Search
- Page Path
- HOME > Search
Original Articles
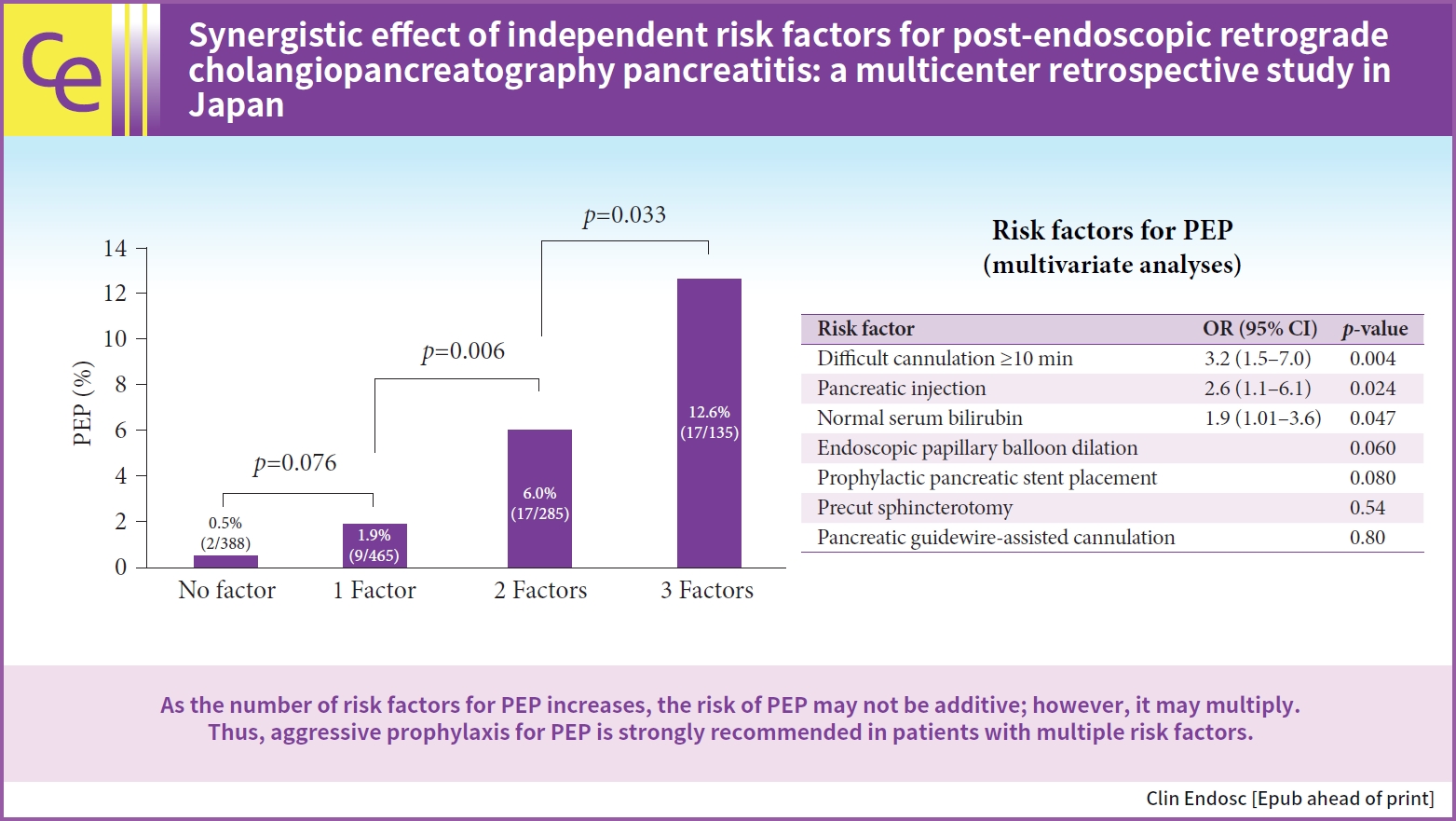
- Synergistic effect of independent risk factors for post-endoscopic retrograde cholangiopancreatography pancreatitis: a multicenter retrospective study in Japan
- Hirokazu Saito, Yoshihiro Kadono, Takashi Shono, Kentaro Kamikawa, Atsushi Urata, Jiro Nasu, Masayoshi Uehara, Ikuo Matsushita, Tatsuyuki Kakuma, Shunpei Hashigo, Shuji Tada
- Received August 14, 2023 Accepted October 10, 2023 Published online April 18, 2024
- DOI: https://doi.org/10.5946/ce.2023.203 [Epub ahead of print]
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: This study aimed to examine the synergistic effect of independent risk factors on post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP).
Methods
This multicenter retrospective study included 1,273 patients with native papillae who underwent ERCP for bile dust stones in Japan. Independent PEP risk factors were identified using univariate and multivariate analyses. Significant risk factors for PEP in the multivariate analysis were included in the final analysis to examine the synergistic effect of independent risk factors for PEP.
Results
PEP occurred in 45 of 1,273 patients (3.5%). Three factors including difficult cannulation ≥10 minutes, pancreatic injection, and normal serum bilirubin level were included in the final analysis. The incidences of PEP in patients with zero, one, two, and three factors were 0.5% (2/388), 1.9% (9/465), 6.0% (17/285), and 12.6% (17/135), respectively. With increasing risk factors for PEP, the incidence of PEP significantly increased (1 factor vs. 2 factors, p=0.006; 2 factors vs. 3 factors, p=0.033).
Conclusions
As the number of risk factors for PEP increases, the risk of PEP may not be additive; however, it may multiply. Thus, aggressive prophylaxis for PEP is strongly recommended in patients with multiple risk factors.
- 2,179 View
- 50 Download

- Double-guidewire technique for selective biliary cannulation does not increase the rate of post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with naïve papilla
- Han Taek Jeong, June Hwa Bae, Ho Gak Kim, Jimin Han
- Clin Endosc 2024;57(2):226-236. Published online January 26, 2024
- DOI: https://doi.org/10.5946/ce.2023.128

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: This study aimed to compare the safety of the double-guidewire technique (DGT) with that of the conventional single-guidewire technique (SGT) in real-world situations.
Methods
A total of 240 patients with naïve papilla who underwent endoscopic retrograde cholangiopancreatography (ERCP) at Daegu Catholic University Medical Center between January 2021 and December 2021 were included. The primary outcome was the rate of post-ERCP pancreatitis (PEP) in the SGT and DGT groups.
Results
A total of 163 patients (67.9%) belonged to the SGT group, and 77 (32.1%) belonged to the DGT group. The rates of successful biliary cannulation were 95.7% and 83.1% in the SGT and DGT groups, respectively (p=0.002). In the study group, PEP occurred in 14 patients (5.8%). The PEP rates were not significantly different between the SGT and DGT groups (4.3% vs. 9.1%, p=0.150). In the multivariate analysis, the age of <50 years (odds ratio [OR], 9.305; 95% confidence interval [CI], 1.367–63.358; p=0.023) and hyperlipidemia (OR, 7.384; 95% CI, 1.103–49.424; p=0.039) were significant risk factors for PEP in the DGT group.
Conclusions
DGT did not increase the PEP rate in patients with naïve papilla. In addition, the age of <50 years and hyperlipidemia were significant risk factors for PEP in the DGT group.
- 3,767 View
- 160 Download

Review
-
Endoscopic retrograde cholangiopancreatography-related complications: risk stratification, prevention, and management

- Clement Chun Ho Wu, Samuel Jun Ming Lim, Christopher Jen Lock Khor
- Clin Endosc 2023;56(4):433-445. Published online July 17, 2023
- DOI: https://doi.org/10.5946/ce.2023.013
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) plays a crucial role in the management of pancreaticobiliary disorders. Although the ERCP technique has been refined over the past five decades, it remains one of the endoscopic procedures with the highest rate of complications. Risk factors for ERCP-related complications are broadly classified into patient-, procedure-, and operator-related risk factors. Although non-modifiable, patient-related risk factors allow for the closer monitoring and instatement of preventive measures. Post-ERCP pancreatitis is the most common complication of ERCP. Risk reduction strategies include intravenous hydration, rectal nonsteroidal anti-inflammatory drugs, and pancreatic stent placement in selected patients. Perforation is associated with significant morbidity and mortality, and prompt recognition and treatment of ERCP-related perforations are key to ensuring good clinical outcomes. Endoscopy plays an expanding role in the treatment of perforations. Specific management strategies depend on the location of the perforation and the patient’s clinical status. The risk of post-ERCP bleeding can be attenuated by preprocedural optimization and adoption of intra-procedural techniques. Endoscopic measures are the mainstay of management for post-ERCP bleeding. Escalation to angioembolization or surgery may be required for refractory bleeding. Post-ERCP cholangitis can be reduced with antibiotic prophylaxis in high risk patients. Bile culture-directed therapy plays an important role in antimicrobial treatment.
-
Citations
Citations to this article as recorded by- Prevention of post-ERCP complications
Lotfi Triki, Andrea Tringali, Marianna Arvanitakis, Tommaso Schepis
Best Practice & Research Clinical Gastroenterology.2024; 69: 101906. CrossRef - International Digestive Endoscopy Network consensus on the management of antithrombotic agents in patients undergoing gastrointestinal endoscopy
Seung Joo Kang, Chung Hyun Tae, Chang Seok Bang, Cheol Min Shin, Young-Hoon Jeong, Miyoung Choi, Joo Ha Hwang, Yutaka Saito, Philip Wai Yan Chiu, Rungsun Rerknimitr, Christopher Khor, Vu Van Khien, Kee Don Choi, Ki-Nam Shim, Geun Am Song, Oh Young Lee
Clinical Endoscopy.2024; 57(2): 141. CrossRef - Double-guidewire technique for selective biliary cannulation does not increase the rate of post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with naïve papilla
Han Taek Jeong, June Hwa Bae, Ho Gak Kim, Jimin Han
Clinical Endoscopy.2024; 57(2): 226. CrossRef - Could assessment of genetic susceptibility be an effective solution to prevent pancreatitis from occurring after endoscopic retrograde cholangiopancreatography?
Jae Min Lee
The Korean Journal of Internal Medicine.2023; 38(6): 783. CrossRef
- Prevention of post-ERCP complications
- 3,242 View
- 311 Download
- 3 Web of Science
- 4 Crossref

