yu.G. Starkov, S.V. Dzhantukhanova, R.D. Zamolodchikov, A.B. Badakhova
Khirurgiya. Zhurnal im. N.I. Pirogova.2023; (11): 123. CrossRef
- Hybrid laparo-endoscopic access: New approach to surgical treatment for giant fibrovascular polyp of esophagus: A case report and review of literature
- 4,751 View
- 79 Download
- 1 Web of Science
- 2 Crossref

- Colonic Postpolypectomy Bleeding Is Related to Polyp Size and Heparin Use
- Flavia Pigò, Helga Bertani, Mauro Manno, Vincenzo Giorgio Mirante, Angelo Caruso, Santi Mangiafico, Raffaele Manta, Anna Maria Rebecchi, Rita Luisa Conigliaro
- Clin Endosc 2017;50(3):287-292. Published online February 9, 2017
- DOI: https://doi.org/10.5946/ce.2016.126
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: We studied factors influencing colon postpolypectomy bleeding (PPB), with a focus on antithrombotic and anticoagulation therapy.
Methods
We conducted a retrospective case-control study of all patients who underwent polypectomy at our tertiary referral center in Italy between 2007 and 2014. Polyp characteristics (number of polyps removed per patient, size, morphology, location, resection technique, prophylactic hemostasis methods) and patient characteristics (age, sex, comorbidities, medication) were analyzed.
Results
The case and control groups included 118 and 539 patients, respectively. The two groups differed in the frequency of comorbidities (69% vs. 40%, p=0.001), polyps removed (27% vs. 18%, p=0.02), and use of heparin therapy (23% vs. 1%, p<0.001). A total of 279 polyps in the case group and 966 in the control group were nonpedunculated (69% vs. 81%, p=0.01) and measured ≥10 mm (78% vs. 32%, p=0.001). Multivariate analysis showed that polyps ≥10 mm (odds ratio [OR], 6.1; 95% confidence interval [CI], 2.3–15.5), administration of heparin (OR, 16.5; 95% CI, 6.2–44), comorbidity (OR, 2.3; 95% CI, 1.4–3.9), and presence of ≥2 risk factors (OR, 3.2; 95% CI, 1.7–6.0) were associated with PPB.
Conclusions
The incidence of PPB increases with polyp size ≥10 mm, heparin use, comorbidity, and presence of ≥2 risk factors. -
Citations
Citations to this article as recorded by- Risk factors for post-polypectomy bleeding in patients with end-stage renal disease undergoing colonoscopic polypectomy
Jung Hyun Ji, Hyun Woo Kim, Jihye Park, Soo Jung Park, Jae Hee Cheon, Tae Il Kim, Jae Jun Park
Surgical Endoscopy.2023;[Epub] CrossRef - Polypectomy for Diminutive and Small Colorectal Polyps
Melissa Zarandi-Nowroozi, Roupen Djinbachian, Daniel von Renteln
Gastrointestinal Endoscopy Clinics of North America.2022; 32(2): 241. CrossRef - Effects of antithrombotic agents on post-operative bleeding after endoscopic resection of gastrointestinal neoplasms and polyps: A systematic review and meta-analysis
Bing-Jie Xiang, Yu-Hong Huang, Min Jiang, Cong Dai
World Journal of Meta-Analysis.2020; 8(5): 410. CrossRef - Effects of antithrombotic agents on post-operative bleeding after endoscopic resection of gastrointestinal neoplasms and polyps: A systematic review and meta-analysis
Bing-Jie Xiang, Yu-Hong Huang, Min Jiang, Cong Dai
World Journal of Meta-Analysis.2020; 8(5): 411. CrossRef - Post-polypectomy Visible Vessel
Matthew Woo, Robert Bechara
Journal of the Canadian Association of Gastroenterology.2018; 1(2): 51. CrossRef - Colorectal cancer screening program using FIT: quality of colonoscopy varies according to hospital type
Isabel Portillo, Isabel Idigoras, Isabel Bilbao, Eunate Arana-Arri, María José Fernández-Landa, Jose Luis Hurtado, Cristina Sarasaqueta, Luis Bujanda
Endoscopy International Open.2018; 06(09): E1149. CrossRef - Prediction and Prevention of Postpolypectomy Bleeding: Necessity of a Different Approach for Patients Using Antithrombotic Agents
Duk Hwan Kim
Clinical Endoscopy.2017; 50(3): 217. CrossRef
- Risk factors for post-polypectomy bleeding in patients with end-stage renal disease undergoing colonoscopic polypectomy
- 7,413 View
- 202 Download
- 5 Web of Science
- 7 Crossref

- Optimal Colonoscopy Surveillance Interval after Polypectomy
- Tae Oh Kim
- Clin Endosc 2016;49(4):359-363. Published online July 29, 2016
- DOI: https://doi.org/10.5946/ce.2016.080
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The detection and removal of adenomatous polyps and postpolypectomy surveillance are considered important for the control of colorectal cancer (CRC). Surveillance using colonoscopy is an effective tool for preventing CRC after colorectal polypectomy, especially if compliance is good. In current practice, the intervals between colonoscopies after polypectomy are variable. Different recommendations for recognizing at risk groups and defining surveillance intervals after an initial finding of colorectal adenomas have been published. However, high-grade dysplasia and the number and size of adenomas are known major cancer predictors. Based on this, a subgroup of patients that may benefit from intensive surveillance colonoscopy can be identified.
-
Citations
Citations to this article as recorded by- Gender disparities in colorectal polyps
A. K. Safiyeva
Klinicheskaia khirurgiia.2021; 88(1-2): 57. CrossRef - Three-year colonoscopy surveillance after polypectomy in Korea: a Korean Association for the Study of Intestinal Diseases (KASID) multicenter prospective study
Won Seok Choi, Dong Soo Han, Chang Soo Eun, Dong Il Park, Jeong-Sik Byeon, Dong-Hoon Yang, Sung-Ae Jung, Sang Kil Lee, Sung Pil Hong, Cheol Hee Park, Suck-Ho Lee, Jeong-Seon Ji, Sung Jae Shin, Bora Keum, Hyun Soo Kim, Jung Hye Choi, Sin-Ho Jung
Intestinal Research.2018; 16(1): 126. CrossRef
- Gender disparities in colorectal polyps
- 9,614 View
- 209 Download
- 2 Web of Science
- 2 Crossref

- Endoscopic Instruments and Electrosurgical Unit for Colonoscopic Polypectomy
- Hong Jun Park
- Clin Endosc 2016;49(4):350-354. Published online July 11, 2016
- DOI: https://doi.org/10.5946/ce.2016.059
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Colorectal polypectomy is an effective method for prevention of colorectal cancer. Many endoscopic instruments have been used for colorectal polypectomy, such as snares, forceps, endoscopic clips, a Coagrasper, retrieval net, injector, and electrosurgery generator unit (ESU). Understanding the characteristics of endoscopic instruments and their proper use according to morphology and size of the colorectal polyp will enable endoscopists to perform effective polypectomy. I reviewed the characteristics of endoscopic instruments for colorectal polypectomy and their appropriate use, as well as the basic principles and settings of the ESU.
-
Citations
Citations to this article as recorded by- Expert consensus on the clinical application of high‐frequency electrosurgery in digestive endoscopy (2020, Shanghai)
Yu Bai, Fan Yang, Cui Liu, De Feng Li, Shi Wang, Rong Lin, Zhen Ding, Wen Bo Meng, Zhao Shen Li, En Qiang Linghu
Journal of Digestive Diseases.2022; 23(1): 2. CrossRef - Thermic Epidermic Tissue Surgical Generator Using Bipolar Electrode
Dhanalakshmi K.S, Azhagu Jaisudhan Pazhani A, Anusha Padmavathy R
Innovations in Information and Communication Technology Series.2021; : 68. CrossRef
- Expert consensus on the clinical application of high‐frequency electrosurgery in digestive endoscopy (2020, Shanghai)
- 11,872 View
- 382 Download
- 1 Web of Science
- 2 Crossref

