Search
- Page Path
- HOME > Search
Review
- Surveillance for metachronous cancers after endoscopic resection of esophageal squamous cell carcinoma
- Ryu Ishihara
- Received October 10, 2023 Accepted December 17, 2023 Published online May 10, 2024
- DOI: https://doi.org/10.5946/ce.2023.263 [Epub ahead of print]

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
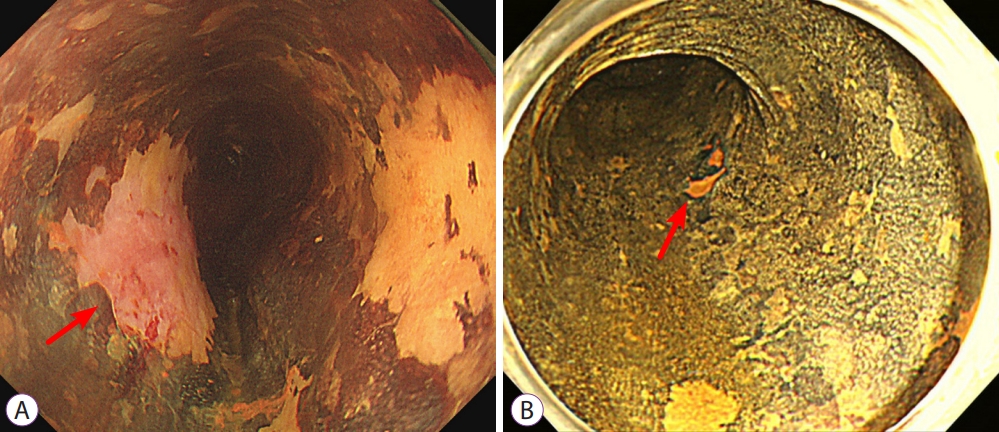
ePub - The literature pertaining to surveillance following treatment for esophageal squamous cell carcinoma (SCC) was reviewed and summarized, encompassing the current status and future perspectives. Analysis of the standardized mortality and incidence ratios for these cancers indicates an elevated risk of cancer in the oral cavity, pharynx, larynx, and lungs among patients with esophageal SCC compared to the general population. To enhance the efficacy of surveillance for these metachronous cancers, risk stratification is needed. Various factors, including multiple Lugol-voiding lesions, multiple foci of dilated vascular areas, young age, and high mean corpuscular volume, have been identified as predictors of metachronous SCCs. Current practice involves stratifying the risk of metachronous esophageal and head/neck SCCs based on the presence of multiple Lugol-voiding lesions. Endoscopic surveillance, scheduled 6–12 months post-endoscopic resection, has demonstrated effectiveness, with over 90% of metachronous esophageal SCCs treatable through minimally invasive modalities. Narrow-band imaging emerges as the preferred surveillance method for esophageal and head/neck SCC based on comparative studies of various imaging techniques. Innovative approaches, such as artificial intelligence-assisted detection systems and radiofrequency ablation of high-risk background mucosa, may improve outcomes in patients following endoscopic resection.
- 1,542 View
- 36 Download

Original Articles
- Clinicopathological and endoscopic features of Helicobacter pylori infection-negative gastric cancer in Japan: a retrospective study
- Kentaro Imamura, Kenshi Yao, Satoshi Nimura, Takao Kanemitsu, Masaki Miyaoka, Yoichiro Ono, Toshiharu Ueki, Hiroshi Tanabe
- Received October 7, 2023 Accepted November 25, 2023 Published online March 22, 2024
- DOI: https://doi.org/10.5946/ce.2023.258 [Epub ahead of print]

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
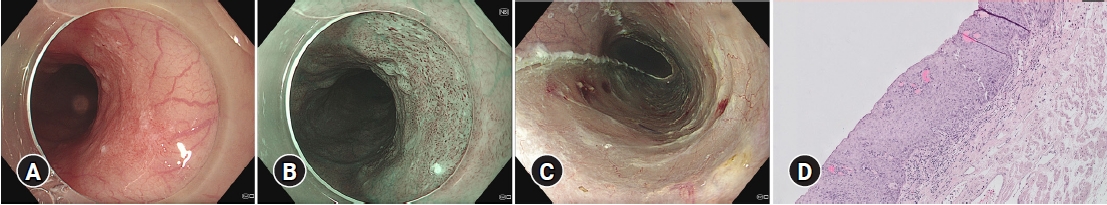
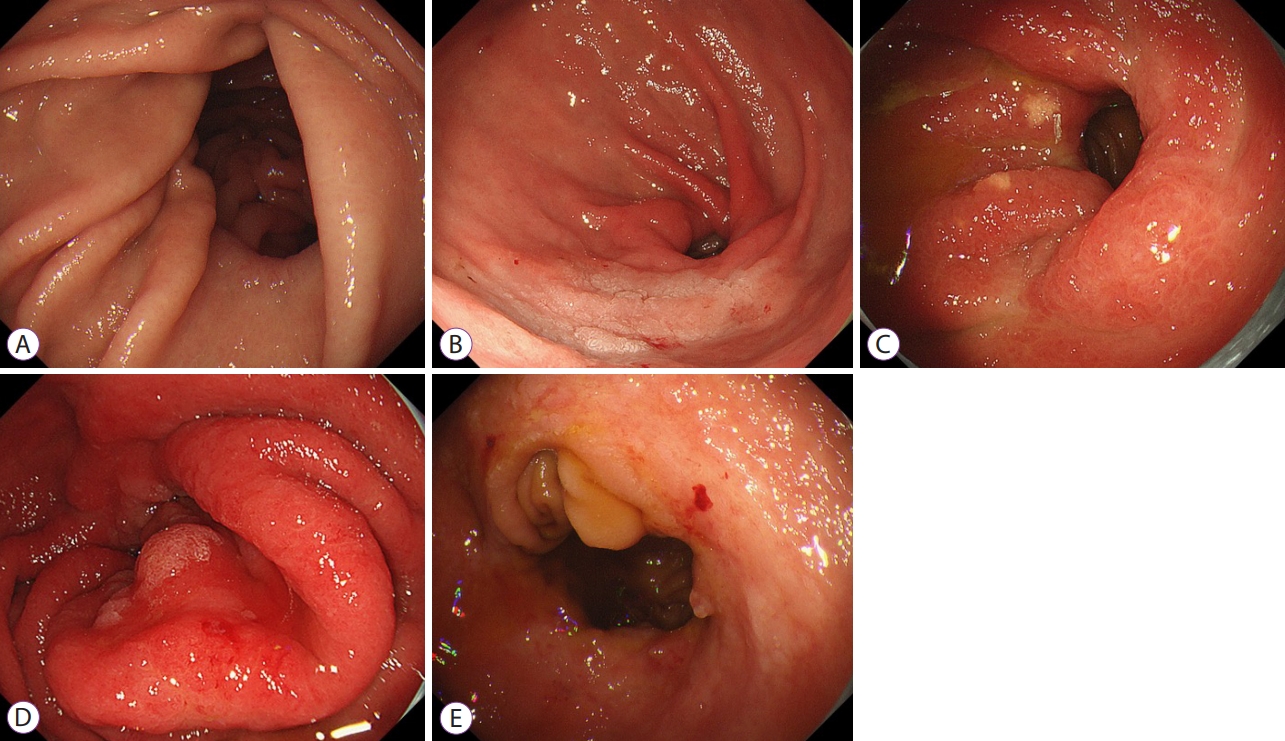
- Background
/Aims: Helicobacter pylori infection-negative gastric cancer (HPNGC) has not been systematically investigated in consecutive patients. Hence, this study aimed to investigate the clinicopathological and endoscopic features of HPNGC.
Methods
This single-center retrospective study selected participants from patients with gastric cancer who were treated at the Fukuoka University Chikushi Hospital between January 2013 and December 2021. Only patients diagnosed with HPNGC were enrolled, and their clinicopathological and endoscopic features were analyzed in detail.
Results
The prevalence of HPNGC in the present study was 2.6% (54/2112). The types of HPNGC observed in each gastric region were as follows: advanced gastric cancer was observed in the cardia; gastric adenocarcinoma of fundic-gland differentiation, gastric adenocarcinoma of foveolar-type presenting with whitish elevation and raspberry-like foveolar-type gastric adenocarcinoma, gastric adenocarcinoma arising in polyposis, and gastric adenocarcinoma with autoimmune gastritis were observed in the fundic gland region ranging from the gastric fornix to the gastric body; signet-ring cell carcinoma was observed in the gastric-pyloric transition region ranging from the lower gastric body to the gastric angle; and well-differentiated tubular adenocarcinoma with low-grade atypia was observed in the antrum.
Conclusions
This study revealed that tumors from each gastric region exhibited distinct macroscopic and histological types in HPNGC.
- 2,556 View
- 74 Download

- Clinical utility of endoscopic ultrasound-guided tissue acquisition for comprehensive genomic profiling of patients with biliary tract cancer, especially with intrahepatic cholangiocarcinoma
- Takafumi Yanaidani, Kazuo Hara, Nozomi Okuno, Shin Haba, Takamichi Kuwahara, Yasuhiro Kuraishi, Nobumasa Mizuno, Sho Ishikawa, Masanori Yamada, Tsukasa Yasuda
- Clin Endosc 2024;57(3):384-392. Published online February 15, 2024
- DOI: https://doi.org/10.5946/ce.2023.139

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: Endoscopic ultrasound-guided tissue acquisition (EUS-TA) is a standard diagnostic method for biliary tract cancer (BTC), and samples obtained in this manner may be used for comprehensive genomic profiling (CGP). This study evaluated the utility of EUS-TA for CGP in a clinical setting and determined the factors associated with the adequacy of CGP in patients with BTC.
Methods
CGP was attempted for 105 samples from 94 patients with BTC at the Aichi Cancer Center, Japan, from October 2019 to April 2022.
Results
Overall, 77.1% (81/105) of the samples were adequate for CGP. For 22-G or 19-G fine-needle biopsy (FNB), the sample adequacy was 85.7% (36/42), which was similar to that of surgical specimens (94%, p=0.45). Univariate analysis revealed that 22-G or larger FNB needle usage (86%, p=0.003), the target primary lesions (88%, p=0.015), a target size ≥30 mm (100%, p=0.0013), and number of punctures (90%, p=0.016) were significantly positively associated with CGP sample adequacy.
Conclusions
EUS-TA is useful for CGP tissue sampling in patients with BTC. In particular, the use of 22-G or larger FNB needles may allow for specimen adequacy comparable to that of surgical specimens. -
Citations
Citations to this article as recorded by- Is genomic analysis possible in a tissue acquired via endoscopic ultrasound-guided fine-needle biopsy in cholangiocarcinoma?
Jonghyun Lee, Sung Yong Han
Clinical Endoscopy.2024; 57(3): 332. CrossRef
- Is genomic analysis possible in a tissue acquired via endoscopic ultrasound-guided fine-needle biopsy in cholangiocarcinoma?
- 1,855 View
- 27 Download
- 1 Web of Science
- 1 Crossref

Reviews
- Role of contrast-enhanced harmonic endoscopic ultrasonography (EUS) and EUS elastography in pancreatic lesions
- Yasunobu Yamashita, Masayuki Kitano
- Clin Endosc 2024;57(2):164-174. Published online January 17, 2024
- DOI: https://doi.org/10.5946/ce.2023.074

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Pancreatic cancers have a poor prognosis, and their incident rates have risen. Endoscopic ultrasonography (EUS) is an efficient and reliable diagnostic modality for pancreatic lesions, providing high spatial resolution. However, while EUS helps to detect minor pancreatic lesions, nearly all solid pancreatic lesions are hypoechoic, which creates difficulty in making differential diagnoses of pancreatic lesions. When diagnosing pancreatic lesions, the performance of image-enhanced EUS techniques is essential, such as EUS elastography or contrast-enhanced harmonic EUS (CH-EUS). CH-EUS diagnosis is based on assessing the vascularity of lesions, whereas tissue elasticity is measured via EUS elastography. Elastography is either strain or shear-wave, depending on the different mechanical properties being evaluated. The usefulness of enhanced EUS techniques is demonstrated in this review for the differential diagnosis of pancreatic lesions, including solid and cystic lesions, and pancreatic cancer staging.
-
Citations
Citations to this article as recorded by- Endoscopic Contrast-Enhanced Ultrasound and Fine-Needle Aspiration or Biopsy for the Diagnosis of Pancreatic Solid Lesions: A Systematic Review and Meta-Analysis
Giorgio Esposto, Giuseppe Massimiani, Linda Galasso, Paolo Santini, Raffaele Borriello, Irene Mignini, Maria Elena Ainora, Alberto Nicoletti, Lorenzo Zileri Dal Verme, Antonio Gasbarrini, Sergio Alfieri, Giuseppe Quero, Maria Assunta Zocco
Cancers.2024; 16(9): 1658. CrossRef
- Endoscopic Contrast-Enhanced Ultrasound and Fine-Needle Aspiration or Biopsy for the Diagnosis of Pancreatic Solid Lesions: A Systematic Review and Meta-Analysis
- 2,990 View
- 205 Download
- 1 Web of Science
- 1 Crossref

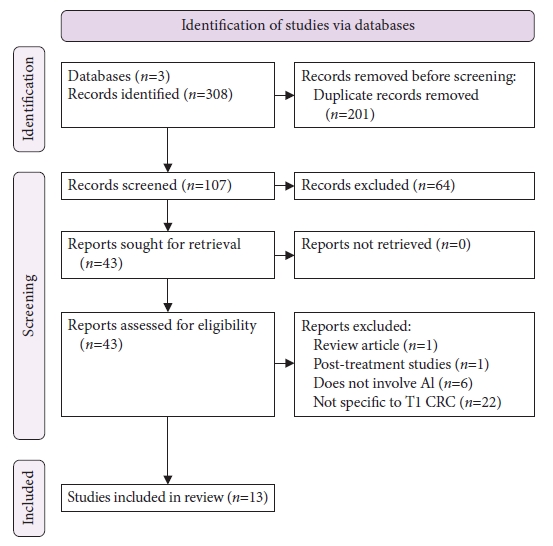
- Use of artificial intelligence in the management of T1 colorectal cancer: a new tool in the arsenal or is deep learning out of its depth?
- James Weiquan Li, Lai Mun Wang, Katsuro Ichimasa, Kenneth Weicong Lin, James Chi-Yong Ngu, Tiing Leong Ang
- Clin Endosc 2024;57(1):24-35. Published online September 25, 2023
- DOI: https://doi.org/10.5946/ce.2023.036
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The field of artificial intelligence is rapidly evolving, and there has been an interest in its use to predict the risk of lymph node metastasis in T1 colorectal cancer. Accurately predicting lymph node invasion may result in fewer patients undergoing unnecessary surgeries; conversely, inadequate assessments will result in suboptimal oncological outcomes. This narrative review aims to summarize the current literature on deep learning for predicting the probability of lymph node metastasis in T1 colorectal cancer, highlighting areas of potential application and barriers that may limit its generalizability and clinical utility.
-
Citations
Citations to this article as recorded by- Prediction of Lymph Node Metastasis in T1 Colorectal Cancer Using Artificial Intelligence with Hematoxylin and Eosin-Stained Whole-Slide-Images of Endoscopic and Surgical Resection Specimens
Joo Hye Song, Eun Ran Kim, Yiyu Hong, Insuk Sohn, Soomin Ahn, Seok-Hyung Kim, Kee-Taek Jang
Cancers.2024; 16(10): 1900. CrossRef
- Prediction of Lymph Node Metastasis in T1 Colorectal Cancer Using Artificial Intelligence with Hematoxylin and Eosin-Stained Whole-Slide-Images of Endoscopic and Surgical Resection Specimens
- 2,382 View
- 262 Download
- 2 Web of Science
- 1 Crossref

