Search
- Page Path
- HOME > Search
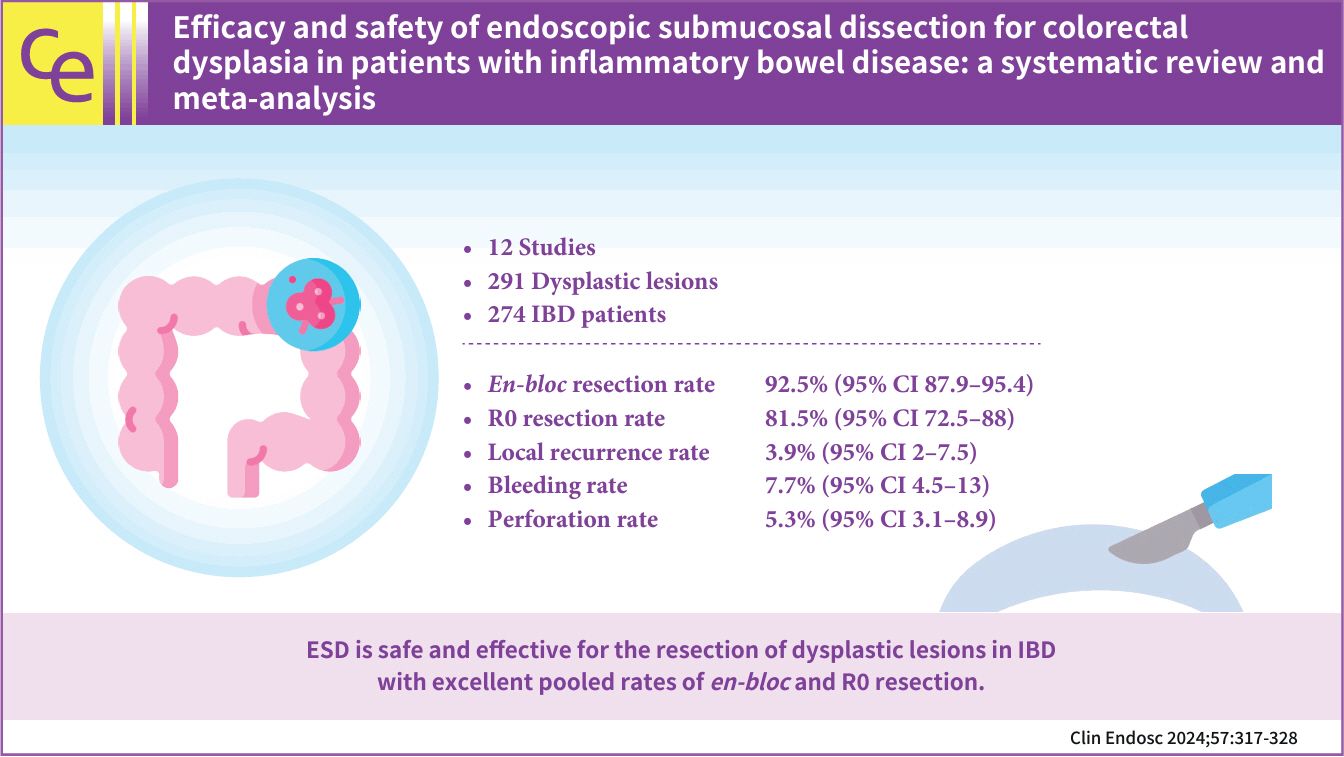
- Efficacy and safety of endoscopic submucosal dissection for colorectal dysplasia in patients with inflammatory bowel disease: a systematic review and meta-analysis
- Talia F. Malik, Vaishnavi Sabesan, Babu P. Mohan, Asad Ur Rahman, Mohamed O. Othman, Peter V. Draganov, Gursimran S. Kochhar
- Clin Endosc 2024;57(3):317-328. Published online February 29, 2024
- DOI: https://doi.org/10.5946/ce.2023.205
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub 
- Background
/Aims: In this meta-analysis, we studied the safety and efficacy of endoscopic submucosal dissection (ESD) for colorectal dysplasia in patients with inflammatory bowel disease (IBD).
Methods
Multiple databases were searched, and studies were retrieved based on pre-specified criteria until October 2022. The outcomes assessed were resection rates, procedural complications, local recurrence, metachronous tumors, and the need for surgery after ESD in IBD. Standard meta-analysis methods were followed using the random-effects model, and I2% was used to assess heterogeneity.
Results
Twelve studies comprising 291 dysplastic lesions in 274 patients were included with a median follow-up of 25 months. The pooled en-bloc resection, R0 resection, and curative resection rates were 92.5% (95% confidence interval [CI], 87.9%–95.4%; I2=0%), 81.5% (95% CI, 72.5%–88%; I2=43%), and 48.9% (95% CI, 32.1%–65.9%; I2=87%), respectively. The local recurrence rate was 3.9% (95% CI, 2%–7.5%; I2=0%). The pooled rates of bleeding and perforation were 7.7% (95% CI, 4.5%–13%; I2=10%) and 5.3% (95% CI, 3.1%–8.9%; I2=0%), respectively. The rates of metachronous recurrence and additional surgery following ESD were 10% (95% CI, 5.2%–18.2%; I2=55%) and 13% (95% CI, 8.5%–19.3%; I2=54%), respectively.
Conclusions
ESD is safe and effective for the resection of dysplastic lesions in IBD with an excellent pooled rate of en-bloc and R0 resection.
- 2,536 View
- 62 Download

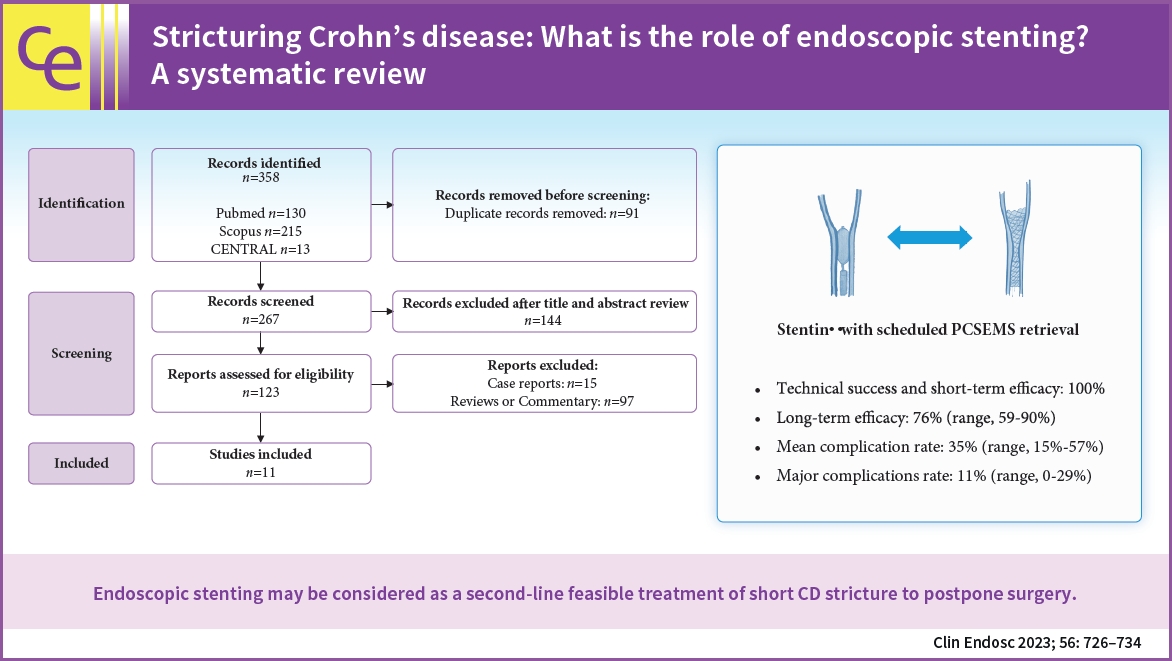
- Stricturing Crohn's disease: what is the role of endoscopic stenting? A systematic review
- Giorgia Burrelli Scotti, Roberto Lorenzetti, Annalisa Aratari, Antonietta Lamazza, Enrico Fiori, Claudio Papi, Stefano Festa
- Clin Endosc 2023;56(6):726-734. Published online October 24, 2023
- DOI: https://doi.org/10.5946/ce.2023.059
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: Endoscopic stenting for stricturing Crohn's disease (CD) is an emerging treatment that achieves more persistent dilatation of the stricture over time than endoscopic balloon dilatation (EBD). We aimed to explore the efficacy and safety of stenting for the treatment of CD strictures.
Methods
A systematic electronic literature search was performed (PROSPERO; no. CRD42022308033). The primary outcomes were technical success, efficacy, complication rate, and the need for further interventions due to reobstruction. The outcomes of partially covered self-expanding metal stents (PCSEMS) with scheduled retrieval after seven days were also analyzed.
Results
Eleven eligible studies were included in the review. Overall, 173 patients with CD were included in this study. Mean percentage of technical success was 95% (range, 80%–100%), short-term efficacy was 100% in all studies, and long-term efficacy was 56% (range, 25%–90%). In patients with a scheduled PCSEMS retrieval, the long-term efficacy was 76% (range, 59%–90%), the mean complication rate was 35% (range, 15%–57%), and the major complication rate was 11% (range, 0%–29%).
Conclusions
Endoscopic stenting with scheduled PCSEMS retrieval may be considered a feasible second-line treatment for short CD strictures to postpone surgery. However, larger head-to-head prospective studies are needed to understand the role of stenting as an alternative or additional treatment to EBD in CD. -
Citations
Citations to this article as recorded by- Perioperative Considerations for the Surgical Treatment of Crohn’s Disease with Discussion on Surgical Antibiotics Practices and Impact on the Gut Microbiome
Shelbi Olson, Lindsay Welton, Cyrus Jahansouz
Antibiotics.2024; 13(4): 317. CrossRef
- Perioperative Considerations for the Surgical Treatment of Crohn’s Disease with Discussion on Surgical Antibiotics Practices and Impact on the Gut Microbiome
- 2,719 View
- 180 Download
- 1 Web of Science
- 1 Crossref