Original Article
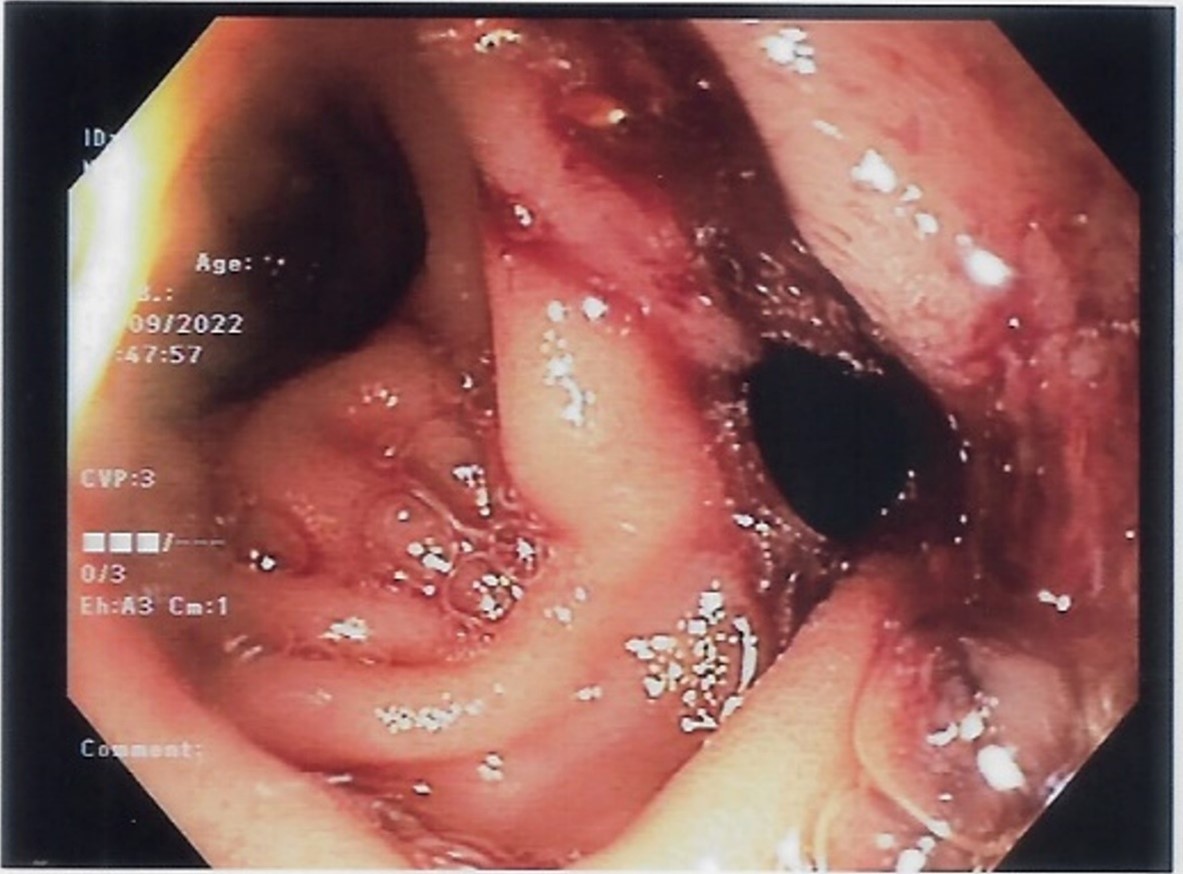
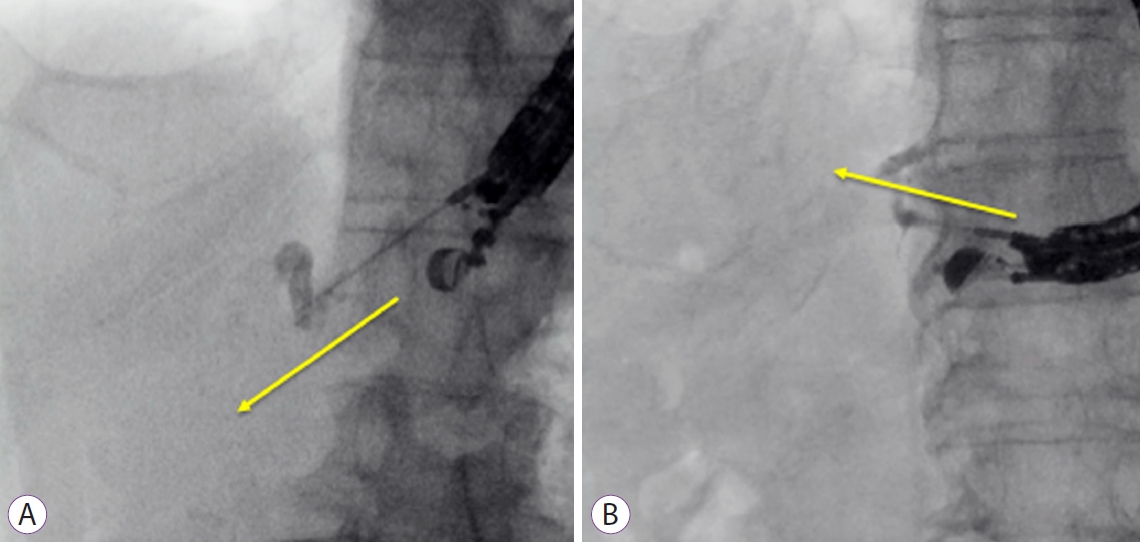
- Risk factors for recurrent stenosis after balloon dilation for benign hepaticojejunostomy anastomotic stricture
- Takafumi Mie, Takashi Sasaki, Takeshi Okamoto, Tsuyoshi Takeda, Chinatsu Mori, Yuto Yamada, Takaaki Furukawa, Akiyoshi Kasuga, Masato Matsuyama, Masato Ozaka, Naoki Sasahira
- Clin Endosc 2024;57(2):253-262. Published online May 16, 2023
- DOI: https://doi.org/10.5946/ce.2022.216
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 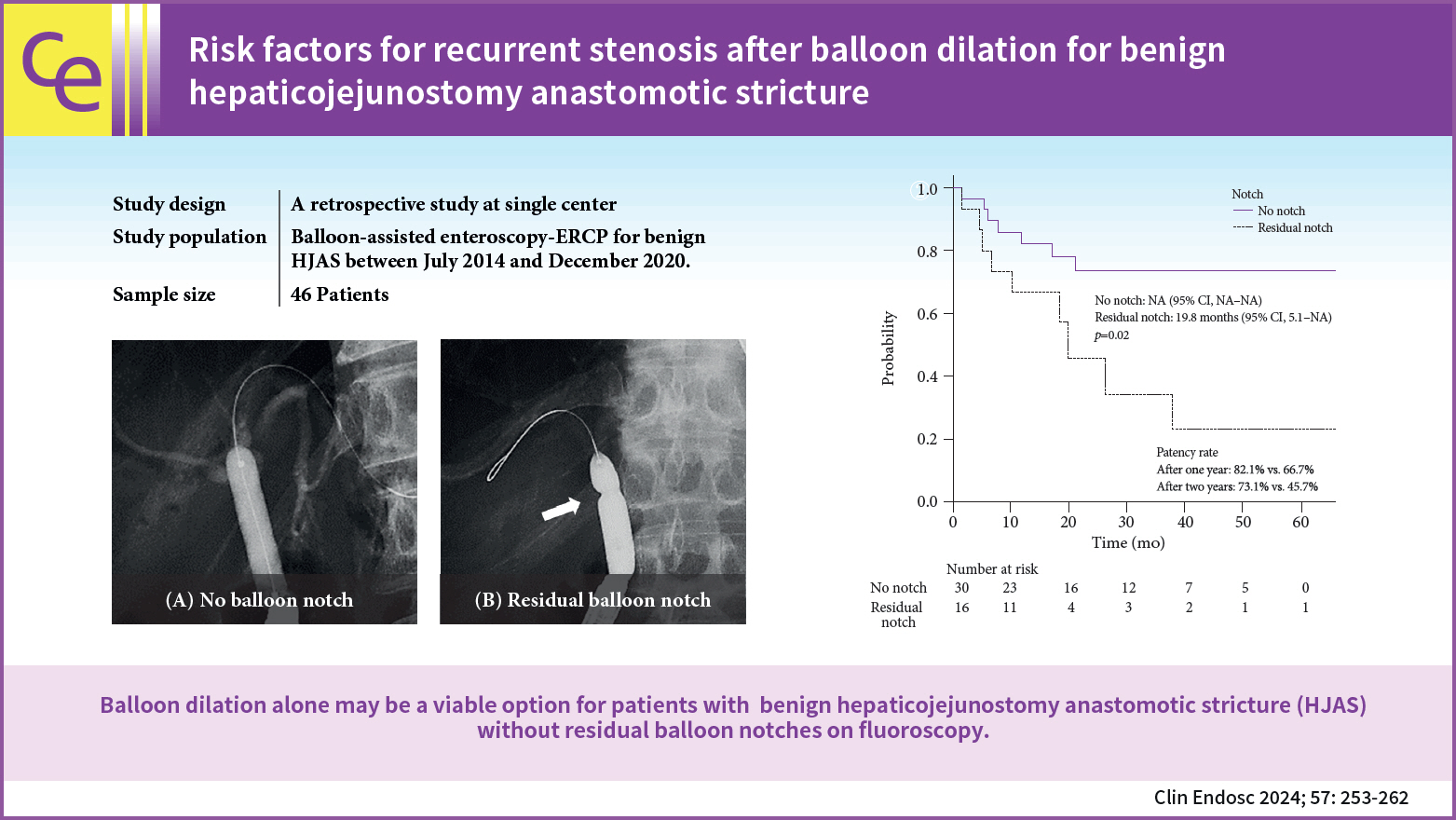
- Background
/Aims: Hepaticojejunostomy anastomotic stricture (HJAS) is a feared adverse event associated with hepatopancreatobiliary surgery. Although balloon dilation for benign HJAS during endoscopic retrograde cholangiopancreatography with balloon-assisted enteroscopy has been reported to be useful, the treatment strategy remains controversial. Therefore, we evaluated the outcomes and risk factors of recurrent stenosis after balloon dilation alone for benign HJAS.
Methods
We retrospectively analyzed consecutive patients who underwent balloon-assisted enteroscopy–endoscopic retrograde cholangiopancreatography for benign HJAS at our institution between July 2014 and December 2020.
Results
Forty-six patients were included, 16 of whom had recurrent HJAS after balloon dilation. The patency rates at 1 and 2 years after balloon dilation were 76.8% and 64.2%, respectively. Presence of a residual balloon notch during balloon dilation was an independent predictor of recurrence (hazard ratio, 2.80; 95% confidence interval, 1.01–7.78; p=0.048), whereas HJAS within postoperative 1 year tended to be associated with recurrence (hazard ratio, 2.43; 95% confidence interval, 0.85–6.89; p=0.096). The patency rates in patients without a residual balloon notch were 82.1% and 73.1% after 1 and 2 years, respectively.
Conclusions
Balloon dilation alone may be a viable option for patients with benign HJAS without residual balloon notches on fluoroscopy.
- 2,076 View
- 172 Download
- 1 Web of Science