- E-learning system to improve the endoscopic diagnosis of early gastric cancer
- Kenshi Yao, Takashi Yao, Noriya Uedo, Hisashi Doyama, Hideki Ishikawa, Satoshi Nimura, Yuichi Takahashi
- Clin Endosc 2024;57(3):283-292. Published online August 3, 2023
- DOI: https://doi.org/10.5946/ce.2023.087

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - We developed three e-learning systems for endoscopists to acquire the necessary skills to improve the diagnosis of early gastric cancer (EGC) and demonstrated their usefulness using randomized controlled trials. The subjects of the three e-learning systems were “detection”, “characterization”, and “preoperative assessment”. The contents of each e-learning system included “technique”, “knowledge”, and “obtaining experience”. All e-learning systems proved useful for endoscopists to learn how to diagnose EGC. Lecture videos describing “the technique” and “the knowledge” can be beneficial. In addition, repeating 100 self-study cases allows learners to gain “experience” and improve their diagnostic skills further. Web-based e-learning systems have more advantages than other teaching methods because the number of participants is unlimited. Histopathological diagnosis is the gold standard for the diagnosis of gastric cancer. Therefore, we developed a comprehensive diagnostic algorithm to standardize the histopathological diagnosis of gastric cancer. Once we have successfully shown that this algorithm is helpful for the accurate histopathological diagnosis of cancer, we will complete a series of e-learning systems designed to assess EGC accurately.
-
Citations
Citations to this article as recorded by- Pitfalls in Endoscopic Submucosal Dissection for Early Gastric Cancer with Papillary Adenocarcinoma
Gwang Ha Kim
Gut and Liver.2024; 18(3): 368. CrossRef
- Pitfalls in Endoscopic Submucosal Dissection for Early Gastric Cancer with Papillary Adenocarcinoma
- 2,499 View
- 359 Download
- 1 Web of Science
- 1 Crossref

Original Articles
-
Significance of rescue hybrid endoscopic submucosal dissection in difficult colorectal cases

- Hayato Yamaguchi, Masakatsu Fukuzawa, Takashi Kawai, Takahiro Muramatsu, Taisuke Matsumoto, Kumiko Uchida, Yohei Koyama, Akira Madarame, Takashi Morise, Shin Kono, Sakiko Naito, Naoyoshi Nagata, Mitsushige Sugimoto, Takao Itoi
- Clin Endosc 2023;56(6):778-789. Published online July 26, 2023
- DOI: https://doi.org/10.5946/ce.2022.268

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub 
- Background
/Aims: Hybrid endoscopic submucosal dissection (ESD), in which an incision is made around a lesion and snaring is performed after submucosal dissection, has some advantages in colorectal surgery, including shorter procedure time and preventing perforation. However, its value for rescue resection in difficult colorectal ESD cases remains unclear. This study evaluated the utility of rescue hybrid ESD (RH-ESD).
Methods
We divided 364 colorectal ESD procedures into the conventional ESD group (C-ESD, n=260), scheduled hybrid ESD group (SH-ESD, n=69), and RH-ESD group (n=35) and compared their clinical outcomes.
Results
Resection time was significantly shorter in the following order: RH-ESD (149 [90–197] minutes) >C-ESD (90 [60–140] minutes) >SH-ESD (52 [29–80] minutes). The en bloc resection rate increased significantly in the following order: RH-ESD (48.6%), SH-ESD (78.3%), and C-ESD (97.7%). An analysis of factors related to piecemeal resection of RH-ESD revealed that the submucosal dissection rate was significantly lower in the piecemeal resection group (25% [20%–30%]) than in the en bloc resection group (40% [20%–60%]).
Conclusions
RH-ESD was ineffective in terms of curative resection because of the low en bloc resection rate, but was useful for avoiding surgery. -
Citations
Citations to this article as recorded by- Planned Hybrid Endoscopic Submucosal Dissection as Alternative for Colorectal Neoplasms: A Propensity Score-Matched Study
Yu-xin Zhang, Xun Liu, Fang Gu, Shi-gang Ding
Digestive Diseases and Sciences.2024; 69(3): 949. CrossRef - Understanding hybrid endoscopic submucosal dissection subtleties
João Paulo de Souza Pontual, Alexandre Moraes Bestetti, Diogo Turiani Hourneaux de Moura
Clinical Endoscopy.2023; 56(6): 738. CrossRef
- Planned Hybrid Endoscopic Submucosal Dissection as Alternative for Colorectal Neoplasms: A Propensity Score-Matched Study
- 2,225 View
- 122 Download
- 2 Web of Science
- 2 Crossref

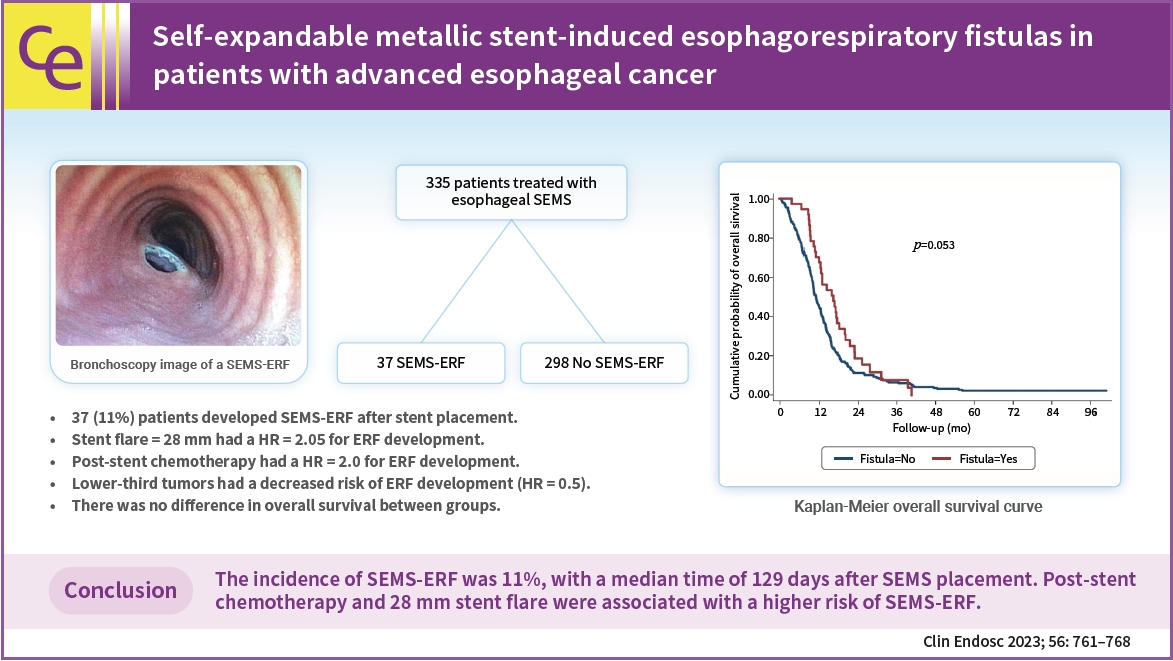
- Self-expandable metallic stent-induced esophagorespiratory fistulas in patients with advanced esophageal cancer
- Iatagan R. Josino, Bruno C. Martins, Andressa A. Machado, Gustavo R. de A. Lima, Martin A. C. Cordero, Amanda A. M. Pombo, Rubens A. A. Sallum, Ulysses Ribeiro Jr, Todd H. Baron, Fauze Maluf-Filho
- Clin Endosc 2023;56(6):761-768. Published online July 25, 2023
- DOI: https://doi.org/10.5946/ce.2022.297
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 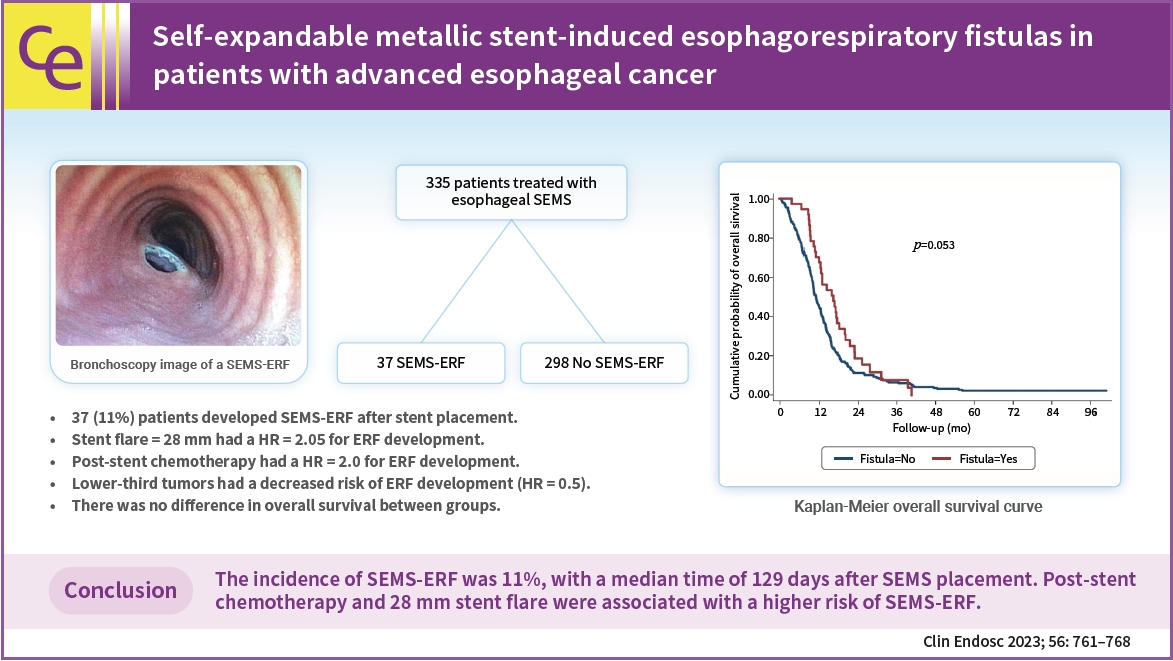
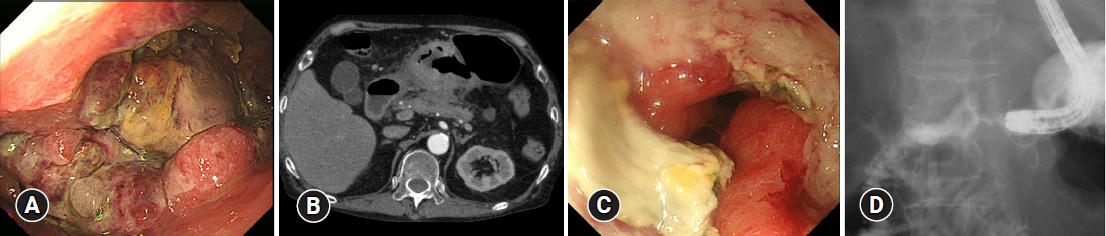
- Background
/Aims: Self-expandable metallic stents (SEMSs) are widely adopted for the palliation of dysphagia in patients with malignant esophageal strictures. An important adverse event is the development of SEMS-induced esophagorespiratory fistulas (SEMS-ERFs). This study aimed to assess the risk factors related to the development of SEMS-ERF after SEMS placement in patients with esophageal cancer.
Methods
This retrospective study was performed at the Instituto do Cancer do Estado de São Paulo. All patients with malignant esophageal strictures who underwent esophageal SEMS placement between 2009 and 2019 were included in the study.
Results
Of the 335 patients, 37 (11.0%) developed SEMS-ERF, with a median time of 129 days after SEMS placement. Stent flare of 28 mm (hazard ratio [HR], 2.05; 95% confidence interval [CI], 1.15–5.51; p=0.02) and post-stent chemotherapy (HR, 2.0; 95% CI, 1.01–4.00; p=0.05) were associated with an increased risk of developing SEMS-ERF, while lower-third tumors were a protective factor (HR, 0.5; 95% CI, 0.26–0.85; p=0.01). No difference was observed in overall survival.
Conclusions
The incidence of SEMS-ERFs was 11%, with a median time of 129 days after SEMS placement. Post-stent chemotherapy and a 28 mm stent flare were associated with a higher risk of SEMS-ERF. -
Citations
Citations to this article as recorded by- How to reduce fistula formation after self-expandable metallic stent insertion for treating malignant esophageal stricture?
Kwang Bum Cho
Clinical Endoscopy.2023; 56(6): 735. CrossRef
- How to reduce fistula formation after self-expandable metallic stent insertion for treating malignant esophageal stricture?
- 2,008 View
- 107 Download
- 1 Web of Science
- 1 Crossref

