Search
- Page Path
- HOME > Search
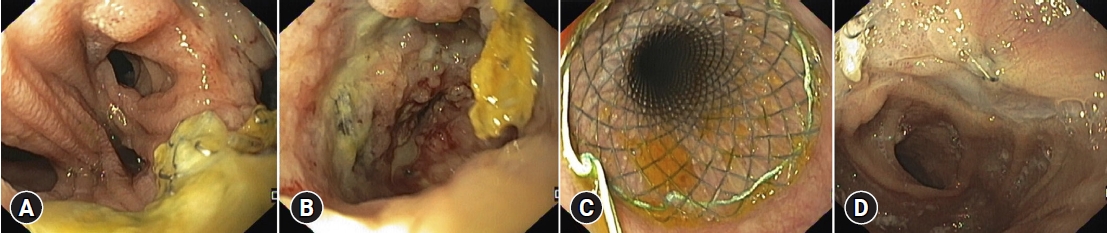
- Colon stenting as a bridge to surgery in obstructive colorectal cancer management
- Dong Hyun Kim, Han Hee Lee
- Received May 23, 2023 Accepted July 29, 2023 Published online March 8, 2024
- DOI: https://doi.org/10.5946/ce.2023.138 [Epub ahead of print]
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Colonic stent placement is a commonly used bridging strategy for surgery in patients with obstructive colorectal cancer. The procedure involves the placement of a self-expandable metallic stent (SEMS) across the obstructive lesion to restore intestinal patency and alleviate the symptoms of obstruction. By allowing patients to receive surgery in a planned and staged manner with time for preoperative optimization and bowel preparation, stent placement may reduce the need for emergency surgery, which is associated with higher complication rates and poorer outcomes. This review focuses on the role of colon stenting as a bridge to surgery in the management of obstructive colorectal cancer. SEMS as a bridge to surgery for left-sided colon cancer has been demonstrated to be particularly useful; however, further research is needed for its application in cases of right-sided colon cancer. Colon stent placement also has limitations and potential complications including stent migration, re-obstruction, and perforation. However, the timing of curative surgery after SEMS placement remains inconclusive. Considering the literature to date, performing surgery at an interval of approximately 2 weeks is considered appropriate. Therefore, colonic stent placement may be an effective strategy as a bridge to surgery in patients with obstructive colorectal cancer.
- 1,966 View
- 115 Download

- Role of endoscopic duodenojejunal bypass liner in obesity management and glycemic control
- Willian Ferreira Igi, Victor Lira de Oliveira, Ayah Matar, Diogo Turiani Hourneaux de Moura
- Clin Endosc 2024;57(3):309-316. Published online February 15, 2024
- DOI: https://doi.org/10.5946/ce.2023.217

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The treatment of obesity and its comorbidities ranges from clinical management involving lifestyle changes and medications to bariatric and metabolic surgery. Various endoscopic bariatric and metabolic therapies recently emerged to address an important therapeutic gap by offering a less invasive alternative to surgery that is more effective than conservative therapies. This article comprehensively reviews the technical aspects, mechanism of action, outcomes, and future perspectives of one of the most promising endoscopic bariatric and metabolic therapies, named duodenojejunal bypass liner. The duodenojejunal bypass liner mimics the mechanism of Roux-en-Y gastric bypass by preventing food contact with the duodenum and proximal jejunum, thereby initiating a series of hormonal changes that lead to delayed gastric emptying and malabsorptive effects. These physiological changes result in significant weight loss and improved metabolic control, leading to better glycemic levels, preventing dyslipidemia and non-alcoholic fatty liver disease, and mitigating cardiovascular risk. However, concern exists regarding the safety profile of this device due to the reported high rates of severe adverse events, particularly liver abscesses. Ongoing technical changes aiming to reduce adverse events are being evaluated in clinical trials and may provide more reliable data to support its routine use in clinical practice.
-
Citations
Citations to this article as recorded by- Bacteroides and NAFLD: pathophysiology and therapy
Jun Zhang, Jing Zhou, Zheyun He, Hongshan Li
Frontiers in Microbiology.2024;[Epub] CrossRef
- Bacteroides and NAFLD: pathophysiology and therapy
- 2,443 View
- 70 Download
- 1 Web of Science
- 1 Crossref

- Endoscopic treatment of upper gastrointestinal postsurgical leaks: a narrative review
- Renato Medas, Eduardo Rodrigues-Pinto
- Clin Endosc 2023;56(6):693-705. Published online July 3, 2023
- DOI: https://doi.org/10.5946/ce.2023.043
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Upper gastrointestinal postsurgical leaks are life-threatening conditions with high mortality rates and are one of the most feared complications of surgery. Leaks are challenging to manage and often require radiological, endoscopic, or surgical intervention. Steady advancements in interventional endoscopy in recent decades have allowed the development of new endoscopic devices and techniques that provide a more effective and minimally invasive therapeutic option compared to surgery. Since there is no consensus regarding the most appropriate therapeutic approach for managing postsurgical leaks, this review aimed to summarize the best available current data. Our discussion specifically focuses on leak diagnosis, treatment aims, comparative endoscopic technique outcomes, and combined multimodality approach efficacy.
- 2,350 View
- 306 Download

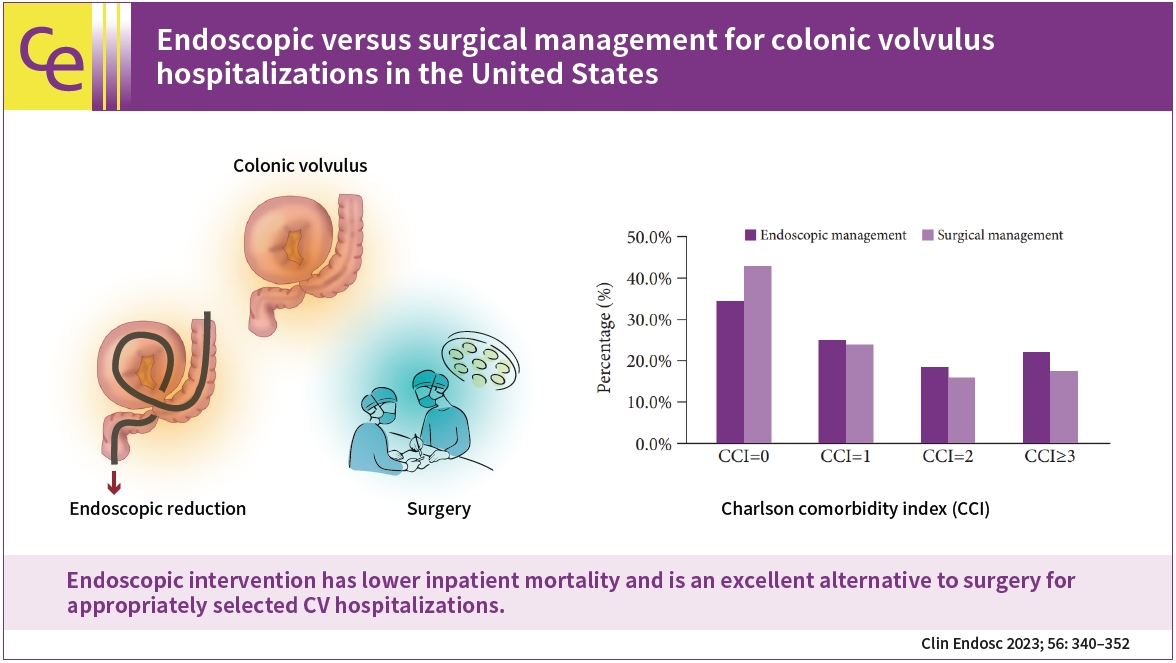
- Endoscopic versus surgical management for colonic volvulus hospitalizations in the United States
- Dushyant Singh Dahiya, Abhilash Perisetti, Hemant Goyal, Sumant Inamdar, Amandeep Singh, Rajat Garg, Chin-I Cheng, Mohammad Al-Haddad, Madhusudhan R. Sanaka, Neil Sharma
- Clin Endosc 2023;56(3):340-352. Published online April 17, 2023
- DOI: https://doi.org/10.5946/ce.2022.166
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: Colonic volvulus (CV), a common cause of bowel obstruction, often requires intervention. We aimed to identify hospitalization trends and CV outcomes in the United States.
Methods
We used the National Inpatient Sample to identify all adult CV hospitalizations in the United States from 2007 to 2017. Patient demographics, comorbidities, and inpatient outcomes were highlighted. Outcomes of endoscopic and surgical management were compared.
Results
From 2007 to 2017, there were 220,666 CV hospitalizations. CV-related hospitalizations increased from 17,888 in 2007 to 21,715 in 2017 (p=0.001). However, inpatient mortality decreased from 7.6% in 2007 to 6.2% in 2017 (p<0.001). Of all CV-related hospitalizations, 13,745 underwent endoscopic intervention, and 77,157 underwent surgery. Although the endoscopic cohort had patients with a higher Charlson comorbidity index, we noted lower inpatient mortality (6.1% vs. 7.0%, p<0.001), mean length of stay (8.3 vs. 11.8 days, p<0.001), and mean total healthcare charge ($68,126 vs. $106,703, p<0.001) compared to the surgical cohort. Male sex, increased Charlson comorbidity index scores, acute kidney injury, and malnutrition were associated with higher odds of inpatient mortality in patients with CV who underwent endoscopic management.
Conclusions
Endoscopic intervention has lower inpatient mortality and is an excellent alternative to surgery for appropriately selected CV hospitalizations. -
Citations
Citations to this article as recorded by- Navigating Abdominal Volvulus: A Comprehensive Review of Management Strategies
Simran Chauhan, Raju K Shinde, Yashraj Jain
Cureus.2024;[Epub] CrossRef - Incidental Sigmoid Volvulus after a Ground-level Fall: An Unusual Case Report
Ziya Karimov, Elchin Shirinov, Gunay Huseynova, Mirhuseyn Mammadov, Meltem Songür Kodik
Caucasian Medical Journal.2023; 1(3): 36. CrossRef - Colonic Volvulus
Samantha L. Savitch, Calista M. Harbaugh
Clinics in Colon and Rectal Surgery.2023;[Epub] CrossRef
- Navigating Abdominal Volvulus: A Comprehensive Review of Management Strategies
- 2,156 View
- 149 Download
- 3 Web of Science
- 3 Crossref

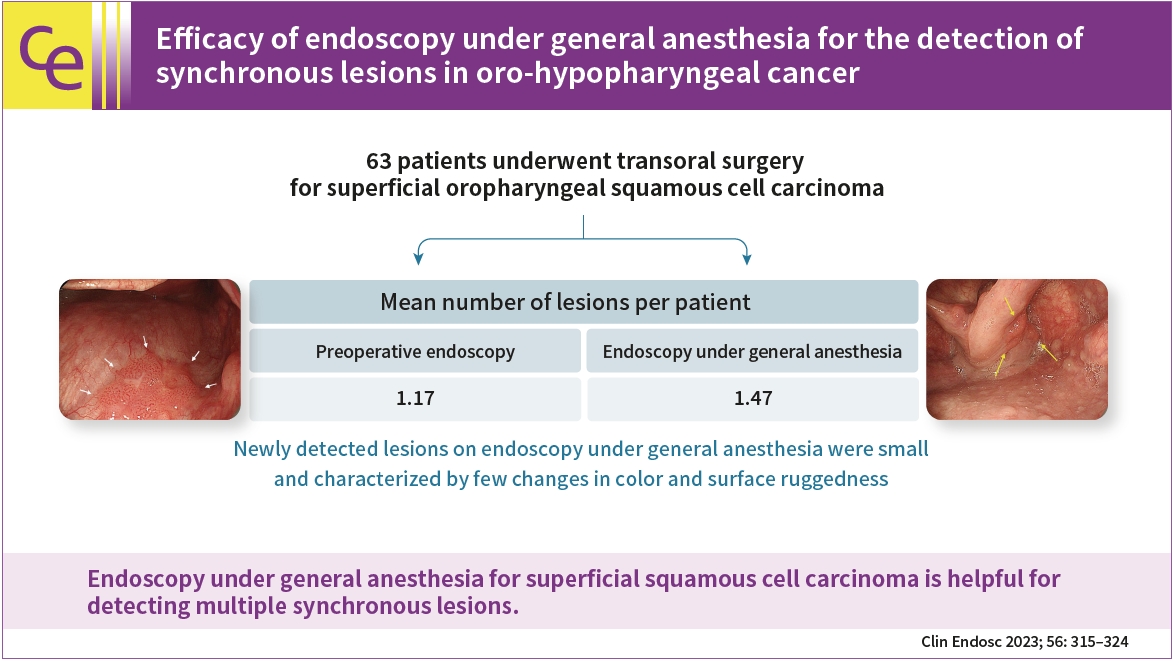
- Efficacy of endoscopy under general anesthesia for the detection of synchronous lesions in oro-hypopharyngeal cancer
- Yoichiro Ono, Kenshi Yao, Yasuhiro Takaki, Satoshi Ishikawa, Kentaro Imamura, Akihiro Koga, Kensei Ohtsu, Takao Kanemitsu, Masaki Miyaoka, Takashi Hisabe, Toshiharu Ueki, Atsuko Ota, Hiroshi Tanabe, Seiji Haraoka, Satoshi Nimura, Akinori Iwashita, Susumu Sato, Rumie Wakasaki
- Clin Endosc 2023;56(3):315-324. Published online January 5, 2023
- DOI: https://doi.org/10.5946/ce.2022.072
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 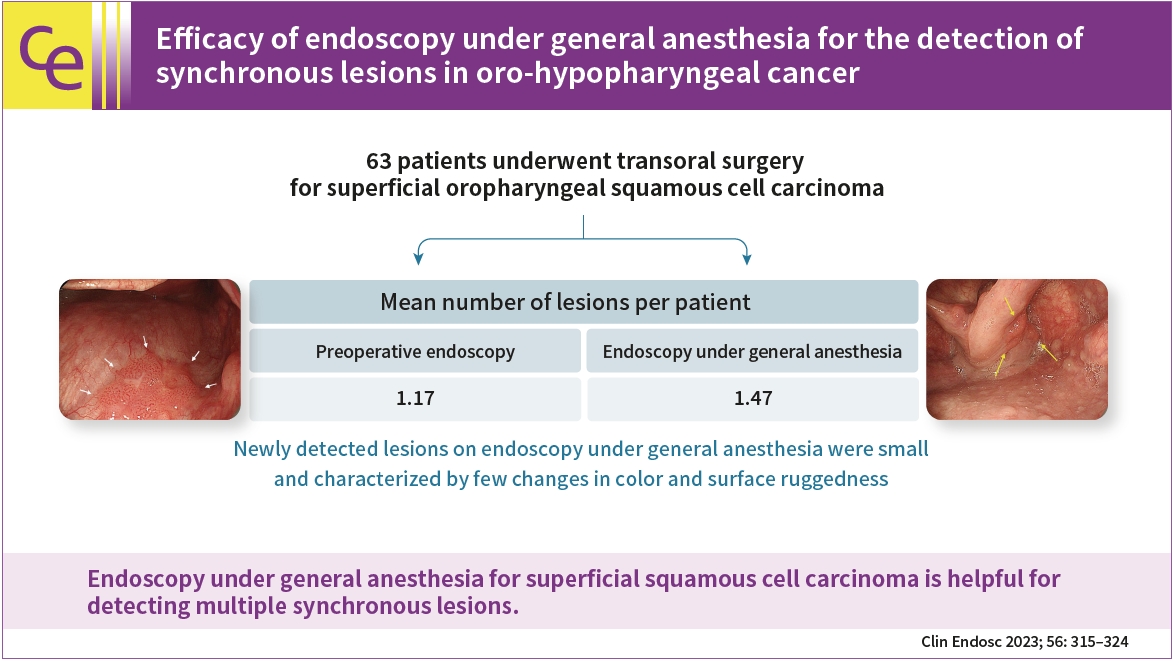
- Background
/Aims: Image-enhanced endoscopy can detect superficial oro-hypopharyngeal squamous cell carcinoma; however, reliable endoscopy of the pharyngeal region is challenging. Endoscopy under general anesthesia during transoral surgery occasionally reveals multiple synchronous lesions that remained undetected on preoperative endoscopy. Therefore, we aimed to determine the lesion detection capability of endoscopy under general anesthesia for superficial oro-hypopharyngeal squamous cell carcinoma.
Methods
This retrospective study included 63 patients who underwent transoral surgery for superficial oropharyngeal squamous cell carcinoma between April 2005 and December 2020. The primary endpoint was to compare the lesion detection capabilities of preoperative endoscopy and endoscopy under general anesthesia. Other endpoints included the comparison of clinicopathological findings between lesions detected using preoperative endoscopy and those newly detected using endoscopy under general anesthesia.
Results
Fifty-eight patients (85 lesions) were analyzed. The mean number of lesions per patient detected was 1.17 for preoperative endoscopy and 1.47 for endoscopy under general anesthesia. Endoscopy under general anesthesia helped detect more lesions than preoperative endoscopy did (p<0.001). The lesions that were newly detected on endoscopy under general anesthesia were small and characterized by few changes in color and surface ruggedness.
Conclusions
Endoscopy under general anesthesia for superficial squamous cell carcinoma is helpful for detecting multiple synchronous lesions. -
Citations
Citations to this article as recorded by- Nasopharyngeal examination during transoral upper gastrointestinal endoscopy
Vui Heng Chong
Clinical Endoscopy.2024; 57(1): 137. CrossRef - Endoscopy under general anesthesia for detecting synchronous lesions of head and neck squamous cell carcinoma
Jin Hee Noh, Do Hoon Kim
Clinical Endoscopy.2023; 56(3): 308. CrossRef
- Nasopharyngeal examination during transoral upper gastrointestinal endoscopy
- 2,134 View
- 192 Download
- 2 Web of Science
- 2 Crossref

