Search
- Page Path
- HOME > Search
Original Articles
- Efficacy of hemostasis by gastroduodenal covered metal stent placement for hemorrhagic duodenal stenosis due to pancreatobiliary cancer invasion: a retrospective study
- Yasunari Sakamoto, Taku Sakamoto, Akihiro Ohba, Mitsuhito Sasaki, Shunsuke Kondo, Chigusa Morizane, Hideki Ueno, Yutaka Saito, Yasuaki Arai, Takuji Okusaka
- Received June 18, 2023 Accepted January 15, 2024 Published online June 14, 2024
- DOI: https://doi.org/10.5946/ce.2023.155 [Epub ahead of print]

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
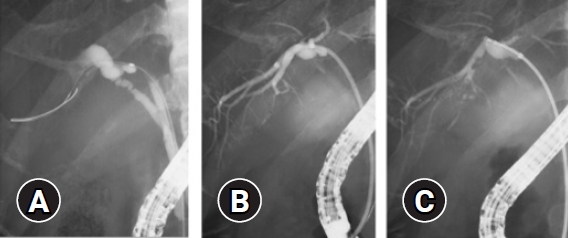
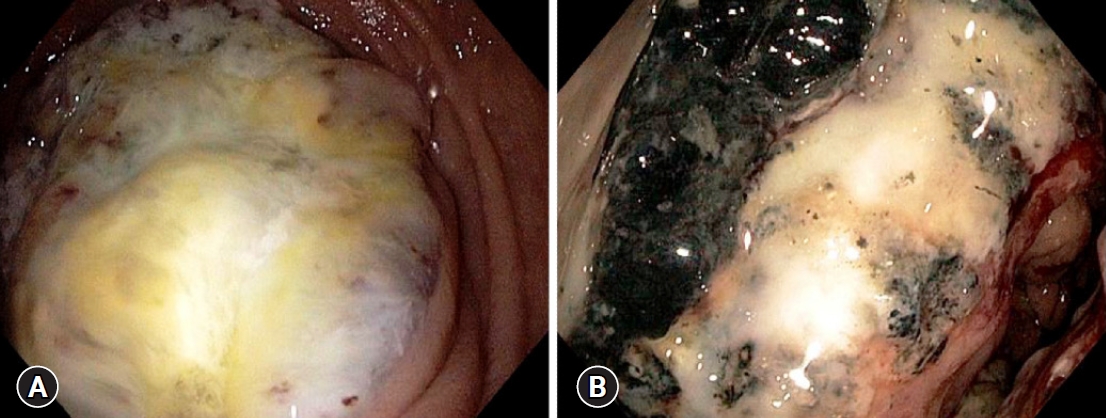
- Background
/Aims: Advanced pancreatic and biliary tract cancers can invade the duodenum and cause duodenal hemorrhagic stenosis. This study aimed to evaluate the efficacy of covered self-expandable metal stents in the treatment of cancer-related duodenal hemorrhage with stenosis.
Methods
Between January 2014 and December 2016, metal stents were placed in 51 patients with duodenal stenosis. Among these patients, a self-expandable covered metal stent was endoscopically placed in 10 patients with hemorrhagic duodenal stenosis caused by pancreatobiliary cancer progression. We retrospectively analyzed the therapeutic efficacy of the stents by evaluating the technical and clinical success rates based on successful stent placement, degree of oral intake, hemostasis, stent patency, and overall survival.
Results
The technical and clinical success rates were 100%. All 10 patients achieved a Gastric Outlet Obstruction Scoring System score of three within two weeks after the procedure and had no recurrence of melena. The median stent patency duration and overall survival after stent placement were 52 days (range, 20–220 days) and 66.5 days (range, 31–220 days), respectively.
Conclusions
Endoscopic placement of a covered metal stent for hemorrhagic duodenal stenosis associated with pancreatic or biliary tract cancer resulted in duodenal hemostasis, recanalization, and improved quality of life.
- 347 View
- 11 Download

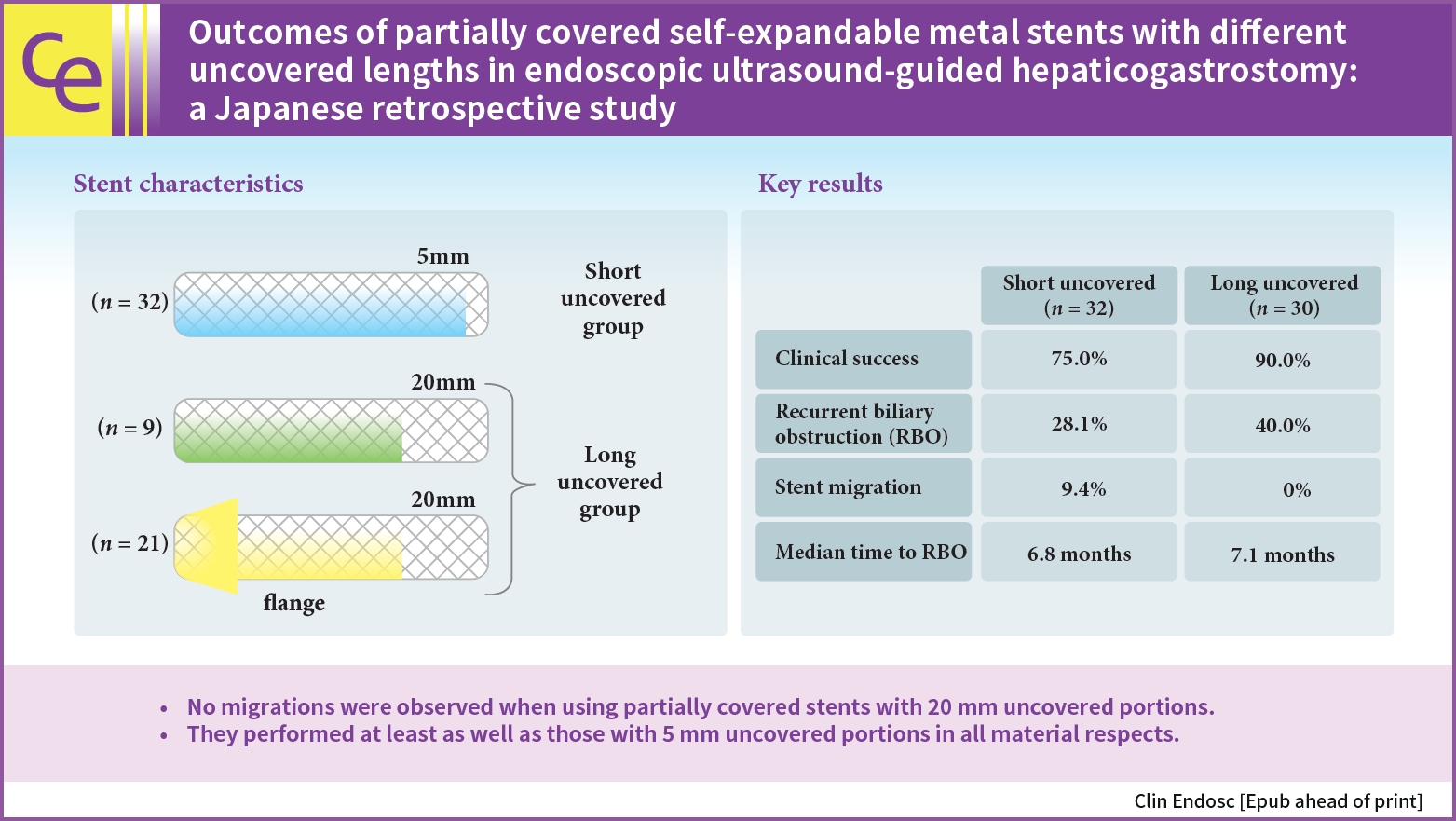
- Outcomes of partially covered self-expandable metal stents with different uncovered lengths in endoscopic ultrasound-guided hepaticogastrostomy: a Japanese retrospective study
- Takeshi Okamoto, Takashi Sasaki, Tsuyoshi Takeda, Tatsuki Hirai, Takahiro Ishitsuka, Manabu Yamada, Hiroki Nakagawa, Takafumi Mie, Takaaki Furukawa, Akiyoshi Kasuga, Masato Ozaka, Naoki Sasahira
- Received May 24, 2023 Accepted September 4, 2023 Published online May 10, 2024
- DOI: https://doi.org/10.5946/ce.2023.142 [Epub ahead of print]
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub 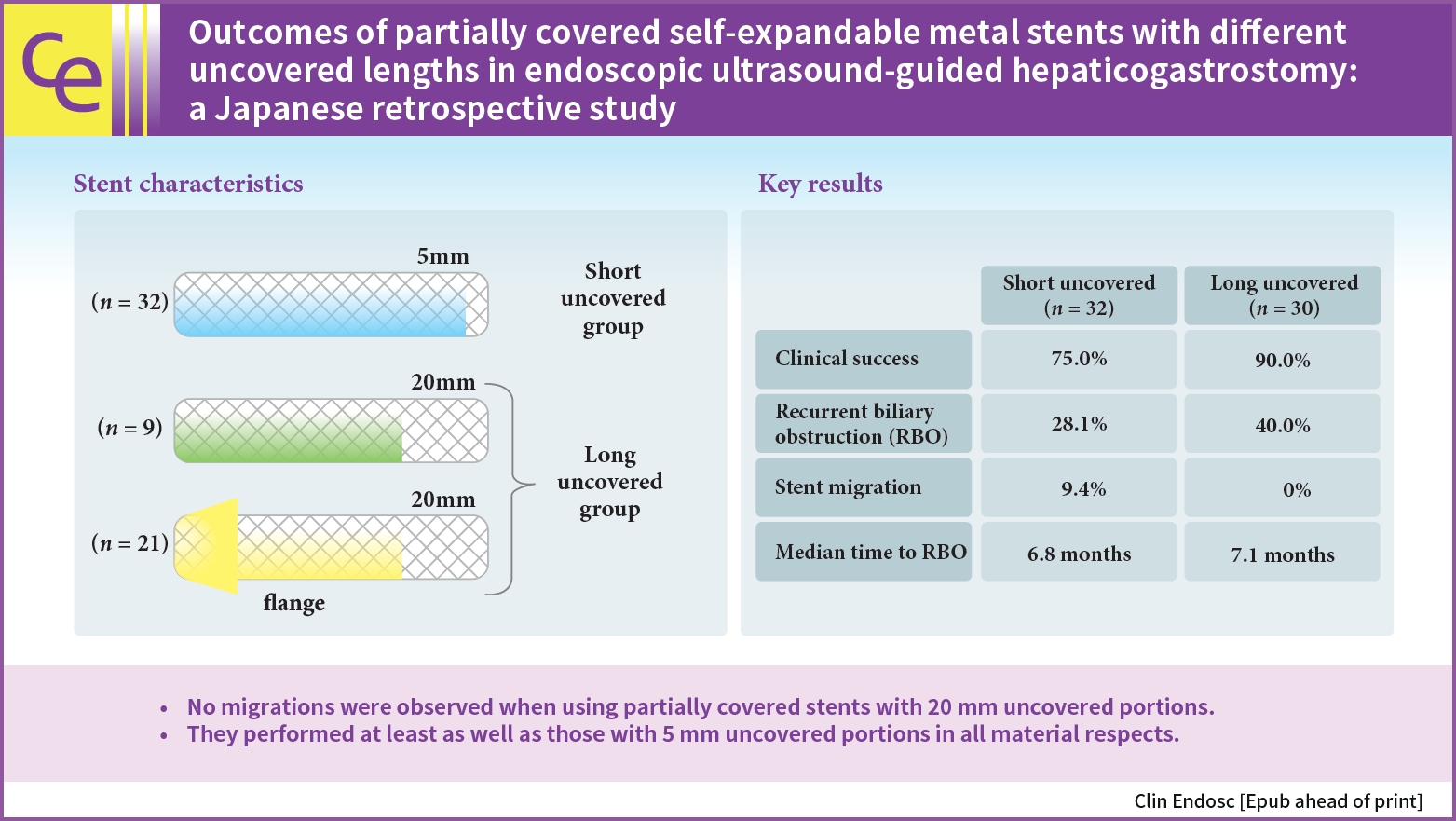
- Background
/Aims: The optimal length of the uncovered portion of partially covered self-expandable metal stents (PCSEMSs) used in endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) remains unclear. This study investigated the safety and efficacy of PCSEMSs with different uncovered lengths, with a focus on stent migration and time to recurrent biliary obstruction (RBO).
Methods
Outcomes of patients undergoing EUS-HGS using PCSEMSs with 5-mm and 20-mm uncovered portions at our institution from January 2016 to December 2021 were compared.
Results
Sixty-two patients underwent EUS-HGS using PCSEMS (5/20-mm uncovered portions: 32/30). Stent migration occurred only in the 5-mm group. There were no differences in RBO rates (28.1% vs. 40.0%) or median time to RBO (6.8 vs. 7.1 months) between the two groups. Median overall survival (OS) was longer in the 20-mm group (3.1 vs. 4.9 months, p=0.037) due to the higher number of patients that resumed chemotherapy after EUS-HGS (56.7 vs. 28.1%, p=0.029). Good performance status, absence of hepatic metastases, and chemotherapy after EUS-HGS were independent predictors of longer OS.
Conclusions
No migration was observed in patients treated with PCSEMS with 20-mm uncovered portions. Patients treated with PCSEMS with 20-mm uncovered portions performed at least as well as those treated with 5-mm uncovered portions in all material respects.
- 1,424 View
- 34 Download