- Current status of image-enhanced endoscopy in inflammatory bowel disease
- Young Joo Yang
- Clin Endosc 2023;56(5):563-577. Published online September 26, 2023
- DOI: https://doi.org/10.5946/ce.2023.070
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - In inflammatory bowel disease (IBD), chronic inflammation leads to unfavorable clinical outcomes and increases the risk of developing colorectal neoplasm (CRN); thereby highlighting the importance of endoscopically evaluating disease activity as well as detecting and characterizing CRN in patients with IBD. With recent advances in image-enhanced endoscopic (IEE) technologies, especially virtual chromoendoscopy (VCE) platforms, this review discusses state-of-the-art IEE techniques and their applicability in assessing disease activity and surveillance colonoscopy in patients with IBD. Among various IEE, VCE demonstrated the capacity to identify quiescent disease activity. And endoscopic remission defined by the new scoring system using VCE platform better predicted clinical outcomes, which may benefit the tailoring of therapeutic strategies in patients with IBD. High-definition dye-chromoendoscopy (HD-DCE) is numerically superior to high-definition white light endoscopy (HD-WLE) in detecting CRN in IBD; however, discrepancy is observed in the statistical significance. VCE showed comparable performance in detecting dysplasia to HD-WLE or DCE and potential for optical diagnosis to differentiate neoplastic from nonneoplastic lesions during surveillance colonoscopy. Applying these novel advanced IEE technologies would provide opportunities for personalized medicine in IBD and optimal treatment of CRN in patients with IBD.
- 2,039 View
- 107 Download

- Recent advances in surveillance colonoscopy for dysplasia in inflammatory bowel disease
- Soo-Young Na, Won Moon
- Clin Endosc 2022;55(6):726-735. Published online November 18, 2022
- DOI: https://doi.org/10.5946/ce.2022.132

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Inflammatory bowel disease (IBD) has a global presence with rapidly increasing incidence and prevalence. Patients with IBD including those with ulcerative colitis and Crohn’s disease have a higher risk of developing colorectal cancer (CRC) compared to the general population. Risk factors for CRC in patients with IBD include long disease duration, extensive colitis, primary sclerosing cholangitis, family history of CRC, stricture, and prior dysplasia. Surveillance colonoscopy for CRC in patients with IBD should be tailored to individualized risk factors and requires careful monitoring every year to every five years. The current surveillance techniques are based on several guidelines. Chromoendoscopy with targeted biopsy is being recommended increasingly, and high-definition colonoscopy is gradually replacing standard-definition colonoscopy. However, it remains unclear whether chromoendoscopy, virtual chromoendoscopy, or white-light endoscopy has better efficiency when a high-definition scope is used. With the development of new endoscopic instruments and techniques, the paradigm of surveillance strategy has gradually changed. In this review, we discuss cutting-edge surveillance colonoscopy in patients with IBD including a review of literature.
-
Citations
Citations to this article as recorded by- Inflammatory bowel disease and primary sclerosing cholangitis: One disease or two?
Kim N. van Munster, Annika Bergquist, Cyriel Y. Ponsioen
Journal of Hepatology.2024; 80(1): 155. CrossRef - Extrachromosomal Circular DNA: An Emerging Potential Biomarker for Inflammatory Bowel Diseases?
Valentina Petito, Federica Di Vincenzo, Lorenza Putignani, Maria T. Abreu, Birgitte Regenberg, Antonio Gasbarrini, Franco Scaldaferri
Genes.2024; 15(4): 414. CrossRef - A Review of Colonoscopy in Intestinal Diseases
Seung Hong, Dong Baek
Diagnostics.2023; 13(7): 1262. CrossRef - Potential Oral Microbial Markers for Differential Diagnosis of Crohn’s Disease and Ulcerative Colitis Using Machine Learning Models
Sang-Bum Kang, Hyeonwoo Kim, Sangsoo Kim, Jiwon Kim, Soo-Kyung Park, Chil-Woo Lee, Kyeong Ok Kim, Geom-Seog Seo, Min Suk Kim, Jae Myung Cha, Ja Seol Koo, Dong-Il Park
Microorganisms.2023; 11(7): 1665. CrossRef - Update on Endoscopic Dysplasia Surveillance in Inflammatory Bowel Disease
Nayantara Coelho-Prabhu, James D. Lewis
American Journal of Gastroenterology.2023; 118(10): 1748. CrossRef
- Inflammatory bowel disease and primary sclerosing cholangitis: One disease or two?
- 2,919 View
- 206 Download
- 5 Web of Science
- 5 Crossref

- Endoscopic activity in inflammatory bowel disease: clinical significance and application in practice
- Kyeong Ok Kim
- Clin Endosc 2022;55(4):480-488. Published online July 28, 2022
- DOI: https://doi.org/10.5946/ce.2022.108

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopy is vital for diagnosing, assessing treatment response, and monitoring surveillance in patients with inflammatory bowel disease (IBD). With the growing importance of mucosal healing as a treatment target, the assessment of disease activity by endoscopy has been accepted as the standard of care for IBD. There are many endoscopic activity indices for facilitating standardized reporting of the gastrointestinal mucosal appearance in IBD, and each index has its strengths and weaknesses. Although most endoscopic indices do not have a clear-cut validated definition, endoscopic remission or mucosal healing is associated with favorable outcomes, such as a decreased risk of relapse. Therefore, experts suggest utilizing endoscopic indices for monitoring disease activity and optimizing treatment to achieve remission. However, the regular monitoring of endoscopic activity is limited in practice owing to several factors, such as the complexity of the procedure, time consumption, inter-observer variability, and lack of a clear-cut, validated definition of endoscopic response or remission. Although experts have recently suggested consensus-based definitions, further studies are needed to define the values that can predict long-term outcomes.
-
Citations
Citations to this article as recorded by- Plasminogen Activator Inhibitor 1 Is a Novel Faecal Biomarker for Monitoring Disease Activity and Therapeutic Response in Inflammatory Bowel Diseases
Boldizsár Jójárt, Tamás Resál, Diána Kata, Tünde Molnár, Péter Bacsur, Viktória Szabó, Árpád Varga, Kata Judit Szántó, Petra Pallagi, Imre Földesi, Tamás Molnár, József Maléth, Klaudia Farkas
Journal of Crohn's and Colitis.2024; 18(3): 392. CrossRef - Ocular endothelial dysfunction in pediatric inflammatory bowel disease
Giovanni Di Nardo, Mariachiara Di Pippo, Letizia Zenzeri, Maurizio Mennini, Marisa Piccirillo, Silvia Furio, Giovanna Quatrale, Melania Evangelisti, Pasquale Parisi, Livia Lucchini, Alessandro Ferretti, Maria Pia Villa, Gianluca Scuderi, David Sarzi Amadè
Journal of Pediatric Gastroenterology and Nutrition.2024; 78(6): 1297. CrossRef - Different levels of healing in inflammatory bowel diseases: mucosal, histological, transmural, barrier and complete healing
Markus F Neurath, Michael Vieth
Gut.2023; 72(11): 2164. CrossRef - Use of Standardized Inflammatory Bowel Disease Endoscopy Scores in Clinical Practice
Jill K J Gaidos, Badr Al Bawardy, Francis A Farraye, Miguel Regueiro
Crohn's & Colitis 360.2023;[Epub] CrossRef - Evaluation of Disease Activity in Inflammatory Bowel Disease: Diagnostic Tools in the Assessment of Histological Healing
Alina Ecaterina Jucan, Otilia Gavrilescu, Mihaela Dranga, Iolanda Valentina Popa, Ioana-Ruxandra Mihai, Vasile-Claudiu Mihai, Gabriela Stefanescu, Vasile Liviu Drug, Cristina Cijevschi Prelipcean, Radu-Alexandru Vulpoi, Oana-Bogdana Barboi, Irina Ciortesc
Biomedicines.2023; 11(11): 3090. CrossRef - Active Assessment of Inflammatory Bowel Disease
金良 肖
Advances in Clinical Medicine.2022; 12(12): 11023. CrossRef
- Plasminogen Activator Inhibitor 1 Is a Novel Faecal Biomarker for Monitoring Disease Activity and Therapeutic Response in Inflammatory Bowel Diseases
- 6,196 View
- 350 Download
- 5 Web of Science
- 6 Crossref