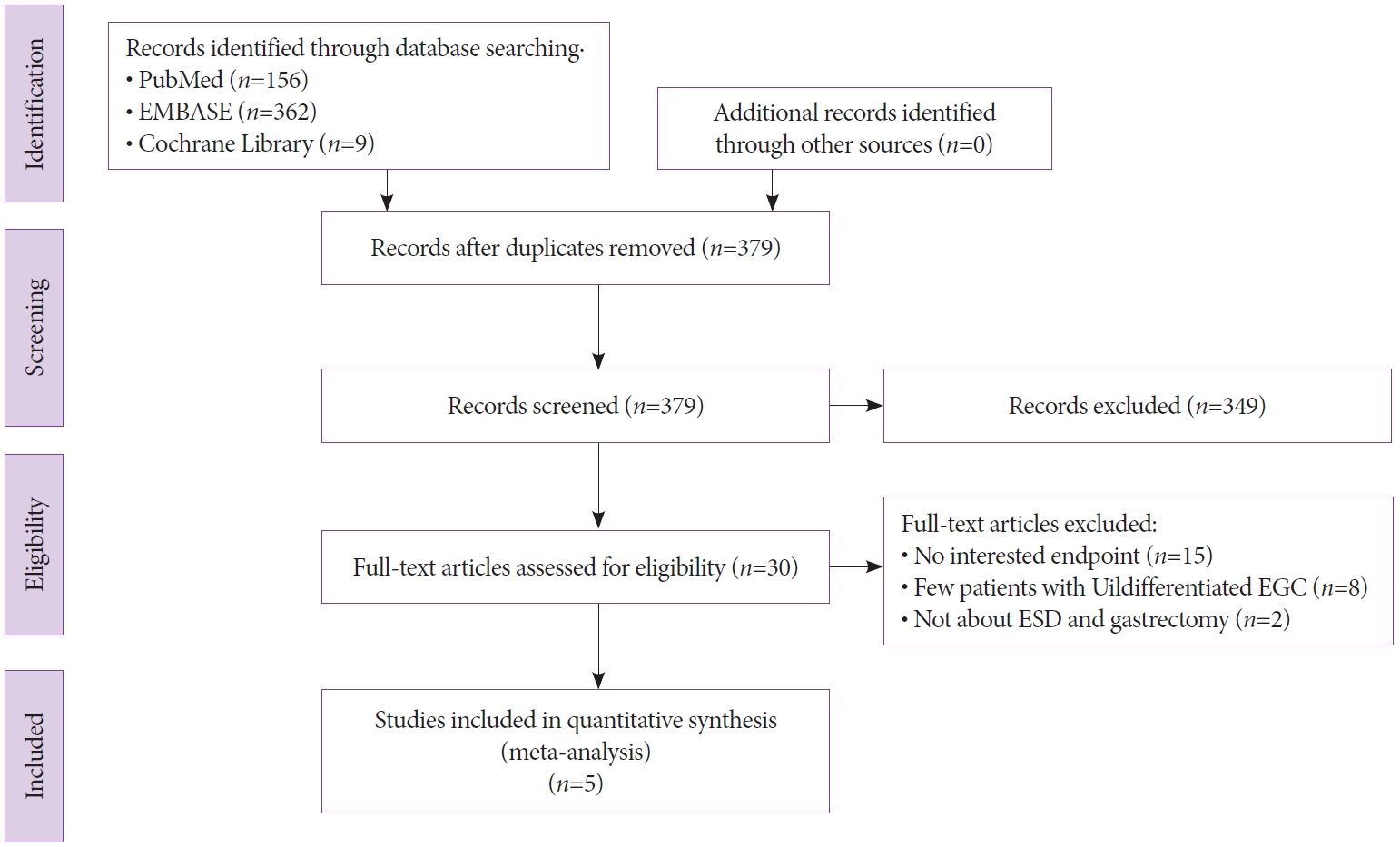
- Endoscopic Submucosal Dissection versus Surgery for Undifferentiated-Type Early Gastric Cancer: A Systematic Review and Meta-Analysis
- Cheal-Wung Huh, Dae Won Ma, Byung-Wook Kim, Joon Sung Kim, Seung Jae Lee
- Clin Endosc 2021;54(2):202-210. Published online February 17, 2021
- DOI: https://doi.org/10.5946/ce.2020.121
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: The use of endoscopic submucosal dissection (ESD) for treating undifferentiated-type early gastric cancer is controversial. The objective of this study was to perform a meta-analysis to compare the long-term outcomes of ESD and surgery for undifferentiated-type early gastric cancer.
Methods
The PubMed, Cochrane Library, and EMBASE databases were used to search for relevant studies comparing ESD and surgery for undifferentiated-type early gastric cancer. The methodological quality of the included publications was evaluated using the Risk of Bias Assessment tool for Nonrandomized Studies. The rates of overall survival, recurrence, adverse event, and complete resection were determined. Odds ratios (ORs) and 95% confidence intervals (CIs) were also evaluated.
Results
This meta-analysis enrolled five studies with 429 and 1,236 participants undergoing ESD and surgery, respectively. No significant difference was found in the overall survival rate between the ESD and surgery groups (OR, 2.29; 95% CI, 0.98–5.36; p=0.06). However, ESD was associated with a higher recurrence rate and a lower complete resection rate. The adverse event rate was similar between the two groups.
Conclusions
ESD with meticulous surveillance esophagogastroduodenoscopy may be as effective and safe as surgery in patients with undifferentiated-type early gastric cancer. Further large-scale, randomized, controlled studies from additional regions are required to confirm these findings. -
Citations
Citations to this article as recorded by- Curative criteria for endoscopic treatment of gastric cancer
João A. Cunha Neves, Pedro G. Delgado-Guillena, Patrícia Queirós, Diogo Libânio, Enrique Rodríguez de Santiago
Best Practice & Research Clinical Gastroenterology.2024; 68: 101884. CrossRef - Chinese national clinical practice guidelines on the prevention, diagnosis, and treatment of early gastric cancer
Peng Li, Ziyu Li, Enqiang Linghu, Jiafu Ji
Chinese Medical Journal.2024; 137(8): 887. CrossRef - Korean Practice Guidelines for Gastric Cancer 2022: An Evidence-based, Multidisciplinary Approach
Tae-Han Kim, In-Ho Kim, Seung Joo Kang, Miyoung Choi, Baek-Hui Kim, Bang Wool Eom, Bum Jun Kim, Byung-Hoon Min, Chang In Choi, Cheol Min Shin, Chung Hyun Tae, Chung sik Gong, Dong Jin Kim, Arthur Eung-Hyuck Cho, Eun Jeong Gong, Geum Jong Song, Hyeon-Su Im
Journal of Gastric Cancer.2023; 23(1): 3. CrossRef - Endoscopic Resection of Early Gastric Cancer and Pre-Malignant Gastric Lesions
Ana Clara Vasconcelos, Mário Dinis-Ribeiro, Diogo Libânio
Cancers.2023; 15(12): 3084. CrossRef - Performance of endoscopic submucosal dissection for undifferentiated early gastric cancer: a multicenter retrospective cohort
Apostolis Papaefthymiou, Michel Kahaleh, Arnaud Lemmers, Sandro Sferrazza, Maximilien Barret, Katsumi Yamamoto, Pierre Deprez, José C. Marín-Gabriel, George Tribonias, Hong Ouyang, Federico Barbaro, Oleksandr Kiosov, Stefan Seewald, Gaurav Patil, Shaimaa
Endoscopy International Open.2023; 11(07): E673. CrossRef - A meta-analysis of the impact on gastrectomy versus endoscopic submucosal dissection for early stomach cancer
Rajesh K. Singh
International Journal of Clinical Medical Research.2023; 1(3): 37. CrossRef - A meta-analysis of the impact on gastrectomy versus endoscopic submucosal dissection for early stomach cancer
Rajesh K. Singh
International Journal of Clinical Medical Research.2023;[Epub] CrossRef - Long-term outcomes of endoscopic submucosal dissection and surgery for undifferentiated intramucosal gastric cancer regardless of size
Gil Ho Lee, Eunyoung Lee, Bumhee Park, Jin Roh, Sun Gyo Lim, Sung Jae Shin, Kee Myung Lee, Choong-Kyun Noh
World Journal of Gastroenterology.2022; 28(8): 840. CrossRef - Comparison of long-term outcomes of endoscopic submucosal dissection and surgery for undifferentiated-type early gastric cancer meeting the expanded criteria: a systematic review and meta-analysis
Hyo-Joon Yang, Jie-Hyun Kim, Na Won Kim, Il Ju Choi
Surgical Endoscopy.2022; 36(6): 3686. CrossRef - Endoscopic submucosal dissection versus surgery for patients with undifferentiated early gastric cancer
Harold Benites-Goñi, Fernando Palacios-Salas, Andrea Carlin-Ronquillo, Carlos Díaz-Arocutipa, Alejandro Piscoya, Adrián Hernández
Revista Española de Enfermedades Digestivas.2022;[Epub] CrossRef - The future of endoscopic resection for early gastric cancer
Raquel Ortigão, Diogo Libânio, Mário Dinis‐Ribeiro
Journal of Surgical Oncology.2022; 125(7): 1110. CrossRef - Endoscopic treatment for early gastric cancer
Ji Yong Ahn
Journal of the Korean Medical Association.2022; 65(5): 276. CrossRef - Therapeutic approach to non-curative resection after endoscopic treatment in early gastric cancer
Eun Jeong Gong, Chang Seok Bang
Journal of the Korean Medical Association.2022; 65(5): 284. CrossRef - Long-Term Outcomes of Endoscopic Submucosal Dissection of Undifferentiated-Type Early Gastric Cancer
Chang Seok Bang
Clinical Endoscopy.2021; 54(2): 143. CrossRef
- Curative criteria for endoscopic treatment of gastric cancer
- 4,839 View
- 199 Download
- 13 Web of Science
- 14 Crossref

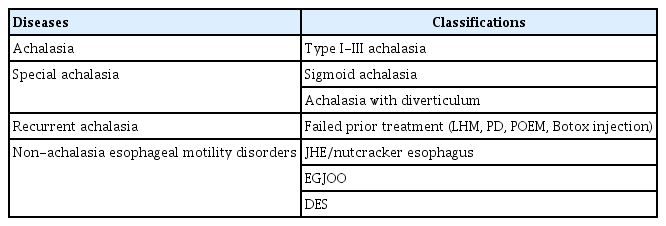
- Peroral Endoscopic Myotomy for Esophageal Motility Disorders
- Jun Young Kim, Yang Won Min
- Clin Endosc 2020;53(6):638-645. Published online November 20, 2020
- DOI: https://doi.org/10.5946/ce.2020.223
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Peroral endoscopic myotomy (POEM) is one of the most clinically successful tunnel-based minimally invasive endoscopic treatments. The classic indications of POEM include achalasia of all types, including failed prior treatments, and expanded indications include the non-achalasia esophageal motility disorders, such as esophagogastric junction outflow obstruction, diffuse esophageal spasm, and jackhammer esophagus. For achalasia treatment, POEM has achieved a comparable surgical efficacy and a safety outcome and, therefore, has emerged as a first-line treatment. For non-achalasia esophageal motility disorders, POEM has also shown high clinical response rates. The complication rate of POEM for esophageal motility disorders is low and most complications are managed with conservative treatment. Currently, POEM is a representative procedure of natural orifice transluminal endoscopic surgery, which has shown a good clinical efficacy with low complication rates for esophageal motility disorders including achalasia. However, further studies are needed to treat non-achalasia motility disorder via POEM.
-
Citations
Citations to this article as recorded by- Diffuse Esophageal Spasm: An Alternative Treatment Approach
McKenzie K Allen , Wayne Frei
Cureus.2024;[Epub] CrossRef - Clinical and financial outcomes of per-oral endoscopic myotomy compared to laparoscopic heller myotomy for treatment of achalasia
Lena Shally, Kashif Saeed, Derek Berglund, Mark Dudash, Katie Frank, Vladan N. Obradovic, Anthony T. Petrick, David L. Diehl, Jon D. Gabrielsen, David M. Parker
Surgical Endoscopy.2023; 37(7): 5526. CrossRef - Benefit of extending the protocol for high resolution manometry according to the version 4.0 of the Chicago criteria. A multicenter study
Luis G. Alcalá‐González, Alberto Ezquerra‐Duran, Ariadna Aguilar, Claudia Barber, Elizabeth Barba, Isis K. Araujo, Ingrid Marin, Juan Naves, Jordi Serra
Neurogastroenterology & Motility.2023;[Epub] CrossRef - Role of Endoscopy in Motility Disorders of Upper Gastrointestinal Tract
Jin Hee Noh, Hwoon-Yong Jung
Journal of Neurogastroenterology and Motility.2023; 29(1): 7. CrossRef - Surveillance Endoscopy After Foregut Surgery: Is It Necessary?
Yahya Alwatari, Daniel Scheese, Graham Gardner, Vignesh Vudatha, Walker Julliard, Carlos Puig Gilbert, Rachit D. Shah
Foregut: The Journal of the American Foregut Society.2023; 3(1): 89. CrossRef - Per oral endoscopic myotomy for achalasia: A Taiwanese single‐center experience
Yu‐Chi Lee, Wei‐Chen Tai, Keng‐Liang Wu, Chih‐Chien Yao, Seng‐Kee Chuah
Advances in Digestive Medicine.2022; 9(4): 241. CrossRef - Pediatric anesthesia and achalasia: 10 years’ experience in peroral endoscopy myotomy management
Fabio Sbaraglia, Pietro Familiari, Federica Maiellare, Marco Mecarello, Annamaria Scarano, Demetrio Del Prete, Rosa Lamacchia, Federica Antonicelli, Marco Rossi
Journal of Anesthesia, Analgesia and Critical Care.2022;[Epub] CrossRef - A rare complication: Tension pneumothorax after peroral endoscopic myotomy
Seokin Kang, Yuri Kim, Do Hoon Kim
International Journal of Gastrointestinal Intervention.2022; 11(3): 139. CrossRef - Endoscopic Management of Dysphagia
Min Ji Kim, Yang Won Min
The Korean Journal of Gastroenterology.2021; 77(2): 77. CrossRef - An update on endoscopic treatment for achalasia: From per oral endoscopic myotomy to endolumenal functional lumen imaging probe
Wei‐Chen Tai, Keng‐Liang Wu, Seng‐Kee Chuah
Advances in Digestive Medicine.2021; 8(1): 8. CrossRef
- Diffuse Esophageal Spasm: An Alternative Treatment Approach
- 4,440 View
- 133 Download
- 10 Web of Science
- 10 Crossref

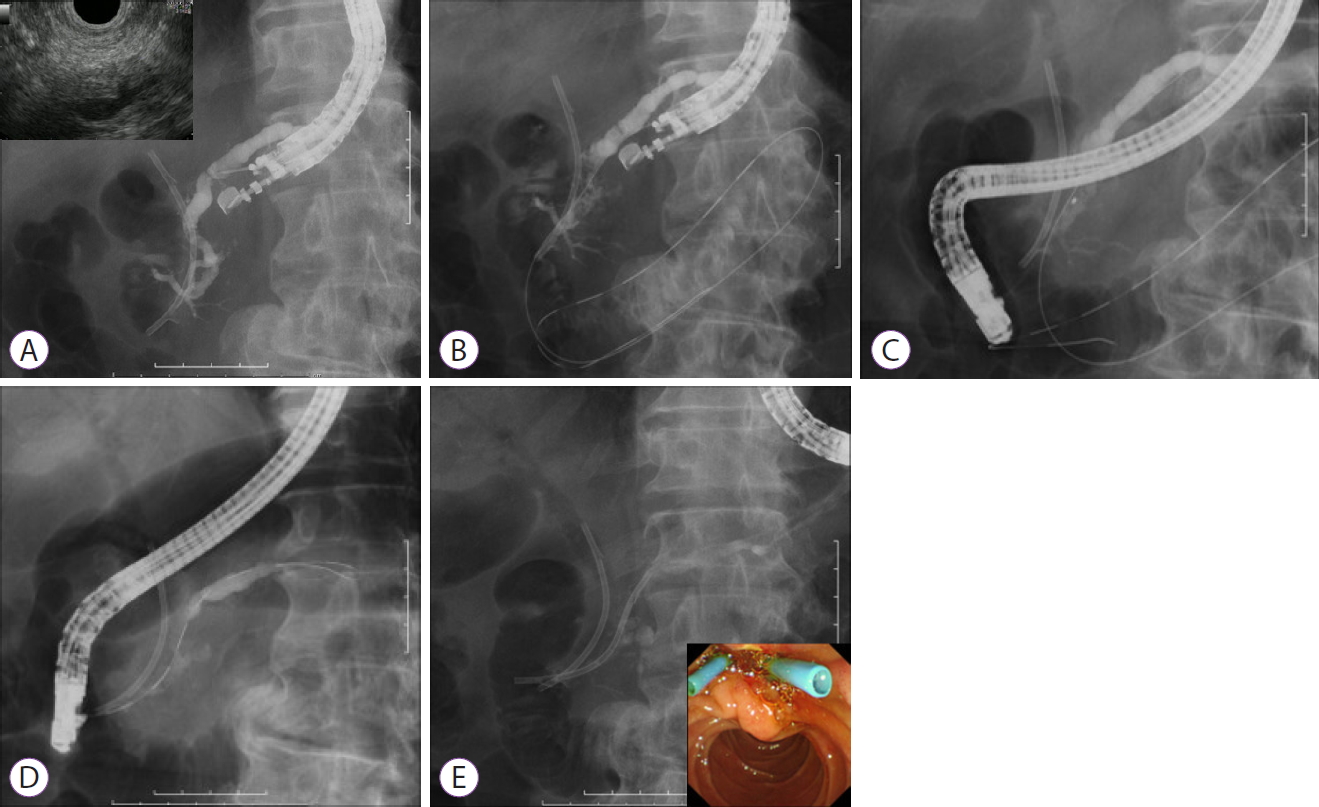
- Endoscopic Ultrasound-Guided Pancreatic Duct Drainage: Techniques and Literature Review of Transmural Stenting
- Akira Imoto, Takeshi Ogura, Kazuhide Higuchi
- Clin Endosc 2020;53(5):525-534. Published online September 24, 2020
- DOI: https://doi.org/10.5946/ce.2020.173
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic ultrasound-guided pancreatic duct drainage (EUS-PD) has emerged as an option in patients with failure of retrograde access to the pancreatic duct (PD) because of difficulty in cannulation or surgically altered anatomy. This article provides a comprehensive review of the techniques and outcomes of EUS-PD, especially EUS-guided pancreatic transmural stenting. The clinical data derived from a total of 401 patients were reviewed in which the overall technical and clinical success rates were 339/401 (85%, range 63%–100%) and 328/372 (88%, range 76%–100%), respectively. Short-term adverse events occurred in 25% (102/401) of the cases, which included abdominal pain (n=45), acute pancreatitis (n=17), bleeding (n=10), and issues associated with pancreatic juice leakage such as perigastric or peripancreatic fluid collection (n=9). In conclusion, although EUS-PD remains a challenging procedure with a high risk of adverse events such as pancreatic juice leakage, perforation, and severe acute pancreatitis, the procedure seems to be a promising alternative for PD drainage in patients with altered anatomy or unsuccessful endoscopic retrograde pancreatography.
-
Citations
Citations to this article as recorded by- Technical review of endoscopic ultrasound‐guided drainage/anastomosis and trans‐endosonographically created route procedures for the treatment of pancreatic diseases
Ko Tomishima, Hiroyuki Isayama, Akinori Suzuki, Shigeto Ishii, Sho Takahashi, Toshio Fujisawa
DEN Open.2025;[Epub] CrossRef - Best Practices in Pancreatico-biliary Stenting and EUS-guided Drainage
Renato Medas, Joel Ferreira-Silva, Mohit Girotra, Monique Barakat, James H. Tabibian, Eduardo Rodrigues-Pinto
Journal of Clinical Gastroenterology.2023; 57(6): 553. CrossRef - Techniques and Outcomes of Endoscopic Ultrasound Guided—Pancreatic Duct Drainage (EUS- PDD)
Jun Liang Teh, Anthony Yuen Bun Teoh
Journal of Clinical Medicine.2023; 12(4): 1626. CrossRef - Endoscopic treatment of biliopancreatic pathology in patients with Whipple's pancreaticoduodenectomy surgical variants: Lessons learned from single-balloon enteroscopy-assisted ERCP
Rodrigo Garcés-Durán, Laurent Monino, Pierre H Deprez, Hubert Piessevaux, Tom G Moreels
Hepatobiliary & Pancreatic Diseases International.2023;[Epub] CrossRef - EUS–guided pancreatic duct drainage using a novel plastic stent with ultratapered tip (with video)
Takeshi Ogura, Atsushi Okuda, Saori Ueno, Nobu Nishioka, Masahiro Yamamura
Endoscopic Ultrasound.2023; 12(3): 345. CrossRef - Treatment of Difficult Pancreatic Duct Strictures Using a Cystotome: A Single-Center Experience
Jonghyun Lee, Dong Uk Kim, Sung Yong Han
The Korean Journal of Pancreas and Biliary Tract.2023; 28(4): 108. CrossRef - Utility of a novel drill dilator for easier EUS‐guided pancreatic duct drainage
Kazuo Hara, Nozomi Okuno, Shin Haba, Takamichi Kuwahara, Yasuhiro Kuraishi, Takafumi Yanaidani, Daiki Fumihara, Masanori Yamada, Tsukasa Yasuda, Sho Ishikawa
Journal of Hepato-Biliary-Pancreatic Sciences.2022;[Epub] CrossRef - Endoscopic Ultrasound-guided Drainage in Pancreatobiliary Diseases
Tae Hyeon Kim, Hyung Ku Chon
The Korean Journal of Gastroenterology.2022; 79(5): 203. CrossRef - Percutaneous transluminal angioplasty balloons for endoscopic ultrasound-guided pancreatic duct interventions
Jad P AbiMansour, Barham K Abu Dayyeh, Michael J Levy, Andrew C Storm, John A Martin, Bret T Petersen, Ryan J Law, Mark D Topazian, Vinay Chandrasekhara
World Journal of Gastrointestinal Endoscopy.2022; 14(8): 487. CrossRef - Interventional endoscopic ultrasound
Christoph F. Dietrich, Barbara Braden, Christian Jenssen
Current Opinion in Gastroenterology.2021; 37(5): 449. CrossRef - Approach to management of pancreatic strictures: the gastroenterologist’s perspective
Vaneet Jearth, Suprabhat Giri, Sridhar Sundaram
Clinical Journal of Gastroenterology.2021; 14(6): 1587. CrossRef - Extracorporeal shock wave lithotripsy after endoscopic ultrasonographically guided pancreatic duct drainage with pancreatic stent placement for pancreatic stone removal: A case report
Mitsuru OKUNO, Tsuyoshi MUKAI, Shota IWATA, Ryuichi TEZUKA, Eiichi TOMITA
Suizo.2021; 36(4): 274. CrossRef
- Technical review of endoscopic ultrasound‐guided drainage/anastomosis and trans‐endosonographically created route procedures for the treatment of pancreatic diseases
- 5,780 View
- 225 Download
- 14 Web of Science
- 12 Crossref