- Use of a Double-Channel Gastroscope Reduces Procedural Time in Large Left-Sided Colonic Endoscopic Mucosal Resections
- Evangelos Voudoukis, Georgios Tribonias, Aikaterini Tavernaraki, Angeliki Theodoropoulou, Emmanouil Vardas, Konstantina Paraskeva, Gregorios Chlouverakis, Gregorios A. Paspatis
- Clin Endosc 2015;48(2):136-141. Published online March 27, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.2.136
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Endoscopic mucosal resection (EMR) of large colorectal lesions is associated with increased procedural time. The objective of this study was to evaluate the effect of double-channel gastroscope (DCG) use on the procedural time of EMRs in the rectosigmoid area.
Methods All EMRs for sessile or flat rectosigmoid lesions ≥2 cm performed between July 2011 and September 2012 were retrospectively analyzed.
Results There were 55 lesions ≥2 cm in the rectosigmoid area in 55 patients, of which 26 were removed by EMR using a DCG (DC group) and 29 by using an ordinary colonoscope or gastroscope (OS group). The mean size of the removed polyps, morphology, adverse effects, and other parameters were similar between the two groups. The mean procedural time was significantly lower in the DC group than in the OS group (24.4±18.3 minutes vs. 36.3±24.4 minutes,
p =0.015). Moreover, in a subgroup of patients with polyps >40 mm, the statistical difference in the mean procedural time between the DC and OS groups was even more pronounced (33±21 minutes vs. 58.7±20.6 minutes,p =0.004).Conclusions Our data suggest that the use of a DCG in the resection of large nonpedunculated rectosigmoid lesions significantly reduces the procedural time.
-
Citations
Citations to this article as recorded by- Dual Channel Endoscopic Mucosal Resection
Julia T. Saraidaridis, Racquel S. Gaetani, Peter W. Marcello
Clinics in Colon and Rectal Surgery.2023;[Epub] CrossRef - Endoscopic management of difficult laterally spreading tumors in colorectum
Edgar Castillo-Regalado, Hugo Uchima
World Journal of Gastrointestinal Endoscopy.2022; 14(3): 113. CrossRef - Novel technique for endoscopic en bloc resection (EMR+) – Evaluation in a porcine model
Benjamin Meier, Andreas Wannhoff, Christoph Klinger, Karel Caca
World Journal of Gastroenterology.2019; 25(28): 3764. CrossRef - Endoscopic mucosal resection and endoscopic submucosal dissection for colorectal lesions: A systematic review
Antonella De Ceglie, Cesare Hassan, Benedetto Mangiavillano, Takahisa Matsuda, Yutaka Saito, Lorenzo Ridola, Pradeep Bhandari, Federica Boeri, Massimo Conio
Critical Reviews in Oncology/Hematology.2016; 104: 138. CrossRef - Is the Double Channel Gastroscope Useful in Endoscopic Mucosal Resection for Large Sessile Colon Polyps?
Kwang An Kwon
Clinical Endoscopy.2015; 48(2): 89. CrossRef
- Dual Channel Endoscopic Mucosal Resection
- 7,073 View
- 57 Download
- 6 Web of Science
- 5 Crossref

- Postpolypectomy Fever, a Rare Adverse Event of Polypectomy: Nested Case-Control Study
- Seung-Hoon Lee, Kyung-Jo Kim, Dong-Hoon Yang, Kee Wook Jeong, Byong Duk Ye, Jeong-Sik Byeon, Seung-Jae Myung, Suk-Kyun Yang, Jin-Ho Kim
- Clin Endosc 2014;47(3):236-241. Published online May 31, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.3.236
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Although postpolypectomy fever (PPF) without colon perforation or hemorrhage is rare, its incidence and risk factors have not been investigated. The objective of this study was to analyze the incidence and risk factors for PPF among inpatients.
Methods Seven patients with PPF were matched with 70 patients without PPF from a total of 3,444 patients who underwent colonoscopic polypectomy. The PPF incidence during index hospitalization after colonoscopy was calculated, and univariate and multivariate analyses were performed to calculate the adjusted odds ratios (ORs) for risk factors.
Results PPF without bleeding or perforation in the colon occurred in seven patients (0.2%). The median age was 58 years for cases and 61 years for controls. The median interval from polypectomy to occurrence of fever was 7 hours, and the median duration of fever was 9 hours. Polyp size >2 cm (adjusted OR, 1.08; 95% confidence interval [CI], 1.01 to 1.15;
p =0.02) and hypertension (adjusted OR, 14.40; 95% CI, 1.23 to 180.87;p =0.03) were associated with a significantly increased risk of PPF. PPF increased the length of hospitalization.Conclusions Although the crude incidence of PPF is low, PPF may prolong hospitalization. Risk factors for PPF include hypertension and large polyps.
-
Citations
Citations to this article as recorded by- Cold Snare Cut Versus Avulsion for Colonic Mucosal Resection: A Randomized Ex Vivo Porcine Study (the CONVINCE Study)
Neal A. Mehta, James K. Stone, Roberto Trasolini, Yuho Ono, Mandeep S. Sawhney
Techniques and Innovations in Gastrointestinal Endoscopy.2023; 25(4): 315. CrossRef - Cold Endoscopic Mucosal Resection (c-EMR) of Nonpedunculated Colorectal Polyps ≥20 mm
Daryl Ramai, Benjamin Clement, Marcello Maida, Melissa Previtera, Olivia W. Brooks, Yichen Wang, Saurabh Chandan, Banreet Dhindsa, Smit Deliwala, Antonio Facciorusso, Mouen Khashab, Andrew Ofosu
Journal of Clinical Gastroenterology.2023;[Epub] CrossRef - Risk factors of medication‐related osteonecrosis of the jaw in preventive tooth extraction before bone resorption inhibitor administration: A multicenter nested case–control study
Taro Saito, Atsushi Nishikawa, Yuko Hara‐Saito, Andrea Rei Estacio Salazar, Akira Kurokawa, Akihiko Iida, Masahiro Yamaga, Hiroyuki Kano, Yusuke Kato, Yoshiyuki Takata, Hideyoshi Nishiyama, Nobutaka Kitamura, Takahiro Tanaka, Ritsuo Takagi
Oral Science International.2022; 19(2): 79. CrossRef - Postpolypectomy fever in patients with serious infection: a report of two cases
Wang Jing, Li Qinghua, Yang Zhiwen
BMC Gastroenterology.2022;[Epub] CrossRef - RoboCap: Robotic mucus-clearing capsule for enhanced drug delivery in the gastrointestinal tract
Shriya S. Srinivasan, Amro Alshareef, Alexandria V. Hwang, Ziliang Kang, Johannes Kuosmanen, Keiko Ishida, Joshua Jenkins, Sabrina Liu, Wiam Abdalla Mohammed Madani, Jochen Lennerz, Alison Hayward, Josh Morimoto, Nina Fitzgerald, Robert Langer, Giovanni T
Science Robotics.2022;[Epub] CrossRef - Pylephlebitis after sigmoid colonic polypectomy
Yuna Saito, Toshinori Nishizawa, Hiroko Arioka
BMJ Case Reports.2022; 15(12): e253095. CrossRef - Management of Pediatric Postendoscopy Fever
Julia M. Boster, Melissa Iwanowski, Robert E. Kramer
Journal of Pediatric Gastroenterology and Nutrition.2021; 72(2): 250. CrossRef - Cold versus hot polypectomy/endoscopic mucosal resection–A review of current evidence
Raquel Ortigão, Jochen Weigt, Ahmed Afifi, Diogo Libânio
United European Gastroenterology Journal.2021; 9(8): 938. CrossRef - Periprocedural adverse events after endoscopic resection of T1 colorectal carcinomas
Steffi E.M. van de Ven, Yara Backes, Mirrian Hilbink, Tom C.J. Seerden, Koen Kessels, Wouter H. de Vos tot Nederveen Cappel, John N. Groen, Frank H.J. Wolfhagen, Joost M.J. Geesing, Frank ter Borg, Jeroen van Bergeijk, B.W.M. Spanier, Marco W. Mundt, H.J.
Gastrointestinal Endoscopy.2020; 91(1): 142. CrossRef - Colección abscesificada en pared abdominal secundaria a polipectomía colonoscópica. Manejo radiológico
María Luisa García-García, Miguel Ángel Jiménez-Ballester, Enrique Girela-Baena, José Luis Aguayo-Albasini
Gastroenterología y Hepatología.2017; 40(7): 463. CrossRef - Endoscopic shielding technique with a newly developed hydrogel to prevent thermal injury in two experimental models
Vicente Lorenzo‐Zúñiga, Jaume Boix, Vicente Moreno de Vega, Ignacio Bon, Ingrid Marín, Ramón Bartolí
Digestive Endoscopy.2017; 29(6): 702. CrossRef - Colorectal endoscopic mucosal resection (EMR)
Pujan Kandel, Michael B. Wallace
Best Practice & Research Clinical Gastroenterology.2017; 31(4): 455. CrossRef - Abdominal wall abscess secondary to colonoscopic polypectomy. Radiological management
María Luisa García-García, Miguel Ángel Jiménez-Ballester, Enrique Girela-Baena, José Luis Aguayo-Albasini
Gastroenterología y Hepatología (English Edition).2017; 40(7): 463. CrossRef - Complications of endoscopic polypectomy, endoscopic mucosal resection and endoscopic submucosal dissection in the colon
Michael X. Ma, Michael J. Bourke
Best Practice & Research Clinical Gastroenterology.2016; 30(5): 749. CrossRef - What Is Different between Postpolypectomy Fever and Postpolypectomy Coagulation Syndrome?
Hyung Wook Kim
Clinical Endoscopy.2014; 47(3): 205. CrossRef
- Cold Snare Cut Versus Avulsion for Colonic Mucosal Resection: A Randomized Ex Vivo Porcine Study (the CONVINCE Study)
- 7,270 View
- 90 Download
- 15 Web of Science
- 15 Crossref