Systematic Review and Meta-analysis
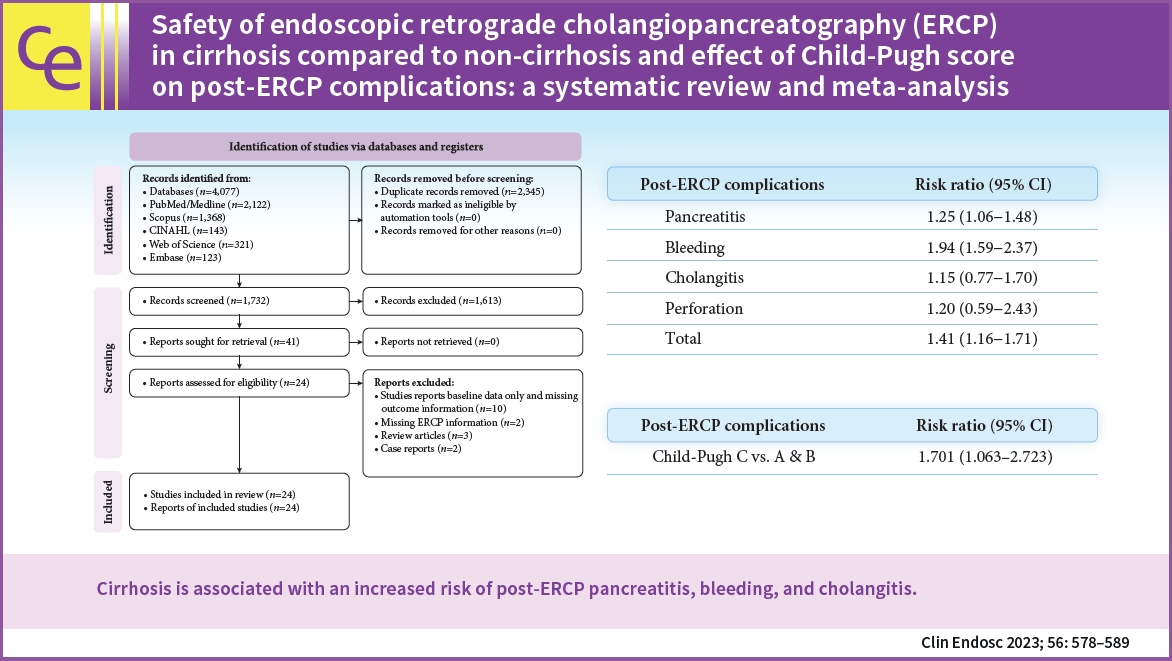
- Safety of endoscopic retrograde cholangiopancreatography (ERCP) in cirrhosis compared to non-cirrhosis and effect of Child-Pugh score on post-ERCP complications: a systematic review and meta-analysis
- Zahid Ijaz Tarar, Umer Farooq, Mustafa Gandhi, Saad Saleem, Ebubekir Daglilar
- Clin Endosc 2023;56(5):578-589. Published online May 2, 2023
- DOI: https://doi.org/10.5946/ce.2023.027
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub 
- Background
/Aims: The safety of endoscopic retrograde cholangiopancreatography (ERCP) in hepatic cirrhosis and the impact of Child-Pugh class on post-ERCP complications need to be better studied. We investigated the post-ERCP complication rates in patients with cirrhosis compared with those without cirrhosis.
Methods
We conducted a literature search of relevant databases to identify studies that reported post-ERCP complications in patients with hepatic cirrhosis.
Results
Twenty-four studies comprising 28,201 patients were included. The pooled incidence of post-ERCP complications in cirrhosis was 15.5% (95% confidence interval [CI], 11.8%–19.2%; I2=96.2%), with an individual pooled incidence of pancreatitis 5.1% (95% CI, 3.1%–7.2%; I2=91.5%), bleeding 3.6% (95% CI, 2.8%–4.5%; I2=67.5%), cholangitis 2.9% (95% CI, 1.9%–3.8%; I2=83.4%), and perforation 0.3% (95% CI, 0.1%–0.5%; I2=3.7%). Patients with cirrhosis had a greater risk of post-ERCP complications (risk ratio [RR], 1.41; 95% CI, 1.16–1.71; I2=56.3%). The risk of individual odds of adverse events between cirrhosis and non-cirrhosis was as follows: pancreatitis (RR, 1.25; 95% CI, 1.06–1.48; I2=24.8%), bleeding (RR, 1.94; 95% CI, 1.59–2.37; I2=0%), cholangitis (RR, 1.15; 95% CI, 0.77–1.70; I2=12%), and perforation (RR, 1.20; 95% CI, 0.59–2.43; I2=0%).
Conclusions
Cirrhosis is associated with an increased risk of post-ERCP pancreatitis, bleeding, and cholangitis. -
Citations
Citations to this article as recorded by- The Impact of Frailty on ERCP-Related Adverse Events: Findings From a National Cohort
Umer Farooq, Zahid Ijaz Tarar, Abdallah El Alayli, Faisal Kamal, Alexander Schlachterman, Anand Kumar, David E. Loren, Thomas E. Kowalski
Techniques and Innovations in Gastrointestinal Endoscopy.2024; 26(2): 138. CrossRef - Applicability of Child-Turcotte-Pugh Score in Anticipating Post-ERCP Adverse Events in Patients With Cirrhosis
Saqr Alsakarneh, Fouad Jaber, Willie Mohammed, Mohammad Almeqdadi, Abdallah Al-Ani, Yassine Kilani, Saeed Abughazaleh, Laith Momani, Muhammad Shah Miran, Hassan Ghoz, John Helzberg, Wendell Clarkston, Mohamed Othman
Journal of Clinical Gastroenterology.2024;[Epub] CrossRef - ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY FOR THE MANAGEMENT OF CHOLEDOCHOLITHIASIS IN OLDER PATIENTS
Júlia Gardenyes, Pere Roura, Helena Vallverdú-Cartie, Judit Hermoso-Bosch, Cl�udia Roca, Mariona Espaulella, Antoni Casals, Héctor Ivo Marani, Joan Saló, Martín Galdín, Marta Gallach, Carles Leal
Revista Española de Enfermedades Digestivas.2023;[Epub] CrossRef
- The Impact of Frailty on ERCP-Related Adverse Events: Findings From a National Cohort
- 2,340 View
- 129 Download
- 2 Web of Science
- 3 Crossref

Original Articles
-
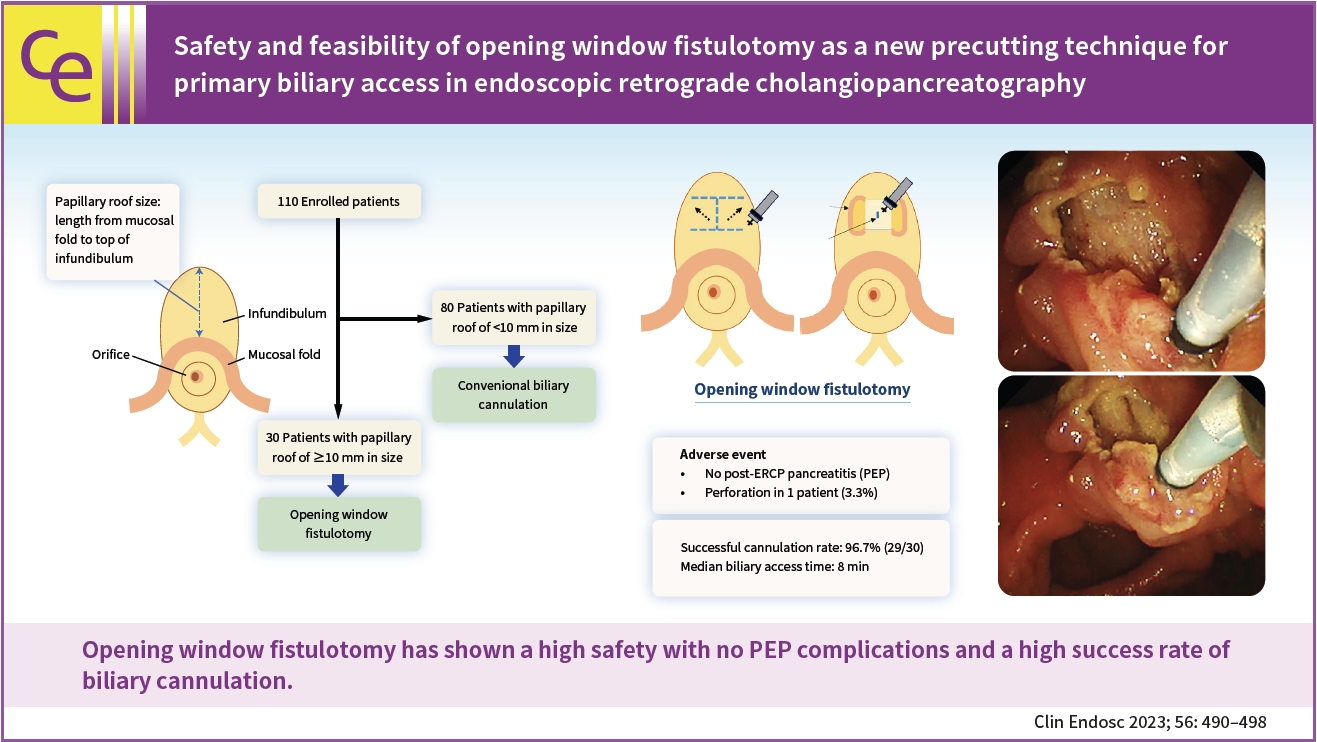
Safety and feasibility of opening window fistulotomy as a new precutting technique for primary biliary access in endoscopic retrograde cholangiopancreatography