- Present Status of Endoscopic Submucosal Dissection for Non-Ampullary Duodenal Epithelial Tumors
- Naomi Kakushima, Masao Yoshida, Yohei Yabuuchi, Noboru Kawata, Kohei Takizawa, Yoshihiro Kishida, Sayo Ito, Kenichiro Imai, Kinichi Hotta, Hirotoshi Ishiwatari, Hiroyuki Matsubayashi, Hiroyuki Ono
- Clin Endosc 2020;53(6):652-658. Published online January 15, 2020
- DOI: https://doi.org/10.5946/ce.2019.184
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Prediction of histology by endoscopic examination is important in the clinical management of non-ampullary duodenal epithelial tumors (NADETs), including adenoma and adenocarcinoma. The use of a simple scoring system based on the findings of white-light endoscopy or magnified endoscopy with narrow-band imaging is useful to differentiate between Vienna category 3 (C3) and C4/5 lesions. Less invasive endoscopic resection procedures, such as cold snare polypectomy, are quick to perform and convenient for small (<10 mm) C3 lesions. Neoplasms with higher grade histology, such as C4/5 lesions, should be treated by endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), or surgery. Although EMR often requires piecemeal resection, the complication rate is acceptable. Excellent complete resection rates could be achieved by ESD; however, it remains a challenging method considering the high risk of complications. Shielding or closure of the ulcer after ESD is effective at decreasing the risk of delayed bleeding and perforation. Laparoscopic endoscopic cooperative surgery is an ideal treatment with a high rate of en bloc resection and a low rate of complications, although it is limited to high-volume centers. Patients with NADETs could benefit from a multidisciplinary approach to stratify the optimal treatment based on endoscopic diagnoses.
-
Citations
Citations to this article as recorded by- The Characteristics and Treatment Outcomes of 71 Duodenal Brunner’s Gland Adenomas with Endoscopic Submucosal Dissection
Ying Xiang, Jinyan Liu, Nan ya Wang, Dehua Tang, Lei Wang, Ping xiao Zou, Guifang Xu, Qin Huang
Digestive Diseases.2023; 41(6): 852. CrossRef - Endoscopic diagnosis and treatment of superficial non-ampullary duodenal epithelial tumors: A review
Zheng Zhao, Yue Jiao, Shuyue Yang, Anni Zhou, Guiping Zhao, Shuilong Guo, Peng Li, Shutian Zhang
Journal of Translational Internal Medicine.2023; 11(3): 206. CrossRef - Current Treatment Strategy for Superficial Nonampullary Duodenal Epithelial Tumors
Tetsuya Suwa, Kohei Takizawa, Noboru Kawata, Masao Yoshida, Yohei Yabuuchi, Yoichi Yamamoto, Hiroyuki Ono
Clinical Endoscopy.2022; 55(1): 15. CrossRef - Rapid and chronological expression of angiogenetic genes is a major mechanism involved in cell sheet transplantation in a rat gastric ulcer model
Shun Yamaguchi, Miki Higashi, Kengo Kanetaka, Yasuhiro Maruya, Shinichiro Kobayashi, Keiichi Hashiguchi, Masaaki Hidaka, Kazuhiko Nakao, Susumu Eguchi
Regenerative Therapy.2022; 21: 372. CrossRef - Survival comparison between endoscopic and surgical resection for non-ampullary duodenal neuroendocrine tumor (1–2 cm)
Jiebin Xie, Yuan Zhang, Ming He, Xu Liu, Pin Xie, Yueshan Pang
Scientific Reports.2022;[Epub] CrossRef - Efficacy, feasibility, and safety of endoscopic double closure in the GI tract
Ahmad M. Al-Taee, Kohtaro Ooka, Gregory B. Haber, Jonathan Cohen
iGIE.2022; 1(1): 19. CrossRef - Current endoscopic diagnosis treatment strategy for superficial nonampullary duodenal tumours
Aichun Li, Jianwei Shen
European Journal of Medical Research.2022;[Epub] CrossRef - The incidence of non‐ampullary duodenal cancer in Japan: The first analysis of a national cancer registry
Masao Yoshida, Yohei Yabuuchi, Naomi Kakushima, Motohiko Kato, Mikitaka Iguchi, Yorimasa Yamamoto, Kengo Kanetaka, Toshio Uraoka, Mitsuhiro Fujishiro, Masayuki Sho
Journal of Gastroenterology and Hepatology.2021; 36(5): 1216. CrossRef - White light and/or magnifying endoscopy with narrow band imaging for superficial nonampullary duodenal epithelial tumors
Naomi Kakushima, Masao Yoshida, Kohei Takizawa, Yohei Yabuuchi, Noboru Kawata, Yoshihiro Kishida, Sayo Ito, Kenichiro Imai, Kinichi Hotta, Hirotoshi Ishiwatari, Hiroyuki Matsubayashi, Hiroyuki Ono
Scandinavian Journal of Gastroenterology.2021; 56(2): 211. CrossRef - Endoscopic management of superficial nonampullary duodenal tumors: European Society of Gastrointestinal Endoscopy (ESGE) Guideline
Geoffroy Vanbiervliet, Alan Moss, Marianna Arvanitakis, Urban Arnelo, Torsten Beyna, Olivier Busch, Pierre H. Deprez, Lumir Kunovsky, Alberto Larghi, Gianpiero Manes, Bertrand Napoleon, Kumanan Nalankilli, Manu Nayar, Enrique Pérez-Cuadrado-Robles, Stefan
Endoscopy.2021; 53(05): 522. CrossRef - Endoscopic Treatment for Superficial Nonampullary Duodenal Tumors
Hyo-Joon Yang
The Korean Journal of Gastroenterology.2021; 77(4): 164. CrossRef - Duodenal endoscopic submucosal dissection: Is it ready for primetime? (with video)
Sergey V. Kantsevoy
Gastrointestinal Endoscopy.2020; 91(5): 1138. CrossRef - Life on a knife edge: the optimal approach to the management of perforations during endoscopic submucosal dissection (ESD)
Shria Kumar, Young Hoon Youn, Jeffrey H. Lee
Expert Review of Gastroenterology & Hepatology.2020; 14(10): 965. CrossRef - Tapering body stiffness shortens upper gastrointestinal examination via transoral insertion with ultrathin endoscope
Satoshi Ono, Shun Ito, Kyohei Maejima, Shosuke Hosaka, Kiyotaka Umeki, Shin-ichiro Sato
Endoscopy International Open.2020; 08(12): E1748. CrossRef
- The Characteristics and Treatment Outcomes of 71 Duodenal Brunner’s Gland Adenomas with Endoscopic Submucosal Dissection
- 7,154 View
- 239 Download
- 14 Web of Science
- 14 Crossref

- Effectiveness of Endoscopic Sclerotherapy with Aluminum Potassium Sulfate and Tannic Acid as a Non-Surgical Treatment for Internal Hemorrhoids
- Yuichi Tomiki, Jun Aoki, Shunsuke Motegi, Rina Takahashi, Toshiaki Hagiwara, Yu Okazawa, Kosuke Mizukoshi, Masaya Kawai, Shinya Munakata, Shun Ishiyama, Kiichi Sugimoto, Kazuhiro Sakamoto
- Clin Endosc 2019;52(6):581-587. Published online July 24, 2019
- DOI: https://doi.org/10.5946/ce.2019.017
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
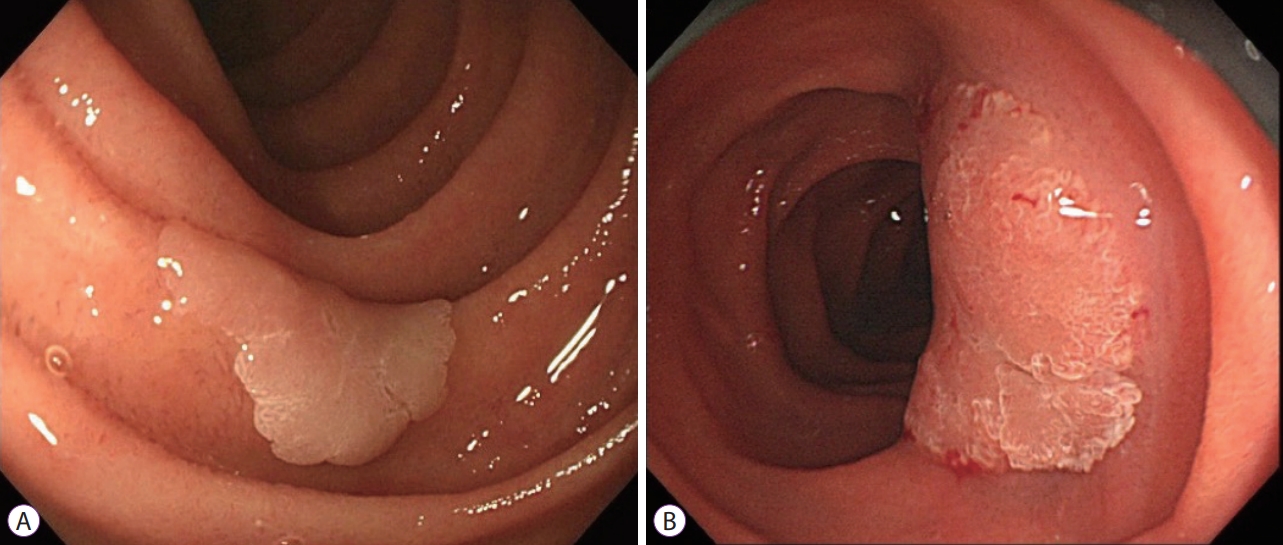
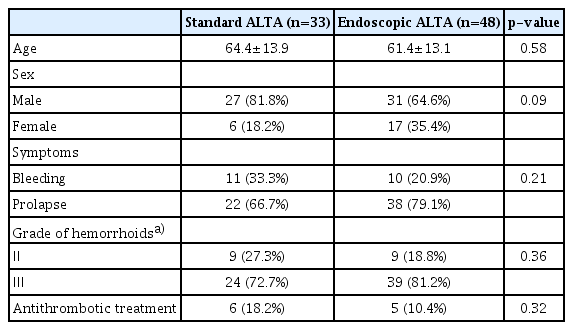
ePub - Background
/Aims: Sclerotherapy with aluminum potassium sulfate and tannic acid (ALTA) has a potent effect on internal hemorrhoids. In this retrospective study, we compared the effects of endoscopic ALTA therapy and standard ALTA therapy.
Methods
We investigated patients who underwent treatment for internal hemorrhoids at our institution between 2014 and 2016. They were divided into a standard ALTA group (n=33, treated using proctoscopy) and an endoscopic ALTA group (n=48). We compared the clinical findings between the 2 groups.
Results
There were no intergroup differences in background factors. The mean ALTA dose was 21.9±7.2 mL and 17.8±3.4 mL in the standard and endoscopic ALTA groups, respectively (p<0.01). Adverse events occurred in 4 patients (12.1%) from the standard ALTA group and 6 patients (12.5%) from the endoscopic ALTA group. In both groups, the patients reported good satisfaction with the therapeutic effect at 1 month after the procedure. Hemorrhoids recurred in 2 patients (6.3%) from the standard ALTA group and 4 patients (8.3%) from the endoscopic ALTA group.
Conclusions
Endoscopic ALTA sclerotherapy is equivalent to standard ALTA therapy in terms of efficacy, adverse events, and recurrence. Therefore, it is a useful non-surgical option for patients with internal hemorrhoids who prefer a less invasive treatment. -
Citations
Citations to this article as recorded by- Sclerotherapy for hemorrhoidal disease: systematic review and meta-analysis
G. Gallo, A. Picciariello, C. Armellin, E. Lori, G. Tomasicchio, G. L. Di Tanna, G. A. Santoro, M. Alharbi, S. Sorrenti, U. Grossi
Techniques in Coloproctology.2024;[Epub] CrossRef - Aluminum potassium sulfate and tannic acid (ALTA) sclerotherapy for hemorrhoidal disease: a systematic review and meta-analysis
Vasiliki Manaki, Vangelis Bontinis, Alkis Bontinis, Argirios Giannopoulos, Ioannis Kontes, Angeliki Chorti, Kiriakos Ktenidis
Acta Chirurgica Belgica.2024; : 1. CrossRef - Sclerotherapy in Hemorrhoids
Anling He, Mingkai Chen
Indian Journal of Surgery.2023; 85(2): 228. CrossRef - Aluminum potassium sulfate and tannic acid (ALTA) sclerotherapy complicating laparoscopic low anterior resection of rectal cancer: Case report
Hiroka Kondo, Ryosuke Nakagawa, Tomoko Yamamoto, Shigeki Yamaguchi
International Journal of Surgery Case Reports.2022; 98: 107543. CrossRef - Laparoscopic anterior resection for rectal stenosis caused by ALTA injection for internal hemorrhoids: A case report
Masanori Yoshimitsu, Hiroyuki Egi, Mayumi Kaneko, Manabu Shimomura, Keishi Hakoda, Masashi Miguchi, Toshihiko Kohashi, Jun Hihara, Naoki Hirabayashi, Hideki Ohdan
Asian Journal of Endoscopic Surgery.2021; 14(2): 271. CrossRef - Rationale, new anus positioning methods, and updated protocols: Expert recommendations on cap-assisted endoscopic sclerotherapy for hemorrhoids from China Gut Conference
Fa-Ming Zhang, Kai-Chun Wu, Jing-Nan Li, Xin Wang, Xing-Xiang He, Rong Wan, Shi-Yao Chen
Chinese Medical Journal.2021; 134(22): 2675. CrossRef - Cap-assisted endoscopic sclerotherapy for internal hemorrhoids: technique protocol and study design for a multi-center randomized controlled trial
Xia Wu, Quan Wen, Bota Cui, Yafei Liu, Min Zhong, Yu Yuan, Lihao Wu, Xiaoyin Zhang, Yunlian Hu, Muhan Lv, Qianneng Wu, Suyu He, Yan Jin, Shuxin Tian, Rong Wan, Xin Wang, Long Xu, Jianling Bai, Guangming Huang, Guozhong Ji, Faming Zhang
Therapeutic Advances in Gastrointestinal Endoscopy.2020; 13: 263177452092563. CrossRef - Gluteal-fold flap repair of rectovaginal fistula caused by aluminum potassium sulfate hydrate-tannic acid injection for internal hemorrhoids: a case report
Masanori Yoshimitsu, Hiroyuki Egi, Shogo Nagamatsu, Manabu Shimomura, Keishi Hakoda, Masashi Miguchi, Toshihiko Kohashi, Masazumi Okajima, Hideki Ohdan
Surgical Case Reports.2020;[Epub] CrossRef - Progress in endoscopic treatment of hemorrhoids
Wenzhuang Ma, Jintao Guo, Fan Yang, Christoph F. Dietrich, Siyu Sun
Journal of Translational Internal Medicine.2020; 8(4): 237. CrossRef - Endoscopic Sclerotherapy with Aluminum Potassium Sulfate and Tannic Acid: An Effective and Less Invasive Strategy for Internal Hemorrhoids
Naoki Muguruma, Tetsuji Takayama
Clinical Endoscopy.2019; 52(6): 521. CrossRef
- Sclerotherapy for hemorrhoidal disease: systematic review and meta-analysis
- 8,119 View
- 190 Download
- 9 Web of Science
- 10 Crossref