- A Polypoid Mucosa-Associated Lymphoid Tissue Lymphoma of the Stomach Treated with Endoscopic Polypectomy
- Shin Young Min, Jun Haeng Lee, Poong-Lyul Rhee
- Clin Endosc 2013;46(6):647-650. Published online November 19, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.6.647
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Mucosa-associated lymphoid tissue (MALT) lymphoma of the stomach is the most common extranodal lymphoma of the gastrointestinal tract. It is usually accompanied by
Helicobacter pylori infection, and eradication ofH. pylori remains the mainstay of treatment for gastric MALT lymphoma. However, there is no consensus on the second-line treatment for patients with gastric MALT lymphoma who do not improve after successfulH. pylori eradication. Here, we report the case of a 34-year-old woman who presented with a polypoid type of gastric MALT lymphoma on the greater curvature side of the upper body. Despite successfulH. pylori eradication, the tumor did not regress after 6 months. Because the tumor had a semipedunculated polypoid morphology, gastric polypectomy was implemented as a second-line treatment. No recurrence occurred during the 3-year follow-up period. We suggest that gastric polypectomy be considered an alternative treatment modality for polypoid gastric MALT lymphoma that is unresponsive toH. pylori eradication.
- 6,215 View
- 42 Download

- New Paradigms for Colonoscopic Management of Diminutive Colorectal Polyps: Predict, Resect, and Discard or Do Not Resect?
- Cesare Hassan, Alessandro Repici, Angelo Zullo, Prateek Sharma
- Clin Endosc 2013;46(2):130-137. Published online March 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.2.130
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub The possibility to predict
in vivo the histology of colorectal polyps by advanced endoscopic imaging has resulted in the implementation of a more conservative management for diminutive lesions detected at colonoscopy. In detail, a predict-and-do-not-resect strategy has been proposed for diminutive lesions located in the rectosigmoid tract, whilst a predict-resect-and-discard policy has been advocated for nonrectosigmoid diminutive polyps. Recently, the American Society for Gastrointestinal Endoscopy set required thresholds to be met, before allowing the adoption of these policies in the clinical field. The ability of current endoscopic imaging in reaching these thresholds would depend on a complex interaction among the accuracy of advanced endoscopic imaging in differentiating between adenomatous and hyperplastic lesions, the prevalence of (advanced) neoplasia within diminutive lesions, and the type of surveillance intervals recommended. Aim of this review is to summarize the data supporting the application of both a predict-and-do-not-resect and a predict-resect-and-discard policies, also addressing the potential pitfalls associated with these strategies.-
Citations
Citations to this article as recorded by- Pit pattern analysis of colorectal polyps using Storz professional image enhancement system (SPIES) endoscopy: A pilot study
Emeka Ray-Offor, FatimahBiade Abdulkareem, NzeJ Jebbin
Journal of West African College of Surgeons.2022; 12(2): 17. CrossRef - Diminutif ve Küçük Kolorektal Poliplerde Kanser Riskinin Değerlendirilmesi
Nurhan DEMİR
Artuklu International Journal of Health Sciences.2022; 2(3): 20. CrossRef - POLYP AND ADENOMA DETECTION RATE AND EVALUATION OF DIFFERENT POLYP RETRIEVAL METHODS IN PATIENTS UNDERGOING COLONOSCOPY IN KURDISTAN CENTER FOR GASTROENTEROLOGY AND HEPATOLOGY/SULAIMANI CITY (KCGH)
Sarkawt Ameen, Muhsin Mohammed, Mohammed Alshaikhani, Mohammed Mohammed, Taha Al-Karbuly, Dana Gharib, Araz Latif
JOURNAL OF SULAIMANI MEDICAL COLLEGE.2021; 11(4): 407. CrossRef - Efficacy and safety of cold versus hot snare polypectomy for resecting small colorectal polyps: Systematic review and meta‐analysis
Satoshi Shinozaki, Yasutoshi Kobayashi, Yoshikazu Hayashi, Hirotsugu Sakamoto, Alan Kawarai Lefor, Hironori Yamamoto
Digestive Endoscopy.2018; 30(5): 592. CrossRef - Clinical, endoscopic and pathological characteristics of colorectal polyps in elderly patients: Single-center experience
Lei Zhou, Heng Zhang, Shengbin Sun, Manling Huang, Jing Liu, Dan Xu, Min Song, Chenming Sun, Hui Li, Dan Zheng, Yan Fan, Yusheng Liao, Ping Wang, Jie Wu
Molecular and Clinical Oncology.2017; 7(1): 81. CrossRef - Results of total colonoscopy in the diagnosis of polyps. Case studies in Villavicencio, Colombia
Mauricio Alberto Melo-Peñaloza
Revista de la Facultad de Medicina.2017; 65(3): 433. CrossRef - Narrow-band Imaging International Colorectal Endoscopic Classification to predict polyp histology: REDEFINE study (with videos)
Alessandro Repici, Camilla Ciscato, Loredana Correale, Raf Bisschops, Pradeep Bhandari, Evelien Dekker, Oliver Pech, Franco Radaelli, Cesare Hassan
Gastrointestinal Endoscopy.2016; 84(3): 479. CrossRef - The Assessment of the Colo-rectal Polyps in Order to the New Diagnostic and Therapeutic Strategies
Diac Andreea Raluca, Brusnic Olga, Gabos Gabriella, Onisor Danusia, Drasoveanu Silvia Cosmina, Boeriu Alina, Dobru Daniela Ecaterina
Acta Medica Marisiensis.2015; 61(3): 161. CrossRef - Risk factors for polyp retrieval failure in colonoscopy
Carlos Fernandes, Rolando Pinho, Iolanda Ribeiro, Joana Silva, Ana Ponte, João Carvalho
United European Gastroenterology Journal.2015; 3(4): 387. CrossRef - Accuracy of visual prediction of pathology of colorectal polyps: how accurate are we?
Prashant Sharma, John Frye, Frank Frizelle
ANZ Journal of Surgery.2014; 84(5): 365. CrossRef
- Pit pattern analysis of colorectal polyps using Storz professional image enhancement system (SPIES) endoscopy: A pilot study
- 7,254 View
- 67 Download
- 10 Crossref

- Endoscopic Resection for Rectal Carcinoid Tumors: Comparision of Polypectomy and Endoscopic Submucosal Resection with Band Ligation
- Sang Heon Lee, Seun Ja Park, Hyung Hun Kim, Kyung Sun Ok, Ji Hyun Kim, Sam Ryong Jee, Sang Young Seol, Bo Mi Kim
- Clin Endosc 2012;45(1):89-94. Published online March 31, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.1.89
- Retraction in: Clin Endosc 2015;48(1):87
- 8,175 View
- 49 Download
- 17 Crossref

