Search
- Page Path
- HOME > Search
- Quality indicators in endoscopic retrograde cholangiopancreatography: a brief review of established guidelines
- Zubin Dev Sharma, Rajesh Puri
- Clin Endosc 2023;56(3):290-297. Published online April 11, 2023
- DOI: https://doi.org/10.5946/ce.2022.210
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) is an invasive endoscopic technique that has many diagnostic and therapeutic implications. It is a procedure with small but significant life-threatening complications. To ensure the best possible care, minimize complications, and improve the quality of health care, a constant review of the performance of the operator using ideal benchmark standards is needed. Hence, quality indicators are necessary. The American and European Societies of Gastrointestinal Endoscopy have provided guidelines on quality measures for ERCP, which describe the skills to be developed and training to be implemented in performing quality ERCP. These guidelines have divided the indicators into pre-procedure, intraprocedural, and post-procedure measures. The focus of this article was to review the quality indicators of ERCP.
-
Citations
Citations to this article as recorded by- Advancements in Research on Challenges in Selective Biliary Cannulation during Endoscopic Retrograde Cholangiopancreatography (ERCP)
天雨 张
Journal of Clinical Personalized Medicine.2024; 03(01): 100. CrossRef - Development of an Automated Endoscopic Retrograde Cholangiopancreatography Quality Report Card Using an Integrated Analytics Suite
Anmol Singh, Eric Swei, Celestina Tolosa, Matthew Alverson, Todd A. Brenner, Avleen Kaur, Aida Metri, Mohammed Rifat Shaik, Nikhil Bush, Branislav Bujnak, Alexandra T. Strauss, Mouen Khashab, Eun Ji Shin, Vikesh K. Singh, Venkata S. Akshintala
Techniques and Innovations in Gastrointestinal Endoscopy.2024;[Epub] CrossRef - Validity of a virtual reality endoscopic retrograde cholangiopancreatography simulator: can it distinguish experts from novices?
Konstantinos Georgiou, Nikola Boyanov, Pantelis Antonakis, Dimitrios Thanasas, Gabriel Sandblom, Lars Enochsson
Frontiers in Surgery.2023;[Epub] CrossRef
- Advancements in Research on Challenges in Selective Biliary Cannulation during Endoscopic Retrograde Cholangiopancreatography (ERCP)
- 2,241 View
- 181 Download
- 1 Web of Science
- 3 Crossref

- COVID-19 Rapid Antigen Test: Role in Screening Prior to Gastrointestinal Endoscopy
- Ashok Dalal, Ujjwal Sonika, Manish Kumar, Roshan George, Ajay Kumar, Siddharth Srivastava, Sanjeev Sachdeva, Barjesh Chander Sharma
- Clin Endosc 2021;54(4):522-525. Published online March 4, 2021
- DOI: https://doi.org/10.5946/ce.2020.295
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
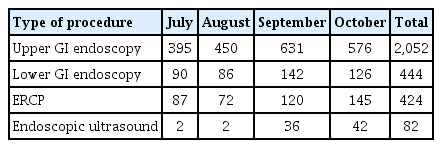
/Aims: The severe acute respiratory syndrome coronavirus 2 pandemic has affected the gastrointestinal (GI) endoscopy units globally owing to the risk of transmission. We present our data on the use of rapid antigen test (RAT) as a screening tool prior to endoscopy to prevent the transmission of coronavirus disease (COVID-19).
Methods
This study was a retrospective analysis of patients who underwent any GI endoscopic procedure from July 2020 to October 2020 at a tertiary referral center in New Delhi, India. All patients underwent screening for COVID-19 using RAT, and endoscopy was performed only when the RAT was negative. The data are presented as numbers and percentages.
Results
A total of 3,002 endoscopic procedures were performed during the study period. Only one endoscopic procedure was performed in a COVID-19 positive patient. A total of 53 healthcare workers were involved in conducting these procedures. Only 2 healthcare workers (3.8%) were diagnosed COVID-19 positive, presumably due to community-acquired infection, during this period.
Conclusions
The COVID-19 RAT is easily usable as a simple screening tool prior to GI endoscopy during the COVID-19 pandemic. -
Citations
Citations to this article as recorded by- Intestinal Damage, Inflammation and Microbiota Alteration during COVID-19 Infection
Angela Saviano, Mattia Brigida, Carmine Petruzziello, Christian Zanza, Marcello Candelli, Maria Rita Morabito Loprete, Faiz Saleem, Veronica Ojetti
Biomedicines.2023; 11(4): 1014. CrossRef - SARS-CoV-2 (COVID-19) pneumonia patient treated with two doses of infliximab within 2 weeks for acute severe ulcerative colitis
Marouf Alhalabi, Kamal Alaa Eddin, Fadwa Ali, Ahmad Abbas
Medicine.2022; 101(4): e28722. CrossRef - Current Status of Screening Clinic due to Changes in the Reimbursement Criteria for COVID-19 Polymerase Chain Reaction Test: Case of a Hospital in Seoul
Song Lee Kim
Health Insurance Review & Assessment Service Research.2022; 2(1): 138. CrossRef - Rapid, point-of-care antigen tests for diagnosis of SARS-CoV-2 infection
Jacqueline Dinnes, Pawana Sharma, Sarah Berhane, Susanna S van Wyk, Nicholas Nyaaba, Julie Domen, Melissa Taylor, Jane Cunningham, Clare Davenport, Sabine Dittrich, Devy Emperador, Lotty Hooft, Mariska MG Leeflang, Matthew DF McInnes, René Spijker, Jan Y
Cochrane Database of Systematic Reviews.2022;[Epub] CrossRef - Risk-based decision-making related to preprocedural coronavirus disease 2019 testing in the setting of GI endoscopy: management of risks, evidence, and behavioral health economics
Naomi Moy, Uwe Dulleck, Ayesha Shah, Helmut Messmann, Aaron P. Thrift, Nicholas J. Talley, Gerald J. Holtmann
Gastrointestinal Endoscopy.2022; 96(5): 735. CrossRef
- Intestinal Damage, Inflammation and Microbiota Alteration during COVID-19 Infection
- 5,448 View
- 129 Download
- 6 Web of Science
- 5 Crossref

- Technical Reports of Endoscopic Retrograde Cholangiopancreatography Guidewires on the Basis of Physical Properties
- Chang-Il Kwon, Dong Hee Koh, Tae Jun Song, Won Suk Park, Dong Hang Lee, Seok Jeong
- Clin Endosc 2020;53(1):65-72. Published online August 6, 2019
- DOI: https://doi.org/10.5946/ce.2019.114
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
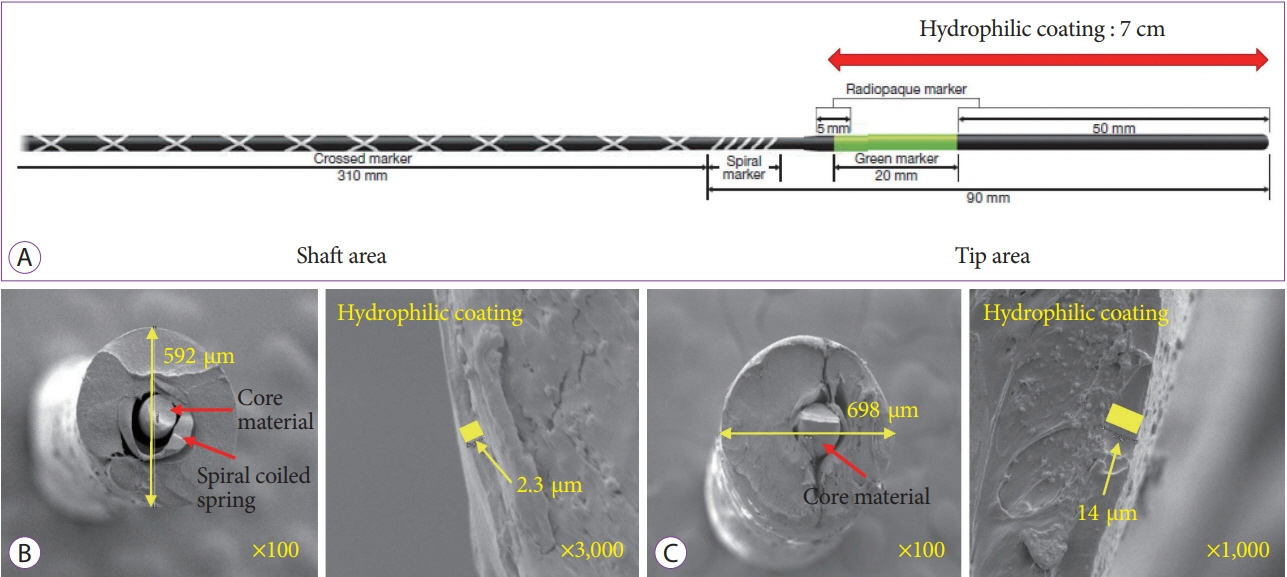
/Aims: Using an appropriate guidewire can increase the success rate of selective cannulation in endoscopic retrograde cholangiopancreatography. The purpose of this technical study was to investigate the characteristics of each guidewire type and to evaluate its efficiency and rapidity of insertion.
Methods
We conducted a three-point bending test using a universal testing machine to investigate the flexibility and bending features of each guidewire. 3D-printed silicone tubes with various types of stricture and a hand-made biliary tree silicone model with six-stranded intrahepatic ducts were used to evaluate the success rate and insertion time of each guidewire.
Results
In the three-point bending test, the characteristics of each guidewire were classified. We found that the bending strengths and times were independent of shaft thickness. Using two in vitro biliary duct models, we determined that the success rate and total insertion time were better for guidewires with a resilient shaft and angled tip than for other types of guidewires (p<0.001). Although thickness of the guidewire affected the success rate (p<0.05), it did not affect the total insertion time (p≥0.05).
Conclusions
Among several types of guidewire, some factors (resilient shaft, highly flexible, and angled tip) appeared to be associated with the efficiency and rapidity of the guidewire insertion. -
Citations
Citations to this article as recorded by- Structural factors influencing the clinical performance of 0.025-inch guidewires for pancreatobiliary endoscopy: An experimental study
Takehiko Koga, Naoaki Tsuchiya, Yusuke Ishida, Takanori Kitaguchi, Keisuke Matsumoto, Makoto Fukuyama, Satoki Kojima, Norihiro Kojima, Fumihito Hirai
Endoscopy International Open.2024; 12(05): E666. CrossRef - Guidewire Impaction in the Main Pancreatic Duct in a Patient with Chronic Pancreatitis: A Case Report
Soyoung Kim, Hoonsub So, Seok Won Jung, Sung Jo Bang
The Korean Journal of Gastroenterology.2023; 81(1): 36. CrossRef - Efficacy of a newly developed guidewire for selective biliary access
Do Hyun Park, Joung-Ho Han, Tae Hoon Lee, Jae Kook Yang, Ji Sung Lee, Yong Hun Lee, Mamoru Takenaka, Sang-Heum Park
Scientific Reports.2023;[Epub] CrossRef - Efficacy of a Newly Developed Guidewire for Selective Biliary Cannulation: A Multicenter Randomized Controlled Trial
Sung Yong Han, Sung Ill Jang, Dong Hee Koh, Jong Hyun Lee, Dong Uk Kim, Jae Hee Cho, Kyong Joo Lee, Seong-Hun Kim, Min Je Sung, Chang-Il Kwon
Journal of Clinical Medicine.2023; 12(10): 3440. CrossRef - Comparison of Two Types of Guidewires for Malignant Hilar Biliary Obstruction by Endoscopic Retrograde Cholangiopancreatography: A Randomized Controlled Trial
Sung Yong Han, Jung Wan Choe, Dong Uk Kim, Jong Jin Hyun, Joung-Ho Han, Hoonsub So, Sung Jo Bang, Dong Hee Koh, Seok Jeong
Journal of Clinical Medicine.2023; 12(10): 3590. CrossRef - Comparison of guidewires for successful cannulation of biliary stenosis and targeting of biliary branches in ERCP
Masanori Kobayashi, Hiromune Katsuda, Kazuo Ohtsuka, Ryuichi Okamoto
Endoscopy International Open.2023; 11(09): E805. CrossRef - Impact of guidewire caliber on ERCP outcomes: Systematic review and meta-analysis comparing 0.025- and 0.035-inch guidewires
Muhammad Aziz, Amna Iqbal, Zohaib Ahmed, Saad Saleem, Wade Lee-Smith, Hemant Goyal, Faisal Kamal, Yaseen Alastal, Ali Nawras, Douglas G. Adler
Endoscopy International Open.2022; 10(07): E990. CrossRef - Experimental study of loop shape using 0.025-inch ERCP guidewires (with videos)
Takeshi Ogura, Saori Ueno, Atsushi Okuda, Nobu Nishioka, Tadahiro Yamada, Masanori Yamada, Kazuya Ueshima, Jun Matsuno, Yoshitaro Yamamoto, Kazuhide Higuchi
Endoscopy International Open.2021; 09(03): E427. CrossRef - Technical Review of Developments in Endoscopic Ultrasound-Guided Hepaticogastrostomy
Takeshi Ogura, Kazuhide Higuchi
Clinical Endoscopy.2021; 54(5): 651. CrossRef - Difficult Biliary Cannulation in Endoscopic Retrograde Cholangiopancreatography: Definitions, Risk Factors, and Implications
Brian M. Fung, Teodor C. Pitea, James H. Tabibian
EMJ Hepatology.2021; : 64. CrossRef - Production of ERCP training model using a 3D printing technique (with video)
Chang-Il Kwon, Yeonsun Shin, Jaeok Hong, Minje Im, Guk Bae Kim, Dong Hee Koh, Tae Jun Song, Won Suk Park, Jong Jin Hyun, Seok Jeong
BMC Gastroenterology.2020;[Epub] CrossRef - Clinical Evaluation of a Newly Developed Guidewire for Pancreatobiliary Endoscopy
Shigeto Ishii, Toshio Fujisawa, Hiroyuki Isayama, Shingo Asahara, Shingo Ogiwara, Hironao Okubo, Hisafumi Yamagata, Mako Ushio, Sho Takahashi, Hiroki Okawa, Wataru Yamagata, Yoshihiro Okawa, Akinori Suzuki, Yusuke Takasaki, Kazushige Ochiai, Ko Tomishima,
Journal of Clinical Medicine.2020; 9(12): 4059. CrossRef
- Structural factors influencing the clinical performance of 0.025-inch guidewires for pancreatobiliary endoscopy: An experimental study
- 6,555 View
- 308 Download
- 10 Web of Science
- 12 Crossref

- Impact of Periampullary Diverticulum on ERCP Performance: A Matched Case-Control Study
- Juan E. Corral, Omar Y. Mousa, Paul T. Kröner, Victoria Gomez, Frank J. Lukens
- Clin Endosc 2019;52(1):65-71. Published online August 21, 2018
- DOI: https://doi.org/10.5946/ce.2018.070

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Periampullary diverticulum (PAD) is frequently encountered during endoscopic retrograde cholangiopancreatography (ERCP) and has been associated with stone formation in the bile duct. The effects of PAD on the ERCP procedure have been often debated. We aimed to compare the therapeutic success of ERCP between patients with PAD and matched controls.
Methods
We reviewed all ERCPs with findings of PAD in a national database (n=1,089) and compared them with age- and gendermatched controls in a 1:3 fashion (n=3,267). Demographics, endoscopic findings, visualization of main structures, and therapeutic success rates were compared between groups. Secondary analysis compared PAD cases and controls who had gallstone disease.
Results
The average cohort age was 68.4±14.3 years and 55.1% were male. ERCP success was similar in both groups, and no significant inter-group differences were found in the multivariate analysis. The presence of PAD did not affect the rates of sphincterotomy or visualization of main biliary structures. Secondary analysis showed similar success rates for gallstone removal between patients with PAD and controls.
Conclusions
PAD may not be considered a hinderance to ERCP success. Further research is needed to determine the best approach to cannulate the ampulla and provide endoscopic therapy for different subtypes of PAD. -
Citations
Citations to this article as recorded by- Impact of periampullary diverticulum on biliary cannulation: A retrospective cohort study
Jing Liang Ho, Aruni Seneviratna, Cherng Hann Benjamin Yip
Advances in Digestive Medicine.2023; 10(4): 232. CrossRef - A new classification of periampullary diverticulum: cannulation of papilla on the inner margins of the diverticulum (Type IIa) is more challenging
He-xian Shi, Yong-qiang Ye, Hai-wang Zhao, De-cai Kong, Shan-zhou Huang, Qian Yan, Yu-bin Chen, Ping Zhang, Sheng Chen, Bao-hua Hou, Chuan-zhao Zhang
BMC Gastroenterology.2023;[Epub] CrossRef - Clinical significance of different periampullary diverticulum classifications for endoscopic retrograde cholangiopancreatography cannulation
Ping Yue, Ke-Xiang Zhu, Hai-Ping Wang, Wen-Bo Meng, Jian-Kang Liu, Lei Zhang, Xiao-Liang Zhu, Hui Zhang, Long Miao, Zheng-Feng Wang, Wen-Ce Zhou, Azumi Suzuki, Kiyohito Tanaka, Xun Li
World Journal of Gastroenterology.2020; 26(19): 2402. CrossRef - Clinical significance of different periampullary diverticulum classifications for endoscopic retrograde cholangiopancreatography cannulation
Ping Yue, Ke-Xiang Zhu, Hai-Ping Wang, Wen-Bo Meng, Jian-Kang Liu, Lei Zhang, Xiao-Liang Zhu, Hui Zhang, Long Miao, Zheng-Feng Wang, Wen-Ce Zhou, Azumi Suzuki, Kiyohito Tanaka, Xun Li
World Journal of Gastroenterology.2020; 26(19): 2403. CrossRef - Periampüller divertikül endoskopik retrograd kolanjiyopankreatografide kanülasyon başarısı ve komplikasyon sıklığını etkiler mi?
Bilal TOKA, Salih TOKMAK
Akademik Gastroenteroloji Dergisi.2020; 19(2): 83. CrossRef - Complications increase in which type of duodenal diverticulum? A retrospective cohort study
Murat AKAYDIN, Tamer AKAY, Metin LEBLEBİCİ
Journal of Surgery and Medicine.2020; 4(11): 938. CrossRef - Presence of Periampullary Diverticulum is Not a Hurdle to Successful Endoscopic Retrograde Cholangiopancreatography
Jimin Han
Clinical Endoscopy.2019; 52(1): 7. CrossRef - ERCP Success Rate and Periampullary Diverticula: The Pocket Makes No Difference
Gyanprakash Ketwaroo, Waqar Qureshi
Digestive Diseases and Sciences.2019; 64(5): 1072. CrossRef
- Impact of periampullary diverticulum on biliary cannulation: A retrospective cohort study
- 5,007 View
- 151 Download
- 6 Web of Science
- 8 Crossref

- Papillary Cannulation Facilitated by Submucosal Saline Injection into an Intradiverticular Papilla
- Kanglock Lee, Ji Wook Choi, Yunhyeong Lee, Joung-Ho Han, Seon Mee Park
- Clin Endosc 2019;52(1):83-86. Published online June 12, 2018
- DOI: https://doi.org/10.5946/ce.2018.060