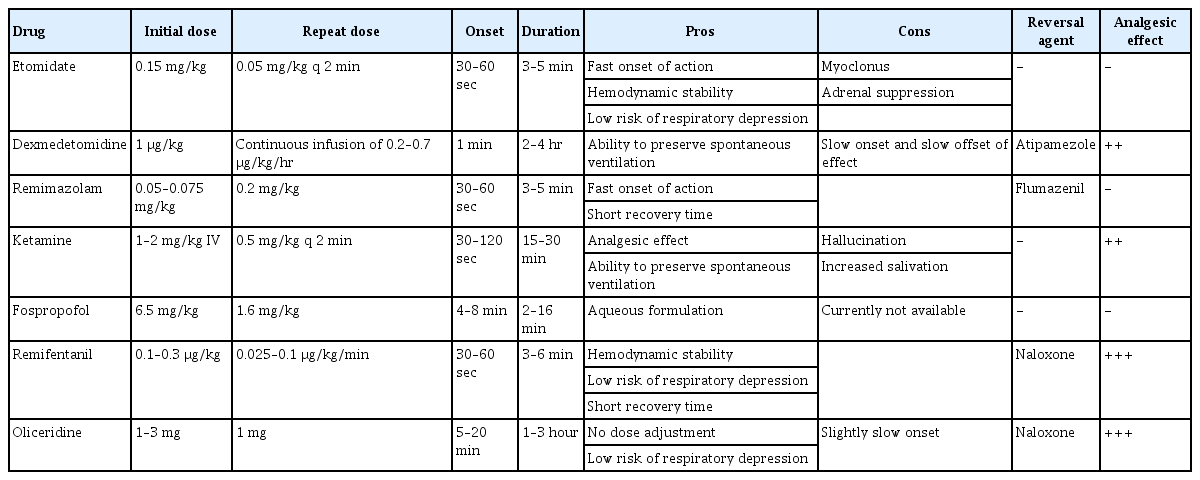
Reviews
- Clinical meaning of sarcopenia in patients undergoing endoscopic treatment
- Hiroyuki Hisada, Yosuke Tsuji, Hikaru Kuribara, Ryohei Miyata, Kaori Oshio, Satoru Mizutani, Hideki Nakagawa, Rina Cho, Nobuyuki Sakuma, Yuko Miura, Hiroya Mizutani, Daisuke Ohki, Seiichi Yakabi, Yu Takahashi, Yoshiki Sakaguchi, Naomi Kakushima, Nobutake Yamamichi, Mitsuhiro Fujishiro
- Received July 26, 2023 Accepted August 18, 2023 Published online March 22, 2024
- DOI: https://doi.org/10.5946/ce.2023.193 [Epub ahead of print]
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - With increasing global life expectancy, the significance of geriatric assessment parameters has increased. Sarcopenia is a crucial assessment parameter and is defined as the age-related loss of muscle mass and strength. Sarcopenia is widely acknowledged as a risk factor for postoperative complications in diverse advanced malignancies and has a detrimental effect on the long-term prognosis. While most studies have primarily concentrated on the correlation between sarcopenia and advanced cancer, more recent investigations have focused on the relationship between sarcopenia and early-stage cancer. Endoscopic submucosal dissection (ESD), which is less invasive than surgical intervention, is extensively employed in the management of early-stage cancer, although it is associated with complications such as bleeding and perforation. In recent years, several reports have revealed the adverse consequences of sarcopenia in patients with early-stage cancer undergoing ESD. This literature review briefly summarizes the recent studies on the association between sarcopenia and ESD.
- 2,055 View
- 42 Download

- Colon stenting as a bridge to surgery in obstructive colorectal cancer management
- Dong Hyun Kim, Han Hee Lee
- Received May 23, 2023 Accepted July 29, 2023 Published online March 8, 2024
- DOI: https://doi.org/10.5946/ce.2023.138 [Epub ahead of print]
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Colonic stent placement is a commonly used bridging strategy for surgery in patients with obstructive colorectal cancer. The procedure involves the placement of a self-expandable metallic stent (SEMS) across the obstructive lesion to restore intestinal patency and alleviate the symptoms of obstruction. By allowing patients to receive surgery in a planned and staged manner with time for preoperative optimization and bowel preparation, stent placement may reduce the need for emergency surgery, which is associated with higher complication rates and poorer outcomes. This review focuses on the role of colon stenting as a bridge to surgery in the management of obstructive colorectal cancer. SEMS as a bridge to surgery for left-sided colon cancer has been demonstrated to be particularly useful; however, further research is needed for its application in cases of right-sided colon cancer. Colon stent placement also has limitations and potential complications including stent migration, re-obstruction, and perforation. However, the timing of curative surgery after SEMS placement remains inconclusive. Considering the literature to date, performing surgery at an interval of approximately 2 weeks is considered appropriate. Therefore, colonic stent placement may be an effective strategy as a bridge to surgery in patients with obstructive colorectal cancer.
- 1,966 View
- 115 Download

- Application of artificial intelligence for diagnosis of early gastric cancer based on magnifying endoscopy with narrow-band imaging
- Yusuke Horiuchi, Toshiaki Hirasawa, Junko Fujisaki
- Clin Endosc 2024;57(1):11-17. Published online January 5, 2024
- DOI: https://doi.org/10.5946/ce.2023.173

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Although magnifying endoscopy with narrow-band imaging is the standard diagnostic test for gastric cancer, diagnosing gastric cancer using this technology requires considerable skill. Artificial intelligence has superior image recognition, and its usefulness in endoscopic image diagnosis has been reported in many cases. The diagnostic performance (accuracy, sensitivity, and specificity) of artificial intelligence using magnifying endoscopy with narrow band still images and videos for gastric cancer was higher than that of expert endoscopists, suggesting the usefulness of artificial intelligence in diagnosing gastric cancer. Histological diagnosis of gastric cancer using artificial intelligence is also promising. However, previous studies on the use of artificial intelligence to diagnose gastric cancer were small-scale; thus, large-scale studies are necessary to examine whether a high diagnostic performance can be achieved. In addition, the diagnosis of gastric cancer using artificial intelligence has not yet become widespread in clinical practice, and further research is necessary. Therefore, in the future, artificial intelligence must be further developed as an instrument, and its diagnostic performance is expected to improve with the accumulation of numerous cases nationwide.
-
Citations
Citations to this article as recorded by- Pitfalls in Endoscopic Submucosal Dissection for Early Gastric Cancer with Papillary Adenocarcinoma
Gwang Ha Kim
Gut and Liver.2024; 18(3): 368. CrossRef
- Pitfalls in Endoscopic Submucosal Dissection for Early Gastric Cancer with Papillary Adenocarcinoma
- 2,463 View
- 184 Download
- 1 Web of Science
- 1 Crossref

- Advanced endoscopic imaging for detection of Barrett’s esophagus
- Netanel Zilberstein, Michelle Godbee, Neal A. Mehta, Irving Waxman
- Clin Endosc 2024;57(1):1-10. Published online January 5, 2024
- DOI: https://doi.org/10.5946/ce.2023.031
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Barrett’s esophagus (BE) is the precursor to esophageal adenocarcinoma (EAC), and is caused by chronic gastroesophageal reflux. BE can progress over time from metaplasia to dysplasia, and eventually to EAC. EAC is associated with a poor prognosis, often due to advanced disease at the time of diagnosis. However, if BE is diagnosed early, pharmacologic and endoscopic treatments can prevent progression to EAC. The current standard of care for BE surveillance utilizes the Seattle protocol. Unfortunately, a sizable proportion of early EAC and BE-related high-grade dysplasia (HGD) are missed due to poor adherence to the Seattle protocol and sampling errors. New modalities using artificial intelligence (AI) have been proposed to improve the detection of early EAC and BE-related HGD. This review will focus on AI technology and its application to various endoscopic modalities such as high-definition white light endoscopy, narrow-band imaging, and volumetric laser endomicroscopy.
-
Citations
Citations to this article as recorded by- Advancements in Barrett's esophagus detection: The role of artificial intelligence and its implications
Sara Massironi
World Journal of Gastroenterology.2024; 30(11): 1494. CrossRef
- Advancements in Barrett's esophagus detection: The role of artificial intelligence and its implications
- 2,817 View
- 208 Download
- 1 Web of Science
- 1 Crossref

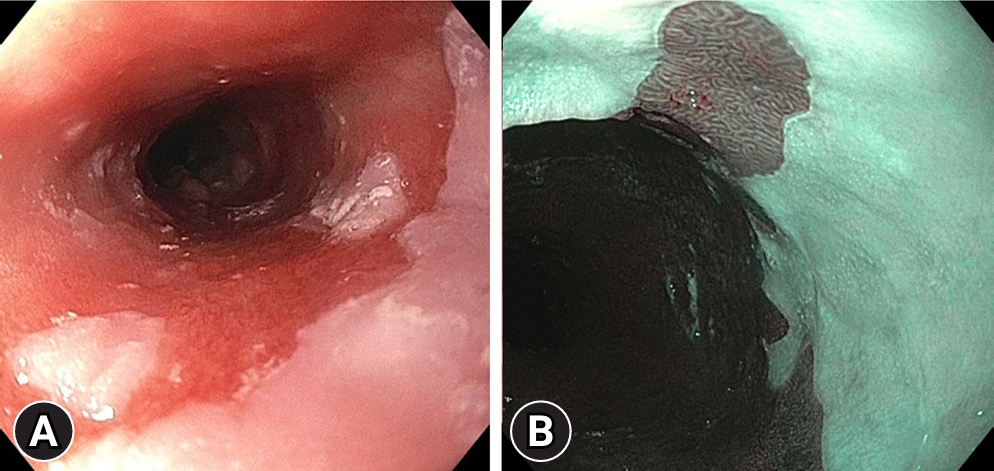
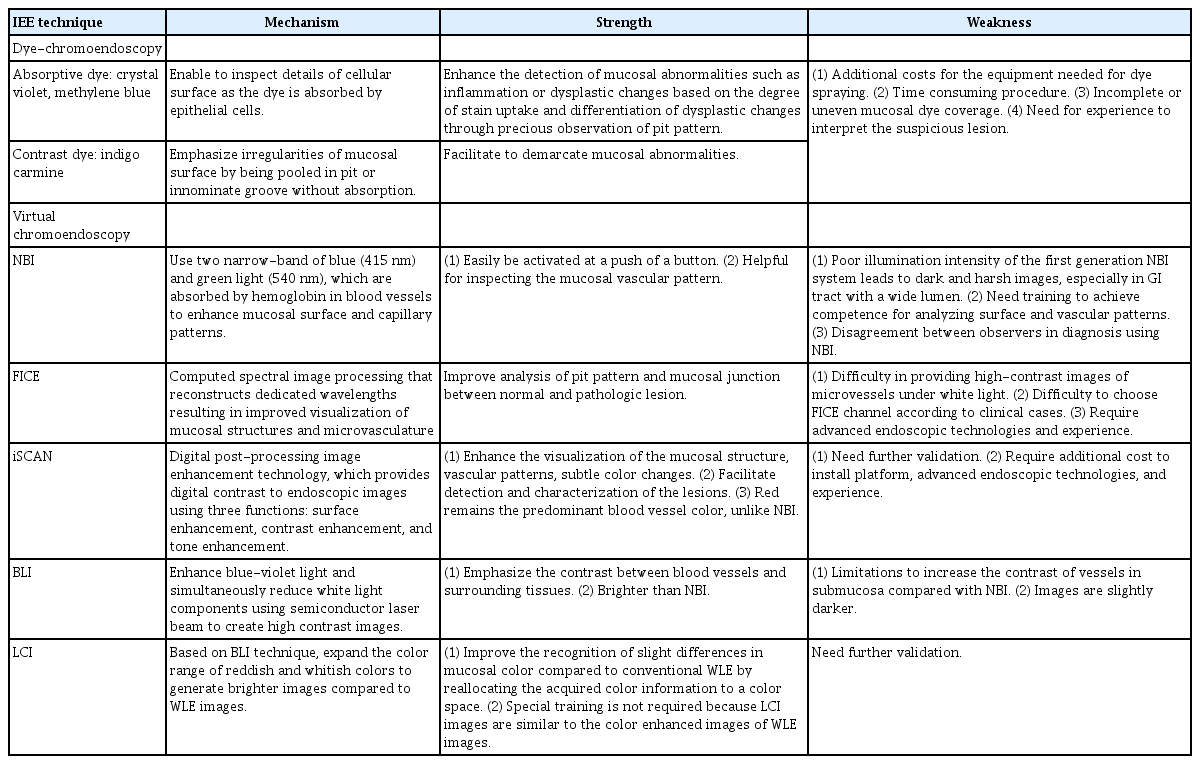
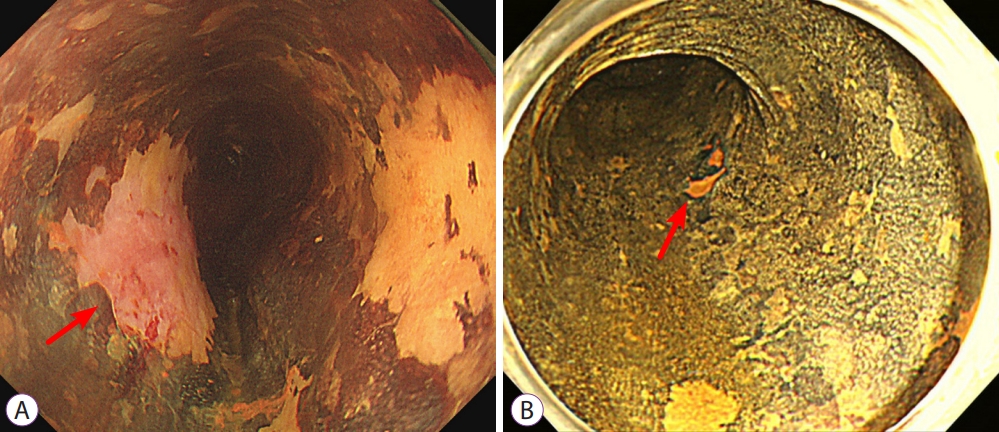
- Current status of image-enhanced endoscopy in inflammatory bowel disease
- Young Joo Yang
- Clin Endosc 2023;56(5):563-577. Published online September 26, 2023
- DOI: https://doi.org/10.5946/ce.2023.070
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - In inflammatory bowel disease (IBD), chronic inflammation leads to unfavorable clinical outcomes and increases the risk of developing colorectal neoplasm (CRN); thereby highlighting the importance of endoscopically evaluating disease activity as well as detecting and characterizing CRN in patients with IBD. With recent advances in image-enhanced endoscopic (IEE) technologies, especially virtual chromoendoscopy (VCE) platforms, this review discusses state-of-the-art IEE techniques and their applicability in assessing disease activity and surveillance colonoscopy in patients with IBD. Among various IEE, VCE demonstrated the capacity to identify quiescent disease activity. And endoscopic remission defined by the new scoring system using VCE platform better predicted clinical outcomes, which may benefit the tailoring of therapeutic strategies in patients with IBD. High-definition dye-chromoendoscopy (HD-DCE) is numerically superior to high-definition white light endoscopy (HD-WLE) in detecting CRN in IBD; however, discrepancy is observed in the statistical significance. VCE showed comparable performance in detecting dysplasia to HD-WLE or DCE and potential for optical diagnosis to differentiate neoplastic from nonneoplastic lesions during surveillance colonoscopy. Applying these novel advanced IEE technologies would provide opportunities for personalized medicine in IBD and optimal treatment of CRN in patients with IBD.
- 2,036 View
- 107 Download

- Management of complications related to colorectal endoscopic submucosal dissection
- Tae-Geun Gweon, Dong-Hoon Yang
- Clin Endosc 2023;56(4):423-432. Published online July 27, 2023
- DOI: https://doi.org/10.5946/ce.2023.104