- Clipping for the Prevention of Immediate Bleeding after Polypectomy of Pedunculated Polyps: A Pilot Study
- Sun-Jin Boo, Jeong-Sik Byeon, Seon Young Park, Jong Sun Rew, Da Mi Lee, Sung Jae Shin, Dong Uk Kim, Geum Am Song
- Clin Endosc 2012;45(1):84-88. Published online March 31, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.1.84
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Immediate postpolypectomy bleeding (IPPB) increases the procedure time and it may disturb performing a safe polypectomy. The purpose of this study is to investigate whether clipping before snare polypectomy of large pedunculated polyps is useful for the prevention of IPPB.
Methods This is a single arm, pilot study. We enrolled patients with pedunculated colorectal polyps that were 1 cm in size or more from 4 university hospitals between June 2009 and June 2010. Clips were applied at the stalk and snare polypectomy was then performed. The complications, including IPPB, were investigated.
Results Fifty six pedunculated polyps in 47 patients (Male:Female=36:11; age, 56±11 years) were included. The size of the polyp heads was 17±8 mm. Tubular adenoma was most common (57%). The number of clips used before snare polypectomy was 2±0.5. The procedure was successful in all cases. IPPB occurred in 2 cases (3.6%), and both of these were managed by additional clipping. Delayed bleeding occurred in another one case (1.8%), which improved with conservative treatment. No perforation occurred.
Conclusions We suggest that clipping before snare polypectomy of pedunculated polyps may be an easy and effective technique for the prevention of IPPB, and this should be confirmed in large scale, prospective, controlled studies.
-
Citations
Citations to this article as recorded by- A novel technique using endoscopic band ligation for removal of long-stalked (>10 mm) pedunculated colon polyps: A prospective pilot study
HyunHo Choi, ChangWhan Kim, Hyung-Keun Kim, SangWoo Kim, SokWon Han, KyungJin Seo, Hiun-Suk Chae
Saudi Journal of Gastroenterology.2021; 27(5): 296. CrossRef - Endoscopic polypectomy devices
Vinay Chandrasekhara, Nikhil A. Kumta, Barham K. Abu Dayyeh, Manoop S. Bhutani, Pichamol Jirapinyo, Kumar Krishnan, John T. Maple, Joshua Melson, Rahul Pannala, Mansour A. Parsi, Amrita Sethi, Guru Trikudanathan, Arvind J. Trindade, David R. Lichtenstein
VideoGIE.2021; 6(7): 283. CrossRef - Prophylactic clip application for large pedunculated polyps before snare polypectomy may decrease immediate postpolypectomy bleeding
Jae Seung Soh, Myeongsook Seo, Kyung-Jo Kim
BMC Gastroenterology.2020;[Epub] CrossRef - Management of colonic polyps: an advancing discipline
Amir Klein, Michael J. Bourke
ANZ Journal of Surgery.2017; 87(5): 327. CrossRef - Massive post‐polypectomy hemorrhage: Successful tulip‐bundle technique with endoloop for hemostasis
Hsu‐Heng Yen, Chia‐Wei Yang, Shun‐Sheng Wu, Maw‐Soan Soon
Advances in Digestive Medicine.2016; 3(3): 128. CrossRef - Advanced Polypectomy and Resection Techniques
Amir Klein, Michael J. Bourke
Gastrointestinal Endoscopy Clinics of North America.2015; 25(2): 303. CrossRef - Comparison of clipping with and without epinephrine injection for the prevention of post‐polypectomy bleeding in pedunculated colon polyps
Yehyun Park, Tae Joo Jeon, Ji Young Park, Soo Jung Park, Jae Hee Cheon, Tae Il Kim, Won Ho Kim, Sung Pil Hong
Journal of Gastroenterology and Hepatology.2015; 30(10): 1499. CrossRef - Endoscopic haemostasis: An overview of procedures and clinical scenarios
Jérémie Jacques, Romain Legros, Stanislas Chaussade, Denis Sautereau
Digestive and Liver Disease.2014; 46(9): 766. CrossRef - Advanced Endoscopic Resection of Colorectal Lesions
Andres Sanchez-Yague, Tonya Kaltenbach, Gottumukkala Raju, Roy Soetikno
Gastroenterology Clinics of North America.2013; 42(3): 459. CrossRef - A Cost-efficacy Decision Analysis of Prophylactic Clip Placement After Endoscopic Removal of Large Polyps
Neehar D. Parikh, Kyle Zanocco, Rajesh N. Keswani, Andrew J. Gawron
Clinical Gastroenterology and Hepatology.2013; 11(10): 1319. CrossRef - Fat Polyp, Thin Blood: Think Clip!
Laura Borodyansky, John R. Saltzman
Clinical Gastroenterology and Hepatology.2013; 11(10): 1333. CrossRef
- A novel technique using endoscopic band ligation for removal of long-stalked (>10 mm) pedunculated colon polyps: A prospective pilot study
- 9,124 View
- 74 Download
- 11 Crossref