- Is Radical Surgery Necessary for All Patients Diagnosed as Having Non-Curative Endoscopic Submucosal Dissection?
- Si Hyung Lee, Byung Sam Park
- Clin Endosc 2019;52(1):21-29. Published online January 30, 2019
- DOI: https://doi.org/10.5946/ce.2019.014
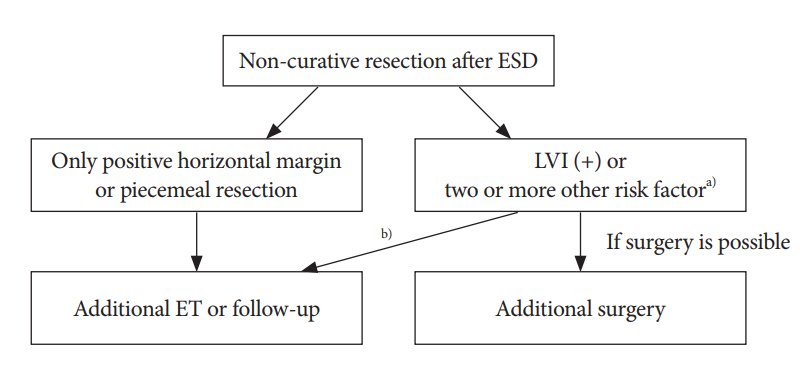
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - If a lesion does not meet the expanded indication criteria for treatment with endoscopic therapy for early gastric cancer or does not have a positive resection margin, it is regarded as suitable for non-curative resection. Non-curative resection is closely related to the risk of local recurrence, lymph node metastasis, and poor prognosis. If the result is confirmed as non-curative resection, additional treatment should be considered depending on the risks of residual tumor, local recurrence, and lymph node metastasis. As lymphatic invasion is the most important risk factor of recurrence and poor prognosis, surgical treatment should be considered if lymphatic invasion is present. If patients are not suitable for additional surgery owing to old age or coexisting severe disease, close surveillance can be an alternative treatment option.
-
Citations
Citations to this article as recorded by- Risk Factors and Clinical Outcomes of Non-Curative Resection in Patients with Early Gastric Cancer Treated with Endoscopic Submucosal Dissection: A Retrospective Multicenter Study in Korea
Si Hyung Lee, Min Cheol Kim, Seong Woo Jeon, Kang Nyeong Lee, Jong Jae Park, Su Jin Hong
Clinical Endoscopy.2020; 53(2): 196. CrossRef
- Risk Factors and Clinical Outcomes of Non-Curative Resection in Patients with Early Gastric Cancer Treated with Endoscopic Submucosal Dissection: A Retrospective Multicenter Study in Korea
- 6,133 View
- 102 Download
- 1 Web of Science
- 1 Crossref

- Laparoscopic Resection of a Jejunal Inflammatory Fibroid Polyp that Caused Occult Gastrointestinal Bleeding, Diagnosed via Capsule Endoscopy and Double-Balloon Enteroscopy: A Case Report
- Chizu Kameda, Hideaki Miwa, Ryohei Kawabata, Daiki Marukawa, Masahiro Murakami, Shingo Noura, Junzo Shimizu, Junichi Hasegawa
- Clin Endosc 2018;51(4):384-387. Published online March 20, 2018
- DOI: https://doi.org/10.5946/ce.2017.162
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - An inflammatory fibroid polyp (IFP) is a mesenchymal tumor of the gastrointestinal tract. IFPs in the small intestine are the most frequently detected with symptoms, such as abdominal pain and tarry stool due to intussusception. Accordingly, few studies have reported jejunal IFP as a cause of occult gastrointestinal bleeding (OGIB) diagnosed via both of capsule endoscopy (CE) and double-balloon enteroscopy (DBE). A 68-year-old woman presented with a progression of anemia and a positive fecal occult blood test result. Esophagogastroduodenoscopy and total colonoscopy findings were unremarkable. CE revealed a tumor with bleeding in the jejunum. DBE also revealed a jejunal polypoid tumor. Bleeding from the tumor seemed to have caused anemia. The patient underwent partial laparoscopic resection of the jejunum, including resection of the tumor. The tumor was histopathologically diagnosed as IFP. To our knowledge, this is the first reported case of laparoscopic resection of jejunal IFP with OGIB diagnosed via CE and DBE preoperatively.
-
Citations
Citations to this article as recorded by- Minimally invasive colonoscopy treatment of inflammatory fibroid polyps in the terminal ileum
Yin-Si Tang, Lu Liu, Ying Gao, Qiao-Chu He, Hai-Mei Guo, Zhi-Feng Zhao
Scientific Reports.2023;[Epub] CrossRef - Where does capsule endoscopy fit in the diagnostic algorithm of small bowel intussusception?
Stefania Chetcuti Zammit, Aman Yadav, Deirdre McNamara, Alejandro Bojorquez, Cristina Carretero-Ribón, Martin Keuchel, Peter Baltes, Reuma Margalit-Yehuda, Uri Kopylov, Reena Sidhu, Clelia Marmo, Maria Elena Riccioni, Xavier Dray, Romain Leenhardt, Emanue
Digestive and Liver Disease.2023; 55(12): 1719. CrossRef - Cystic lymphangioma in the peripheral jejunal mesentery in an adult and excision with laparoscopic-assisted surgery: a case report
Hideki Nagano, Toshihisa Kimura, Atsushi Iida, Tamotsu Togawa, Takanori Goi, Yasunori Sato
World Journal of Surgical Oncology.2019;[Epub] CrossRef
- Minimally invasive colonoscopy treatment of inflammatory fibroid polyps in the terminal ileum
- 5,565 View
- 92 Download
- 4 Web of Science
- 3 Crossref

- Current Status of Peroral Endoscopic Myotomy
- Young Kwan Cho, Seong Hwan Kim
- Clin Endosc 2018;51(1):13-18. Published online January 31, 2018
- DOI: https://doi.org/10.5946/ce.2017.165
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Peroral endoscopic myotomy (POEM) has been established as an optional treatment for achalasia. POEM is an endoluminal procedure that involves dissection of esophageal muscle fibers followed by submucosal tunneling. Inoue first attempted to use POEM for the treatment of achalasia in humans. Expanded indications of POEM include classic indications such as type I, type II, type III achalasia, failed prior treatments, including Botulinum toxin injection, endoscopic balloon dilation, laparoscopic Heller myotomy, and hypertensive motor disorders such as diffuse esophageal spasm, jackhammer esophagus. Contraindications include prior radiation therapy to the esophagus and prior extensive esophageal mucosal resection/ablation involving the POEM field. Most of the complications are minor and self-limited and can be managed conservatively. As POEM emerged as the main treatment for achalasia, various adaptations to tunnel endoscopic surgery have been attempted. Tunnel endoscopic surgery includes POEM, peroral endoscopic tumor resection, gastric peroral endoscopic pyloromyotomy. POEM has been widely accepted as a treatment for all types of achalasia, even for specific cases such as achalasia with failed prior treatments, and hypertensive motor disorders.
-
Citations
Citations to this article as recorded by- Quality of Life of Patients with Achalasia After Minimally Invasive Interventions
E.A. Drobyazgin, Yu.V. Chikinev, N.I. Mitko
Dokazatel'naya gastroenterologiya.2023; 12(3): 43. CrossRef - Colorectal Endoscopic Submucosal Dissection: Performance of a Novel Hybrid-Technology Knife in an Animal Trial
Jérémie Jacques, Horst Neuhaus, Markus D. Enderle, Ulrich Biber, Walter Linzenbold, Martin Schenk, Kareem Khalaf, Alessandro Repici
Diagnostics.2023; 13(21): 3347. CrossRef - Outcomes of Per-Oral Endoscopic Myotomy in the Treatment of Esophageal Achalasia: Over One Hundred Cases in a Single Tertiary Center
Kannikar Laohavichitra, Jerasak Wannaprasert, Thawee Raranachu-ek
Siriraj Medical Journal.2023; 75(9): 629. CrossRef - Geriatric patients with esophageal motility disorders benefit more from minimally invasive peroral endoscopic myotomy: a multicenter study in Japan
Naoto Ujiie, Hiroki Sato, Mary Raina Angeli Fujiyoshi, Shinwa Tanaka, Hironari Shiwaku, Junya Shiota, Ryo Ogawa, Hiroshi Yokomichi, Takashi Kamei, Haruhiro Inoue
Diseases of the Esophagus.2022;[Epub] CrossRef - Nonachalasic esophageal motor disorders, from diagnosis to therapy
Mentore Ribolsi, Matteo Ghisa, Edoardo Savarino
Expert Review of Gastroenterology & Hepatology.2022; 16(3): 205. CrossRef - Peroral endoscopic longer vs shorter esophageal myotomy for achalasia treatment: A systematic review and meta-analysis
Chun-Yan Weng, Cheng-Hai He, Ming-Yang Zhuang, Jing-Li Xu, Bin Lyu
World Journal of Gastrointestinal Surgery.2022; 14(3): 247. CrossRef - Features and results of minimally invasive treatment of recurrent achalasia
E.A. Gallyamov, S.A. Erin, G.Yu. Gololobov, A.I. Burmistrov, M.A. Chicherina, A.A. Rikunova
Khirurgiya. Zhurnal im. N.I. Pirogova.2022; (3): 16. CrossRef - Anesthesia for Per-oral endoscopic myotomy (POEM) – not so poetic!
Soumya Sarkar, Puneet Khanna, Deepak Gunjan
Journal of Anaesthesiology Clinical Pharmacology.2022; 38(1): 28. CrossRef - A rare complication: Tension pneumothorax after peroral endoscopic myotomy
Seokin Kang, Yuri Kim, Do Hoon Kim
International Journal of Gastrointestinal Intervention.2022; 11(3): 139. CrossRef - Endoscopic management of mucosal incision site dehiscence following peroral endoscopic myotomy
Suryaprakash Bhandari, Darshan Parekh, Smita Bhandari
Endoscopy International Open.2022; 10(09): E1307. CrossRef - The POEM bottom-up technique for achalasia
Gad Marom, Harold Jacob, Ariel Benson, Tiberiu Hershcovici, Rachel Gefen, Jonathan B. Yuval, Ronit Brodie, Avraham I Rivkind, Yoav Mintz
Surgical Endoscopy.2021; 35(11): 6117. CrossRef - Per-oral endoscopic myotomy for esophageal diverticula with or without esophageal motility disorders
Beatrice Orlandini, Maximilien Barret, Marie-Anne Guillaumot, Chloé Léandri, Sarah Leblanc, Frédéric Prat, Stanislas Chaussade
Clinics and Research in Hepatology and Gastroenterology.2020; 44(1): 82. CrossRef - Experience with Peroral Endoscopic Myotomy for Achalasia and Spastic Esophageal Motility Disorders at a Tertiary U.S. Center
Maen Masadeh, Peter Nau, Subhash Chandra, Jagpal Klair, John Keech, Kalpaj Parekh, Rami El Abiad, Henning Gerke
Clinical Endoscopy.2020; 53(3): 321. CrossRef - Intraoperative use of a functional lumen imaging probe during peroral endoscopic myotomy in patients with achalasia: A single-institute experience and systematic review
Hyeon Jeong Goong, Su Jin Hong, Shin Hee Kim, Shawn Groth
PLOS ONE.2020; 15(6): e0234295. CrossRef - How does per-oral endoscopic myotomy compare to Heller myotomy? The Latin American perspective
Michel Kahaleh, Amy Tyberg, Supriya Suresh, Arnon Lambroza, Monica Gaidhane, Felipe Zamarripa, Guadalupe Ma Martínez, Juan C. Carames, Eduardo T. Moura, Galileu F. Farias, Maria G. Porfilio, Jose Nieto, Mario Rey, Fernando Rodriguez Casas, Oscar V. Mondra
Endoscopy International Open.2020; 08(10): E1392. CrossRef - Endoscopic Equipment—From Simple to Advanced
Sarah Choi, Kevin El-Hayek
Surgical Clinics of North America.2020; 100(6): 993. CrossRef - Peroral Endoscopic Myotomy for Esophageal Motility Disorders
Jun Young Kim, Yang Won Min
Clinical Endoscopy.2020; 53(6): 638. CrossRef - Anesthesia for peroral endoscopic myotomy in Japan
Hiroaki Murata, Taiga Ichinomiya, Tetsuya Hara
Current Opinion in Anaesthesiology.2019; 32(4): 511. CrossRef - Anesthetic Consideration for Peroral Endoscopic Myotomy
Yun-Sic Bang, Chunghyun Park
Clinical Endoscopy.2019; 52(6): 549. CrossRef
- Quality of Life of Patients with Achalasia After Minimally Invasive Interventions
- 8,694 View
- 316 Download
- 20 Web of Science
- 19 Crossref

- Introduction to Endoscopic Submucosal Surgery
- Weon Jin Ko, Joo Young Cho
- Clin Endosc 2018;51(1):8-12. Published online January 23, 2018
- DOI: https://doi.org/10.5946/ce.2017.154
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The concept of using natural orifices to reduce the complications of surgery, Natural Orifices Transluminal Endoscopic Surgery, has also been applied to therapeutic endoscopy. Endoscopic submucosal surgery (ESS) provides more treatment options for various gastrointestinal diseases than traditional therapeutic endoscopy by using the submucosal layer as a working space. ESS has been performed in various fields ranging from transluminal peritoneoscopy to peroral endoscopic myotomy. With further advances in technology, ESS will be increasingly useful for diagnosis and treatment of gastrointestinal diseases.
-
Citations
Citations to this article as recorded by- Design and validation of performance-oriented injectable chitosan thermosensitive hydrogels for endoscopic submucosal dissection
Jia Liu, Panxianzhi Ni, Yi Wang, Zhengkui Zhou, Junlin Li, Tianxu Chen, Tun Yuan, Jie Liang, Yujiang Fan, Jing Shan, Xiaobin Sun, Xingdong Zhang
Biomaterials Advances.2023; 146: 213286. CrossRef - Comparison of peroral endoscopic myotomy between de-novo achalasia and achalasia with prior treatment
Abdullah Ozgur Yeniova, In kyung Yoo, Eunju Jeong, Joo Young Cho
Surgical Endoscopy.2021; 35(1): 200. CrossRef - Tunnel endoscopic interventions in esophageal diseases
E. A. Drobyazgin, Yu. V. Chikinev, D. A. Arkhipov, N. I. Mit’ko, M. N. Chekanov, E. I. Vereshchagin, I. V. Peshkova, A. S. Polyakevich
Experimental and Clinical Gastroenterology.2021; 1(6): 75. CrossRef
- Design and validation of performance-oriented injectable chitosan thermosensitive hydrogels for endoscopic submucosal dissection
- 5,361 View
- 157 Download
- 3 Web of Science
- 3 Crossref

- Endoscopic Full-Thickness Resection Combined with Laparoscopic Surgery
- Chan Gyoo Kim
- Clin Endosc 2018;51(1):33-36. Published online January 12, 2018
- DOI: https://doi.org/10.5946/ce.2017.153
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic full-thickness resection combined with laparoscopic surgery was recently developed. These procedures could be categorized as “Cut first and then suture” and “Suture first and then cut”. “Cut first and then suture” includes laparoscopic and endoscopic cooperative surgery (LECS) and laparoscopy-assisted endoscopic full-thickness resection (LAEFR). Recent studies have demonstrated the safety and efficacy of LECS and LAEFR. However, these techniques are limited by the related exposure of the tumor and gastric mucosa to the peritoneal cavity and manipulation of these organs, which could lead to viable cancer cell seeding and the spillage of gastric juice into the peritoneal cavity. In the “Suture first and then cut” technique, the serosal side of the stomach is sutured to invert the stomach and subsequently endoscopic resection is performed. In this article, details of these techniques, including their advantages and limitations, are described.
-
Citations
Citations to this article as recorded by- ‘The parachute method’: A novel technique for laparoscopic tumour handling
Noriaki Kashu, Noriyuki Nishiwaki, Tetsuya Kagawa, Tomokazu Kakishita, Shinji Hato
Journal of Minimal Access Surgery.2024; 20(1): 111. CrossRef - Endoscopic Full Thickness Resection: A Systematic Review
Partha Pal, Mohan Ramchandani, Pradev Inavolu, Duvvuru Nageshwar Reddy, Manu Tandan
Journal of Digestive Endoscopy.2022; 13(03): 152. CrossRef - Choice of LECS Procedure for Benign and Malignant Gastric Tumors
Jae-Seok Min, Kyung Won Seo, Sang-Ho Jeong
Journal of Gastric Cancer.2021; 21(2): 111. CrossRef - Combined surgical and endoscopic approaches to full-thickness resection
Thomas C. Tsai, Ozanan R. Meireles
Techniques in Gastrointestinal Endoscopy.2019; 21(1): 26. CrossRef - Combined Laparoscopic-Endoscopic Techniques for Removal of Small Gastric Tumors: Advantages and Tricks
Eva Intagliata, Rosario Vecchio
Clinical Endoscopy.2019; 52(4): 390. CrossRef - Laparoscopic and endoscopic cooperative surgery for gastric tumors: Perspective for actual practice and oncological benefits
Yuki Aisu, Daiki Yasukawa, Yusuke Kimura, Tomohide Hori
World Journal of Gastrointestinal Oncology.2018; 10(11): 381. CrossRef
- ‘The parachute method’: A novel technique for laparoscopic tumour handling
- 5,757 View
- 201 Download
- 8 Web of Science
- 6 Crossref

- Long -Term Survival in Stage IV Esophageal Adenocarcinoma with Chemoradiation and Serial Endoscopic Cryoablation
- Zachary Spiritos, Parit Mekaroonkamol, Bassel F. El- Rayes, Seth D. Force, Steven A. Keilin, Qiang Cai, Field F. Willingham
- Clin Endosc 2017;50(5):491-494. Published online April 24, 2017
- DOI: https://doi.org/10.5946/ce.2017.006
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Esophageal cancer has a poor overall prognosis and is frequently diagnosed at a late stage. Conventional treatment for metastatic esophageal cancer involves chemotherapy and radiation. Local disease control plays a significant role in improving survival. Endoscopic spray cryotherapy is a novel modality that involves freezing and thawing to produce local ablation of malignant tissue via ischemic mechanisms. Spray cryotherapy has been shown to be effective, particularly for early T-stage, superficial esophageal adenocarcinomas. We present the case of a 72-year-old-male with locally recurrent stage IV esophageal adenocarcinoma and long-term survival of 7 years to date, with concurrent chemoradiation and serial cryoablation. He remains asymptomatic and continues to undergo chemotherapy and sequential cryoablation. The findings highlight the long-term safety and efficacy of cryotherapy in combination with chemoradiation, and suggest that cryoablation may have an additive role in the treatment of advanced stage esophageal adenocarcinoma.
-
Citations
Citations to this article as recorded by- Endoscopic Palliative Therapies for Esophageal Cancer
Youssef Y. Soliman, Madappa Kundranda, Toufic Kachaamy
Gastrointestinal Endoscopy Clinics of North America.2024; 34(1): 91. CrossRef - Role of oesophageal balloon cryoablation in combination with personalised immunotherapy to achieve luminal control in metastatic oesophageal cancer: a case report
Benjamin Charles Norton, Apostolis Papaefthymiou, Andrea Telese, Margaret Duku, Imran Chaudhry, Alberto Murino, Gavin Johnson, Charles Murray, Rehan Haidry
Frontline Gastroenterology.2024; 15(4): 336. CrossRef - Cryoballoon ablation as salvage therapy after nonradical resection of a high-risk T1b esophageal adenocarcinoma: a case report
Charlotte N. Frederiks, Jolanda M.W. van de Water, Gati Ebrahimi, Bas L.A.M. Weusten
European Journal of Gastroenterology & Hepatology.2022; 34(3): 354. CrossRef - Surgery to the primary tumor is associated with improved survival of patients with metastatic esophageal cancer: propensity score-matched analyses of a large retrospective cohort
Rui Zhang, Jiahua Zou, Ping Li, Qin Li, Yunfeng Qiao, Jianglong Han, Kejie Huang, Peng Ruan, Huiqing Lin, Qibin Song, Zhenming Fu
Diseases of the Esophagus.2019;[Epub] CrossRef
- Endoscopic Palliative Therapies for Esophageal Cancer
- 6,805 View
- 129 Download
- 3 Web of Science
- 4 Crossref