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Compared to endoscopic mucosal resection (EMR), colonoscopic endoscopic submucosal dissection (C-ESD) has the advantages of higher en bloc resection rates and lower recurrence rates of colorectal neoplasms. Therefore, C-ESD is considered an effective treatment method for laterally spread tumors and early colorectal cancer. However, C-ESD is technically more difficult and requires a longer procedure time than EMR. In addition to therapeutic efficacy and procedural difficulty, safety concerns should always be considered when performing C-ESD in clinical practice. Bleeding and perforation are the main adverse events associated with C-ESD and can occur during C-ESD or after the completion of the procedure. Most bleeding associated with C-ESD can be managed endoscopically, even if it occurs during or after the procedure. More recently, most perforations identified during C-ESD can also be managed endoscopically, unless the mural defect is too large to be sutured with endoscopic devices or the patient is hemodynamically unstable. Delayed perforations are quite rare, but they require surgical treatment more frequently than endoscopically identified intraprocedural perforations or radiologically identified immediate postprocedural perforations. Post-ESD coagulation syndrome is a relatively underestimated adverse event, which can mimic localized peritonitis from perforation. Here, we classify and characterize the complications associated with C-ESD and recommend management options for them.
-
Citations
Citations to this article as recorded by- International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
Seung Joo Kang, Chung Hyun Tae, Chang Seok Bang, Cheol Min Shin, Young-Hoon Jeong, Miyoung Choi, Joo Ha Hwang, Yutaka Saito, Philip Wai Yan Chiu, Rungsun Rerknimitr, Christopher Khor, Vu Van Khien, Kee Don Choi, Ki-Nam Shim, Geun Am Song, Oh Young Lee
Clinical Endoscopy.2024; 57(2): 141. CrossRef - Is there a best choice of equipment for colorectal endoscopic submucosal dissection?
Francesco Cocomazzi, Sonia Carparelli, Nunzia Labarile, Antonio Capogreco, Marco Gentile, Roberta Maselli, Jahnvi Dhar, Jayanta Samanta, Alessandro Repici, Cesare Hassan, Francesco Perri, Antonio Facciorusso
Expert Review of Medical Devices.2024; : 1. CrossRef
- International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
- 1,724 View
- 130 Download
- 4 Web of Science
- 2 Crossref

- Role of linked color imaging for upper gastrointestinal disease: present and future
- Sang Pyo Lee
- Clin Endosc 2023;56(5):546-552. Published online June 9, 2023
- DOI: https://doi.org/10.5946/ce.2023.015

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Techniques for upper gastrointestinal endoscopy are advancing to facilitate lesion detection and improve prognosis. However, most early tumors in the upper gastrointestinal tract exhibit subtle color changes or morphological features that are difficult to detect using white light imaging. Linked color imaging (LCI) has been developed to overcome these shortcomings; it expands or reduces color information to clarify color differences, thereby facilitating the detection and observation of lesions. This article summarizes the characteristics of LCI and advances in LCI-related research in the upper gastrointestinal tract field.
-
Citations
Citations to this article as recorded by- Upper gastrointestinal signs and symptoms: assessment, management and referral pathways
Hasan Alsararatee
Gastrointestinal Nursing.2024; 22(4): 192. CrossRef - Endoscopic submucosal dissection for early gastric cancer: It is time to consider the quality of its outcomes
Gwang Ha Kim
World Journal of Gastroenterology.2023; 29(43): 5800. CrossRef
- Upper gastrointestinal signs and symptoms: assessment, management and referral pathways
- 2,234 View
- 195 Download
- 1 Web of Science
- 2 Crossref

Original Articles
- Management of esophageal neoplasms by endoscopic submucosal dissection: experience over 100 consecutive procedures
- Josué Aliaga Ramos, Yoshinori Morita, Takashi Toyonaga, Danilo Carvalho, Moises Salgado Pedrosa, Vitor N. Arantes
- Clin Endosc 2023;56(5):613-622. Published online May 17, 2023
- DOI: https://doi.org/10.5946/ce.2022.245

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: Endoscopic submucosal dissection (ESD) is currently considered the first-line treatment for the eradication of superficial neoplasms of the esophagus in Eastern countries. However, in the West, particularly in Latin America, the experience with esophageal ESD is still limited because of the high technical complexity required for its execution. This study aimed to present the results of the clinical application of ESD to manage superficial esophageal neoplasms in a Latin American center in over 100 consecutive cases.
Methods
This retrospective study included consecutive patients who underwent endoscopic ESD for superficial esophageal neoplasms between 2009 and 2022. The following clinical outcomes were assessed: en bloc, complete, and curative resection rates, local recurrence, adverse events, and procedure-related mortality.
Results
Esophageal ESD was performed mainly for squamous cell carcinoma (66.6%), high-grade intraepithelial neoplasia (17.1%), and adenocarcinoma (11.4%). En bloc and complete resection rates were 96.2% and 81.0%, respectively. The curative resection rate was 64.8%. Adverse events occurred in six cases (5.7%). Endoscopic follow-up was performed for an average period of 29.7 months.
Conclusions
ESD performed by trained operators is feasible, safe, and clinically effective for managing superficial neoplastic lesions of the esophagus in Latin America.
- 1,737 View
- 82 Download

- Accuracy of administrative claim data for gastric adenoma after endoscopic resection
- Ga-Yeong Shin, Hyun Ho Choi, Jae Myung Park, Sang Yoon Kim, Jun Young Park, Donghoon Kang, Yu Kyung Cho, Sung Soo Kim, Myung-Gyu Choi
- Clin Endosc 2023;56(3):325-332. Published online March 21, 2023
- DOI: https://doi.org/10.5946/ce.2022.147

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: Administrative databases provide valuable information for large-cohort studies. This study aimed to evaluate the diagnostic accuracy of an administrative database for resected gastric adenomas.
Methods
Data of patients who underwent endoscopic resection for benign gastric lesions were collected from three hospitals. Gastric adenoma cases were identified in the hospital database using International Classification of Diseases (ICD) 10-codes. The non-adenoma group included patients without gastric adenoma codes. The diagnostic accuracy for gastric adenoma was analyzed based on the pathological reports of the resected specimen.
Results
Among 5,095 endoscopic resections with codes for benign gastric lesions, 3,909 patients were included in the analysis. Among them, 2,831 and 1,078 patients were allocated to the adenoma and non-adenoma groups, respectively. Regarding the overall diagnosis of gastric adenoma with ICD-10 codes, the sensitivity, specificity, positive predictive value, and negative predictive value were 98.7%, 88.5%, 95.2%, and 96.8%, respectively. There were no significant differences in these parameters between the tertiary and secondary centers.
Conclusions
Administrative codes of gastric adenoma, according to ICD-10 codes, showed good accuracy and can serve as a useful tool to study prognosis of these patients in real-world data studies in the future. -
Citations
Citations to this article as recorded by- Gastric Cancer Incidence and Mortality After Endoscopic Resection of Gastric Adenoma: A Nationwide Cohort Study
Jae Myung Park, Songhee Cho, Ga-Yeong Shin, Jayoun Lee, Minjee Kim, Hyeon Woo Yim
American Journal of Gastroenterology.2023; 118(12): 2166. CrossRef
- Gastric Cancer Incidence and Mortality After Endoscopic Resection of Gastric Adenoma: A Nationwide Cohort Study
- 2,272 View
- 119 Download
- 1 Web of Science
- 1 Crossref

- Clinical utility of endoscopic ultrasound-guided tissue acquisition for comprehensive genomic profiling of pancreatic cancer
- Nozomi Okuno, Kazuo Hara, Nobumasa Mizuno, Shin Haba, Takamichi Kuwahara, Yasuhiro Kuraishi, Daiki Fumihara, Takafumi Yanaidani
- Clin Endosc 2023;56(2):221-228. Published online March 7, 2023
- DOI: https://doi.org/10.5946/ce.2022.086

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic ultrasound-guided tissue acquisition (EUS-TA) is essential for the diagnosis of pancreatic cancer. The feasibility of comprehensive genomic profiling (CGP) using samples obtained by EUS-TA has been under recent discussion. This study aimed to evaluate the utility of EUS-TA for CGP in a clinical setting.
Methods
CGP was attempted in 178 samples obtained from 151 consecutive patients with pancreatic cancer at the Aichi Cancer Center between October 2019 and September 2021. We evaluated the adequacy of the samples for CGP and determined the factors associated with the adequacy of the samples obtained by EUS-TA retrospectively.
Results
The overall adequacy for CGP was 65.2% (116/178), which was significantly different among the four sampling methods (EUS-TA vs. surgical specimen vs. percutaneous biopsy vs. duodenal biopsy, 56.0% [61/109] vs. 80.4% [41/51] vs. 76.5% [13/17] vs. 100.0% [1/1], respectively; p=0.022). In a univariate analysis, needle gauge/type was associated with adequacy (22 G fine-needle aspiration vs. 22 G fine-needle biopsy [FNB] vs. 19 G-FNB, 33.3% (5/15) vs. 53.5% (23/43) vs. 72.5% (29/40); p=0.022). The sample adequacy of 19 G-FNB for CGP was 72.5% (29/40), and there was no significant difference between 19 G-FNB and surgical specimens (p=0.375).
Conclusions
To obtain adequate samples for CGP with EUS-TA, 19 G-FNB was shown to be the best in clinical practice. However, 19 G-FNB was not still sufficient, so further efforts are required to improve adequacy for CGP. -
Citations
Citations to this article as recorded by- Tissue acquisition for comprehensive genomic profiling of gallbladder cancer using a forward-viewing echoendoscope in a patient who underwent Roux-en-Y reconstruction
Michihiro Ono, Shutaro Oiwa, Atsushi Uesugi, Seiya Saito, Ryota Yokoyama, Makoto Usami, Tomoyuki Abe, Miri Fujita, Kohichi Takada, Masahiro Maeda
Clinical Journal of Gastroenterology.2024; 17(1): 164. CrossRef - Endoscopic ultrasound-guided tissue acquisition for comprehensive genomic profiling
Nozomi Okuno, Kazuo Hara
Journal of Medical Ultrasonics.2024; 51(2): 253. CrossRef - Oil blotting paper for formalin fixation increases endoscopic ultrasound‐guided tissue acquisition‐collected sample volumes on glass slides
Takuo Yamai, Kenji Ikezawa, Yusuke Seiki, Ko Watsuji, Yasuharu Kawamoto, Takeru Hirao, Kazuma Daiku, Shingo Maeda, Makiko Urabe, Yugo Kai, Ryoji Takada, Kaori Mukai, Tasuku Nakabori, Hiroyuki Uehara, Sayoko Tsuzaki, Ayumi Ryu, Satoshi Tanada, Shigenori Na
Cancer Medicine.2024;[Epub] CrossRef - Endoscopic ultrasound-guided tissue acquisition for personalized treatment in pancreatic adenocarcinoma
Sang Myung Woo
Clinical Endoscopy.2023; 56(2): 183. CrossRef - Comparison of the novel Franseen needle versus the fine‐needle aspiration needle in endoscopic ultrasound‐guided tissue acquisition for cancer gene panel testing: A propensity score‐matching analysis
Tomotaka Mori, Eisuke Ozawa, Akane Shimakura, Kosuke Takahashi, Satoshi Matsuo, Kazuaki Tajima, Yasuhiko Nakao, Masanori Fukushima, Ryu Sasaki, Satoshi Miuma, Hisamitsu Miyaaki, Shinji Okano, Kazuhiko Nakao
JGH Open.2023; 7(9): 652. CrossRef - Editorial: Endoscopic ultrasound‐guided tissue acquisition in the era of precision medicine
Tiing Leong Ang, James Weiquan Li, Lai Mun Wang
Journal of Gastroenterology and Hepatology.2023; 38(10): 1677. CrossRef
- Tissue acquisition for comprehensive genomic profiling of gallbladder cancer using a forward-viewing echoendoscope in a patient who underwent Roux-en-Y reconstruction
- 1,939 View
- 157 Download
- 4 Web of Science
- 6 Crossref

- A multicenter comparative study of endoscopic ultrasound-guided fine-needle biopsy using a Franseen needle versus conventional endoscopic ultrasound-guided fine-needle aspiration to evaluate microsatellite instability in patients with unresectable pancreatic cancer
- Tadayuki Takagi, Mitsuru Sugimoto, Hidemichi Imamura, Yosuke Takahata, Yuki Nakajima, Rei Suzuki, Naoki Konno, Hiroyuki Asama, Yuki Sato, Hiroki Irie, Jun Nakamura, Mika Takasumi, Minami Hashimoto, Tsunetaka Kato, Ryoichiro Kobashi, Yuko Hashimoto, Goro Shibukawa, Shigeru Marubashi, Takuto Hikichi, Hiromasa Ohira
- Clin Endosc 2023;56(1):107-113. Published online January 16, 2023
- DOI: https://doi.org/10.5946/ce.2022.019

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Immune checkpoint blockade has recently been reported to be effective in treating microsatellite instability (MSI)-high tumors. Therefore, sufficient sampling of histological specimens is necessary in cases of unresectable pancreatic cancer (UR-PC). This multicenter study investigated the efficacy of endoscopic ultrasound-guided fine-needle biopsy (EUS-FNB) using a Franseen needle for MSI evaluation in patients with UR-PC.
Methods
A total of 89 patients with UR-PC who underwent endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) or EUS-FNB using 22-G needles at three hospitals in Japan (2018–2021) were enrolled. Fifty-six of these patients (FNB 23 and FNA 33) were followed up or evaluated for MSI. Patient characteristics, UR-PC data, and procedural outcomes were compared between patients who underwent EUS-FNB and those who underwent EUS-FNA.
Results
No significant difference in terms of sufficient tissue acquisition for histology was observed between patients who underwent EUS-FNB and those who underwent EUS-FNA. MSI evaluation was possible significantly more with tissue samples obtained using EUS-FNB than with tissue samples obtained using EUS-FNA (82.6% [19/23] vs. 45.5% [15/33], respectively; p<0.01). In the multivariate analysis, EUS-FNB was the only significant factor influencing the possibility of MSI evaluation.
Conclusions
EUS-FNB using a Franseen needle is desirable for ensuring sufficient tissue acquisition for MSI evaluation. -
Citations
Citations to this article as recorded by- Oil blotting paper for formalin fixation increases endoscopic ultrasound‐guided tissue acquisition‐collected sample volumes on glass slides
Takuo Yamai, Kenji Ikezawa, Yusuke Seiki, Ko Watsuji, Yasuharu Kawamoto, Takeru Hirao, Kazuma Daiku, Shingo Maeda, Makiko Urabe, Yugo Kai, Ryoji Takada, Kaori Mukai, Tasuku Nakabori, Hiroyuki Uehara, Sayoko Tsuzaki, Ayumi Ryu, Satoshi Tanada, Shigenori Na
Cancer Medicine.2024;[Epub] CrossRef
- Oil blotting paper for formalin fixation increases endoscopic ultrasound‐guided tissue acquisition‐collected sample volumes on glass slides
- 2,154 View
- 125 Download
- 1 Crossref