- Korean Guidelines for Postpolypectomy Colonoscopy Surveillance
- Dong-Hoon Yang, Sung Noh Hong, Young-Ho Kim, Sung Pil Hong, Sung Jae Shin, Seong-Eun Kim, Bo In Lee, Suck-Ho Lee, Dong Il Park, Hyun-Soo Kim, Suk-Kyun Yang, Hyo Jong Kim, Se Hyung Kim, Hyun Jung Kim, Multi-Society Task Force for Development of Guidelines for Colorectal Polyp Screening, Surveillance and Management
- Clin Endosc 2012;45(1):44-61. Published online March 31, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.1.44
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub Postpolypectomy surveillance has become a major indication for colonoscopy as a result of increased use of screening colonoscopy in Korea. In this report, a careful analytic approach was used to address all available evidences to delineate the predictors for advanced neoplasia at surveillance colonoscopy and we elucidated the high risk findings of the index colonoscopy as follows: 3 or more adenomas, any adenoma larger than 10 mm, any tubulovillous or villous adenoma, any adenoma with high-grade dysplasia, and any serrated polyps larger than 10 mm. Surveillance colonoscopy should be performed five years after the index colonoscopy for those without any high-risk findings and three years after the index colonoscopy for those with one or more high risk findings. However, the surveillance interval can be shortened considering the quality of the index colonoscopy, the completeness of polypectomy, the patient's general condition, and family and medical history.
-
Citations
Citations to this article as recorded by- Post-colonoscopy colorectal cancers in a national fecal immunochemical test-based colorectal cancer screening program
Pieter H. A. Wisse, Sybrand Y. de Boer, Marco Oudkerk Pool, Jochim S Terhaar sive Droste, Claudia Verveer, Gerrit A. Meijer, Evelien Dekker, Manon C. W. Spaander
Endoscopy.2024; 56(05): 364. CrossRef - Recurrence rates of advanced colorectal neoplasia (ACN) in subjects with baseline ACN followed up at different surveillance intervals
Martin C.S. Wong, Eman Yee-man Leung, Sam C.C. Chun, Yunyang Deng, Thomas Lam, Raymond S.Y. Tang, Junjie Huang
Digestive and Liver Disease.2023; 55(12): 1742. CrossRef - Risk of recurrent advanced colorectal neoplasia in individuals with baseline non‐advanced neoplasia followed up at 5 vs 7–10 years
Martin C. S. Wong, Eman Yee‐man Leung, Sam C. C. Chun, Yunyang Deng, Thomas Lam, Raymond S. Y. Tang, Junjie Huang
Journal of Gastroenterology and Hepatology.2023; 38(12): 2122. CrossRef - Third Asia-Pacific consensus recommendations on colorectal cancer screening and postpolypectomy surveillance
Joseph J Y Sung, Han-Mo Chiu, David Lieberman, Ernst J Kuipers, Matthew D Rutter, Finlay Macrae, Khay-Guan Yeoh, Tiing Leong Ang, Vui Heng Chong, Sneha John, Jingnan Li, Kaichun Wu, Simon S M Ng, Govind K Makharia, Murdani Abdullah, Nozomu Kobayashi, Masa
Gut.2022; 71(11): 2152. CrossRef - Optimization of the surveillance strategy in patients with colorectal adenomas: A combination of clinical parameters and index colonoscopy findings
Chan Hyuk Park, Yoon Suk Jung, Nam Hee Kim, Jung Ho Park, Dong Il Park, Chong Il Sohn
Journal of Gastroenterology and Hepatology.2021; 36(4): 974. CrossRef - Increasing changes in visceral adiposity is associated with higher risk for colorectal adenoma: Multilevel analysis in a prospective cohort
Jung Min Moon, Jong Pil Im, Donghee Kim, Yoo Min Han, Hosim Soh, Ji Hyun Song, Sun Young Yang, Young Sun Kim, Jeong Yoon Yim, Seon Hee Lim, Joo Sung Kim
Journal of Gastroenterology and Hepatology.2021; 36(7): 1836. CrossRef - Strategies for colorectal cancer screening and post-polypectomy surveillance for young adults under age 50
Yoon Suk Jung
Precision and Future Medicine.2021; 5(2): 69. CrossRef - Adherence to Surveillance Guidelines after the Removal of Colorectal Polyps: A Multinational, Multicenter, Prospective Survey
Chang Kyo Oh, Satimai Aniwan, Panida Piyachaturawat, Zhiqin Wong, Thida Soe, Bayasgalan Luvsandagva, Quang Trung Tran, Achmad Fauzi, Jeong-Sik Byeon, Young-Seok Cho
Gut and Liver.2021; 15(6): 878. CrossRef - Colon Polyp Detection in Primary Health Care Institutions of Korea: Detection Rate and Issues with Following the Guidelines
Sang Hyun Park, Kwang Il Hong, Hyun Chul Park, Young Sun Kim, Gene Hyun Bok, Kyung Ho Kim, Dong Suk Shin, Jae Yong Han, Young Kwan Kim, Yeun Jong Choi, Soo Hoon Eun, Byung Hoon Lim, Kyeong Kun Kwack
The Korean Journal of Gastroenterology.2021; 78(6): 328. CrossRef - Effect of Cotinine-Verified Change in Smoking Status on Risk of Metachronous Colorectal Neoplasia After Polypectomy
Yoon Suk Jung, Nam Hee Kim, Mi Yeon Lee, Jung Ho Park, Dong Il Park, Chong Il Sohn
Clinical Gastroenterology and Hepatology.2020; 18(1): 163. CrossRef - Risk of developing metachronous advanced colorectal neoplasia after resection of low-risk diminutive versus small adenomas
Nam Hee Kim, Yoon Suk Jung, Jung Ho Park, Dong Il Park, Chong Il Sohn
Gastrointestinal Endoscopy.2020; 91(3): 622. CrossRef - Colorectal sessile serrated lesion with large size or synchronous neoplasm: a prospective study
Laxmi B. Chavali, Kun Hu, Anish Sheth, Nan Gao, Wei Xiong, Lanjing Zhang
European Journal of Gastroenterology & Hepatology.2020; 32(2): 199. CrossRef - Colorectal Polyp Prevalence According to Alcohol Consumption, Smoking and Obesity
Kyujin Lee, Yong Hwan Kim
International Journal of Environmental Research and Public Health.2020; 17(7): 2387. CrossRef - Comparative systematic review and meta-analysis of 1- to 5-mm versus 6- to 9-mm adenomas on the risk of metachronous advanced colorectal neoplasia
Yoon Suk Jung, Tae Jun Kim, Eunwoo Nam, Chan Hyuk Park
Gastrointestinal Endoscopy.2020; 92(3): 692. CrossRef - The current capacity and quality of colonoscopy in Korea
Jae Ho Choi, Jae Myung Cha, Jin Young Yoon, Min Seob Kwak, Jung Won Jeon, Hyun Phil Shin
Intestinal Research.2019; 17(1): 119. CrossRef - Appropriate Surveillance Interval after Colonoscopic Polypectomy in Patients Younger than 50 Years
Yoon Suk Jung, Nam Hee Kim, Jung Ho Park, Dong Il Park, Chong Il Sohn
Journal of Korean Medical Science.2019;[Epub] CrossRef - Terminology, Molecular Features, Epidemiology, and Management of Serrated Colorectal Neoplasia
Seth D. Crockett, Iris D. Nagtegaal
Gastroenterology.2019; 157(4): 949. CrossRef - Risk of Developing Metachronous Advanced Colorectal Neoplasia After Polypectomy in Patients With Multiple Diminutive or Small Adenomas
Nam Hee Kim, Yoon Suk Jung, Mi Yeon Lee, Jung Ho Park, Dong Il Park, Chong Il Sohn
American Journal of Gastroenterology.2019; 114(10): 1657. CrossRef - Visceral obesity as a risk factor for colorectal adenoma occurrence in surveillance colonoscopy
Jong Pil Im, Donghee Kim, Su Jin Chung, Eun Hyo Jin, Yoo Min Han, Min Jung Park, Ji Hyun Song, Sun Young Yang, Young Sun Kim, Jeong Yoon Yim, Seon Hee Lim, Joo Sung Kim
Gastrointestinal Endoscopy.2018; 88(1): 119. CrossRef - Guideline Adherence to Colonoscopic Surveillance Intervals after Polypectomy in Korea: Results from a Nationwide Survey
Seri Hong, Mina Suh, Kui Son Choi, Boyoung Park, Jae Myung Cha, Hyun-Soo Kim, Jae Kwan Jun, Dong Soo Han
Gut and Liver.2018; 12(4): 426. CrossRef - Risk factors of nonadherence to colonoscopy surveillance after polypectomy and its impact on clinical outcomes: a KASID multicenter study
Chung Hyun Tae, Chang Mo Moon, Seong-Eun Kim, Sung-Ae Jung, Chang Soo Eun, Jae Jun Park, Geom Seog Seo, Jae Myung Cha, Sung Chul Park, Jaeyoung Chun, Hyun Jung Lee, Yunho Jung, Jin Oh Kim, Young-Eun Joo, Dong Il Park
Journal of Gastroenterology.2017; 52(7): 809. CrossRef - Unusual Local Recurrence with Distant Metastasis after Successful Endoscopic Submucosal Dissection for Colorectal Mucosal Cancer
Hyo Jeong Lee, Byong Duk Ye, Jeong-Sik Byeon, Jihun Kim, Young Soo Park, Yong Sang Hong, Yong Sik Yoon, Dong-Hoon Yang
Clinical Endoscopy.2017; 50(1): 91. CrossRef - Determining the optimal surveillance interval after a colonoscopic polypectomy for the Korean population?
Jung Lok Lee, Jae Myung Cha, Hye Min Lee, Jung Won Jeon, Min Seob Kwak, Jin Young Yoon, Hyun Phil Shin, Kwang Ro Joo, Joung Il Lee, Dong Il Park
Intestinal Research.2017; 15(1): 109. CrossRef - Advanced Colonic Neoplasia at Follow-up Colonoscopy According to Risk Components and Adenoma Location at Index Colonoscopy: A Retrospective Study of 1,974 Asymptomatic Koreans
Su Jung Baik, Hyojin Park, Jae Jun Park, Hyun Ju Lee, So Young Jo, Yoo Mi Park, Hye Sun Lee
Gut and Liver.2017; 11(5): 667. CrossRef - The Serrated Polyp Pathway: Is It Time to Alter Surveillance Guidelines?
Brendon O’Connell, Nazar Hafiz, Seth Crockett
Current Gastroenterology Reports.2017;[Epub] CrossRef - Optimizing post‐polypectomy surveillance: A practical guide for the endoscopist
Roel Bogie, Silvia Sanduleanu
Digestive Endoscopy.2016; 28(3): 348. CrossRef - Cap-assisted EMR for rectal neuroendocrine tumors: comparisons with conventional EMR and endoscopic submucosal dissection (with videos)
Dong-Hoon Yang, Yangsoon Park, Sang Hyoung Park, Kyung-Jo Kim, Byong Duk Ye, Jeong-Sik Byeon, Seung-Jae Myung, Suk-Kyun Yang
Gastrointestinal Endoscopy.2016; 83(5): 1015. CrossRef - Colorectal cancer screening of the general population in East Asia
Yasushi Sano, Jeong‐Sik Byeon, Xiao‐Bo Li, Martin C.S. Wong, Han‐Mo Chiu, Rungsun Rerknimitr, Takahiro Utsumi, Santa Hattori, Wataru Sano, Mineo Iwatate, Philip Chiu, Joseph Sung
Digestive Endoscopy.2016; 28(3): 243. CrossRef - Surveillance colonoscopy after endoscopic treatment for colorectal neoplasia: From the standpoint of the Asia–Pacific region
Takahisa Matsuda, Han‐Mo Chiu, Yasushi Sano, Takahiro Fujii, Akiko Ono, Yutaka Saito
Digestive Endoscopy.2016; 28(3): 342. CrossRef - Long-Term Outcome and Surveillance Colonoscopy after Successful Endoscopic Treatment of Large Sessile Colorectal Polyps
Bun Kim, A Ra Choi, Soo Jung Park, Jae Hee Cheon, Tae Il Kim, Won Ho Kim, Sung Pil Hong
Yonsei Medical Journal.2016; 57(5): 1106. CrossRef - Probability of High-Risk Colorectal Neoplasm Recurrence Based on the Results of Two Previous Colonoscopies
Hye Won Park, Seungbong Han, Ji Young Lee, Hye-Sook Chang, Jaewon Choe, Yunsik Choi, Hoonsub So, Dong-Hoon Yang, Seung-Jae Myung, Suk-Kyun Yang, Jin-Ho Kim, Jeong-Sik Byeon
Digestive Diseases and Sciences.2015; 60(1): 226. CrossRef - Distribution of the Colonoscopic Adenoma Detection Rate According to Age: Is Recommending Colonoscopy Screening for Koreans Over the Age of 50 Safe?
Taeseok Bae, Yunhyung Ha, Changkyun Kim, Jihyun Lee, Kwangil Ha, Sanghyun Shin, Youngcheol Lee, Yoonsik Kang
Annals of Coloproctology.2015; 31(2): 46. CrossRef - Risk of adenomas with high‐risk characteristics based on two previous colonoscopy
Kang‐Heum Suh, Ja Seol Koo, Jong Jin Hyun, Jungsoon Choi, Jang Soo Han, Seung Young Kim, Sung Woo Jung, Yoon Tae Jeen, Sang Woo Lee, Jai Hyun Choi
Journal of Gastroenterology and Hepatology.2014; 29(12): 1985. CrossRef - Only the Size of Resected Polyps Is an Independent Risk Factor for Delayed Postpolypectomy Hemorrhage: A 10-Year Single-Center Case-Control Study
Hee Seok Moon, Sun Wook Park, Dong Hwan Kim, Sun Hyung Kang, Jae Kyu Sung, Hyun Yong Jeong
Annals of Coloproctology.2014; 30(4): 182. CrossRef - Prevalence of and Risk Factors for Gastrointestinal Diseases in Korean Americans and Native Koreans Undergoing Screening Endoscopy
Hee Sun Kim, Su Jung Baik, Kyung Hee Kim, Cho Rong Oh, Jung Hyun Lee, Wan Jae Jo, Hye Kyoung Kim, Eun Young Kim, Min Jung Kim
Gut and Liver.2013; 7(5): 539. CrossRef - Proximal colon cancer and serrated adenomas – hunting the missing 10%
Pelvender Gill, Hannah Rafferty, David Munday, Adam Bailey, Lai Mun Wang, James E East, Runjan Chetty, Simon J Leedham
Clinical Medicine.2013; 13(6): 557. CrossRef - Relationship of Non-Alcoholic Fatty Liver Disease to Colorectal Neoplasia
Jue Yong Lee, Ja Won Kim
Korean Journal of Medicine.2013; 84(3): 363. CrossRef - Highlights of International Digestive Endoscopy Network 2013
Kwang An Kwon, Il Ju Choi, Eun Young Kim, Seok Ho Dong, Ki Baik Hahm
Clinical Endoscopy.2013; 46(5): 425. CrossRef
- Post-colonoscopy colorectal cancers in a national fecal immunochemical test-based colorectal cancer screening program
- 10,175 View
- 161 Download
- 38 Crossref