- Yasuhiro Kuraishi, Kazuo Hara, Shin Haba, Takamichi Kuwahara, Nozomi Okuno, Takafumi Yanaidani, Sho Ishikawa, Tsukasa Yasuda, Masanori Yamada, Nobumasa Mizuno
- Clin Endosc 2023;56(4):490-498. Published online April 27, 2023
- DOI: https://doi.org/10.5946/ce.2022.130
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub 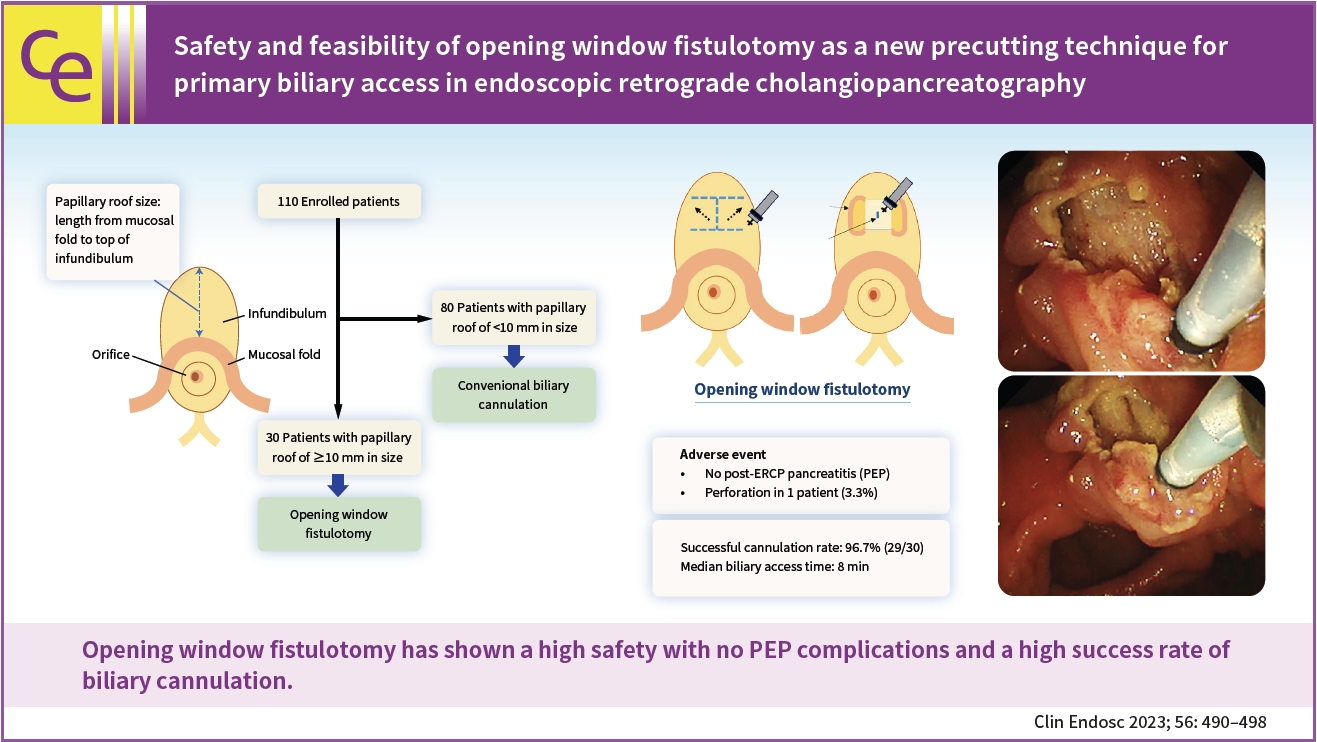
- Background
/Aims: Post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP) is the most common and serious complication of endoscopic retrograde cholangiopancreatography. To prevent this event, a unique precutting method, termed opening window fistulotomy, was performed in patients with a large infundibulum as the primary procedure for biliary cannulation, whereby a suprapapillary laid-down H-shaped incision was made without touching the orifice. This study aimed to assess the safety and feasibility of this novel technique.
Methods
One hundred and ten patients were prospectively enrolled in this study. Patients with a papillary roof size ≥10 mm underwent opening window fistulotomy for primary biliary access. In addition, the incidence of complications and success rate of biliary cannulation were evaluated.
Results
The median size of the papillary roof was 6 mm (range, 3–20 mm). Opening window fistulotomy was performed in 30 patients (27.3%), none of whom displayed PEP. Duodenal perforation was recorded in one patient (3.3%), which was resolved by conservative treatment. The cannulation rate was high (96.7%, 29/30 patients). The median duration of biliary access was 8 minutes (range, 3–15 minutes).
Conclusions
Opening window fistulotomy demonstrated its feasibility for primary biliary access by achieving great safety with no PEP complications and a high success rate for biliary cannulation. -
Citations
Citations to this article as recorded by- Comments on ‘Safety and feasibility of opening window fistulotomy as a new precutting technique for primary biliary access in endoscopic retrograde cholangiopancreatography’
Masood Muhammad Karim, Adeel Ur Rehman, Faisal Wasim Ismail, Om Parkash
Clinical Endoscopy.2024; 57(2): 280. CrossRef
- Comments on ‘Safety and feasibility of opening window fistulotomy as a new precutting technique for primary biliary access in endoscopic retrograde cholangiopancreatography’
- 2,781 View
- 125 Download
- 1 Web of Science
- 1 Crossref

- Outcomes of endoscopic retrograde cholangiopancreatography in patients with situs inversus viscerum
- Long Le, Nicholas McDonald, Anders Westanmo, Mohammad Bilal, Dharma Sunjaya
- Clin Endosc 2023;56(6):790-794. Published online April 26, 2023
- DOI: https://doi.org/10.5946/ce.2022.292

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: Situs inversus viscerum (SIV) is a congenital condition defined by left-to-right transposition of all visceral organs. This anatomical variant has caused technical challenges in endoscopic retrograde cholangiopancreatography (ERCP). Data on ERCP in patients with SIV are limited to case reports of unknown clinical and technical success rates. This study aimed to evaluate the clinical and technical success rates of ERCP in patients with SIV.
Methods
Data from patients with SIV who underwent ERCP were retrospectively reviewed. The data were collected by querying the nationwide Veterans Affairs Health System database for patients diagnosed with SIV who underwent ERCP. Patient demographics and procedural characteristics were collected.
Results
Eight patients with SIV who underwent ERCP were included. Choledocholithiasis was the most common indication for ERCP (62.5%). The technical success rate was 63%. Subsequent ERCP with interventional radiology–assisted rendezvous has increased the technical success rate to 100%. Clinical success was achieved in 63% of cases. Among cases of subsequent rendezvous ERCP after conventional ERCP failure, clinical success was achieved in 100%.
Conclusions
The clinical and technical success rates of ERCP in patients with SIV were both 63%. In patients with SIV in whom ERCP fails, interventional radiology–assisted rendezvous ERCP can be considered. -
Citations
Citations to this article as recorded by- Adaptability in the Midst of Anatomical Challenges: A Case of Situs Inversus Totalis in Laparoscopic Cholecystectomy
Christopher Nguyen, David Schutter
Cureus.2024;[Epub] CrossRef
- Adaptability in the Midst of Anatomical Challenges: A Case of Situs Inversus Totalis in Laparoscopic Cholecystectomy
- 1,441 View
- 103 Download
- 1 Web of Science
- 1 Crossref

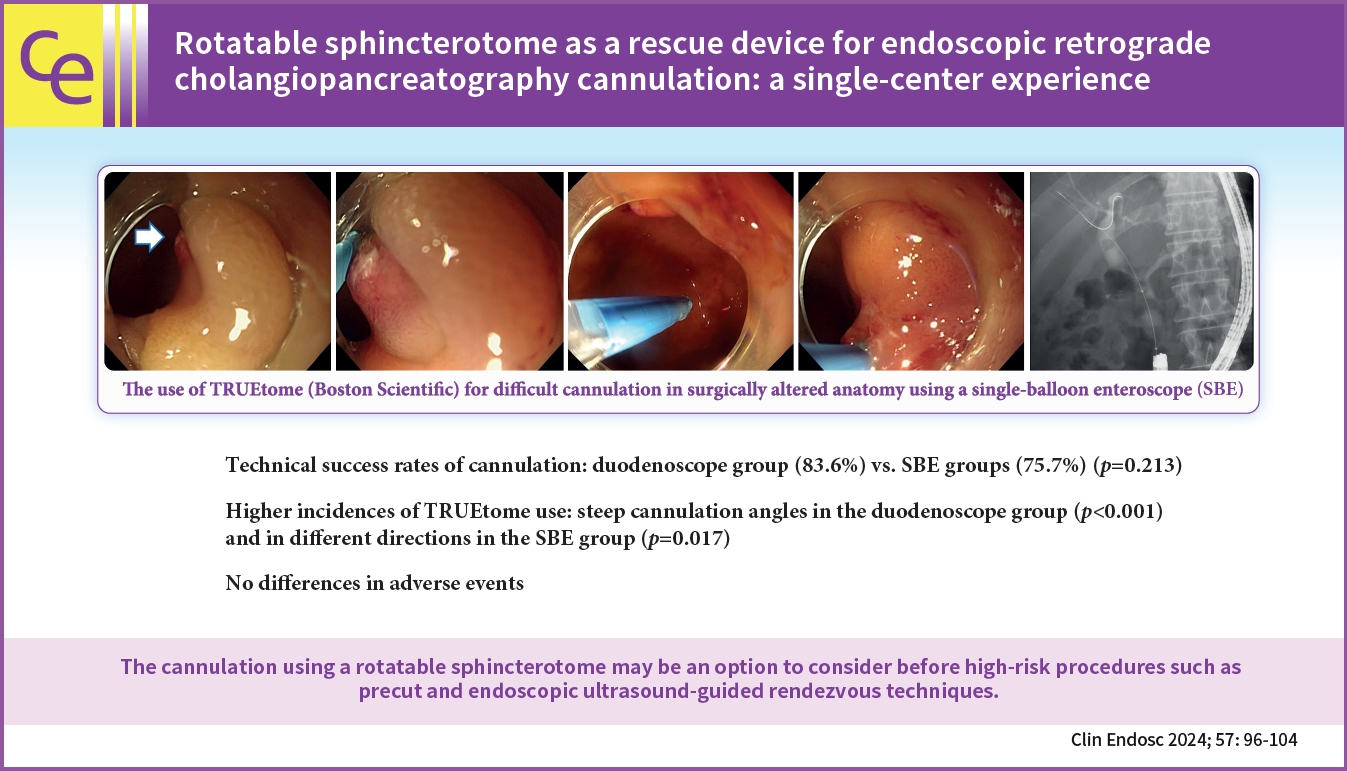
- Rotatable sphincterotome as a rescue device for endoscopic retrograde cholangiopancreatography cannulation: a single-center experience
- Takeshi Okamoto, Takashi Sasaki, Tsuyoshi Takeda, Takafumi Mie, Chinatsu Mori, Takaaki Furukawa, Yuto Yamada, Akiyoshi Kasuga, Masato Matsuyama, Masato Ozaka, Naoki Sasahira
- Clin Endosc 2024;57(1):96-104. Published online April 25, 2023
- DOI: https://doi.org/10.5946/ce.2022.248
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 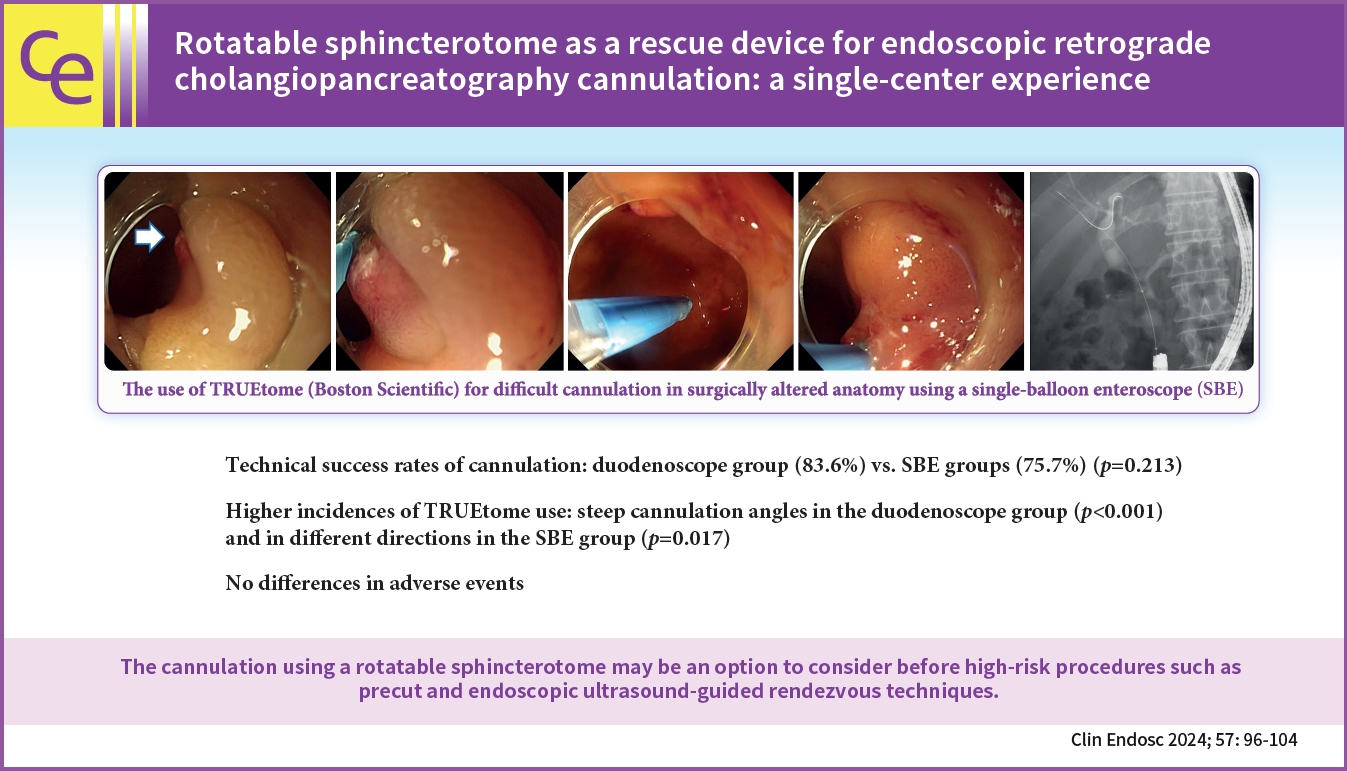
- Background
/Aims: Selective bile duct or pancreatic duct cannulation remains a significant initial hurdle in endoscopic retrograde cholangiopancreatography (ERCP) despite advances in endoscopy and accessories. This study evaluated our experience with a rotatable sphincterotome in cases of difficult cannulation.
Methods
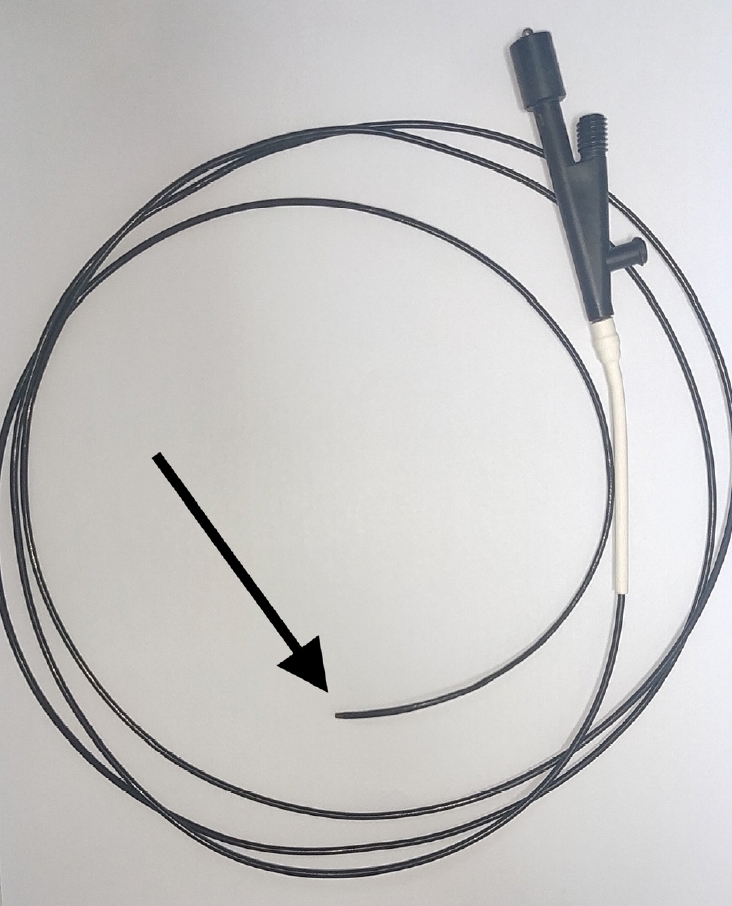
We retrospectively reviewed ERCP cases using TRUEtome, a rotatable sphincterotome, as a rescue device for cannulation at a cancer institute in Japan from October 2014 to December 2021.
Results
TRUEtome was used in 88 patients. Duodenoscopes were used for 51 patients, while single-balloon enteroscopes (SBE) were used for 37 patients. TRUEtome was used for biliary and pancreatic duct cannulation (84.1%), intrahepatic bile duct selection (12.5%), and strictures of the afferent limb (3.4%). Cannulation success rates were similar in the duodenoscope and SBE groups (86.3% vs. 75.7%, p=0.213). TRUEtome was more commonly used in cases with steep cannulation angles in the duodenoscope group and in cases requiring cannulation in different directions in the SBE group. There were no significant differences in adverse events between the two groups.
Conclusions
The cannulation sphincterotome was useful for difficult cannulations in both unaltered and surgically altered anatomies. It may be an option to consider before high-risk procedures such as precut and endoscopic ultrasound-guided rendezvous techniques. -
Citations
Citations to this article as recorded by- Non-tip and rotatable sphincterotome for biliary cannulation in patients with Roux-en-Y gastrectomy
Haruo Miwa, Kazuya Sugimori, Kazuki Endo, Ritsuko Oishi, Hiromi Tsuchiya, Takashi Kaneko, Shin Maeda
Endoscopy.2024; 56(S 01): E103. CrossRef
- Non-tip and rotatable sphincterotome for biliary cannulation in patients with Roux-en-Y gastrectomy
- 2,048 View
- 152 Download
- 1 Crossref