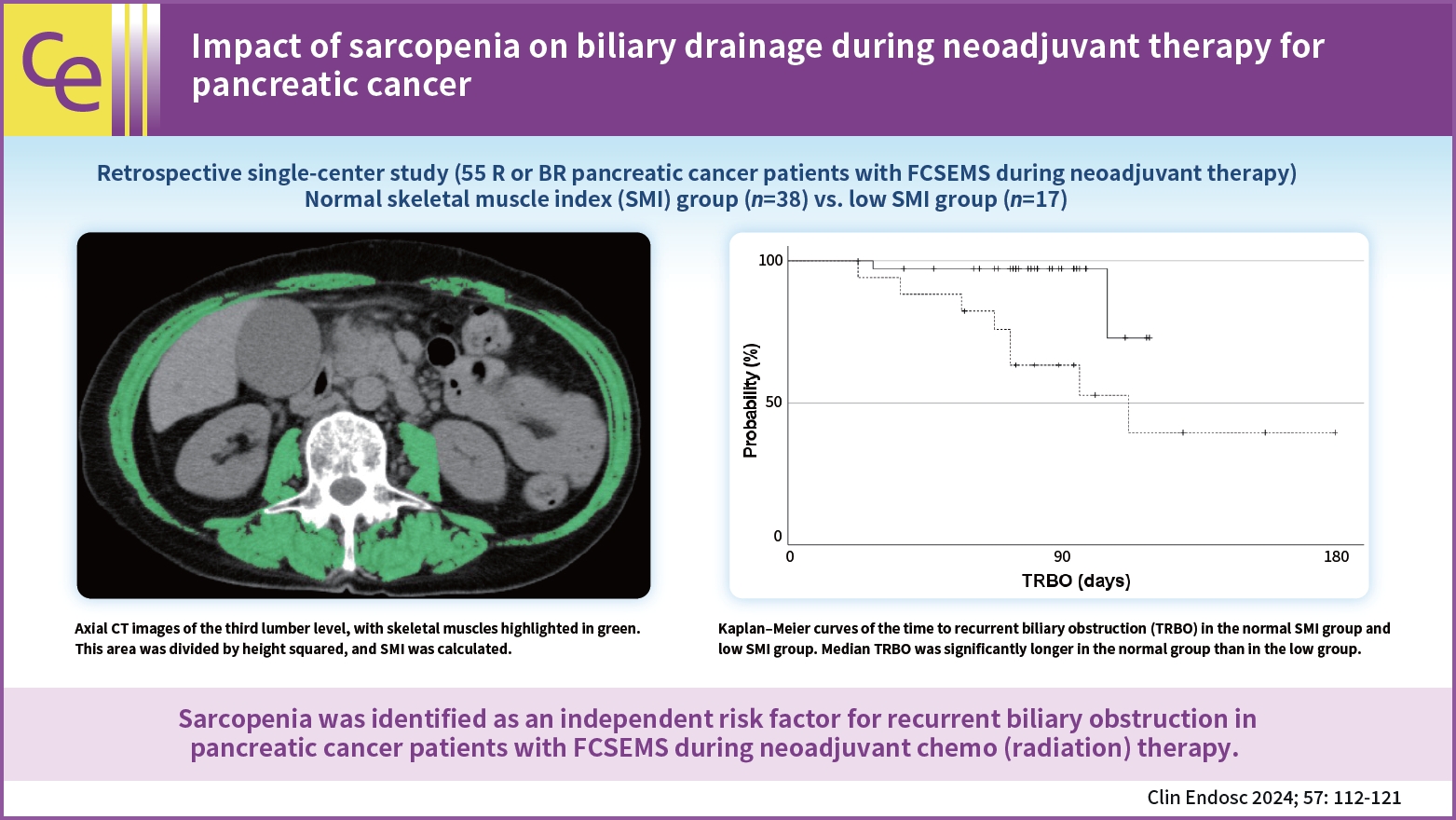
- Impact of sarcopenia on biliary drainage during neoadjuvant therapy for pancreatic cancer
- Kunio Kataoka, Eizaburo Ohno, Takuya Ishikawa, Kentaro Yamao, Yasuyuki Mizutani, Tadashi Iida, Hideki Takami, Osamu Maeda, Junpei Yamaguchi, Yukihiro Yokoyama, Tomoki Ebata, Yasuhiro Kodera, Hiroki Kawashima
- Clin Endosc 2024;57(1):112-121. Published online July 18, 2023
- DOI: https://doi.org/10.5946/ce.2022.278
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 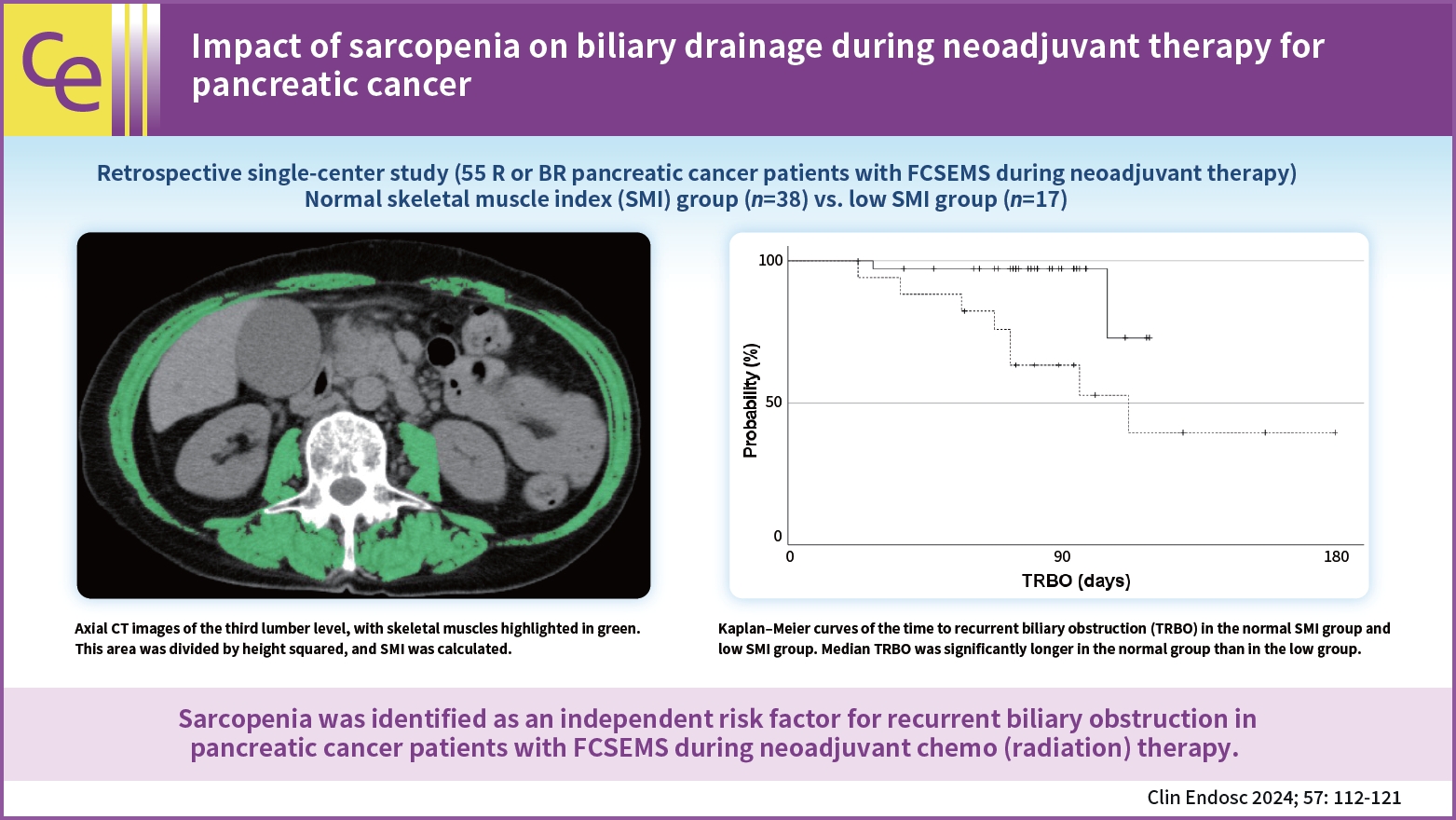
- Background
/Aims: Since the usefulness of neoadjuvant chemo(radiation) therapy (NAT) for pancreatic cancer has been demonstrated, recurrent biliary obstruction (RBO) in patients with pancreatic cancer with a fully covered self-expandable metal stent (FCSEMS) during NAT is expected to increase. This study investigated the impact of sarcopenia on RBO in this setting.
Methods
Patients were divided into normal and low skeletal muscle index (SMI) groups and retrospectively analyzed. Patient characteristics, overall survival, time to RBO (TRBO), stent-related adverse events, and postoperative complications were compared between the two groups. A Cox proportional hazard model was used to identify the risk factors for short TRBO.
Results
A few significant differences were observed in patient characteristics, overall survival, stent-related adverse events, and postoperative complications between 38 patients in the normal SMI group and 17 in the low SMI group. The median TRBO was not reached in the normal SMI group and was 112 days in the low SMI group (p=0.004). In multivariate analysis, low SMI was the only risk factor for short TRBO, with a hazard ratio of 5.707 (95% confidence interval, 1.148–28.381; p=0.033).
Conclusions
Sarcopenia was identified as an independent risk factor for RBO in patients with pancreatic cancer with FCSEMS during NAT. -
Citations
Citations to this article as recorded by- Endeavors to prevent stent malfunction: new insights into the risk factors for recurrent biliary obstruction
Sung-Jo Bang
Clinical Endoscopy.2024; 57(1): 56. CrossRef - Skeletal muscle status and survival among patients with advanced biliary tract cancer
Shinya Takaoka, Tsuyoshi Hamada, Naminatsu Takahara, Kei Saito, Go Endo, Ryunosuke Hakuta, Kota Ishida, Kazunaga Ishigaki, Sachiko Kanai, Kohei Kurihara, Hiroki Oyama, Tomotaka Saito, Tatsuya Sato, Tatsunori Suzuki, Yukari Suzuki, Shuichi Tange, Yurie Tok
International Journal of Clinical Oncology.2024; 29(3): 297. CrossRef
- Endeavors to prevent stent malfunction: new insights into the risk factors for recurrent biliary obstruction
- 2,177 View
- 125 Download
- 2 Web of Science
- 2 Crossref

- Management of esophageal neoplasms by endoscopic submucosal dissection: experience over 100 consecutive procedures
- Josué Aliaga Ramos, Yoshinori Morita, Takashi Toyonaga, Danilo Carvalho, Moises Salgado Pedrosa, Vitor N. Arantes
- Clin Endosc 2023;56(5):613-622. Published online May 17, 2023
- DOI: https://doi.org/10.5946/ce.2022.245

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
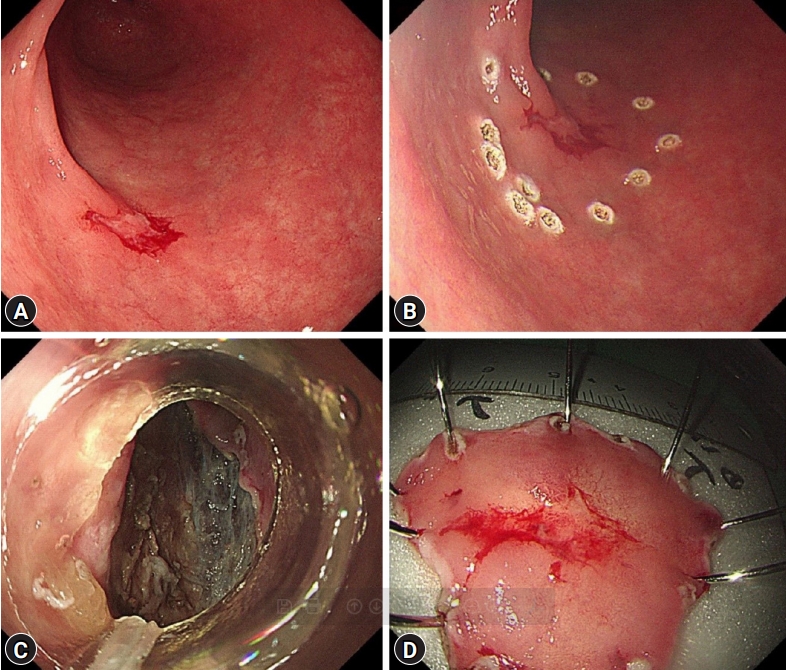
- Background
/Aims: Endoscopic submucosal dissection (ESD) is currently considered the first-line treatment for the eradication of superficial neoplasms of the esophagus in Eastern countries. However, in the West, particularly in Latin America, the experience with esophageal ESD is still limited because of the high technical complexity required for its execution. This study aimed to present the results of the clinical application of ESD to manage superficial esophageal neoplasms in a Latin American center in over 100 consecutive cases.
Methods
This retrospective study included consecutive patients who underwent endoscopic ESD for superficial esophageal neoplasms between 2009 and 2022. The following clinical outcomes were assessed: en bloc, complete, and curative resection rates, local recurrence, adverse events, and procedure-related mortality.
Results
Esophageal ESD was performed mainly for squamous cell carcinoma (66.6%), high-grade intraepithelial neoplasia (17.1%), and adenocarcinoma (11.4%). En bloc and complete resection rates were 96.2% and 81.0%, respectively. The curative resection rate was 64.8%. Adverse events occurred in six cases (5.7%). Endoscopic follow-up was performed for an average period of 29.7 months.
Conclusions
ESD performed by trained operators is feasible, safe, and clinically effective for managing superficial neoplastic lesions of the esophagus in Latin America.
- 1,739 View
- 82 Download

Case Report
- Gastric cancer presenting with ramucirumab-related gastrocolic fistula successfully managed by colonic stenting: a case report
- Hiroki Fukuya, Yoichiro Iboshi, Masafumi Wada, Yorinobu Sumida, Naohiko Harada, Makoto Nakamuta, Hiroyuki Fujii, Eikichi Ihara
- Clin Endosc 2023;56(6):812-816. Published online May 11, 2023
- DOI: https://doi.org/10.5946/ce.2022.117
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - We report a rare case of gastric cancer presenting with a gastrocolic fistula during ramucirumab and paclitaxel combination therapy that was successfully managed with colonic stenting. A 75-year-old man was admitted to our hospital with the chief complaint of melena. Esophagogastroduodenoscopy revealed a large ulcerated tumor in the lower stomach, judged by laparoscopy as unresectable (sT4bN1M0). After four cycles of first-line chemotherapy with S-1 plus oxaliplatin, the patient showed disease progression, and second-line therapy with ramucirumab and paclitaxel was started. At the end of the third cycle, the patient had gastric antral stenosis, which necessitated the placement of a gastroduodenal stent. When the patient complained of diarrhea 10 days later, esophagogastroduodenoscopy revealed a fistula between the greater curvature of the stomach and the transverse colon. The fistula was covered by double colonic stenting, with a covered metal stent placed within an uncovered metal stent, after which leakage from the stomach to the colon stopped.
-
Citations
Citations to this article as recorded by- Ramucirumab
Reactions Weekly.2024; 1989(1): 189. CrossRef - Metastatic bladder cancer forming a sigmoidorectal fistula after enfortumab vedotin therapy: a case report
Shinji Tamada, Daiki Ikarashi, Naoki Yanagawa, Moe Toyoshima, Kenta Takahashi, Tomohiko Matsuura, Shigekatsu Maekawa, Renpei Kato, Mitsugu Kanehira, Ryo Takata, Wataru Obara
Frontiers in Oncology.2023;[Epub] CrossRef
- Ramucirumab
- 1,808 View
- 140 Download
- 1 Web of Science
- 2 Crossref