- Korean Guideline for Colonoscopic Polypectomy
- Suck-Ho Lee, Sung Jae Shin, Dong Il Park, Seong-Eun Kim, Hae Jeong Jeon, Se Hyung Kim, Sung Pil Hong, Sung Noh Hong, Dong-Hoon Yang, Bo In Lee, Young-Ho Kim, Hyun-Soo Kim, Hyun Jung Kim, Suk-Kyun Yang, Hyo Jong Kim, Multi-Society Task Force for Development of Guidelines for Colorectal Polyp Screening, Surveillance and Management
- Clin Endosc 2012;45(1):11-24. Published online March 31, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.1.11
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub There is indirect evidence to suggest that 80% of colorectal cancers (CRC) develop from adenomatous polyps and that, on average, it takes 10 years for a small polyp to transform into invasive CRC. In multiple cohort studies, colonoscopic polypectomy has been shown to significantly reduce the expected incidence of CRC by 76% to 90%. Colonoscopic polypectomy is performed frequently in primary outpatient clinics and secondary and tertiary medical centers in Korea. However, there are no evidence-based, procedural guidelines for the appropriate performance of this procedure, including the technical aspects. For the guideline presented here, PubMed, Medline, and Cochrane Library literature searches were performed. When little or no data from well-designed prospective trials were available, an emphasis was placed on the results from large series and reports from recognized experts. Thus, these guidelines for colonoscopic polypectomy are based on a critical review of the available data as well as expert consensus. Further controlled clinical studies are needed to clarify aspects of this statement, and revision may be necessary as new data become available. This guideline is intended to be an educational device to provide information that may assist endoscopists in providing care to patients. This guideline is not a rule and should not be construed as a legal standard of care or as encouraging, advocating, requiring, or discouraging any particular treatment. Clinical decisions for any particular case involve a complex analysis of the patient's condition and the available courses of action.
-
Citations
Citations to this article as recorded by- Modified underwater endoscopic mucosal resection for intermediate-sized sessile colorectal polyps
Dong Hyun Kim, Seon-Young Park, Hye-Su You, Yong-Wook Jung, Young-Eun Joo, Dae-Seong Myung, Hyun-Soo Kim, Nah Ihm Kim, Seong-Jung Kim, Jae Kyun Ju
Frontiers in Medicine.2023;[Epub] CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef - Circumferential submucosal incision prior to endoscopic mucosal resection versus conventional endoscopic mucosal resection for colorectal lesions with endoscopic features of sessile serrated lesions
Chang Kyo Oh, Bo-In Lee, Sung Hak Lee, Seung-Jun Kim, Han Hee Lee, Chul-Hyun Lim, Jin Su Kim, Yu Kyung Cho, Jae Myung Park, Young-Seok Cho, In Seok Lee, Myung-Gyu Choi
Surgical Endoscopy.2022; 36(3): 2087. CrossRef - Polypectomy for Diminutive and Small Colorectal Polyps
Melissa Zarandi-Nowroozi, Roupen Djinbachian, Daniel von Renteln
Gastrointestinal Endoscopy Clinics of North America.2022; 32(2): 241. CrossRef - Risk of post-polypectomy bleeding after endoscopic mucosal resection in patients receiving antiplatelet medication: comparison between the continue and hold groups
Sang Hyun Park, Soo-Kyung Park, Hyo-Joon Yang, Yoon Suk Jung, Jung Ho Park, Chong Il Sohn, Dong Il Park
Surgical Endoscopy.2022; 36(9): 6410. CrossRef - Hot snare polypectomy versus endoscopic mucosal resection for small colorectal polyps: a randomized controlled trial
Seung-Jun Kim, Bo-In Lee, Eun Sun Jung, Joon Sung Kim, Sun-Young Jun, Woohyeon Kim, Hyoju Ham, Minah Kim, Sung Hak Lee, Han Hee Lee, Jae Myung Park, Myung-Gyu Choi
Surgical Endoscopy.2021; 35(9): 5096. CrossRef - Gastrointestinal and Nongastrointestinal Complications of Esophagogastroduodenoscopy and Colonoscopy in the Real World: A Nationwide Standard Cohort Using the Common Data Model Database
Ha Il Kim, Jin Young Yoon, Min Seob Kwak, Jae Myung Cha
Gut and Liver.2021; 15(4): 569. CrossRef - Clinical Practice Guideline for the Management of Antithrombotic Agents in Patients Undergoing Gastrointestinal Endoscopy
Hyun Lim, Eun Jeong Gong, Byung-Hoon Min, Seung Joo Kang, Cheol Min Shin, Jeong-Sik Byeon, Miyoung Choi, Chan Guk Park, Joo Young Cho, Soo Teik Lee, Ho Gak Kim, Hoon Jai Chun
The Korean Journal of Gastroenterology.2020; 76(6): 282. CrossRef - Endoscopic Submucosal Dissection for Colitis-Associated Dysplasia
Dong-Hoon Yang, Imelda Rey
Clinical Endoscopy.2019; 52(2): 120. CrossRef - Prospective analysis of delayed colorectal post-polypectomy bleeding
Soo-Kyung Park, Jeong Yeon Seo, Min-Gu Lee, Hyo-Joon Yang, Yoon Suk Jung, Kyu Yong Choi, Hungdai Kim, Hyung Ook Kim, Kyung Uk Jung, Ho-Kyung Chun, Dong Il Park
Surgical Endoscopy.2018; 32(7): 3282. CrossRef - Endoscopic Instruments and Electrosurgical Unit for Colonoscopic Polypectomy
Hong Jun Park
Clinical Endoscopy.2016; 49(4): 350. CrossRef - Effectiveness of adjuvant radiotherapy after local excision of rectal cancer with deep submucosal invasion: a single-hospital, case–control analysis
Seohyun Lee, Chang Gok Woo, Hyo Jeong Lee, Kyung-Jo Kim, Byong Duk Ye, Jeong-Sik Byeon, Seung-Jae Myung, Suk-Kyun Yang, Young Soo Park, Jin-hong Park, Jong Hoon Kim, Seok-Byung Lim, Jin Cheon Kim, Chang Sik Yu, Dong-Hoon Yang
Surgical Endoscopy.2015; 29(11): 3231. CrossRef - The Feasibility of Performing Colorectal Endoscopic Submucosal Dissection Without Previous Experience in Performing Gastric Endoscopic Submucosal Dissection
Dong-Hoon Yang, Gwi Hong Jeong, Yerim Song, Sang Hyoung Park, Soo-Kyung Park, Jong Wook Kim, Kee Wook Jung, Kyung-Jo Kim, Byong Duk Ye, Seung-Jae Myung, Suk-Kyun Yang, Jin-Ho Kim, Young Soo Park, Jeong-Sik Byeon
Digestive Diseases and Sciences.2015; 60(11): 3431. CrossRef - Association between the Position of Colorectal Polyps and Clinical Outcomes of Polypectomy: Focused on Procedure Time, Complication and Histopatholgic Result
Jung Hyun Park, Jae Hyeok Choi, Hyeong Jung Na, Won Geon Kwak, Jong Sun Choi, Eo Jin Kim, Jae Hak Kim
Intestinal Research.2013; 11(3): 191. CrossRef - Preparation and Patient Evaluation for Safe Gastrointestinal Endoscopy
Seong Hee Kang, Jong Jin Hyun
Clinical Endoscopy.2013; 46(3): 212. CrossRef - International Digestive Endoscopy Network to Strengthen Network for Lower Gastrointestinal Diseases Including Inflammatory Bowel Disease and Colorectal Cancer
Kwang An Kwon
Clinical Endoscopy.2012; 45(3): 251. CrossRef
- Modified underwater endoscopic mucosal resection for intermediate-sized sessile colorectal polyps
- 10,371 View
- 137 Download
- 16 Crossref