Review
-
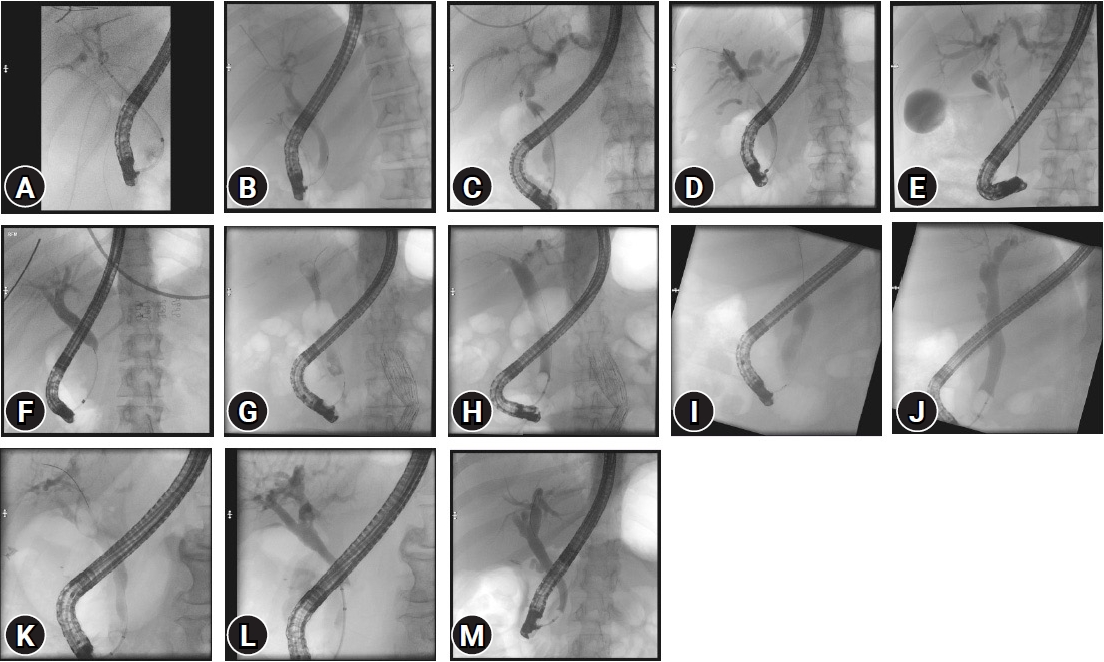
Single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: a technical review

- Yuki Tanisaka, Masafumi Mizuide, Akashi Fujita, Rie Shiomi, Takahiro Shin, Kei Sugimoto, Shomei Ryozawa
- Clin Endosc 2023;56(6):716-725. Published online April 17, 2023
- DOI: https://doi.org/10.5946/ce.2023.023

-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered anatomy is technically challenging. For example, scope insertion, selective cannulation, and intended procedures, such as stone extraction or stent placement, can be difficult. Single-balloon enteroscopy (SBE)-assisted ERCP has been used to effectively and safely address these technical issues in clinical practice. However, the small working channel limits its therapeutic potential. To address this shortcoming, a short-type SBE (short SBE) with a working length of 152 cm and a channel of 3.2 mm diameter has recently been introduced. Short SBE facilitates the use of larger accessories to complete certain procedures, such as stone extraction or self-expandable metallic stent placement. Despite the development in the SBE endoscope, various steps have to be overcome to successfully perform such procedure. To improve success, the challenging factors of each procedure must be identified. At the same time, endoscopists need to be mindful of adverse events, such as perforation, which can arise due to adhesions specific to the surgically altered anatomy. This review discussed technical tips regarding SBE-assisted ERCP in patients with surgically altered anatomy to increase success and reduce the risk of adverse events associated with ERCP.
-
Citations
Citations to this article as recorded by- Advanced technical tips and recent insights in ERCP using balloon‐assisted endoscopy
Masaaki Shimatani, Toshiyuki Mitsuyama, Takeshi Yamashina, Masahiro Takeo, Shunsuke Horitani, Natsuko Saito, Hironao Matsumoto, Masahiro Orino, Masataka Kano, Takafumi Yuba, Takuya Takayama, Tatsuya Nakagawa, Shoji Takayama
DEN Open.2024;[Epub] CrossRef - Efficacy of texture and color enhancement imaging for short‐type single‐balloon enteroscopy‐assisted biliary cannulation in patients with Roux‐en‐Y gastrectomy: Multicenter study (with video)
Yuki Tanisaka, Mamoru Takenaka, Masafumi Mizuide, Akashi Fujita, Ryuhei Jinushi, Takahiro Shin, Kei Sugimoto, Ken Kamata, Kosuke Minaga, Shunsuke Omoto, Tomohiro Yamazaki, Shomei Ryozawa
Digestive Endoscopy.2024;[Epub] CrossRef - Development and evaluation of artificial organ models for ERCP training in patients with surgically altered anatomies
Kai Koch, Benedikt Duckworth-Mothes, Ulrich Schweizer, Karl-Ernst Grund, Tom G. Moreels, Alfred Königsrainer, Dörte Wichmann
Scientific Reports.2023;[Epub] CrossRef
- Advanced technical tips and recent insights in ERCP using balloon‐assisted endoscopy
- 2,599 View
- 333 Download
- 3 Web of Science
- 3 Crossref

Original Articles
- Medical disputes related to advanced endoscopic procedures with endoscopic retrograde cholangiopancreatography or endoscopic ultrasonography for the management of pancreas and biliary tract diseases
- Yoon Suk Lee, Jae-Young Jang, Jun Yong Bae, Eun Hye Oh, Yehyun Park, Yong Hwan Kwon, Jeong Eun Shin, Jun Kyu Lee, Tae Hee Lee, Chang Nyol Paik
- Clin Endosc 2023;56(4):499-509. Published online March 28, 2023
- DOI: https://doi.org/10.5946/ce.2022.208