- Comparison of tube-assisted mapping biopsy with digital single-operator peroral cholangioscopy for preoperative evaluation of biliary tract cancer
- Tsuyoshi Takeda, Takashi Sasaki, Takafumi Mie, Takeshi Okamoto, Chinatsu Mori, Takaaki Furukawa, Yuto Yamada, Akiyoshi Kasuga, Masato Matsuyama, Masato Ozaka, Naoki Sasahira
- Clin Endosc 2022;55(4):549-557. Published online July 20, 2022
- DOI: https://doi.org/10.5946/ce.2021.227
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Digital single-operator cholangioscopy (DSOC)-guided mapping biopsy (DMB) and tube-assisted mapping biopsy (TMB) are two techniques used for preoperative evaluation of biliary tract cancer (BTC). However, data regarding the diagnostic performance of these techniques are limited.
Methods
We retrospectively examined consecutive patients with BTC who underwent either technique at our institution between 2018 and 2020. We evaluated the technical success rate, adequate tissue acquisition rate, and diagnostic performance of these techniques for the evaluation of lateral spread of BTC.
Results
A total of 54 patients were included in the study. The technical success rate of reaching the target sites was 95% for DMB and 100% for TMB. The adequate tissue acquisition rate was 61% for DMB and 69% for TMB. The adequate tissue acquisition rate was low, especially for target sites beyond the secondary biliary radicles. The sensitivity of DMB alone was 39%, which improved to 65% when combined with visual impression. Experts demonstrated a higher negative predictive value and diagnostic accuracy with respect to both DSOC visual impression and DMB for the evaluation of lateral spread of BTC compared to trainees.
Conclusions
Adequate tissue acquisition rates were similar between the two techniques. Since DMB requires expertise, TMB may be an acceptable option when DSOC is unavailable or when DSOC expertise is limited. -
Citations
Citations to this article as recorded by
- 2,274 View
- 151 Download
- 2 Web of Science
- 2 Crossref

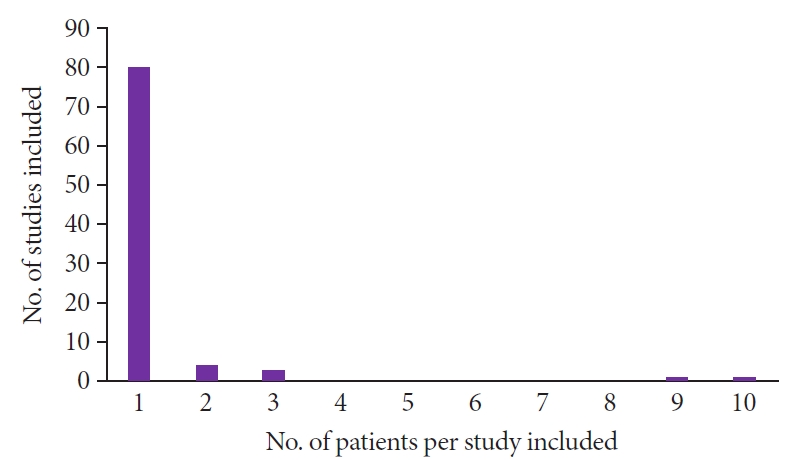
Systematic Review and Meta-Analysis
- Endoscopic diagnosis of gastric metastases from malignant melanoma: systematic review
- Helena Campoli Reggiani, Ana Clara Aguiar Pongeluppi, Vitória Froes Miraglia Martins Ferreira, Isadora Pinheiro Felix, Paulo Moacir de Oliveira Campoli
- Clin Endosc 2022;55(4):507-515. Published online June 28, 2022
- DOI: https://doi.org/10.5946/ce.2022.035
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Metastases of malignant melanoma (MM) are rare and associated with poor prognosis. The objective of this study was to analyze the clinical and endoscopic characteristics of gastric metastases of MM by systematically reviewing cases and case series involving patients diagnosed using upper gastrointestinal endoscopy.
Methods
The PubMed and LILACS databases were searched. Reports containing individual patient data were included. Outcomes such as clinical data, endoscopic findings, treatments, and survival were analyzed.
Results
A total of 88 studies with individual data from 113 patients with gastric metastases of MM were included. The primary sites of MM were the skin (62%), eyes (10%), and mucous membranes (6%). Most patients (56%) had multiple metastases in the stomach, located predominantly in the gastric body (approximately 80%). The overall survival rate at 2 years was 4%. There was a significant reduction in the survival of patients with multiple gastric metastases compared to that of patients with single metastasis (hazard ratio, 0.459; 95% confidence interval, 0.235−0.895; p=0.022).
Conclusions
Gastric metastases of MM have a poor prognosis, especially in patients with multiple implants in the stomach. Additional studies are needed to verify whether ocular and mucosal melanomas are associated with a higher risk of gastric metastases than that of cutaneous melanomas. -
Citations
Citations to this article as recorded by- Case report: Malignant melanoma of the lower limb with gastric metastasis
Qiang Hu, Fengru Zhou, Yuanshui Sun
Frontiers in Oncology.2023;[Epub] CrossRef
- Case report: Malignant melanoma of the lower limb with gastric metastasis
- 2,390 View
- 172 Download
- 1 Web of Science
- 1 Crossref

Original Article
- Underestimation of endoscopic size in large gastric epithelial neoplasms
- Jae Sun Song, Byung Sun Kim, Min A Yang, Young Jae Lee, Gum Mo Jung, Ji Woong Kim, Jin Woong Cho
- Clin Endosc 2022;55(6):760-766. Published online May 19, 2022
- DOI: https://doi.org/10.5946/ce.2021.269
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic submucosal dissection (ESD) is an effective method for resecting gastric adenomas and adenocarcinomas. A significant discrepancy was observed between endoscopic and pathological sizes in samples obtained from patients undergoing ESD. This study elucidates the factors affecting size discrepancy after formalin fixation.
Methods
The records of 64 patients with 69 lesions were analyzed, including 50 adenomas and 19 adenocarcinomas. Data on location, gross shape, histology, and size after fixation in formalin were collected.
Results
The mean size of the resected specimen appeared to decrease after formalin fixation (37.5 mm prefixation vs. 35.8 mm postfixation, p<0.05). The mean long axis diameter of the lesions was 20.3±7.9 mm prefixation and 13.4±7.9 mm postfixation. Size differences in lesions smaller than 20 mm were significantly greater than those in lesions larger than 20 mm (7.6±5.6 mm vs. 2.5±5.8 mm, p<0.01). In multivariate analysis, a tumor size of ≥20 mm was found to be an independent factor affecting size postformalin fixation (p<0.05).
Conclusions
The endoscopic size of lesions before ESD may be underestimated in tumors larger than 20 mm in size. Therefore, increased attention must be paid during ESD to avoid instances of incomplete resection.
- 1,683 View
- 109 Download

Reviews
- Comparing palliative treatment options for cholangiocarcinoma: photodynamic therapy vs. radiofrequency ablation
- Tayyaba Mohammad, Michel Kahaleh
- Clin Endosc 2022;55(3):347-354. Published online May 17, 2022
- DOI: https://doi.org/10.5946/ce.2021.274
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Referral to an endoscopist is often done once curative resection is no longer an option for cholangiocarcinoma management. In such cases, palliation has become the main objective of the treatment. Photodynamic therapy and radiofrequency ablation can be performed to achieve palliation, with both procedures associated with improved stent patency and survival. Despite the greatly increased cost and association with photosensitivity, photodynamic therapy allows transmission to the entire biliary tree. In contrast, radiofrequency ablation is cheaper and faster to apply but requires intraductal contact. This paper reviews both modalities and compares their efficacy and safety for bile duct cancer palliation.
-
Citations
Citations to this article as recorded by- Current interventional options for palliative care for patients with advanced-stage cholangiocarcinoma
Maryam Makki, Malak Bentaleb, Mohammed Abdulrahman, Amal Abdulla Suhool, Salem Al Harthi, Marcelo AF Ribeiro Jr
World Journal of Clinical Oncology.2024; 15(3): 381. CrossRef - Endoskopisch gesteuerte Diagnostik und Therapie von Cholangiokarzinomen
Ulrike Denzer, Alexander Dechêne
Die Gastroenterologie.2023; 18(1): 16. CrossRef - Recent Updates on Local Ablative Therapy Combined with Chemotherapy for Extrahepatic Cholangiocarcinoma: Photodynamic Therapy and Radiofrequency Ablation
Tadahisa Inoue, Masashi Yoneda
Current Oncology.2023; 30(2): 2159. CrossRef - Role of radiofrequency ablation in advanced malignant hilar biliary obstruction
Mamoru Takenaka, Tae Hoon Lee
Clinical Endoscopy.2023; 56(2): 155. CrossRef - Impact of endobiliary radiofrequency ablation on survival of patients with unresectable cholangiocarcinoma: a narrative review
Elena Di Girolamo, Andrea Belli, Alessandro Ottaiano, Vincenza Granata, Valentina Borzillo, Luca Tarotto, Fabiana Tatangelo, Raffaele Palaia, Corrado Civiletti, Mauro Piccirillo, Valentina D’Angelo, Francesco Fiore, Pietro Marone, Guglielmo Nasti, Frances
Frontiers in Oncology.2023;[Epub] CrossRef - Thermal ablative therapies in the gastrointestinal tract
Hendrik Manner
Current Opinion in Gastroenterology.2023; 39(5): 370. CrossRef - Photodynamic Therapy: From the Basics to the Current Progress of N-Heterocyclic-Bearing Dyes as Effective Photosensitizers
Eurico Lima, Lucinda V. Reis
Molecules.2023; 28(13): 5092. CrossRef - Balloon‐assisted laser application for endoscopic treatment of biliary stricture
Seonghee Lim, Van Gia Truong, Seok Jeong, Jiho Lee, Byeong‐il Lee, Hyun Wook Kang
Lasers in Surgery and Medicine.2023; 55(10): 912. CrossRef - Emerging Systemic Therapies in Advanced Unresectable Biliary Tract Cancer: Review and Canadian Perspective
Vincent C. Tam, Ravi Ramjeesingh, Ronald Burkes, Eric M. Yoshida, Sarah Doucette, Howard J. Lim
Current Oncology.2022; 29(10): 7072. CrossRef
- Current interventional options for palliative care for patients with advanced-stage cholangiocarcinoma
- 3,460 View
- 217 Download
- 9 Web of Science
- 9 Crossref

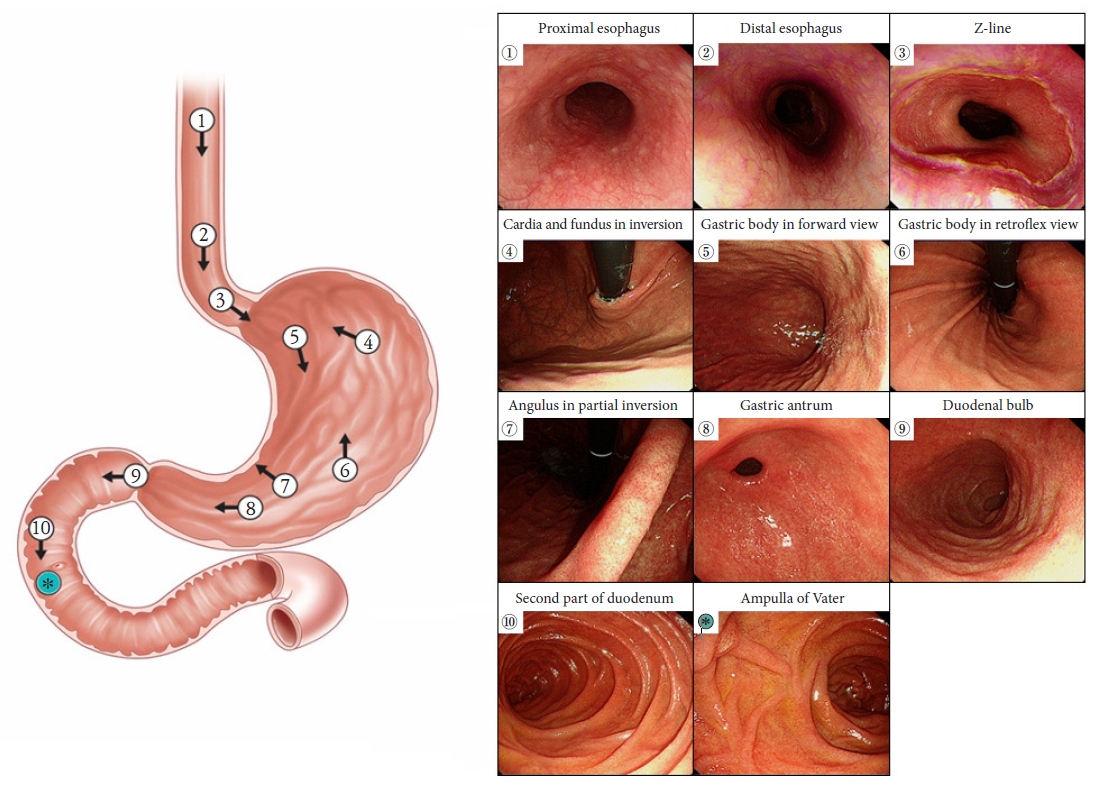
- Quality indicators in esophagogastroduodenoscopy
- Sang Yoon Kim, Jae Myung Park
- Clin Endosc 2022;55(3):319-331. Published online May 16, 2022
- DOI: https://doi.org/10.5946/ce.2022.094
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Esophagogastroduodenoscopy (EGD) has been used to diagnose a wide variety of upper gastrointestinal diseases. In particular, EGD is used to screen high-risk subjects of gastric cancer. Quality control of EGD is important because the diagnostic rate is examiner-dependent. However, there is still no representative quality indicator that can be uniformly applied in EGD. There has been growing awareness of the importance of quality control in improving EGD performance. Therefore, we aimed to review the available and emerging quality indicators for diagnostic EGD.
-
Citations
Citations to this article as recorded by- Current status of quality control in screening esophagogastroduodenoscopy and the emerging role of artificial intelligence
Lihui Zhang, Liwen Yao, Zihua Lu, Honggang Yu
Digestive Endoscopy.2024; 36(1): 5. CrossRef - Relationship between observation time and detection rate of focal lesions in Esophagogastroduodenoscopy: a single-center, retrospective study
Li Dong, Xiaodan Zhang, Yuting Xuan, Peiling Xiong, Yumei Ning, Bing Zhang, Fan Wang, Qiu Zhao, Jun Fang
BMC Gastroenterology.2024;[Epub] CrossRef - The Effect of Esophagogastroduodenoscopy on Intraocular Pressure
Maddalena De Bernardo, Antonella Santonicola, Marco Gioia, Livio Vitiello, Ferdinando Cione, Sergio Pagliarulo, Paola Iovino, Nicola Rosa
Journal of Clinical Medicine.2024; 13(5): 1224. CrossRef - The Diagnostic Performance of Linked Color Imaging Compared to White Light Imaging in Endoscopic Diagnosis of Helicobacter pylori Infection: A Systematic Review and Meta-Analysis
Jae Gon Lee, In Kyung Yoo, Abdullah Ozgur Yeniova, Sang Pyo Lee
Gut and Liver.2024; 18(3): 444. CrossRef - Endoscopic Imaging for the Diagnosis of Neoplastic and Pre-Neoplastic Conditions of the Stomach
Bruno Costa Martins, Renata Nobre Moura, Angelo So Taa Kum, Carolina Ogawa Matsubayashi, Sergio Barbosa Marques, Adriana Vaz Safatle-Ribeiro
Cancers.2023; 15(9): 2445. CrossRef - The effect of short-term training about depth predicting score on the diagnostic ability of invasion depth for differentiated early gastric Cancer among non-expert endoscopists
Hui Li, Hui Hu, Ping Geng, Panhui Guo, Yuanrong Zhu, Lulu Zeng, Jun Liu, Xiangpeng Hu
BMC Medical Education.2023;[Epub] CrossRef - Variation in the rate of detection of minute and small early gastric cancers at diagnostic endoscopy may reflect the performance of individual endoscopists
Daisuke Murakami, Masayuki Yamato, Yuji Amano, Takayoshi Nishino, Makoto Arai
BMJ Open Gastroenterology.2023; 10(1): e001143. CrossRef - Improving the quality of the esophagogastroduodenoscopy in Helicobacter pylori-naïve gastric cancer
Jae Myung Park
Clinical Endoscopy.2023; 56(4): 453. CrossRef - Simethicone and N-acetyl cysteine in improving mucosal visibility: Towards a “clearer view” during endoscopy
Akash Roy, Mahesh K. Goenka
Indian Journal of Gastroenterology.2023;[Epub] CrossRef - Enhancing the Quality of Upper Gastrointestinal Endoscopy: Current Indicators and Future Trends
Caesar Ferrari, Micheal Tadros
Gastroenterology Insights.2023; 15(1): 1. CrossRef - Antispasmodic Agent Administration Improves Gastric Neoplasm Detection Rates during Esophagogastroduodenoscopy
Sang Yoon Kim, Jae Myung Park
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2022; 22(3): 246. CrossRef - Clinical features of gastric adenoma detected within 3 years after negative screening endoscopy in Korea
Hyun Young Kim
Gastroenterology Report.2022;[Epub] CrossRef
- Current status of quality control in screening esophagogastroduodenoscopy and the emerging role of artificial intelligence
- 8,424 View
- 509 Download
- 12 Web of Science
- 12 Crossref