Original Articles
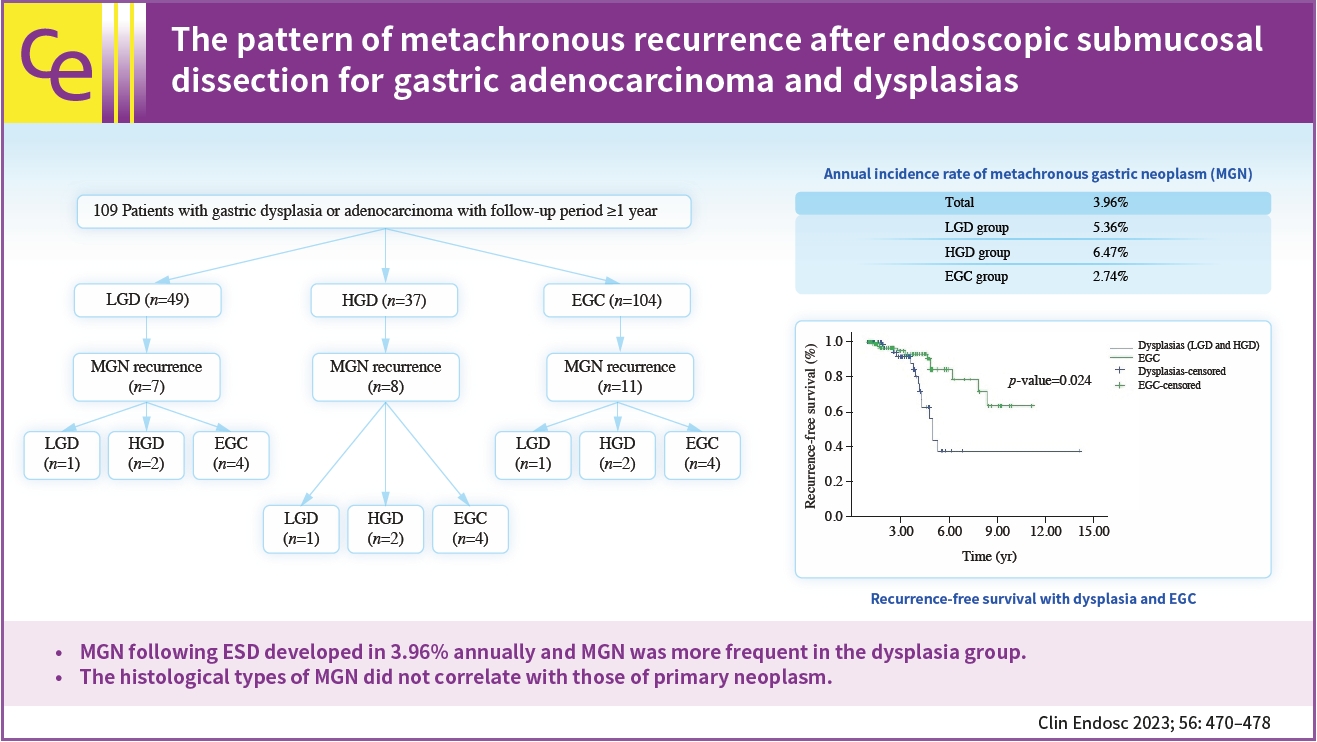
- The pattern of metachronous recurrence after endoscopic submucosal dissection for gastric adenocarcinoma and dysplasias
- Sunah Suk, Yeon Joo Seo, Dae Young Cheung, Han Hee Lee, Jin Il Kim, Soo-Heon Park
- Clin Endosc 2023;56(4):470-478. Published online April 18, 2023
- DOI: https://doi.org/10.5946/ce.2022.259
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: Metachronous recurrence incidences and risk factors following endoscopic submucosal dissection (ESD) for gastric adenocarcinoma and dysplasias were investigated.
Methods
Retrospective review of electronic medical records of patients who underwent gastric ESD at The Catholic University of Korea, Yeouido St. Mary’s Hospital.
Results
A total of 190 subjects were enrolled for analysis during the study period. The mean age was 64.4 years-old and the male sex occupied 73.7%. The mean observation period following ESD was 3.45 years. The annual incidence rate of metachronous gastric neoplasms (MGN) was about 3.96%. The annual incidence rate was 5.36% for the low-grade dysplasia group, 6.47% for the high-grade dysplasia group, and 2.74% for the EGC group. MGN was more frequent in the dysplasia group than in the EGC group (p<0.05). For those with MGN development, the mean time interval from ESD to MGN was 4.1 (±1.8) years. By using the Kaplan–Meier model, the estimated mean MGN free survival time was 9.97 years (95% confidence interval, 8.53–11.40) The histological types of MGN were not related to the primary histology types.
Conclusions
MGN following ESD developed in 3.96% annually and MGN was more frequent in the dysplasia group. The histological types of MGN did not correlate with those of primary neoplasm. -
Citations
Citations to this article as recorded by- Research Progress in ESD Treatment of Early Gastric Cancer
亭 贺
Advances in Clinical Medicine.2024; 14(02): 4201. CrossRef
- Research Progress in ESD Treatment of Early Gastric Cancer
- 1,366 View
- 75 Download
- 1 Crossref

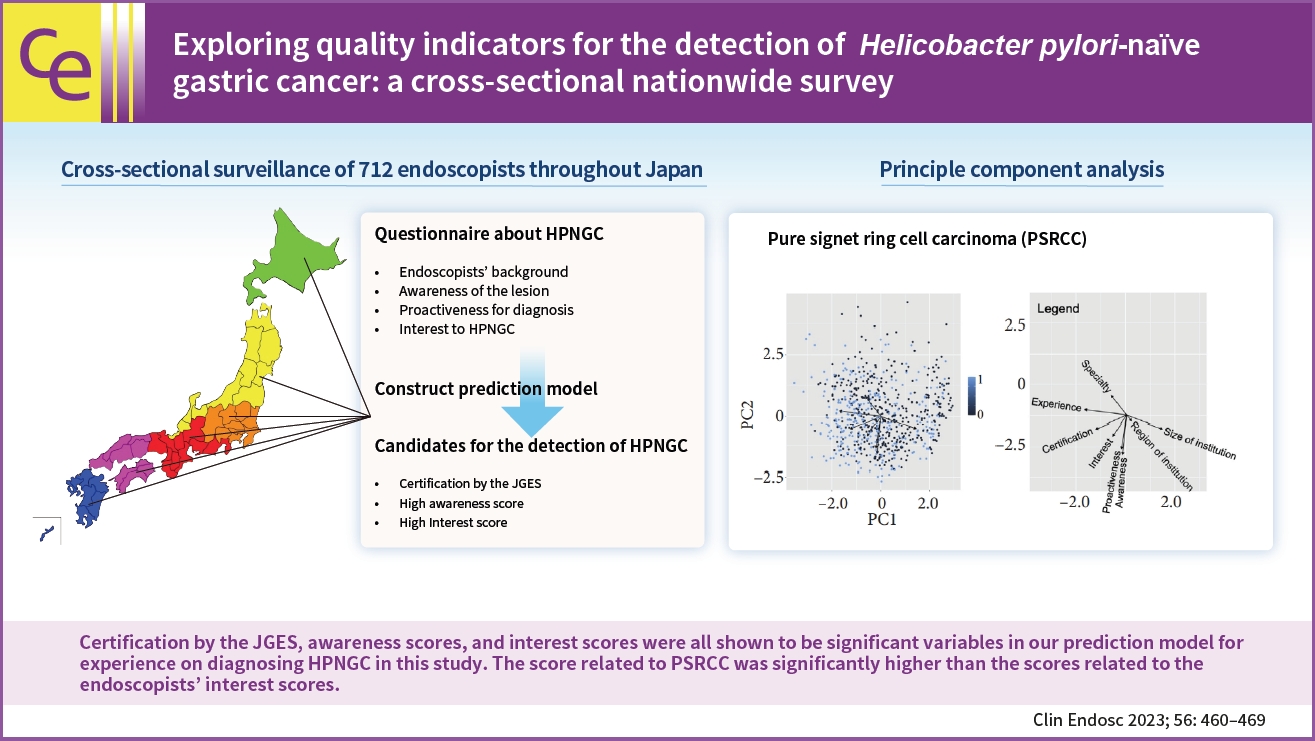
- Exploring quality indicators for the detection of Helicobacter pylori-naïve gastric cancer: a cross-sectional nationwide survey
- Fumiaki Ishibashi, Toshiaki Hirasawa, Hiroya Ueyama, Yohei Minato, Sho Suzuki
- Clin Endosc 2023;56(4):460-469. Published online April 4, 2023
- DOI: https://doi.org/10.5946/ce.2022.167
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub 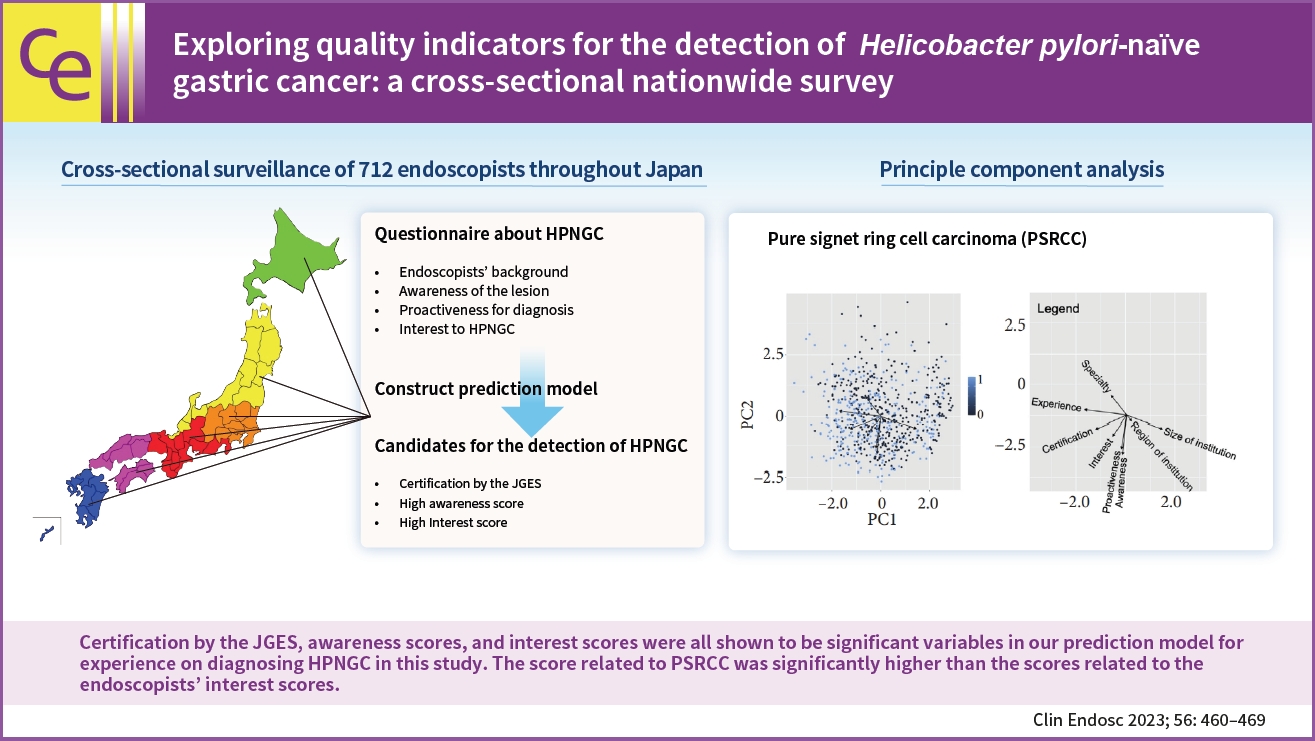
- Background
/Aims: Diagnosis of Helicobacter pylori-naïve gastric cancer (HPNGC) is becoming increasingly important. This study aimed to explore the quality indicators for HPNGC detection.
Methods
We conducted a cross-sectional, nationwide, web-based survey of gastrointestinal endoscopists in Japan. In addition to questions about the number of HPNGC cases detected in a year and basic information, the questionnaire also consisted of 28 questions: (1) 18 about HPNGC awareness, (2) six about diagnostic proactiveness, and (3) four about interest in HPNGC.
Results
Valid responses were obtained from 712 endoscopists. The Japan Gastroenterological Endoscopy Society-certified endoscopists had a significantly higher HPNGC detection rate than the nonspecialists (0.42% vs. 0.32%, respectively; p=0.008). The results of the multiple regression analysis showed that Japan Gastroenterological Endoscopy Society certification and high awareness and interest scores were independent predictors of the HPNGC detection rate (p=0.012, p<0.001, p=0.024, respectively). Principal component analysis showed that the endoscopists who attended conferences for collecting information on HPNGC had a higher level of awareness.
Conclusions
To improve the detection of HPNGC, it is necessary to increase the awareness of the disease. It is hoped that relevant societies will play an important role in endoscopists’ education. -
Citations
Citations to this article as recorded by- Prevalence of Gastric Epithelial Tumors in Helicobacter pylori-uninfected Individuals Undergoing a Medical Checkup
Eiko Okimoto, Kyoichi Adachi, Yuri Ebisutani, Norihisa Ishimura, Shunji Ishihara
Internal Medicine.2024;[Epub] CrossRef - Improving the quality of the esophagogastroduodenoscopy in Helicobacter pylori-naïve gastric cancer
Jae Myung Park
Clinical Endoscopy.2023; 56(4): 453. CrossRef
- Prevalence of Gastric Epithelial Tumors in Helicobacter pylori-uninfected Individuals Undergoing a Medical Checkup
- 2,616 View
- 130 Download
- 1 Web of Science
- 2 Crossref

- Endoscopic submucosal dissection for superficial esophageal squamous cell carcinoma: long-term follow-up in a Western center
- Andreas Probst, Alanna Ebigbo, Stefan Eser, Carola Fleischmann, Tina Schaller, Bruno Märkl, Stefan Schiele, Bernd Geissler, Gernot Müller, Helmut Messmann
- Clin Endosc 2023;56(1):55-64. Published online January 13, 2023
- DOI: https://doi.org/10.5946/ce.2022.093
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic submucosal dissection (ESD) has been established as a treatment modality for superficial esophageal squamous cell carcinoma (ESCC). Long-term follow-up data are lacking in Western countries. The aim of this study was to analyze long-term survival in a Western center.
Methods
Patients undergoing ESD for ESCC were included. The analysis was performed retrospectively using a prospectively collected database.
Results
R0 resection rate was 96.7% (59/61 lesions in 58 patients). Twenty-seven patients (46.6%) fulfilled the curative resection criteria (M1/M2) (group A), 11 patients (19.0%) had M3 lesions without lymphovascular invasion (LVI) (group B), and 20 patients (34.5%) had lesions with submucosal invasion or LVI (group C). Additional treatment was recommended after non-curative resection. It was not performed in 20/31 patients (64.5%), mainly because of comorbidities (75%). Twenty-nine out of 58 (50.0%) patients died during a mean follow-up of 3.7 years. Death was related to ESCC in 17.2% (5/29) of patients. The disease-specific survival rate after curative resection was 100%. Overall survival rates after 5 years were 61.5%, 63.6% and 28.1% for groups A, B, and C, respectively. The overall survival was significantly worse after non-curative resection (p=0.038).
Conclusions
Non-curative resection is frequent after ESD for ESCC in Western patients. The long-term prognosis is limited and mainly determined by comorbidity. Early diagnosis and pre-interventional assessments need to be improved. -
Citations
Citations to this article as recorded by- Endoscopic submucosal dissection for early esophageal squamous cell carcinoma: long-term results from a Western cohort
Ilse N. Beaufort, Charlotte N. Frederiks, Anouk Overwater, Lodewijk A.A. Brosens, Arjun D. Koch, Roos E. Pouw, Jacques J.G.H.M. Bergman, Bas L.A.M. Weusten
Endoscopy.2024; 56(05): 325. CrossRef - Endoscopic Submucosal Dissection for Esophageal Cancer: Current and Future
Yuki Okubo, Ryu Ishihara
Life.2023; 13(4): 892. CrossRef
- Endoscopic submucosal dissection for early esophageal squamous cell carcinoma: long-term results from a Western cohort
- 2,267 View
- 137 Download
- 2 Web of Science
- 2 Crossref