- Role of Endoscopic Gastroplasty Techniques in the Management of Obesity
- Yunho Jung
- Clin Endosc 2017;50(1):21-25. Published online January 30, 2017
- DOI: https://doi.org/10.5946/ce.2016.147
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Health and wellness represent a major global concern. Trends such as a lack of exercise and excessive consumption of calories are major causes of the rapid increase in obesity worldwide. Obesity should be controlled because it can result in other illnesses, such as diabetes, high blood pressure, high cholesterol, coronary artery disease, stroke, breathing disorders, or cancer. However, many people have difficulty in managing obesity through exercise, dietary control, behavioral modifications, and drug therapy. Bariatric surgery is not commonly used due to a variety of complications, even though it has been demonstrated to produce reliable results with respect to adequate weight loss when performed using an open or a laparoscopic approach. Endoscopic bariatric procedures are emerging techniques that are less invasive and safer compared with current surgical approaches. However, the evaluation of endoluminal procedures is limited by the small number of studies and their short-term follow-up.
-
Citations
Citations to this article as recorded by- Left gastric artery embolization for obesity treatment: a systematic review and meta-analysis of human and animal studies
Malkhaz Mizandari, Pedram Keshavarz, Tamta Azrumelashvili, Fereshteh Yazdanpanah, Elnaz Lorzadeh, Hamidreza Hosseinpour, Amir Bazyar, Seyed Faraz Nejati, Faranak Ebrahimian Sadabad
Abdominal Radiology.2021; 46(9): 4440. CrossRef - Bariatric Embolization of the Left Gastric Arteries for the Treatment of Obesity: 9-Month Data in 5 Patients
Zhi-Bin Bai, Yong-Lin Qin, Gang Deng, Guo-Feng Zhao, Bin-Yan Zhong, Gao-Jun Teng
Obesity Surgery.2018; 28(4): 907. CrossRef - Bariatric Arterial Embolization for Obesity: A Review of Early Clinical Evidence
Bin-Yan Zhong, Godwin Abiola, Clifford R. Weiss
CardioVascular and Interventional Radiology.2018; 41(11): 1639. CrossRef - Incidence of nausea and vomiting after intragastric balloon placement in bariatric patients – A systematic review and meta-analysis
Judy Trang, Seung Su Lee, Assia Miller, Christian X. Cruz Pico, Angelina Postoev, Isaac Ibikunle, Christopher Alade Ibikunle
International Journal of Surgery.2018; 57: 22. CrossRef
- Left gastric artery embolization for obesity treatment: a systematic review and meta-analysis of human and animal studies
- 10,207 View
- 217 Download
- 3 Web of Science
- 4 Crossref

- Endoscopic Approach for Major Complications of Bariatric Surgery
- Moon Kyung Joo
- Clin Endosc 2017;50(1):31-41. Published online December 23, 2016
- DOI: https://doi.org/10.5946/ce.2016.140
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - As lifestyle and diet patterns have become westernized in East Asia, the prevalence of obesity has rapidly increased. Bariatric surgeries, such as Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (SG), and laparoscopic adjustable gastric banding (LAGB), are considered the first-line treatment option in patients with severe obesity. However, postoperative complications have increased and the proper management of these complications, including the use of endoscopic procedures, has become important. The most serious complications, such as leaks and fistulas, can be treated with endoscopic stent placement and injection of fibrin glue, and a novel full-thickness closure over-the-scope clip (OTSC) has been used for treatment of postoperative leaks. Stricture at the gastrojejunal (GJ) anastomosis site after RYGB or incisura angularis in SG can be managed using stents or endoscopic balloon dilation. Dilation of the GJ anastomosis or gastric pouch may lead to failure of weight loss, and the use of endoscopic sclerotherapy, novel endoscopic suturing devices, and OTSCs have been attempted. Intragastric migration of the gastric band can be successfully treated using various endoscopic tools. Endoscopy plays a pivotal role in the management of post-bariatric complications, and close cooperation between endoscopists and bariatric surgeons may further increase the success rate of endoscopic procedures.
-
Citations
Citations to this article as recorded by- Advanced endolumenal management of acute and chronic leaks after bariatric surgery
Andrew R. Harner, Francisco Jr Guerra, Shinil K. Shah, Kulvinder S. Bajwa, Peter A. Walker, Erik B. Wilson, Melissa M. Felinski
Mini-invasive Surgery.2024;[Epub] CrossRef - Current Management and Treatment Paradigms of Gastroesophageal Reflux Disease following Sleeve Gastrectomy
Muaaz Masood, Donald E. Low, Shanley B. Deal, Richard A. Kozarek
Journal of Clinical Medicine.2024; 13(5): 1246. CrossRef - Endoscopic Management of Post-Sleeve Gastrectomy Complications
Muaaz Masood, Donald E. Low, Shanley B. Deal, Richard A. Kozarek
Journal of Clinical Medicine.2024; 13(7): 2011. CrossRef - A Systemic Review on Photodynamic Therapy: Emerging Technology with
Healing Process
Prachi Varshney, Yogesh Kumar, Devdhar Yadav, Amit Singh, Naga Rani Kagithala, Pramod Kumar Sharma, Omji Porwal, Neeraj Kumar Fuloria, Pradeep Kumar Sharma, Ashok Kumar Gupta, G.S.N. Koteswara Rao
Current Cancer Therapy Reviews.2024; 20(3): 283. CrossRef - Endoscopic closure techniques of bariatric surgery complications: a meta-analysis
William N. Doyle, Alexander Netzley, Rahul Mhaskar, Abdul-Rahman F. Diab, Samer Ganam, Joseph Sujka, Christopher DuCoin, Salvatore Docimo
Surgical Endoscopy.2024; 38(5): 2894. CrossRef - Digestive neo-epithelialization after endoscopic stenting for upper digestive tract complete disunion
Sohaib Ouazzani, Arnaud Lemmers, Jean-Michel Gonzalez, Jean Closset, Imad El Moussaoui, Jacques Devière, Marc Barthet
Endoscopy.2024;[Epub] CrossRef - The Efficacy and Safety of Endoscopic Balloon Dilatation in the Treatment of Functional Post-Sleeve-Gastrectomy Stenosis
Mohamed A. Elsebaey, Mohamed Elsayed Enaba, Heba Elashry, Waleed Elrefaey, Rasha Youssef Hagag, Neveen A. Shalaby, Mohamed Sabry Aboelnasr, Mohamed Elsayed Sarhan, Omneya Mohamed Darrag, Assem Mohamed Elsokkary, Mohamed Abd Allah Alabd, Ahmed Mohamed El N
Medicina.2024; 60(5): 833. CrossRef - Bariatric Surgery Emergencies in Acute Care Surgery
Kalyana C. Nandipati, Kristin C. Bremer
Surgical Clinics of North America.2023; 103(6): 1113. CrossRef - Massive enlargement of gastric pouch as a complication of gastrojejunal anastomotic stenosis following one anastomosis laparoscopic gastric bypass: A case report
A. Martel-Vilchis, V. Gallardo-Chavez, P. León-Cabral, A. Paz-Fernández, E. Luna-Martinez, M. Sierra-Salazar
International Journal of Surgery Case Reports.2023; 110: 108557. CrossRef - Unexplained recurrent left lower lobe pneumonia, haematemesis and splenomegaly in a 32‐year‐old gentleman
Cynthuja Thilakanathan, Matthew Hall, Wassim Rahman, Mark Magdy, John Jorgensen
ANZ Journal of Surgery.2022; 92(1-2): 258. CrossRef - An innovative endoscopic management strategy for postoperative fistula after laparoscopic sleeve gastrectomy
Haiming Fang, Tingting Yao, Yating Chen, Yan Lu, Kangwei Xiong, Yuan Su, Yujue Zhang, Yong Wang, Lijiu Zhang
Surgical Endoscopy.2022; 36(9): 6439. CrossRef - Stent Management of Leaks After Bariatric Surgery: a Systematic Review and Meta-analysis
Andreu Martínez Hernández, Homero Beltrán Herrera, Vicente Martínez García, Miguel Ibáñez Belenguer, Raquel Queralt Martín, Ana Karina Maiocchi Segredo, Elena Aliaga Hilario, José Manuel Laguna Sastre
Obesity Surgery.2022; 32(4): 1034. CrossRef - Status of bariatric endoscopy–what does the surgeon need to know? A review
Diogo Turiani Hourneaux de Moura, Anna Carolina Batista Dantas, Igor Braga Ribeiro, Thomas R McCarty, Flávio Roberto Takeda, Marco Aurelio Santo, Sergio Carlos Nahas, Eduardo Guimarães Hourneaux de Moura
World Journal of Gastrointestinal Surgery.2022; 14(2): 185. CrossRef - Personalized Health Care Technology in Managing Postoperative Gastrointestinal Surgery Complications: Proof of Concept Study
Yaqeen Qudah, Mohammed Abdallah, Juan S. Barajas-Gamboa, Gabriel Diaz Del Gobbo, Juan Pablo Pantoja, Ricard Corcelles, John Rodriguez, Numan Balci, Matthew Kroh
Journal of Laparoendoscopic & Advanced Surgical Techniques.2022; 32(11): 1170. CrossRef - Role of Primary Use of Mega Stents Alone and Combined with Other Endoscopic Procedures for Early Leak and Stenosis After Bariatric Surgery, Single-Institution Experience
Mohamed Hany, Mohamed Ibrahim, Ahmed Zidan, Mohamed Samir, Amr Elsherif, Mohamed Selema, Mohamed Sharaan, Mohamed Elhashash
Obesity Surgery.2021; 31(5): 2050. CrossRef - A Comprehensive Review of Endoscopic Management of Sleeve Gastrectomy Leaks
Mihajlo Gjeorgjievski, Zaid Imam, Mitchell S. Cappell, Laith H. Jamil, Michel Kahaleh
Journal of Clinical Gastroenterology.2021; 55(7): 551. CrossRef - Foregut Issues After Bariatric Surgery
Fareed Cheema, Aurora D. Pryor
Foregut: The Journal of the American Foregut Society.2021; 1(4): 386. CrossRef - Endoscopic Stents in the Management of Bariatric Complications: Our Algorithm and Outcomes
Shyam Vedantam, Jay Roberts
Obesity Surgery.2020; 30(3): 1150. CrossRef - Mini gastric bypass for the management of gastrobronchial fistula: A case report
Abdulhamid Alharbi, Mohammed Alnaami, Abdulrahman Alsayyari, Mana Almuhaideb
International Journal of Surgery Case Reports.2020; 66: 192. CrossRef - Incidence and Efficacy of Stent Placement in Leak Management After Bariatric Surgery
Arielle E. Kanters, Sarah P. Shubeck, Oliver A. Varban, Justin B. Dimick, Dana A. Telem
Annals of Surgery.2020; 271(1): 134. CrossRef - Evolving procedural options for the treatment of obesity
Talar Tatarian, Kais A. Rona, Daniel H. Shin, Daniel G. Chen, Christopher G. Ducoin, Rachel L. Moore, Vitor O. Brunaldi, Manoel Galvão-Neto, Jessica Ardila-Gatas, Salvatore Docimo, Diogo T. Hourneax de Moura, Pichamol Jirapinyo, Christopher C. Thompson, H
Current Problems in Surgery.2020; 57(4): 100742. CrossRef - Endoscopic treatment of early leaks and strictures after laparoscopic one anastomosis gastric bypass
Fadi Younis, Mati Shnell, Nathan Gluck, Subhi Abu-Abeid, Shai Eldar, Sigal Fishman
BMC Surgery.2020;[Epub] CrossRef - Endoscopic balloon dilation for treatment of sleeve gastrectomy stenosis: a systematic review and meta-analysis
Steven H. Chang, Violeta B. Popov, Christopher C. Thompson
Gastrointestinal Endoscopy.2020; 91(5): 989. CrossRef - Long-term outcomes following endoscopic stenting in the management of leaks after foregut and bariatric surgery
Varun Krishnan, Kevin Hutchings, Andrew Godwin, Jonathan T. Wong, Julio Teixeira
Surgical Endoscopy.2019; 33(8): 2691. CrossRef - A Spanish Society joint SECO and SEEDO approach to the Post-operative management of the patients undergoing surgery for obesity
R Vilallonga, JL Pereira-Cunill, S Morales-Conde, I Alarcón, I Breton, E Domínguez-Adame, JV Ferrer, A Garcia Ruiz-de-Gordejuela, A Goday, A Lecube, E Martín García-Almenta, MÁ Rubio, FJ Tinahones, PP García-Luna
Obesity Surgery.2019; 29(12): 3842. CrossRef - Endoscopic Abscess Septotomy: A Less Invasive Approach for the Treatment of Sleeve Gastrectomy Leaks
Camila B. Ortega, Alfredo D. Guerron, Dana Portenier
Journal of Laparoendoscopic & Advanced Surgical Techniques.2018; 28(7): 859. CrossRef - Management of gastric fistula complicating laparoscopic sleeve gastrectomy with biological glue in a combined percutaneous and endoscopic approach
Ahmad Assalia, Anat Ilivitzki, Amos Ofer, Alain Suissa, Elias Manassa, Iyad Khamaysi, Ahmad Mahajna
Surgery for Obesity and Related Diseases.2018; 14(8): 1093. CrossRef - A Retrospective 2-Year Follow-up of Late Complications Treated Surgically and Endoscopically After Laparoscopic Roux-en-Y Gastric Bypass (LRYGB) and Laparoscopic Sleeve Gastrectomy (LSG) for Morbid Obesity
Mervi Javanainen, Anne Penttilä, Harri Mustonen, Anne Juuti, Tom Scheinin, Marja Leivonen
Obesity Surgery.2018; 28(4): 1055. CrossRef - Acute bleeding obstruction pancreatitis after Roux-en-Y anastomosis in total gastrectomy: a single center experience
J. Weindelmayer, S. Laiti, R. La Mendola, M. Bencivenga, L. Scorsone, V. Mengardo, S. Giacopuzzi
Updates in Surgery.2018; 70(2): 301. CrossRef - Management of Bariatric Complications Using Endoscopic Stents: a Multi-Center Study
Rena C. Moon, Andre F. Teixeira, Lyz Bezerra, Helga Cristina Almeida Wahnon Alhinho, Josemberg Campos, Luiz Gustavo de Quadros, Artagnan Menezes Barbosa de Amorim, Manoel Galvao Neto, Muhammad A. Jawad
Obesity Surgery.2018; 28(12): 4034. CrossRef - Endoscopic management of surgical complications
Robert J. Bowles-Cintron, Armando Perez-Ginnari, Jose M. Martinez
Techniques in Gastrointestinal Endoscopy.2018; 20(4): 182. CrossRef - A nutrition problem solved by a two-step endoscopic removal of a non-adjustable gastric band
Christer D Johansen, Jan Norum, Bernt E Engebretsen, Uwe Agledahl
Journal of Surgical Case Reports.2018;[Epub] CrossRef - Organization of future training in bariatric gastroenterology
Timothy R Koch, Timothy R Shope, Christopher J Gostout
World Journal of Gastroenterology.2017; 23(35): 6371. CrossRef
- Advanced endolumenal management of acute and chronic leaks after bariatric surgery
- 10,362 View
- 329 Download
- 31 Web of Science
- 33 Crossref