Original Article
-
Feasibility and safety of endoscopic submucosal dissection for lesions in proximity to a colonic diverticulum

- Nobuaki Ikezawa, Takashi Toyonaga, Shinwa Tanaka, Tetsuya Yoshizaki, Toshitatsu Takao, Hirofumi Abe, Hiroya Sakaguchi, Kazunori Tsuda, Satoshi Urakami, Tatsuya Nakai, Taku Harada, Kou Miura, Takahisa Yamasaki, Stuart Kostalas, Yoshinori Morita, Yuzo Kodama
- Clin Endosc 2022;55(3):417-425. Published online May 12, 2022
- DOI: https://doi.org/10.5946/ce.2021.245
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: Endoscopic submucosal dissection (ESD) for diverticulum-associated colorectal lesions is generally contraindicated because of the high risk of perforation. Several studies on patients with such lesions treated with ESD have been reported recently. However, the feasibility and safety of ESD for lesions in proximity to a colonic diverticulum (D-ESD) have not been fully clarified. The aim of this study was to evaluate the feasibility and safety of D-ESD.
Methods
D-ESD was defined as ESD for lesions within approximately 3 mm of a diverticulum. Twenty-six consecutive patients who underwent D-ESD were included. Two strategic approaches were used depending on whether submucosal dissection of the diverticulum-related part was required (strategy B) or not (strategy A). Treatment outcomes and adverse events associated with each strategy were analyzed.
Results
The en bloc resection rate was 96.2%. The rates of R0 and curative resection in strategies A and B were 80.8%, 73.1%, 84.6%, and 70.6%, respectively. Two cases of intraoperative perforation and one case of delayed perforation occurred. The delayed perforation case required emergency surgery, but the other cases were managed conservatively.
Conclusions
D-ESD may be a feasible treatment option. However, it should be performed in a high-volume center by expert hands because it requires highly skilled endoscopic techniques. -
Citations
Citations to this article as recorded by- Endoscopic submucosal dissection for diverticulum using combination of countertraction and circumferential-inversion method
Hiroshi Takayama, Yoshinori Morita, Toshitatsu Takao, Douglas Motomura, Madoka Takao, Takashi Toyonaga, Yuzo Kodama
Endoscopy.2024; 56(S 01): E91. CrossRef - Traction-assisted endoscopic submucosal dissection for resection of ileocecal valve neoplasia: a French retrospective multicenter case series
Clara Yzet, Timothée Wallenhorst, Jérémie Jacques, Mariana Figueiredo Ferreira, Jérôme Rivory, Florian Rostain, Louis-Jean Masgnaux, Jean Grimaldi, Romain Legros, Pierre Lafeuille, Jérémie Albouys, Fabien Subtil, Marion Schaefer, Mathieu Pioche
Endoscopy.2024;[Epub] CrossRef - The role of cap-assisted endoscopy and its future implications
Sol Kim, Bo-In Lee
Clinical Endoscopy.2024; 57(3): 293. CrossRef - Successful planned piecemeal endoscopic resection using gel immersion and an over-the-scope clip for a lesion extensively extended into the colonic diverticulum
Tomoaki Tashima, Takahiro Muramatsu, Tomonori Kawasaki, Tsubasa Ishikawa, Shomei Ryozawa
VideoGIE.2023; 8(4): 167. CrossRef - Future therapeutic implications of new molecular mechanism of colorectal cancer
Sen Lu, Cheng-You Jia, Jian-She Yang
World Journal of Gastroenterology.2023; 29(16): 2359. CrossRef - Iatrogenic colorectal perforation caused by a clip
Hirotaka Oura, Yasuki Hatayama, Erika Nomura, Harutoshi Sugiyama, Daisuke Murakami, Makoto Arai, Takayoshi Nishino
Endoscopy.2023; 55(S 01): E1091. CrossRef
- Endoscopic submucosal dissection for diverticulum using combination of countertraction and circumferential-inversion method
- 3,725 View
- 171 Download
- 4 Web of Science
- 6 Crossref

Systematic Review and Meta-Analysis
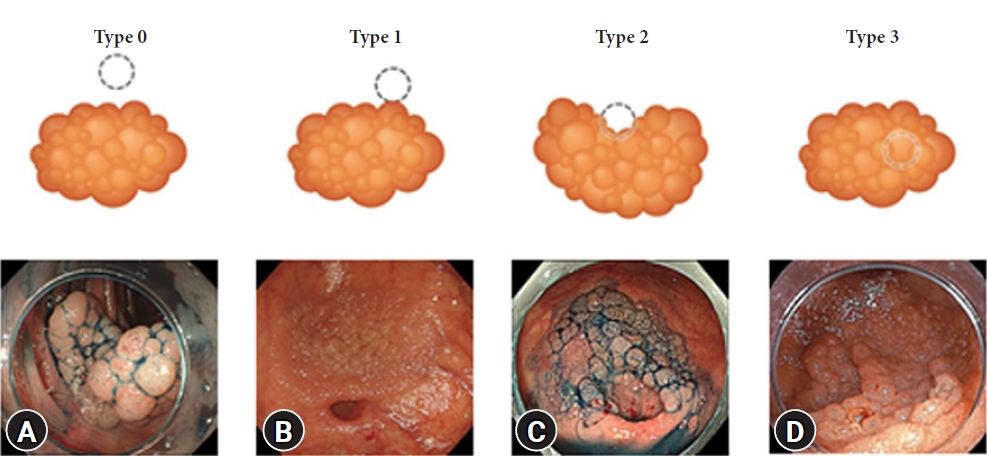
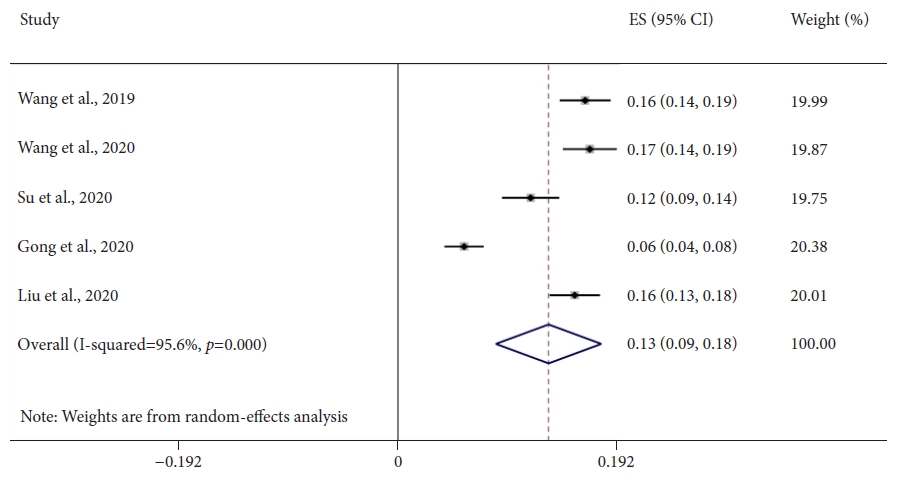
- Does computer-aided diagnostic endoscopy improve the detection of commonly missed polyps? A meta-analysis
- Arun Sivananthan, Scarlet Nazarian, Lakshmana Ayaru, Kinesh Patel, Hutan Ashrafian, Ara Darzi, Nisha Patel
- Clin Endosc 2022;55(3):355-364. Published online May 12, 2022
- DOI: https://doi.org/10.5946/ce.2021.228
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Colonoscopy is the gold standard diagnostic method for colorectal neoplasia, allowing detection and resection of adenomatous polyps; however, significant proportions of adenomas are missed. Computer-aided detection (CADe) systems in endoscopy are currently available to help identify lesions. Diminutive (≤5 mm) and nonpedunculated polyps are most commonly missed. This meta-analysis aimed to assess whether CADe systems can improve the real-time detection of these commonly missed lesions.
Methods
A comprehensive literature search was performed. Randomized controlled trials evaluating CADe systems categorized by morphology and lesion size were included. The mean number of polyps and adenomas per patient was derived. Independent proportions and their differences were calculated using DerSimonian and Laird random-effects modeling.
Results
Seven studies, including 2,595 CADe-assisted colonoscopies and 2,622 conventional colonoscopies, were analyzed. CADe-assisted colonoscopy demonstrated an 80% increase in the mean number of diminutive adenomas detected per patient compared with conventional colonoscopy (0.31 vs. 0.17; effect size, 0.13; 95% confidence interval [CI], 0.09–0.18); it also demonstrated a 91.7% increase in the mean number of nonpedunculated adenomas detected per patient (0.32 vs. 0.19; effect size, 0.05; 95% CI, 0.02–0.07).
Conclusions
CADe-assisted endoscopy significantly improved the detection of most commonly missed adenomas. Although this method is a potentially exciting technology, limitations still apply to current data, prompting the need for further real-time studies. -
Citations
Citations to this article as recorded by- Use of artificial intelligence in the management of T1 colorectal cancer: a new tool in the arsenal or is deep learning out of its depth?
James Weiquan Li, Lai Mun Wang, Katsuro Ichimasa, Kenneth Weicong Lin, James Chi-Yong Ngu, Tiing Leong Ang
Clinical Endoscopy.2024; 57(1): 24. CrossRef - As how artificial intelligence is revolutionizing endoscopy
Jean-Francois Rey
Clinical Endoscopy.2024; 57(3): 302. CrossRef - Eye tracking technology in endoscopy: Looking to the future
Arun Sivananthan, Jabed Ahmed, Alexandros Kogkas, George Mylonas, Ara Darzi, Nisha Patel
Digestive Endoscopy.2023; 35(3): 314. CrossRef - Artificial intelligence and the push for small adenomas: all we need?
Katharina Zimmermann-Fraedrich, Thomas Rösch
Endoscopy.2023; 55(04): 320. CrossRef - Recent advances in devices and technologies that might prove revolutionary for colonoscopy procedures
Jonathan S. Galati, Kevin Lin, Seth A. Gross
Expert Review of Medical Devices.2023; 20(12): 1087. CrossRef - Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Mizuki Nagai, Sho Suzuki, Yohei Minato, Fumiaki Ishibashi, Kentaro Mochida, Ken Ohata, Tetsuo Morishita
Clinical Endoscopy.2023; 56(5): 553. CrossRef - KI-Werkzeuge als smarte Helfer in Klinik und Forschung
Zeitschrift für Gastroenterologie.2023; 61(11): 1544. CrossRef - AI-powered medical devices for practical clinicians including the diagnosis of colorectal polyps
Donghwan Kim, Eunsun Kim
Journal of the Korean Medical Association.2023; 66(11): 658. CrossRef - The Role of Artificial Intelligence in Colorectal Cancer Screening: Lesion Detection and Lesion Characterization
Edward Young, Louisa Edwards, Rajvinder Singh
Cancers.2023; 15(21): 5126. CrossRef - Artificial intelligence for colorectal neoplasia detection during colonoscopy: a systematic review and meta-analysis of randomized clinical trials
Shenghan Lou, Fenqi Du, Wenjie Song, Yixiu Xia, Xinyu Yue, Da Yang, Binbin Cui, Yanlong Liu, Peng Han
eClinicalMedicine.2023; 66: 102341. CrossRef - Pouring some water into the wine—Poor performance of endoscopists in artificial intelligence studies
Jochen Weigt
United European Gastroenterology Journal.2022; 10(8): 793. CrossRef
- Use of artificial intelligence in the management of T1 colorectal cancer: a new tool in the arsenal or is deep learning out of its depth?
- 3,031 View
- 155 Download
- 11 Web of Science
- 11 Crossref