- A Case of Postpolypectomy Coagulation Syndrome Had a Hemicolectomy
- Song Yi Song, M.D., Young Kyung Sung, M.D., Hye Jeong Kim, M.D., Soyoung Bae, M.D., Silvia Park, M.D., Yong Beom Cho, M.D.*, Jin Yong Kim, M.D. and Seung Min Chung, M.D.
- Korean J Gastrointest Endosc 2010;41(4):236-239. Published online October 30, 2010
-
 Abstract
Abstract
 PDF
PDF - Colonoscopy is commonly used as a screening tool for colorectal polyps and cancer. It also offers a chance to remove polyps via the polypectomy technique. Colonoscopic polypectomy is a relatively safe procedure, yet there is the possibility of serious complications such as perforation and bleeding. Postpolypectomy coagulation syndrome presents with pain, fever, an elevated white blood cell count and signs of peritoneal irritation, and usually within 12 hours of the procedure. No free air is seen on plain films or a CT scan, which is different from frank bowel perforation. The management of postpolypectomy coagulation syndrome includes fasting, antibiotics and intravenous hydration. We report here on a case of a 53-year-old woman who underwent right hemicolectomy because she presented with fever, signs of peritoneal irritation and shock after colonoscopic polypectomy. The final diagnosis was postpolypectomy coagulation syndrome as there was no perforation in the resected specimen. (Korean J Gastrointest Endosc 2010;41:236-239)
- 2,520 View
- 23 Download

- Partial Duodenal Obstruction Caused by an Impacted Gastritis Cystica Polyposa
- Ju Hwan Kim, M.D., Chang Il Kwon, M.D., Seung Won Koo, M.D., Kwang Ho Yoo, M.D., Gwang Il Kim, M.D.*, So Young Chong, M.D., Kwang Hyun Ko, M.D. and Sung Pyo Hong, M.D.
- Korean J Gastrointest Endosc 2010;41(4):228-231. Published online October 30, 2010
-
 Abstract
Abstract
 PDF
PDF - Gastritis cystica polyposa is an uncommon lesion that usually occurs at the gastroenterostomy site, but it may also develop in the non-operated stomach. This malady is characterized by polypoid mucosal changes with hyperplasia and cystic dilatation of glands that infiltrate into the submucosal layer. We report here on a case of gastritis cystica polyposa that presented as a mass impacted in the duodenum in a 63-year-old male, and this patient had been admitted for evaluation of progressive epigastric fullness and dyspepsia. Esophagogastroduodenoscopy revealed that the partial duodenal obstruction was caused by impaction of a huge polypoid mass with a stalk that originated from the lower body of the stomach. We fished out the impacted mass with a forceps catheter while holding the neck with a snare catheter. Thereafter, an endoloop was applied to the stalk of mass, and this was followed by polypectomy using a snare catheter. (Korean J Gastrointest Endosc 2010;41:228-231)
- 2,102 View
- 5 Download

- A Case of Colonic Intussusception Occurring after Colonoscopic Polypectomy
- Sa Il Kim, M.D., Yong Cheol Jeon, M.D., Gil Woo Lee, M.D., Young Taek Kim, M.D., Tae Yeob Kim, M.D., Chang Soo Eun, M.D., Dong Soo Han, M.D. and Joo Hyun Sohn, M.D.
- Korean J Gastrointest Endosc 2010;41(3):172-175. Published online September 30, 2010
-
 Abstract
Abstract
 PDF
PDF - Intestinal intussusception in adults is a rare disease. Most of the cases of adult intussusception are secondary to a definable lesion, and so surgical treatment generally needed. Intussusception that occurs after colonoscopic polypectomy is apparently a rare malady. A 77-year old man undergoing colonoscopic polypectomy was diagnosed as having colonic intussusception at the hepatic flexure. As there was no clinical improvement with conservative treatment, he underwent segmental resection of the ascending and transverse colon. Pathologic examination revealed that the colonoscopic polypectomy site was a leading point of the intussusception. (Korean J Gastrointest Endosc 2010;41:172-175)
- 2,277 View
- 18 Download

- A Case of Hamartomatous Polyp without Peutz-Jeghers Syndrome Arising from Appendix
- Wee Sik Sohn, M.D., Ju Sang Park, M.D., Ji Eun Kim, M.D., Bong Hwan Kim, M.D., Seung Hee Yoo, M.D. and Eun Mee Han, M.D.*
- Korean J Gastrointest Endosc 2010;41(1):36-40. Published online July 31, 2010
-
 Abstract
Abstract
 PDF
PDF - Peutz-Jeghers syndrome is a familial syndrome consisting of mucocutaneous pigmentation and gastrointestinal polyposis and appears to be inherited as a single pleiotropic autosomal dominant gene with variable and incomplete penetrance. Cases of hamartomatous polyps of the Peutz-Jeghers type without Peutz-Jeghers syndrome have only rarely been reported. Moreover, only one case of a Peutz-Jeghers polyp at the appendix has been reported; it was resected by appendectomy. We report here on a case of a 45 year old man who had a hamartomatous polyp of the Peutz-Jeghers type arising from the appendix. The polyp was successfully removed by endoscopic polypectomy. To our knowledge, this is the first case of a hamartomatous polyp of the Peutz-Jeghers type that originated from the appendix and that was resected endoscopically. (Korean J Gastrointest Endosc 2010;41:36-40)
- 2,088 View
- 15 Download