- Capsule enteroscopy versus small-bowel ultrasonography for the detection and differential diagnosis of intestinal diseases
- Luca Elli, Erica Centorrino, Andrea Costantino, Maurizio Vecchi, Stefania Orlando, Mirella Fraquelli
- Clin Endosc 2022;55(4):532-539. Published online July 28, 2022
- DOI: https://doi.org/10.5946/ce.2021.224
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Capsule enteroscopy (CE) and intestinal ultrasonography (IUS) are techniques that are currently used for investigating small-bowel (SB) diseases. The aim of this study was to compare the main imaging findings and the lesion detection rate (LDR) of CE and IUS in different clinical scenarios involving the SB.
Methods
We retrospectively enrolled patients who underwent CE and IUS for obscure gastrointestinal bleeding (OGIB), complicated celiac disease (CeD), and suspected or known inflammatory bowel disease (IBD). We evaluated the LDR of both techniques. The accuracy of IUS was determined using CE as the reference standard.
Results
A total of 159 patients (113 female; mean age, 49±19 years) were enrolled. The LDR was 55% and 33% for CE and IUS (p<0.05), respectively. Subgroup analysis showed that the LDR of CE was significantly higher than that of IUS in patients with OGIB (62% vs. 14%, p<0.05) and CeD (55% vs. 35%, p<0.05). IUS showed a similar LDR to CE in patients with suspected or known IBD (51% vs. 46%, p=0.83).
Conclusions
CE should be preferred in cases of OGIB and CeD, whereas IUS should be considered an early step in the diagnosis and follow-up of IBD even in patients with a proximal SB localization of the disease. -
Citations
Citations to this article as recorded by- Past, Present, and Future of Noninvasive Tests to Assess Gluten Exposure, Celiac Disease Activity, and End-Organ Damage
Jocelyn A. Silvester, Luca Elli, Chaitan Khosla, Jason A. Tye-Din
Gastroenterology.2024; 167(1): 159. CrossRef - A practical approach for small bowel bleeding
Sung Eun Kim, Hyun Jin Kim, Myeongseok Koh, Min Cheol Kim, Joon Sung Kim, Ji Hyung Nam, Young Kwan Cho, A Reum Choe
Clinical Endoscopy.2023; 56(3): 283. CrossRef - Small Bowel Imaging in Celiac Disease: Is there a role for Small Bowel Ultrasound?
Roberta Elisa Rossi, Anita Busacca, Luca Brandaleone, Benedetta Masoni, Sara Massironi, Mirella Fraquelli, Alessandro Repici
Current Gastroenterology Reports.2023; 25(12): 430. CrossRef
- Past, Present, and Future of Noninvasive Tests to Assess Gluten Exposure, Celiac Disease Activity, and End-Organ Damage
- 2,130 View
- 139 Download
- 1 Web of Science
- 3 Crossref

- Endoscopic Diagnosis and Differentiation of Inflammatory Bowel Disease
- Ji Min Lee, Kang-Moon Lee
- Clin Endosc 2016;49(4):370-375. Published online July 29, 2016
- DOI: https://doi.org/10.5946/ce.2016.090
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Patients with inflammatory bowel disease have significantly increased in recent decades in Korea. Intestinal tuberculosis (ITB) and intestinal Behcet’s disease (BD), which should be differentiated from Crohn’s disease (CD), are more frequent in Korea than in the West. Thus, the accurate diagnosis of these inflammatory diseases is problematic in Korea and clinicians should fully understand their clinical and endoscopic characteristics. Ulcerative colitis mostly presents with rectal inflammation and continuous lesions, while CD presents with discontinuous inflammatory lesions and frequently involves the ileocecal area. Involvement of fewer than four segments, a patulous ileocecal valve, transverse ulcers, and scars or pseudopolyps are more frequently seen in ITB than in CD. A few ulcers with discrete margins are a typical endoscopic finding of intestinal BD. However, the differential diagnosis is difficult in many clinical situations because typical endoscopic findings are not always observed. Therefore, clinicians should also consider symptoms and laboratory, pathological, and radiological findings, in addition to endoscopic findings.
-
Citations
Citations to this article as recorded by- Recent Trends in Non-Invasive Methods of Diagnosis and Evaluation of Inflammatory Bowel Disease: A Short Review
Dan Vălean, Roxana Zaharie, Roman Țaulean, Lia Usatiuc, Florin Zaharie
International Journal of Molecular Sciences.2024; 25(4): 2077. CrossRef - Differential diagnosis of Crohn’s disease and intestinal tuberculosis based on ATR-FTIR spectroscopy combined with machine learning
Yuan-Peng Li, Tian-Yu Lu, Fu-Rong Huang, Wei-Min Zhang, Zhen-Qiang Chen, Pei-Wen Guang, Liang-Yu Deng, Xin-Hao Yang
World Journal of Gastroenterology.2024; 30(10): 1377. CrossRef - The quality of life of patients with inflammatory bowel diseases and the multidisciplinary team
Roxana-Ioana Ghenade, Ilie-Marius Ciorbă
Medic.ro.2024; 3(159): 24. CrossRef - A Case Report and Literature Review of Rectosigmoid Crohn’s Disease: A Diagnostic Pitfall Ultimately Leading to Spontaneous Colonic Perforation
Muhammad Z Ali, Muhammad Usman Tariq, Muhammad Hasan Abid, Hamma Abdulaziz, Mohmmad AlAdwani, Arif Khurshid, Muhammad Rashid, Fawaz Al Thobaiti , Amjad Althagafi
Cureus.2023;[Epub] CrossRef - Identification of cuproptosis-associated subtypes and signature genes for diagnosis and risk prediction of Ulcerative colitis based on machine learning
Dadong Tang, Baoping Pu, Shiru Liu, Hongyan Li
Frontiers in Immunology.2023;[Epub] CrossRef - Endoscopic features of the intestinal mucosa in patients with ulcerative colitis depending on the level of IgG4
Yu.M. Stepanov, M.V. Stoykevich, Yu.A. Gaidar, T.S. Tarasova, O.V. Simonova, O.M. Tatarchuk, O.P. Petishko
GASTROENTEROLOGY.2023; 57(1): 30. CrossRef - Standardizing Scoring Conventions for Crohn’s Disease Endoscopy: An International RAND/UCLA Appropriateness Study
Reena Khanna, Christopher Ma, Malcolm Hogan, Guangyong Zou, Talat Bessissow, Brian Bressler, Jean-Frédéric Colombel, Silvio Danese, Marco Daperno, James E. East, Lawrence Hookey, Edward V. Loftus, John W.D. McDonald, Remo Panaccione, Laurent Peyrin-Biroul
Clinical Gastroenterology and Hepatology.2023; 21(11): 2938. CrossRef - Creeping fat exhibits distinct Inflammation-specific adipogenic preadipocytes in Crohn’s disease
Nahee Hwang, Dongwoo Kang, Su-Jin Shin, Bo Kyung Yoon, Jaeyoung Chun, Jae-woo Kim, Sungsoon Fang
Frontiers in Immunology.2023;[Epub] CrossRef - PD-1-positive cells contribute to the diagnosis of inflammatory bowel disease and can aid in predicting response to vedolizumab
Min Kyu Kim, Su In Jo, Sang-Yeob Kim, Hyun Lim, Ho Suk Kang, Sung‑Hoon Moon, Byong Duk Ye, Jae Seung Soh, Sung Wook Hwang
Scientific Reports.2023;[Epub] CrossRef - Inflammatory bowel disease in adults
Umang Qazi
InnovAiT: Education and inspiration for general practice.2022; 15(2): 97. CrossRef - Integrative computational approach identifies immune‐relevant biomarkers in ulcerative colitis
Tianzhen He, Kai Wang, Peng Zhao, Guanqun Zhu, Xinbao Yin, Yulian Zhang, Zongliang Zhang, Kai Zhao, Zhenlin Wang, Ke Wang
FEBS Open Bio.2022; 12(2): 500. CrossRef - Absent X‐linked inhibitor of apoptosis protein expression in T cell blasts and causal mutations including non‐coding deletion
Shimaa Said Mohamed Ali Abdrabou, Nariaki Toita, Shin Ichihara, Yusuke Tozawa, Michiko Takahashi, Shin‐ichi Fujiwara, Toshifumi Ashida, Osamu Ohara, Tadashi Ariga, Atsushi Manabe, Mutsuko Konno, Masafumi Yamada
Pediatrics International.2022;[Epub] CrossRef - Mechanisms of mucosal healing: treating inflammatory bowel disease without immunosuppression?
Eduardo J. Villablanca, Katja Selin, Charlotte R. H. Hedin
Nature Reviews Gastroenterology & Hepatology.2022; 19(8): 493. CrossRef - Role of multidetector computed tomography in patients with acute infectious colitis
Seung Jung Yu, Jae Hyuk Heo, Eun Jeong Choi, Jong Hyuk Kim, Hong Sub Lee, Sun Young Kim, Jae Hoon Lim
World Journal of Clinical Cases.2022; 10(12): 3686. CrossRef - Differential Diagnosis of Crohn’s Disease and Ulcerative Primary Intestinal Lymphoma: A Scoring Model Based on a Multicenter Study
Hong Yang, Huimin Zhang, Wei Liu, Bei Tan, Tao Guo, Xiang Gao, Rui Feng, Kaichun Wu, Qian Cao, Zhihua Ran, Zhanju Liu, Naizhong Hu, Liangru Zhu, Yamin Lai, Congling Wang, Wei Han, Jiaming Qian
Frontiers in Oncology.2022;[Epub] CrossRef - Gut inflammation induced by drugs: Can pathology help to differentiate from inflammatory bowel disease?
Naoimh Herlihy, Roger Feakins
United European Gastroenterology Journal.2022; 10(5): 451. CrossRef - A Rare Case of New-Onset Ulcerative Colitis in a Nonagenarian
Emmanuel U Emeasoba, Cece E Ibeson, Sanchit Kundal, Stefanie Biondi, Ifeanyi Nwosu, Shmuel Golfeyz, Michael Kantrowitz, Dimitry Khodorskiy
Cureus.2022;[Epub] CrossRef - Application value of tissue tuberculosis antigen combined with Xpert MTB/RIF detection in differential diagnoses of intestinal tuberculosis and Crohn’s disease
Baoying Fei, Lin Zhou, Yu Zhang, Linhe Luo, Yuanyuan Chen
BMC Infectious Diseases.2021;[Epub] CrossRef - De Novo Inflammatory Bowel Disease Rarely Occurs During Posttransplant Immunosuppression
Jiayun M Fang, Laura Lamps, Amoah Yeboah-Korang, Jerome Cheng, Maria Westerhoff
American Journal of Clinical Pathology.2021; 156(6): 1113. CrossRef - Diterpenoids Isolated from Podocarpus macrophyllus Inhibited the Inflammatory Mediators in LPS-Induced HT-29 and RAW 264.7 Cells
ChoEen Kim, DucDat Le, Mina Lee
Molecules.2021; 26(14): 4326. CrossRef - Retrospective study of the differential diagnosis between cryptogenic multifocal ulcerous stenosing enteritis and small bowel Crohn’s disease
Dan Chen, Wei Liu, Weixun Zhou, Weiyang Zheng, Dong Wu, Jiaming Qian
BMC Gastroenterology.2020;[Epub] CrossRef - PREVALENCE AND FACTORS ASSOCIATED WITH SMALL INTESTINAL BACTERIAL OVERGROWTH IN PATIENTS WITH CROHN’S DISEASE: A RETROSPECTIVE STUDY AT A REFERRAL CENTER
Erika Ruback BERTGES, Júlio Maria Fonseca CHEBLI
Arquivos de Gastroenterologia.2020; 57(3): 283. CrossRef - Can natural language processing help differentiate inflammatory intestinal diseases in China? Models applying random forest and convolutional neural network approaches
Yuanren Tong, Keming Lu, Yingyun Yang, Ji Li, Yucong Lin, Dong Wu, Aiming Yang, Yue Li, Sheng Yu, Jiaming Qian
BMC Medical Informatics and Decision Making.2020;[Epub] CrossRef - Chronological Review of Endoscopic Indices in Inflammatory Bowel Disease
Joon Seop Lee, Eun Soo Kim, Won Moon
Clinical Endoscopy.2019; 52(2): 129. CrossRef - Illuminating an Invisible Epidemic: A Systemic Review of the Clinical and Economic Benefits of Early Diagnosis and Treatment in Inflammatory Disease and Related Syndromes
Wylezinski, Gray, Polk, Harmata, Spurlock
Journal of Clinical Medicine.2019; 8(4): 493. CrossRef - Anti-IL-13Rα2 therapy promotes recovery in a murine model of inflammatory bowel disease
Erik P. Karmele, Trisha S. Pasricha, Thirumalai R. Ramalingam, Robert W. Thompson, Richard L. Gieseck, Kayla J. Knilans, Martin Hegen, Mark Farmer, Fang Jin, Aaron Kleinman, David A. Hinds, Thiago Almeida Pereira, Rafael de Queiroz Prado, Nan Bing, Lioudm
Mucosal Immunology.2019; 12(5): 1174. CrossRef - A challenge in diagnosis and management of ulcerative colitis in elderly patient with atypical presentation: A reported case
Panutchaya Kongon, Vorapatu Tangsirapat, Vittawat Ohmpornuwat, Kannakrit Sumtong, Vichack Chakrapan Na Ayudhya, Kobkool Chakrapan Na Ayudhya, Paiboon Sookpotarom, Paisarn Vejchapipat
International Journal of Surgery Case Reports.2019; 61: 234. CrossRef - Primary hypertrophic osteoarthropathy related gastrointestinal complication has distinctive clinical and pathological characteristics: two cases report and review of the literature
Qiang Wang, Ying-he Li, Guo-le Lin, Yue Li, Wei-xun Zhou, Jia-ming Qian, Wei-bo Xia, Dong Wu
Orphanet Journal of Rare Diseases.2019;[Epub] CrossRef - Intestinal granulomatous disease: what is the first call
Alex Guri, Michal Kori, Pearl Herskovitz, Oren Zimhony
BMJ Case Reports.2018; : bcr-2017-223094. CrossRef - Aspecific ileitis: Crohn’s disease or not Crohn’s disease? A prospective study
Cristina Bezzio, Ilaria Arena, Massimo Devani, Barbara Omazzi, Gianpiero Manes, Simone Saibeni
International Journal of Colorectal Disease.2017; 32(7): 1025. CrossRef - Endoscopic Bamboo Joint-like Appearance of the Stomach in Crohn's Disease
Kwang Il Seo, Won Moon
The Korean Journal of Gastroenterology.2017; 69(2): 151. CrossRef - Management of Crohn's disease in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease
Shu-Chen Wei, Ting-An Chang, Te-Hsin Chao, Jinn-Shiun Chen, Jen-Wei Chou, Yenn-Hwei Chou, Chiao-Hsiung Chuang, Wen-Hung Hsu, Tien-Yu Huang, Tzu-Chi Hsu, Chun-Chi Lin, Hung-Hsin Lin, Jen-Kou Lin, Wei-Chen Lin, Yen-Hsuan Ni, Ming-Jium Shieh, I-Lun Shih, Chi
Intestinal Research.2017; 15(3): 285. CrossRef
- Recent Trends in Non-Invasive Methods of Diagnosis and Evaluation of Inflammatory Bowel Disease: A Short Review
- 26,395 View
- 773 Download
- 30 Web of Science
- 32 Crossref