- Endoscopic Management of Gastroesophageal Reflux Disease: Revisited
- Zaheer Nabi, D. Nageshwar Reddy
- Clin Endosc 2016;49(5):408-416. Published online September 30, 2016
- DOI: https://doi.org/10.5946/ce.2016.133
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Gastroesophageal reflux disease (GERD) is defined by the presence of troublesome symptoms resulting from the reflux of gastric contents. The prevalence of GERD is increasing globally. An incompetent lower esophageal sphincter underlies the pathogenesis of GERD. Proton pump inhibitors (PPIs) form the core of GERD management. However, a substantial number of patients do not respond well to PPIs. The next option is anti-reflux surgery, which is efficacious, but it has its own limitations, such as gas bloating, inability to belch or vomit, and dysphagia. Laparoscopic placement of magnetic augmentation device is emerging as a useful alternative to conventional anti-reflux surgery. However, invasiveness of a surgical procedure remains a concern for the patients. The proportion of PPI non-responders or partial responders who do not wish for anti-reflux surgery defines the ‘treatment gap’ and needs to be addressed. The last decade has witnessed the fall and rise of many endoscopic devices for GERD. Major endoscopic strategies include radiofrequency ablation and endoscopic fundoplication devices. Current endoscopic devices score high on subjective improvement, but have been unimpressive in objective improvement like esophageal acid exposure. In this review, we discuss the current endoscopic anti-reflux therapies and available evidence for their role in the management of GERD.
-
Citations
Citations to this article as recorded by- Frontiers in Endoscopic Treatment for Gastroesophageal Reflux Disease
Kazuhiro Ota, Toshihisa Takeuchi, Kazuhide Higuchi, Shun Sasaki, Yosuke Mori, Hironori Tanaka, Akitoshi Hakoda, Noriaki Sugawara, Taro Iwatsubo, Hiroki Nishikawa
Digestion.2024; 105(1): 5. CrossRef - Refractory Gastroesophageal Reflux Disease: Diagnosis and Management
Trevor A Davis, C Prakash Gyawali
Journal of Neurogastroenterology and Motility.2024; 30(1): 17. CrossRef - Short-term results of laparoscopic anti-reflux surgery with the RefluxStop device in patients with gastro-esophageal reflux disease and ineffective esophageal motility
Yannick Fringeli, Ioannis Linas, Ulf Kessler, Joerg Zehetner
Langenbeck's Archives of Surgery.2024;[Epub] CrossRef - Management of Gastroesophageal Reflux Disease after Sleeve Gastrectomy: Effectiveness of Medical, Endoscopic, and Surgical Therapies
Diana I. Rapolti, Manuela Monrabal Lezama, Emiliano G. Manueli Laos, Francisco Schlottmann, Mario A. Masrur
Journal of Laparoendoscopic & Advanced Surgical Techniques.2024;[Epub] CrossRef - Therapeutic endoscopy: Recent updates and future directions
Zaheer Nabi, D. Nageshwar Reddy
Digestive and Liver Disease.2024;[Epub] CrossRef - Antitussive efficacy of the current treatment protocol for refractory chronic cough: our real-world experience in a retrospective cohort study
Mengru Zhang, Alyn H. Morice, Fengli Si, Li Zhang, Qiang Chen, Shengyuan Wang, Yiqing Zhu, Xianghuai Xu, Li Yu, Zhongmin Qiu
Therapeutic Advances in Respiratory Disease.2023; 17: 175346662311677. CrossRef - Endoscopic management of gastroesophageal reflux disease: Panacea for proton pump inhibitors dependent/refractory patients
Rakesh Kalapala, Neeraj Singla, Duvvur Nageshwar Reddy
Digestive Endoscopy.2022; 34(4): 687. CrossRef - The role of endoscopy in the management of gastroesophageal reflux disease
Shiko Kuribayashi, Hiroko Hosaka, Fumihiko Nakamura, Ko Nakata, Keigo Sato, Yuki Itoi, Yu Hashimoto, Kengo Kasuga, Hirohito Tanaka, Toshio Uraoka
DEN Open.2022;[Epub] CrossRef - Objective Outcomes of an Extended Anti-reflux Mucosectomy in the Treatment of PPI-Dependent Gastroesophageal Reflux Disease (with Video)
Jian He, Yani Yin, Wen Tang, Jiahui Jiang, Lei Gu, Jun Yi, Lu Yan, Shuijiao Chen, Yu Wu, Xiaowei Liu
Journal of Gastrointestinal Surgery.2022; 26(8): 1566. CrossRef - How much ARMS twisting is needed to treat GERD?
Sridhar Sundaram
Digestive Endoscopy.2021; 33(3): 464. CrossRef - Anti-reflux mucosectomy (ARMS) results in improved recovery and similar reflux quality of life outcomes compared to laparoscopic Nissen fundoplication
Harry J Wong, Bailey Su, Mikhail Attaar, Kristine Kuchta, Stephen Stearns, John G Linn, Stephen P Haggerty, Woody Denham, Michael B Ujiki
Surgical Endoscopy.2021; 35(12): 7174. CrossRef - Endoscopic Anti-Reflux Procedures: Ready for Clinical Use?
Fahmi Shibli, Ronnie Fass
Current Treatment Options in Gastroenterology.2021; 19(3): 399. CrossRef - Utilizing multimodal imaging to visualize potential mechanism for sudden death in epilepsy
Ranajay Mandal, Ryan Budde, Georgia L. Lawlor, Pedro Irazoqui
Epilepsy & Behavior.2021; 122: 108124. CrossRef - The Usefulness of the Measurement of Esophagogastric Junction Distensibility by EndoFLIP in the Diagnosis of Gastroesophageal Reflux Disease
Jung Min Lee, In Kyung Yoo, Eunju Kim, Sung Pyo Hong, Joo Young Cho
Gut and Liver.2021; 15(4): 546. CrossRef - Advanced Endoscopic Imaging and Interventions in GERD: An Update and Future Directions
Rupinder Mann, Mahesh Gajendran, Abhilash Perisetti, Hemant Goyal, Shreyas Saligram, Chandraprakash Umapathy
Frontiers in Medicine.2021;[Epub] CrossRef - Anti-reflux mucosectomy using a cap-assisted endoscopic mucosal resection method for refractory gastroesophageal disease: a prospective feasibility study
In kyung Yoo, Weon Jin Ko, Hak Su Kim, Hee Kyung Kim, Jung Hyun Kim, Won Hee Kim, Sung Pyo Hong, Abdullah Özgür Yeniova, Joo Young Cho
Surgical Endoscopy.2020; 34(3): 1124. CrossRef - A potential simple endoscopic antireflux method, “the Ripple Procedure” to reduce distensibility at the esophagogastric junction in a porcine model
Hyunsoo Chung, Se Hoon Kim, Sung Kwan Shin
Surgical Endoscopy.2020; 34(11): 5017. CrossRef - 7RECENT Advances in Endoscopic Treatments for Gastroesophageal Reflux Disease
Farhan Quader, C. Prakash Gyawali
Current Treatment Options in Gastroenterology.2020; 18(3): 504. CrossRef - Reflux Hypersensitivity: How to Approach Diagnosis and Management
Pankaj Aggarwal, Afrin N. Kamal
Current Gastroenterology Reports.2020;[Epub] CrossRef - Clinical feasibility of a new antireflux ablation therapy on gastroesophageal reflux disease (with video)
Oscar Víctor Hernández Mondragón, Raúl Antonio Zamarripa Mottú, Luís Fernando García Contreras, Raul Alberto Gutiérrez Aguilar, Omar Michel Solórzano Pineda, Gerardo Blanco Velasco, Enrique Murcio Perez
Gastrointestinal Endoscopy.2020; 92(6): 1190. CrossRef - Rethinking gastroesophageal reflux disorder
Samuel P. Banting, Henry E. Badgery, Matthew Read, Hiroshi Mashimo
Annals of the New York Academy of Sciences.2020; 1482(1): 177. CrossRef - Refractory regurgitation responds to magnetic sphincter augmentation but not to increased proton pump inhibitor dose
Kenneth R. DeVault
Gastrointestinal Endoscopy.2019; 89(1): 23. CrossRef - Per-oral endoscopic myotomy and gastroesophageal reflux: Where do we stand after a decade of “POETRY”?
Zaheer Nabi, Mohan Ramchandani, D. Nageshwar Reddy
Indian Journal of Gastroenterology.2019; 38(4): 287. CrossRef - Editor’s Pick: Refractory Gastroesophageal Reflux Disease: Pathophysiology, Diagnosis, and Management
Zaheer Nabi, Arun Karyampudi, D. Nageshwar Reddy
EMJ Gastroenterology.2019; : 62. CrossRef - Comparing the Effect of Psyllium Seed on Gastroesophageal Reflux Disease With Oral Omeprazole in Patients With Functional Constipation
Mousalreza Hosseini, Roshanak Salari, Mina Akbari Rad, Maryam Salehi, Batul Birjandi, Masoumeh Salari
Journal of Evidence-Based Integrative Medicine.2018; 23: 2515690X1876329. CrossRef - Evaluating an effectiveness of surgical treatment of gastroesophageal reflux disease combined with hiatal hernia
V. V. Mozharovskiy, A. A. Tsyganov, K. V. Mozharovskiy, A. A. Tarasov
Khirurgiya. Zhurnal im. N.I. Pirogova.2017; (6): 28. CrossRef
- Frontiers in Endoscopic Treatment for Gastroesophageal Reflux Disease
- 19,315 View
- 590 Download
- 27 Web of Science
- 26 Crossref

- Current Techniques for Treating Gastrointestinal Stromal Tumors in the Upper Gastrointestinal Tract
- Weon Jin Ko, Joo Young Cho
- Clin Endosc 2016;49(3):226-228. Published online May 23, 2016
- DOI: https://doi.org/10.5946/ce.2016.061
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Most gastrointestinal stromal tumors (GISTs) arise from the proper muscle layer of the upper gastrointestinal (GI) tract and have a low malignant potential. They are sometimes accompanied by symptoms, but in most cases are detected by chance. Endoscopic surgery of subepithelial tumors in the upper GI tract has been actively performed, and its merits include the need for fewer medical devices compared with other surgical procedures and post-resection organ preservation. However, because endoscopic procedures are still limited to small or pilot studies, a multidisciplinary approach combining laparoscopy and endoscopy is needed for more effective and pathologically acceptable management of GISTs. Many new endoscopic surgeries have been developed, and this review describes the current status of and the new approaches for endoscopic surgery of GISTs in the upper GI tract.
-
Citations
Citations to this article as recorded by- Endoscopic resection of gastric gastrointestinal stromal tumor using clip-and-cut endoscopic full-thickness resection: a single-center, retrospective cohort in Korea
Yuri Kim, Ji Yong Ahn, Hwoon-Yong Jung, Seokin Kang, Ho June Song, Kee Don Choi, Do Hoon Kim, Jeong Hoon Lee, Hee Kyong Na, Young Soo Park
Clinical Endoscopy.2024; 57(3): 350. CrossRef - New data on the types of sulfide copper-nickel ores of the Kharaelakh trough and the main patterns of their distribution
I. O. Krylov, I. I. Nikulin
Moscow University Bulletin. Series 4. Geology.2023; (3): 98. CrossRef - Advances in endoscopic resection techniques of small gastric tumors originating from the muscularis propria
Suliman Khan, Xiaona Cui, Safyan Nasir, Shoaib Mohammad Rafiq, Bo Qin, Qian Bai
Frontiers in Oncology.2022;[Epub] CrossRef - New data on the composition of plagioclase on the western flank of the Oktyabrsky deposit according to infrared spectroscopy
I. O. Krylov, I. I. Nikulin, A. A. Samsonov, D. M. Korshunov, D. I. Vildanov
Moscow University Bulletin. Series 4. Geology.2022; (2): 27. CrossRef - A modified endoscopic full thickness resection for gastric subepithelial tumors from muscularis propria layer: Novel method
Jung Min Lee, In Kyung Yoo, Sung Pyo Hong, Joo Young Cho, Young Kwan Cho
Journal of Gastroenterology and Hepatology.2021; 36(9): 2558. CrossRef - Endoskopische Vollwandresektion im oberen Gastrointestinaltrakt – erste Erfahrungen
T. Heuer, C. D. Gerharz, M. Banysch, G. M. Kaiser, M. Hornstein, E. Kasim
Der Gastroenterologe.2020; 15(5): 403. CrossRef - Endoscopic full‐thickness resection for gastrointestinal submucosal tumors
Ming‐Yan Cai, Francisco Martin Carreras‐Presas, Ping‐Hong Zhou
Digestive Endoscopy.2018; 30(S1): 17. CrossRef - The fourth space surgery: endoscopic subserosal dissection for upper gastrointestinal subepithelial tumors originating from the muscularis propria layer
Fei Liu, Song Zhang, Wei Ren, Tian Yang, Ying Lv, Tingsheng Ling, Xiaoping Zou, Lei Wang
Surgical Endoscopy.2018; 32(5): 2575. CrossRef - Tumor rupture of gastric gastrointestinal stromal tumors during endoscopic resection: a risk factor for peritoneal metastasis?
Shiyi Song, Wei Ren, Yi Wang, Shu Zhang, Song Zhang, Fei Liu, Qiang Cai, Guifang Xu, Xiaoping Zou, Lei Wang
Endoscopy International Open.2018; 06(08): E950. CrossRef
- Endoscopic resection of gastric gastrointestinal stromal tumor using clip-and-cut endoscopic full-thickness resection: a single-center, retrospective cohort in Korea
- 6,426 View
- 108 Download
- 10 Web of Science
- 9 Crossref

- Hybrid Natural Orifice Transluminal Endoscopic Surgery with Sentinel Lymph Node Navigation for Deep Early Gastric Cancer in the Fundic Region
- Yoon Suk Park, Seong Hwan Kim, Hee Yun Ryu, Young Kwan Cho, Yun Ju Jo, Tae il Son, Young Ok Hong
- Clin Endosc 2016;49(3):298-302. Published online March 29, 2016
- DOI: https://doi.org/10.5946/ce.2015.114
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - For patients refusing surgical treatment for deep early gastric cancer, hybrid natural orifice transluminal endoscopic surgery with sentinel lymph node navigation is a potential treatment option, particularly when the anatomic location of the cancer has low probability of lymph node metastasis. We report a case of deep early gastric cancer of the fundus beyond the endoscopic submucosal dissection indication that was treated by hybrid natural orifice transluminal endoscopic surgery with sentinel lymph node navigation. In a conventional approach, a total gastrectomy would have been needed; however, the patient refused surgical intervention. In this case, since the patient showed no positivity of the sentinel lymph node on intraoperative navigation, laparoscopic basin lymph node dissection was not performed. Hybrid natural orifice transluminal endoscopic surgery might be considered for specific regions such as the safety zone where lymph node metastases are less likely to occur.
-
Citations
Citations to this article as recorded by- Endoscopic trans-esophageal submucosal tunneling surgery: A new therapeutic approach for diseases located around the aorta ventralis
Ying Xiong, Qian-Qian Chen, Ning-Li Chai, Shun-Chang Jiao, En-Qiang Ling Hu
World Journal of Gastroenterology.2019; 25(1): 85. CrossRef - Hysterectomy and salpingo-oophorectomy by transvaginal natural orifice transluminal endoscopic surgery (V-NOTES) assisted by an umbilical camera: Case report and new hybrid technique in gynecology
Hasan Terzi, Unal Turkay, Navdar Dogus Uzun, Mehmet Salıcı
International Journal of Surgery Case Reports.2018; 51: 349. CrossRef - Current Status of Endoscopic Resection of Early Gastric Cancer in Korea
Hwoon-Yong Jung
The Korean Journal of Gastroenterology.2017; 70(3): 121. CrossRef
- Endoscopic trans-esophageal submucosal tunneling surgery: A new therapeutic approach for diseases located around the aorta ventralis
- 6,801 View
- 92 Download
- 3 Web of Science
- 3 Crossref

- Optimal Methods for the Management of Iatrogenic Colonoscopic Perforation
- Dae Kyu Shin, Sun Young Shin, Chi Young Park, Sun Mi Jin, Yang Hyun Cho, Won Hee Kim, Chang-Il Kwon, Kwang Hyun Ko, Ki Baik Hahm, Pil Won Park, Jong Woo Kim, Sung Pyo Hong
- Clin Endosc 2016;49(3):282-288. Published online February 18, 2016
- DOI: https://doi.org/10.5946/ce.2015.046
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Colonoscopic perforations have been managed with exploratory laparotomy, and have resulted in some morbidity and mortality. Recently, laparoscopic surgery is commonly performed for this purpose. The aim of this study was to compare the outcomes of several management strategies for iatrogenic colonoscopic perforations.
Methods
We retrospectively reviewed the medical records of patients who had been treated for colonoscopic perforation between January 2004 and April 2013 at CHA Bundang Medical Center in Korea.
Results
A total of 41 patients with colonoscopic perforation were enrolled. Twenty patients underwent conservative management with a success rate of 90%. Surgical management was performed in 23 patients including two patients who were converted to surgical management after the failure of the initial conservative management. Among 14 patients who underwent surgery at 8 hours after the perforation, there was no considerable difference in adverse outcomes between the laparotomy group and the laparoscopic surgery group. The medical costs and claim rate were 1.45 and 1.87 times greater in the exploratory laparotomy group, respectively.
Conclusions
Conservative management of colonoscopic perforation could be an option for patients without overt symptoms of peritonitis or with a small defect size. If surgical management is required, laparoscopic surgery may be considered as the initial procedure even with a delayed diagnosis. -
Citations
Citations to this article as recorded by- Surgical repair of endoscopy-induced colonic perforations: a case-matched study of short-term morbidity and mortality
Fady DANIEL, Suha JABAK, Mohammad HOSNI, Hani TAMIM, Aurelie MAILHAC, Ayman ALRAZIM, Noura AL-ALI, Robert CHURCH, Mohammad KHALIFE, Shafik SIDANI, Faek JAMALI
Minerva Surgery.2024;[Epub] CrossRef - Laparoscopic versus open surgery for colonoscopic perforation: A systematic review and meta-analysis
Wu Zhong, Chuanyuan Liu, Chuanfa Fang, Lei Zhang, Xianping He, Weiquan Zhu, Xueyun Guan
Medicine.2023; 102(24): e34057. CrossRef - Elastography for Pediatric Chronic Liver Disease
Giovanna Ferraioli, Richard G. Barr, Jonathan R. Dillman
Journal of Ultrasound in Medicine.2021; 40(5): 909. CrossRef - Clinical outcomes of laparoscopic versus open surgery for repairing colonoscopic perforation: a multicenter study
Jae Seok Lee, Jeong Yeon Kim, Byung Mo Kang, Sang Nam Yoon, Jun Ho Park, Bo Young Oh, Jong Wan Kim
Surgery Today.2021; 51(2): 285. CrossRef - The analysis of outcomes of surgical management for colonoscopic perforations: A 16-years experiences at a single institution
Dae Ro Lim, Jung Kul Kuk, Taehyung Kim, Eung Jin Shin
Asian Journal of Surgery.2020; 43(5): 577. CrossRef - Multicenter retrospective evaluation of ileocecocolic perforations associated with diagnostic lower gastrointestinal endoscopy in dogs and cats
Vanessa L. Woolhead, Jacqueline C. Whittemore, Sarah A. Stewart
Journal of Veterinary Internal Medicine.2020; 34(2): 684. CrossRef - Endoscopic Management of the Ascending Colon Perforation Secondary to a Rare-Earth Magnets Ingestion in a Pediatric Patient
Sandra Mabel Camacho-Gomez, James Meredith Noel, Robert Adam Noel
ACG Case Reports Journal.2020; 7(8): e00436. CrossRef - Pseudo‐obstruction But a Real Perforation
AORN Journal.2019; 109(1): 142. CrossRef - Treatment of colonoscopic perforation: outcomes from a major single tertiary institution
Carolyn R. Chew, Justin M. C. Yeung, Ian G. Faragher
ANZ Journal of Surgery.2019; 89(5): 546. CrossRef - Management of colonoscopic perforations: A systematic review
Alexander T. Hawkins, Kenneth W. Sharp, Molly M. Ford, Roberta L. Muldoon, M. Benjamin Hopkins, Timothy M. Geiger
The American Journal of Surgery.2018; 215(4): 712. CrossRef - 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation
Nicola de’Angelis, Salomone Di Saverio, Osvaldo Chiara, Massimo Sartelli, Aleix Martínez-Pérez, Franca Patrizi, Dieter G. Weber, Luca Ansaloni, Walter Biffl, Offir Ben-Ishay, Miklosh Bala, Francesco Brunetti, Federica Gaiani, Solafah Abdalla, Aurelien Ami
World Journal of Emergency Surgery.2018;[Epub] CrossRef - Management Outcomes of Colonoscopic Perforations Are Affected by the General Condition of the Patients
Jae Ho Park, Kyung Jong Kim
Annals of Coloproctology.2018; 34(1): 16. CrossRef - Abdominal Sepsis: An Update
Mircea Gabriel Mureșan, Ioan Alexandru Balmoș, Iudita Badea, Ario Santini
The Journal of Critical Care Medicine.2018; 4(4): 120. CrossRef - Laparoscopic vs. open surgery for the treatment of iatrogenic colonoscopic perforations: a systematic review and meta-analysis
Aleix Martínez-Pérez, Nicola de’Angelis, Francesco Brunetti, Yann Le Baleur, Carmen Payá-Llorente, Riccardo Memeo, Federica Gaiani, Marco Manfredi, Paschalis Gavriilidis, Giorgio Nervi, Federico Coccolini, Aurelien Amiot, Iradj Sobhani, Fausto Catena, Gia
World Journal of Emergency Surgery.2017;[Epub] CrossRef - Urinary Bladder Injury During Colonoscopy Without Colon Perforation
Jung Wook Suh, Jun Won Min, Hwan Namgung, Dong-Guk Park
Annals of Coloproctology.2017; 33(3): 112. CrossRef - The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections
Massimo Sartelli, Alain Chichom-Mefire, Francesco M. Labricciosa, Timothy Hardcastle, Fikri M. Abu-Zidan, Abdulrashid K. Adesunkanmi, Luca Ansaloni, Miklosh Bala, Zsolt J. Balogh, Marcelo A. Beltrán, Offir Ben-Ishay, Walter L. Biffl, Arianna Birindelli, M
World Journal of Emergency Surgery.2017;[Epub] CrossRef - How Should We Manage Iatrogenic Perforation Caused by Colonoscopy?
Eun Sun Kim
Clinical Endoscopy.2016; 49(3): 214. CrossRef
- Surgical repair of endoscopy-induced colonic perforations: a case-matched study of short-term morbidity and mortality
- 8,245 View
- 151 Download
- 20 Web of Science
- 17 Crossref