- Risk Factors for Delayed Bleeding after Colonoscopic Polypectomy
- Woo Jin Han, M.D., Yoon Jae Kim, M.D., Jung Gon Kim, M.D., Tae Kyung Kim, M.D., Seo Young Lee, M.D., Moon Sook Cho, M.D., Jun Won Chung, M.D., Dong Kyun Park, M.D., Ki Baik Hahm, M.D., Yun Soo Kim, M.D. and Ju Hyun Kim, M.D.
- Korean J Gastrointest Endosc 2010;40(3):164-169. Published online March 30, 2010
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: The aim of this study was to identify risk factors for delayed bleeding after colonoscopic polypectomy.
Methods
3,530 polypectomies in 1,542 patients were evaluated. Risk factors were identified among patient-related factors (age, sex, comorbidity, anticoagulants, antiplatelets), polyp-related factors (size, shape, location, histology), and procedure-related factors (experience of the endoscopist, sedation, resection method).
Results
Delayed bleeding occurred in 26 lesions (0.7%) of 24 patients (1.6%). Polyp-based multivariate analysis revealed that polyp size greater than 15 mm (OR, 2.882; 95% CI, 1.106 to 7.506; p=0.030) and sedation-free colonoscopy (OR, 2.606; 95% CI, 1.116 to 6.084; p=0.027) were significant risk factors for delayed bleeding after polypectomy. In colonoscopy-based analysis, hypertension increased the risk of delayed bleeding after polypectomy (OR, 2.938; 95% CI, 1.009 to 8.557; p=0.048).
Conclusions
Large polyp size, sedation-free colonoscopy, and hypertension are associated with delayed bleeding after colonoscopic polypectomy. (Korean J Gastrointest Endosc 2010;40:164-169)
- 2,368 View
- 11 Download

- Endoscopic Polypectomy of Small Intestinal Peutz-Jeghers Polyps with Double Balloon Enteroscopy
- Mi-Young Kim, M.D., Jeong-Sik Byeon, M.D., Kee Don Choi, M.D., Byong Duk Ye, M.D., Dong-Hoon Yang, M.D., Soon Man Yoon, M.D., Kyung-Jo Kim, M.D., Seung-Jae Myung, M.D., Suk-Kyun Yang, M.D. and Jin-Ho Kim, M.D.
- Korean J Gastrointest Endosc 2009;39(6):338-345. Published online December 30, 2009
-
 Abstract
Abstract
 PDF
PDF - Background
/Aims: Small intestinal polyps in patients with Peutz-Jeghers (PJ) syndrome cause therapeutic difficulties because of the necessity for repeated laparotomy. We evaluated the short-term outcomes and long-term usefulness of double balloon enteroscopy (DBE) polypectomy for treating small intestinal PJ polyps.
Methods
We retrospectively reviewed 10 patients with PJ syndrome (M:F=7:3, mean age 22.7 years) and whose small intestinal polyps were resected with DBE between January 2005 and July 2008. We analyzed their clinical, endoscopic and pathologic features, the short-term outcomes and the long-term follow-up results.
Results
Among 10 patients, 2 complained hematochezia and 2 presented with intussusceptions. DBE polypectomy was performed by the oral route in 4 patients, by the anal route in 1 and by both routes in 5 without significant complications, except for only one perforation. The polyps were 0.5∼6 cm in size and most of them were pedunculated. The histopathology revealed hamartomatous polyps in most cases. Follow-up small bowel series was performed in 6 of 10 patients, and 3 showed remnant polyps. Two of them underwent repeated DBE polypectomy without significant complications.
Conclusions
We suggest that DBE polypectomy is a useful treatment for PJ small intestinal polyps because of the good short-term outcome and the effectiveness of repeated polypectomy for the remnant or recurrent polyps. (Korean J Gastrointest Endosc 2009;39:338-345)
- 2,174 View
- 8 Download

- Endoscopic Polypectomy of Primary Rectal Mature Teratoma: A Case Report
- Jongha Park, M.D., Jeong-Sik Byeon, M.D., Jeong-Hyeon Jo, M.D.*, Kyung-Jo Kim, M.D., Byong Duk Ye, M.D., Seung-Jae Myung, M.D., Suk-Kyun Yang, M.D. and Jin-Ho Kim, M.D.
- Korean J Gastrointest Endosc 2009;39(5):308-312. Published online November 30, 2009
-
 Abstract
Abstract
 PDF
PDF - Teratoma is a type of benign germ cell tumor that often contains several different types of tissue such as hair, muscle and bone, and these tissues arise from the three germinal layers. It occurs most often in the tailbones of children, the ovaries of women and the testicles of men. Primary rectal teratoma is extremely rare. We report here on a case of a 49-year-old woman with a primary rectal teratoma, and this was incidentally found during routine health screening. The rectal teratoma was a 15 mm-sized pedunculated polyp with a short stalk at the rectum, about 15 cm from anal verge as seen on CT colonography. On sigmoidoscopy and EUS, a fat and calcium containing well-defined polypoid lesion was noted in the upper rectum, with a narrow stalk attached to the colonic wall. The tumor was successfully excised by endoscopic polypectomy in order to obtain the histologic diagnosis and administer the proper treatment. (Korean J Gastrointest Endosc 2009;39:308-312)
- 1,963 View
- 18 Download

- Rectal Leiomyoma Diagnosed by Endoscopic Ultrasonography and Endoscopic Polypectomy
- Sung Whan Cho, M.D., Hyung Yook Kim, M.D.* and Ung Suk Yang, M.D.
- Korean J Gastrointest Endosc 2009;38(3):151-155. Published online March 30, 2009
-
 Abstract
Abstract
 PDF
PDF - Leiomyoma of the rectum is a rare tumor and it usually present in 40 to 60 year-old individuals, and it is more frequent in men. It originates from either the muscularis mucosa or muscularis externa and those arising from the muscularis mucosa are typically small and they are identified incidentally in patients who are undergoing sigmoidoscopy. In contrast, the larger leiomyomas arising from the muscularis externa generally present symptoms that are consistent with rectal stenosis or a rectal mass. Endoscopic ultrasonography can help to define the tumor location, extension and size. Surgical resection is the treatment for most leiomyomas of the rectum, but endoscopic electroexcision is a safe and appropriate treatment for small polypoid rectal leiomyoma. We report here on a case of a semipedunculated rectal leiomyoma in a 59 year-old female patient. It was found incidentally during a colonoscopic examination and it was diagnosed by endoscopic ultrasonography. We performed endoscopic mucosal resection with colonoscopic snare electrocoagulation. (Korean J Gastrointest Endosc 2009;38:151-155)
- 2,560 View
- 16 Download

- A Case of Delayed Massive Hemorrhage after Endoscopic Resecting a Rectal Carcinoid Tumor
- So Mi Kim, M.D., Se Young Yun, M.D., Hoon Choi, M.D., Jae Huan Kong, M.D. and Sung Soo La, M.D.
- Korean J Gastrointest Endosc 2009;38(2):111-115. Published online February 27, 2009
-
 Abstract
Abstract
 PDF
PDF - Endoscopic resection is currently accepted as a standard therapy for colon polyp because of its safety and efficiency. The indications for endoscopic resection have been expanded to treat mucosal colon cancer and submucosal tumor. The major complications of endoscopic resection are hemorrhage, perforation and post- polypectomy coagulation syndrome. Hemorrhage is the most common complication, and this can occur immediately following colonoscopic polypectomy or it can be delayed after completion of the procedure. Delayed hemorrhage usually occurs within 7 days and this can stop by itself or the hemorrhage can be controlled endoscopically in the majority of patients, with only the unusual and serious cases requiring transfusion, angiography and surgery. We experienced a case of delayed massive hemorrhage with hypotension that required transfusion 12 days after performing endoscopic resection for rectal carcinoid tumor. We report here on this case to provide a good example and to place emphasis on delayed massive hemorrhage after endoscopic resection. (Korean J Gastrointest Endosc 2009;38: 111-115)
- 2,450 View
- 5 Download


 KSGE
KSGE

 First
First Prev
Prev