Original Article
- Outcomes of endoscopic submucosal dissection for superficial esophageal neoplasms in patients with liver cirrhosis
- Young Kwon Choi, Jin Hee Noh, Do Hoon Kim, Hee Kyong Na, Ji Yong Ahn, Jeong Hoon Lee, Kee Wook Jung, Kee Don Choi, Ho June Song, Gin Hyug Lee, Hwoon-Yong Jung
- Clin Endosc 2022;55(3):381-389. Published online April 20, 2022
- DOI: https://doi.org/10.5946/ce.2021.242

-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: The treatment of superficial esophageal neoplasms (SENs) in cirrhotic patients is challenging and rarely investigated. We evaluated the outcomes of endoscopic submucosal dissection (ESD) to determine the efficacy and safety of treating SENs in patients with liver cirrhosis.
Methods
The baseline characteristics and treatment outcomes of patients who underwent ESD for SENs between November 2005 and December 2017 were retrospectively reviewed.
Results
ESD was performed in 437 patients with 481 SENs, including 15 cirrhotic patients with 17 SENs. En bloc resection (88.2% vs. 97.0%) and curative resection (64.7% vs. 78.9%) rates were not different between the cirrhosis and non-cirrhosis groups (p=0.105 and p=0.224, respectively). Bleeding was more common in cirrhotic patients (p=0.054), and all cases were successfully controlled endoscopically. The median procedure and hospitalization duration did not differ between the groups. Overall survival was lower in cirrhotic patients (p=0.003), while disease-specific survival did not differ between the groups (p=0.85).
Conclusions
ESD could be a safe and effective treatment option for SENs in patients with cirrhosis. Detailed preprocedural assessments are needed, including determination of liver function, esophageal varix status, and remaining life expectancy, to identify patients who will obtain the greatest benefit. -
Citations
Citations to this article as recorded by- Clinical outcomes of endoscopic submucosal dissection for esophageal squamous cell carcinoma with esophageal varices: Multicenter retrospective study
Yosuke Toya, Waku Hatta, Tomohiro Shimada, Tamotsu Matsuhashi, Takeharu Shiroki, Yu Sasaki, Tetsuya Tatsuta, Jun Nakamura, Norihiro Hanabata, Yohei Horikawa, Ko Nagino, Tomoyuki Koike, Atsushi Masamune, Yoshihiro Harada, Tetsuya Ohira, Katsunori Iijima, Y
Digestive Endoscopy.2024; 36(3): 314. CrossRef - Risk associated with endoscopic treatment of early upper gastrointestinal cancer in patients with liver cirrhosis and management strategies
Yu-Yong Tan, Yu-Min Qing, Jian Gong, De-Liang Liu
World Chinese Journal of Digestology.2024; 32(2): 102. CrossRef - Endoscopic submucosal dissection for early cancers or precancerous lesions of the upper GI tract in cirrhotic patients with esophagogastric varices: 10-year experience from a large tertiary center in China
Shuai Zhang, Ying-Di Liu, Ning-Li Chai, Yi Yao, Fei Gao, Bo Liu, Zhan-Di He, Lu Bai, Xin Huang, Chao Gao, En-Qiang Linghu, Lian-Yong Li
Gastrointestinal Endoscopy.2023; 97(6): 1031. CrossRef - Endoscopic Submucosal Dissection for Treatment of Early-Stage Cancer or Precancerous Lesion in the Upper Gastrointestinal Tract in Patients with Liver Cirrhosis
Yuyong Tan, Yumin Qing, Deliang Liu, Jian Gong
Journal of Clinical Medicine.2023; 12(20): 6509. CrossRef - Clinical outcomes of endoscopic submucosal dissection for superficial esophageal neoplasia in close proximity to esophageal varices: a multicenter international experience
Shruti Mony, Bing Hu, Abel Joseph, Hiroyuki Aihara, Lorenzo Ferri, Amit Bhatt, Amit Mehta, Peng-Sheng Ting, Alex Chen, Andrew Kalra, Jad Farha, Manabu Onimaru, Long He, Qi Luo, Andrew Y. Wang, Haruhiro Inoue, Saowanee Ngamruengphong
Endoscopy.2023;[Epub] CrossRef
- Clinical outcomes of endoscopic submucosal dissection for esophageal squamous cell carcinoma with esophageal varices: Multicenter retrospective study
- 2,695 View
- 129 Download
- 4 Web of Science
- 5 Crossref

Review
- Radiation Proctitis and Management Strategies
- Dushyant Singh Dahiya, Asim Kichloo, Faiz Tuma, Michael Albosta, Farah Wani
- Clin Endosc 2022;55(1):22-32. Published online November 18, 2021
- DOI: https://doi.org/10.5946/ce.2020.288

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Radiotherapy (RT) is a treatment modality that uses high-energy rays or radioactive agents to generate ionizing radiation against rapidly dividing cells. The main objective of using radiation in cancer therapy is to impair or halt the division of the tumor cells. Over the past few decades, advancements in technology, the introduction of newer methods of RT, and a better understanding of the pathophysiology of cancers have enabled physicians to deliver doses of radiation that match the exact dimensions of the tumor for greater efficacy, with minimal exposure of the surrounding tissues. However, RT has numerous complications, the most common being radiation proctitis (RP). It is characterized by damage to the rectal epithelium by secondary ionizing radiation. Based on the onset of signs and symptoms, post-radiotherapy RP can be classified as acute or chronic, each with varying levels of severity and complication rates. The treatment options available for RP are limited, with most of the data on treatment available from case reports or small studies. Here, we describe the types of RT used in modern-day medicine and radiation-mediated tissue injury. We have primarily focused on the classification, epidemiology, pathogenesis, clinical features, treatment strategies, complications, and prognosis of RP.
-
Citations
Citations to this article as recorded by- Concurrent rectal perforation and obstruction following neoadjuvant chemoradiation for locally advanced rectal cancer: A case report
Tahmineh Tahouri, Sahand Hedayati Omami, Maryam Hosseini, Ehsanollah Rahimi-Movaghar
International Journal of Surgery Case Reports.2024; 116: 109337. CrossRef - Endoscopic resection of residual rectal neoplasia after definitive chemoradiotherapy for rectal cancer
Robert Klimkowski, Jakub Krzyzkowiak, Nastazja Dagny Pilonis, Krzysztof Bujko, Michal F. Kaminski
Best Practice & Research Clinical Gastroenterology.2024; 68: 101896. CrossRef - Radiation injuries of organs and tissues: mechanisms of occurrence, methods of prevention and treatment: A review
Daiana A. Balaeva, Denis S. Romanov, Oxana P. Trofimova, Zarina Z. Gadzhibabaeva, Yury Yu. Gorchak, Garia A. Gariaev
Journal of Modern Oncology.2024; 25(4): 504. CrossRef - Interventions for Managing Late Gastrointestinal Symptoms Following Pelvic Radiotherapy: a Systematic Review and Meta-analysis
H. Berntsson, A. Thien, D. Hind, L. Stewart, M. Mahzabin, W.S. Tung, M. Bradburn, M. Kurien
Clinical Oncology.2024; 36(5): 318. CrossRef - Intestinal microecological transplantation for a patient with chronic radiation enteritis: A case report
Lin Wang, Yan Li, Yu-Jing Zhang, Li-Hua Peng
World Journal of Gastroenterology.2024; 30(19): 2603. CrossRef - Intrarectal formalin treatment for haemorrhagic radiation‐induced proctopathy: efficacy and safety
Darina Kohoutova, Ana Wilson, Caroline Gee, Ramy Elhusseiny, Linda Wanders, David Cunningham
Colorectal Disease.2024; 26(5): 932. CrossRef - Emodin ameliorates acute radiation proctitis in mice by regulating AKT/MAPK/NF-κB/VEGF pathways
Jinsheng Gao, Yousong Li, Jiaohua Chen, Wen Feng, Jianchen Bu, Zixuan Lu, Jiandong Wang
International Immunopharmacology.2024; 132: 111945. CrossRef - Protocolo diagnóstico de la rectitis (proctitis)
C. Iniesta Cavero, L. Menchén-Viso
Medicine - Programa de Formación Médica Continuada Acreditado.2024; 14(8): 468. CrossRef - Administration of modified Gegen Qinlian decoction for hemorrhagic chronic radiation proctitis: A case report and review of literature
Shao-Yong Liu, Liu-Ling Hu, Shi-Jun Wang, Zhong-Li Liao
World Journal of Clinical Cases.2023; 11(5): 1129. CrossRef - A Retrospective Single-Arm Cohort Study in a Single Center of Radiofrequency Ablation in Treatment of Chronic Radiation Proctitis
Chien-En Tang, Kung-Chuan Cheng, Kuen-Lin Wu, Hong-Hwa Chen, Ko-Chao Lee
Life.2023; 13(2): 566. CrossRef - Survivorship in Early-Stage Rectal Cancer Patients Who Have Received Combined Modality Therapy
Saboor E. Randhawa, Laura Tenner
Clinical Colorectal Cancer.2023; 22(4): 375. CrossRef - A Systematic Review of Population-Based Studies of Chronic Bowel Symptoms in Cancer Survivors following Pelvic Radiotherapy
Adam Biran, Iakov Bolnykh, Ben Rimmer, Anthony Cunliffe, Lisa Durrant, John Hancock, Helen Ludlow, Ian Pedley, Colin Rees, Linda Sharp
Cancers.2023; 15(16): 4037. CrossRef - The effectiveness of hyperbaric oxygen therapy for managing radiation-induced proctitis – results of a 10-year retrospective cohort study
António Moreira Monteiro, Diogo Alpuim Costa, Virgínia Mareco, Carla Espiney Amaro
Frontiers in Oncology.2023;[Epub] CrossRef - Chinese clinical practice guidelines for the prevention and treatment of radiation‐induced rectal injury
Hui Zhang, Zhen Zhang, Shuanghu Yuan
Precision Radiation Oncology.2023; 7(4): 237. CrossRef - Progress in multidisciplinary treatment of hemorrhagic radiation proctitis
Qiulian Li, Guangjie Liao
Annals of Oncology Research and Therapy.2022; 2(1): 10. CrossRef
- Concurrent rectal perforation and obstruction following neoadjuvant chemoradiation for locally advanced rectal cancer: A case report
- 6,844 View
- 548 Download
- 13 Web of Science
- 15 Crossref

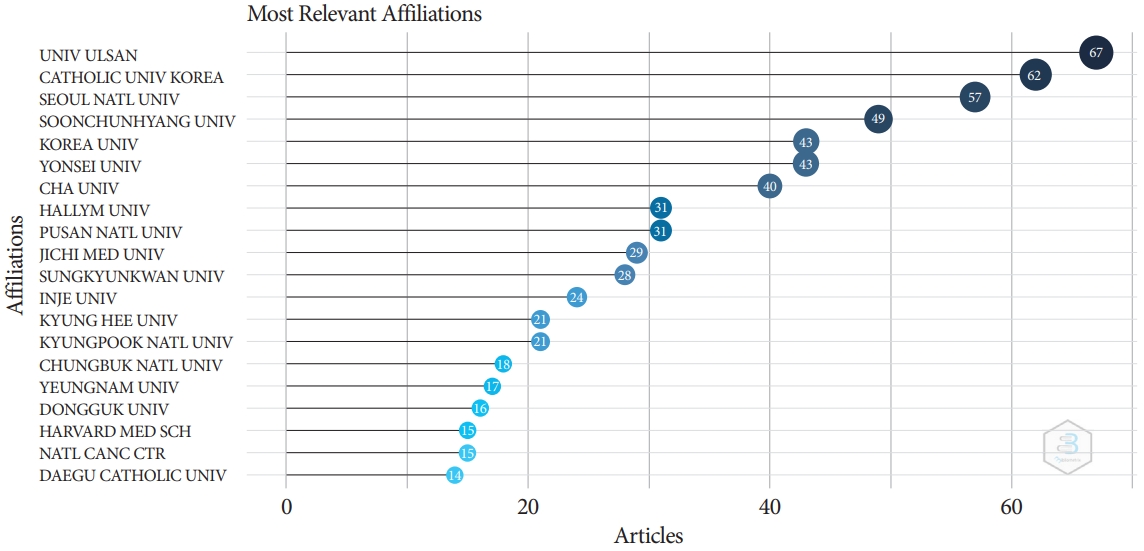
Special Article: Celebrating the 10th Anniversary of Clinical Endoscopy
- Document Network and Conceptual and Social Structures of Clinical Endoscopy from 2015 to July 2021 Based on the Web of Science Core Collection: A Bibliometric Study
- Sun Huh
- Clin Endosc 2021;54(5):641-650. Published online September 30, 2021
- DOI: https://doi.org/10.5946/ce.2021.207
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: The present study investigated the relevance and network of institutions, keywords, and authors’ countries of the articles in Clinical Endoscopy published from 2015 to May 2021 based on the Web of Science Core Collection.
Methods
The Web of Science Core Collection was searched with the term Clinical Endoscopy as the publication title on July 12, 2021. All 776 citations published from 2015 to May 2021 and 2,964 articles citing those 776 articles were analyzed using Biblioshiny.
Results
The corresponding authors were from 73 countries. Document coupling showed that the colorectal cancer-colonoscopyrandomized controlled trial cluster had the most significant impact and highest centrality. There were 442 articles with corresponding authors from Korea (57.0%). The number of collaborative works by Korean authors with the authors of other countries was 33 (7.5%). The articles were cited 2,964 times by corresponding authors from 37 countries.
Conclusions
The above results show that Clinical Endoscopy has published several studies on gastrointestinal endoscopy. A large proportion of citations (84.7 %) were from outside Korea, indicating that the journal content is useful for global physicians. Collaborative work between authors from Korea and other countries should be encouraged to promote the journal. -
Citations
Citations to this article as recorded by- Research Progress in Land Consolidation and Rural Revitalization: Current Status, Characteristics, Regional Differences, and Evolution Laws
Shuchang Li, Wei Song
Land.2023; 12(1): 210. CrossRef - Journal metrics, document network, and conceptual and social structures of the Korean Journal of Anesthesiology from 2017 to July 2022: a bibliometric study
Sun Huh
Korean Journal of Anesthesiology.2023; 76(1): 3. CrossRef - Promotion to Top-Tier Journal and Development Strategy of the Annals of Laboratory Medicine for Strengthening its Leadership in the Medical Laboratory Technology Category: A Bibliometric Study
Sun Huh
Annals of Laboratory Medicine.2022; 42(3): 321. CrossRef - Research trends on endoscopic mucosal resection: A bibliometric analysis from 1991 to 2021
Yihan Yang, Xuan Xu, Menghui Wang, Yang Zhang, Pinglang Zhou, Sifan Yang, Xu Shu, Chuan Xie
Frontiers in Surgery.2022;[Epub] CrossRef - Riesgo de sangrado gastrointestinal por uso de anticoagulantes directos orales: ¿cuál es más seguro?
Ivan David Lozada Martinez, Luis Carlos Solano Díaz, Marcela Barbosa Pérez, Víctor Andrés Rueda Oviedo, Brainerd Lenin Caicedo Moncada, Gustavo Andrés Diaz Cruz, Adriana cristina Ceballos Espitia, David Esteban Diaz Gómez, Daiana Andrea Rojas Ramí
Revista Cuarzo.2022; 28(2): 31. CrossRef
- Research Progress in Land Consolidation and Rural Revitalization: Current Status, Characteristics, Regional Differences, and Evolution Laws
- 3,432 View
- 61 Download
- 4 Web of Science
- 5 Crossref