- Tracheal Involvement in Crohn Disease: the First Case in Korea
- Seunghyun Park, Jongha Park, Hyun-Kuk Kim, Ji Yeon Kim, So Chong Hur, Ju Hyung Lee, Jae Won Jung, Juwon Lee
- Clin Endosc 2016;49(2):202-206. Published online February 16, 2016
- DOI: https://doi.org/10.5946/ce.2015.059
- Correction in: Clin Endosc 2016;49(3):310
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Respiratory involvement in Crohn disease (CD) is rare condition with only about a dozen reported cases. We report the first case of CD with tracheal involvement in Korea. An 18-year-old woman with CD was hospitalized because of coughing, dyspnea, and fever sustained for 3 weeks. Because she had stridor in her neck, we performed computed tomography of the neck, which showed circumferential wall thickening of the larynx and hypopharynx. Bronchoscopy revealed mucosal irregularity, ulceration, and exudates debris in the proximal trachea, and bronchial biopsy revealed chronic inflammation with granulation tissue. Based on these findings, we suspected CD with tracheal involvement and began administering intravenous methylprednisolone at 1 mg/kg per day, after which her symptoms and bronchoscopic findings improved.
-
Citations
Citations to this article as recorded by- Tracheobronchitis and laryngitis associated with Crohn's disease
Shogo Nakai, Moeko Morikawa, Toshiya Hiramatsu, Yurina Murakami, Koji Nishimoto, Sayomi Matsushima, Masanori Harada, Tomohiro Uto, Jun Sato, Shiro Imokawa, Takafumi Suda
Respiratory Medicine Case Reports.2023; 46: 101918. CrossRef - Tracheobronchial Crohn’s Disease: Case Report and Systematic Review of the Literature
Rao G Raghava, Vishal Sharma, Srikant Kashinath Malegaonkar, Sahajal Dhooria, Inderpaul Singh Sehgal, Kuruswamy Thurai Prasad, Amanjit Bal, Ritesh Agarwal, Valliappan Muthu
Inflammatory Bowel Diseases.2022; 28(3): e33. CrossRef - Granulomatous tracheo‐bronchitis from Crohn's disease
Amr J. Alwakeel, Stéphane Beaudoin
Respirology Case Reports.2022;[Epub] CrossRef - Nonasthmatic eosinophilic bronchitis in an ulcerative colitis patient – a putative adverse reaction to mesalazine: A case report and review of literature
Andrei Tudor Cernomaz, Gabriela Bordeianu, Cristina Terinte, Cristina Maria Gavrilescu
World Journal of Clinical Cases.2020; 8(18): 4162. CrossRef - Obstrucción de la vía aérea central por enfermedad inflamatoria intestinal y rescate terapéutico con membrana de oxigenación extracorpórea
M. Ramírez-Romero, B. Hernández-Alonso, C. García-Polo, A.J. Abraldes-Bechiarelli, A. Garrino-Fernández, A. Gordillo-Brenes
Medicina Intensiva.2018; 42(5): 317. CrossRef - Central airway obstruction due to inflammatory bowel disease and rescue with extracorporeal membrane oxygenation
M. Ramírez-Romero, B. Hernández-Alonso, C. García-Polo, A.J. Abraldes-Bechiarelli, A. Garrino-Fernández, A. Gordillo-Brenes
Medicina Intensiva (English Edition).2018; 42(5): 317. CrossRef - MORPHOMETRIC DIFFERENTIAL DIAGNOSIS OF INTESTINAL TUBERCULOSIS AND CROHN’S DISEASE
TA A Fedorina, GV V Nedugov
Science and Innovations in Medicine.2018; 3(3): 57. CrossRef - Managing Head and Neck Malignancy Arising in a Field of Crohn Disease Inflammation: Report of a Case
Christina Yver, Darshana Jhala, Amanda Muir, Devraj Basu
Ear, Nose & Throat Journal.2017; 96(10-11): E1. CrossRef
- Tracheobronchitis and laryngitis associated with Crohn's disease
- 8,596 View
- 83 Download
- 9 Web of Science
- 8 Crossref