- Asymptomatic Gastric Band Erosion Detected during Routine Gastroduodenoscopy
- Gee Young Yun, Woo Sub Kim, Hye Jin Kim, Sun Hyung Kang, Hee Seok Moon, Jae Kyu Sung, Hyun Yong Jeong
- Clin Endosc 2016;49(3):294-297. Published online February 11, 2016
- DOI: https://doi.org/10.5946/ce.2016.001
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The incidence of gastric band erosion has decreased to 1%. Gastric band erosion can manifest with various clinical symptoms, although some patients remain asymptomatic. We present a case of a mostly asymptomatic patient who was diagnosed with gastric band erosion during a routine health check-up. A 32-year-old man without any underlying diseases except for non-alcoholic fatty liver underwent laparoscopic adjustable gastric band surgery in 2010. He had no significant complications postoperatively. He underwent routine health check-ups with near-normal gastroduodenoscopic findings through 2014. However, in 2015, routine gastroduodenoscopy showed that the gastric band had eroded into the stomach. His gastric band was removed laparoscopically, and the remaining gastric ulcer perforation was repaired using an omental patch. Due to the early diagnosis, the infection was not serious. The patient was discharged on postoperative day 3 with oral antibiotics. This patient was fortunately diagnosed early by virtue of a routine health check-up, thus eliminating the possibility of serious complications.
-
Citations
Citations to this article as recorded by- Retrieval of Gastric Band Eroding Into the Stomach: A Gastrointestinal Fistula Case Managed Through a Combined Laparoscopic and Colonoscopic Approach
Ahmed Binjaloud , Ahad Alotaibi, Samar Alsubhi , Anfal Altamimi, Osamah Nafea, Zeyad Al Yousef
Cureus.2024;[Epub] CrossRef - Late-Onset Gastric Band Erosion Following Heavy Nonsteroidal Anti-inflammatory Drug Use
Zachary Makovich, Brijesh Patel
ACG Case Reports Journal.2024; 11(4): e01343. CrossRef - Management of Laparoscopic Adjustable Gastric Band Erosion: A Case Report
Taylor F Faust, Emma Schnittka, Michael B Steadman, Garrett M Cail, Bradley S Rice
Cureus.2023;[Epub] CrossRef - Complications from Laparoscopic Adjustable Gastric Banding: 364 Cases Experience
GV Ramiro
Global Journal of Obesity, Diabetes and Metabolic Syndrome.2017; 4(1): 001. CrossRef
- Retrieval of Gastric Band Eroding Into the Stomach: A Gastrointestinal Fistula Case Managed Through a Combined Laparoscopic and Colonoscopic Approach
- 7,552 View
- 56 Download
- 3 Web of Science
- 4 Crossref

- Endoscopic Electrosurgery in Patients with Cardiac Implantable Electronic Devices
- Myong Ki Baeg, Sang-Woo Kim, Sun-Hye Ko, Yoon Bum Lee, Seawon Hwang, Bong-Woo Lee, Hye Jin Choi, Jae Myung Park, In-Seok Lee, Yong-Seog Oh, Myung-Gyu Choi
- Clin Endosc 2016;49(2):176-181. Published online February 11, 2016
- DOI: https://doi.org/10.5946/ce.2015.023
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Patients with cardiac implantable electronic devices (CIEDs) undergoing endoscopic electrosurgery (EE) are at a risk of electromagnetic interference (EMI). We aimed to analyze the effects of EE in CIED patients.
Methods
Patients with CIED who underwent EE procedures such as snare polypectomy, endoscopic submucosal dissection (ESD), and endoscopic retrograde cholangiopancreatography (ERCP) with endoscopic sphincterotomy (EST) were retrospectively analyzed. Postprocedural symptoms as well as demographic and outpatient follow-up data were reviewed through medical records. Electrical data, including preprocedural and postprocedural arrhythmia records, were reviewed through pacemaker interrogation, 24-hour Holter monitoring, or electrocardiogram.
Results
Fifty-nine procedures in 49 patients were analyzed. Fifty procedures were performed in 43 patients with a pacemaker, and nine were performed in six patients with an implantable cardioverter-defibrillator. There were one gastric and 44 colon snare polypectomies, five gastric and one colon ESDs, and eight ERCPs with EST. Fifty-five cases of electrical follow-up were noted, with two postprocedural changes not caused by EE. Thirty-one pacemaker interrogations had procedure recordings, with two cases of asymptomatic tachycardia. All patients were asymptomatic with no adverse events.
Conclusions
Our study reports no adverse events from EE in patients with CIED, suggesting that this procedure is safe. However, because of the possibility of EMI, recommendations on EE should be followed. -
Citations
Citations to this article as recorded by- Electrosurgical unit in GI endoscopy: the proper settings for practice
Anuraag Jena, Shubham Jain, Sridhar Sundaram, Anupam Kumar Singh, Sanjay Chandnani, Pravin Rathi
Expert Review of Gastroenterology & Hepatology.2023; 17(8): 825. CrossRef - 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery
Sigrun Halvorsen, Julinda Mehilli, Salvatore Cassese, Trygve S Hall, Magdy Abdelhamid, Emanuele Barbato, Stefan De Hert, Ingrid de Laval, Tobias Geisler, Lynne Hinterbuchner, Borja Ibanez, Radosław Lenarczyk, Ulrich R Mansmann, Paul McGreavy, Christian Mu
European Heart Journal.2022; 43(39): 3826. CrossRef - EHRA consensus on prevention and management of interference due to medical procedures in patients with cardiac implantable electronic devices
Markus Stühlinger, Haran Burri, Kevin Vernooy, Rodrigue Garcia, Radoslaw Lenarczyk, Arian Sultan, Michael Brunner, Avi Sabbag, Emin Evren Özcan, Jorge Toquero Ramos, Giuseppe Di Stolfo, Mahmoud Suleiman, Florian Tinhofer, Julian Miguel Aristizabal, Ivan C
EP Europace.2022; 24(9): 1512. CrossRef - Electromagnetic interference on cardiac pacemakers and implantable cardioverter defibrillators during endoscopy as reported to the US Federal Drug Administration
Jason M. Samuels, Douglas M. Overbey, Krzysztof J. Wikiel, Teresa S. Jones, Thomas N. Robinson, Edward L. Jones
Surgical Endoscopy.2021; 35(7): 3796. CrossRef - SAFETY IN THE GASTROENTEROLOGY SETTING
Gastroenterology Nursing.2021; 44(6): 467. CrossRef - Practice Advisory for the Perioperative Management of Patients with Cardiac Implantable Electronic Devices: Pacemakers and Implantable Cardioverter–Defibrillators 2020
Anesthesiology.2020; 132(2): 225. CrossRef - Safety and outcomes of noncardiac surgery in patients with cardiac implantable electronic devices
Bahman Akhondi, Mohammadmostafa Ansari-Ramandi, Mona Heidarali, Farzad Kamali, Majid Haghjoo
Research in Cardiovascular Medicine.2019; 8(3): 76. CrossRef - Critical analysis of guidelines for providing sedation to patients undergoing gastrointestinal endoscopy procedures
Basavana Goudra, PreetMohinder Singh
Anesthesia: Essays and Researches.2019; 13(4): 601. CrossRef - Is It Safe to Perform Therapeutic Endoscopic Procedures in Patients with Implanted Electronic Cardiac Devices?
Eun Young Kim
Clinical Endoscopy.2016; 49(2): 104. CrossRef
- Electrosurgical unit in GI endoscopy: the proper settings for practice
- 11,367 View
- 142 Download
- 9 Web of Science
- 9 Crossref

- Novel Endoscopic Management of Obesity
- Jerome Dargent
- Clin Endosc 2016;49(1):30-36. Published online January 28, 2016
- DOI: https://doi.org/10.5946/ce.2016.49.1.30
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic procedures have been well-documented in the obesity field, but have not yet reached a sufficient level of evidence as stand-alone methods for treating obesity. It is unclear if they should take over. Although expanding, the array of bariatric surgical techniques does not fully meet the current needs, and there are not enough resources for increasing surgery. Surgery is avoided by a majority of patients, so that less aggressive procedures are necessary. For the time being, relevant endoscopic methods include intra-gastric balloons, gastric partitioning (Endo-plication), and the metabolic field (Endo-barrier). Surgical novelties and basic research are also important contributors owing to their potential combination with endoscopy. Conditions have been listed for implementation of bariatric endoscopy, because innovation is risky, expensive, and faces ethical challenges. A scientific background is being built (e.g., hormonal studies). Some techniques require additional study, while others are not ready but should be priorities. Steps and goals include the search for conceptual similarities and the respect of an ethical frame. Minimally invasive bariatric techniques are not ready for prime time, but they are already being successful as re-do procedures. A time-frame for step-strategies can be defined, and more investments from the industry are mandatory.
-
Citations
Citations to this article as recorded by- Nutritional Management and Role of Multidisciplinary Follow-Up after Endoscopic Bariatric Treatment for Obesity
Anuradha Negi, Ravishankar Asokkumar, Rajesh Ravi, Gontrand Lopez-Nava, Inmaculada Bautista-Castaño
Nutrients.2022; 14(16): 3450. CrossRef - You Can’t Have One Without the Other: Innovation and Ethical Dilemmas in Gastroenterology and Hepatology
Thomas Couri, Andrew Aronsohn
Clinical Gastroenterology and Hepatology.2021; 19(10): 2015. CrossRef - The role of silent helicobacter pylori infection in intragastric ulcers induced by balloon insertion used for management of obesity
Tamer Haydara, Ahmed M. Kabel, Ayman M. Elsaka
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 116. CrossRef - Novelties in the treatment of obesity
Pavol Holéczy
Medicína pro praxi.2019; 16(4): 259. CrossRef - Un nouveau ballon gastrique : le modèle avalable Elipse
S. Kolmer, J. Dargent
Obésité.2018; 13(1): 13. CrossRef - Commentaire sur l’éditorial de Laurent Brunaud
J. Dargent
Journal de Chirurgie Viscérale.2018; 155(1): 84. CrossRef - Managing the popularity of bariatric surgery in France, comments on the editorial by Laurent Brunaud
J. Dargent
Journal of Visceral Surgery.2018; 155(1): 87. CrossRef - Improvement of Body Composition and Quality of Life Following Intragastric Balloon
Silvia Mansur Reimão, Maria Elizabeth Rossi da Silva, Gabriel Cairo Nunes, Luiz Henrique Mazzonetto Mestieri, Rosa Ferreira dos Santos, Eduardo Guimarães Hourneaux de Moura
Obesity Surgery.2018; 28(6): 1806. CrossRef - Partie VII — La chirurgie bariatrique, sinon rien ? Fogel–Étude ICAPS (2008–2014)
J. Dargent
Obésité.2018; 13(4): 212. CrossRef - Endoscopic gastric plication for obesity: Where might it fit in the scheme of things?
David E. Cummings, Philip R. Schauer
Obesity.2017; 25(2): 284. CrossRef - Making sense of metabolic obesity and hedonic obesity
Yi‐Hao Yu
Journal of Diabetes.2017; 9(7): 656. CrossRef - Gastrointestinal Surgery and Endoscopy: Recent Trends in Competition and Collaboration
György Baffy, P. Marco Fisichella
Clinical Gastroenterology and Hepatology.2017; 15(6): 799. CrossRef - Medical devices for the treatment of obesity
Phong Ching Lee, John Dixon
Nature Reviews Gastroenterology & Hepatology.2017; 14(9): 553. CrossRef
- Nutritional Management and Role of Multidisciplinary Follow-Up after Endoscopic Bariatric Treatment for Obesity
- 8,945 View
- 130 Download
- 9 Web of Science
- 13 Crossref

- Delayed Perforation Occurring after Endoscopic Submucosal Dissection for Early Gastric Cancer
- Soo Hoon Kang, Kyungho Lee, Hyun Woo Lee, Ga Eun Park, Yun Soo Hong, Byung-Hoon Min
- Clin Endosc 2015;48(3):251-255. Published online May 29, 2015
- DOI: https://doi.org/10.5946/ce.2015.48.3.251
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Delayed perforation is a very rare complication of endoscopic submucosal dissection (ESD), with a reported incidence of 0.1% to 0.45%. Few reports exist on the clinical features and outcomes of delayed perforation after ESD, and it is unclear whether the optimal management strategy is emergency surgery or endoscopic closure with conservative treatment. Here, we report two cases of delayed perforation occurring after ESD for early gastric cancer. In both cases, lesions were located in the antrum, and tumor depths were confined to the mucosal layer. Total procedure times for ESD were 25 and 45 minutes, respectively. Because delayed perforation may be associated with excessive thermal damage and necrosis of the muscle layer, treatment with emergency surgery should be used instead of conservative management in cases of delayed perforation after ESD.
-
Citations
Citations to this article as recorded by- Delayed Perforation Occurring after Gastric Endoscopic Submucosal Dissection: Clinical Features and Management Strategy
Tae-Se Kim, Byung-Hoon Min, Yang Won Min, Hyuk Lee, Poong-Lyul Rhee, Jae J. Kim, Jun Haeng Lee
Gut and Liver.2024; 18(1): 40. CrossRef - Complications of endoscopic resection in the upper gastrointestinal tract
Takeshi Uozumi, Seiichiro Abe, Mai Ego Makiguchi, Satoru Nonaka, Haruhisa Suzuki, Shigetaka Yoshinaga, Yutaka Saito
Clinical Endoscopy.2023; 56(4): 409. CrossRef - Novel image enhancement technology that helps find bleeding points during endoscopic submucosal dissection of gastric neoplasms
Kohei Funasaka, Ryoji Miyahara, Noriyuki Horiguchi, Takafumi Omori, Hayato Osaki, Dai Yoshida, Hyuga Yamada, Keishi Koyama, Mitsuo Nagasaka, Yoshiyuki Nakagawa, Senju Hashimoto, Tomoyuki Shibata, Yoshiki Hirooka
Journal of Gastroenterology and Hepatology.2022; 37(10): 1955. CrossRef - Clinical practice guideline for endoscopic resection of early gastrointestinal cancer
Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong
Intestinal Research.2021; 19(2): 127. CrossRef - Endoscopic Resection of Gastric Cancer
Ga Hee Kim, Hwoon-Yong Jung
Gastrointestinal Endoscopy Clinics of North America.2021; 31(3): 563. CrossRef - Clinical Practice Guideline for Endoscopic Resection of Early Gastrointestinal Cancer
Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong
Clinical Endoscopy.2020; 53(2): 142. CrossRef - Clinical Practice Guideline for Endoscopic Resection of Early Gastrointestinal Cancer
Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong
The Korean Journal of Gastroenterology.2020; 75(5): 264. CrossRef - Clinical Practice Guideline for Endoscopic Resection of Early Gastrointestinal Cancer
Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2020; 20(2): 117. CrossRef - Delayed perforation occurring on the 24th day after endoscopic submucosal dissection for early gastric cancer
Satoru Homma, Kazuaki Tokodai, Minami Watanabe, Kai Takaya, Eiji Hashizume
Clinical Journal of Gastroenterology.2017; 10(2): 124. CrossRef - Clinical Factors of Delayed Perforation after Endoscopic Submucosal Dissection for Gastric Neoplasms
Yoshinobu Yamamoto, Hogara Nishisaki, Hideki Sakai, Nagahiro Tokuyama, Hiroaki Sawai, Aya Sakai, Takuya Mimura, Saeko Kushida, Hidetaka Tsumura, Takeshi Sakamoto, Ikuya Miki, Masahiro Tsuda, Hideto Inokuchi
Gastroenterology Research and Practice.2017; 2017: 1. CrossRef - Management and associated factors of delayed perforation after gastric endoscopic submucosal dissection
Haruhisa Suzuki
World Journal of Gastroenterology.2015; 21(44): 12635. CrossRef
- Delayed Perforation Occurring after Gastric Endoscopic Submucosal Dissection: Clinical Features and Management Strategy
- 8,732 View
- 103 Download
- 9 Web of Science
- 11 Crossref