- Non-atrophic gastric mucosa is an independently associated factor for superficial non-ampullary duodenal epithelial tumors: a multicenter, matched, case-control study
- Azusa Kawasaki, Kunihiro Tsuji, Noriya Uedo, Takashi Kanesaka, Hideaki Miyamoto, Ryosuke Gushima, Yosuke Minoda, Eikichi Ihara, Ryosuke Amano, Kenshi Yao, Yoshihide Naito, Hiroyuki Aoyagi, Takehiro Iwasaki, Kunihisa Uchita, Hisatomi Arima, Hisashi Doyama
- Clin Endosc 2023;56(1):75-82. Published online January 5, 2023
- DOI: https://doi.org/10.5946/ce.2022.059
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: The etiology of superficial non-ampullary duodenal epithelial tumors (SNADETs) remains unclear. Recent studies have reported conflicting associations between duodenal tumor development and Helicobacter pylori infection or endoscopic gastric mucosal atrophy. As such, the present study aimed to clarify the relationship between SNADETs and H. pylori infection and/or endoscopic gastric mucosal atrophy.
Methods
This retrospective case-control study reviewed data from 177 consecutive patients with SNADETs who underwent endoscopic or surgical resection at seven institutions in Japan over a three-year period. The prevalence of endoscopic gastric mucosal atrophy and the status of H. pylori infection were compared in 531 sex- and age-matched controls selected from screening endoscopies at two of the seven participating institutions.
Results
For H. pylori infection, 85 of 177 (48.0%) patients exhibited SNADETs and 112 of 531 (21.1%) control patients were non-infected (p<0.001). Non-atrophic mucosa (C0 to C1) was observed in 96 of 177 (54.2%) patients with SNADETs and 112 of 531 (21.1%) control patients (p<0.001). Conditional logistic regression analysis revealed that non-atrophic gastric mucosa was an independent risk factor for SNADETs (odds ratio, 5.10; 95% confidence interval, 2.44–8.40; p<0.001).
Conclusions
Non-atrophic gastric mucosa, regardless of H. pylori infection status, was a factor independently associated with SNADETs.
- 2,320 View
- 137 Download

Review
- Korean guidelines for postpolypectomy colonoscopic surveillance: 2022 revised edition
- Su Young Kim, Min Seob Kwak, Soon Man Yoon, Yunho Jung, Jong Wook Kim, Sun-Jin Boo, Eun Hye Oh, Seong Ran Jeon, Seung-Joo Nam, Seon-Young Park, Soo-Kyung Park, Jaeyoung Chun, Dong Hoon Baek, Mi-Young Choi, Suyeon Park, Jeong-Sik Byeon, Hyung Kil Kim, Joo Young Cho, Moon Sung Lee, Oh Young Lee, Korean Society of Gastrointestinal Endoscopy, Korean Society of Gastroenterology, Korean Association for the Study of Intestinal Diseases
- Clin Endosc 2022;55(6):703-725. Published online October 13, 2022
- DOI: https://doi.org/10.5946/ce.2022.136
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
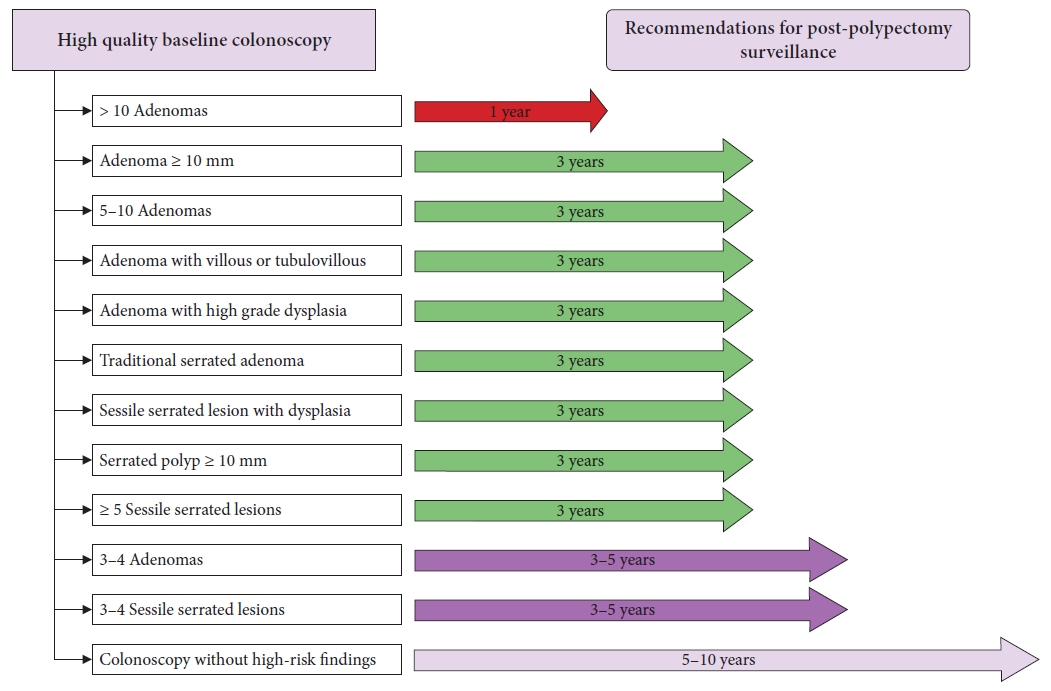
ePub - Colonoscopic polypectomy is effective in decreasing the incidence and mortality of colorectal cancer (CRC). Premalignant polyps discovered during colonoscopy are associated with the risk of metachronous advanced neoplasia. Postpolypectomy surveillance is the most important method for the management of advanced metachronous neoplasia. A more efficient and evidence-based guideline for postpolypectomy surveillance is required because of limited medical resources and concerns regarding colonoscopy complications. In these consensus guidelines, an analytic approach was used to address all reliable evidence to interpret the predictors of CRC or advanced neoplasia during surveillance colonoscopy. The key recommendations state that the high-risk findings for metachronous CRC following polypectomy are as follows: (1) adenoma ≥10 mm in size; (2) 3 to 5 (or more) adenomas; (3) tubulovillous or villous adenoma; (4) adenoma containing high-grade dysplasia; (5) traditional serrated adenoma; (6) sessile serrated lesion (SSL) containing any grade of dysplasia; (7) serrated polyp of at least 10 mm in size; and (8) 3 to 5 (or more) SSLs. More studies are needed to fully comprehend the patients most likely to benefit from surveillance colonoscopy and the ideal surveillance interval to prevent metachronous CRC.
-
Citations
Citations to this article as recorded by- Association between Atherosclerosis and High-Risk Colorectal Adenomas based on Cardio-Ankle Vascular Index and Ankle-Brachial Index
Jung Ho Lee, Hyunseok Cho, Sang Hoon Lee, Sung Joon Lee, Chang Don Kang, Dae Hee Choi, Jin Myung Park, Seung-Joo Nam, Tae Suk Kim, Ji Hyun Kim, Sung Chul Park
The Korean Journal of Gastroenterology.2024; 83(4): 143. CrossRef - A survey of current practices in post-polypectomy surveillance in Korea
Jeongseok Kim, Tae-Geun Gweon, Min Seob Kwak, Su Young Kim, Seong Jung Kim, Hyun Gun Kim, Eun Ran Kim, Sung Noh Hong, Eun Sun Kim, Chang Mo Moon, Dae Seong Myung, Dong Hoon Baek, Shin Ju Oh, Hyun Jung Lee, Ji Young Lee, Yunho Jung, Jaeyoung Chun, Dong-Hoo
Intestinal Research.2024; 22(2): 186. CrossRef - Korean Guidelines for Postpolypectomy Colonoscopic Surveillance: 2022 Revision
Su Young Kim
The Korean Journal of Medicine.2023; 98(3): 102. CrossRef - Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Mizuki Nagai, Sho Suzuki, Yohei Minato, Fumiaki Ishibashi, Kentaro Mochida, Ken Ohata, Tetsuo Morishita
Clinical Endoscopy.2023; 56(5): 553. CrossRef - Understanding colorectal polyps to prevent colorectal cancer
Dong-Hoon Yang
Journal of the Korean Medical Association.2023; 66(11): 626. CrossRef - Classification and endoscopic diagnosis of colorectal polyps
Ji Hyun Kim, Sung Chul Park
Journal of the Korean Medical Association.2023; 66(11): 633. CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef - Strategy for post-polypectomy colonoscopy surveillance: focus on the revised Korean guidelines
Yong Soo Kwon, Su Young Kim
Journal of the Korean Medical Association.2023; 66(11): 652. CrossRef
- Association between Atherosclerosis and High-Risk Colorectal Adenomas based on Cardio-Ankle Vascular Index and Ankle-Brachial Index
- 5,244 View
- 515 Download
- 8 Web of Science
- 8 Crossref

Original Articles
- Endoscopic submucosal dissection in colorectal neoplasia performed with a waterjet system-assisted knife: higher en-bloc resection rate than conventional technique
- Paolo Cecinato, Matteo Lucarini, Francesco Azzolini, Mariachiara Campanale, Fabio Bassi, Annalisa Cippitelli, Romano Sassatelli
- Clin Endosc 2022;55(6):775-783. Published online October 6, 2022
- DOI: https://doi.org/10.5946/ce.2022.099

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Colorectal endoscopic submucosal dissection (ESD) is burdened by its associated high risk of adverse events and long procedure time. Recently, a waterjet-assisted knife was introduced to simplify and speed up the procedure. The aim of this study was to evaluate the efficacy and safety of waterjet-assisted ESD (WESD) compared to that of the conventional ESD (CESD) technique.
Methods
The charts of 254 consecutive patients who underwent colorectal ESD between January 2014 and February 2021 for colorectal neoplasms were analyzed. The primary outcome was the en-bloc resection rate. Secondary outcomes were complete and curative resection rates, the need to switch to a hybrid ESD, procedure speed, the adverse event rates, and the recurrence rates.
Results
Approximately 174 neoplasias were considered, of which, 123 were removed by WESD and 51 by CESD. The en-bloc resection rate was higher in the WESD group (94.3% vs. 84.3%). Complete resection rates and curative resection rates were similar. The need to switch to a hybrid ESD was greater during CESD (39.2% vs. 13.8%). Procedure speed and adverse event rates were similar. During follow-up, one recurrence occurred after a WESD.
Conclusions
WESD allows a high rate of en-bloc resections and less frequently requires a rescue switch to the hybrid ESD compared to CESD. -
Citations
Citations to this article as recorded by- Is there a best choice of equipment for colorectal endoscopic submucosal dissection?
Francesco Cocomazzi, Sonia Carparelli, Nunzia Labarile, Antonio Capogreco, Marco Gentile, Roberta Maselli, Jahnvi Dhar, Jayanta Samanta, Alessandro Repici, Cesare Hassan, Francesco Perri, Antonio Facciorusso
Expert Review of Medical Devices.2024; : 1. CrossRef - Colorectal Endoscopic Submucosal Dissection: Performance of a Novel Hybrid-Technology Knife in an Animal Trial
Jérémie Jacques, Horst Neuhaus, Markus D. Enderle, Ulrich Biber, Walter Linzenbold, Martin Schenk, Kareem Khalaf, Alessandro Repici
Diagnostics.2023; 13(21): 3347. CrossRef
- Is there a best choice of equipment for colorectal endoscopic submucosal dissection?
- 2,026 View
- 127 Download
- 3 Web of Science
- 2 Crossref

-
Intralesional steroid infusion using a spray tube to prevent stenosis after endoscopic submucosal dissection of esophageal cancer

- Atsushi Goto, Takeshi Okamoto, Ryo Ogawa, Kouichi Hamabe, Shinichi Hashimoto, Jun Nishikawa, Taro Takami
- Clin Endosc 2022;55(4):520-524. Published online July 28, 2022
- DOI: https://doi.org/10.5946/ce.2021.262
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
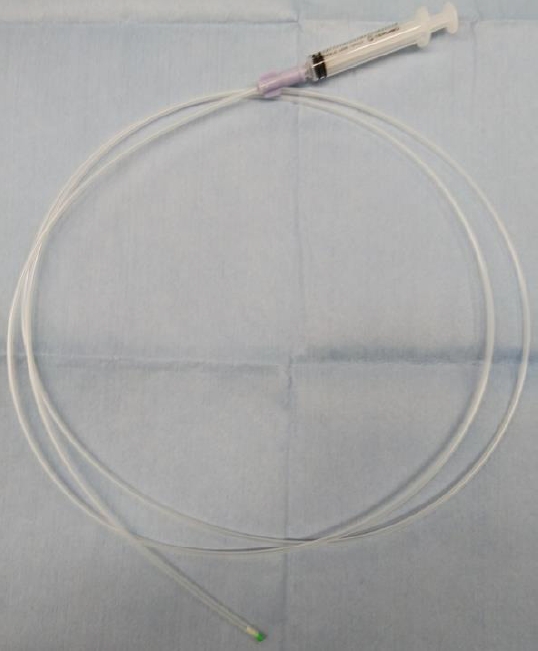
/Aims: Intralesional steroid injections have been administered as prophylaxis for stenosis after esophageal endoscopic submucosal dissection. However, this method carries a risk of potential complications such as perforation because a fine needle is used to directly puncture the postoperative ulcer. We devised a new method of steroid intralesional infusion using a spray tube and evaluated its efficacy and safety.
Methods
Intralesional steroid infusion using a spray tube was performed on 27 patients who underwent endoscopic submucosal dissection for superficial esophageal cancer with three-quarters or more of the lumen circumference resected. The presence or absence of stenosis, complications, and the number of endoscopic balloon dilations (EBDs) performed were evaluated after treatment.
Results
Although stenosis was not observed in 22 of the 27 patients, five patients had stenosis and dysphagia requiring EBD. The stenosis in these five patients was relieved after four EBDs. No complications related to intralesional steroid infusion using the spray tube were observed.
Conclusions
Intralesional steroid infusion using a spray tube is a simple and safe technique that is adequately effective in preventing stenosis Clinical trial number (UMIN000037567).
- 2,738 View
- 133 Download
- 1 Web of Science