- Colon Cancer Screening and Surveillance in Inflammatory Bowel Disease
- Song I Bae, You Sun Kim
- Clin Endosc 2014;47(6):509-515. Published online November 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.6.509
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Patients with inflammatory bowel disease (IBD) have an increased risk of developing colorectal cancer (CRC). Accordingly, the duration and anatomic extent of the disease have been known to affect the development of IBD-related CRC. When CRC occurs in patients with IBD, unlike in sporadic CRC, it is difficult to detect the lesions because of mucosal changes caused by inflammation. In addition, the tumor types vary with ill-circumscribed lesions, and the cancer is difficult to diagnose and remedy at an early stage. For the diagnosis of CRC in patients with IBD, screening endoscopy is recommended 8 to 10 years after the IBD diagnosis, and surveillance colonoscopy is recommended every 1 to 2 years thereafter. The recent development of targeted biopsies using chromoendoscopy and relatively newer endoscopic techniques helps in the early diagnosis of CRC in patients with IBD. A total proctocolectomy is advisable when high-grade dysplasia or multifocal low-grade dysplasia is confirmed by screening endoscopy or surveillance colonoscopy or if a nonadenoma-like dysplasia-associated lesion or mass is detected. Currently, pharmacotherapies are being extensively studied as a way to prevent IBD-related CRC.
-
Citations
Citations to this article as recorded by- Risk of Cancer in Inflammatory Bowel Disease and Pitfalls in Oncologic Therapy
Renata D. Peixoto, Artur R. Ferreira, James M. Cleary, João P. Fogacci, João P. Vasconcelos, Alexandre A. Jácome
Journal of Gastrointestinal Cancer.2023; 54(2): 357. CrossRef - A20 Restricts NOS2 Expression and Intestinal Tumorigenesis in a Mouse Model of Colitis-Associated Cancer
David W. Basta, Mandy Vong, Adolat Beshimova, Brooke N. Nakamura, Iulia Rusu, Michael G. Kattah, Ling Shao
Gastro Hep Advances.2023; 2(1): 96. CrossRef - Association of inflammatory bowel disease in first‐degree relatives with risk of colorectal cancer: A nationwide case‐control study in Sweden
Kai Wang, Ola Olén, Louise Emilsson, Hamed Khalili, Jonas Halfvarson, Mingyang Song, Jonas F. Ludvigsson
International Journal of Cancer.2023; 152(11): 2303. CrossRef - Evaluation of intestinal ultrasound for disease activity assessment in patients with inflammatory bowel disease: A cross-sectional study at a tertiary centre in Malaysia
Kuan Yee Lim, Raja Affendi Raja Ali, Zhiqin Wong, Faizah Mohd Zaki, Juliana Fairuz Maktar, Khairul Najmi Muhammad Nawawi
Saudi Journal of Gastroenterology.2023; 29(5): 300. CrossRef - Implementing a Combined Phone and Mail Recall to Increase Screening Colonoscopy Rates in Adults With Chronic Ulcerative Colitis
Gypsy Glover
Gastroenterology Nursing.2023; 46(4): 275. CrossRef - Impact of previous diverticulitis on 5-year survival and recurrence rates in patients with colorectal cancer
Hannah Sahli, Cecilia Dahlbäck, Marie-Louise Lydrup, Pamela Buchwald
Scandinavian Journal of Gastroenterology.2023; 58(11): 1280. CrossRef - Colorectal cancer screening
Burton James Mollman
JAAPA.2023; 36(8): 15. CrossRef - Age- and sex-specific risk of colorectal cancer in incident ulcerative colitis during the first 10 years after diagnosis: a nationwide population-based study
Hee Man Kim, Ji Hoon Kim, Jung Kuk Lee, Dae Ryong Kang, Hyunil Kim, Su Young Kim, Hyun-Soo Kim
Scandinavian Journal of Gastroenterology.2021; 56(11): 1279. CrossRef - Risks and Safety of Advanced Therapies and Biologics in Inflammatory Bowel Disease
Cynthia Morvillo, Katherine Vinci, Lauren Hedenschoug, Leah Mancini, Carrie Mize, Kayce Tugg, Steven Stein
Gastroenterology Nursing.2020; 43(4): E159. CrossRef - Diagnosis and survival values of neutrophil-lymphocyte ratio (NLR) and red blood cell distribution width (RDW) in esophageal cancer
Fuyan Han, Yiqing Liu, Shiqing Cheng, Zhaohui Sun, Chenchen Sheng, Xiya Sun, Xuming Shang, Wenjun Tian, Xiaoying Wang, Jiamei Li, Dong Liu, Yong Wang, Bingchang Zhang, Ying Ju
Clinica Chimica Acta.2019; 488: 150. CrossRef - Haem iron reshapes colonic luminal environment: impact on mucosal homeostasis and microbiome through aldehyde formation
Océane C. B. Martin, Maïwenn Olier, Sandrine Ellero-Simatos, Nathalie Naud, Jacques Dupuy, Laurence Huc, Sylviane Taché, Vanessa Graillot, Mathilde Levêque, Valérie Bézirard, Cécile Héliès-Toussaint, Florence Blas Y. Estrada, Valérie Tondereau, Yannick Li
Microbiome.2019;[Epub] CrossRef - Optical Diagnosis of Colorectal Cancer
红梅 于
Medical Diagnosis.2019; 09(02): 52. CrossRef - Surgical Management of Dysplasia and Cancer in Inflammatory Bowel Disease
James Ansell, Fabian Grass, Amit Merchea
Surgical Clinics of North America.2019; 99(6): 1111. CrossRef - Methods of extraction of optical properties from diffuse reflectance measurements of ex-vivo human colon tissue using thin film silicon photodetector arrays
Ben LaRiviere, N. Lynn Ferguson, Katherine S. Garman, Deborah A. Fisher, Nan M. Jokerst
Biomedical Optics Express.2019; 10(11): 5703. CrossRef - Intestinal and Extraintestinal Cancers Associated With Inflammatory Bowel Disease
Minna Chang, Liisa Chang, Hanna M. Chang, Fuju Chang
Clinical Colorectal Cancer.2018; 17(1): e29. CrossRef - N-Methylcytisine Ameliorates Dextran-Sulfate-Sodium-Induced Colitis in Mice by Inhibiting the Inflammatory Response
Yan-Fang Jiao, Min Lu, Yu-Ping Zhao, Ning Liu, Ya-Ting Niu, Yang Niu, Ru Zhou, Jian-Qiang Yu
Molecules.2018; 23(3): 510. CrossRef - Cancer Risk in Patients with Intestinal Behçet’s Disease: A Nationwide Population-Based Study
Minkyung Han, Yoon Suk Jung, Won Ho Kim, Jae Hee Cheon, Sohee Park
Gut and Liver.2018; 12(4): 433. CrossRef - Endoscopy in Pediatric Inflammatory Bowel Disease
Salvatore Oliva, Mike Thomson, Lissy de Ridder, Javier Martín‐de‐Carpi, Stephanie Van Biervliet, Christian Braegger, Jorge Amil Dias, Sanja Kolacek, Erasmo Miele, Stephan Buderus, Jiri Bronsky, Harland Winter, Víctor Manuel Navas‐López, Amit Assa, Sonny K
Journal of Pediatric Gastroenterology and Nutrition.2018; 67(3): 414. CrossRef - Getting a Low Grade for Missing High-Grade Dysplasia and Colorectal Cancer in IBD
James R. Conner, Robert H. Riddell
Digestive Diseases and Sciences.2017; 62(12): 3594. CrossRef - Tianfoshen oral liquid: a CFDA approved clinical traditional Chinese medicine, normalizes major cellular pathways disordered during colorectal carcinogenesis
Siliang Wang, Hengbin Wang, Yin Lu
Oncotarget.2017; 8(9): 14549. CrossRef - Cancer surveillance in ulcerative colitis and Crohnʼs disease
Bincy P. Abraham
Current Opinion in Gastroenterology.2016; 32(1): 32. CrossRef - C-glycosyl flavonoid orientin improves chemically induced inflammatory bowel disease in mice
Aning Sun, Gaiyan Ren, Chao Deng, Jingjing Zhang, Xiaoping Luo, Xiaojun Wu, Sridhar Mani, Wei Dou, Zhengtao Wang
Journal of Functional Foods.2016; 21: 418. CrossRef - Colorectal Cancer in Patients With Inflammatory Bowel Disease: The Need for a Real Surveillance Program
Rosario Fornaro, Michela Caratto, Elisa Caratto, Giuseppe Caristo, Francesco Fornaro, Davide Giovinazzo, Camilla Sticchi, Marco Casaccia, Enzo Andorno
Clinical Colorectal Cancer.2016; 15(3): 204. CrossRef - A Comprehensive Meta-Analysis of MicroRNAs for Predicting Colorectal Cancer
Lin Yan, Wenhua Zhao, Haihua Yu, Yansen Wang, Yuanshui Liu, Chao Xie
Medicine.2016; 95(9): e2738. CrossRef - The continuing uncertainty about cancer risk in inflammatory bowel disease
Hans-Olov Adami, Michael Bretthauer, Louise Emilsson, Miguel A Hernán, Mette Kalager, Jonas F Ludvigsson, Anders Ekbom
Gut.2016; 65(6): 889. CrossRef - Risk factors for developing colorectal cancer in Japanese patients with ulcerative colitis: a retrospective observational study—CAPITAL (Cohort and Practice for IBD total management in Kyoto-Shiga Links) study I
Takuya Yoshino, Hiroshi Nakase, Tomohisa Takagi, Shigeki Bamba, Yusuke Okuyama, Takuji Kawamura, Teruki Oki, Hirozumi Obata, Chiharu Kawanami, Shinji Katsushima, Toshihiro Kusaka, Tomoyuki Tsujikawa, Yuji Naito, Akira Andoh, Takafumi Kogawa
BMJ Open Gastroenterology.2016; 3(1): e000122. CrossRef - Introducing Vedolizumab to Clinical Practice: Who, When, and How?
RV Bryant, WJ Sandborn, SPL Travis
Journal of Crohn's and Colitis.2015; 9(4): 356. CrossRef - Interaction analysis of IL-12A and IL-12B polymorphisms with the risk of colorectal cancer
Ruifen Sun, Fu Jia, Yundan Liang, Lijuan Li, Peng Bai, Fang Yuan, Linbo Gao, Lin Zhang
Tumor Biology.2015; 36(12): 9295. CrossRef - Utility of Peripheral Blood Parameters in Predicting Breast Cancer Risk
Yildiz Okuturlar, Meral Gunaldi, Elif Eda Tiken, Bugra Oztosun, Yesim Ozdem Inan, Tarik Ercan, Savas Tuna, Ali Osman Kaya, Ozlem Harmankaya, Abdulbaki Kumbasar
Asian Pacific Journal of Cancer Prevention.2015; 16(6): 2409. CrossRef - Interval colorectal carcinoma: An unsolved debate
Mark Benedict
World Journal of Gastroenterology.2015; 21(45): 12735. CrossRef
- Risk of Cancer in Inflammatory Bowel Disease and Pitfalls in Oncologic Therapy
- 10,961 View
- 129 Download
- 34 Web of Science
- 30 Crossref