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) of the intradiverticular papilla with its invisible orifice remains challenging. Several techniques have been introduced to evert the papillary opening to facilitate cannulation. A 79-year-old woman with bile duct stones underwent ERCP, which revealed that the papilla was located inside a large diverticulum and tended to rotate inward with a trial of papillary cannulation. Submucosal papillary injection of 3 cc of normal saline was performed at 3 and 9 o’clock. Eversion and fixation of a papilla in the diverticulum with this technique allowed selective cannulation of the biliary tree. Stones were retrieved after endoscopic papillary balloon dilation without complications. She had an uneventful post-procedural course. Our findings suggest that submucosal saline injection technique is safe and effective for selective cannulation and can be recommended when cannulation is very difficult because of an intradiverticular papilla.
-
Citations
Citations to this article as recorded by- Two-devices-in-one-channel method: a challenging cannulation of intradiverticular major papilla
Renato Medas, Eduardo Rodrigues-Pinto, Pedro Pereira, Guilherme Macedo
VideoGIE.2024; 9(3): 141. CrossRef - A “One Accessory and One Guidewire-in-One Channel” Technique in a Patient with Billroth II Anastomosis
Kook Hyun Kim, Sung Bum Kim, Tae Nyeun Kim
Clinical Endoscopy.2021; 54(1): 139. CrossRef - Difficult Biliary Cannulation in Endoscopic Retrograde Cholangiopancreatography: An Overview of Advanced Techniques
Brian M. Fung, Teodor C. Pitea, James H. Tabibian
EMJ Hepatology.2021; : 73. CrossRef - Make mission impossible successful: clip-with-line traction facilitates difficult pancreatic duct cannulation in a patient with duodenal duplication
Wei-hui Liu, Zhao-shen Li, Dong Wang
Endoscopy.2020; 52(09): E346. CrossRef
- Two-devices-in-one-channel method: a challenging cannulation of intradiverticular major papilla
- 6,393 View
- 213 Download
- 2 Web of Science
- 4 Crossref

- Advanced Therapeutic Gastrointestinal Endoscopy in Children – Today and Tomorrow
- Zaheer Nabi, Duvvur Nageshwar Reddy
- Clin Endosc 2018;51(2):142-149. Published online December 12, 2017
- DOI: https://doi.org/10.5946/ce.2017.102
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Gastrointestinal (GI) endoscopy plays an indispensable role in the diagnosis and management of various pediatric GI disorders. While the pace of development of pediatric GI endoscopy has increased over the years, it remains sluggish compared to the advancements in GI endoscopic interventions available in adults. The predominant reasons that explain this observation include lack of formal training courses in advanced pediatric GI interventions, economic constraints in establishing a pediatric endoscopy unit, and unavailability of pediatric-specific devices and accessories. However, the situation is changing and more pediatric GI specialists are now performing complex GI procedures such as endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography for various pancreatico-biliary diseases and more recently, per-oral endoscopic myotomy for achalasia cardia. Endoscopic procedures are associated with reduced morbidity and mortality compared to open surgery for GI disorders. Notable examples include chronic pancreatitis, pancreatic fluid collections, various biliary diseases, and achalasia cardia for which previously open surgery was the treatment modality of choice. A solid body of evidence supports the safety and efficacy of endoscopic management in adults. However, additions continue to be made to literature describing the pediatric population. An important consideration in children includes size of children, which in turn determines the selection of endoscopes and type of sedation that can be used for the procedure.
-
Citations
Citations to this article as recorded by- Endoscopic ultrasound-guided drainage of peripancreatic fluid collections: What impacts treatment duration?
Adam Przybyłkowski, Piotr Nehring
Hepatobiliary & Pancreatic Diseases International.2023; 22(3): 310. CrossRef - Echo-Endoscopy Combined with Virtual Reality: A Whole Perspective of Laparoscopic Common Bile Duct Exploration in Children
Francesca Destro, Raffaele Salerno, Valeria Calcaterra, Sandro Ardizzone, Milena Meroni, Margherita Roveri, Ugo Maria Pierucci, Alberta Zaja, Francesco Rizzetto, Alessandro Campari, Maurizio Vertemati, Paolo Milani, Gloria Pelizzo
Children.2023; 10(4): 760. CrossRef - A National Survey of the Training and Practice Patterns of Practicing Pediatric Advanced Endoscopists in the United States
Christopher Chu, Paul Tran, Christopher Moreau, Jacob A. Mark, Robert E. Kramer, Travis L. Piester
Journal of Pediatric Gastroenterology & Nutrition.2023; 77(3): 407. CrossRef - Endoscopic Ultrasound-guided Hepaticogastrostomy in a Seven-year-old Girl
Shigeto Ishii, Hiroyuki Koga, Hiroaki Saito, Shogo Seo, Mako Ushio, Sho Takahashi, Yusuke Takasaki, Akinori Suzuki, Koichi Ito, Kazushige Ochiai, Ko Tomishima, Toshio Fujisawa, Atsuyuki Yamataka, Shuichiro Shiina, Hiroyuki Isayama
Internal Medicine.2022; 61(23): 3521. CrossRef - Interventional endoscopy for abdominal transplant patients
Tom K. Lin, Maisam Abu-El-Haija, Juan P. Gurria, Michelle Saad, David S. Vitale
Seminars in Pediatric Surgery.2022; 31(3): 151190. CrossRef - Acute recurrent and chronic pancreatitis in children
Mitsuyoshi Suzuki, Kei Minowa, Hiroyuki Isayama, Toshiaki Shimizu
Pediatrics International.2021; 63(2): 137. CrossRef - Evolution in the Practice of Pediatric Endoscopy and Sedation
Conrad B. Cox, Trevor Laborda, J. Matthew Kynes, Girish Hiremath
Frontiers in Pediatrics.2021;[Epub] CrossRef - EUS in Pediatrics: A Multicenter Experience and Review
Travis L. Piester, Quin Y. Liu
Frontiers in Pediatrics.2021;[Epub] CrossRef - The Roles of Endoscopic Ultrasound and Endoscopic Retrograde Cholangiopancreatography in the Evaluation and Treatment of Chronic Pancreatitis in Children
Quin Y. Liu, Roberto Gugig, David M. Troendle, Samuel Bitton, Nishant Patel, David S. Vitale, Maisam Abu‐El‐Haija, Sohail Z. Husain, Veronique D. Morinville
Journal of Pediatric Gastroenterology and Nutrition.2020; 70(5): 681. CrossRef - Genetic Abnormalities in Pancreatitis: An Update on Diagnosis, Clinical Features, and Treatment
Mitsuyoshi Suzuki, Kei Minowa, Satoshi Nakano, Hiroyuki Isayama, Toshiaki Shimizu
Diagnostics.2020; 11(1): 31. CrossRef - Outcome of radiological interventions in pediatric gastrointestinal diseases: A large tertiary center experience
Zaheer Nabi, Jagadeesh R Singh, Arafat Haris, Upender Shava, Radhika Chavan, Duvvur Nageshwar Reddy
JGH Open.2019; 3(2): 140. CrossRef - Choledocholithiasis treated with a pediatric duodenoscope in a neonate
Akihiko Kida, Koichiro Matsuda, Akito Sakai
Digestive Endoscopy.2019; 31(3): 334. CrossRef - INTRALUMINAL ENDOSCOPY IN CHILDREN - PAST, PRESENT, FUTURE
Maksim M. Lokhmatov, T. N. Budkina, V. I. Oldakovsky, A. V. Tupylenko, S. I. Ibragimov
Russian Pediatric Journal.2019; 21(4): 230. CrossRef - Gastrointestinal Polyposis in Pediatric Patients
Suzanne P. MacFarland, Kristin Zelley, Bryson W. Katona, Benjamin J. Wilkins, Garrett M. Brodeur, Petar Mamula
Journal of Pediatric Gastroenterology and Nutrition.2019; 69(3): 273. CrossRef - Endoscopic treatment of chronic pancreatitis in pediatric population: Long‐term efficacy and safety
D Kohoutova, A Tringali, G Papparella, V Perri, I Boškoski, J Hamanaka, G Costamagna
United European Gastroenterology Journal.2019; 7(2): 270. CrossRef - Pancreatic disorders in children: New clues on the horizon
Claudia Della Corte, Simona Faraci, Fabio Majo, Vincenzina Lucidi, Douglas S. Fishman, Valerio Nobili
Digestive and Liver Disease.2018; 50(9): 886. CrossRef
- Endoscopic ultrasound-guided drainage of peripancreatic fluid collections: What impacts treatment duration?
- 6,885 View
- 228 Download
- 14 Web of Science
- 16 Crossref

- Endoscopic Retrograde Cholangiopancreatography in Nonagenarian Patients: Is It Really Safe?
- Zain A Sobani, Daria Yunina, Anna Abbasi, Kevin Tin, Daniel Simkin, Mary Rojas, Yuriy Tsirlin, Ira Mayer, Rabin Rahmani
- Clin Endosc 2018;51(4):375-380. Published online September 18, 2017
- DOI: https://doi.org/10.5946/ce.2017.123
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Literature on the safety of endoscopic retrograde cholangiopancreatography (ERCP) in elderly patients is divided. Based on this we decided to examine the safety of ERCP in nonagenarian patients. Methods: A total of 1,389 patients, with a mean age of 63.94±19.62 years, underwent ERCP during the study period. There were 74 patients aged 90 years or older with a mean age of 92.07±1.8. Logistic regression showed that nonagenarian patients had a significantly increased odds of in-patient mortality (adjusted odds ratio [AOR]=9.6; 95% confidence interval [CI]=4, 23; p≤0.001). Charlson Comorbidity Index (CCI) ≥2 was also an independent predictor of in-patient mortality (AOR=2.4; 95% CI=1.2, 5.2; p=0.021). Age ≥90 was not associated with increased adverse events; however emergency procedures (AOR=2.4; 95% CI=1.5, 4; p<0.001) and CCI ≥2 (AOR=2.6; 95% CI=1.7, 4.0; p<0.001) were more likely to have adverse events. Conclusions: Age ≥90 and CCI ≥2 are independently associated with increased odds of in-patient mortality in patients undergoing ERCP, whereas emergency procedures and CCI ≥2 are associated with an increased adverse event rate. Caution must be exercised when considering ERCP in patients aged ≥90 years and those with a CCI ≥2 -
Citations
Citations to this article as recorded by- Impact of frailty on endoscopic retrograde cholangiopancreatography outcomes in nonagenarians: A United States national experience
Sanket Dhirubhai Basida, Dushyant Singh Dahiya, Muhammad Nadeem Yousaf, Brinda Basida, Bhanu Siva Mohan Pinnam, Manesh Kumar Gangwani, Hassam Ali, Sahib Singh, Yash R Shah, Daksh Ahluwalia, Mihir Prakash Shah, Saurabh Chandan, Neil R Sharma, Shyam Thakkar
World Journal of Gastrointestinal Endoscopy.2024; 16(3): 148. CrossRef - Racial disparities in endoscopic retrograde cholangiopancreatography (ERCP) utilization in the United States: are we getting better?
Dushyant Singh Dahiya, Abhilash Perisetti, Neil Sharma, Sumant Inamdar, Hemant Goyal, Amandeep Singh, Laura Rotundo, Rajat Garg, Chin-I Cheng, Sailaja Pisipati, Mohammad Al-Haddad, Madhusudhan Sanaka
Surgical Endoscopy.2023; 37(1): 421. CrossRef - Endoscopic removal of common bile duct stones in nonagenarians: a tertiary centre experience
Mustafa Jalal, Amaan Khan, Sijjad Ijaz, Mohammed Gariballa, Yasser El-Sherif, Amer Al-Joudeh
Clinical Endoscopy.2023; 56(1): 92. CrossRef - ERCP in patients over 90 years old: Safety and efficacy comparison with a younger cohort
Ana E Colmenero Gargari, Fernando E Melgar Somoza, Jorge Vera, Carlos G Micames
Endoscopy International Open.2023; 11(09): E893. CrossRef - ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY FOR THE MANAGEMENT OF CHOLEDOCHOLITHIASIS IN OLDER PATIENTS
Júlia Gardenyes, Pere Roura, Helena Vallverdú-Cartie, Judit Hermoso-Bosch, Cl�udia Roca, Mariona Espaulella, Antoni Casals, Héctor Ivo Marani, Joan Saló, Martín Galdín, Marta Gallach, Carles Leal
Revista Española de Enfermedades Digestivas.2023;[Epub] CrossRef - Safety and Efficacy of Endoscopic Retrograde Cholangiopancreatography in Nonagenarians: A Systematic Review and Meta-Analysis
Umair Iqbal, Hafsa Anwar, Muhammad Ali Khan, Simcha Weissman, Shivangi T. Kothari, Truptesh H. Kothari, Bradley D. Confer, Harshit S. Khara
Digestive Diseases and Sciences.2022; 67(4): 1352. CrossRef - Safety of Nonagenarians Receiving Therapeutic ERCP, Single Center Experience
Chia-Chang Chen, Wan-Tzu Lin, Chun-Fang Tung, Shou-Wu Lee, Chi-Sen Chang, Yen-Chun Peng
Journal of Clinical Medicine.2022; 11(17): 5197. CrossRef - Long-term Outcomes of Therapeutic Endoscopic Retrograde Cholangiopancreatography for Choledocholithiasis in Patients ≥90 Years Old: A Multicenter Retrospective Study
Shinya Sugimoto, Aiji Hattori, Yuri Maegawa, Haruka Nakamura, Naoko Okuda, Toshifumi Takeuchi, Jun Oyamada, Akira Kamei, Hiroyuki Kawabata, Masatoshi Aoki, Hiroaki Naota
Internal Medicine.2021; 60(13): 1989. CrossRef - Complications of common bile duct stones: A risk factors analysis
Dong Jun Oh, Ji Hyung Nam, Dong Kee Jang, Jun Kyu Lee
Hepatobiliary & Pancreatic Diseases International.2021; 20(4): 361. CrossRef - Is complete stone removal for choledocholithiasis always necessary in extremely elderly patients?
Naoko Okuda, Shinya Sugimoto, Haruka Nakamura, Hirohisa Hisada, Taishi Temma, Yuki Hashimoto, Satoshi Hayashi, Tatsuya Ito, Mayuko Takami, Jun Oyamada, Akira Kamei
JGH Open.2020; 4(1): 16. CrossRef - The efficacy and safety of one-stage endoscopic treatment for ascending acute cholangitis caused by choledocholithiasis with severe comorbidities
Xiaoping Zhang, Guiqin Li, Liang Pan, Yue Chen, Ruihua Shi, Wei Xu, Kun Zhou, Yajun Cheng, Yadong Feng, Aijun Zhou, Kai Zhao
Surgical Endoscopy.2020; 34(9): 3963. CrossRef - The efficacy and safety of colonoscopy in nonagenarians: A multicenter study
Yoshikazu Inagaki, Naohisa Yoshida, Daisuke Hasegawa, Kyoichi Kassai, Ritsu Yasuda, Ken Inoue, Ryohei Hirose, Osamu Dohi, Takashi Okuda, Yutaka Inada, Kotaro Okuda, Kiyoshi Ogiso, Akira Tomie, Koichi Soga, Takaaki Murakami, Yoshito Itoh
Indian Journal of Gastroenterology.2020; 39(6): 557. CrossRef - Risk factors of adverse events in endoscopic retrograde cholangiopancreatography for patients aged ≥85 years
Koji Takahashi, Toshio Tsuyuguchi, Harutoshi Sugiyama, Junichiro Kumagai, Masato Nakamura, Yotaro Iino, Ayako Shingyoji, Mutsumi Yamato, Hiroshi Ohyama, Yuko Kusakabe, Shin Yasui, Rintaro Mikata, Naoya Kato
Geriatrics & Gerontology International.2018; 18(7): 1038. CrossRef - Age is Important, but Patient Status is also Important in Endoscopic Retrograde Cholangiopancreatography
Dong Wook Lee, Ho Gak Kim
Clinical Endoscopy.2018; 51(4): 315. CrossRef
- Impact of frailty on endoscopic retrograde cholangiopancreatography outcomes in nonagenarians: A United States national experience
- 9,734 View
- 164 Download
- 3 Web of Science
- 14 Crossref

- Management of Benign and Malignant Pancreatic Duct Strictures
- Enad Dawod, Michel Kahaleh
- Clin Endosc 2018;51(2):156-160. Published online July 20, 2017
- DOI: https://doi.org/10.5946/ce.2017.085
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The diagnosis and management of pancreatic strictures, whether malignant or benign, remain challenging. The last 2 decades have seen dramatic progress in terms of both advanced imaging and endoscopic therapy. While plastic stents remain the cornerstone of the treatment of benign strictures, the advent of fully covered metal stents has initiated a new wave of interest in calibrating the pancreatic duct with fewer sessions. In malignant disease, palliation remains the priority and further data are necessary before offering systematic pancreatic stenting.
-
Citations
Citations to this article as recorded by- Role of peroral cholangioscopy and pancreatoscopy in the diagnosis and treatment of biliary and pancreatic disease: past, present, and future
Harishankar Gopakumar, Neil R. Sharma
Frontiers in Gastroenterology.2023;[Epub] CrossRef - EUS-guided drainage of the pancreatic duct for the treatment of postoperative stenosis of pancreatico-digestive anastomosis or pancreatic duct stenosis complicating chronic pancreatitis: Experience at a tertiary care center
Franz Rudler, Fabrice Caillol, Jean-Philippe Ratone, Christian Pesenti, Jean-Christophe Valats, Alexei Soloveyv, Marc Giovannini
Endoscopic Ultrasound.2022; 11(4): 296. CrossRef - Ruptured Splenic Artery Pseudoaneurysm Causing Hemorrhage Into a Pancreatic Pseudocyst
Zo C. Overton-Hennessy, A. Michael Devane, Steve Fiester, Noah Schammel, Christine Schammel, James W. Fulcher
American Journal of Forensic Medicine & Pathology.2022; 43(1): 76. CrossRef - Percutaneous transluminal angioplasty balloons for endoscopic ultrasound-guided pancreatic duct interventions
Jad P AbiMansour, Barham K Abu Dayyeh, Michael J Levy, Andrew C Storm, John A Martin, Bret T Petersen, Ryan J Law, Mark D Topazian, Vinay Chandrasekhara
World Journal of Gastrointestinal Endoscopy.2022; 14(8): 487. CrossRef - Image-Guided Percutaneous Pancreatic Duct Drainage: A 10-Year Observational Study
Malkhaz Mizandari, Tamta Azrumelashvili, Pedram Keshavarz, Nagy Habib
Journal of Vascular and Interventional Radiology.2021; 32(7): 1075. CrossRef - Long-term outcomes of fully covered self-expandable metal stents versus plastic stents in chronic pancreatitis
Sang Hoon Lee, Yeon Suk Kim, Eui Joo Kim, Hee Seung Lee, Jeong Youp Park, Seung Woo Park, Si Young Song, Jae Hee Cho, Seungmin Bang
Scientific Reports.2021;[Epub] CrossRef - Approach to management of pancreatic strictures: the gastroenterologist’s perspective
Vaneet Jearth, Suprabhat Giri, Sridhar Sundaram
Clinical Journal of Gastroenterology.2021; 14(6): 1587. CrossRef - International consensus guidelines on interventional endoscopy in chronic pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with the International Association of Pancr
Masayuki Kitano, Thomas M. Gress, Pramod K. Garg, Takao Itoi, Atsushi Irisawa, Hiroyuki Isayama, Atsushi Kanno, Kei Takase, Michael Levy, Ichiro Yasuda, Phillipe Lévy, Shuiji Isaji, Carlos Fernandez-Del Castillo, Asbjørn M. Drewes, Andrea R.G. Sheel, John
Pancreatology.2020; 20(6): 1045. CrossRef - Recent advances in the diagnosis and management of chronic pancreatitis
Chang-Il Kwon, Jae Hee Cho, Sung Hoon Choi, Kwang Hyun Ko, Temel Tirkes, Mark A. Gromski, Glen A. Lehman
The Korean Journal of Internal Medicine.2019; 34(2): 242. CrossRef - Endoscopic and Conservative Management of Chronic Pancreatitis and Its Complications
Alexander Waldthaler, Roberto Valente, Urban Arnelo, J.-Matthias Löhr
Visceral Medicine.2019; 35(2): 98. CrossRef
- Role of peroral cholangioscopy and pancreatoscopy in the diagnosis and treatment of biliary and pancreatic disease: past, present, and future
- 38,321 View
- 264 Download
- 11 Web of Science
- 10 Crossref