Reviews
- Post-polypectomy surveillance: the present and the future
- Masau Sekiguchi, Takahisa Matsuda, Kinichi Hotta, Yutaka Saito
- Clin Endosc 2022;55(4):489-495. Published online July 11, 2022
- DOI: https://doi.org/10.5946/ce.2022.097
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
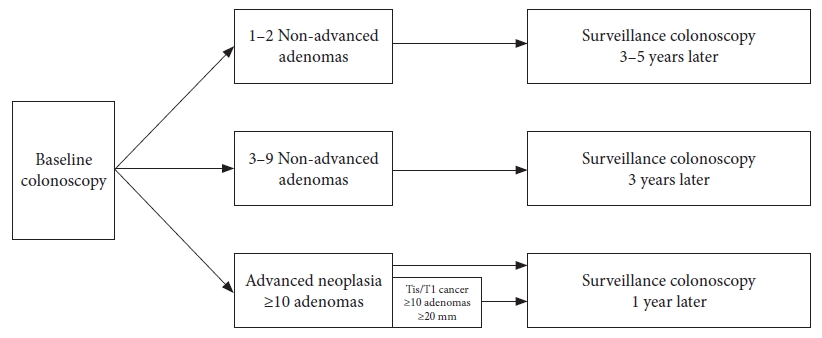
ePub - An appropriate post-polypectomy surveillance program requires the effectiveness of reducing colorectal cancer and safety. In addition, the post-polypectomy surveillance program should consider the burden of limited medical resource capacity, cost-effectiveness, and patient adherence. In this sense, a risk-stratified surveillance program based on baseline colonoscopy results is ideal. Major international guidelines for post-polypectomy surveillance, such as those from the European Union and the United States, have recommended risk-stratified surveillance programs. Both guidelines have recently been updated to better differentiate between high- and low-risk individuals. In both updated guidelines, more individuals have been downgraded to lower-risk groups that require less frequent or no surveillance. Furthermore, increased attention has been paid to the surveillance of patients who undergo serrated polyp removal. Previous guidelines in Japan did not clearly outline the risk stratification in post-polypectomy surveillance. However, the new colonoscopy screening and surveillance guidelines presented by the Japan Gastroenterological Endoscopy Society include a risk-stratified post-polypectomy surveillance program. Further discussion and analysis of unresolved issues in this field, such as the optimal follow-up after the first surveillance, the upper age limit for surveillance, and the ideal method for improving adherence to surveillance guidelines, are warranted.
-
Citations
Citations to this article as recorded by- Protocolo diagnóstico del seguimiento de pólipos colónicos
S. Redondo Evangelista, M. Sierra Morales, I. Bartolomé Oterino, P. García Centeno, A. Santos Rodríguez
Medicine - Programa de Formación Médica Continuada Acreditado.2024; 14(4): 219. CrossRef - Metabolic‐associated fatty liver disease is associated with colorectal adenomas in young and older Korean adults
Jiwon Chang, Yoosoo Chang, Yoosun Cho, Hyun‐Suk Jung, Dong‐Il Park, Soo‐Kyung Park, Soo‐Youn Ham, Sarah H. Wild, Christopher D. Byrne, Seungho Ryu
Liver International.2023; 43(11): 2548. CrossRef - Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Mizuki Nagai, Sho Suzuki, Yohei Minato, Fumiaki Ishibashi, Kentaro Mochida, Ken Ohata, Tetsuo Morishita
Clinical Endoscopy.2023; 56(5): 553. CrossRef - Strategy for post-polypectomy colonoscopy surveillance: focus on the revised Korean guidelines
Yong Soo Kwon, Su Young Kim
Journal of the Korean Medical Association.2023; 66(11): 652. CrossRef - Endoscopic treatment of colorectal polyps and early colorectal cancer
Yunho Jung
Journal of the Korean Medical Association.2023; 66(11): 642. CrossRef - Understanding colorectal polyps to prevent colorectal cancer
Dong-Hoon Yang
Journal of the Korean Medical Association.2023; 66(11): 626. CrossRef
- Protocolo diagnóstico del seguimiento de pólipos colónicos
- 3,561 View
- 249 Download
- 5 Web of Science
- 6 Crossref

- Can Computed Tomography Colonography Replace Optical Colonoscopy in Detecting Colorectal Lesions?: State of the Art
- Alessia Chini, Michele Manigrasso, Grazia Cantore, Rosa Maione, Marco Milone, Francesco Maione, Giovanni Domenico De Palma
- Clin Endosc 2022;55(2):183-190. Published online February 24, 2022
- DOI: https://doi.org/10.5946/ce.2021.254
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
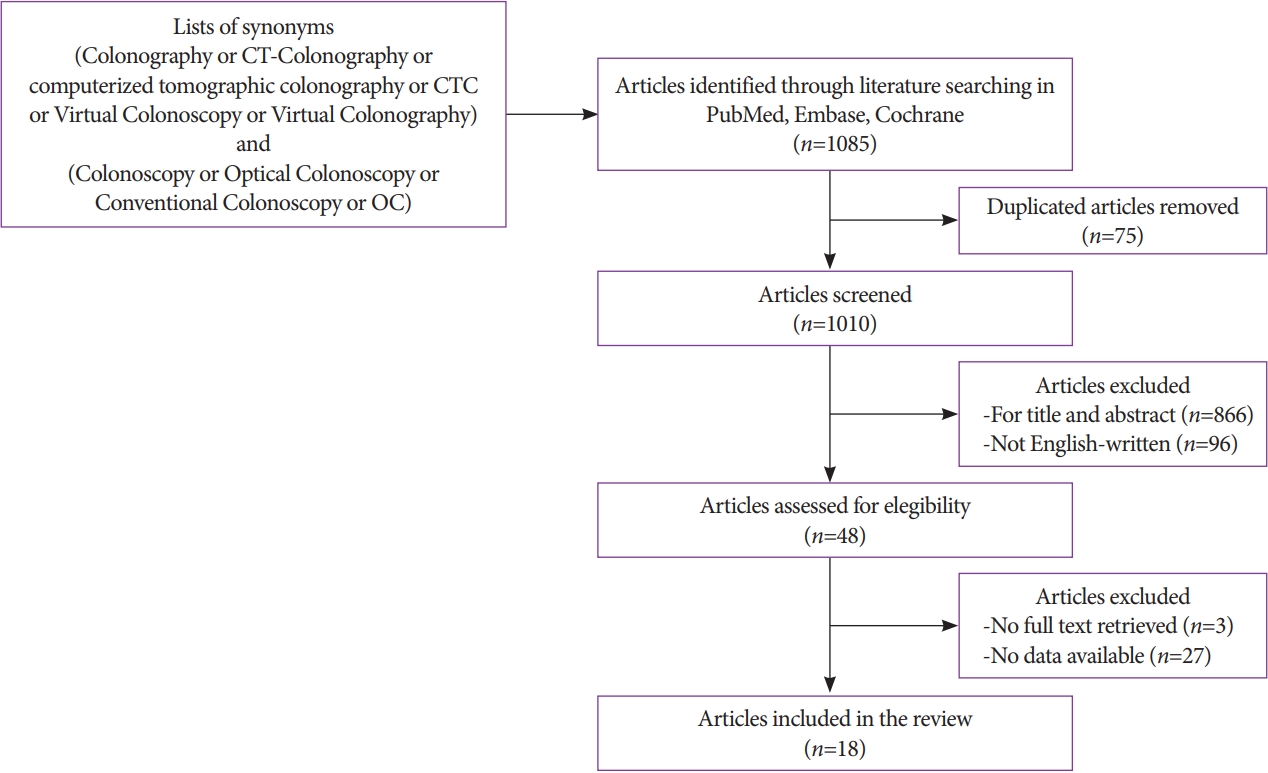
ePub - Colorectal cancer is an important cause of morbidity and mortality worldwide. Optical colonoscopy (OC) is widely accepted as the reference standard for the screening of colorectal polyps and cancers, and computed tomography colonography (CTC) is a valid alternative to OC. The purpose of this review was to assess the diagnostic accuracy of OC and CTC for colorectal lesions. A literature search was performed in PubMed, Embase, and Cochrane Library, and 18 articles were included. CTC has emerged in recent years as a potential screening examination with high accuracy for the detection of colorectal lesions. However, the clinical application of CTC as a screening technique is limited because it is highly dependent on the size of the lesions and has poor performance in detecting individual lesions <5 mm or flat lesions, which, although rarely, can have a malignant potential.
-
Citations
Citations to this article as recorded by- Multi-view orientational attention network combining point-based affinity for polyp segmentation
Yan Liu, Yan Yang, Yongquan Jiang, Zhuyang Xie
Expert Systems with Applications.2024; 249: 123663. CrossRef - The Influence of Mechanical Bowel Preparation on Volatile Organic Compounds for the Detection of Gastrointestinal Disease—A Systematic Review
Ashwin Krishnamoorthy, Subashini Chandrapalan, Sofie Bosch, Ayman Bannaga, Nanne K.H. De Boer, Tim G.J. De Meij, Marcis Leja, George B. Hanna, Nicoletta De Vietro, Donato Altomare, Ramesh P. Arasaradnam
Sensors.2023; 23(3): 1377. CrossRef - The Detection of Colorectal Cancer through Machine Learning-Based Breath Sensor Analysis
Inese Poļaka, Linda Mežmale, Linda Anarkulova, Elīna Kononova, Ilona Vilkoite, Viktors Veliks, Anna Marija Ļeščinska, Ilmārs Stonāns, Andrejs Pčolkins, Ivars Tolmanis, Gidi Shani, Hossam Haick, Jan Mitrovics, Johannes Glöckler, Boris Mizaikoff, Mārcis Lej
Diagnostics.2023; 13(21): 3355. CrossRef
- Multi-view orientational attention network combining point-based affinity for polyp segmentation
- 3,802 View
- 233 Download
- 4 Web of Science
- 3 Crossref

Original Article
- Risk Stratification in Cancer Patients with Acute Upper Gastrointestinal Bleeding: Comparison of Glasgow-Blatchford, Rockall and AIMS65, and Development of a New Scoring System
- Matheus Cavalcante Franco, Sunguk Jang, Bruno da Costa Martins, Tyler Stevens, Vipul Jairath, Rocio Lopez, John J. Vargo, Alan Barkun, Fauze Maluf-Filho
- Clin Endosc 2022;55(2):240-247. Published online January 21, 2022
- DOI: https://doi.org/10.5946/ce.2021.115
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
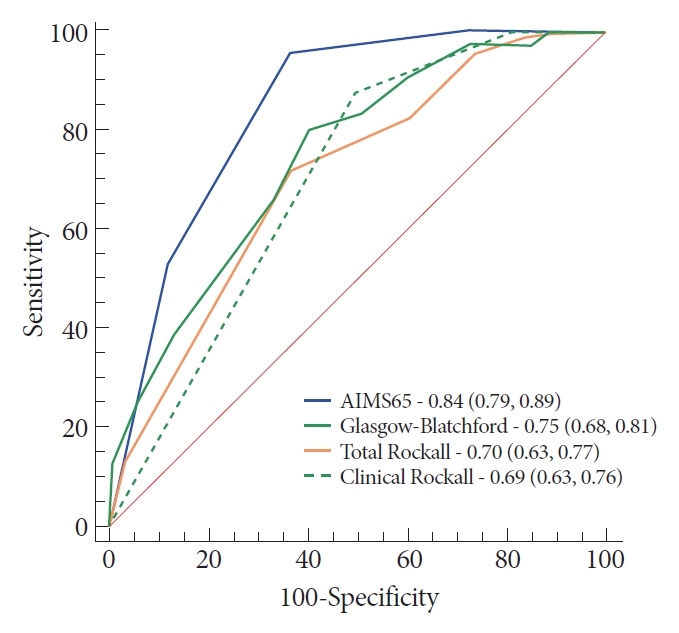
ePub - Background
/Aims: Few studies have measured the accuracy of prognostic scores for upper gastrointestinal bleeding (UGIB) among cancer patients. Thereby, we compared the prognostic scores for predicting major outcomes in cancer patients with UGIB. Secondarily, we developed a new model to detect patients who might require hemostatic care.
Methods
A prospective research was performed in a tertiary hospital by enrolling cancer patients admitted with UGIB. Clinical and endoscopic findings were obtained through a prospective database. Multiple logistic regression analysis was performed to gauge the power of each score.
Results
From April 2015 to May 2016, 243 patients met the inclusion criteria. The AIMS65 (area under the curve [AUC] 0.85) best predicted intensive care unit admission, while the Glasgow-Blatchford score best predicted blood transfusion (AUC 0.82) and the low-risk group (AUC 0.92). All scores failed to predict hemostatic therapy and rebleeding. The new score was superior (AUC 0.74) in predicting hemostatic therapy. The AIMS65 (AUC 0.84) best predicted in-hospital mortality.
Conclusions
The scoring systems for prognostication were validated in the group of cancer patients with UGIB. A new score was developed to predict hemostatic therapy. Following this result, future prospective research should be performed to validate the new score. -
Citations
Citations to this article as recorded by- Endoscopic Management of Tumor Bleeding
Frances Dang, Marc Monachese
Gastrointestinal Endoscopy Clinics of North America.2024; 34(1): 155. CrossRef - The Accuracy of Pre-Endoscopic Scores for Mortality Prediction in Patients with Upper GI Bleeding and No Endoscopy Performed
Sergiu Marian Cazacu, Dragoș Ovidiu Alexandru, Răzvan-Cristian Statie, Sevastița Iordache, Bogdan Silviu Ungureanu, Vlad Florin Iovănescu, Petrică Popa, Victor Mihai Sacerdoțianu, Carmen Daniela Neagoe, Mirela Marinela Florescu
Diagnostics.2023; 13(6): 1188. CrossRef - Progress in the Evaluation of Acute Upper Gastrointestinal Bleeding with AIMS65 Scoring System
莉 王
Advances in Clinical Medicine.2023; 13(05): 8163. CrossRef - Interpretations of the Role of Plasma Albumin in Prognostic Indices: A Literature Review
Kim Oren Gradel
Journal of Clinical Medicine.2023; 12(19): 6132. CrossRef
- Endoscopic Management of Tumor Bleeding
- 3,226 View
- 231 Download
- 3 Web of Science
- 4 Crossref

Case Report
- Gastric wall abscess after endoscopic submucosal dissection
- Seung Jung Yu, Sang Heon Lee, Jun Sik Yoon, Hong Sub Lee, Sam Ryong Jee
- Clin Endosc 2023;56(1):114-118. Published online January 3, 2022
- DOI: https://doi.org/10.5946/ce.2021.203
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Gastric wall abscess, a localized form of phlegmonous gastritis, is a rare complication of endoscopic resection. We report the first case of gastric wall abscess developing after endoscopic submucosal dissection in Korea. A 72-year-old woman visited our clinic to receive treatment for gastric adenoma. The patient successfully underwent endoscopic submucosal dissection with no complications. The final diagnosis was well-differentiated tubular adenocarcinoma. We performed follow-up endoscopy 10 weeks later and found a large subepithelial lesion on the posterior wall of the gastric antrum. Abdominal computed tomography revealed hypodense wall thickening and a 5 cm heterogenous multilobular mass in the submucosal layer of the gastric antrum. Submucosal invasion with mucin-producing adenocarcinomas could therefore not be excluded. The patient agreed to undergo additional gastrectomy due to the possibility of a highly malignant lesion. The final diagnosis was acute suppurative inflammation with the formation of multiple abscesses in the mural layers and omentum. The patient was discharged with no complications.
-
Citations
Citations to this article as recorded by- Phlegmonous gastritis after biloma drainage: A case report and review of the literature
Kai-Chun Yang, Hsin-Yu Kuo, Jui-Wen Kang
World Journal of Clinical Cases.2022; 10(33): 12430. CrossRef
- Phlegmonous gastritis after biloma drainage: A case report and review of the literature
- 3,875 View
- 261 Download
- 1 Web of Science
- 1 Crossref

Original Articles
- Efficacy and Safety of Endoscopic Submucosal Dissection for Superficial Gastric Neoplasms: A Latin American Cohort Study
- Fernando Palacios-Salas, Harold Benites-Goñi, Luis Marin-Calderón, Paulo Bardalez-Cruz, Jorge Vásquez-Quiroga, Edgar Alva-Alva, Bryan Medina-Morales, Jairo Asencios-Cusihuallpa
- Clin Endosc 2022;55(2):248-255. Published online November 12, 2021
- DOI: https://doi.org/10.5946/ce.2021.192