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub 
- Background
/Aims: This study aimed to evaluate the characteristics of endoscopic retrograde cholangiopancreatography (ERCP) or endoscopic ultrasonography (EUS)-related adverse events (AEs) that eventually lead to medical disputes or claims on medical professional liability.
Methods
Medical disputes for ERCP/EUS-related AEs filed in the Korea Medical Dispute Mediation and Arbitration Agency between April 2012 and August 2020 were evaluated using corresponding medical records. AEs were categorized into three sections: procedure-related, sedation-related, and safety-related AEs.
Results
Among a total of 34 cases, procedure-related AEs were 26 (76.5%; 12 duodenal perforations, 7 post-ERCP pancreatitis, 5 bleedings, 2 perforations combined with post-ERCP pancreatitis); sedation-related AEs were 5 (14.7%; 4 cardiac arrests, 1 desaturation), and safety-related AEs were 5 (8.8%; 1 follow-up loss for stent removal, 1 asphyxia, 1 fall). Regarding clinical outcomes, 20 (58.8%) were fatal and eventually succumbed to AEs. For the types of medical institutions, 21 cases (61.8%) occurred at tertiary or academic hospitals, and 13 (38.2%) occurred at community hospitals.
Conclusions
The ERCP/EUS-related AEs filed in Korea Medical Dispute Mediation and Arbitration Agency showed distinct features: duodenal perforation was the most frequent AE, and clinical outcomes were fatal, resulting in at least more than permanent physical impairment.
- 1,948 View
- 106 Download

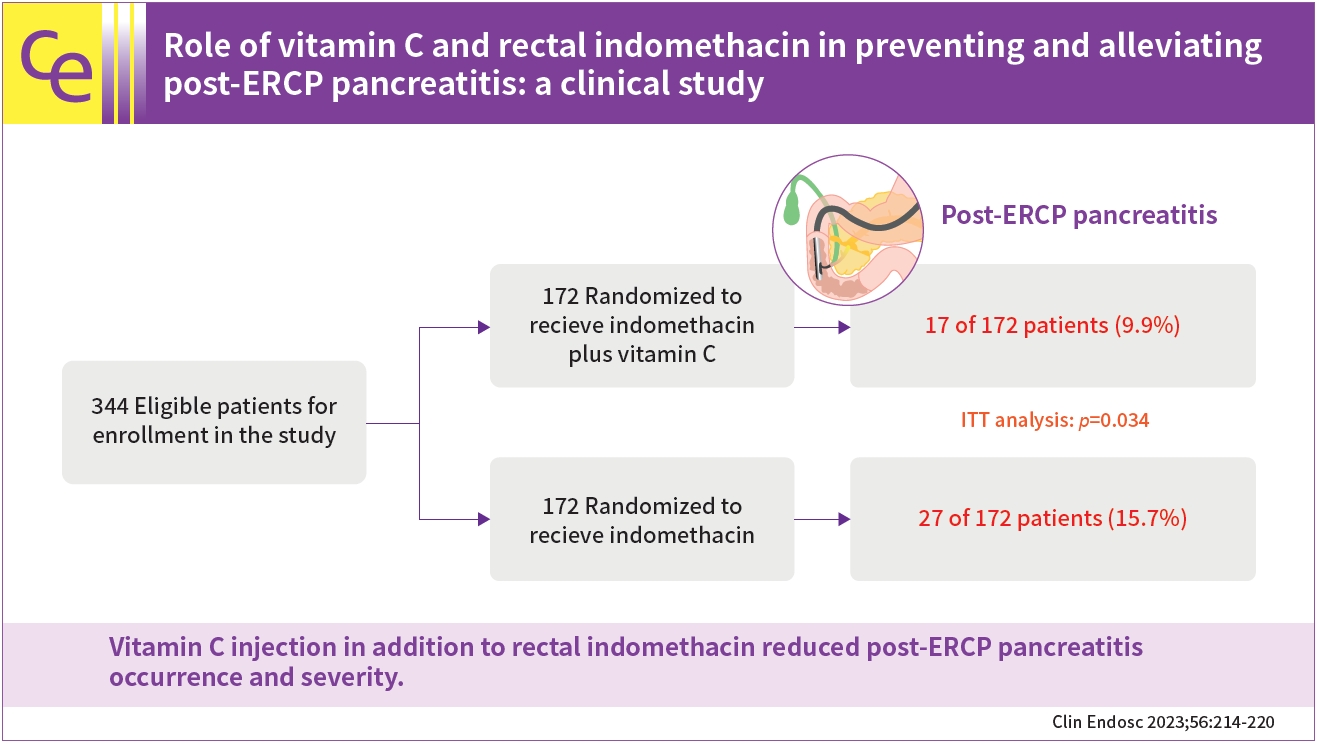
- Role of vitamin C and rectal indomethacin in preventing and alleviating post-endoscopic retrograde cholangiopancreatography pancreatitis: a clinical study
- Amir Sadeghi, Rana Jafari-Moghaddam, Sara Ataei, Mahboobe Asadiafrooz, Mohammad Abbasinazari
- Clin Endosc 2023;56(2):214-220. Published online March 6, 2023
- DOI: https://doi.org/10.5946/ce.2022.165
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 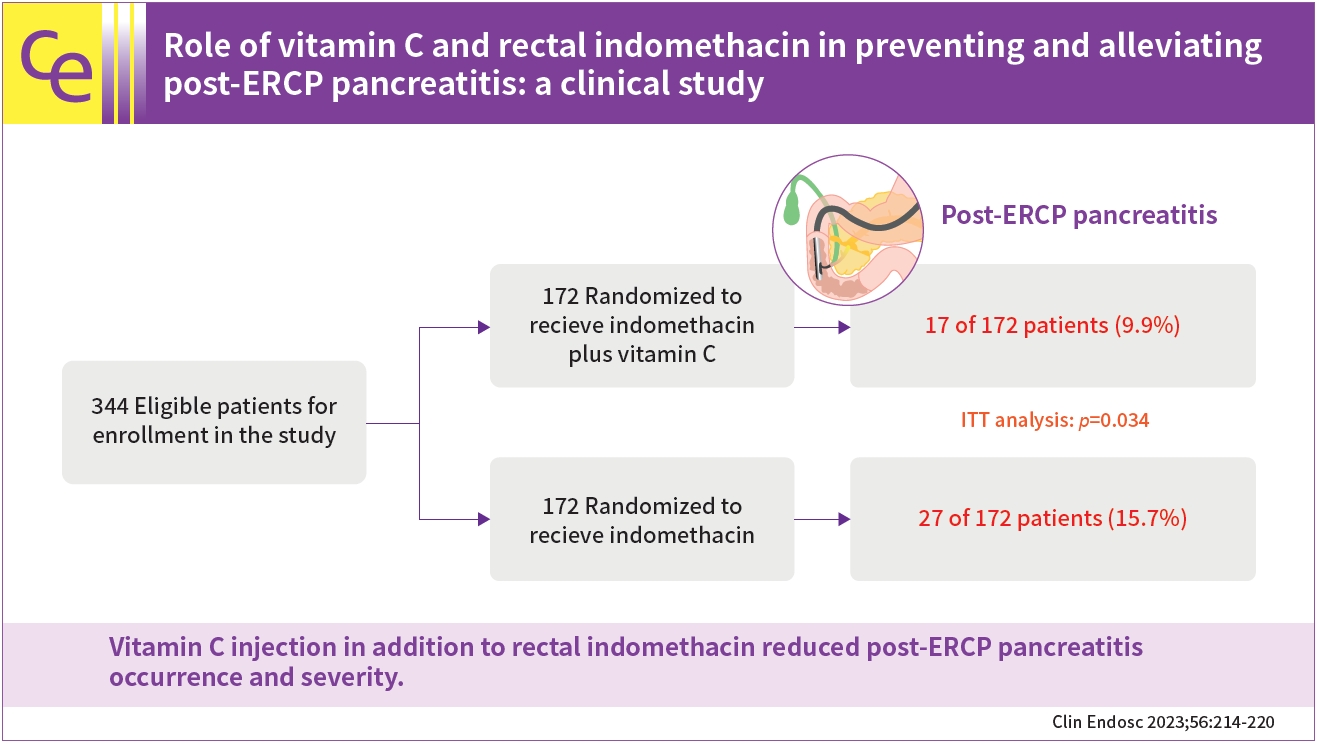
- Background
/Aims: This study aimed to determine whether vitamin C in addition to indomethacin decreases the occurrence and severity of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP) occurrence and severity.
Methods
This randomized clinical trial included patients undergoing ERCP. The participants were administered either rectal indomethacin (100 mg) plus an injection of vitamin C (500 mg) or rectal indomethacin (100 mg) alone just before ERCP. The primary outcomes were PEP occurrence and severity. The secondary amylase and lipase levels were determined after 24 hours.
Results
A total of 344 patients completed the study. Based on intention-to-treat analysis, the PEP rates were 9.9% for indomethacin plus vitamin C plus indomethacin and 15.7% for indomethacin alone. Regarding the per-protocol analysis, the PEP rates were 9.7% and 15.7% in the combination and indomethacin arms, respectively. There was a remarkable difference between the two arms in PEP occurrence and severity on intention-to-treat and per-protocol analyses (p=0.034 and p=0.031, respectively). The post-ERCP lipase and amylase concentrations were lower in the combination arm than in the indomethacin alone arm (p=0.034 and p=0.029, respectively).
Conclusions
Vitamin C injection in addition to rectal indomethacin reduced PEP occurrence and severity. -
Citations
Citations to this article as recorded by- Effect of CoQ10 Addition to Rectal Indomethacin on Clinical Pancreatitis and Related Biomarkers in Post-endoscopic Retrograde Cholangiopancreatography
Saeed Abdi, Roja Qobadighadikolaei, Faezeh Jamali, Maryam Shahrokhi, Farzaneh Dastan, Mohammad Abbasinazari
Journal of Cellular & Molecular Anesthesia.2024;[Epub] CrossRef - Double-guidewire technique for selective biliary cannulation does not increase the rate of post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with naïve papilla
Han Taek Jeong, June Hwa Bae, Ho Gak Kim, Jimin Han
Clinical Endoscopy.2024; 57(2): 226. CrossRef
- Effect of CoQ10 Addition to Rectal Indomethacin on Clinical Pancreatitis and Related Biomarkers in Post-endoscopic Retrograde Cholangiopancreatography
- 1,851 View
- 160 Download
- 1 Web of Science
- 2 Crossref