- Training in Endoscopy: Endoscopic Retrograde Cholangiopancreatography
- Jaihwan Kim
- Clin Endosc 2017;50(4):334-339. Published online July 13, 2017
- DOI: https://doi.org/10.5946/ce.2017.068
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) is a key endoscopy skill used to diagnose and treat pancreatobiliary diseases. However, its diagnostic use is decreasing in favor of other less invasive methods such as magnetic resonance cholangiopancreatography and endoscopic ultrasound. Alternatively, its use has become more important in the therapeutic area. ERCP trainees must know the anatomy and physiology of the pancreatobiliary system, several key basic skills, and complications of a successful procedure. This article briefly introduces basic ERCP knowledge, techniques, numbers necessary to achieve competency, and complications for new ERCP operators.
-
Citations
Citations to this article as recorded by- Comparing sedation protocols for endoscopic retrograde cholangiopancreatography (ERCP): A retrospective study
Ning Zhang, Guanjun Li
Heliyon.2024; 10(5): e27447. CrossRef - Lợi ích của siêu âm nội soi trước nội soi mật tụy ngược dòng trong chẩn đoán và điều trị bệnh lý tắc nghẽn đường mật tụy
Xuân Nguyễn
Journal of Clinical Medicine- Hue Central Hospital.2023;[Epub] CrossRef - Clinical safety and outcomes of glucagon use during endoscopic retrograde cholangiopancreatography (ERCP)
Abhilash Perisetti, Hemant Goyal, Neil Sharma
Endoscopy International Open.2022; 10(04): E558. CrossRef - Gallstone pancreatitis: general clinical approach and the role of endoscopic retrograde cholangiopancreatography
Shanker Kundumadam, Evan L. Fogel, Mark Andrew Gromski
The Korean Journal of Internal Medicine.2021; 36(1): 25. CrossRef - Training in endoscopic retrograde cholangio-pancreatography: a critical assessment of the broad scenario of training programs and models
Camilla Gallo, Ivo Boškoski, Maria Valeria Matteo, Beatrice Orlandini, Guido Costamagna
Expert Review of Gastroenterology & Hepatology.2021; 15(6): 675. CrossRef - Causes and Countermeasures of Difficult Selective Biliary Cannulation: A Large Sample Size Retrospective Study
Yang Liu, Wei Liu, Junbo Hong, Guohua Li, Youxiang Chen, Yong Xie, Xiaojiang Zhou
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2021; 31(5): 533. CrossRef - Impact of mechanical simulator practice on clinical ERCP performance by novice surgical trainees: a randomized controlled trial
Wenbo Meng, Ping Yue, Joseph W. Leung, Haiping Wang, Xiyan Wang, Fangzhao Wang, Kexiang Zhu, Lei Zhang, Xiaoliang Zhu, Zhengfeng Wang, Hui Zhang, Wence Zhou, Xun Li
Endoscopy.2020; 52(11): 1004. CrossRef - Does melatonin addition to indomethacin decrease post endoscopic retrograde cholangiopancreatography pancreatitis? A randomized double-blind controlled trial
Amir Sadeghi, Mohammad Abbasinazari, Hamid Asadzadeh Aghdaei, Saeed Abdi, Behzad Hatami, Mehrnaz Rasoolinezhad, Shaghayegh Jamshidzadeh, Saeede Saadati
European Journal of Gastroenterology & Hepatology.2019; 31(11): 1350. CrossRef - Does rectal ketoprofen prevent post ERCP pancreatitis?
Elias Makhoul, Joe El Mir, Marc Harb
Arab Journal of Gastroenterology.2019; 20(3): 141. CrossRef - Colangiopancreatografía retrógrada endoscópica: indicaciones y procedimiento
Ángel Pichel Loureiro, Fátima Barcala del Caño, Beatriz Romero Mosquera, Javier Robles Fernández, Nerea Catarina Quintaáns Pinazas
FMC - Formación Médica Continuada en Atención Primaria.2018; 25(9): 529. CrossRef
- Comparing sedation protocols for endoscopic retrograde cholangiopancreatography (ERCP): A retrospective study
- 6,793 View
- 239 Download
- 8 Web of Science
- 10 Crossref

- An Update on Endoscopic Management of Post-Liver Transplant Biliary Complications
- Hyun Woo Lee, Najmul Hassan Shah, Sung Koo Lee
- Clin Endosc 2017;50(5):451-463. Published online April 17, 2017
- DOI: https://doi.org/10.5946/ce.2016.139
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Biliary complications are the most common post-liver transplant (LT) complications with an incidence of 15%–45%. Furthermore, such complications are reported more frequently in patients who undergo a living-donor LT (LDLT) compared to a deceased-donor LT (DDLT). Most post-LT biliary complications involve biliary strictures, bile leakage, and biliary stones, although many rarer events, such as hemobilia and foreign bodies, contribute to a long list of related conditions. Endoscopic treatment of post-LT biliary complications has evolved rapidly, with new and effective tools improving both outcomes and success rates; in fact, the latter now consistently reach up to 80%. In this regard, conventional endoscopic retrograde cholangiopancreatography (ERCP) remains the preferred initial treatment. However, percutaneous transhepatic cholangioscopy (PTCS) is now central to the management of endoscopy-resistant cases involving complex hilar or multiple strictures with associated stones. Many additional endoscopic tools and techniques—such as the rendezvous method, magnetic compression anastomosis (MCA), and peroral cholangioscopy (POCS)—combined with modified biliary stents have significantly improved the success rate of endoscopic management. Here, we review the current status of endoscopic treatment of post-LT biliary complications and discuss conventional as well as the aforementioned new tools and techniques.
-
Citations
Citations to this article as recorded by- Asian Pacific Association for the Study of the Liver clinical practice guidelines on liver transplantation
Dong-Sik Kim, Young-In Yoon, Beom Kyung Kim, Ashok Choudhury, Anand Kulkarni, Jun Yong Park, Jongman Kim, Dong Hyun Sinn, Dong Jin Joo, YoungRok Choi, Jeong-Hoon Lee, Ho Joong Choi, Ki Tae Yoon, Sun Young Yim, Cheon-Soo Park, Deok-Gie Kim, Hae Won Lee, Wo
Hepatology International.2024; 18(2): 299. CrossRef - Surgical and Interventional Radiology Management of Vascular and Biliary Complications in Liver Transplantation: Narrative Review
Camilo Barragan, Alonso Vera, Sergio Hoyos, Diana Bejarano, Ana Maria Lopez-Ruiz, Francisco Grippi, Alejandro Mejia, María del Pilar Bayona Molano
Digestive Disease Interventions.2024; 08(01): 7. CrossRef - Management of biliary complications in liver transplant recipients using a fully covered self-expandable metal stent with antimigration features
Andrew CANAKIS, Andrew J. GILMAN, Todd H. BARON
Minerva Gastroenterology.2024;[Epub] CrossRef - Anatomical classification and clinical outcomes of biliary strictures in living donor liver transplantation using right liver grafts
Hansang Park, Eui Soo Han, Sae‐Jin Park, Su Young Hong, Sanggyun Suh, Sola Lee, Jeong‐Moo Lee, Suk Kyun Hong, YoungRok Choi, Kwang‐Woong Lee, Kyung‐Suk Suh, Nam‐Joon Yi, Joon Koo Han
Liver Transplantation.2023; 29(3): 307. CrossRef - Do We Need to Use a Stent in Biliary Reconstruction to Decrease the Incidence of Biliary Complications in Liver Transplantation? A Systematic Review and Meta-Analysis
Beshoy Effat Elkomos, Amr Abdelaal
Journal of Gastrointestinal Surgery.2023; 27(1): 180. CrossRef - Biliary and Vascular Complications after Liver Transplantation–From Diagnosis to Treatment
Gina Gheorghe, Camelia Diaconu, Simona Bungau, Nicolae Bacalbasa, Natalia Motas, Vlad-Alexandru Ionescu
Medicina.2023; 59(5): 850. CrossRef - Immediate and Late Complications After Liver Transplantation
Christopher Buros, Atman Ashwin Dave, Alessandro Furlan
Radiologic Clinics of North America.2023; 61(5): 785. CrossRef - Antimigration versus conventional fully covered metal stents in the endoscopic treatment of anastomotic biliary strictures after deceased-donor liver transplantation
Esteban Fuentes-Valenzuela, Marina de Benito Sanz, Félix García-Pajares, José Estradas, Irene Peñas-Herrero, Miguel Durá-Gil, Ana Yaiza Carbajo, Carlos de la Serna-Higuera, Ramon Sanchez-Ocana, Carmen Alonso-Martín, Carolina Almohalla, Gloria Sánchez-Anto
Surgical Endoscopy.2023; 37(9): 6975. CrossRef - Endoscopic and Percutaneous Biliary Interventions after Liver Transplantation: Nationwide Data in Korea
Seung Bae Yoon, Jungmee Kim, Chang Nyol Paik, Dong Kee Jang, Jun Kyu Lee, Won Jae Yoon, Jung-Wook Kim, Tae Hee Lee, Jae-Young Jang
Gut and Liver.2022; 16(2): 300. CrossRef - “When two scopes meet”—Use of double cholangioscopy allows for a controlled perforation of an occluded postliver transplantation anastomotic stricture
Jonathan Ng, Leonardo Zorron Cheng Tao Pu, Kim Hay Be, Rhys Vaughan, Marios Efthymiou, Sujievvan Chandran
Liver Transplantation.2022; 28(7): 1254. CrossRef - Endoscopic Management of Biliary Strictures after Orthotopic Liver Transplantation: A Single Center Experience Study
Vasile Sandru, Madalina Stan-Ilie, Oana-Mihaela Plotogea, Catalina Vladut, Bogdan Silviu Ungureanu, Gheorghe G. Balan, Dan Ionut Gheonea, Gabriel Constantinescu
Diagnostics.2022; 12(5): 1221. CrossRef - Post-transplant biliary complications: advances in pathophysiology, diagnosis, and treatment
Matthew Fasullo, Milan Patel, Lauren Khanna, Tilak Shah
BMJ Open Gastroenterology.2022; 9(1): e000778. CrossRef - Incidence of Ischemia Reperfusion Injury Related Biliary Complications in Liver Transplantation: Effect of Different Types of Donors
Yafei Guo, Jizhou Wang, Wei Wu, Dehao Huang, Hao Zheng, Zhijun Xu, Xuefeng Li, Ning Wang, Jiwei Qin, Zebin Zhu, Yang Liu, Ziqin Yao, Haibo Wang, Qiang Huang, Lianxin Liu, Björn Nashan
Transplantation Proceedings.2022; 54(7): 1865. CrossRef - Risk factors and management of biliary stones after living donor liver transplant and its effect on graft outcome
Hany Dabbous, Ashraf Elsayed, Manar Salah, Iman Montasser, Mohamed Atef, Mahmoud Elmetenini
Frontiers in Medicine.2022;[Epub] CrossRef - Intensive care management of liver transplant recipients
Jody C. Olson, Ram Subramanian, Constantine J. Karvellas
Current Opinion in Critical Care.2022; 28(6): 709. CrossRef - Interventional Radiology Management of Adult Liver Transplant Complications
Sailendra G. Naidu, Sadeer J. Alzubaidi, Indravadan J. Patel, Chris Iwuchukwu, Kenneth S. Zurcher, Dania G. Malik, Martha-Gracia Knuttinen, J. Scott Kriegshauser, Alex L. Wallace, Nitin N. Katariya, Amit K. Mathur, Rahmi Oklu
RadioGraphics.2022; 42(6): 1705. CrossRef - Are short‐term complications associated with poor allograft and patient survival after liver transplantation? A systematic review of the literature and expert panel recommendations
Felipe Alconchel, Pascale Tinguely, Carlo Frola, Michael Spiro, Ruben Ciria, Gonzalo Rodríguez, Henrik Petrowsky, Dimitri Aristotle Raptis, Elizabeth W. Brombosz, Mark Ghobrial
Clinical Transplantation.2022;[Epub] CrossRef - Post-liver transplant biliary complications: Current knowledge and therapeutic advances
Irina Boeva, Petko Ivanov Karagyozov, Ivan Tishkov
World Journal of Hepatology.2021; 13(1): 66. CrossRef - Recurrent Primary Sclerosing Cholangitis: Current Understanding, Management, and Future Directions
Kristel K. Leung, Maya Deeb, Sandra E. Fischer, Aliya Gulamhusein
Seminars in Liver Disease.2021; 41(03): 409. CrossRef - Biliary Complications Following Adult Deceased Donor Liver Transplantation: Risk Factors and Implications at a High-volume US Center
Abraham J. Matar, Katie Ross-Driscoll, Lisa Kenney, Hannah K. Wichmann, Joseph F. Magliocca, William H. Kitchens
Transplantation Direct.2021; 7(10): e754. CrossRef - Endoscopic management of difficult common bile duct stones: Where are we now? A comprehensive review
Alberto Tringali, Deborah Costa, Alessandro Fugazza, Matteo Colombo, Kareem Khalaf, Alessandro Repici, Andrea Anderloni
World Journal of Gastroenterology.2021; 27(44): 7597. CrossRef - Graft Dysfunction and Management in Liver Transplantation
Beverley Kok, Victor Dong, Constantine J. Karvellas
Critical Care Clinics.2019; 35(1): 117. CrossRef - A Review on the Management of Biliary Complications after Orthotopic Liver Transplantation
Brian T. Moy, John W. Birk
Journal of Clinical and Translational Hepatology.2019; 7(1): 1. CrossRef - Endoscopic management of anastomotic stricture after living-donor liver transplantation
Dong Wook Lee, Jimin Han
The Korean Journal of Internal Medicine.2019; 34(2): 261. CrossRef - Endoscopic retrograde cholangiography and percutaneous transhepatic cholangiodrainage in biliary strictures after liver transplantation: Long‐term outcome predictors and influence on patient survival
Melina Heinemann, Bita Tafrishi, Sven Pischke, Lutz Fischer, Thomas Rösch, Ansgar W. Lohse, Martina Sterneck, Ulrike W. Denzer
Liver International.2019; 39(6): 1155. CrossRef - Endoscopic management of biliary strictures post-liver transplantation
Ahmed Akhter, Patrick Pfau, Mark Benson, Anurag Soni, Deepak Gopal
World Journal of Meta-Analysis.2019; 7(4): 120. CrossRef - Large-duct cholangiopathies: aetiology, diagnosis and treatment
Shyam Menon, Andrew Holt
Frontline Gastroenterology.2019; 10(3): 284. CrossRef - Endoscopic treatment of biliary complications after duct-to-duct biliary anastomosis in pediatric liver transplantation
M. Harputluoglu, U. Demirel, A. R. Caliskan, A. Selimoglu, Y. Bilgic, M. Aladag, M. A. Erdogan, R. Dertli, Y. Atayan, S. Yilmaz
Langenbeck's Archives of Surgery.2019; 404(7): 875. CrossRef
- Asian Pacific Association for the Study of the Liver clinical practice guidelines on liver transplantation
- 10,437 View
- 380 Download
- 29 Web of Science
- 28 Crossref

- Endoscopic Ultrasound-Guided Biliary Access, with Focus on Technique and Practical Tips
- Woo Hyun Paik, Do Hyun Park
- Clin Endosc 2017;50(2):104-111. Published online March 30, 2017
- DOI: https://doi.org/10.5946/ce.2017.036
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - In 1980, endoscopic ultrasound (EUS) was introduced as a diagnostic tool for evaluation of the pancreas. Since the introduction of curvilinear-array echoendoscopy, EUS has been used for a variety of gastrointestinal interventions, including fine needle aspiration, tumor ablation, and pancreatobiliary access. One of the main therapeutic roles of EUS is biliary drainage as an alternative to endoscopic retrograde biliary drainage (ERBD) or percutaneous transhepatic biliary drainage (PTBD). This article summarizes three different methods of EUS-guided biliary access, with focus on technique and practical tips.
-
Citations
Citations to this article as recorded by- Endoscopic Management of Malignant Biliary Obstruction
Woo Hyun Paik, Do Hyun Park
Gastrointestinal Endoscopy Clinics of North America.2024; 34(1): 127. CrossRef - A Systematic Review of Endoscopic Treatments for Concomitant Malignant Biliary Obstruction and Malignant Gastric Outlet Obstruction and the Outstanding Role of Endoscopic Ultrasound-Guided Therapies
Giacomo Emanuele Maria Rizzo, Lucio Carrozza, Dario Quintini, Dario Ligresti, Mario Traina, Ilaria Tarantino
Cancers.2023; 15(9): 2585. CrossRef - Endoscopic ultrasound-guided biliary drainage-current status and future perspectives
Petko Ivanov Karagyozov, Ivan Tishkov, Irina Boeva, Kiril Draganov
World Journal of Gastrointestinal Endoscopy.2021; 13(12): 607. CrossRef - EUS-Guided Versus ERCP-Guided Biliary Drainage for Primary Treatment of Distal Malignant Biliary Obstruction
Woo Hyun Paik, Do Hyun Park
Current Treatment Options in Gastroenterology.2020; 18(2): 188. CrossRef - Endoscopic Retrograde Cholangiopancreatography Results 3 Days After a Failed Pre-cut
Arecio Peñaloza-Ramirez, Dumar Rodriguez-Tello, Andres Murillo-Arias, Jonathan Barreto-Perez, Pedro Aponte-Ordoñez
Revista Española de Enfermedades Digestivas.2020;[Epub] CrossRef - Endoscopic Ultrasound-Guided Biliary Drainage
Jeremy S. Nussbaum, Nikhil A. Kumta
Gastrointestinal Endoscopy Clinics of North America.2019; 29(2): 277. CrossRef - Endoscopic Ultrasound-Guided Biliary Drainage for Benign Biliary Diseases
Yousuke Nakai, Hirofumi Kogure, Hiroyuki Isayama, Kazuhiko Koike
Clinical Endoscopy.2019; 52(3): 212. CrossRef - Relief of Obstruction in the Management of Pancreatic Cancer
Chang-Il Kwon
The Korean Journal of Gastroenterology.2019; 74(2): 69. CrossRef - Current Status of Endoscopic Ultrasound Techniques for Pancreatic Neoplasms
Yousuke Nakai, Naminatsu Takahara, Suguru Mizuno, Hirofumi Kogure, Kazuhiko Koike
Clinical Endoscopy.2019; 52(6): 527. CrossRef - Endoscopic Ultrasound–Guided Biliary Drainage
Brian R. Boulay, Simon K. Lo
Gastrointestinal Endoscopy Clinics of North America.2018; 28(2): 171. CrossRef - Endoscopic ultrasound–guided biliary and pancreatic duct access and intervention
Patrick Pfau
Techniques in Gastrointestinal Endoscopy.2017; 19(4): 207. CrossRef
- Endoscopic Management of Malignant Biliary Obstruction
- 9,807 View
- 274 Download
- 7 Web of Science
- 11 Crossref