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic submucosal dissection (ESD) is the preferred technique for treating early gastric cancer (EGC). However, very few studies have been conducted in South America. This study aimed to assess the efficacy and safety of ESD for EGC.
Methods
We analyzed data from a prospective cohort from 2013 to 2020. A total of 152 superficial gastric neoplasms that fulfilled the absolute or expanded criteria for ESD were included. Outcomes were en bloc, R0, and curative resection rates, incidence of adverse events, and length of procedure.
Results
The age of the enrolled patients was 68.4±11.3 years. The number of included patients based on the absolute and expanded indications was 150 and 2, respectively. En bloc, R0, and curative resections were achieved in 98.0%, 96.1%, and 89.5% of the cases, respectively. Bleeding and perforation were reported in 5.9% and 6.6% of the cases, respectively. Histopathological examination revealed lowgrade dysplasia, high-grade dysplasia, well-differentiated adenocarcinoma, and poorly differentiated adenocarcinoma in 13, 20, 117, and 2 cases, respectively.
Conclusions
Our study shows that ESD performed by properly trained endoscopists in reference centers is safe and effective, with comparable therapeutic outcomes to those reported in the Eastern series. -
Citations
Citations to this article as recorded by- Short-Term and Long-Term Outcomes of Liver Cirrhosis in Gastric Neoplasm Patients Undergoing Endoscopic Submucosal Dissection
Xu-Rui Liu, Lian-Shuo Li, Fei Liu, Zi-Wei Li, Xiao-Yu Liu, Wei Zhang, Dong Peng
Journal of Laparoendoscopic & Advanced Surgical Techniques.2023; 33(7): 640. CrossRef - Endoscopic submucosal dissection for early gastric cancer: It is time to consider the quality of its outcomes
Gwang Ha Kim
World Journal of Gastroenterology.2023; 29(43): 5800. CrossRef - Endoscopic diagnosis of early gastric cancer
Dong Chan Joo, Gwang Ha Kim
Journal of the Korean Medical Association.2022; 65(5): 267. CrossRef - Therapeutic approach to non-curative resection after endoscopic treatment in early gastric cancer
Eun Jeong Gong, Chang Seok Bang
Journal of the Korean Medical Association.2022; 65(5): 284. CrossRef
- Short-Term and Long-Term Outcomes of Liver Cirrhosis in Gastric Neoplasm Patients Undergoing Endoscopic Submucosal Dissection
- 3,967 View
- 218 Download
- 5 Web of Science
- 4 Crossref

- Clinical Impact of Different Reconstruction Methods on Remnant Gastric Cancer at the Anastomotic Site after Distal Gastrectomy
- Kei Matsumoto, Shinwa Tanaka, Takashi Toyonaga, Nobuaki Ikezawa, Mari Nishio, Masanao Uraoka, Tomoatsu Yoshihara, Hiroya Sakaguchi, Hirofumi Abe, Tetsuya Yoshizaki, Madoka Takao, Toshitatsu Takao, Yoshinori Morita, Hiroshi Yokozaki, Yuzo Kodama
- Clin Endosc 2022;55(1):86-94. Published online August 13, 2021
- DOI: https://doi.org/10.5946/ce.2021.084
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: The anastomotic site after distal gastrectomy is the area most affected by duodenogastric reflux. Different reconstruction methods may affect the lesion characteristics and treatment outcomes of remnant gastric cancers at the anastomotic site. We retrospectively investigated the clinicopathologic and endoscopic submucosal dissection outcomes of remnant gastric cancers at the anastomotic site.
Methods
We recruited 34 consecutive patients who underwent endoscopic submucosal dissection for remnant gastric cancer at the anastomotic site after distal gastrectomy. Clinicopathology and treatment outcomes were compared between the Billroth II and non-Billroth II groups.
Results
The tumor size in the Billroth II group was significantly larger than that in the non-Billroth II group (22 vs. 19 mm; p=0.048). More severe gastritis was detected endoscopically in the Billroth II group (2 vs. 1.33; p=0.0075). Moreover, operation time was longer (238 vs. 121 min; p=0.004) and the frequency of bleeding episodes was higher (7.5 vs. 3.1; p=0.014) in the Billroth II group.
Conclusions
Compared to remnant gastric cancers in non-Billroth II patients, those in the Billroth II group had larger lesions with a background of severe remnant gastritis. Endoscopic submucosal dissection for remnant gastric cancers in Billroth II patients involved longer operative times and more frequent bleeding episodes than that in patients without Billroth II.
- 4,132 View
- 144 Download

Focused Review Series: Image-Enhanced Endoscopy: Update on Clinical Practice
- Current Status of Image-Enhanced Endoscopy for Early Identification of Esophageal Neoplasms
- Shin Hee Kim, Su Jin Hong
- Clin Endosc 2021;54(4):464-476. Published online July 26, 2021
- DOI: https://doi.org/10.5946/ce.2021.186
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Advanced esophageal cancer is known to have a poor prognosis. The early detection of esophageal neoplasms, including esophageal dysplasia and early esophageal cancer, is highly important for the accurate treatment of the disease. However, esophageal dysplasia and early esophageal cancer are usually subtle and can be easily missed. In addition to the early detection, proper pretreatment evaluation of the depth of invasion of esophageal cancer is very important for curative treatment. The progression of non-invasive diagnosis via image-enhanced endoscopy techniques has been shown to aid the early detection and estimate the depth of invasion of early esophageal cancer and, as a result, may provide additional opportunities for curative treatment. Here, we review the advancement of image-enhanced endoscopy-related technologies and their role in the early identification of esophageal neoplasms.
-
Citations
Citations to this article as recorded by- An umbrella-inspired snap-on robotic 3D photoacoustic endoscopic probe for augmented intragastric sensing: Proof of concept study
Li Liu, Ang Li, Yisong Zhao, Luyao Zhu, Yongjian Zhao, Fei Gao
Photoacoustics.2024; 35: 100568. CrossRef - Curative criteria for endoscopic treatment of oesophageal adenocarcinoma
Annemijn D.I. Maan, Prateek Sharma, Arjun D. Koch
Best Practice & Research Clinical Gastroenterology.2024; 68: 101886. CrossRef - Biomarkers for Early Detection, Prognosis, and Therapeutics of Esophageal Cancers
Vikrant Rai, Joe Abdo, Devendra K. Agrawal
International Journal of Molecular Sciences.2023; 24(4): 3316. CrossRef - Magnifying Endoscopy with Narrow-Band Imaging for Duodenal Neuroendocrine Tumors
Gwang Ha Kim, Kiyoun Yi, Dong Chan Joo, Moon Won Lee, Hye Kyung Jeon, Bong Eun Lee
Journal of Clinical Medicine.2023; 12(9): 3106. CrossRef - Role of linked color imaging for upper gastrointestinal disease: present and future
Sang Pyo Lee
Clinical Endoscopy.2023; 56(5): 546. CrossRef - Analysis of Colorectal and Gastric Cancer Classification: A Mathematical Insight Utilizing Traditional Machine Learning Classifiers
Hari Mohan Rai, Joon Yoo
Mathematics.2023; 11(24): 4937. CrossRef - Application of artificial intelligence-assisted endoscopic detection of early esophageal cancer
Qing Li, Bing-Rong Liu
World Chinese Journal of Digestology.2021; 29(24): 1389. CrossRef
- An umbrella-inspired snap-on robotic 3D photoacoustic endoscopic probe for augmented intragastric sensing: Proof of concept study
- 4,976 View
- 260 Download
- 6 Web of Science
- 7 Crossref

Original Articles
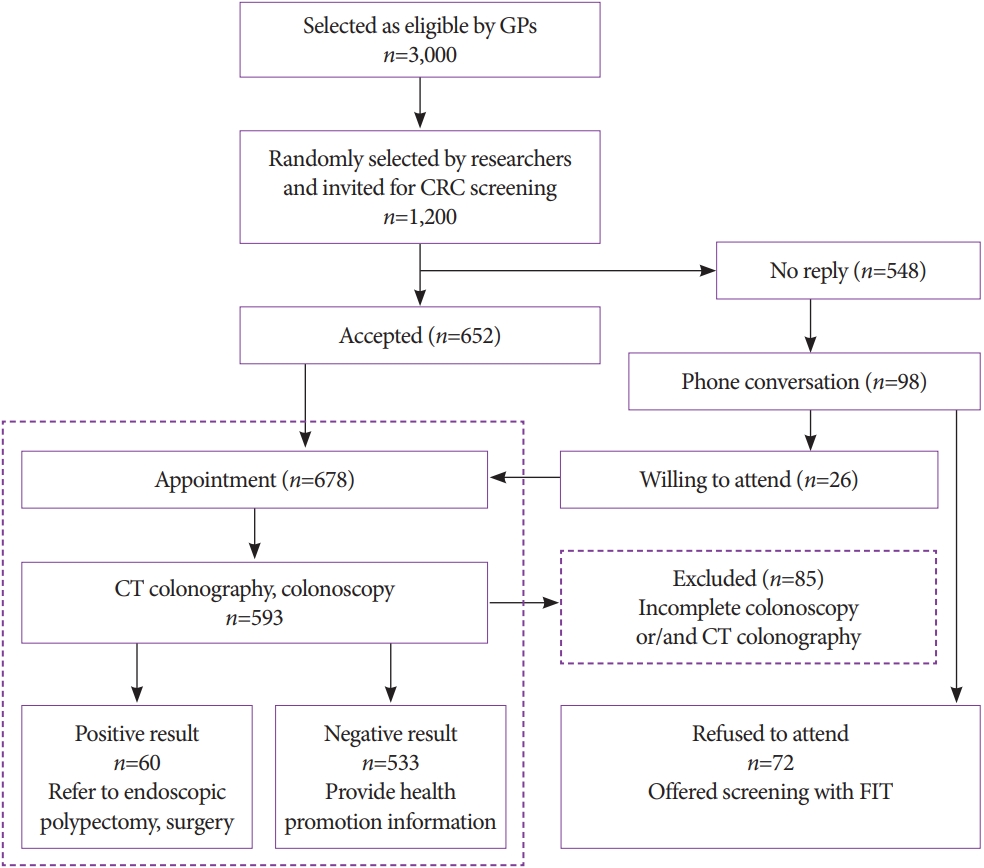
- Colorectal Cancer Screening with Computed Tomography Colonography: Single Region Experience in Kazakhstan
- Jandos Amankulov, Dilyara Kaidarova, Zhamilya Zholdybay, Marianna Zagurovskaya, Nurlan Baltabekov, Madina Gabdullina, Akmaral Ainakulova, Dias Toleshbayev, Alexandra Panina, Elvira Satbayeva, Zhansaya Kalieva
- Clin Endosc 2022;55(1):101-112. Published online July 15, 2021
- DOI: https://doi.org/10.5946/ce.2021.066
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: The aim of our study was to determine the efficacy of computed tomography colonography (CTC) in screening for colorectal cancer (CRC).
Methods
A total of 612 females and 588 males aged 45 to 75 years were enrolled in CTC screening. CTC was performed following standard bowel preparation and colonic insufflation with carbon dioxide. The main outcomes were the detection rate of CRC and advanced adenoma (AA), prevalence of colorectal lesions in relation to socio-demographic and health factors, and overall diagnostic performance of CTC.
Results
Overall, 56.5% of the 1,200 invited subjects underwent CTC screening. The sensitivity for CRC and AA was 0.89 and 0.97, respectively, while the specificity was 0.71 and 0.99, respectively. The prevalence of CRC and AA was 3.0% (18/593) and 7.1% (42/593), respectively, with the highest CRC prevalence in the 66-75 age group (≥12 times; odds ratio [OR], 12.11; 95% confidence interval [CI], 4.45-32.92). CRC and AA prevalence were inversely correlated with Asian descent, physical activity, and negative fecal immunochemical test results (OR=0.43; 95% CI, 0.22-0.83; OR=0.16; 95% CI, 0.04-0.68; OR=0.5; 95% CI, 0.07-3.85, respectively).
Conclusions
Our study revealed high accuracy of CTC in diagnosing colonic neoplasms, good compliance with CTC screening, and high detection rate of CRC.
- 5,707 View
- 205 Download
- 1 Web of Science

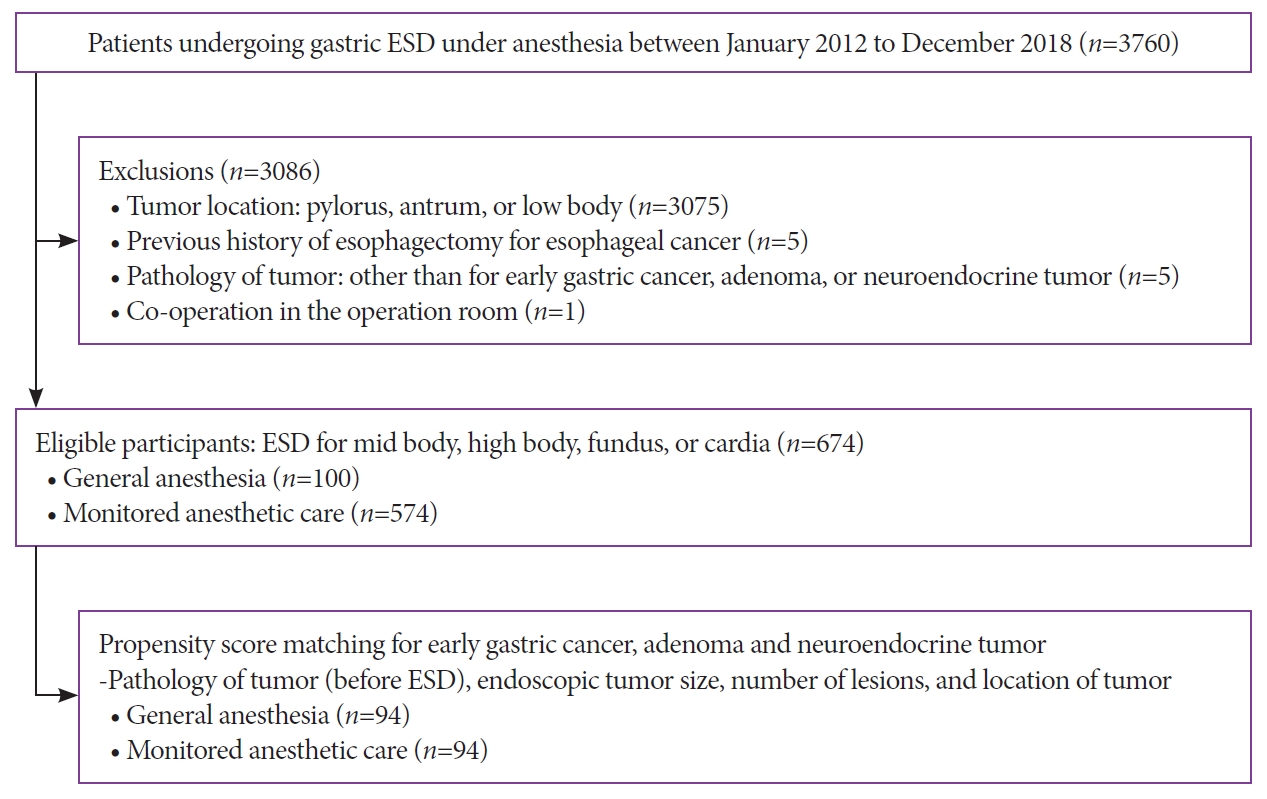
- Clinical Outcomes and Adverse Events of Gastric Endoscopic Submucosal Dissection of the Mid to Upper Stomach under General Anesthesia and Monitored Anesthetic Care
- Jong-In Chang, Tae Jun Kim, Na Young Hwang, Insuk Sohn, Yang Won Min, Hyuk Lee, Byung-Hoon Min, Jun Haeng Lee, Poong-Lyul Rhee, Jae J Kim
- Clin Endosc 2022;55(1):77-85. Published online July 5, 2021
- DOI: https://doi.org/10.5946/ce.2021.002
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic submucosal dissection (ESD) of gastric tumors in the mid-to-upper stomach is a technically challenging procedure. This study compared the therapeutic outcomes and adverse events of ESD of tumors in the mid-to-upper stomach performed under general anesthesia (GA) or monitored anesthesia care (MAC).
Methods
Between 2012 and 2018, 674 patients underwent ESD for gastric tumors in the midbody, high body, fundus, or cardia (100 patients received GA; 574 received MAC). The outcomes of the propensity score (PS)-matched (1:1) patients receiving either GA or MAC were analyzed.
Results
The PS matching identified 94 patients who received GA and 94 patients who received MAC. Both groups showed high rates of en bloc resection (GA, 95.7%; MAC, 97.9%; p=0.68) and complete resection (GA, 81.9%; MAC, 84.0%; p=0.14). There were no significant differences between the rates of adverse events (GA, 16.0%; MAC, 8.5%; p=0.18) in the anesthetic groups. Logistic regression analysis indicated that the method of anesthesia did not affect the rates of complete resection or adverse events.
Conclusions
ESD of tumors in the mid-to-upper stomach at our high-volume center had good outcomes, regardless of the method of anesthesia. Our results demonstrate no differences between the efficacies and safety of ESD performed under MAC and GA. -
Citations
Citations to this article as recorded by- General Anesthesia and Endoscopic Upper Gastrointestinal Tumor Resection
Seung Hyun Kim
Journal of Digestive Cancer Research.2023; 11(3): 125. CrossRef - Is General Anesthesia Needed in Endoscopic Submucosal Dissection for Lesions Located in the Mid to Upper Stomach?
Prasit Mahawongkajit, Jirawat Swangsri
Clinical Endoscopy.2022; 55(1): 43. CrossRef - Therapeutic approach to non-curative resection after endoscopic treatment in early gastric cancer
Eun Jeong Gong, Chang Seok Bang
Journal of the Korean Medical Association.2022; 65(5): 284. CrossRef - Paneth Cell Carcinoma of the Stomach
Jun Wan Kim, Gwang Ha Kim, Kyung Bin Kim
The Korean Journal of Gastroenterology.2022; 80(1): 34. CrossRef - Comparing Different Anesthesia Methods on Anesthetic Effect and Postoperative Pain in Patients with Early Gastric Cancer during Endoscopic Submucosal Dissection
Jie Zhang, Yanlei Chen, Zhiwu Liu, Zhihao Pan, Jinghua Pan
Journal of Oncology.2022; 2022: 1. CrossRef
- General Anesthesia and Endoscopic Upper Gastrointestinal Tumor Resection
- 3,709 View
- 173 Download
- 5 Web of Science
- 5 Crossref