- Computed Tomography Enterography for Evaluation of Inflammatory Bowel Disease
- Min Jung Park, Joon Seok Lim
- Clin Endosc 2013;46(4):327-366. Published online July 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.4.327
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Computed tomography enterography (CTE) has become a main modality for the evaluation of inflammatory bowel disease (IBD). It simultaneously offers visualization of the small bowel and extraintestinal status, which is helpful for diagnosing IBD. Crohn disease has long segmental enhancing wall thickening related with the eccentric longitudinal distribution. In addition, mural stratification, fibrofatty proliferation, positive comb sign by increased mesenteric vascularity and internal/perianal fistula are characteristics of Crohn disease and can be identified on CTE. Short segmental inflammatory wall thickening and the central low attenuated lymph nodes are favorable CT finding of intestinal tuberculosis. A geographic, relatively large, and deep penetrating ulcer with bowel wall thickening and mural hyperenhancement in ileocecal area are characteristics of intestinal Behcet disease. Each of CTE findings for the IBDs is helpful for differential diagnosis. The main disadvantage of this technique is the requisite radiation exposure of patients, particularly in young patients. However, recent development of advanced CT techniques is promising for radiation dose reduction without compromising diagnostic image quality.
-
Citations
Citations to this article as recorded by- Differential diagnosis of Crohn’s disease and intestinal tuberculosis based on ATR-FTIR spectroscopy combined with machine learning
Yuan-Peng Li, Tian-Yu Lu, Fu-Rong Huang, Wei-Min Zhang, Zhen-Qiang Chen, Pei-Wen Guang, Liang-Yu Deng, Xin-Hao Yang
World Journal of Gastroenterology.2024; 30(10): 1377. CrossRef - Imaging of Gastrointestinal Tract Ailments
Boyang Sun, Jingang Liu, Silu Li, Jonathan F. Lovell, Yumiao Zhang
Journal of Imaging.2023; 9(6): 115. CrossRef - Computed tomography enterography-based multiregional radiomics model for differential diagnosis of Crohn’s disease from intestinal tuberculosis
Tong Gong, Mou Li, Hong Pu, Long-lin Yin, Sheng-kun Peng, Zhou Zhou, Mi Zhou, Hang Li
Abdominal Radiology.2023; 48(6): 1900. CrossRef - The treatment principles and targets for intestinal Behcet’s disease
Kun He, Dong Wu
Therapeutic Advances in Gastroenterology.2023; 16: 175628482311672. CrossRef - Differentiating gastrointestinal tuberculosis and Crohn's disease- a comprehensive review
Arup Choudhury, Jasdeep Dhillon, Aravind Sekar, Pankaj Gupta, Harjeet Singh, Vishal Sharma
BMC Gastroenterology.2023;[Epub] CrossRef - New score models for assessing disease activity in Crohn's disease based on bowel ultrasound and biomarkers: Ideal surrogates for endoscopy or imaging
Qingyang Zhou, Qingli Zhu, Wei Liu, Wenbo Li, Li Ma, Mengsu Xiao, Jingjuan Liu, Hong Yang, Jiaming Qian
Clinical and Translational Science.2023; 16(9): 1639. CrossRef - Appearance of the Bowel and Mesentery During Surgery Is Not Predictive of Postoperative Recurrence After Ileocecal Resection for Crohn’s Disease: A Prospective Monocentric Study
Gabriele Bislenghi, Julie Van Den Bossch, Steffen Fieuws, Albert Wolthuis, Marc Ferrante, Gert de Hertogh, Severine Vermeire, André D’Hoore
Inflammatory Bowel Diseases.2023;[Epub] CrossRef - Results of the Eighth Scientific Workshop of ECCO: Pathophysiology and Risk Factors of Postoperative Crohn’s Disease Recurrence after an Ileocolonic Resection
Pauline Rivière, Gabriele Bislenghi, Nassim Hammoudi, Bram Verstockt, Steven Brown, Melissa Oliveira-Cunha, Willem Bemelman, Gianluca Pellino, Paulo Gustavo Kotze, Gabriele Dragoni, Mariangela Allocca, Nurulamin M Noor, Lieven Pouillon, Míriam Mañosa, Edo
Journal of Crohn's and Colitis.2023; 17(10): 1557. CrossRef - How can the surgeon reduce recurrence after surgery for ileocolic Crohn's disease?
Steven R. Brown
Seminars in Colon and Rectal Surgery.2023; 34(4): 100985. CrossRef - Machine Learning and Radiomics: Changing the Horizon of Crohn’s Disease Assessment
Raseen Tariq, Saam Dilmaghani
Inflammatory Bowel Diseases.2023;[Epub] CrossRef - Magnetic resonance colonography with intestine-absorbable nanoparticle contrast agents in evaluation of colorectal inflammation
Xue Dong, Jingfeng Luo, Pengxun Lan, Xiuyu Guo, Xin Zhao, Xiaoyan Wang, Fei Zhou, Qiangfeng Wang, Hong Yuan, Jihong Sun
European Radiology.2021; 31(7): 4615. CrossRef - Intestinal tuberculosis or Crohn’s disease: a review of the diagnostic models designed to differentiate between these two gastrointestinal diseases
Julajak Limsrivilai, Nonthalee Pausawasdi
Intestinal Research.2021; 19(1): 21. CrossRef - Diagnostic role of computed tomography enterography (CTE) in assessment of intra-mural and extra-intestinal CT findings in active Crohn’s disease (CD)
Rasha Mostafa Mohamed Ali, Mai Bahgat Ibrahim Ghonimy
Egyptian Journal of Radiology and Nuclear Medicine.2021;[Epub] CrossRef - Computed tomography enterography for crohn’s disease: correlation between the imaging findings and histopathologic scoring system
Liang Ma, Xing Shen, Yi-Jing Chen, Qi Zhang, Bo Li, Wei Zhang
Abdominal Radiology.2021; 46(9): 4121. CrossRef - Wireless Capsule Endoscopy for Diagnosis and Management of Post-Operative Recurrence of Crohn’s Disease
Adil Mir, Vu Q. Nguyen, Youssef Soliman, Dario Sorrentino
Life.2021; 11(7): 602. CrossRef - COMPARATIVE ANALYSIS OF TWO ORAL CONTRAST AGENT VOLUMES FOR COMPUTED TOMOGRAPHY ENTEROGRAPHY IN CROHN’S DISEASE PATIENTS
Fernanda Lofiego RENOSTO, Jaqueline Ribeiro de BARROS, Guilherme A BERTOLDI, Sergio Ribeiro MARRONE, Ligia Yukie SASSAKI, Rogerio SAAD-HOSSNE
Arquivos de Gastroenterologia.2021; 58(3): 322. CrossRef - Crohn’s disease at radiological imaging: focus on techniques and intestinal tract
Giuseppe Cicero, Silvio Mazziotti
Intestinal Research.2021; 19(4): 365. CrossRef - Computed Tomography Enterography Demonstrates Association to Histopathological Grading of Small Bowel Crohn’s Activity
Husam H Mansour, Yasser S Alajerami, Ahmed A Najim, Khaled M Abushab
Electronic Journal of General Medicine.2021; 18(6): em330. CrossRef - Autoinflammatory diseases in childhood, part 2: polygenic syndromes
María Navallas, Emilio J. Inarejos Clemente, Estíbaliz Iglesias, Mónica Rebollo-Polo, Joan Calzada Hernández, Oscar M. Navarro
Pediatric Radiology.2020; 50(3): 431. CrossRef - Diagnostic efficacy of double-balloon enteroscopy in patients with suspected isolated small bowel Crohn’s disease
Zihan Huang, Xiang Liu, Fei Yang, Guoxin Wang, Nan Ge, Sheng Wang, Jintao Guo, Siyu Sun
BMC Gastroenterology.2020;[Epub] CrossRef - Evidence-based diagnosis and clinical practice guidelines for intestinal Behçet’s disease 2020 edited by Intractable Diseases, the Health and Labour Sciences Research Grants
Kenji Watanabe, Satoshi Tanida, Nagamu Inoue, Reiko Kunisaki, Kiyonori Kobayashi, Masakazu Nagahori, Katsuhiro Arai, Motoi Uchino, Kazutaka Koganei, Taku Kobayashi, Mitsuhiro Takeno, Fumiaki Ueno, Takayuki Matsumoto, Nobuhisa Mizuki, Yasuo Suzuki, Tadakaz
Journal of Gastroenterology.2020; 55(7): 679. CrossRef - Retrospective study of the differential diagnosis between cryptogenic multifocal ulcerous stenosing enteritis and small bowel Crohn’s disease
Dan Chen, Wei Liu, Weixun Zhou, Weiyang Zheng, Dong Wu, Jiaming Qian
BMC Gastroenterology.2020;[Epub] CrossRef - The Role of Active Inflammation and Surgical Therapy in Crohn’s Disease Recurrence
S. Ingallinella, M. Campanelli, A. Antonelli, C. Arcudi, V. Bellato, A. Divizia, M. Franceschilli, L. Petagna, B. Sensi, S. Sibio, L. Siragusa, G. S. Sica, Lukas J.A.C. Hawinkels
Gastroenterology Research and Practice.2020; 2020: 1. CrossRef - The Mesentery, Systemic Inflammation, and Crohn’s Disease
Edgardo D Rivera, John Calvin Coffey, Dara Walsh, Eli D Ehrenpreis
Inflammatory Bowel Diseases.2019; 25(2): 226. CrossRef - Intestinal fibrosis
Marco Vincenzo Lenti, Antonio Di Sabatino
Molecular Aspects of Medicine.2019; 65: 100. CrossRef - Evaluation of CT enterography findings for endoscopic complete remission after anti-TNF-α therapy in patients with Crohn’s disease
Jieun Kim, Seung Ho Kim, Tae Oh Kim
Acta Radiologica.2019; 60(10): 1200. CrossRef - Crohn's disease: A retrospective analysis between computed tomography enterography, colonoscopy, and histopathology
C. Saade, L. Nasr, A. Sharara, K. Barada, A. Soweid, F. Murad, A. Tawil, D. Ghieh, K. Asmar, H. Tamim, N.J. Khoury
Radiography.2019; 25(4): 349. CrossRef - Cinematic rendering: a new imaging approach for ulcerative colitis
Jun Yang, Xu Liu, Chengde Liao, Qinqing Li, Dan Han
Japanese Journal of Radiology.2019; 37(8): 590. CrossRef - CT ENTEROCLYSIS VERSUS CT ENTEROGRAPHY IN THE EVALUATION OF SUSPECTED SMALL BOWEL PATHOLOGIES - A CASE SERIES
Monisha Jacob, Jeffrey Ralph, Praveen Kumar Vasanthraj, Prithiviraj P. V, Sushmitha M. S
Journal of Evidence Based Medicine and Healthcare.2019; 6(7): 458. CrossRef - The effect of without using anisodamine during CT enterography on image quality, diagnostic performance and latent side effects
Didi Wen, Jian Xu, Ying Liu, Rui An, Jian Li, Hongliang Zhao, Minwen Zheng
Clinical Imaging.2018; 48: 106. CrossRef - Comparison of diagnostic performance between 1 millisievert CT enterography and half-standard dose CT enterography for evaluating active inflammation in patients with Crohn’s disease
Jung Hee Son, Seung Ho Kim, Een Young Cho, Kyeong Hwa Ryu
Abdominal Radiology.2018; 43(7): 1558. CrossRef - Management of Crohn’s Disease and Complications in Patients With Ostomies
Xinying Wang, Bo Shen
Inflammatory Bowel Diseases.2018; 24(6): 1167. CrossRef - Value of dual-energy CT enterography in the analysis of pathological bowel segments in patients with Crohn's disease
A.M. Villanueva Campos, G. Tardáguila de la Fuente, E. Utrera Pérez, C. Jurado Basildo, D. Mera Fernández, C. Martínez Rodríguez
Radiología (English Edition).2018; 60(3): 223. CrossRef - Valor de la enterografía por tomografía computarizada con doble energía en el análisis de segmentos intestinales patológicos en pacientes con enfermedad de Crohn
A.M. Villanueva Campos, G. Tardáguila de la Fuente, E. Utrera Pérez, C. Jurado Basildo, D. Mera Fernández, C. Martínez Rodríguez
Radiología.2018; 60(3): 223. CrossRef - Role of surgery in the management of Crohn's disease
Alessandro Fichera, Francisco Schlottmann, Mukta Krane, Greta Bernier, Erin Lange
Current Problems in Surgery.2018; 55(5): 162. CrossRef - Intestinal Behçet Disease: Evaluation With MR Enterography—A Case-Control Study
Elif Peker, Ayşe Erden, İlhan Erden, Nurşen Düzgün
American Journal of Roentgenology.2018; 211(4): 767. CrossRef - 18 F-FDG PET/CT in Extensive Graft-Versus-Host Disease of the Gastrointestinal Tract Following Autologous Stem Cell Transplantation
Danijela Dejanovic, Annemarie Amtoft, Annika Loft
Diagnostics.2018; 8(4): 72. CrossRef - The Association of Coloproctology of Great Britain and Ireland consensus guidelines in surgery for inflammatory bowel disease
S. R. Brown, N. S. Fearnhead, O. D. Faiz, J. F. Abercrombie, A. G. Acheson, R. G. Arnott, S. K. Clark, S. Clifford, R. J. Davies, M. M. Davies, W. J. P. Douie, M. G. Dunlop, J. C. Epstein, M. D. Evans, B. D. George, R. J. Guy, R. Hargest, A. B. Hawthorne,
Colorectal Disease.2018; 20(S8): 3. CrossRef - Meta-Analytic Bayesian Model For Differentiating Intestinal Tuberculosis from Crohn's Disease
Julajak Limsrivilai, Andrew B Shreiner, Ananya Pongpaibul, Charlie Laohapand, Rewat Boonanuwat, Nonthalee Pausawasdi, Supot Pongprasobchai, Sathaporn Manatsathit, Peter D R Higgins
American Journal of Gastroenterology.2017; 112(3): 415. CrossRef - Structured reporting of CT enterography for inflammatory bowel disease: effect on key feature reporting, accuracy across training levels, and subjective assessment of disease by referring physicians
Benjamin Wildman-Tobriner, Brian C. Allen, Mustafa R. Bashir, Morgan Camp, Chad Miller, Lauren E. Fiorillo, Alan Cubre, Sanaz Javadi, Alex D. Bibbey, Wendy L. Ehieli, Nancy McGreal, Reinaldo Quevedo, Julie K. Thacker, Maciej Mazurowski, Tracy A. Jaffe
Abdominal Radiology.2017; 42(9): 2243. CrossRef - Magnetic Resonance Enterography Findings of Intestinal Behçet Disease in a Child
Tommaso D’Angelo, Romina Gallizzi, Claudio Romano, Giuseppe Cicero, Silvio Mazziotti
Case Reports in Radiology.2017; 2017: 1. CrossRef - Nanoparticle‐based imaging of inflammatory bowel disease
Yingwei Wu, Karen Briley, Xiaofeng Tao
WIREs Nanomedicine and Nanobiotechnology.2016; 8(2): 300. CrossRef - Misdiagnosis and Mistherapy of Crohn's Disease as Intestinal Tuberculosis
Jiang-Peng Wei, Xiao-Yan Wu, Sen-Yang Gao, Qiu-Yu Chen, Tong Liu, Gang Liu
Medicine.2016; 95(1): e2436. CrossRef - Role of Computed Tomography in Pediatric Abdominal Conditions
Anu Eapen, Sridhar Gibikote
The Indian Journal of Pediatrics.2016; 83(7): 691. CrossRef - The Role of the Mesentery in Crohnʼs Disease
Yi Li, Weiming Zhu, Lugen Zuo, Bo Shen
Inflammatory Bowel Diseases.2016; 22(6): 1483. CrossRef - Diagnostic imaging and radiation exposure in inflammatory bowel disease
Nekisa Zakeri, Richard CG Pollok
World Journal of Gastroenterology.2016; 22(7): 2165. CrossRef
- Differential diagnosis of Crohn’s disease and intestinal tuberculosis based on ATR-FTIR spectroscopy combined with machine learning
- 12,333 View
- 155 Download
- 46 Crossref