- Sensitivity and Specificity of Magnetic Resonance Cholangiopancreatography versus Endoscopic Ultrasonography against Endoscopic Retrograde Cholangiopancreatography in Diagnosing Choledocholithiasis: The Indonesian Experience
- Dadang Makmun, Achmad Fauzi, Hamzah Shatri
- Clin Endosc 2017;50(5):486-490. Published online February 28, 2017
- DOI: https://doi.org/10.5946/ce.2016.159
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Biliary stone disease is one of the most common conditions leading to hospitalization. In addition to endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasonography (EUS) and magnetic resonance cholangiopancreatography (MRCP) are required in diagnosing choledocholithiasis. This study aimed to compare the sensitivity and specificity of EUS and MRCP against ERCP in diagnosing choledocholithiasis.
Methods
This retrospective study was conducted after prospective collection of data involving 62 suspected choledocholithiasis patients who underwent ERCP from June 2013 to August 2014. Patients were divided into two groups. The first group (31 patients) underwent EUS and the second group (31 patients) underwent MRCP. Then, ERCP was performed in both groups. Sensitivity, specificity, and diagnostic accuracy of EUS and MRCP were determined by comparing them to ERCP, which is the gold standard.
Results
The male to female ratio was 3:2. The mean ages were 47.25 years in the first group and 52.9 years in the second group. Sensitivity, specificity, accuracy, positive predictive value (PPV), and negative predictive value (NPV) for EUS were 96%, 57%, 87%, 88%, and 80% respectively, and for MRCP were 81%, 40%, 68%, 74%, and 50%, respectively.
Conclusions
EUS is a better diagnostic tool than MRCP for diagnosing choledocholithiasis. -
Citations
Citations to this article as recorded by- Comparison of Endoscopic Ultrasound and Transabdominal Ultrasound in the Detection of Gallbladder and Common Bile Duct Microlithiasis
Khurshid Ul Hassan Khurshid, Rashk e Hinna, Rao Saad Ali Khan, Arshman Rauf Asghar, Aalia Mushtaq Chaudhary, Muhammad Afzal, Uzair Ali Khan, Zoya Ali Khan, Ayaan Ali Khan, Rao Zaid Ali Khan
Cureus.2024;[Epub] CrossRef - Magnetic resonance cholangiopancreatography versus endoscopic ultrasound for diagnosis of choledocholithiasis: an updated systematic review and meta-analysis
Shivaraj Afzalpurkar, Suprabhat Giri, Sunil Kasturi, Sushrut Ingawale, Sridhar Sundaram
Surgical Endoscopy.2023; 37(4): 2566. CrossRef - Incidence and management of choledocholithiasis on routine intraoperative cholangiogram: a 5‐year tertiary centre experience
Justin Ng, Roy Teng, Sara Izwan, Erick Chan, Maarisha Kumar, Ramesh Damodaran Prabha, Harald Puhalla
ANZ Journal of Surgery.2023; 93(1-2): 139. CrossRef - ERCP findings provide further justification for a “surgery-first” mindset in choledocholithiasis
Gloria Sanin, Gabriel Cambronero, James Patterson, Maggie Bosley, Aravindh Ganapathy, Carl Wescott, Lucas Neff
Surgical Endoscopy.2023; 37(11): 8714. CrossRef - Integration of ICG-fluorescence cholangiography into the safety system of laparoscopic cholecystectomy
V.A. Kashchenko, S.I. Emelyanov, V.V. Strizheletsky, M.A. Kossovich, M.L. Tariverdiev, G.M. Rutenburg, A.A. Bogatikov, A.V. Lodygin, S.V. Gornov, F.M. Sultanova
Khirurgiya. Zhurnal im. N.I. Pirogova.2023; (11): 89. CrossRef - The efficacy and safety of preoperative cholangiography via percutaneous transhepatic gallbladder drainage (PTGBD) for difficult laparoscopic cholecystectomy (LC)
Bingran Yu, Xuting Zhi, Qiong Li, Bowen Xu, Zhaoru Dong, Tao Li, Zhiqiang Chen
Surgical Endoscopy.2022; 36(2): 1355. CrossRef - Beyond acute cholecystitis—gallstone-related complications and what the emergency radiologist should know
Andrew Tran, Carrie Hoff, Karunesh Polireddy, Arie Neymotin, Kiran Maddu
Emergency Radiology.2022; 29(1): 173. CrossRef - Endoscopic retrograde cholangiopancreatography‐related adverse events in Korea: A nationwide assessment
Dong Kee Jang, Jungmee Kim, Chang Nyol Paik, Jung‐Wook Kim, Tae Hee Lee, Jae‐Young Jang, Seung Bae Yoon, Jun Kyu Lee
United European Gastroenterology Journal.2022; 10(1): 73. CrossRef - PATOLOGIA BILIAR
Xavier Eduardo Torres Maldonado, Marco Vinicio Urgiles Rivas, Carmen Angélica Vélez Peralta
Tesla Revista Científica.2022;[Epub] CrossRef - Diagnostic accuracy of magnetic resonance cholangiopancreatography in patients with extrahepatic cholestasis: a retrospective cohort study
Beyza YÜKSEL, Nihat OKÇU
Ahi Evran Medical Journal.2022;[Epub] CrossRef - Az endoszkópos ultrahangvizsgálat diagnosztikus érzékenysége epeúti kövesség gyanúja esetén
Bánk Keczer, Zsolt Dubravcsik, Attila †Szepes, László Madácsy, Attila Szijártó, István Hritz
Orvosi Hetilap.2022; 163(10): 400. CrossRef - Gallstone Disease Complicated by Choledocholithiasis: Modern Aspects of Diagnostics
V. B. Borysenko
Ukraïnsʹkij žurnal medicini, bìologìï ta sportu.2021; 6(2): 66. CrossRef - Evaluación del rendimiento diagnóstico de los criterios predictivos de la sociedad británica para el diagnóstico de coledocolitiasis en una población colombiana
Johanna Alexandra Gastelbondo Morales, William Otero Regino, Martín Alonso Gómez Zuleta
Revista Colombiana de Gastroenterología.2020; 35(3): 269. CrossRef - Diagnostic Accuracy of Endoscopic Ultrasonography Versus the Gold Standard Endoscopic Retrograde Cholangiopancreatography in Detecting Common Bile Duct Stones
Mohsin Anwer, Muhammad Sohaib Asghar, Sheeraz Rahman, Shanil Kadir, Farah Yasmin, Dania Mohsin, Rumael Jawed, Gul Muhammad Memon, Uzma Rasheed, Maira Hassan
Cureus.2020;[Epub] CrossRef - Accuracy and timeliness of an abbreviated emergency department MRCP protocol for choledocholithiasis
David K. Tso, Renata R. Almeida, Anand M. Prabhakar, Ajay K. Singh, Ali S. Raja, Efren J. Flores
Emergency Radiology.2019; 26(4): 427. CrossRef - Modern imaging modalities for diseases associated with obstructive jaundice syndrome
V. V. Zarubin, A. P. Kurazhov, V. D. Zavadovskaja, O. V. Rodionova, O. S. Tonkikh, I. Ju. Klinovitskiy
The Siberian Medical Journal.2019; 34(3): 161. CrossRef - The accuracy of 3T magnetic resonance cholangiopancreatography in suspected choledocholithiasis
Önder Yeniçeri, Neşat Çullu, Burak Özşeker, Emine Neşe Yeniçeri
Polish Journal of Radiology.2019; 84: 419. CrossRef - Optimal Evaluation of Suspected Choledocholithiasis: Does This Patient Really Have Choledocholithiasis?
Tae Yoon Lee
Clinical Endoscopy.2017; 50(5): 415. CrossRef
- Comparison of Endoscopic Ultrasound and Transabdominal Ultrasound in the Detection of Gallbladder and Common Bile Duct Microlithiasis
- 16,607 View
- 347 Download
- 14 Web of Science
- 18 Crossref

- Endoscopic Retrograde Cholangiopancreatography in Post Gastrectomy Patients
- Chang-Hwan Park
- Clin Endosc 2016;49(6):506-509. Published online November 29, 2016
- DOI: https://doi.org/10.5946/ce.2016.124
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) in post-gastrectomy patients with Billroth II (BII) reconstruction and Roux-en-Y (RY) reconstruction presents a challenge to therapeutic endoscopists. Major difficulties, including intubation to the ampulla of Vater, selective cannulation, and ampullary intervention, must be overcome in these patients. Recent data have shown that device-assisted ERCP allows for high success rates in these patients because various devices are useful for overcoming major difficulties. Therefore, good knowledge of postoperative anatomy and various devices is mandatory before performing ERCP procedures for post-gastrectomy patients.
-
Citations
Citations to this article as recorded by- Optimal choice of stapler and digestive tract reconstruction method after distal gastrectomy for gastric cancer: A prospective case–control study
Zhen Wu, Zhi-Gang Zhou, Ling-Yu Li, Wen-Jing Gao, Ting Yu
World Journal of Gastrointestinal Surgery.2023; 15(7): 1354. CrossRef - Experience of endoscopic retrograde cholangiopancreatography with side-viewing duodenoscope in patients with previous gastric surgery
Mehmet Emin Gürbüz, Dursun Özgür Karakaş
Turkish Journal of Surgery.2022; 38(2): 149. CrossRef - Efficacy and safety of the rotatable sphincterotome during ERCP in patients with prior Billroth II gastrectomy (with videos)
Feng Zhu, Yaping Guan, Jing Wang
Surgical Endoscopy.2021; 35(8): 4849. CrossRef - Single Balloon Enteroscopy-Guided Endoscopic Retrograde Cholangiopancreatography in Surgically Altered Anatomy: Long vs. Short Type
Chang-Hwan Park
The Korean Journal of Pancreas and Biliary Tract.2021; 26(3): 181. CrossRef - The feasibility of cap‐assisted routine adult colonoscope for therapeutic endoscopic retrograde cholangiopancreatography in patients with Roux‐en‐Y reconstruction after total gastrectomy
Jian Bo Ni, Mei Ying Zhu, Kai Li, Wei Ming Dai, Lun Gen Lu, Xin Jian Wan, Rong Wan, Xiao Bo Cai
Journal of Digestive Diseases.2021; 22(12): 721. CrossRef - Challenges in ERCP post-Billroth II gastrectomy: Is it the scope, tools or technique?
IhabI El Hajj, Mohammad Al-Haddad
Saudi Journal of Gastroenterology.2019;[Epub] CrossRef - Challenges of endoscopic retrograde cholangiopancreatography in patients with Billroth II gastrointestinal anatomy: A review article
Rabbinu Rangga Pribadi, Abdul Aziz Rani, Murdani Abdullah
Journal of Digestive Diseases.2019; 20(12): 631. CrossRef - Endoscopic retrograde cholangiopancreatography in Billroth II gastrectomy patients: Outcomes and potential factors affecting technical failure
Jia-Su Li, Duo-Wu Zou, Zhen-Dong Jin, Jie Chen, Xin-Gang Shi, Zhao-Shen Li, Feng Liu
Saudi Journal of Gastroenterology.2019; 25(6): 355. CrossRef
- Optimal choice of stapler and digestive tract reconstruction method after distal gastrectomy for gastric cancer: A prospective case–control study
- 7,486 View
- 128 Download
- 8 Web of Science
- 8 Crossref

- Conversion of Percutaneous Cholecystostomy to Endoscopic Gallbladder Stenting by Using the Rendezvous Technique
- Kwangwoo Nam, Jun-Ho Choi
- Clin Endosc 2017;50(3):301-304. Published online November 7, 2016
- DOI: https://doi.org/10.5946/ce.2016.120
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - We report the successful conversion of percutaneous cholecystostomy (PC) to endoscopic transpapillary gallbladder stenting (ETGS) with insertion of an antegrade guidewire into the duodenum. An 84-year-old man presented with severe acute cholecystitis and septic shock. He had significant comorbidities, and emergent PC was successfully performed. Subsequent ETGS was attempted but unsuccessful owing to difficulties with cystic duct cannulation. However, via the PC tract, the guidewire was passed antegradely into the duodenum, and ETGS with a double-pigtail plastic stent was successfully performed with the rendezvous technique. The PC tube was removed, and no recurrence was reported during the 17-month follow-up period. Conversion of PC to ETGS is a viable option in patients with acute cholecystitis who are not candidates for surgery. Antegrade guidewire insertion via the PC tract may increase the success rate of conversion and decrease the risk of procedure-related complications.
- 6,274 View
- 181 Download

- Optimal Use of Wire-Assisted Techniques and Precut Sphincterotomy
- Tae Hoon Lee, Sang-Heum Park
- Clin Endosc 2016;49(5):467-474. Published online September 19, 2016
- DOI: https://doi.org/10.5946/ce.2016.103
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Various endoscopic techniques have been developed to overcome the difficulties in biliary or pancreatic access during endoscopic retrograde cholangiopancreatography, according to the preference of the endoscopist or the aim of the procedures. In terms of endoscopic methods, guidewire-assisted cannulation is a commonly used and well-known initial cannulation technique, or an alternative in cases of difficult cannulation. In addition, precut sphincterotomy encompasses a range of available rescue techniques, including conventional precut, precut fistulotomy, transpancreatic septotomy, and precut after insertion of pancreatic stent or pancreatic duct guidewire-guided septal precut. We present a literature review of guidewire-assisted cannulation as a primary endoscopic method and the precut technique for the facilitation of selective biliary access.
-
Citations
Citations to this article as recorded by- Clinical application of ERCP concurrent laparoscopic cholecystectomy in the treatment of cholecystolithiasis complicated with extrahepatic bile duct stones
Jiang-Bo Shen, Peng-Cheng Chen, Jin-Gen Su, Qing-Chun Feng, Pei-Dong Shi
Heliyon.2024; 10(10): e31022. CrossRef - Efficacy of a newly developed guidewire for selective biliary access
Do Hyun Park, Joung-Ho Han, Tae Hoon Lee, Jae Kook Yang, Ji Sung Lee, Yong Hun Lee, Mamoru Takenaka, Sang-Heum Park
Scientific Reports.2023;[Epub] CrossRef - Factors Predicting Difficult Biliary Cannulation during Endoscopic Retrograde Cholangiopancreatography for Common Bile Duct Stones
Hirokazu Saito, Yoshihiro Kadono, Takashi Shono, Kentaro Kamikawa, Atsushi Urata, Jiro Nasu, Haruo Imamura, Ikuo Matsushita, Tatsuyuki Kakuma, Shuji Tada
Clinical Endoscopy.2022; 55(2): 263. CrossRef - Management of difficult or failed biliary access in initial ERCP: A review of current literature
Qinghai Chen, Peng Jin, Xiaoyan Ji, Haiwei Du, Junhua Lu
Clinics and Research in Hepatology and Gastroenterology.2019; 43(4): 365. CrossRef - Comparison of efficacy and safety of transpancreatic septotomy, needle-knife fistulotomy or both based on biliary cannulation unintentional pancreatic access and papillary morphology
Jun Wen, Tao Li, Yi Lu, Li-Ke Bie, Biao Gong
Hepatobiliary & Pancreatic Diseases International.2019; 18(1): 73. CrossRef - Wire-guided biliary cannulation: a comprehensive approach to a set of techniques
Vincenzo Cennamo, Marco Bassi, Stefano Landi, Cecilia Binda, Carlo Fabbri, Stefania Ghersi, Antonio Gasbarrini
European Journal of Gastroenterology & Hepatology.2019; 31(11): 1299. CrossRef - TRANSPAPILLARY ENDOSCOPIC SURGERY: COMPLICATIONS AND PREVENTION OF THEIR DEVELOPMENT
P N Romashchenko, A A Filin, N A Maistrenko, A A Fekliunin, E S Zherebtsov
Bulletin of the Russian Military Medical Academy.2019; 21(1): 54. CrossRef - Modified transprepancreatic septotomy reduces postoperative complications after intractable biliary access
Henggao Zhong, Xiaohong Wang, Lihua Yang, Lin Miao, Guozhong Ji, Zhining Fan
Medicine.2018; 97(1): e9522. CrossRef
- Clinical application of ERCP concurrent laparoscopic cholecystectomy in the treatment of cholecystolithiasis complicated with extrahepatic bile duct stones
- 8,304 View
- 252 Download
- 6 Web of Science
- 8 Crossref

- A Review of Probe-Based Confocal Laser Endomicroscopy for Pancreaticobiliary Disease
- Kunal Karia, Michel Kahaleh
- Clin Endosc 2016;49(5):462-466. Published online September 19, 2016
- DOI: https://doi.org/10.5946/ce.2016.086
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Confocal laser endomicroscopy (CLE) is a novel in vivo imaging technique that can provide real-time optical biopsies in the evaluation of pancreaticobiliary strictures and pancreatic cystic lesions (PCLs), both of which are plagued by low sensitivities of routine evaluation techniques. Compared to pathology alone, CLE is associated with a higher sensitivity and accuracy for the evaluation of indeterminate pancreaticobiliary strictures. CLE has the ability to determine the malignant potential of PCLs. As such, CLE can increase the diagnostic yield of endoscopic retrograde cholangiopancreatography and endoscopic ultrasound, reducing the need for repeat procedures. It has been shown to be safe, with an adverse event rate of ≤1%. Published literature regarding its cost-effectiveness is needed.
-
Citations
Citations to this article as recorded by- Basic Principles and Role of Endoscopic Ultrasound in Diagnosis and Differentiation of Pancreatic Cancer from Other Pancreatic Lesions: A Comprehensive Review of Endoscopic Ultrasound for Pancreatic Cancer
Dushyant Singh Dahiya, Yash R. Shah, Hassam Ali, Saurabh Chandan, Manesh Kumar Gangwani, Andrew Canakis, Daryl Ramai, Umar Hayat, Bhanu Siva Mohan Pinnam, Amna Iqbal, Sheza Malik, Sahib Singh, Fouad Jaber, Saqr Alsakarneh, Islam Mohamed, Meer Akbar Ali, M
Journal of Clinical Medicine.2024; 13(9): 2599. CrossRef - Fluorescence Confocal Microscopy in Urological Malignancies: Current Applications and Future Perspectives
Luca Ongaro, Giulio Rossin, Arianna Biasatti, Matteo Pacini, Michele Rizzo, Fabio Traunero, Andrea Piasentin, Alessandro Perotti, Carlo Trombetta, Riccardo Bartoletti, Alessandro Zucchi, Alchiede Simonato, Nicola Pavan, Giovanni Liguori, Francesco Claps
Life.2023; 13(12): 2301. CrossRef - Improving Diagnostic Yield in Indeterminate Biliary Strictures
David J. Restrepo, Chris Moreau, Cyrus V. Edelson, Ameesh Dev, Shreyas Saligram, Hari Sayana, Sandeep N. Patel
Clinics in Liver Disease.2022; 26(1): 69. CrossRef - EUS-guided biopsy versus confocal laser endomicroscopy in patients with pancreatic cystic lesions: A systematic review and meta-analysis
Bojan Kovacevic, Giulio Antonelli, Pia Klausen, Cesare Hassan, Alberto Larghi, Peter Vilmann, JohnGásdal Karstensen
Endoscopic Ultrasound.2021; 10(4): 270. CrossRef - Approach to management of pancreatic strictures: the gastroenterologist’s perspective
Vaneet Jearth, Suprabhat Giri, Sridhar Sundaram
Clinical Journal of Gastroenterology.2021; 14(6): 1587. CrossRef - Image computing for fibre-bundle endomicroscopy: A review
Antonios Perperidis, Kevin Dhaliwal, Stephen McLaughlin, Tom Vercauteren
Medical Image Analysis.2020; 62: 101620. CrossRef - The Diagnostic Dilemma of Malignant Biliary Strictures
Robert Dorrell, Swati Pawa, Yi Zhou, Neeraj Lalwani, Rishi Pawa
Diagnostics.2020; 10(5): 337. CrossRef - Confocal endomicroscopy for the diagnosis of pancreatic lesions
Sabbah Meriam, Trad Dorra, Ouakaa Asma, Bibani Norsaf, Jouini Raja, Zaafouri Heithem, Elloumi Hela, Gargouri Dalila
Arab Journal of Gastroenterology.2020; 21(3): 139. CrossRef - Diagnostic Performance of Confocal Laser Endomicroscopy for the Detection of Bladder Cancer: Systematic Review and Meta-Analysis
Jie Wu, Yu-Chen Wang, Wen-Jie Luo, Bo Dai, Ding-Wei Ye, Yi-Ping Zhu
Urologia Internationalis.2020; 104(7-8): 523. CrossRef - Practical Management of Indeterminate Biliary Strictures
Aleksey Novikov, Thomas E. Kowalski, David E. Loren
Gastrointestinal Endoscopy Clinics of North America.2019; 29(2): 205. CrossRef - Shape-adapting panoramic photoacoustic endomicroscopy
Kedi Xiong, Wei Wang, Ting Guo, Zhen Yuan, Sihua Yang
Optics Letters.2019; 44(11): 2681. CrossRef - Indications for Single-Operator Cholangioscopy and Pancreatoscopy: an Expert Review
Enrique Pérez-Cuadrado-Robles, Pierre H. Deprez
Current Treatment Options in Gastroenterology.2019; 17(3): 408. CrossRef - Indeterminate biliary strictures: a simplified approach
Chencheng Xie, Khalil Aloreidi, Bhavesh Patel, Timothy Ridgway, Thavam Thambi-Pillai, Gary Timmerman, Adeel Khan, Muslim Atiq
Expert Review of Gastroenterology & Hepatology.2018; 12(2): 189. CrossRef - Pancreatic Cystic Lesions
Filipe Vilas-Boas, Guilherme Macedo
Journal of Clinical Gastroenterology.2018; 52(1): 13. CrossRef - Endoscopic ultrasound‐through‐the‐needle biopsy in pancreatic cystic lesions: A multicenter study
Luca Barresi, Stefano F. Crinò, Carlo Fabbri, Fabia Attili, Jan W. Poley, Silvia Carrara, Ilaria Tarantino, Laura Bernardoni, Silvia Giovanelli, Milena Di Leo, Erminia Manfrin, Matteo Tacelli, Marco J. Bruno, Mario Traina, Alberto Larghi
Digestive Endoscopy.2018; 30(6): 760. CrossRef - Stomach wall structure and vessels imaging by acoustic resolution photoacoustic microscopy
Cheng Wang, Yu-Fei Lu, Chun-Miao Cai, Hua-Zhong Xiang, Gang Zheng
World Journal of Gastroenterology.2018; 24(31): 3531. CrossRef
- Basic Principles and Role of Endoscopic Ultrasound in Diagnosis and Differentiation of Pancreatic Cancer from Other Pancreatic Lesions: A Comprehensive Review of Endoscopic Ultrasound for Pancreatic Cancer
- 11,469 View
- 163 Download
- 16 Web of Science
- 16 Crossref

- Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUS: Mid-Term Analysis of an Emerging Procedure
- Amy Tyberg, Jose Nieto, Sanjay Salgado, Kristen Weaver, Prashant Kedia, Reem Z. Sharaiha, Monica Gaidhane, Michel Kahaleh
- Clin Endosc 2017;50(2):185-190. Published online September 19, 2016
- DOI: https://doi.org/10.5946/ce.2016.030
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Performing endoscopic retrograde cholangiopancreatography (ERCP) in patients who have undergone Rouxen-Y gastric bypass (RYGB) is challenging. Standard ERCP and enteroscopy-assisted ERCP are associated with limited success rates. Laparoscopy- or laparotomy-assisted ERCP yields improved efficacy rates, but with higher complication rates and costs. We present the first multicenter experience regarding the efficacy and safety of endoscopic ultrasound (EUS)-directed transgastric ERCP (EDGE) or EUS.
Methods
All patients who underwent EDGE at two academic centers were included. Clinical success was defined as successful ERCP and/or EUS through the use of lumen-apposing metal stents (LAMS). Adverse events related to EDGE were separated from ERCP- or EUS-related complications and were defined as bleeding, stent migration, perforation, and infection.
Results
Sixteen patients were included in the study. Technical success was 100%. Clinical success was 90% (n=10); five patients were awaiting maturation of the fistula tract prior to ERCP or EUS, and one patient had an aborted ERCP due to perforation. One perforation occurred, which was managed endoscopically. Three patients experienced stent dislodgement; all stents were successfully repositioned or bridged with a second stent. Ten patients (62.5%) had their LAMS removed. The average weight change from LAMS insertion to removal was negative 2.85 kg.
Conclusions
EDGE is an effective, minimally invasive, single-team solution to the difficulties associated with ERCP in patients with RYGB. -
Citations
Citations to this article as recorded by- Approaches to Pancreaticobiliary Endoscopy in Roux-en-Y Gastric Bypass Anatomy
Khaled Elfert, Michel Kahaleh
Gastrointestinal Endoscopy Clinics of North America.2024; 34(3): 475. CrossRef - Fixation of the proximal flange of a lumen-apposing metal stent using a through-the-scope endoscopic suturing system to prevent stent migration in single-session EUS-directed transgastric ERCP: a pilot study
Hafiz Muzaffar Akbar Khan, Azhar Hussain, Vishnu Charan Suresh Kumar, Dennis Yang, Muhammad Khalid Hasan
Gastrointestinal Endoscopy.2024;[Epub] CrossRef - Endoscopic Ultrasound-Directed Transgastric ERCP (EDGE) Utilization of Trends Among Interventional Endoscopists
Sardar M. Shah-Khan, Eric Zhao, Amy Tyberg, Sardar Sarkar, Haroon M. Shahid, Rodrigo Duarte-Chavez, Monica Gaidhane, Michel Kahaleh
Digestive Diseases and Sciences.2023; 68(4): 1167. CrossRef - Factors predictive of persistent fistulas in EUS-directed transgastric ERCP: a multicenter matched case-control study
Bachir Ghandour, Margaret G. Keane, Brianna Shinn, Qais M. Dawod, Sima Fansa, Abdul Hamid El Chafic, Shayan S. Irani, Rishi Pawa, Aditya Gutta, Yervant Ichkhanian, Bharat Paranandi, Swati Pawa, Mohammad A. Al-Haddad, Tobias Zuchelli, Matthew T. Huggett, R
Gastrointestinal Endoscopy.2023; 97(2): 260. CrossRef - Suturing a 20-mm lumen-apposing metal stent allows for safe same-session EUS-directed transgastric intervention in patients with Roux-en-Y gastric bypass anatomy: a multicenter study (with video)
Margaret G. Keane, Jennifer T. Higa, Danielle La Selva, Mouen A. Khashab, Shayan S. Irani
Gastrointestinal Endoscopy.2023; 97(2): 291. CrossRef - Efficacy & safety of EUS-directed transgastric endoscopic retrograde cholangiopancreatography (EDGE) in Roux-en-Y gastric bypass anatomy: a systematic review & meta-analysis
Smit S. Deliwala, Babu P. Mohan, Pradeep Yarra, Shahab R. Khan, Saurabh Chandan, Daryl Ramai, Lena L. Kassab, Antonio Facciorusso, Manish Dhawan, Douglas G. Adler, Vivek Kaul, Saurabh Chawla, Gursimran S. Kochhar
Surgical Endoscopy.2023; 37(6): 4144. CrossRef - Risk factors of anastomosis‐related difficult endoscopic retrograde cholangiopancreatography following endoscopic ultrasound‐guided gastro‐gastrostomy using a standardized protocol (with video)
Enrique Pérez‐Cuadrado‐Robles, Hadrien Alric, Lucille Quénéhervé, Laurent Monino, Tigran Poghosyan, Hedi Benosman, Ariane Vienne, Guillaume Perrod, Lionel Rebibo, Ali Aidibi, Elena Tenorio‐González, Emilia Ragot, Mehdi Karoui, Christophe Cellier, Gabriel
Digestive Endoscopy.2023; 35(7): 909. CrossRef - Endoscopic ultrasound-directed transgastric ERCP (EDGE): A multicenter US study on long-term follow-up and fistula closure
Prashant Kedia, Sardar Shah-Khan, Amy Tyberg, Monica Gaidhane, Avik Sarkar, Haroon Shahid, Eric Zhao, Shyam Thakkar, Mason Winkie, Matthew Krafft, Shailendra Singh, Eugene Zolotarevsky, Jeremy Barber, Mitchelle Zolotarevsky, Ian Greenberg, Dhiemeziem Eke,
Endoscopy International Open.2023; 11(05): E529. CrossRef - Endoscopic-Directed Trans-Gastric Retrograde Cholangiopancreatography in Patients With Roux-en-Y gastric Bypasses
Tong Su, Tianjie Chen, Jing Wang, Yuemin Feng, Ruixia Wang, Shulei Zhao
Journal of Clinical Gastroenterology.2023; 57(9): 871. CrossRef - Safety and efficacy of LA-ERCP procedure following Roux-en-Y gastric bypass: a systematic review and meta-analysis
Baraa Saad, Maya Nasser, Reem H. Matar, Hayato Nakanishi, Danijel Tosovic, Christian A. Than, Stephanie Taha-Mehlitz, Anas Taha
Surgical Endoscopy.2023; 37(9): 6682. CrossRef - Clinical application and follow-up of electrocautery-enhanced lumen-apposing metal stents for endoscopic ultrasonography-guided interventions
Yu Mo She, Nan Ge
Annals of Medicine.2023;[Epub] CrossRef - Endoscopic Biliary Drainage in Surgically Altered Anatomy
Marco Spadaccini, Carmelo Marco Giacchetto, Matteo Fiacca, Matteo Colombo, Marta Andreozzi, Silvia Carrara, Roberta Maselli, Fabio Saccà, Alessandro De Marco, Gianluca Franchellucci, Kareem Khalaf, Glenn Koleth, Cesare Hassan, Andrea Anderloni, Alessandro
Diagnostics.2023; 13(24): 3623. CrossRef - Laparoscopic-assisted ERCP following RYGB: a 12-year assessment of outcomes and learning curve at a high-volume pancreatobiliary center
Samer AlMasri, Mazen S. Zenati, Georgios I. Papachristou, Adam Slivka, Michael Sanders, Jennifer Chennat, Mordechai Rabinowitz, Asif Khalid, Andres Gelrud, John Nasr, Savreet Sarkaria, Rohit Das, Kenneth K. Lee, Wolfgang Schraut, Steve J. Hughes, A. James
Surgical Endoscopy.2022; 36(1): 621. CrossRef - Endoscopic ultrasound-directed transgastric ERCP (EDGE): a systematic review describing the outcomes, adverse events, and knowledge gaps
Shaurya Prakash, B. Joseph Elmunzer, Erin M. Forster, Gregory A. Cote, Robert A. Moran
Endoscopy.2022; 54(01): 52. CrossRef - “Innocent as a LAMS”: Does Spontaneous Fistula Closure (Secondary Intention), After EUS-Directed Transgastric ERCP (EDGE) via 20-mm Lumen-Apposing Metal Stent, Confer an Increased Risk of Persistent Fistula and Unintentional Weight Gain?
Matthew Richard Krafft, Alyssa Lorenze, Michael P. Croglio, Wei Fang, Todd H. Baron, John Y. Nasr
Digestive Diseases and Sciences.2022; 67(6): 2337. CrossRef - Biliopancreatic access following anatomy-altering bariatric surgery: a literature review
Pavlos Papasavas, Salvatore Docimo, Rodolfo J. Oviedo, Dan Eisenberg
Surgery for Obesity and Related Diseases.2022; 18(1): 21. CrossRef - Extrapancreatic Advanced Endoscopic Interventions
Haresh Vijay Naringrekar, Haroon Shahid, Cyril Varghese, Alex Schlachterman, Sandeep P. Deshmukh, Christopher G. Roth
RadioGraphics.2022; 42(2): 379. CrossRef - EUS-directed transgastric ERCP: a step-by-step approach (with video)
Michel Kahaleh
Gastrointestinal Endoscopy.2022; 95(4): 787. CrossRef - Comparison of endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography outcomes using various technical approaches
Firas Bahdi, Rollin George, Kavea Paneerselvam, Dang Nguyen, Wasif M. Abidi, Mohamed O. Othman, Isaac Raijman
Endoscopy International Open.2022; 10(04): E459. CrossRef - Endoscopic retrieval of a blocked double-pigtail plastic biliary stent through an endoscopic ultrasound-guided gastrojejunostomy in a patient with gastric outlet obstruction
Sridhar Sundaram, Kiran Mane, Unique Tyagi, Aadish Kumar Jain, Utkarsh Chhanchure, Prachi Patil, Shaesta Mehta
Endoscopy.2022; 54(S 02): E806. CrossRef - Endoscopic Approaches to the Management of Biliary Tract Pathology: The Use of Therapeutic Endoscopic Ultrasound
Amy E. Hosmer
Digestive Disease Interventions.2022; 06(03): 197. CrossRef - EUS-directed transgastric interventions in Roux-en-Y gastric bypass anatomy: a multicenter experience
Bachir Ghandour, Brianna Shinn, Qais M. Dawod, Sima Fansa, Abdul Hamid El Chafic, Shayan S. Irani, Rishi Pawa, Aditya Gutta, Yervant Ichkhanian, Bharat Paranandi, Swati Pawa, Mohammad A. Al-Haddad, Tobias Zuchelli, Matthew T. Huggett, Michael Bejjani, Ree
Gastrointestinal Endoscopy.2022; 96(4): 630. CrossRef - Endoscopic ultrasound guided access procedures following surgery
Khaled Elfert, Ebrahim Zeid, Rodrigo Duarte-Chavez, Michel Kahaleh
Best Practice & Research Clinical Gastroenterology.2022; 60-61: 101812. CrossRef - Shortened-Interval Dual-Session EDGE Reduces the Risk of LAMS Dislodgement While Facilitating Timely ERCP
Matthew R. Krafft, Wei Fang, John Y. Nasr
Digestive Diseases and Sciences.2021; 66(8): 2776. CrossRef - A comparison of clinical outcomes and cost utility among laparoscopy, enteroscopy, and temporary gastric access-assisted ERCP in patients with Roux-en-Y gastric bypass anatomy
Thomas J. Wang, Pedro Cortes, Pichamol Jirapinyo, Christopher C. Thompson, Marvin Ryou
Surgical Endoscopy.2021; 35(8): 4469. CrossRef - Endoscopic ultrasound-directed transgastric ERCP facilitating extensive ampullectomy in Roux-en-Y gastric bypass patient
Petr Vaněk, Martin L. Freeman, Guru Trikudanathan
Endoscopy.2021; 53(07): E261. CrossRef - Lumen-apposing metal stents for approved and off-label indications: a single-centre experience
Pieter Hindryckx, Helena Degroote
Surgical Endoscopy.2021; 35(11): 6013. CrossRef - Endoscopic ultrasound-directed transgastric ERCP (EDGE): a retrospective multicenter study
Thomas M. Runge, Austin L. Chiang, Thomas E. Kowalski, Theodore W. James, Todd H. Baron, Jose Nieto, David L. Diehl, Matthew R. Krafft, John Y. Nasr, Vikas Kumar, Harshit S. Khara, Shayan Irani, Arpan Patel, Ryan J. Law, David E. Loren, Alex Schlachterman
Endoscopy.2021; 53(06): 611. CrossRef - Endoscopy in Patients With Surgically Altered Anatomy
Monique T. Barakat, Douglas G. Adler
American Journal of Gastroenterology.2021; 116(4): 657. CrossRef - EUS-directed transgastric ERCP: A first-line option for ERCP following Roux-en-Y gastric bypass
MoniqueT Barakat, DouglasG Adler
Endoscopic Ultrasound.2021; 10(3): 151. CrossRef - Maximizing success in single-session EUS-directed transgastric ERCP: a retrospective cohort study to identify predictive factors of stent migration
Brianna Shinn, Tina Boortalary, Isaac Raijman, Jose Nieto, Harshit S. Khara, S. Vikas Kumar, Bradley Confer, David L. Diehl, Maan El Halabi, Yervant Ichkhanian, Thomas Runge, Vivek Kumbhari, Mouen Khashab, Amy Tyberg, Haroon Shahid, Avik Sarkar, Monica Ga
Gastrointestinal Endoscopy.2021; 94(4): 727. CrossRef - Endoscopic ultrasound-guided biliary drainage: Are we there yet?
Rishi Pawa, Troy Pleasant, Chloe Tom, Swati Pawa
World Journal of Gastrointestinal Endoscopy.2021; 13(8): 302. CrossRef - Novel Uses of Lumen-apposing Metal Stents
Prashant Bhenswala, Muhddesa Lakhana, Frank G. Gress, Iman Andalib
Journal of Clinical Gastroenterology.2021; 55(8): 641. CrossRef - Biliopancreatic Endoscopy in Altered Anatomy
Ilaria Tarantino, Giacomo Emanuele Maria Rizzo
Medicina.2021; 57(10): 1014. CrossRef - Endoscopic management of difficult common bile duct stones: Where are we now? A comprehensive review
Alberto Tringali, Deborah Costa, Alessandro Fugazza, Matteo Colombo, Kareem Khalaf, Alessandro Repici, Andrea Anderloni
World Journal of Gastroenterology.2021; 27(44): 7597. CrossRef - Interventional endoscopic ultrasonography in patients with surgically altered anatomy: Techniques and literature review
Akio Katanuma, Tusyoshi Hayashi, Toshifumi Kin, Haruka Toyonaga, Shunsuke Honta, Kouki Chikugo, Hidetaro Ueki, Tastuya Ishii, Kuniyuki Takahashi
Digestive Endoscopy.2020; 32(2): 263. CrossRef - Endoscopic ultrasound-directed transgastric ERCP in patients with Roux-en-Y gastric bypass using lumen-apposing metal stents or duodenal self-expandable metal stents. A European single-center experience
Marina de Benito Sanz, Ana Yaiza Carbajo López, Ramón Sánchez-Ocaña Hernández, Carlos Chavarría Herbozo, Sergio Bagaza Pérez de Rozas, Javier García-Alonso, Carlos de la Serna Higuera, Manuel Pérez-Miranda Castillo
Revista Española de Enfermedades Digestivas.2020;[Epub] CrossRef - Tailored access to the hepatobiliary system in post-bariatric patients: a tertiary care bariatric center experience
Dino Kröll, Alexandra Charlotte Müller, Philipp C. Nett, Reiner Wiest, Johannes Maubach, Guido Stirnimann, Daniel Candinas, Yves Michael Borbély
Surgical Endoscopy.2020; 34(12): 5469. CrossRef - Endoscopic Retrograde Cholangiopancreatography in Patients With Roux-en-Y Gastric Bypass
Erin Forster, B. Joseph Elmunzer
American Journal of Gastroenterology.2020; 115(2): 155. CrossRef - Endoscopic Retrograde Cholangiopancreatography in Patients With Surgically Altered Anatomy
Nasim Parsa, Yervant Ichkhanian, Mouen A. Khashab
Current Treatment Options in Gastroenterology.2020; 18(2): 212. CrossRef - Temporary Trans-gastric Stent Deployment Over a 20 French Gastrostomy for Single-Stage Endoscopic Retrograde Cholangiopancreatography After Gastric Bypass
Gianfranco Donatelli, Fabrizio Cereatti, Andrea Spota, Thierry Tuszynski, David Danan, Jean-Loup Dumont
Obesity Surgery.2020; 30(10): 4130. CrossRef - Endoscopic devices and techniques for the management of bariatric surgical adverse events (with videos)
Allison R. Schulman, Rabindra R. Watson, Barham K. Abu Dayyeh, Manoop S. Bhutani, Vinay Chandrasekhara, Pichamol Jirapinyo, Kumar Krishnan, Nikhil A. Kumta, Joshua Melson, Rahul Pannala, Mansour A. Parsi, Guru Trikudanathan, Arvind J. Trindade, John T. Ma
Gastrointestinal Endoscopy.2020; 92(3): 492. CrossRef - Endoscopic management of gastric outlet obstruction of remnant stomach in a patient with Roux-en-Y gastric bypass
Vivek Kesar, John Magulick, Varun Kesar, Thiruvengadam Muniraj, Harry R. Aslanian
VideoGIE.2020; 5(11): 557. CrossRef - After you Roux, what do you do? A systematic review of most successful advanced assisted ERCP techniques in patients with various altered upper gastrointestinal surgical anatomical reconstructions with particular focus on RYGB (last 10 years)
Mohamed Elsharif, Adam Gary Hague, Hussam Ahmed, Roger Ackroyd
Clinical Journal of Gastroenterology.2020; 13(6): 985. CrossRef - Endoscopic Ultrasound
Shelini Sooklal, Prabhleen Chahal
Surgical Clinics of North America.2020; 100(6): 1133. CrossRef - Endoscopic approach to gastric remnant outlet obstruction after gastric bypass: A case report
Arash Zarrin, Sufian Sorathia, Vivek Choksi, Steven Robert Kaplan, Franklin Kasmin
World Journal of Gastrointestinal Endoscopy.2020; 12(9): 297. CrossRef - Recent developments in endoscopic ultrasonography-guided gastroenterostomy
Kenjiro Yamamoto, Takao Itoi
International Journal of Gastrointestinal Intervention.2020; 9(4): 177. CrossRef - ERCP with overtube-assisted enteroscopy in patients with Roux-en-Y gastric bypass anatomy: a systematic review and meta-analysis
Jagpal Singh Klair, Mahendran Jayaraj, Viveksandeep Thoguluva Chandrasekar, Harshith Priyan, Joanna Law, Arvind R. Murali, Dhruv Singh, Michael Larsen, Shayan Irani, Richard Kozarek, Andrew Ross, Rajesh Krishnamoorthi
Endoscopy.2020; 52(10): 824. CrossRef - Bariatric endoscopy: current primary therapies and endoscopic management of complications and other related conditions
Melissa Castro, Alfredo Daniel Guerron
Mini-invasive Surgery.2020;[Epub] CrossRef - Duodenal endoscopic submucosal dissection and sutured defect closure across a lumen-apposing metal stent
Phillip S. Ge, Hiroyuki Aihara, Christopher C. Thompson, Marvin Ryou
VideoGIE.2019; 4(4): 172. CrossRef - Endoscopic Ultrasound-Directed Transgastric ERCP (EDGE): a Single-Center US Experience with Follow-up Data on Fistula Closure
Theodore W. James, Todd Huntley Baron
Obesity Surgery.2019; 29(2): 451. CrossRef - Endoscopic Management of Complex Biliary Stone Disease
Prashant Kedia, Paul R. Tarnasky
Gastrointestinal Endoscopy Clinics of North America.2019; 29(2): 257. CrossRef - ERCP in patients with Roux-en-Y gastric bypass: one size does not fit all
Dennis Yang, Peter V. Draganov
Gastrointestinal Endoscopy.2019; 89(3): 646. CrossRef - Response
Majidah Bukhari, Mouen A Khashab
Gastrointestinal Endoscopy.2019; 89(3): 646. CrossRef - EUS-directed Transgastric ERCP (EDGE) Versus Laparoscopy-assisted ERCP (LA-ERCP) for Roux-en-Y Gastric Bypass (RYGB) Anatomy
Prashant Kedia, Paul R. Tarnasky, Jose Nieto, Stephen L. Steele, Ali Siddiqui, Ming-ming Xu, Amy Tyberg, Monica Gaidhane, Michel Kahaleh
Journal of Clinical Gastroenterology.2019; 53(4): 304. CrossRef - Advanced Endoscopic Procedures: An Update for Radiologists
Preethi Guniganti, Andrea S. Kierans
American Journal of Roentgenology.2019; 213(2): 332. CrossRef - Endoscopic retrograde cholangiopancreatography in Roux-en-Y gastric bypass patients
Tom G. Moreels
Minerva Chirurgica.2019;[Epub] CrossRef - An adverse event of EUS-directed transgastric ERCP: stent-in-stent technique to bridge the peritoneal gap
Anna Duloy, Hazem Hammad, Raj J. Shah
VideoGIE.2019; 4(11): 508. CrossRef - Accès à l’estomac exclu après by-pass gastrique : expérience d’un centre expert dépourvu de plateau technique permettant la cholangiopancréaticographie rétrograde endoscopique
D. Verscheure, G. Donatelli, P. Tammaro, J.L. Dumont, J.P. Marmuse, K. Arapis
Journal de Chirurgie Viscérale.2018; 155(3): 194. CrossRef - Multicenter evaluation of the clinical utility of laparoscopy-assisted ERCP in patients with Roux-en-Y gastric bypass
Ali M. Abbas, Andrew T. Strong, David L. Diehl, Brian C. Brauer, Iris H. Lee, Rebecca Burbridge, Jaroslav Zivny, Jennifer T. Higa, Marcelo Falcão, Ihab I. El Hajj, Paul Tarnasky, Brintha K. Enestvedt, Alexander R. Ende, Adarsh M. Thaker, Rishi Pawa, Priya
Gastrointestinal Endoscopy.2018; 87(4): 1031. CrossRef - Spiral enteroscopy–assisted ERCP in bariatric-length Roux-en-Y anatomy: a large single-center series and review of the literature (with video)
Mohammad F. Ali, Rani Modayil, Krishna C. Gurram, Collin E.M. Brathwaite, David Friedel, Stavros N. Stavropoulos
Gastrointestinal Endoscopy.2018; 87(5): 1241. CrossRef - EUS-guided colo-enterostomy as a salvage drainage procedure in a high surgical risk patient with small bowel obstruction due to severe ileocolonic anastomotic stricture: a new application of lumen-apposing metal stent (LAMS)
Hugh D. Mai, Ethan Dubin, Arun A. Mavanur, Marvin Feldman, Sudhir Dutta
Clinical Journal of Gastroenterology.2018; 11(4): 282. CrossRef - Response to Alkhatib and Alasadi
Allison R. Schulman, Christopher C. Thompson
American Journal of Gastroenterology.2018; 113(5): 777. CrossRef - Single Session EUS-Guided Temporary Gastro-Gastrostomy and ERCP Following Gastric Bypass
Dario Ligresti, Michele Amata, Antonino Granata, Fabio Cipolletta, Luca Barresi, Mario Traina, Ilaria Tarantino
Obesity Surgery.2018; 28(3): 886. CrossRef - Avoidance, Recognition, and Management of Complications Associated with Lumen-Apposing Metal Stents
Stuart K. Amateau, Martin L. Freeman
Gastrointestinal Endoscopy Clinics of North America.2018; 28(2): 219. CrossRef - An international, multicenter, comparative trial of EUS-guided gastrogastrostomy-assisted ERCP versus enteroscopy-assisted ERCP in patients with Roux-en-Y gastric bypass anatomy
Majidah Bukhari, Thomas Kowalski, Jose Nieto, Rastislav Kunda, Nitin K. Ahuja, Shayan Irani, Apeksha Shah, David Loren, Olaya Brewer, Omid Sanaei, Yen-I Chen, Saowanee Ngamruengphong, Vivek Kumbhari, Vikesh Singh, Hanaa Dakour Aridi, Mouen A. Khashab
Gastrointestinal Endoscopy.2018; 88(3): 486. CrossRef - Updates in Therapeutic Endoscopic Ultrasonography
Shawn L. Shah, Manuel Perez-Miranda, Michel Kahaleh, Amy Tyberg
Journal of Clinical Gastroenterology.2018; 52(9): 765. CrossRef - Endoscopic Ultrasound-Guided Creation of a Gastrogastric Conduit After Pancreaticoduodenectomy in a Patient with Prior Roux-en-Y Gastric Bypass
Rohit Das, Herbert Zeh, Amer Zureikat, Adam Slivka, Georgios I. Papachristou
ACG Case Reports Journal.2018; 5(12): e1001. CrossRef - Endoscopic Ultrasound-Guided Creation of a Gastrogastric Conduit After Pancreaticoduodenectomy in a Patient with Prior Roux-en-Y Gastric Bypass
Rohit Das, Herbert Zeh, Amer Zureikat, Adam Slivka, Georgios I. Papachristou
ACG Case Reports Journal.2018; 5(1): e100. CrossRef - Commentary on “Endoscopic Ultrasound (EUS)-Directed Transgastric Endoscopic Retrograde Cholangiopancreatography or EUS”
Se Woo Park
Clinical Endoscopy.2017; 50(2): 102. CrossRef - Techniques for endoscopic retrograde cholangiopancreatography in altered gastrointestinal anatomy
Tom G. Moreels
Current Opinion in Gastroenterology.2017; 33(5): 339. CrossRef - Complications of Bariatric Surgery: What You Can Expect to See in Your GI Practice
Allison R Schulman, Christopher C Thompson
American Journal of Gastroenterology.2017; 112(11): 1640. CrossRef - Endoscopic Evaluation/Management of Bariatric Surgery Complications
Allison R. Schulman, Christopher C. Thompson
Current Treatment Options in Gastroenterology.2017; 15(4): 701. CrossRef
- Approaches to Pancreaticobiliary Endoscopy in Roux-en-Y Gastric Bypass Anatomy
- 11,027 View
- 261 Download
- 77 Web of Science
- 73 Crossref