Reviews
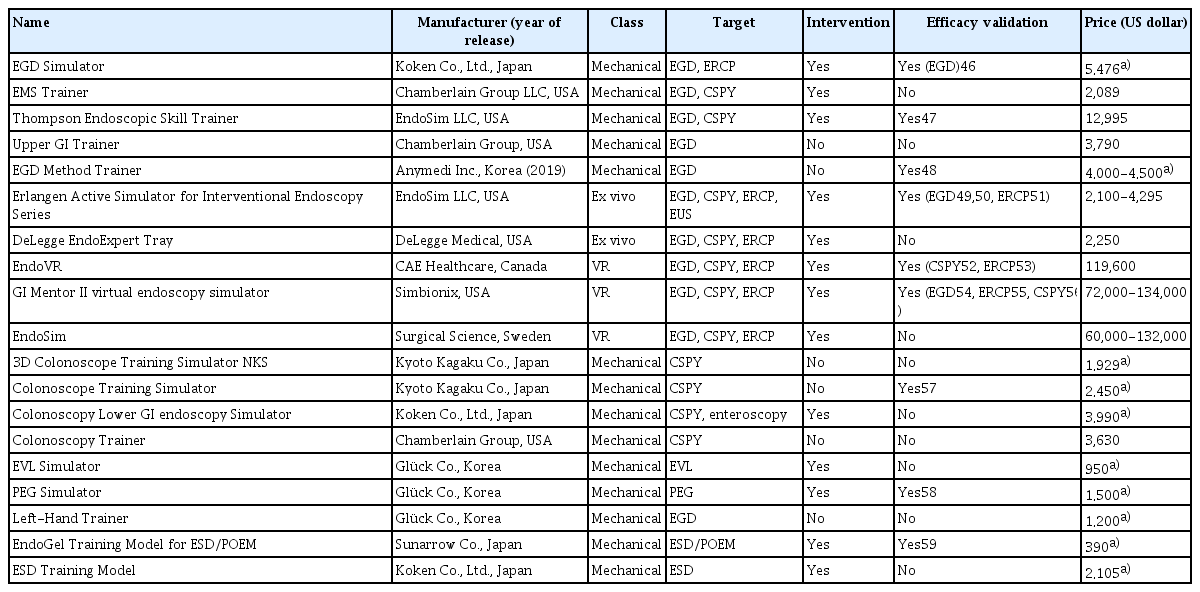
- Simulator-based training method in gastrointestinal endoscopy training and currently available simulators
- Yuri Kim, Jeong Hoon Lee, Gin Hyug Lee, Ga Hee Kim, Gunn Huh, Seung Wook Hong, Hwoon-Yong Jung
- Clin Endosc 2023;56(1):1-13. Published online January 6, 2023
- DOI: https://doi.org/10.5946/ce.2022.191
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The apprenticeship-based training method (ABTM) is highly effective for gastrointestinal (GI) endoscopic training. However, the conventional ABTM has significant issues. Although many supplementary training methods (TMs) have been developed and utilized, they cannot entirely replace the ABTM, which remains the major TM strategy. Currently, new TM construction is crucial and necessary due to financial constraints, difficulty of obtaining sufficient training time due to patient safety-related regulations, and catastrophic damage caused by disasters such as the coronavirus disease 2019 pandemic. The simulator-based TM (SBTM) is widely accepted as an alternative to the ABTM, owing to the SBTM’s advantages. Since the 1960s, many GI endoscopy training simulators have been developed and numerous studies have been published on their effectiveness. While previous studies have focused on the simulator’s validity, this review focused on the accessibility of simulators that were introduced by the end of 2021. Although the current SBTM is effective in GI endoscopic education, extensive improvements are needed to replace the ABTM. Incorporating simulator-incorporated TMs into an improved ABTM is an attempt to overcome the incompleteness of the current SBTM. Until a new simulator is developed to replace the ABTM, it is desirable to operate a simulator-integrated and well-coordinated TM that is suitable for each country and institution.
-
Citations
Citations to this article as recorded by- Impact and assessment of training models in interventional endoscopic ultrasound
Bogdan Miutescu, Vinay Dhir
Digestive Endoscopy.2024; 36(1): 59. CrossRef - A Multicenter Survey of Percutaneous Endoscopic Gastrostomy in 2019 at Korean Medical Institutions
Jun Woo Park, Tae Gyun Kim, Kwang Bum Cho, Jeong Seok Kim, Jin Woong Cho, Jung Won Jeon, Sun Gyo Lim, Chan Gyoo Kim, Hong Jun Park, Tae Jun Kim, Eun Sun Kim, Su Jin Jeong, Yong Hwan Kwon
Gut and Liver.2024; 18(1): 77. CrossRef - Exploring Endoscopic Competence in Gastroenterology Training: A Simulation-Based Comparative Analysis of GAGES, DOPS, and ACE Assessment Tools
Faisal Wasim Ismail, Azam Afzal, Rafia Durrani, Rayyan Qureshi, Safia Awan, Michelle R Brown
Advances in Medical Education and Practice.2024; Volume 15: 75. CrossRef - Assemblage of a functional and versatile endoscopy trainer reusing medical waste: Step‐by‐step video tutorial
Riccardo Vasapolli, Jörg Schirra, Christian Schulz
Digestive Endoscopy.2024; 36(5): 634. CrossRef - Navigating the learning landscape: Comprehensive training in third space endoscopy - training, techniques, and practical recommendations
D. Roser, S. Nagl, A. Ebigbo
Best Practice & Research Clinical Gastroenterology.2024; : 101918. CrossRef - EUS and ERCP training in Europe: Time for simulation, optimization, and standardization
Selma J. Lekkerkerker, Rogier P. Voermans
United European Gastroenterology Journal.2023; 11(5): 407. CrossRef - There is no royal road: a shortcut for endoscopic submucosal dissection training
Seong Woo Jeon
Clinical Endoscopy.2023; 56(5): 590. CrossRef - Enhancing the Quality of Upper Gastrointestinal Endoscopy: Current Indicators and Future Trends
Caesar Ferrari, Micheal Tadros
Gastroenterology Insights.2023; 15(1): 1. CrossRef
- Impact and assessment of training models in interventional endoscopic ultrasound
- 2,795 View
- 215 Download
- 7 Web of Science
- 8 Crossref

- Optimal endoscopic drainage strategy for unresectable malignant hilar biliary obstruction
- Itaru Naitoh, Tadahisa Inoue
- Clin Endosc 2023;56(2):135-142. Published online January 5, 2023
- DOI: https://doi.org/10.5946/ce.2022.150

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic biliary drainage strategies for managing unresectable malignant hilar biliary obstruction differ in terms of stent type, drainage area, and deployment method. However, the optimal endoscopic drainage strategy remains unclear. Uncovered self-expandable metal stents (SEMS) are the preferred type because of their higher functional success rate, longer time to recurrent biliary obstruction (RBO), and fewer cases of reintervention than plastic stents (PS). Other PS subtypes and covered SEMS, which feature a longer time to RBO than PS, can be removed during reintervention for RBO. Bilateral SEMS placement is associated with a longer time to RBO and a longer survival time than unilateral SEMS placement. Unilateral drainage is acceptable if a drainage volume of greater than 50% of the total liver volume can be achieved. In terms of deployment method, no differences were observed in clinical outcomes between side-by-side (SBS) and stent-in-stent deployment. Simultaneous SBS boasts a shorter procedure time and higher technical success rate than sequential SBS. This review of previous studies aimed to clarify the optimal endoscopic biliary drainage strategy for unresectable malignant hilar biliary obstruction.
-
Citations
Citations to this article as recorded by- Comparison of unilateral and bilateral intraductal plastic stent placement for unresectable malignant hilar biliary obstruction: A propensity score‐matched cohort analysis
Mitsuru Okuno, Keisuke Iwata, Tsuyoshi Mukai, Yuhei Iwasa, Shinya Uemura, Kensaku Yoshida, Akinori Maruta, Takuji Iwashita, Ichiro Yasuda, Masahito Shimizu
Journal of Hepato-Biliary-Pancreatic Sciences.2024; 31(4): 284. CrossRef - Preoperative endoscopic biliary drainage by metal versus plastic stents for resectable perihilar cholangiocarcinoma
David M. de Jong, Timothy M. Gilbert, Lynn E. Nooijen, Eva Braunwarth, Marijana Ninkovic, Florian Primavesi, Hassan Z. Malik, Nick Stern, Richard Sturgess, Joris I. Erdmann, Rogier P. Voermans, Marco J. Bruno, Bas Groot Koerkamp, Lydi M.J.W. van Driel
Gastrointestinal Endoscopy.2024; 99(4): 566. CrossRef - TOKYO criteria 2024 for the assessment of clinical outcomes of endoscopic biliary drainage
Hiroyuki Isayama, Tsuyoshi Hamada, Toshio Fujisawa, Mitsuharu Fukasawa, Kazuo Hara, Atsushi Irisawa, Shigeto Ishii, Ken Ito, Takao Itoi, Yoshihide Kanno, Akio Katanuma, Hironari Kato, Hiroshi Kawakami, Hirofumi Kawamoto, Masayuki Kitano, Hirofumi Kogure,
Digestive Endoscopy.2024;[Epub] CrossRef - Research progress on biliary stents
Progress in Medical Devices.2023;[Epub] CrossRef
- Comparison of unilateral and bilateral intraductal plastic stent placement for unresectable malignant hilar biliary obstruction: A propensity score‐matched cohort analysis
- 2,996 View
- 320 Download
- 2 Web of Science
- 4 Crossref

Original Article
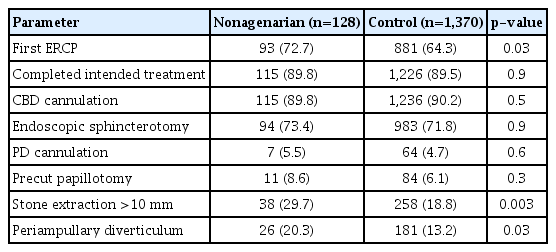
- Endoscopic removal of common bile duct stones in nonagenarians: a tertiary center experience
- Mustafa Jalal, Amaan Khan, Sijjad Ijaz, Mohammed Gariballa, Yasser El-Sherif, Amer Al-Joudeh
- Clin Endosc 2023;56(1):92-99. Published online January 5, 2023
- DOI: https://doi.org/10.5946/ce.2022.020
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: There are few studies assessed the efficacy and mortality of endoscopic retrograde cholangiopancreatography (ERCP) for the removal of common bile duct (CBD) stones in the elderly aged ≥90 years. We aimed to assess the safety and efficacy of endoscopic removal of CBD stones in nonagenarians.
Methods
We retrospectively reviewed ERCP reports for CBD stone removal. The endoscopic and therapeutic outcomes were collected. The length of stay (LOS), the total number of adverse events, and mortality rate were compared between groups.
Results
A total of 125 nonagenarians were compared with 1,370 controls (65–89 years old individuals). The mean LOS for nonagenarians was significantly higher than in controls (13.6 days vs. 6.5 days). Completed intended treatment was similar in the nonagenarians and controls (89.8% and 89.5%, respectively). The overall complication rate did not differ between the groups. However, nonagenarians had a higher incidence of post-ERCP pneumonia (3.9%). None of the nonagenarians were readmitted to the hospital within 7 days. Four nonagenarians (3.2%) and 25 (1.8%) controls died within 30 days.
Conclusions
Advanced age alone did not affect the decision to perform the procedure. However, prompt diagnosis and treatment of post-ERCP pneumonia in nonagenarians could improve the outcomes and reduce mortality. -
Citations
Citations to this article as recorded by- Efficacy and Safety of Electrohydraulic Lithotripsy Using Peroral Cholangioscopy under Endoscopic Retrograde Cholangiopancreatography Guidance in Older Adults: A Single-Center Retrospective Study
Koji Takahashi, Hiroshi Ohyama, Yuichi Takiguchi, Yu Sekine, Shodai Toyama, Nana Yamada, Chihei Sugihara, Motoyasu Kan, Mayu Ouchi, Hiroki Nagashima, Yotaro Iino, Yuko Kusakabe, Kohichiroh Okitsu, Izumi Ohno, Naoya Kato
Medicina.2023; 59(4): 795. CrossRef
- Efficacy and Safety of Electrohydraulic Lithotripsy Using Peroral Cholangioscopy under Endoscopic Retrograde Cholangiopancreatography Guidance in Older Adults: A Single-Center Retrospective Study
- 2,019 View
- 143 Download
- 1 Web of Science
- 1 Crossref