Case Report
- Colorectal carcinoma and chronic inflammatory demyelinating polyneuropathy: is there a possible paraneoplastic association?
- Adnan Malik, Faisal Inayat, Muhammad Hassan Naeem Goraya, Gul Nawaz, Ahmad Mehran, Atif Aziz, Saad Saleem
- Clin Endosc 2023;56(2):245-251. Published online July 28, 2021
- DOI: https://doi.org/10.5946/ce.2021.076
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - A plethora of paraneoplastic syndromes have been reported as remote effects of colorectal carcinoma (CRC). However, there is a dearth of data pertaining to the association of this cancer with demyelinating neuropathies. Herein, we describe the case of a young woman diagnosed with chronic inflammatory demyelinating polyneuropathy (CIDP). Treatment with intravenous immunoglobulins and prednisone did not improve her condition, and her neurological symptoms worsened. Subsequently, she was readmitted with exertional dyspnea, lightheadedness, malaise, and black stools. Colonoscopy revealed a necrotic mass in the ascending colon, which directly invaded the second part of the duodenum. Pathologic results confirmed the diagnosis of locally advanced CRC. Upon surgical resection of the cancer, her CIDP showed dramatic resolution without any additional therapy. Patients with CRC may develop CIDP as a type of paraneoplastic syndrome. Clinicians should remain cognizant of this potential association, as it is of paramount importance for the necessary holistic clinical management.
- 4,092 View
- 323 Download

Focused Review Series: Image-Enhanced Endoscopy: Update on Clinical Practice
- Current Status of Image-Enhanced Endoscopy for Early Identification of Esophageal Neoplasms
- Shin Hee Kim, Su Jin Hong
- Clin Endosc 2021;54(4):464-476. Published online July 26, 2021
- DOI: https://doi.org/10.5946/ce.2021.186
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Advanced esophageal cancer is known to have a poor prognosis. The early detection of esophageal neoplasms, including esophageal dysplasia and early esophageal cancer, is highly important for the accurate treatment of the disease. However, esophageal dysplasia and early esophageal cancer are usually subtle and can be easily missed. In addition to the early detection, proper pretreatment evaluation of the depth of invasion of esophageal cancer is very important for curative treatment. The progression of non-invasive diagnosis via image-enhanced endoscopy techniques has been shown to aid the early detection and estimate the depth of invasion of early esophageal cancer and, as a result, may provide additional opportunities for curative treatment. Here, we review the advancement of image-enhanced endoscopy-related technologies and their role in the early identification of esophageal neoplasms.
-
Citations
Citations to this article as recorded by- An umbrella-inspired snap-on robotic 3D photoacoustic endoscopic probe for augmented intragastric sensing: Proof of concept study
Li Liu, Ang Li, Yisong Zhao, Luyao Zhu, Yongjian Zhao, Fei Gao
Photoacoustics.2024; 35: 100568. CrossRef - Curative criteria for endoscopic treatment of oesophageal adenocarcinoma
Annemijn D.I. Maan, Prateek Sharma, Arjun D. Koch
Best Practice & Research Clinical Gastroenterology.2024; 68: 101886. CrossRef - Biomarkers for Early Detection, Prognosis, and Therapeutics of Esophageal Cancers
Vikrant Rai, Joe Abdo, Devendra K. Agrawal
International Journal of Molecular Sciences.2023; 24(4): 3316. CrossRef - Magnifying Endoscopy with Narrow-Band Imaging for Duodenal Neuroendocrine Tumors
Gwang Ha Kim, Kiyoun Yi, Dong Chan Joo, Moon Won Lee, Hye Kyung Jeon, Bong Eun Lee
Journal of Clinical Medicine.2023; 12(9): 3106. CrossRef - Role of linked color imaging for upper gastrointestinal disease: present and future
Sang Pyo Lee
Clinical Endoscopy.2023; 56(5): 546. CrossRef - Analysis of Colorectal and Gastric Cancer Classification: A Mathematical Insight Utilizing Traditional Machine Learning Classifiers
Hari Mohan Rai, Joon Yoo
Mathematics.2023; 11(24): 4937. CrossRef - Application of artificial intelligence-assisted endoscopic detection of early esophageal cancer
Qing Li, Bing-Rong Liu
World Chinese Journal of Digestology.2021; 29(24): 1389. CrossRef
- An umbrella-inspired snap-on robotic 3D photoacoustic endoscopic probe for augmented intragastric sensing: Proof of concept study
- 4,970 View
- 260 Download
- 6 Web of Science
- 7 Crossref

Original Articles
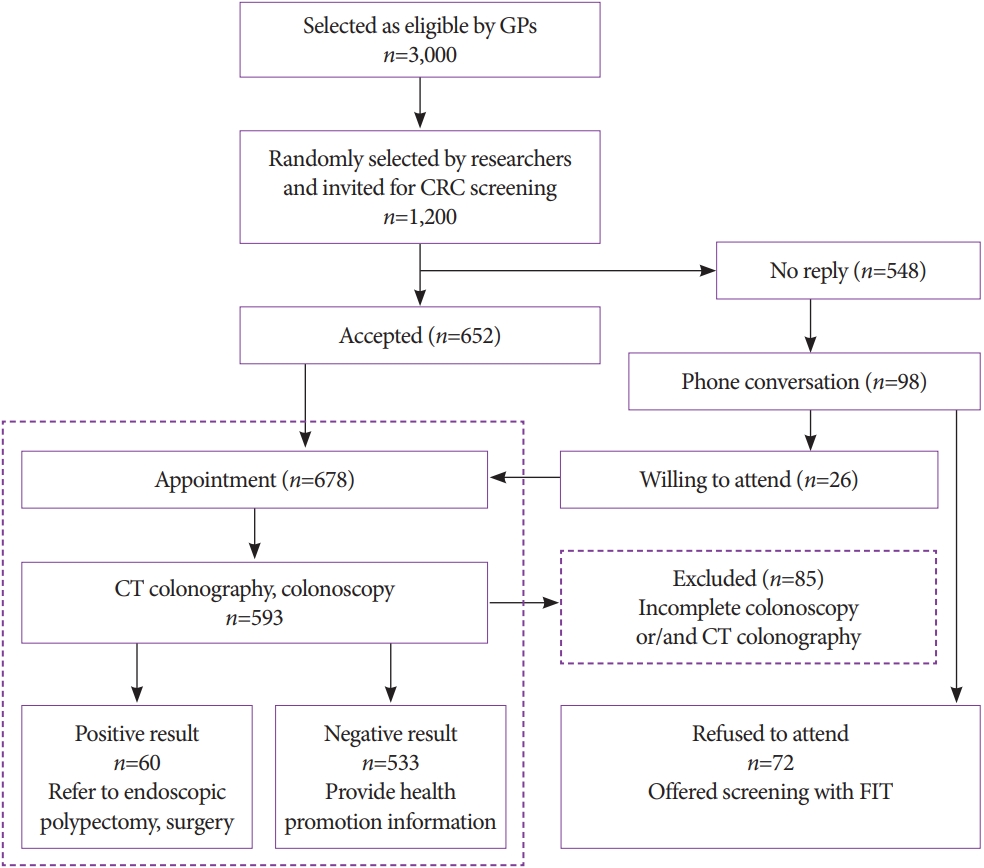
- Colorectal Cancer Screening with Computed Tomography Colonography: Single Region Experience in Kazakhstan
- Jandos Amankulov, Dilyara Kaidarova, Zhamilya Zholdybay, Marianna Zagurovskaya, Nurlan Baltabekov, Madina Gabdullina, Akmaral Ainakulova, Dias Toleshbayev, Alexandra Panina, Elvira Satbayeva, Zhansaya Kalieva
- Clin Endosc 2022;55(1):101-112. Published online July 15, 2021
- DOI: https://doi.org/10.5946/ce.2021.066
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: The aim of our study was to determine the efficacy of computed tomography colonography (CTC) in screening for colorectal cancer (CRC).
Methods
A total of 612 females and 588 males aged 45 to 75 years were enrolled in CTC screening. CTC was performed following standard bowel preparation and colonic insufflation with carbon dioxide. The main outcomes were the detection rate of CRC and advanced adenoma (AA), prevalence of colorectal lesions in relation to socio-demographic and health factors, and overall diagnostic performance of CTC.
Results
Overall, 56.5% of the 1,200 invited subjects underwent CTC screening. The sensitivity for CRC and AA was 0.89 and 0.97, respectively, while the specificity was 0.71 and 0.99, respectively. The prevalence of CRC and AA was 3.0% (18/593) and 7.1% (42/593), respectively, with the highest CRC prevalence in the 66-75 age group (≥12 times; odds ratio [OR], 12.11; 95% confidence interval [CI], 4.45-32.92). CRC and AA prevalence were inversely correlated with Asian descent, physical activity, and negative fecal immunochemical test results (OR=0.43; 95% CI, 0.22-0.83; OR=0.16; 95% CI, 0.04-0.68; OR=0.5; 95% CI, 0.07-3.85, respectively).
Conclusions
Our study revealed high accuracy of CTC in diagnosing colonic neoplasms, good compliance with CTC screening, and high detection rate of CRC.
- 5,700 View
- 205 Download
- 1 Web of Science

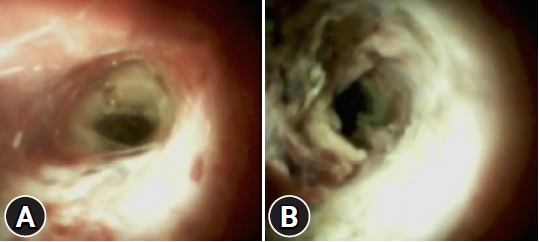
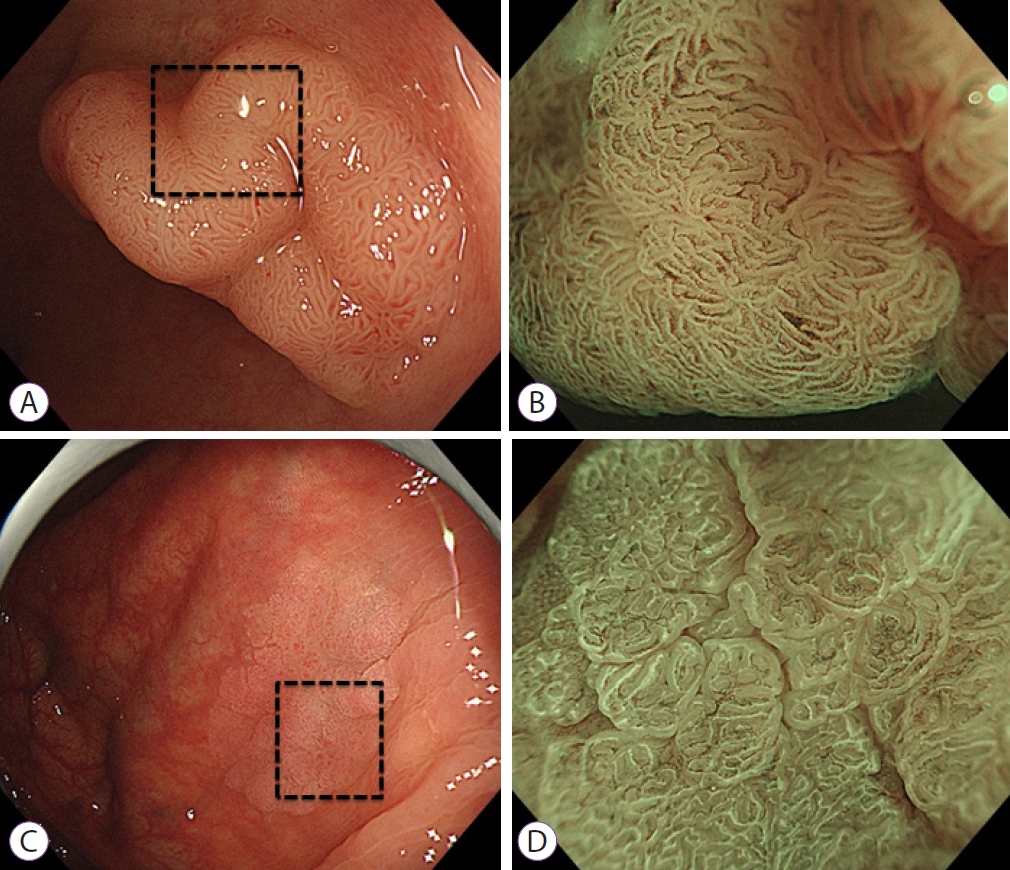
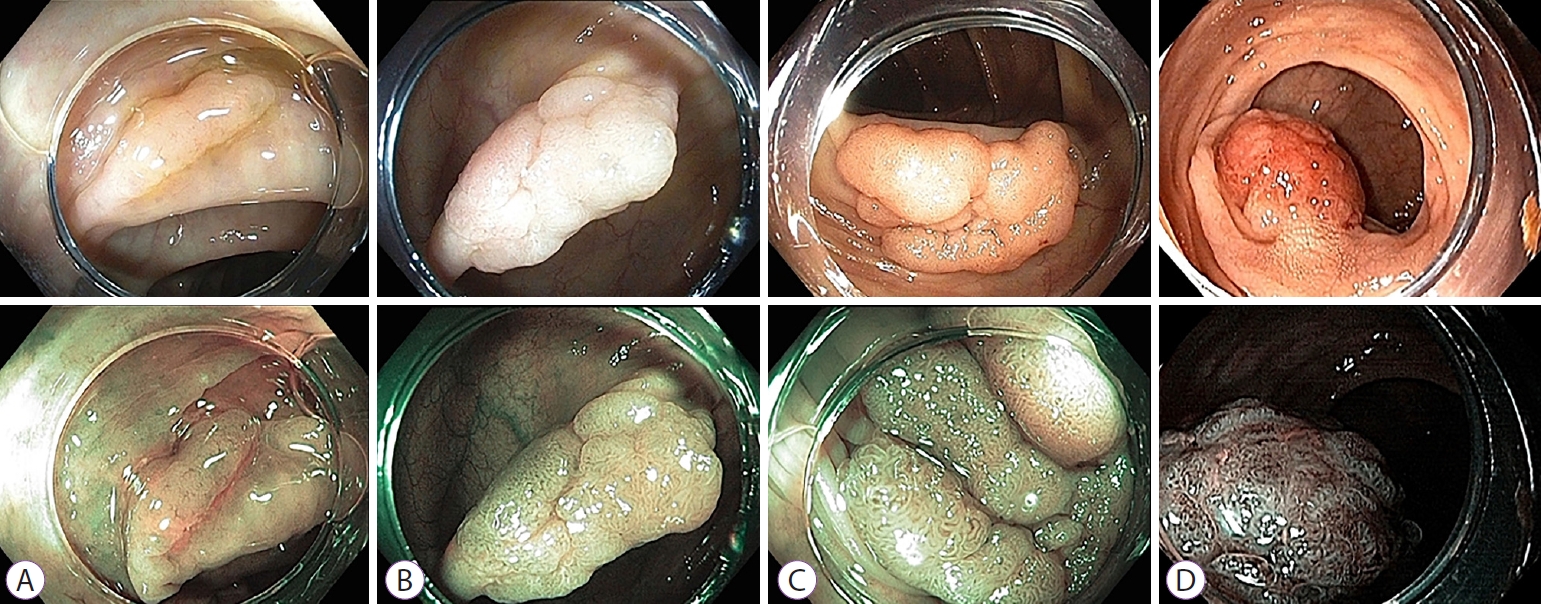
- White Opaque Substance, a New Optical Marker on Magnifying Endoscopy: Usefulness in Diagnosing Colorectal Epithelial Neoplasms
- Kazutomo Yamasaki, Takashi Hisabe, Kenshi Yao, Hiroshi Ishihara, Kentaro Imamura, Tatsuhisa Yasaka, Hiroshi Tanabe, Akinori Iwashita, Toshiharu Ueki
- Clin Endosc 2021;54(4):570-577. Published online January 13, 2021
- DOI: https://doi.org/10.5946/ce.2020.205
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: A white substance that is opaque to endoscopic light is sometimes observed in the epithelium during narrowband imaging with magnifying endoscopy of gastric or colorectal epithelial neoplasms. This prospective observational study aimed to determine whether the morphology of the white opaque substance (WOS) allows differential diagnosis between colorectal adenoma and carcinoma.
Methods
A consecutive series of patients with colorectal adenomas or early carcinomas who underwent endoscopic resection or surgical excision were studied. The morphology of the WOS was determined based on endoscopic images before the histopathological diagnosis was performed. The primary outcome was the diagnostic performance of an irregular WOS as a marker of colorectal carcinoma.
Results
The study analyzed 125 lesions. A total of 33 lesions showed an irregular WOS, and 92 lesions showed a regular WOS. Among the 33 lesions found to show an irregular WOS, 30 were carcinomas. Among the 92 lesions showing a regular WOS, 79 were adenomas. With irregular WOS as a marker of carcinoma, the diagnostic accuracy was 87%, sensitivity was 91%, and specificity was 86%.
Conclusions
This study demonstrated the potential usefulness of the morphology of the WOS as a marker for the differential diagnosis between adenoma and carcinoma in cases of colorectal epithelial neoplasms. -
Citations
Citations to this article as recorded by- Emergence of a New Optical Marker for Colorectal Neoplasms: To What Extent Should We Accept It?
Han Hee Lee
Clinical Endoscopy.2022; 55(2): 315. CrossRef
- Emergence of a New Optical Marker for Colorectal Neoplasms: To What Extent Should We Accept It?
- 4,090 View
- 106 Download
- 1 Web of Science
- 1 Crossref