- The Role of Colonoscopy in Inflammatory Bowel Disease
- Yong Gil Kim, Byung Ik Jang
- Clin Endosc 2013;46(4):317-320. Published online July 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.4.317
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub An endoscopic evaluation, particularly ileocolic mucosal and histological findings, is essential for the diagnosis of inflammatory bowel disease (IBD). The introduction of antitumor necrosis factor agents has changed the therapeutic paradigm of patients with IBD, but an endoscopic evaluation is more important to guide therapeutic decision-making. In the future, endoscopy with a histological evaluation will be increasingly used in patients with IBD. Both Crohn colitis and ulcerative colitis result in an increased incidence of colorectal carcinoma. Thus, surveillance colonoscopy is important to detect early neoplastic lesions. Surveillance ileocolonoscopy has also changed recently from multiple random biopsies to pancolonic dye spraying with targeted biopsies of abnormal areas.
-
Citations
Citations to this article as recorded by- YouTube® en español como fuente de información para pacientes con enfermedad inflamatoria intestinal
C.E. Lombo-Moreno, O.M. Muñoz-Velandia, D.G. Fernández-Ávila, J.E. Barahona-Correa, V. López-Ramírez, A. Rodriguez-Varon
Revista de Gastroenterología de México.2024; 89(2): 176. CrossRef - YouTube® in Spanish as a source of information for patients with inflammatory bowel disease
C.E. Lombo-Moreno, O.M. Muñoz-Velandia, D.G. Fernández-Ávila, J.E. Barahona-Correa, V. López-Ramírez, A. Rodriguez-Varon
Revista de Gastroenterología de México (English Edition).2024; 89(2): 176. CrossRef - Role of MR enterography versus ileo-colonoscopy in the assessment of inflammatory bowel diseases
Rasha Mostafa Mohamed Ali, Aya Fawzy Abd El Salam, Ismail Anwar, Hany Shehab, Maryse Youssef Awadallah
Egyptian Journal of Radiology and Nuclear Medicine.2023;[Epub] CrossRef - HISTOPATHOLOGICAL FEATURES IN RELAPSE OF ULCERATIVE COLITIS.
Saroash Iqbal, Aman Ur Rehman, Nausheen Henna, Zara Madiha, Sahar Moeed, Uzma Aslam
JAIMC: Journal of Allama Iqbal Medical College.2023;[Epub] CrossRef - Prevalence and risk factors of cytomegalovirus colitis in inflammatory bowel disease patients in Riyadh, Saudi Arabia: A tertiary center experience
Yazeed Alotaibi, Abed AlLehibi, Abdullah Almtawa, Nawaf Alotaibi, Adel Alghamdi, Saad Alrajhi, Adel AlQutub, Ahmad AlEid, Abdulrhman Alamr, Bashaar Al Ibrahim, Mohammed Alahmari, Hussam Alhamidi, Shameem Ahmad, Fouad Alshammari, Fahad Almotawa, Youssef Al
Saudi Journal of Medicine and Medical Sciences.2023; 11(4): 305. CrossRef - Mango (Mangifera indica L.) polyphenols reduce IL-8, GRO, and GM-SCF plasma levels and increase Lactobacillus species in a pilot study in patients with inflammatory bowel disease
Hyemee Kim, Vinicius P. Venancio, Chuo Fang, Andrew W. Dupont, Stephen T Talcott, Susanne U Mertens-Talcott
Nutrition Research.2020; 75: 85. CrossRef - Can microscopic ileitis in patients with clinically suspected inflammatory bowel disease predict the future?
Fadi Abu Baker, Jesus Alonso Z’cruz De La Garza, Smadar Nafrin, Amir Mari, Muhammed Suki, Baruch Ovadia, Oren Gal, Yael Kopelamn
BMC Gastroenterology.2020;[Epub] CrossRef - Breath Analysis Using eNose and Ion Mobility Technology to Diagnose Inflammatory Bowel Disease—A Pilot Study
Tiele, Wicaksono, Kansara, Arasaradnam, Covington
Biosensors.2019; 9(2): 55. CrossRef - The value of mRNA expression of S100A8 and S100A9 as blood-based biomarkers of inflammatory bowel disease
Tayebeh Azramezani Kopi, Azade Amini Kadijani, Hadi Parsian, Shabnam Shahrokh, Hamid Asadzadeh Aghdaei, Alireza Mirzaei, Hedieh Balaii, Mohammad Reza Zali
Arab Journal of Gastroenterology.2019; 20(3): 135. CrossRef - MR Enterography of Inflammatory Bowel Disease with Endoscopic Correlation
Pankaj Kaushal, Alexander S. Somwaru, Aline Charabaty, Angela D. Levy
RadioGraphics.2017; 37(1): 116. CrossRef - Diagnosing inflammatory bowel disease and differentiating it from potential mimics
Kindra D. Clark-Snustad, Scott D. Lee
Techniques in Gastrointestinal Endoscopy.2016; 18(3): 108. CrossRef
- YouTube® en español como fuente de información para pacientes con enfermedad inflamatoria intestinal
- 9,126 View
- 83 Download
- 11 Crossref