- Peroral Endoscopic Myotomy: Establishing a New Program
- Nikhil A. Kumta, Shivani Mehta, Prashant Kedia, Kristen Weaver, Reem Z. Sharaiha, Norio Fukami, Hitomi Minami, Fernando Casas, Monica Gaidhane, Arnon Lambroza, Michel Kahaleh
- Clin Endosc 2014;47(5):389-397. Published online September 30, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.5.389
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Achalasia is an esophageal motility disorder characterized by incomplete relaxation of the lower esophageal sphincter (LES) and aperistalsis of the esophageal body. Treatment of achalasia is aimed at decreasing the resting pressure in the LES. Peroral endoscopic myotomy (POEM), derived from natural orifice transluminal endoscopic surgery (NOTES) and advances in endoscopic submucosal dissection (ESD), presents a novel, minimally invasive, and curative endoscopic treatment for achalasia. POEM involves an esophageal mucosal incision followed by creation of a submucosal tunnel crossing the esophagogastric junction and myotomy before closure of the mucosal incision. Although the procedure is technically demanding and requires a certain degree of skill and competency, treatment success is high (90%) with low complication rates. Since the first described POEM in humans in 2010, it has been used increasingly at centers worldwide. This article reviews available published clinical studies demonstrating POEM efficacy and safety in order to present a proposal on how to establish a dedicated POEM program and reach base proficiency for the procedure.
-
Citations
Citations to this article as recorded by- Esophageal bronchogenic cyst treated with submucosal tunneling endoscopic resection: two case reports
Hui Sha, Zong-Dan Jiang
Journal of Medical Case Reports.2024;[Epub] CrossRef - Efficacy of peroral endoscopic myotomy for the treatment of functional esophagogastric junction outflow obstruction
Madhusudhan R. Sanaka, Prabhat Kumar, Abdul Mohammed, Rajat Garg, Prashanthi N. Thota, Scott Gabbard, Yi Qin, Monisha Sudarshan, Sudish Murthy, Siva Raja
iGIE.2023; 2(4): 464. CrossRef - Per-oral Endoscopic Myotomy
Jennifer Liu-Burdowski, Rodrigo Duarte-Chavez, Michel Kahaleh
Journal of Clinical Gastroenterology.2022; 56(1): 16. CrossRef - How to Develop a Training Program for Third-Space Endoscopic Procedures in Western Countries
Tony S. Brar, Patrick L. Stoner, Dennis Yang, Peter V. Draganov
Current Treatment Options in Gastroenterology.2020; 18(2): 232. CrossRef - Establishing a submucosal endoscopy program in a gastrointestinal unit
Poornima Varma, Payal Saxena
International Journal of Gastrointestinal Intervention.2020; 9(2): 36. CrossRef - Experience with Peroral Endoscopic Myotomy for Achalasia and Spastic Esophageal Motility Disorders at a Tertiary U.S. Center
Maen Masadeh, Peter Nau, Subhash Chandra, Jagpal Klair, John Keech, Kalpaj Parekh, Rami El Abiad, Henning Gerke
Clinical Endoscopy.2020; 53(3): 321. CrossRef - POEM for Treatment of Achalasia: Our Early Experience and Technical Details of the Procedure
Pravin R. Suryawanshi, Ashok R. Mohite
Indian Journal of Surgery.2019; 81(5): 452. CrossRef - 2007–2019: a “Third”-Space Odyssey in the Endoscopic Management of Gastrointestinal Tract Diseases
Anastassios C. Manolakis, Haruhiro Inoue, Akiko Ueno, Yuto Shimamura
Current Treatment Options in Gastroenterology.2019; 17(2): 202. CrossRef - POEM in Latin America
Michel Kahaleh, Ming-ming Xu, Felipe Zamarripa, Guadalupe Martínez, Vitor N. Arantes, Fernando Casas Rodriguez, Bismarck Castillo, Iman Andalib, Amy Tyberg, Arnon Lambroza, Monica Saumoy, Juan C. Carames, Alberto Baptista, Carlos Robles-Medranda, Hanna Lu
Journal of Clinical Gastroenterology.2019; 53(8): e352. CrossRef - An Update on Current Management Strategies for Achalasia and Future Perspectives
Ioana Smith, Michel Kahaleh
Journal of Clinical Gastroenterology.2018; 52(4): 277. CrossRef - Treatment of Achalasia with Per-Oral Endoscopic Myotomy: Analysis of 50 Consecutive Patients
Erica D. Kane, David J. Desilets, Donna Wilson, Marc Leduc, Vikram Budhraja, John R. Romanelli
Journal of Laparoendoscopic & Advanced Surgical Techniques.2018; 28(5): 514. CrossRef - Per-oral endoscopic myotomy (with video)
Rahul Pannala, Barham K. Abu Dayyeh, Harry R. Aslanian, Brintha K. Enestvedt, Sri Komanduri, Michael Manfredi, John T. Maple, Udayakumar Navaneethan, Mansour A. Parsi, Zachary L. Smith, Shelby A. Sullivan, Nirav Thosani, Subhas Banerjee
Gastrointestinal Endoscopy.2016; 83(6): 1051. CrossRef - POEM, the Prototypical “New NOTES” Procedure and First Successful NOTES Procedure
Robert Bechara, Haruhiro Inoue
Gastrointestinal Endoscopy Clinics of North America.2016; 26(2): 237. CrossRef - Optical coherence tomography (OCT) prior to peroral endoscopic myotomy (POEM) reduces procedural time and bleeding: a multicenter international collaborative study
Amit P. Desai, Amy Tyberg, Prashant Kedia, Michael S. Smith, Guadalupe Martinez, Felipe Zamarripa, Yecheskel Schneider, Helga Bertani, Marzio Frazzoni, Fernando Casas, Lauren G. Khanna, Arnon Lambroza, Nikhil A. Kumta, Ali Khan, Reem Z. Sharaiha, Sanjay S
Surgical Endoscopy.2016; 30(11): 5126. CrossRef - UEG Week 2016 Poster Presentations
United European Gastroenterology Journal.2016; 4(5_suppl): A157. CrossRef - Idiopathic (primary) achalasia: a review
Dhyanesh A. Patel, Hannah P. Kim, Jerry S. Zifodya, Michael F. Vaezi
Orphanet Journal of Rare Diseases.2015;[Epub] CrossRef - Per-Oral Endoscopic Myotomy (POEM) After Previous Laparoscopic Heller Myotomy Is Feasible and Safe in a Porcine Model
Luke F. Miles, Matthew J. Frelich, Jon C. Gould, Kulwinder S. Dua, Eric S. Jensen, Andrew S. Kastenmeier
Surgical Laparoscopy, Endoscopy & Percutaneous Techniques.2015; 25(5): 408. CrossRef - Peroral endoscopic myotomy: an evolving treatment for achalasia
Robert Bechara, Haruo Ikeda, Haruhiro Inoue
Nature Reviews Gastroenterology & Hepatology.2015; 12(7): 410. CrossRef
- Esophageal bronchogenic cyst treated with submucosal tunneling endoscopic resection: two case reports
- 10,201 View
- 112 Download
- 18 Web of Science
- 18 Crossref

- Endoscopic Treatment of Pancreatic Calculi
- Yong Hoon Kim, Sung Ill Jang, Kwangwon Rhee, Dong Ki Lee
- Clin Endosc 2014;47(3):227-235. Published online May 31, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.3.227
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Chronic pancreatitis is a progressive inflammatory disease that destroys pancreatic parenchyma and alters ductal stricture, leading to ductal destruction and abdominal pain. Pancreatic duct stones (PDSs) are a common complication of chronic pancreatitis that requires treatment to relieve abdominal pain and improve pancreas function. Endoscopic therapy, extracorporeal shock wave lithotripsy (ESWL), and surgery are treatment modalities of PDSs, although lingering controversies have hindered a consensus recommendation. Many comparative studies have reported that surgery is the superior treatment because of reduced duration and frequency of hospitalization, cost, pain relief, and reintervention, while endoscopic therapy is effective and less invasive but cannot be used in all patients. Surgery is the treatment of choice when endoscopic therapy has failed, malignancy is suspected, or duodenal stricture is present. However, in patients with the appropriate indications or at high-risk for surgery, endoscopic therapy in combination with ESWL can be considered a first-line treatment. We expect that the development of advanced endoscopic techniques and equipment will expand the role of endoscopic treatment in PDS removal.
-
Citations
Citations to this article as recorded by- Pancreatic duct stones treated by Whipple as a last resort: A case report
Usra I. Ghanem, Peter R. Bael, Izzeddin Bakri, Bashar Jaber, Omar Abu-Zaydeh, Khaled N. Al-Shawa
International Journal of Surgery Case Reports.2024; 115: 109286. CrossRef - Endoscopic Retrograde Cholangiopancreatography for Management of Chronic Pancreatitis
Aliana Bofill-Garcia, Camille Lupianez-Merly
Gastrointestinal Endoscopy Clinics of North America.2024; 34(3): 449. CrossRef - Management of Pancreatic Duct Stones
Christian Gerges, Torsten Beyna, Horst Neuhaus
Gastrointestinal Endoscopy Clinics of North America.2023; 33(4): 821. CrossRef - Transpapillary Pancreatoscopy in an Emergency Hospital
L. L. Generdukayev, Yu. S. Teterin, D. A. Blagovestnov, E. S. Yeletskaya, K. A. Nugumanova, P. A. Yartsev
Russian Sklifosovsky Journal "Emergency Medical Care".2023; 12(2): 316. CrossRef - Rectal indometacin to prevent pancreatitis after extracorporeal shock wave lithotripsy (RIPEP): a single-centre, double-blind, randomised, placebo-controlled trial
Yang-Yang Qian, Nan Ru, Hui Chen, Wen-Bin Zou, Hao Wu, Jun Pan, Bo Li, Lei Xin, Ji-Yao Guo, Xin-Ying Tang, Liang-Hao Hu, Zhen-Dong Jin, Dong Wang, Yi-Qi Du, Luo-Wei Wang, Zhao-Shen Li, Zhuan Liao
The Lancet Gastroenterology & Hepatology.2022; 7(3): 238. CrossRef - ESWL pancreatitis: yet another post-procedural pancreatitis to worry about?
Lars Aabakken, Vemund Paulsen
The Lancet Gastroenterology & Hepatology.2022; 7(3): 199. CrossRef - Per-oral pancreatoscopy with intraductal lithotripsy for difficult pancreatic duct stones: a systematic review and meta-analysis
Thomas R. McCarty, Zain Sobani, Tarun Rustagi
Endoscopy International Open.2020; 08(10): E1460. CrossRef - Pancreatoscopy in endoscopic treatment of pancreatic duct stones: a systematic review
Christian Gerges, David Pullmann, Markus Schneider, Peter Siersema, Erwin van Geenen, Horst Neuhaus, Torsten Beyna
Minerva Chirurgica.2019;[Epub] CrossRef - Management Algorithm of Pancreatic Calculi
Dong Kee Jang, Jun Kyu Lee
The Korean Journal of Pancreas and Biliary Tract.2019; 24(3): 89. CrossRef - Basket impaction during the extraction of a pancreatic ductal stone
Ankit Dalal, Gaurav K. Patil, Amit P. Maydeo, Arun Iyer, Nikhil Patil
Indian Journal of Gastroenterology.2019; 38(6): 550. CrossRef - Laparoscopic pancreatic duct incision and stone removal and T-type tube drainage for pancreatic duct stone: A case report and review of literature
Yang Bai, Shi-An Yu, Li-Yuan Wang, Dao-Jun Gong
World Journal of Clinical Cases.2018; 6(13): 679. CrossRef - Endoscopic Therapies for Chronic Pancreatitis
Jeffrey M. Adler, Timothy B. Gardner
Digestive Diseases and Sciences.2017; 62(7): 1729. CrossRef - Rectally administered indomethacin to prevent post-ESWL-pancreatitis (RIPEP): study protocol for a randomized controlled trial
Yang-Yang Qian, Hui Chen, Xin-Ying Tang, Xi Jiang, Wei Qian, Wen-Bin Zou, Lei Xin, Bo Li, Yan-Fen Qi, Liang-Hao Hu, Duo-Wu Zou, Zhen-Dong Jin, Dong Wang, Yi-Qi Du, Luo-Wei Wang, Feng Liu, Zhao-Shen Li, Zhuan Liao
Trials.2017;[Epub] CrossRef - Recent Advances in Management of Chronic Pancreatitis
Seon Mee Park
The Korean Journal of Gastroenterology.2015; 66(3): 144. CrossRef
- Pancreatic duct stones treated by Whipple as a last resort: A case report
- 9,628 View
- 119 Download
- 10 Web of Science
- 14 Crossref

- Endoscopic Treatment of Various Gastrointestinal Tract Defects with an Over-the-Scope Clip: Case Series from a Tertiary Referral Hospital
- Woong Cheul Lee, Weon Jin Ko, Jun-Hyung Cho, Tae Hee Lee, Seong Ran Jeon, Hyun Gun Kim, Joo Young Cho
- Clin Endosc 2014;47(2):178-182. Published online March 31, 2014
- DOI: https://doi.org/10.5946/ce.2014.47.2.178
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub Recently, increasingly invasive therapeutic endoscopic procedures and more complex gastrointestinal surgeries such as endoscopic mucosal resection, endoscopic submucosal dissection, and novel laparoscopic approaches have resulted in endoscopists being confronted more frequently with perforations, fistulas, and anastomotic leakages, for which nonsurgical closure is desired. In this article, we present our experiences with the use of over-the-scope clip (OTSC) for natural orifice transluminal endoscopic surgery (NOTES) closure, prevention of perforation, anastomotic leakages, and fistula closures. The OTSC is a valuable device for closing intestinal perforations and fistulas, for NOTES closure, and for the prevention of perforation after the excision of a tumor from the proper muscle layer. Furthermore, it seems to be quite safe to perform, even by endoscopists with little experience of the technique.
-
Citations
Citations to this article as recorded by- Experimental Evaluation of the Optimal Suture Pattern With a Flexible Endoscopic Suturing System
Peter Halvax, Michele Diana, Yoshihiro Nagao, Jacques Marescaux, Lee Swanström
Surgical Innovation.2017; 24(3): 201. CrossRef - Management of non-acute gastrointestinal defects using the over-the-scope clips (OTSCs): a retrospective single-institution experience
Joshua S. Winder, Afif N. Kulaylat, Jane R. Schubart, Hassan M. Hal, Eric M. Pauli
Surgical Endoscopy.2016; 30(6): 2251. CrossRef - Early endoscopic closure of colocutaneous fistula adjacent to unmatured low colorectal anastomosis with the Over-The-Scope Clip (OTSC)
Constantinos Avgoustou, K. Paraskeva
Hellenic Journal of Surgery.2016; 88(3): 193. CrossRef - Endoscopic Closure for Full-Thickness Gastrointestinal Defects: Available Applications and Emerging Innovations
Nobuyoshi Takeshita, Khek Yu Ho
Clinical Endoscopy.2016; 49(5): 438. CrossRef
- Experimental Evaluation of the Optimal Suture Pattern With a Flexible Endoscopic Suturing System
- 6,117 View
- 58 Download
- 3 Web of Science
- 4 Crossref

- Endoscopic Management of Refractory Benign Colorectal Strictures
- Yong Hwan Kwon, Seong Woo Jeon, Yong Kook Lee
- Clin Endosc 2013;46(5):472-475. Published online September 30, 2013
- DOI: https://doi.org/10.5946/ce.2013.46.5.472
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub In colonoscopic study, benign colorectal strictures with or without symptomatic pain are not rarely encountered. Benign colorectal stricture can be caused by a number of problems, such as anastomotic stricture after surgery, inflammatory bowel disease, postendoscopic submucosal dissection, diverticular disease, ischemic colitis, and so on. There are various modalities for the management of benign colorectal stricture. Endoscopic balloon dilatation is generally considered as the primary treatment for benign colorectal stricture. In refractory benign colorectal strictures, several treatment sessions of balloon dilatation are needed for successful dilatation. The self-expandable metal stent and many combined techniques are performed at present. However, there is no specific algorithmic modality for refractory benign colorectal strictures.
-
Citations
Citations to this article as recorded by- Endoscopic removal of lumen-apposing metal stents – risk factors for stent embedment, complex removals, and adverse events: analysis from a multicenter prospective case series
Sergio Bazaga, Francisco Javier García-Alonso, Jose Ramon Aparicio Tormo, Belen Martinez Moreno, Vicente Sanchiz, Carles Suria, Albert Garcia-Sumalla, Joan B. Gornals, Carlos Chavarría, Carme Loras, Francisco Jose García-Fernandez, Álvaro Terán, Enrique V
Endoscopy.2023; 55(07): 591. CrossRef - Comparison of the Efficacy of Endoscopic Radial Incision and Cutting Procedure and Endoscopic Balloon Dilation for Benign Anastomotic Stricture After Low Anterior Resection Combined With Preventive Loop Ileostomy in Rectal Cancer
Shijie Wang, Jinliang Wan, Zhiming Li, Chenyan Long, Renyi Zhang, Yaxin Luo, Zelong Han, Jun Yan
Diseases of the Colon & Rectum.2023; 66(10): 1392. CrossRef - Endoscopic Management of Luminal Strictures: Beyond Dilation
Nader D. Daoud, Hassan Ghoz, Obaie Mzaik, Himesh B. Zaver, Micah McKinney, Bhaumik Brahmbhatt, Timothy Woodward
Digestive Diseases and Sciences.2022; 67(5): 1480. CrossRef - Diagnosis and Treatment of Lack of Benign Anastomosis of Colorectal Cancer
豪原 秦
Advances in Clinical Medicine.2022; 12(05): 3770. CrossRef - State-of-the-art surgery for Crohn’s disease: Part II—colonic Crohn’s disease and associated neoplasms
Anne Macleod, Sandra L. Kavalukas, Katharina M. Scheurlen, Susan Galandiuk
Langenbeck's Archives of Surgery.2022; 407(7): 2595. CrossRef - Clinical efficacy of endoscopic dilation combined with bleomycin injection for benign anastomotic stricture after rectal surgery
Xin Miao, Li Liu, Xiang Wang, Zhining Fan, Lin Miao, Jiankun Wang
Medicine.2022; 101(33): e30036. CrossRef - Advances in Imaging of Inflammation, Fibrosis, and Cancer in the Gastrointestinal Tract
Kylene M. Harold, William M. MacCuaig, Jennifer Holter-Charkabarty, Kirsten Williams, Kaitlyn Hill, Alex X. Arreola, Malika Sekhri, Steven Carter, Jorge Gomez-Gutierrez, George Salem, Girish Mishra, Lacey R. McNally
International Journal of Molecular Sciences.2022; 23(24): 16109. CrossRef - Minimally Invasive Treatment of a Completely Obstructed Rectal Anastomosis by Using a Transanal Plasmakinetic Resectoscope: a Case Report and Review of Literature
Na Wang, Daguang Wang, Weihua Tong, Jinguo Wang
Indian Journal of Surgery.2021; 83(5): 1127. CrossRef - A Novel Approach to Dilation of Complete Colorectal Anastomotic Stricture Using Transillumination
Umair M. Nasir, Brandon Rodgers, Catherine Choi, Dayna Panchal, Qasim Salimi, Sushil Ahlawat
ACG Case Reports Journal.2020; 7(7): e00418. CrossRef - Uncovered self-expandable metal stents for the treatment of refractory benign colorectal anastomotic stricture
Ji Taek Hong, Tae Jun Kim, Sung Noh Hong, Young-Ho Kim, Dong Kyung Chang, Eun Ran Kim
Scientific Reports.2020;[Epub] CrossRef - Biodegradable stent insertion for ischaemic colorectal strictures: Tiger country
Pavan Singh Najran, Damian Mullan, Hans-Ulrich Laasch
International Journal of Gastrointestinal Intervention.2017; 6(2): 145. CrossRef - The Problem of Anastomotic Stricture After Rectosigmoid Resection in Deep Infiltrating Endometriosis
Vincent Anaf, Sashka Gocevska, Olivier Lemoine, Issam El Nakadi, Alexis Buggenhout, Marc Zalcman, Jean-Christophe Noël
Journal of Gynecologic Surgery.2016; 32(1): 35. CrossRef - Transanal anorectal stricturoplasty using the Heineke–Mikulicz principle: a novel technique
S. W. Lee, R. Niec, N. Melnitchouk, T. Samdani
Colorectal Disease.2016; 18(1): 101. CrossRef - Stents for colorectal obstruction: Past, present, and future
Eui Joo Kim
World Journal of Gastroenterology.2016; 22(2): 842. CrossRef - Intestinal Stricture in Crohn's Disease
Chen-Wang Chang, Jau-Min Wong, Chien-Chih Tung, I-Lun Shih, Horng-Yuan Wang, Shu-Chen Wei
Intestinal Research.2015; 13(1): 19. CrossRef - Evaluation of the intestinal blood flow near the rectosigmoid junction using the indocyanine green fluorescence method in a colorectal cancer surgery
Jun Watanabe, Mitsuyoshi Ota, Yusuke Suwa, Shinsuke Suzuki, Hirokazu Suwa, Masasi Momiyama, Atsushi Ishibe, Kazuteru Watanabe, Hidenobu Masui, Kaoru Nagahori, Yasushi Ichikawa, Itaru Endo
International Journal of Colorectal Disease.2015; 30(3): 329. CrossRef - Endoscopic stenting for recurrence-related colorectal anastomotic site obstruction: Preliminary experience
Jung Ho Kim
World Journal of Gastroenterology.2014; 20(38): 13936. CrossRef
- Endoscopic removal of lumen-apposing metal stents – risk factors for stent embedment, complex removals, and adverse events: analysis from a multicenter prospective case series
- 6,664 View
- 109 Download
- 17 Crossref


 KSGE
KSGE


 First
First Prev
Prev