- Repair of an Endoscopic Retrograde Cholangiopancreatography-Related Large Duodenal Perforation Using Double Endoscopic Band Ligation and Endoclipping
- Keunmo Kim, Eun Bee Kim, Yong Hyeok Choi, Youngmin Oh, Joung-Ho Han, Seon Mee Park
- Clin Endosc 2017;50(2):202-205. Published online September 13, 2016
- DOI: https://doi.org/10.5946/ce.2016.112
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic closure techniques have been introduced for the repair of duodenal wall perforations that occur during endoscopic retrograde cholangiopancreatography (ERCP). We report a case of successful repair of a large duodenal wall perforation by using double endoscopic band ligation (EBL) and an endoclip. Lateral duodenal wall perforation occurred during ERCP in a 93-year-old woman with acute calculous cholangitis. We switched to a forward endoscope that had a transparent band apparatus. A 2.0-cm ovalshaped perforation was found at the lateral duodenal wall. We repaired the perforation by sequentially performing double EBL and endoclipping. The first EBL was performed at the proximal edge of the perforation orifice, and two-thirds of the perforation were repaired. The second EBL, which also included the contents covered under the first EBL, repaired the defect almost completely. Finally, to account for the possible presence of a residual perforation, an endoclip was applied at the distal end of the perforation. The detection and closure of the perforation were completed within 10 minutes. We suggest that double EBL is an effective method for closure.
-
Citations
Citations to this article as recorded by- Endoscopic treatment of ERCP-related duodenal perforation
Nicole Evans, James L. Buxbaum
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 83. CrossRef
- Endoscopic treatment of ERCP-related duodenal perforation
- 8,835 View
- 183 Download
- 2 Web of Science
- 1 Crossref

- Mediastinal Pancreatic Pseudocysts
- Krzysztof Dąbkowski, Andrzej Białek, Maciej Kukla, Janusz Wójcik, Andrzej Smereczyński, Katarzyna Kołaczyk, Tomasz Grodzki, Teresa Starzyńska
- Clin Endosc 2017;50(1):76-80. Published online September 13, 2016
- DOI: https://doi.org/10.5946/ce.2016.089
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Mediastinal pseudocysts are a rare complication of acute pancreatitis. Lack of uniform treatment standards makes the management of this condition a clinical challenge. We report the case of a 43-year-old patient who presented with a left pleural effusion. Pleural fluid revealed a high amylase concentration consistent with a pancreaticopleural fistula. Endoscopic retrograde cholangiopancreatography (ERCP) revealed a disruption of the pancreatic duct with free outflow of contrast medium into the thoracic cavity. A pancreatic stent was placed. The second day after the ERCP, the patient developed septic shock and was admitted to the intensive care unit. Computed tomography (CT) revealed mediastinal pseudocysts and bilateral pleural effusions. After bilateral drainage of the pleural cavities, the patient improved clinically, and a follow-up CT scan showed that the fluid collection and pseudocysts had resolved. We discuss the optimal strategies for diagnosing and treating patients with pancreatic thoracic pseudocysts and fistulas, as well as review the management of these conditions.
-
Citations
Citations to this article as recorded by- Unveiling Rare Complications: Pancreatic Pseudocysts and Monomicrobial Non-neutrocytic Bacterascites in Decompensated Cirrhosis
Harshitha Reddy, Rushikesh H Dhondge, Sunil Kumar, Sourya Acharya
Cureus.2024;[Epub] CrossRef - A Rare Cause of Peri-esophageal Cystic Lesion
Xiying Dong, Dong Wu
Gastroenterology.2023; 164(2): 191. CrossRef - Diagnostic approach for mediastinal masses with radiopathological correlation
Masashi Taka, Satoshi Kobayashi, Kaori Mizutomi, Dai Inoue, Shigeyuki Takamatsu, Toshifumi Gabata, Isao Matsumoto, Hiroko Ikeda, Takeshi Kobayashi, Hiroshi Minato, Hitoshi Abo
European Journal of Radiology.2023; 162: 110767. CrossRef - Mediastinal extension of pancreatic pseudocysts causing portal hypertension
Leni Santiana, Viola Stephanie Warokko, Dikki Drajat Kusmayadi Surachman, Harry Galuh Nugraha
Radiology Case Reports.2023; 18(11): 4226. CrossRef - Acute pancreatitis: A review of diagnosis, severity prediction and prognosis assessment from imaging technology, scoring system and artificial intelligence
Jian-Xiong Hu, Cheng-Fei Zhao, Shu-Ling Wang, Xiao-Yan Tu, Wei-Bin Huang, Jun-Nian Chen, Ying Xie, Cun-Rong Chen
World Journal of Gastroenterology.2023; 29(37): 5268. CrossRef - Mediastinal pancreatobiliary pseudocysts
G.I. Dryazhenkov, I.G. Dryazhenkov, S.I. Balnykov, E.V. Kalashyan, A.A. Stepankov
Khirurgiya. Zhurnal im. N.I. Pirogova.2022; (3): 56. CrossRef - The Role of Endoscopic Ultrasound in the Interventional Management of Mediastinal Collections: A Narrative Review
Julio G Velasquez-Rodriguez, Sandra Maisterra, Ricard Ramos, Ignacio Escobar, Joan B Gornals
Cureus.2022;[Epub] CrossRef - Mediastinal Extension of Pancreatic Pseudocyst: A Rare Pediatric Presentation
Shruti Tewari, A Sushma, Rajeev Redkar
Journal of Indian Association of Pediatric Surgeons.2021; 26(1): 44. CrossRef - Predictors for external and internal pancreatic fistulas after pancreatic necrosis
L. P. Kotelnikova, S. A. Plaksin, I. G. Burnyshev, D. V. Trushnikov
Annaly khirurgicheskoy gepatologii = Annals of HPB Surgery.2021; 26(2): 39. CrossRef - Pancreatic Pseudocyst with Mediastinal Extension Presenting as Pseudo-Kirklin Sign—Multimodality Imaging
Harshini Udayakumar, Venkatraman Indiran, Kalaichezhian Mariappan, Prabakaran Maduraimuthu
Journal of Gastrointestinal and Abdominal Radiology.2020; 3(S 01): S54. CrossRef - Mediastinal pancreatic cysts: review and own clinical observations
L. P. Kotelnikova, S. A. Plaksin, L. I. Farshatova
Khirurgiya. Zhurnal im. N.I. Pirogova.2019; (7): 80. CrossRef - Isolated Mediastinal Pseudocyst of the Pancreas
Pankaj Halder, Kartik Chandra Mandal, Bidyut Debnath, Sumedha Mukherjee
Indian Pediatrics.2018; 55(3): 251. CrossRef - Pancreaticopleural Fistula: A Review of Imaging Diagnosis and Early Endoscopic Intervention
Ali Kord Valeshabad, Jennifer Acostamadiedo, Lekui Xiao, Winnie Mar, Karen L. Xie
Case Reports in Gastrointestinal Medicine.2018; 2018: 1. CrossRef
- Unveiling Rare Complications: Pancreatic Pseudocysts and Monomicrobial Non-neutrocytic Bacterascites in Decompensated Cirrhosis
- 7,644 View
- 186 Download
- 9 Web of Science
- 13 Crossref

- Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations
- Seon Mee Park
- Clin Endosc 2016;49(4):376-382. Published online July 29, 2016
- DOI: https://doi.org/10.5946/ce.2016.088
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The management strategy for endoscopic retrograde cholangiopancreatography-related duodenal perforation can be determined based on the site and extent of injury, the patient’s condition, and time to diagnosis. Most cases of perivaterian or bile duct perforation can be managed with a biliary stent or nasobiliary drainage. Duodenal wall perforations had been treated with immediate surgical repair. However, with the development of endoscopic devices and techniques, endoscopic closure has been reported to be a safe and effective treatment that uses through-the-scope clips, ligation band, fibrin glue, endoclips and endoloops, an over-the-scope clipping device, suturing devices, covering luminal stents, and open-pore film drainage. Endoscopic therapy could be instituted in selected patients in whom perforation was identified early or during the procedure. Early diagnosis, proper conservative management, and effective endoscopic closure are required for favorable outcomes of non-surgical management. If endoscopic treatment fails, or in the cases of clinical deterioration, prompt surgical management should be considered.
-
Citations
Citations to this article as recorded by- ERCP-induced perforation: review and revisit after half a century
Abdel Rahman A. A. Al Manasra, Zaid Mesmar, Tarek Manasreh, Hanan M . Hammouri, Anas Husein, Khaled Jadallah, Mohammed Bani hani, Niazy Abu Farsakh, Shatha K. Shahwan, Doaa Al-qaoud, Jehad Fataftah
F1000Research.2024; 12: 612. CrossRef - ERCP-induced perforation: review and revisit after half a century
Abdel Rahman A. A. Al Manasra, Zaid Mesmar, Tarek Manasreh, Hanan M . Hammouri, Anas Husein, Khaled Jadallah, Mohammed Bani hani, Niazy Abu Farsakh, Shatha K. Shahwan, Doaa Al-qaoud, Jehad Fataftah
F1000Research.2023; 12: 612. CrossRef - Fully covered self-expandable metal stent for intraprocedural or late-diagnosed Type-II endoscopic retrograde cholangiopancreatography-related perforations
Osman Bozbiyik, Bartu Cetin, Tufan Gumus, Fatih Tekin, Alper Uguz
BMC Gastroenterology.2022;[Epub] CrossRef - Clinical analysis of 45 cases of perforation were identified during endoscopic retrograde cholangiopancreatography procedure
Yin-Shui Miao, Yuan-Yuan Li, Bo-Wen Cheng, Yan-Fang Zhan, Sheng Zeng, Xiao-Jiang Zhou, You-Xiang Chen, Nong-Hua Lv, Guo-Hua Li
Frontiers in Medicine.2022;[Epub] CrossRef - AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review
Jeffrey H. Lee, Prashant Kedia, Stavros N. Stavropoulos, David Carr-Locke
Clinical Gastroenterology and Hepatology.2021; 19(11): 2252. CrossRef - Evaluation of complications after endoscopic retrograde cholangiopancreatography using a short type double balloon endoscope in patients with altered gastrointestinal anatomy: a single‐center retrospective study of 1,576 procedures
Mitsuo Tokuhara, Masaaki Shimatani, Toshiyuki Mitsuyama, Masataka Masuda, Takashi Ito, Sachi Miyamoto, Norimasa Fukata, Hideaki Miyoshi, Tsukasa Ikeura, Makoto Takaoka, Katsuyasu Kouda, Kazuichi Okazaki
Journal of Gastroenterology and Hepatology.2020; 35(8): 1387. CrossRef - Retracted: Endoscopic Treatment of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
Ding Shi, Jian feng Yang, Yong pan Liu
Journal of Laparoendoscopic & Advanced Surgical Techniques.2019; 29(3): 385. CrossRef - Duodenal perforation after the cutting an ENPD tube in a patient with pancreatic cancer and acute suppurative pancreatic ductitis
Akihisa OHNO, Nao FUJIMORI, Kazuhide MATSUMOTO, Katsuhito TERAMATSU, Yu TAKAMATSU, Masami MIKI, Takehiro TAKAOKA, Takamasa OONO
Suizo.2019; 34(1): 30. CrossRef - Endoscopic treatment of ERCP-related duodenal perforation
Nicole Evans, James L. Buxbaum
Techniques in Gastrointestinal Endoscopy.2019; 21(2): 83. CrossRef - Endoscopic management of iatrogenic gastrointestinal perforations
Kan Wang, Jihao Shi, Linna Ye
Laparoscopic, Endoscopic and Robotic Surgery.2019; 2(2): 41. CrossRef - The Management of Duodenal Perforation: Change Over Time. A Case Series and Literature Review
Amit Nehra, Rajesh Godara
Hellenic Journal of Surgery.2019; 91(5-6): 159. CrossRef - A Case of Unresolved and Worsening Retroperitoneal Abscess
Raghav Bansal, Mohamed Barakat, Soohwan Chun, Sonam Rosberger, Joel Baum, Melik Tiba
Case Reports in Gastrointestinal Medicine.2018; 2018: 1. CrossRef - On the feasibility of the computational modelling of the endoluminal vacuum-assisted closure of an oesophageal anastomotic leakage
Ester Comellas, Facundo J. Bellomo, Iván Rosales, Luis F. del Castillo, Ricardo Sánchez, Pau Turon, Sergio Oller
Royal Society Open Science.2018; 5(2): 171289. CrossRef - Endoscopic retrograde cholangiopancreatography complications: Techniques to reduce risk and management strategies
Paul R. Tarnasky, Prashant Kedia
International Journal of Gastrointestinal Intervention.2017; 6(1): 37. CrossRef - A systematic review of the management and outcome of ERCP related duodenal perforations using a standardized classification system
Roberto Cirocchi, Michael Denis Kelly, Ewen A. Griffiths, Renata Tabola, Massimo Sartelli, Luigi Carlini, Stefania Ghersi, Salomone Di Saverio
The Surgeon.2017; 15(6): 379. CrossRef
- ERCP-induced perforation: review and revisit after half a century
- 11,732 View
- 295 Download
- 14 Web of Science
- 15 Crossref