Focused Review Series: Recent Updates on the Role of EUS in Pancreatobiliary Disease
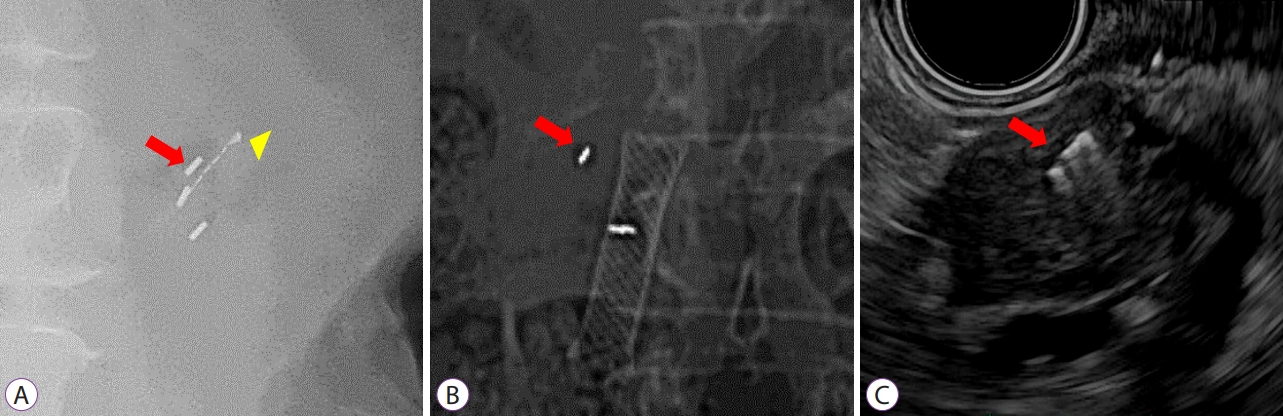
- Endoscopic Ultrasound–Guided Fiducial Placement for Stereotactic Body Radiation Therapy in Pancreatic Malignancy
- Seong-Hun Kim, Eun Ji Shin
- Clin Endosc 2021;54(3):314-323. Published online May 28, 2021
- DOI: https://doi.org/10.5946/ce.2021.102
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Stereotactic body radiation therapy (SBRT) is an important treatment option for pancreatic cancer, which is known to be one of the malignancies with the worst prognosis. However, the high radiation doses delivered during SBRT may cause damage to adjacent radiosensitive organs. To minimize such damage, fiducial markers are used for localization during SBRT for pancreatic cancer. The development of endoscopic ultrasound (EUS) has enabled fiducial markers to be inserted into the pancreas using an EUS fine-needle aspiration (FNA) needle, unlike in the past when percutaneous placement was generally performed. For successful EUS-guided fiducial marker placement, it is necessary for the fiducial markers to be loaded within the EUS-FNA needles to have a low probability of complications and a low migration risk, and to be stably observed in SBRT imaging. A systematic review has shown that the technical success rate of EUS-guided fiducial marker placement is 96.27%, whereas the fiducial marker migration and adverse event rates are 4.33% and 4.85%, respectively. Nonetheless, standardized techniques for fiducial marker placement and the characteristics of optimal fiducial markers have not yet been established. This review will introduce the characteristics (e.g., materials and shapes) of fiducial markers used in fiducial marker placement for pancreatic cancer and will discuss conventional techniques along with their success rates, difficulties, and adverse events.
-
Citations
Citations to this article as recorded by- EUS-guided interventional therapies for pancreatic diseases
Rongmin Xu, Kai Zhang, Nan Ge, Siyu Sun
Frontiers in Medicine.2024;[Epub] CrossRef - Cardiac migration of an implanted hepatic fiducial marker used for stereotactic body radiation therapy - A case report
Youstina Soliman, Febin Antony, Mark Vivian, Sankar Venkatraman, Maged Nashed
Journal of Cancer Research and Therapeutics.2024;[Epub] CrossRef - Development of devices for interventional endoscopic ultrasound for the management of pancreatobiliary diseases
Masahiro Itonaga, Masayuki Kitano, Reiko Ashida
Digestive Endoscopy.2023; 35(3): 302. CrossRef - Endoscopic Ultrasound-Guided Fiducial Placement for Stereotactic Body Radiation Therapy in Patients with Pancreatic Cancer
Irina M. Cazacu, Ben S. Singh, Rachael M. Martin-Paulpeter, Sam Beddar, Stephen Chun, Emma B. Holliday, Albert C. Koong, Prajnan Das, Eugene J. Koay, Cullen Taniguchi, Joseph M. Herman, Manoop S. Bhutani
Cancers.2023; 15(22): 5355. CrossRef - A Preliminary Controlled Trial of Endoscopic Ultrasound-guided Fiducial Markers to Guide Pancreas Surgery
Patrick W. Chang, Jonathan Sadik, Ara B. Sahakian, Ravi Kankotia, Christopher Ko, Jessica Serna, Alex Rodriguez, Helen Lee, Sujit Kulkarni, Yuri Genyk, Mohd Sheikh, James L. Buxbaum
Journal of Clinical Gastroenterology.2023;[Epub] CrossRef - Endoscopic Management of Pancreatobiliary Malignancies
Dong Wook Lee, Eun Young Kim
Digestive Diseases and Sciences.2022; 67(5): 1635. CrossRef - Hot topics in therapeutic EUS
Daniela Tabacelia, Alexandru Martiniuc, DanielaElena Burtea, Adrian Saftoiu, Cezar Stroescu
Endoscopic Ultrasound.2022; 11(3): 153. CrossRef
- EUS-guided interventional therapies for pancreatic diseases
- 4,357 View
- 191 Download
- 6 Web of Science
- 7 Crossref

Review
- Current Status of Colorectal Cancer and Its Public Health Burden in Thailand
- Kasenee Tiankanon, Satimai Aniwan, Rungsun Rerknimitr
- Clin Endosc 2021;54(4):499-504. Published online March 15, 2021
- DOI: https://doi.org/10.5946/ce.2020.245-IDEN

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Colorectal cancer (CRC) accounts for approximately 10.3% of new cancer cases in Thailand and is currently the 3rd most prevalent cancer found among the Thai population. Starting in 2017, the Thai government announced the national CRC screening program as a response to this important issue. Among the 70 million people currently residing in Thailand, 14 million require screening, while there are approximately a total of 1,000 endoscopists available to perform colonoscopy. Due to the limited resources and shortage of endoscopists in Thailand, applying a population-based one-step colonoscopy program as a primary screening method is not feasible. To reduce colonoscopy workload, with the help of others, including village health volunteers, institution-based health personnel, reimbursement coders, pathologists, and patients due for CRC screening, a two-step approach of one-time fecal immunochemical test (FIT), which prioritizes and filters out subjects for colonoscopy, is chosen. Moreover, additional adjustments to the optimal FIT cutoff value and the modified Asia-Pacific Colorectal Screening risk score, including body weight, were proposed to stratify the priority of colonoscopy schedule. This article aims to give an overview of the past and current policy developmental strategies and the current status of the Thailand CRC screening program.
-
Citations
Citations to this article as recorded by- Integrated Care Model by the Village Health Volunteers to Prevent and Slow down Progression of Chronic Kidney Disease in a Rural Community, Thailand
Ampornpan Theeranut, Nonglak Methakanjanasak, Sunee Lertsinudom, Pattama Surit, Nichanun Panyaek, Saisamon Leeladapattarakul, Peangtikumporn Nilpetch, Pattapong Kessomboon, Chalongchai Chalermwat, Watcharapong Rintara, Wudipong Khongtong, Pawich Paktipat,
Journal of Primary Care & Community Health.2024;[Epub] CrossRef - Dynamics of colorectal cancer screening in low and middle-income countries: A modeling analysis from Thailand
Peeradon Wongseree, Zeynep Hasgul, Borwornsom Leerapan, Cherdsak Iramaneerat, Pochamana Phisalprapa, Mohammad S. Jalali
Preventive Medicine.2023; 175: 107694. CrossRef - An Assessment of Physicians’ Recommendations for Colorectal Cancer Screening and International Guidelines Awareness and Adherence: Results From a Thai National Survey
Nonthalee Pausawasdi, Pongkamon Tongpong, Tanawat Geeratragool, Phunchai Charatcharoenwitthaya
Frontiers in Medicine.2022;[Epub] CrossRef - Cytotoxic effect of metformin on butyrate-resistant PMF-K014 colorectal cancer spheroid cells
Kesara Nittayaboon, Kittinun Leetanaporn, Surasak Sangkhathat, Sittirak Roytrakul, Raphatphorn Navakanitworakul
Biomedicine & Pharmacotherapy.2022; 151: 113214. CrossRef
- Integrated Care Model by the Village Health Volunteers to Prevent and Slow down Progression of Chronic Kidney Disease in a Rural Community, Thailand
- 5,166 View
- 168 Download
- 5 Web of Science
- 4 Crossref

Case Report
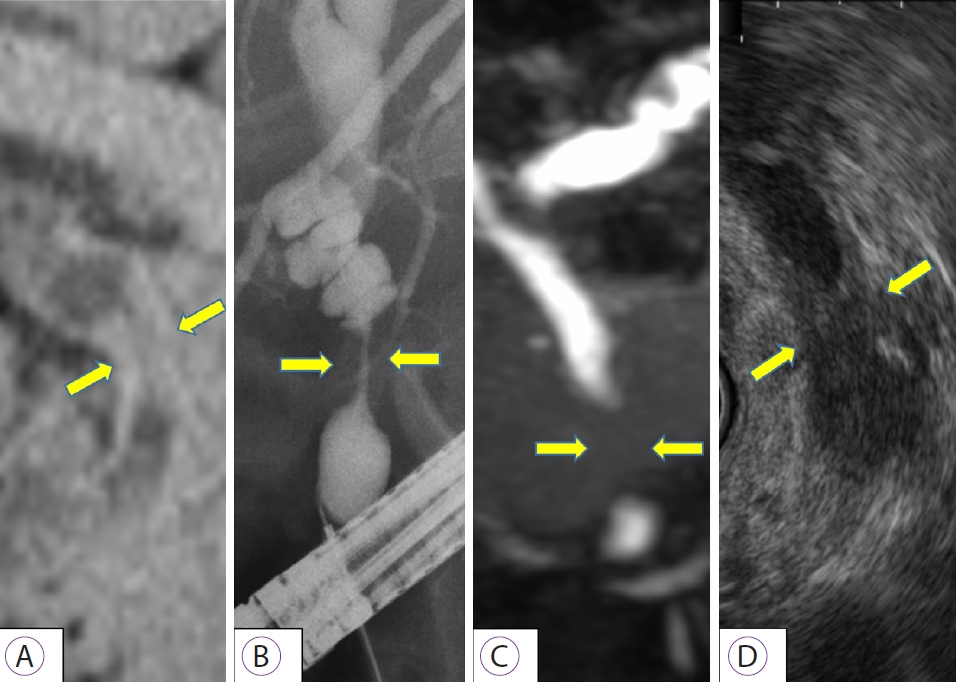
- High-Resolution Probe-Based Confocal Laser Endomicroscopy for Diagnosing Biliary Diseases
- Hiroki Koda, Kazuo Hara, Okuno Nozomi, Takamichi Kuwahara, Mizuno Nobumasa, Shin Haba, Miyano Akira, Isomoto Hajime
- Clin Endosc 2021;54(6):924-929. Published online March 15, 2021
- DOI: https://doi.org/10.5946/ce.2020.191
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Probe-based confocal laser endomicroscopy is an endoscopic technique that enables in vivo histological evaluation using fluorescent pigment. The ability to diagnostically differentiate between benign and malignant biliary disease using the “CholangioFlexTM”, a dedicated biliary device, has been reported. However, the Miami and Paris classifications, used as diagnostic criteria, mainly evaluate findings in the submucosa, and visualizing the epithelium as the main site of lesions remains difficult. To address this problem, we verified the imaging findings and diagnostic ability of three types of probes: CholangioFlexTM, GastroFlexTM, and AlveoFlexTM. With GastroFlexTM, the clear mucosal epithelium was observed, and differential diagnoses as benign/malignant could be made based on epithelial findings. GastroFlexTM may be a good first-choice probe for probe-based confocal laser endomicroscopy of biliary diseases, and a new diagnostic classification based on bile duct epithelial findings may provide useful criteria independent of the Miami or Paris classifications.
- 3,700 View
- 63 Download
- 1 Web of Science


 KSGE
KSGE


 First
First Prev
Prev