- The Early Onset of Disease May Be a Risk Factor for Decreased Bone Mineral Density in Patients with Inflammatory Bowel Disease
- Hwa Jong Kim, Su Jin Hong, Young Woo Jeon, Jae Pil Han, Seung Hyo Han, Jee Heon Kang, Jae Woong Tae, Hee Sook Lim, Hee Kyung Kim, Bong Min Ko, Moon Sung Lee
- Clin Endosc 2013;46(1):71-76. Published online January 31, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.1.71
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Background/Aims The pathogenesis of bone loss in patients with inflammatory bowel disease (IBD) is complex, multifactorial, and only partly understood. We aimed to examine the extent and risk factors of bone mass reduction and to analyze the impact of early onset of a disease before attaining peak bone mass in IBD patients.
Methods We compared the risk factors for osteoporosis and BMD at the lumbar spine and the hip bone in IBD patients.
Results A total of 44 patients with IBD were enrolled. Twenty-one and 23 patients were diagnosed as IBD before and after the age of 30 and designated as group A and group B, respectively. Group A had significant bone mass reduction at the lumbar spine than group B (BMD, 1.01±0.10 vs. 1.14±0.17,
p <0.01; T-score, -1.22±0.84 vs. -0.08±1.39,p <0.01; Z-score, -1.11±0.81 vs. -0.03±1.32,p <0.01, respectively). Multivariate analysis showed that patients diagnosed as IBD before the age of 30 had possible risk factor of bone mass reduction (hazard ratio, 3.96;p =0.06).Conclusions Bone mass reduction was more severe in patients who were diagnosed with IBD before the age of 30 than in those diagnosed after the age of 30.
-
Citations
Citations to this article as recorded by- Small and Large Intestine (II): Inflammatory Bowel Disease, Short Bowel Syndrome, and Malignant Tumors of the Digestive Tract
Yolanda Ber, Santiago García-Lopez, Carla J. Gargallo-Puyuelo, Fernando Gomollón
Nutrients.2021; 13(7): 2325. CrossRef - Infliximab for very early‐onset inflammatory bowel disease: A tertiary center experience in Japan
Ichiro Takeuchi, Yoichiro Kaburaki, Katsuhiro Arai, Hirotaka Shimizu, Yuri Hirano, Satoru Nagata, Toshiaki Shimizu
Journal of Gastroenterology and Hepatology.2020; 35(4): 593. CrossRef - Advances in nutritional therapy in inflammatory bowel diseases: Review
Andrzej Wędrychowicz
World Journal of Gastroenterology.2016; 22(3): 1045. CrossRef - Nutritional aspect of pediatric inflammatory bowel disease: its clinical importance
Seung Kim, Hong Koh
Korean Journal of Pediatrics.2015; 58(10): 363. CrossRef - Biomarkers of Cartilage and Surrounding Joint Tissue
Anne S Siebuhr, Yi He, Natasja S Gudmann, Aurelie Gram, Cecilie F Kjelgaard-Petersen, Per Qvist, Morten A Karsdal, Anne C Bay-Jensen
Biomarkers in Medicine.2014; 8(5): 713. CrossRef - Crohn's disease and growth deficiency in children and adolescents
Marco Gasparetto
World Journal of Gastroenterology.2014; 20(37): 13219. CrossRef - Can Early Onset of Disease Be One of the Risk Factors for Low Bone Mineral Density in Patients with Inflammatory Bowel Disease?
Kwang An Kwon, Yang Suh Ku
Clinical Endoscopy.2013; 46(1): 5. CrossRef
- Small and Large Intestine (II): Inflammatory Bowel Disease, Short Bowel Syndrome, and Malignant Tumors of the Digestive Tract
- 6,103 View
- 53 Download
- 6 Web of Science
- 7 Crossref

- Role of Computed Tomography Enterography/Magnetic Resonance Enterography: Is It in Prime Time?
- Ah Young Kim
- Clin Endosc 2012;45(3):269-273. Published online August 22, 2012
- DOI: https://doi.org/10.5946/ce.2012.45.3.269
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Today, cross-sectional imaging modalities, such as computed tomography enterography (CTE) and magnetic resonance enterography (MRE), are particularly suited to evaluate small bowel diseases, especially Crohn's disease (CD). It is well known that CTE/MRE can provide excellent assessment of disease activity as well as the macroscopic features, extramural abnormalities, and complications of the small intestine in patients with CD. In general, CTE is considered as the first-line modality for the evaluation of suspected inflammatory bowel disease and for long-term assessment or follow-up of these patients. Because of the advantage of lack of radiation, MRE is being used more frequently, especially in children or young patients with CD.
-
Citations
Citations to this article as recorded by- Indian guidelines on imaging of the small intestine in Crohn’s disease: A joint Indian Society of Gastroenterology and Indian Radiology and Imaging Association consensus statement
Saurabh Kedia, Raju Sharma, Govind Makharia, Vineet Ahuja, Devendra Desai, Devasenathipathy Kandasamy, Anu Eapen, Karthik Ganesan, Uday C Ghosha, Naveen Kalra, R Karthikeyan, Kumble Seetharama Madhusudhan, Mathew Philip, Amarender Puri, Sunil Puri, Saroj
Indian Journal of Radiology and Imaging.2019; 29(02): 111. CrossRef - Imaging in discriminating intestinal tuberculosis and Crohn’s disease: past, present and the future
Pradeep Goyal, Jimil Shah, Sonali Gupta, Pankaj Gupta, Vishal Sharma
Expert Review of Gastroenterology & Hepatology.2019; 13(10): 995. CrossRef - The effect of without using anisodamine during CT enterography on image quality, diagnostic performance and latent side effects
Didi Wen, Jian Xu, Ying Liu, Rui An, Jian Li, Hongliang Zhao, Minwen Zheng
Clinical Imaging.2018; 48: 106. CrossRef - Ileal Crohn's disease activity predicted by ruler: CT enterography histopathology correlation
Tamer W. Kassem
The Egyptian Journal of Radiology and Nuclear Medicine.2017; 48(1): 7. CrossRef - Faecal biomarkers for screening small bowel inflammation in patients with Crohn’s disease: a prospective study
Takahiro Shimoyama, Takayuki Yamamoto, Satoru Umegae, Koichi Matsumoto
Therapeutic Advances in Gastroenterology.2017; 10(8): 577. CrossRef - Imaging of the small intestine in Crohn’s disease: Joint position statement of the Indian Society of Gastroenterology and Indian Radiological and Imaging Association
Saurabh Kedia, Raju Sharma, Govind K. Makharia, Vineet Ahuja, Devendra Desai, Devasenathipathy Kandasamy, Anu Eapen, Karthik Ganesan, Uday C. Ghoshal, Naveen Kalra, D. Karthikeyan, Kumble Seetharama Madhusudhan, Mathew Philip, Amarender Singh Puri, Sunil
Indian Journal of Gastroenterology.2017; 36(6): 487. CrossRef - Diagnosis of Small-Bowel Diseases: Prospective Comparison of Multi–Detector Row CT Enterography with MR Enterography
Gabriele Masselli, Marco Di Tola, Emanuele Casciani, Elisabetta Polettini, Francesca Laghi, Riccardo Monti, Maria Giulia Bernieri, Gianfranco Gualdi
Radiology.2016; 279(2): 420. CrossRef - Value of Computerized Tomography Enterography in Predicting Crohn’s Disease Activity: Correlation with Crohn’s Disease Activity Index and C-Reactive Protein
Eun Kyung Park, Na Yeon Han, Beom Jin Park, Deuk Jae Sung, Sung Beom Cho, Yoon Tae Jeen, Bora Keum, Min Ju Kim
Iranian Journal of Radiology.2016;[Epub] CrossRef - Identifying the inflammatory and fibrotic bowel stricture: MRI diffusion-weighted imaging in Crohn's disease
Jianguo Zhu, Faming Zhang, Fei Liu, Wenwen He, Jun Tian, Huiyun Han, Peng Cao
Radiology of Infectious Diseases.2015; 2(3): 128. CrossRef - Imaging Inflammatory Bowel Disease with CT and MR Enterography
Piotr Starakiewicz, David J. Grand
Current Radiology Reports.2013; 1(4): 277. CrossRef
- Indian guidelines on imaging of the small intestine in Crohn’s disease: A joint Indian Society of Gastroenterology and Indian Radiology and Imaging Association consensus statement
- 6,293 View
- 68 Download
- 10 Crossref


 KSGE
KSGE


 First
First Prev
Prev