- Delayed Severe Hemobilia after Endoscopic Biliary Plastic Stent Insertion
- Sung Hak Lee, Seung Goun Hong, Kyoung yong Lee, Pyung Kang Park, Sung Du Kim, Mahn Lee, Dong Wook Yu, Man Yong Hong
- Clin Endosc 2016;49(3):303-307. Published online March 25, 2016
- DOI: https://doi.org/10.5946/ce.2015.081
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Hemobilia is a rare gastrointestinal bleeding, usually caused by injury to the bile duct. Hemobilia after endoscopic retrograde cholangiopancreatography (ERCP) is generally self-limiting and patients will spontaneously recover, but some severe and fatal hemorrhages have been reported. ERCP-related bowel or bile duct perforation should be managed promptly, according to the type of injury and the status of the patient. We recently experienced a case of late-onset severe hemobilia in which the patient recovered after endoscopic biliary stent insertion. The problem was attributable to ERCP-related bile duct perforation during stone removal, approximately 5 weeks prior to the hemorrhagic episode. The removal of the stent was performed 10 days before the onset of hemobilia. The bleeding was successfully treated by two sessions of transarterial coil embolization.
-
Citations
Citations to this article as recorded by- A rare incidence of a hepatic artery pseudoaneurysm following plastic biliary stent insertion
Toshihiko Motohara, Kensuke Yamamura, Shigenori Ueno, Hiroshi Takeno, Yasunori Nagayama, Eri Oda, Ryuichi Karashima, Nobuyuki Ozaki, Toshiro Masuda, Toru Beppu
Clinical Journal of Gastroenterology.2024; 17(2): 352. CrossRef - A Study on the Spectrum of Imaging Findings of Post-ERCP-Specific Complications: A Retrospective Descriptive Study
Ruchira Mukherji, Manoj Gopinath
Indian Journal of Radiology and Imaging.2024;[Epub] CrossRef - Delayed Hemobilia Caused by Penetration of Biliary Plastic Stent into Portal Vein
Jinhyong Kang, Yang Tae Park, Hyo Jung Kim, Jae Seon Kim
The Korean Journal of Pancreas and Biliary Tract.2022; 27(3): 135. CrossRef - Complications of endoscopic retrograde cholangiopancreatography: an imaging review
Dinesh Manoharan, Deep Narayan Srivastava, Arun Kumar Gupta, Kumble Seetharama Madhusudhan
Abdominal Radiology.2019; 44(6): 2205. CrossRef - Recurrent Bleeding from a Hepatic Artery Pseudoaneurysm after Biliary Stent Placement
Kenji Yamauchi, Daisuke Uchida, Hironari Kato, Hiroyuki Okada
Internal Medicine.2018; 57(1): 49. CrossRef - Transcatheter arterial embolization for iatrogenic bleeding after endoscopic ultrasound-guided pancreaticobiliary drainage
N.J. Lee, J.H. Shin, S.S. Lee, D.H. Park, S.K. Lee, H.-K. Yoon
Diagnostic and Interventional Imaging.2018; 99(11): 717. CrossRef - Hemobilia due to arteriobiliary fistula complicating ERCP for residual bile duct stone in a case of Mirizzi syndrome
Surendrakumar Mathur, Vinaykumar Thapar, Vasudev Chowda
Annals of Hepato-Biliary-Pancreatic Surgery.2017; 21(2): 88. CrossRef
- A rare incidence of a hepatic artery pseudoaneurysm following plastic biliary stent insertion
- 9,343 View
- 76 Download
- 8 Web of Science
- 7 Crossref

- The Clinical Usefulness of Simultaneous Placement of Double Endoscopic Nasobiliary Biliary Drainage
- Hong Jun Kim, Sung Koo Lee, Choong Heon Ryu, Do Hyun Park, Sang Soo Lee, Dong Wan Seo, Myung-Hwan Kim
- Clin Endosc 2015;48(6):542-548. Published online November 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.6.542
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: To evaluate the technical feasibility and clinical efficacy of double endoscopic nasobiliary drainage (ENBD) as a new method of draining multiple bile duct obstructions.
Methods
A total of 38 patients who underwent double ENBD between January 2004 and February 2010 at the Asan Medical Center were retrospectively analyzed. We evaluated indications, laboratory results, and the clinical course.
Results
Of the 38 patients who underwent double ENBD, 20 (52.6%) had Klatskin tumors, 12 (31.6%) had hepatocellular carcinoma, 3 (7.9%) had strictures at the anastomotic site following liver transplantation, and 3 (7.9%) had acute cholecystitis combined with cholangitis. Double ENBD was performed to relieve multiple biliary obstruction in 21 patients (55.1%), drain contrast agent filled during endoscopic retrograde cholangiopancreatography in 4 (10.5%), obtain cholangiography in 4 (10.5%), drain hemobilia in 3 (7.9%), relieve Mirizzi syndrome with cholangitis in 3 (7.9%), and relieve jaundice in 3 (7.9%).
Conclusions
Double ENBD may be useful in patients with multiple biliary obstructions. -
Citations
Citations to this article as recorded by- High-throughput metabolomics reveals the perturbed metabolic pathways and biomarkers of Yang Huang syndrome as potential targets for evaluating the therapeutic effects and mechanism of geniposide
Heng Fang, Aihua Zhang, Xiaohang Zhou, Jingbo Yu, Qi Song, Xijun Wang
Frontiers of Medicine.2020; 14(5): 651. CrossRef - Can Endoscopic Nasobiliary Drainage Involving Two Catheters Be Used to Treat Various Conditions?
Dong Wook Lee, Ho Gak Kim
Clinical Endoscopy.2015; 48(6): 464. CrossRef
- High-throughput metabolomics reveals the perturbed metabolic pathways and biomarkers of Yang Huang syndrome as potential targets for evaluating the therapeutic effects and mechanism of geniposide
- 13,053 View
- 95 Download
- 2 Web of Science
- 2 Crossref

- Single Balloon Enteroscopy-Assisted Endoscopic Retrograde Cholangiopancreatography in Patients Who Underwent a Gastrectomy with Roux-en-Y Anastomosis: Six Cases from a Single Center
- Jae Seung Soh, Dong-Hoon Yang, Sang Soo Lee, Seohyun Lee, Jungho Bae, Jeong-Sik Byeon, Seung-Jae Myung, Suk-Kyun Yang
- Clin Endosc 2015;48(5):452-457. Published online September 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.5.452
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Patients with altered anatomy such as a Roux-en-Y anastomosis often present with various pancreaticobiliary problems requiring therapeutic intervention. However, a conventional endoscopic approach to the papilla is very difficult owing to the long afferent limb and acute angle of a Roux-en-Y anastomosis. Balloon-assisted enteroscopy can be used for endoscopic retrograde cholangiopancreatography (ERCP) in patients with altered anatomy. We experienced six cases of Roux-en-Y anastomosis with biliary problems, and attempted ERCP using single balloon enteroscopy (SBE). SBE insertion followed by replacement with a conventional endoscope was attempted in five of six patients. The papilla was successfully approached using SBE in all cases. However, therapeutic intervention was completed in only three cases because of poor maneuverability caused by postoperative adhesion. We conclude that in patients with Roux-en-Y anastomosis, the ampulla can be readily accessed with SBE, but longer dedicated accessories are necessary to improve this therapeutic intervention.
-
Citations
Citations to this article as recorded by- Single Balloon Enteroscopy-Guided Endoscopic Retrograde Cholangiopancreatography in Surgically Altered Anatomy: Long vs. Short Type
Chang-Hwan Park
The Korean Journal of Pancreas and Biliary Tract.2021; 26(3): 181. CrossRef - Direct Insertion of a Short-Type Single-Balloon Enteroscope and Using a Stent Retriever to Treat Difficult Bile Duct Stones in Surgically Altered Anatomy
Takashi Sasaki, Naoki Sasahira
Clinical Endoscopy.2021; 54(6): 937. CrossRef - Single-balloon enteroscopy-assisted ERCP in patients with Roux-en-Y anatomy and choledocholithiasis: do technical improvements mean better outcomes?
Jesús Espinel Díez, María Eugenia Pinedo Ramos
Revista Española de Enfermedades Digestivas.2020;[Epub] CrossRef - Application of single balloon enteroscopy-assisted therapeutic endoscopic retrograde cholangiopancreatography in patients after bilioenteric Roux-en-Y anastomosis: Experience of multi-disciplinary collaboration
Wen-Guang Wu, Lu-Cui Qin, Xiao-Ling Song, Ming-Ning Zhao, Wen-Jie Zhang, Jun Gu, Hao Weng, Ying-Bin Liu, Yi Zhang, Chun-Ying Qu, Lei-Ming Xu, Xue-Feng Wang
World Journal of Gastroenterology.2019; 25(36): 5505. CrossRef - Comparison between Enteroscopy-Based and Laparoscopy-Assisted ERCP for Accessing the Biliary Tree in Patients with Roux-en-Y Gastric Bypass: Systematic Review and Meta-analysis
Alberto Machado da Ponte-Neto, Wanderley M. Bernardo, Lara M. de A. Coutinho, Iatagan Rocha Josino, Vitor Ottoboni Brunaldi, Diogo T. H. Moura, Paulo Sakai, Rogério Kuga, Eduardo G. H. de Moura
Obesity Surgery.2018; 28(12): 4064. CrossRef - Impact of a Newly Developed Short Double-Balloon Enteroscope on Stent Placement in Patients with Surgically Altered Anatomies
Koichiro Tsutsumi, Hironari Kato, Hiroyuki Okada
Gut and Liver.2017; 11(2): 306. CrossRef
- Single Balloon Enteroscopy-Guided Endoscopic Retrograde Cholangiopancreatography in Surgically Altered Anatomy: Long vs. Short Type
- 8,102 View
- 79 Download
- 5 Web of Science
- 6 Crossref

- Current Issues in Duodenoscope-Associated Infections: Now Is the Time to Take Action
- Junghoon Ha, Byoung Kwan Son
- Clin Endosc 2015;48(5):361-363. Published online September 30, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.5.361
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub A duodenoscope has a very complex structure that contains many small parts which make reprocessing more challenging. The difficulty in cleaning duodenoscopes contributes to a higher risk of infection than that of conventional gastrointestinal endoscopes. However, a duodenoscope shares similar disinfection process with other gastrointestinal endoscopes. Recent outbreaks of carbapenem-resistant Enterobacteriaceae (CRE) infections associated with duodenoscopes used for endoscopic retrograde cholangiopancreatography procedures have raised many concerns worldwide. Duodenoscope-associated infections involving CRE or other multidrug-resistant bacteria pose a great threat to patients undergoing procedures using duodenoscopes and should be dealt with a great concern. Updated guidelines regarding cleaning and disinfection of duodenoscope needs to be developed urgently to prevent transmission of infection and ensure patient safety. Meanwhile, healthcare staff should pay special attention to thorough cleaning and disinfection of duodenoscopes.
-
Citations
Citations to this article as recorded by- ERCP with single-use disposable duodenoscopes in four different set-ups
Ronja Lagström, Svend Knuhtsen, Trine Stigaard, Mustafa Bulut
BMJ Case Reports.2023; 16(2): e251514. CrossRef - Disposable duodenoscopes. Is healthcare system affordability the main hindrance?
Enrique Vázquez-Sequeiros, Juan Ángel González Martín, Agustín Albillos Martínez
Revista Española de Enfermedades Digestivas.2022;[Epub] CrossRef - Storage of gastrointestinal endoscopes: when is the safe time for re-use?
Naiara Bussolotti Garcia, Adriana Cristina de Oliveira
Revista Brasileira de Enfermagem.2022;[Epub] CrossRef - Single Use (Disposable) Duodenoscope: Recent Development and Future
Kihyun Ryu, Sunguk Jang
Clinical Endoscopy.2022; 55(2): 191. CrossRef - Duodenoscope-related infections: patient-ready versus single-use duodenoscopes. Is a new era for endoscopic retrograde cholangiopancreatography on the horizon?
Damiano BISOGNI, Roberto MANETTI, Luca TALAMUCCI, Michele ROSSI, Fabio STADERINI, Maurizio MORONI, Fabio CIANCHI
Minerva Surgery.2021;[Epub] CrossRef - Results of duodenoscope culture and quarantine after manufacturer-recommended cleaning process
Jacob A. Mark, Karin Underberg, Robert E. Kramer
Gastrointestinal Endoscopy.2020; 91(6): 1328. CrossRef - Elevating the standard of endoscope processing: Terminal sterilization of duodenoscopes using a hydrogen peroxide–ozone sterilizer
Vanessa Molloy-Simard, Jean-Luc Lemyre, Karine Martel, Bradley J. Catalone
American Journal of Infection Control.2019; 47(3): 243. CrossRef - Getting to zero: Enhanced reprocessing and future directions
M. Phillip Fejleh, Jennifer Phan, Neil B. Marya, Stephen Kim, Zachary A. Rubin, V. Raman Muthusamy
Techniques in Gastrointestinal Endoscopy.2019; 21(4): 150626. CrossRef - Duodenoscope-Associated Infections: A Literature Review and Update
Il Hwan Oh, Byoung Kwan Son
The Korean Journal of Pancreas and Biliary Tract.2018; 23(4): 145. CrossRef
- ERCP with single-use disposable duodenoscopes in four different set-ups
- 5,276 View
- 110 Download
- 10 Web of Science
- 9 Crossref

- IgG4 Levels in Bile for Distinguishing IgG4-Associated Cholangiopathy from Other Biliary Disorders: A Single Blinded Pilot Study
- Udayakumar Navaneethan, Norma G. Gutierrez, Ramprasad Jegadeesan, Preethi GK Venkatesh, Earl Poptic, Madhusudhan R. Sanaka, John J. Vargo, Mansour A. Parsi
- Clin Endosc 2014;47(6):555-559. Published online November 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.6.555
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Immunoglobulin G4 (IgG4)-associated cholangiopathy (IAC) is an inflammatory disease and may mimic primary sclerosing cholangitis (PSC), cholangiocarcinoma (CCA), or pancreatic cancer on cholangiography. We investigated whether IgG4 levels in bile aspirated during endoscopic retrograde cholangiopancreatography (ERCP) can distinguish IAC from PSC, CCA, and pancreatic cancer.
Methods Bile was aspirated directly from the common bile duct during ERCP in patients with IAC prior to steroid therapy. For control purposes, bile was obtained from patients with PSC, CCA, pancreatic cancer, and benign biliary conditions (sphincter of oddi dysfunction/choledocholithiasis).
Results Biliary IgG4 levels were measured in 54 patients. The median bile IgG4 levels were markedly elevated in patients with IAC (5.5 mg/dL; interquartile range [IQR], 5.1 to 15.6) as compared to patients with benign biliary conditions (0 mg/dL; IQR, 0 to 0.1;
p =0.003). The median biliary IgG4 levels in PSC, CCA, and pancreatic cancer were 1.2 (IQR, 0.2 to 3.8), 0.9 (IQR, 0.2 to 3.4), and 0.2 mg/dL (IQR, 0.1 to 0.8), respectively. A cutoff value of 3.8 mg/dL distinguished IAC from PSC and CCA patients with 100% and 76.9% sensitivity and specificity, respectively.Conclusions The results of this pilot study suggest that measurement of biliary IgG4 levels may have clinical value in distinguishing patients with IAC from biliary disorders that can mimic IAC.
-
Citations
Citations to this article as recorded by- Clinical Features, Differential Diagnosis and Treatment of IgG4-Related Sclerosing Cholangitis
A. K. Guseva, A. V. Okhlobystin
The Russian Archives of Internal Medicine.2024; 14(2): 96. CrossRef - Review of primary sclerosing cholangitis with increased IgG4 levels
Charis D Manganis, Roger W Chapman, Emma L Culver
World Journal of Gastroenterology.2020; 26(23): 3126. CrossRef - Immunoglobulin G4-related cholangiopathy
Lucas J. Maillette de Buy Wenniger, Ulrich Beuers
Current Opinion in Gastroenterology.2015; 31(3): 252. CrossRef - Diagnosis of Immunoglobulin G4-Related Sclerosing Cholangitis
Ji Kon Ryu
Clinical Endoscopy.2014; 47(6): 476. CrossRef
- Clinical Features, Differential Diagnosis and Treatment of IgG4-Related Sclerosing Cholangitis
- 6,158 View
- 56 Download
- 3 Web of Science
- 4 Crossref