- Comparative Study of Narrow-Band Imaging and i-scan for Predicting the Histology of Intermediate-to-Large Colorectal Polyps: A Prospective, Randomized Pilot Study
- Joon Seop Lee, Seong Woo Jeon, Yong Hwan Kwon
- Clin Endosc 2021;54(6):881-887. Published online January 6, 2021
- DOI: https://doi.org/10.5946/ce.2020.257
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: To date, no reports have compared the diagnostic efficacy of narrow-band imaging (NBI) and i-scan for the histologic prediction of intermediate-to-large colorectal polyps. We aimed to compare the diagnostic accuracy of NBI and i-scan in predicting histology, and their inter-/intra-observer agreement.
Methods
We performed a prospective, randomized study that included 66 patients (NBI, n=33 vs. i-scan, n=33) with colorectal polyps (size >10 mm but <50 mm) who underwent colonoscopic resection. During the procedure, three endoscopists documented their prediction using the Japan NBI Expert Team (JNET) classification. Two months after study completion, the endoscopists reviewed still images and video clips for analysis.
Results
The overall diagnostic accuracies in the NBI and i-scan groups were 73.7% (73/99) and 75.8% (75/99), respectively, and there was no statistical significance between the two groups (p=0.744). The JNET classification as applied to NBI and i-scan showed substantial inter-observer agreement (NBI κ-value 0.612, p=0.001 vs. i-scan κ-value 0.662, p=0.002). Additionally, the κ-values of intra-observer agreement were in the range of 0.385–0.660 with NBI and 0.364–0.741 with i-scan.
Conclusions
NBI and i-scan have similar diagnostic accuracies for the histologic prediction of intermediate-to-large colorectal polyps. Furthermore, the inter-/intra-observer agreement was acceptable for both modalities when the JNET classification was applied. -
Citations
Citations to this article as recorded by- Ultra-minimally invasive endoscopic techniques and colorectal diseases: Current status and its future
Nalini Kanta Ghosh, Ashok Kumar
Artificial Intelligence in Gastrointestinal Endoscopy.2024;[Epub] CrossRef - The Utility of Narrow-Band Imaging International Colorectal Endoscopic Classification in Predicting the Histologies of Diminutive Colorectal Polyps Using I-Scan Optical Enhancement: A Prospective Study
Yeo Wool Kang, Jong Hoon Lee, Jong Yoon Lee
Diagnostics.2023; 13(16): 2720. CrossRef - Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
Mizuki Nagai, Sho Suzuki, Yohei Minato, Fumiaki Ishibashi, Kentaro Mochida, Ken Ohata, Tetsuo Morishita
Clinical Endoscopy.2023; 56(5): 553. CrossRef - Classification and endoscopic diagnosis of colorectal polyps
Ji Hyun Kim, Sung Chul Park
Journal of the Korean Medical Association.2023; 66(11): 633. CrossRef - Usefulness of optical enhancement endoscopy combined with magnification to improve detection of intestinal metaplasia in the stomach
Sergio Sobrino-Cossío, Oscar Teramoto-Matsubara, Fabian Emura, Raúl Araya, Vítor Arantes, Elymir S. Galvis-García, Marisi Meza-Caballero, Blanca Sinahi García-Aguilar, Arturo Reding-Bernal, Noriya Uedo
Endoscopy International Open.2022; 10(04): E441. CrossRef - Interventions to improve adenoma detection rates for colonoscopy
Aasma Shaukat, Anne Tuskey, Vijaya L. Rao, Jason A. Dominitz, M. Hassan Murad, Rajesh N. Keswani, Fateh Bazerbachi, Lukejohn W. Day
Gastrointestinal Endoscopy.2022; 96(2): 171. CrossRef - A modified fujinon intelligent color enhancement (FICE) in the diagnostics of superficial epithelial neoplasms of the colon
V. A. Duvanskiy, A. V. Belkov
Experimental and Clinical Gastroenterology.2022; (5): 154. CrossRef - Mucosal imaging in colon polyps: New advances and what the future may hold
Edward John Young, Arvinf Rajandran, Hamish Lachlan Philpott, Dharshan Sathananthan, Sophie Fenella Hoile, Rajvinder Singh
World Journal of Gastroenterology.2022; 28(47): 6632. CrossRef - Commentary on “Comparative Study of Narrow-Band Imaging and i-scan for Predicting the Histology of Intermediate-to-Large Colorectal Polyps: A Prospective, Randomized Pilot Study”
Yunho Jung, Masayuki Kato
Clinical Endoscopy.2021; 54(6): 781. CrossRef
- Ultra-minimally invasive endoscopic techniques and colorectal diseases: Current status and its future
- 4,427 View
- 145 Download
- 8 Web of Science
- 9 Crossref

Focused Review Series: Endoscopic Ultrasound-Guided Therapeutic Intervention: Focus on Technique and Practical Tips
- Endoscopic Ultrasound-Guided Local Therapy for Pancreatic Neoplasms
- Jun Seong Hwang, Hyun Don Joo, Tae Jun Song
- Clin Endosc 2020;53(5):535-540. Published online September 29, 2020
- DOI: https://doi.org/10.5946/ce.2020.181
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Surgical resection is considered the only treatment option for pancreatic cancer and other pancreatic neoplasms with malignant potential, such as neuroendocrine tumors, mucinous cystic neoplasms, and intraductal papillary mucinous neoplasms. However, only 10%–20% of all patients with pancreatic cancer present with resectable forms of the disease as the symptoms are rarely manifested during the early stages, and the disease tends to progress rapidly. Furthermore, pancreatic surgery is associated with high rates of morbidity and mortality. The development of linear-array endoscopic ultrasound (EUS) techniques has increased the indications of EUS-guided local therapy for pancreatic neoplasms. We assessed the studies that investigated various treatment modalities, such as fine-needle injection, radiofrequency ablation, irreversible electroporation, and radiotherapy, under EUS guidance to better understand the usefulness of these techniques with respect to the efficacy and associated complications.
-
Citations
Citations to this article as recorded by- Anticancer effect of a pyrrole‐imidazole polyamide‐triphenylphosphonium conjugate selectively targeting a common mitochondrial DNA cancer risk variant in cervical cancer cells
Jihang Yao, Keizo Takenaga, Nobuko Koshikawa, Yuki Kida, Jason Lin, Takayoshi Watanabe, Yoshiaki Maru, Yoshitaka Hippo, Seigi Yamamoto, Yuyan Zhu, Hiroki Nagase
International Journal of Cancer.2023; 152(5): 962. CrossRef - Endoscopic Ultrasound-Guided Local Ablative Therapies for the Treatment of Pancreatic Neuroendocrine Tumors and Cystic Lesions: A Review of the Current Literature
Alexander M. Prete, Tamas A. Gonda
Journal of Clinical Medicine.2023; 12(9): 3325. CrossRef - Response of Locally Advanced Pancreatic Cancer to Intratumoral Injection of Large Surface Area Microparticle Paclitaxel
Neil R. Sharma, Simon K. Lo, Andrew Hendifar, Mohamed O. Othman, Kalpesh Patel, Antonio Mendoza-Ladd, Shelagh Verco, Holly A. Maulhardt, James Verco, Alison Wendt, Alyson Marin, Christian Max Schmidt, Gere diZerega
Pancreas.2023; 52(3): e179. CrossRef - Multisite Is Superior to Single-Site Intratumoral Chemotherapy to Retard the Outcomes of Pancreatic Ductal Adenocarcinoma in a Murine Model
Janette Lazarovits, Ron Epelbaum, Jesse Lachter, Yaron Amikam, Jacob Ben Arie
Cancers.2023; 15(24): 5801. CrossRef - Endoscopic ultrasound-guided injectable therapy for pancreatic cancer: A systematic review
Jyotroop Kaur, Veeravich Jaruvongvanich, Vinay Chandrasekhara
World Journal of Gastroenterology.2022; 28(21): 2383. CrossRef
- Anticancer effect of a pyrrole‐imidazole polyamide‐triphenylphosphonium conjugate selectively targeting a common mitochondrial DNA cancer risk variant in cervical cancer cells
- 4,270 View
- 148 Download
- 5 Web of Science
- 5 Crossref

Original Article
- Endoscopic Ultrasound-Guided Random Omental Fine Needle Aspiration: A Novel Technique for the Diagnosis of Peritoneal Carcinomatosis
- Pradeep Kumar Siddappa, Neha Jain, Naveen K. Agarwal, Monika Jain, Gurwant Singh Lamba
- Clin Endosc 2020;53(5):594-599. Published online September 29, 2020
- DOI: https://doi.org/10.5946/ce.2019.175
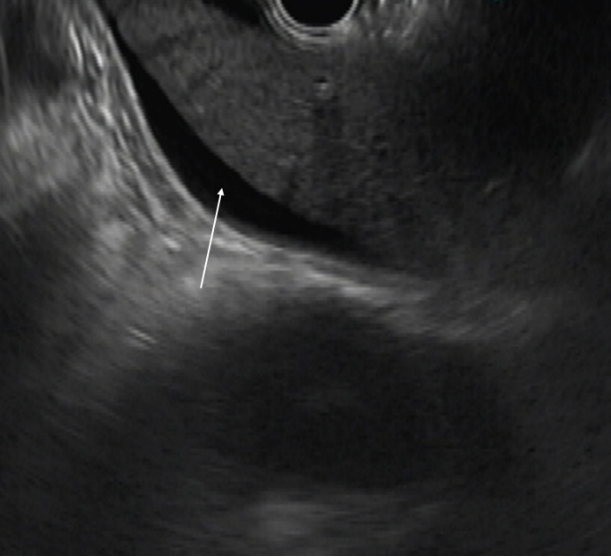
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Diagnostic abdominal paracentesis has been described in literature to have variable sensitivity of 50%–75% for the detection of peritoneal carcinomatosis (PC). We believe that random needle aspirates from the omentum, even in the absence of obvious deposits by endoscopic ultrasound (EUS), could prove malignancy in patients with PC.
Methods
Consecutive patients who underwent EUS for diagnosis and staging of cancer and found to have ascites were included after obtaining informed consent. EUS-guided fine needle aspiration (EUS-FNA) from random sites in the omentum was performed through the transgastric route using a linear echoendoscope.
Results
Fifty-four patients underwent EUS during October 2015 to April 2017 for detection, staging, or FNA of a suspected malignant lesion. Ascites was seen in 17 patients and 15 patients who fulfilled the criteria were included. The procedure was successful in all patients. Cytology was suggestive of malignancy in 12 (80%) but not suggestive of malignancy in 3 (20%) patients. Three patients who tested negative had hyperbilirubinemia with biliary obstruction. Their ascitic fluid analysis result was also negative.
Conclusions
Random FNA of the omentum in patients with malignancy-related ascites is highly effective in the diagnosis of PC and could be employed during EUS evaluation of malignancies. -
Citations
Citations to this article as recorded by- Role of Endoscopic Ultrasound in Diagnosis of Pancreatic Ductal Adenocarcinoma
Abhirup Chatterjee, Jimil Shah
Diagnostics.2023; 14(1): 78. CrossRef
- Role of Endoscopic Ultrasound in Diagnosis of Pancreatic Ductal Adenocarcinoma
- 3,925 View
- 73 Download
- 1 Web of Science
- 1 Crossref


 KSGE
KSGE


 First
First Prev
Prev