- The Management of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforation
- Kwang Bum Cho
- Clin Endosc 2014;47(4):341-345. Published online July 28, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.4.341
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Uneventful duodenal perforation during endoscopic retrograde cholangiopancreatography (ERCP) is an uncommon but occasionally fatal complication. ERCP-related perforations may occur during sphincterotomy and improper manipulation of the equipment and scope. Traditionally, duodenal perforation has been treated with early surgical repair. Recently, nonoperative early endoscopic management techniques including clips or fibrin glue have been reported. In the present paper we review the literature pertaining to the treatment of perforations.
-
Citations
Citations to this article as recorded by- A Study on the Spectrum of Imaging Findings of Post-ERCP-Specific Complications: A Retrospective Descriptive Study
Ruchira Mukherji, Manoj Gopinath
Indian Journal of Radiology and Imaging.2024;[Epub] CrossRef - Outcomes and risk factors for ERCP-related complications in a predominantly black urban population
Nathaniel Kwak, Daniel Yeoun, Fray Arroyo-Mercado, Ghassan Mubarak, Derrick Cheung, Shivakumar Vignesh
BMJ Open Gastroenterology.2020; 7(1): e000462. CrossRef - Retracted: Endoscopic Treatment of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
Ding Shi, Jian feng Yang, Yong pan Liu
Journal of Laparoendoscopic & Advanced Surgical Techniques.2019; 29(3): 385. CrossRef - Complications of endoscopic retrograde cholangiopancreatography: an imaging review
Dinesh Manoharan, Deep Narayan Srivastava, Arun Kumar Gupta, Kumble Seetharama Madhusudhan
Abdominal Radiology.2019; 44(6): 2205. CrossRef - Duodenal perforation after the cutting an ENPD tube in a patient with pancreatic cancer and acute suppurative pancreatic ductitis
Akihisa OHNO, Nao FUJIMORI, Kazuhide MATSUMOTO, Katsuhito TERAMATSU, Yu TAKAMATSU, Masami MIKI, Takehiro TAKAOKA, Takamasa OONO
Suizo.2019; 34(1): 30. CrossRef - Efficacy and safety of endoscopic submucosal dissection for non-ampullary duodenal polyps: A systematic review and meta-analysis
Daisuke Watanabe, Hiroki Hayashi, Yuki Kataoka, Tadayuki Hashimoto, Katsuro Ichimasa, Hideyuki Miyachi, Shinwa Tanaka, Takashi Toyonaga
Digestive and Liver Disease.2019; 51(6): 774. CrossRef - Endoscopic management of iatrogenic gastrointestinal perforations
Kan Wang, Jihao Shi, Linna Ye
Laparoscopic, Endoscopic and Robotic Surgery.2019; 2(2): 41. CrossRef - Current approaches to the treatment of complications of endoscopic transpapillary interventions
S. G. Shapovaliyants, S. A. Budzinskiy, E. D. Fedorov, M. V. Bordikov, M. A. Zakharova
Annaly khirurgicheskoy gepatologii = Annals of HPB Surgery.2019; 24(2): 74. CrossRef - Surgical Treatment for Septic Complications in Patients with Duodenal Perforation Following Endoscopic Retrograde Transpapillary Interventions
V. L. Korobka, S. V. Tolstopyatov, A. M. Shapovalov
Innovative medicine of Kuban.2019; 14(2): 13. CrossRef - Nadir bir ERCP komplikasyonu nedeniyle olgu sunumu; retroperitoneal perforasyon
Pınar YILDIZ, Tuncer TEMEL, Erkin ÖZTAŞ, Selçuk DİŞİBEYAZ
Endoskopi Gastrointestinal.2019; 27(3): 97. CrossRef - ERCP-Related Duodenal Perforation Presenting as Pneumoscrotum
Mohammad Saud Khan, Faisal Jamal, Zubair Khan, Abhinav Tiwari, Hermann Simo, Himani Sharma
Case Reports in Gastroenterology.2018; 12(1): 1. CrossRef - Emergent Endoscopic Retrograde Cholangiopancreatography with Placement of Biliary Double Stents to Salvage Endoscopic Retrograde Cholangiopancreatography-Induced Stapfer's Type II Perforation
Ping Yue, Wen-Bo Meng, Joseph W Leung, Lei Zhang, Xiao-Liang Zhu, Hui Zhang, Hai-Ping Wang, Zheng-Feng Wang, Ke-Xiang Zhu, Long Miao, Wen-Ce Zhou, Xun Li
Chinese Medical Journal.2018; 131(19): 2346. CrossRef - What is your diagnosis? Abdominal pain complicating endoscopic retrograde cholangiopancreatography
Haifa Al Awadhi, Ali Al Mehaidib
International Journal of Pediatrics and Adolescent Medicine.2016; 3(2): 85. CrossRef - Answer
Haifa Al Awadhi, Ali Al Mehaidib
International Journal of Pediatrics and Adolescent Medicine.2016; 3(2): e1. CrossRef - Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations
Seon Mee Park
Clinical Endoscopy.2016; 49(4): 376. CrossRef - Unexpectedly Discovered Duodenal Perforation
Hye Min Park, Min Young Do, Sei Myung Choi, Kyung Ho Yang, Chang Jae Hur, Kwang Bum Cho
Korean Journal of Pancreas and Biliary Tract.2015; 20(4): 241. CrossRef - Duodenal perforation following esophagogastroduodenoscopy (EGD) with cautery and epinephrine injection for peptic ulcer disease: An interesting case of nonoperative management in the medical intensive care unit (MICU)
Jason Chertoff, Vikas Khullar, Lucas Burke
International Journal of Surgery Case Reports.2015; 10: 121. CrossRef - ERCP-induced duodenal perforation successfully treated with endoscopic purse-string suture: a case report
Quanpeng Li, Jie Ji, Fei Wang, Xianxiu Ge, Junjie Nie, Boming Xu, Xiuhua Zhang, Guobing Jiang, Lin Miao
Oncotarget.2015; 6(19): 17847. CrossRef
- A Study on the Spectrum of Imaging Findings of Post-ERCP-Specific Complications: A Retrospective Descriptive Study
- 10,038 View
- 190 Download
- 16 Web of Science
- 18 Crossref

- Preparation of High-Risk Patients and the Choice of Guidewire for a Successful Endoscopic Retrograde Cholangiopancreatography Procedure
- Tae Hoon Lee, Young Kyu Jung, Sang-Heum Park
- Clin Endosc 2014;47(4):334-340. Published online July 28, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.4.334
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Endoscopic retrograde cholangiopancreatography (ERCP) is an essential technique for the diagnosis and treatment of pancreatobiliary diseases. However, ERCP-related complications such as pancreatitis, cholangitis, hemorrhage, and perforation may be problematic. For a successful and safe ERCP, preprocedural evaluations of the patients and intervention-related risk factors are needed. Furthermore, in light of the recent population aging and increase in chronic cardiopulmonary diseases in Korea, precautions including endoscopic sedation and prevention of cardiopulmonary complications should be considered. In this literature review, we describe these risk factors and the use of endoscopic sedation. In addition, we reviewed the commonly available guidewires, including their materials and options, used as a basic accessory for ERCP procedures.
-
Citations
Citations to this article as recorded by- Structural factors influencing the clinical performance of 0.025-inch guidewires for pancreatobiliary endoscopy: An experimental study
Takehiko Koga, Naoaki Tsuchiya, Yusuke Ishida, Takanori Kitaguchi, Keisuke Matsumoto, Makoto Fukuyama, Satoki Kojima, Norihiro Kojima, Fumihito Hirai
Endoscopy International Open.2024; 12(05): E666. CrossRef - Racial disparities in endoscopic retrograde cholangiopancreatography (ERCP) utilization in the United States: are we getting better?
Dushyant Singh Dahiya, Abhilash Perisetti, Neil Sharma, Sumant Inamdar, Hemant Goyal, Amandeep Singh, Laura Rotundo, Rajat Garg, Chin-I Cheng, Sailaja Pisipati, Mohammad Al-Haddad, Madhusudhan Sanaka
Surgical Endoscopy.2023; 37(1): 421. CrossRef - Comparison of guidewires for successful cannulation of biliary stenosis and targeting of biliary branches in ERCP
Masanori Kobayashi, Hiromune Katsuda, Kazuo Ohtsuka, Ryuichi Okamoto
Endoscopy International Open.2023; 11(09): E805. CrossRef - Prevention of Post-ERCP Pancreatitis: Pro-gress in Different Procedural Techniques
永烜 张
Advances in Clinical Medicine.2022; 12(11): 10124. CrossRef - Bedside Percutaneous Approach in a Critically Ill ICU Patient with Complex Pancreatobiliary Disorder Followed by Endoscopic Approach: Lessons Learnt from a Tertiary Referral Center
Cosmas Rinaldi Adithya Lesmana, Caecilia Herjuningtyas, Sri Inggriani, Yulia Estu Pratiwi, Laurentius A. Lesmana
Case Reports in Gastroenterology.2021; 15(1): 210. CrossRef - Technical Reports of Endoscopic Retrograde Cholangiopancreatography Guidewires on the Basis of Physical Properties
Chang-Il Kwon, Dong Hee Koh, Tae Jun Song, Won Suk Park, Dong Hang Lee, Seok Jeong
Clinical Endoscopy.2020; 53(1): 65. CrossRef - PREDICTIVE FACTORS FOR POST-ERCP BLEEDING. INFLUENCE OF DIRECT ORAL ANTICOAGULANTS
Ernesto Parras Castañera, Pelayo Rodríguez López, Alberto Álvarez Delgado, Fernando Muñoz Núñez, Fernando Geijo Martínez, Antonio Velasco Guardado
Revista Española de Enfermedades Digestivas.2020;[Epub] CrossRef - Current approaches to the treatment of complications of endoscopic transpapillary interventions
S. G. Shapovaliyants, S. A. Budzinskiy, E. D. Fedorov, M. V. Bordikov, M. A. Zakharova
Annaly khirurgicheskoy gepatologii = Annals of HPB Surgery.2019; 24(2): 74. CrossRef - Efficacy of midazolam‐ versus propofol‐based sedations by non‐anesthesiologists during therapeutic endoscopic retrograde cholangiopancreatography in patients aged over 80 years
Su Jung Han, Tae Hoon Lee, Sang‐Heum Park, Young Sin Cho, Yun Nah Lee, Yunho Jung, Hyun Jong Choi, Il‐Kwun Chung, Sang‐Woo Cha, Jong Ho Moon, Young Deok Cho, Sun‐Joo Kim
Digestive Endoscopy.2017; 29(3): 369. CrossRef - Pancreatic Stenting Reduces Post-ERCP Pancreatitis and Biliary Sepsis in High-Risk Patients: A Randomized, Controlled Study
He-Kun Yin, Hai-En Wu, Qi-Xiang Li, Wei Wang, Wei-Lin Ou, Harry Hua-Xiang Xia
Gastroenterology Research and Practice.2016; 2016: 1. CrossRef - Optimal Use of Wire-Assisted Techniques and Precut Sphincterotomy
Tae Hoon Lee, Sang-Heum Park
Clinical Endoscopy.2016; 49(5): 467. CrossRef - Highlights from the 50th Seminar of the Korean Society of Gastrointestinal Endoscopy
Eun Young Kim, Il Ju Choi, Kwang An Kwon, Ji Kon Ryu, Seok Ho Dong, Ki Baik Hahm
Clinical Endoscopy.2014; 47(4): 285. CrossRef
- Structural factors influencing the clinical performance of 0.025-inch guidewires for pancreatobiliary endoscopy: An experimental study
- 7,785 View
- 84 Download
- 10 Web of Science
- 12 Crossref

- Acute Duodenal Ischemia and Periampullary Intramural Hematoma after an Uneventful Endoscopic Retrograde Cholangiopancreatography in a Patient with Primary Myelofibrosis
- Chang Ho Jung, Jong Jin Hyun, Dae Hoe Gu, Eul Sun Moon, Jae Seon Kim, Hong Sik Lee, Chang Duck Kim
- Clin Endosc 2014;47(3):270-274. Published online May 31, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.3.270
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Acute duodenal ischemia and periampullary intramural hematoma are rare complications after endoscopic retrograde cholangiopancreatography (ERCP). A 77-year-old man with splenomegaly complained of abdominal pain caused by common bile duct (CBD) stone. After successful removal of the CBD stone without immediate complications, the patient developed intramural hematoma around the ampulla of Vater along with diffuse duodenal edema. The findings were compatible with acute intestinal ischemia, and further evaluation revealed that he had underlying primary myelofibrosis. Myeloproliferative diseases are known to be significantly associated with an increased risk of thrombohemorrhagic complications. Therefore, particular attention should be given to this group of patients when a high-risk procedure such as ERCP is performed.
-
Citations
Citations to this article as recorded by- Ischemic duodenitis after endoscopic retrograde cholangiopancreatography‐related procedure
Yuki Tanisaka, Akashi Fujita, Shomei Ryozawa
Digestive Endoscopy.2022; 34(6): 1264. CrossRef - Ruptured Dissecting Intramural Duodenal Hematoma Following Endoscopic Retrograde Cholangiopancreatography
Eric Weiss, Madeline Tadley, Pak S. Leung, Mark Kaplan
ACG Case Reports Journal.2017; 4(1): e70. CrossRef
- Ischemic duodenitis after endoscopic retrograde cholangiopancreatography‐related procedure
- 6,265 View
- 66 Download
- 2 Web of Science
- 2 Crossref

- Comparison between Midazolam Used Alone and in Combination with Propofol for Sedation during Endoscopic Retrograde Cholangiopancreatography
- Yu Seok Kim, Myung-Hwan Kim, Seung Uk Jeong, Byung Uk Lee, Sang Soo Lee, Do Hyun Park, Dong-Wan Seo, Sung Koo Lee
- Clin Endosc 2014;47(1):94-100. Published online January 24, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.1.94
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims Endoscopic retrograde cholangiopancreatography (ERCP) is an uncomfortable procedure that requires adequate sedation for its successful conduction. We investigated the efficacy and safety of the combined use of intravenous midazolam and propofol for sedation during ERCP.
Methods A retrospective review of patient records from a single tertiary care hospital was performed. Ninety-four patients undergoing ERCP received one of the two medication regimens, which was administered by a nurse under the supervision of a gastroenterologist. Patients in the midazolam (M) group (
n =44) received only intravenous midazolam, which was titrated to achieve deep sedation. Patients in the midazolam pulse propofol (MP) group (n =50) initially received an intravenous combination of midazolam and propofol, and then propofol was titrated to achieve deep sedation.Results The time to the initial sedation was shorter in the MP group than in the M group (1.13 minutes vs. 1.84 minutes, respectively;
p <0.001). The recovery time was faster in the MP group than in the M group (p =0.031). There were no significant differences between the two groups with respect to frequency of adverse events, pain experienced by the patient, patient discomfort, degree of amnesia, and gag reflex. Patient cooperation, rated by the endoscopist as excellent, was greater in the MP group than in the M group (p =0.046).Conclusions The combined use of intravenous midazolam and propofol for sedation during ERCP is more effective than midazolam alone. There is no difference in the safety of the procedure.
-
Citations
Citations to this article as recorded by- Sedation in the Endoscopy Suite
Katherine B. Hagan, Selvi Thirumurthi, Raju Gottumukkala, John Vargo
Current Treatment Options in Gastroenterology.2016; 14(2): 194. CrossRef - Sedation during endoscopic retrograde cholangiopancreatography: a randomized controlled study of patient-controlled propofol sedation and that given by a nurse anesthetist
Andreas Nilsson, Benjamin Grossmann, Eric Kullman, Eva Uustal, Folke Sjöberg, Lena Nilsson
Scandinavian Journal of Gastroenterology.2015; 50(10): 1285. CrossRef - Non‐radiation endoscopic retrograde cholangiopancreatography in the management of choledocholithiasis during pregnancy
Wenming Wu, Douglas O. Faigel, Gang Sun, Yunsheng Yang
Digestive Endoscopy.2014; 26(6): 691. CrossRef - Monitored Anesthesia Care for Sedation during Endoscopic Retrograde Cholangiopancreatography
Young Duck Shin
Korean Journal of Pancreas and Biliary Tract.2014; 19(2): 59. CrossRef - Prerequisites of Colonoscopy
Kyong Hee Hong, Yun Jeong Lim
Clinical Endoscopy.2014; 47(4): 324. CrossRef
- Sedation in the Endoscopy Suite
- 7,283 View
- 79 Download
- 5 Web of Science
- 5 Crossref

- Histological Changes in the Bile Duct after Long-Term Placement of a Fully Covered Self-Expandable Metal Stent within a Common Bile Duct: A Canine Study
- Sang Soo Lee, Tae Jun Song, Mee Joo, Do Hyun Park, Dong Wan Seo, Sung Koo Lee, Myung-Hwan Kim
- Clin Endosc 2014;47(1):84-93. Published online January 24, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.1.84
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims To date, it has been difficult to determine the optimal stenting duration of a fully covered self-expandable metal stent (FCSEMS) in a benign biliary stricture. The purpose of this study was to identify the histopathological changes in a bile duct resulting from long-term placement of a FCSEMS.
Methods An FCSEMS was inserted into the common bile duct of 12 canines, and the animals were divided into four groups. Posteuthanasia, necropsy was performed to examine the histopathological changes in the bile ducts after 1, 3, 6, and 9 months.
Results The results of necropsy showed that the covered membranes of the FCSEMSs were intact and easily removed from the bile ducts in 11 of the canines. Severe epithelial hyperplasia of the stented bile duct and epithelial ingrowth into the stent occurred in one animal (from the 3-month group). On histopathological examination, mild inflammatory changes were observed in the stented bile ducts, and there was no significant difference between the four groups. Among the 12 animals, five had
de novo stricture.Conclusions An FCSEMS can be inserted into the bile duct without severe histopathological changes up until 9 months. However, a
de novo stricture and severe epithelial hyperplasia relating to the stent insertion might occur.-
Citations
Citations to this article as recorded by- Clinical use of uncovered balloon‐expandable metallic biliary stents for treatment of extrahepatic biliary tract obstructions in cats and dogs: 11 cases (2012–2022)
Julia L. Bergen, Blake M. Travis, Fred S. Pike
Veterinary Surgery.2024; 53(2): 320. CrossRef - Feasibility of in vivo swine models using guide wire-assisted intraductal radiofrequency ablation for benign biliary stricture
Jae Keun Park, Ju-Il Yang, Joo Kyung Park, Kwang Hyuck Lee, Jong Kyun Lee, Kyu Taek Lee
Scientific Reports.2023;[Epub] CrossRef - Outcomes of double-layer continuous suture hepaticojejunostomy in pancreatoduodenectomy and total pancreatectomy
Niccolò Napoli, Emanuele F. Kauffmann, Rosilde Caputo, Michael Ginesini, Fabio Asta, Cesare Gianfaldoni, Gabriella Amorese, Fabio Vistoli, Ugo Boggi
HPB.2022; 24(10): 1738. CrossRef - Controversial issues of biliary stenting in patients with proximal biliary obstruction
J. V. Kulezneva, O. V. Melekhina, A. B. Musatov, M. G. Efanov, V. V. Tsvirkun, I. Yu. Nedoluzhko, K. V. Shishin, K. K. Salnikov, D. F. Kantimerov
Annaly khirurgicheskoy gepatologii = Annals of HPB Surgery.2021; 26(3): 79. CrossRef - A systematic review of biodegradable biliary stents: promising biocompatibility without stent removal
Antti Siiki, Juhani Sand, Johanna Laukkarinen
European Journal of Gastroenterology & Hepatology.2018; 30(8): 813. CrossRef - Novel flower-type covered metal stent to prevent cholecystitis: experimental study in a pig model
Young Sik Woo, Kwang Hyuck Lee, Jong Kyun Lee, Dong Hyo Noh, Joo Kyung Park, Kyu Taek Lee, Kee-Taek Jang
Surgical Endoscopy.2016; 30(3): 1141. CrossRef - Biodegradable biliary stents have a different effect than covered metal stents on the expression of proteins associated with tissue healing in benign biliary strictures
Antti Siiki, Ralf Jesenofsky, Matthias Löhr, Isto Nordback, Minna Kellomäki, Heidi Gröhn, Joonas Mikkonen, Juhani Sand, Johanna Laukkarinen
Scandinavian Journal of Gastroenterology.2016; 51(7): 880. CrossRef - Fabrication of a silver particle-integrated silicone polymer-covered metal stent against sludge and biofilm formation and stent-induced tissue inflammation
Tae Hoon Lee, Bong Seok Jang, Min Kyo Jung, Chan Gi Pack, Jun-Ho Choi, Do Hyun Park
Scientific Reports.2016;[Epub] CrossRef - Metal Stenting in Benign Biliary Strictures
Ji Kon Ryu
Clinical Endoscopy.2014; 47(1): 5. CrossRef - Best endoscopic stents for the biliary tree and pancreas
Todd H. Baron
Current Opinion in Gastroenterology.2014; 30(5): 453. CrossRef
- Clinical use of uncovered balloon‐expandable metallic biliary stents for treatment of extrahepatic biliary tract obstructions in cats and dogs: 11 cases (2012–2022)
- 7,630 View
- 87 Download
- 10 Web of Science
- 10 Crossref


 KSGE
KSGE


 First
First Prev
Prev