Case Report
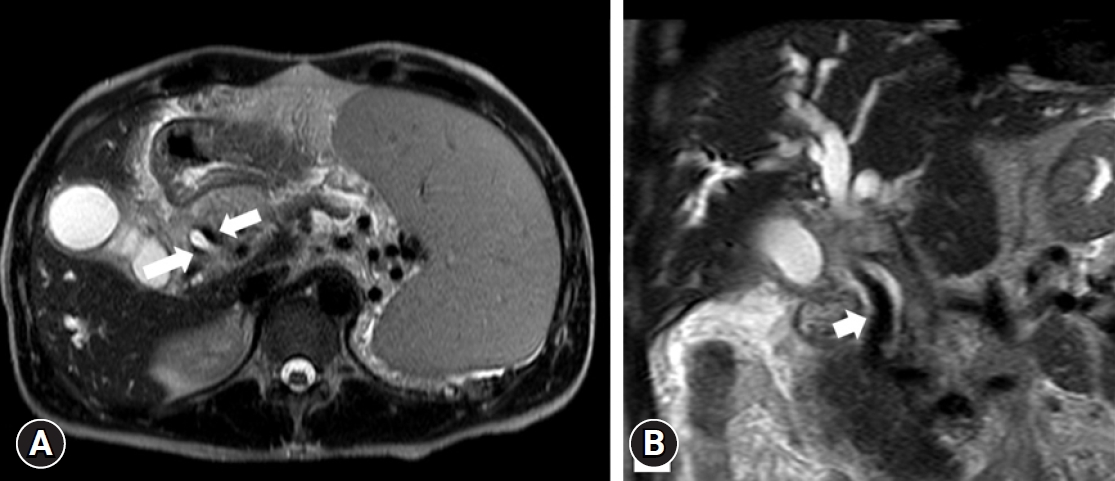
- Portal cavernography during endoscopic retrograde cholangiopancreatography: from bilhemia to hemobilia
- Rawad A. Yared, Paraskevas Gkolfakis, Arnaud Lemmers, Vincent Huberty, Thierry Degrez, Jacques Devière, Daniel Blero
- Clin Endosc 2023;56(4):521-526. Published online January 5, 2023
- DOI: https://doi.org/10.5946/ce.2021.276
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Portobiliary fistulas are rare but may lead to life-threatening complications. Biliary plastic stent-induced portobiliary fistulas during endoscopic retrograde cholangiopancreatography have been described. Herein, we present a case of portal cavernography and recurrent hemobilia after endoscopic retrograde cholangiopancreatography in which a portobiliary fistula was detected in a patient with portal biliopathy. This likely indicates a change in clinical presentation (from bilhemia to hemobilia) after biliary drainage that was successfully treated by placement of a fully covered, self-expandable metallic stent.
- 1,456 View
- 119 Download

Original Article
- Pancreatic duct lavage cytology combined with a cell-block method for patients with possible pancreatic ductal adenocarcinomas, including pancreatic carcinoma in situ
- Hiroaki Kusunose, Shinsuke Koshita, Yoshihide Kanno, Takahisa Ogawa, Toshitaka Sakai, Keisuke Yonamine, Kazuaki Miyamoto, Fumisato Kozakai, Hideyuki Anan, Kazuki Endo, Haruka Okano, Masaya Oikawa, Takashi Tsuchiya, Takashi Sawai, Yutaka Noda, Kei Ito
- Clin Endosc 2023;56(3):353-366. Published online November 16, 2022
- DOI: https://doi.org/10.5946/ce.2022.021

-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub 
- Background
/Aims: This study aimed to clarify the efficacy and safety of pancreatic duct lavage cytology combined with a cell-block method (PLC-CB) for possible pancreatic ductal adenocarcinomas (PDACs).
Methods
This study included 41 patients with suspected PDACs who underwent PLC-CB mainly because they were unfit for undergoing endoscopic ultrasonography-guided fine needle aspiration. A 6-Fr double lumen catheter was mainly used to perform PLC-CB. Final diagnoses were obtained from the findings of resected specimens or clinical outcomes during surveillance after PLC-CB.
Results
Histocytological evaluations using PLC-CB were performed in 87.8% (36/41) of the patients. For 31 of the 36 patients, final diagnoses (invasive PDAC, 12; pancreatic carcinoma in situ, 5; benignancy, 14) were made, and the remaining five patients were excluded due to lack of surveillance periods after PLC-CB. For 31 patients, the sensitivity, specificity, and accuracy of PLC-CB for detecting malignancy were 94.1%, 100%, and 96.8%, respectively. In addition, they were 87.5%, 100%, and 94.1%, respectively, in 17 patients without pancreatic masses detectable using endoscopic ultrasonography. Four patients developed postprocedural pancreatitis, which improved with conservative therapy.
Conclusions
PLC-CB has an excellent ability to detect malignancies in patients with possible PDACs, including pancreatic carcinoma in situ. -
Citations
Citations to this article as recorded by- Early diagnosis of pancreatic cancer via pancreatic juice cytology with a cell-block method in a patient with altered anatomy
Yasuo Otsuka, Kosuke Minaga, Akane Hara, Kentaro Yamao, Mamoru Takenaka, Takaaki Chikugo, Masatoshi Kudo
Endoscopy International Open.2024; 12(06): E764. CrossRef - Cell block created from pancreatic duct lavage is another jigsaw puzzle to diagnose early pancreatic ductal adenocarcinoma
Rungsun Rerknimitr
Clinical Endoscopy.2023; 56(3): 313. CrossRef
- Early diagnosis of pancreatic cancer via pancreatic juice cytology with a cell-block method in a patient with altered anatomy
- 2,296 View
- 199 Download
- 2 Web of Science
- 2 Crossref

Reviews
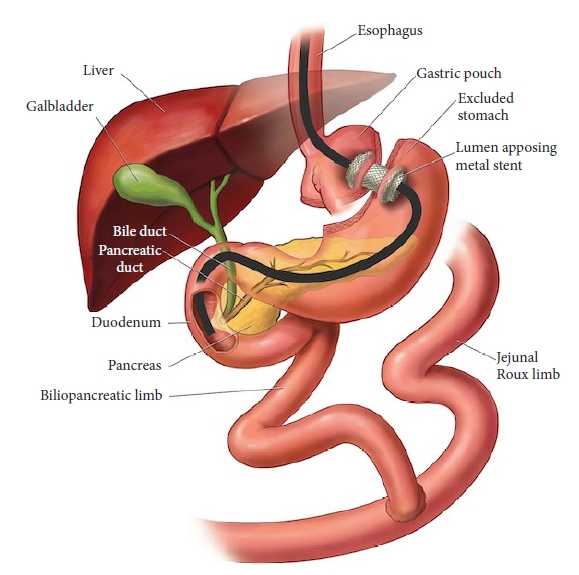
- Endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography for patients with Roux-en-Y gastric bypass anatomy: technical overview
- Hirokazu Honda, Jeffrey D. Mosko, Ryosuke Kobayashi, Andras Fecso, Bong Sik Kim, Schoeman Scott, Gary R. May
- Clin Endosc 2022;55(6):736-741. Published online October 5, 2022
- DOI: https://doi.org/10.5946/ce.2022.114
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic retrograde cholangiopancreatography (ERCP) in patients with Roux-en-Y gastric bypass anatomy is a well-documented challenge. Traditionally, this problem has been overcome with adjunctive techniques, such as device-assisted ERCP, including double-balloon or single-balloon enteroscopy and laparoscopy-assisted transgastric ERCP. Endoscopic ultrasound-directed transgastric ERCP (EDGE) is a novel technique that enables access to the ampulla using a duodenoscope without surgical intervention and has shown high clinical and technical success rates in recent studies. However, this approach is technically demanding, necessitating a thorough understanding of the gastrointestinal anatomy as well as high operator experience. In this review, we provide a technical overview of EDGE in parallel with our personal experience at our center and propose a simple algorithm to select patients for its appropriate application. In conjunction, the outcomes of EDGE compared with those of device-assisted and laparoscopy-assisted transgastric ERCP will be discussed.
-
Citations
Citations to this article as recorded by- Endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography procedure for choledocholithiasis after sleeve gastrectomy and Roux-en-Y
Reid D. Wasserman, Varun Kesar, Vivek Kesar, Paul Yeaton, Shehriyar Mehershahi
Endoscopy.2024; 56(S 01): E390. CrossRef - A novel endoscopic ultrasound-guided transluminal anchor device
Abhishek Agnihotri, Alexander Schlachterman
Endoscopy.2023; 55(S 01): E775. CrossRef
- Endoscopic ultrasound-directed transgastric endoscopic retrograde cholangiopancreatography procedure for choledocholithiasis after sleeve gastrectomy and Roux-en-Y
- 2,020 View
- 138 Download
- 2 Web of Science
- 2 Crossref

- Usefulness of the double-guidewire technique for endoscopic procedures in the field of biliary and pancreatic diseases
- Mamoru Takenaka, Masatoshi Kudo
- Clin Endosc 2022;55(5):605-614. Published online August 23, 2022
- DOI: https://doi.org/10.5946/ce.2022.032

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The double-guidewire method has been increasingly used in endoscopic procedures for biliary and pancreatic diseases in recent years, including endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography-related procedures. In addition, double-lumen catheters with uneven distal and proximal lumen openings have been introduced, making it possible to easily create a double-guidewire situation, and the usefulness of the double-guidewire technique using uneven double-lumen cannulas has been widely reported. Although the advantages of using two guidewires depend on the particular situation and the appropriate use of the two guidewires, deepening the knowledge of the double-guidewire method will contribute greatly to troubleshooting in daily practice. In this review, the usefulness of the double-guidewire technique is discussed with respect to two main areas: selective insertion of guidewires and devices and biliary cannulation.
-
Citations
Citations to this article as recorded by- Advancements in Research on Challenges in Selective Biliary Cannulation during Endoscopic Retrograde Cholangiopancreatography (ERCP)
天雨 张
Journal of Clinical Personalized Medicine.2024; 03(01): 100. CrossRef - Double-guidewire technique for selective biliary cannulation does not increase the rate of post-endoscopic retrograde cholangiopancreatography pancreatitis in patients with naïve papilla
Han Taek Jeong, June Hwa Bae, Ho Gak Kim, Jimin Han
Clinical Endoscopy.2024; 57(2): 226. CrossRef - Dedicated Echoendoscope for Interventional Endoscopic Ultrasound: Comparison with a Conventional Echoendoscope
Toshio Fujisawa, Shigeto Ishii, Yousuke Nakai, Hirofumi Kogure, Ko Tomishima, Yusuke Takasaki, Koichi Ito, Sho Takahashi, Akinori Suzuki, Hiroyuki Isayama
Journal of Clinical Medicine.2024; 13(10): 2840. CrossRef - INTRAOPERATIVE SIGNS OF ACUTE BILIARY PANCREATITIS
S. M. Vasyliuk, O. V. Prudnikov, V. V. Ivanyna, O. S. Tkachuk, N. M. Pavliuk, B. V. Krysa, V. M. Atamaniuk
Kharkiv Surgical School.2022; (4-5): 55. CrossRef
- Advancements in Research on Challenges in Selective Biliary Cannulation during Endoscopic Retrograde Cholangiopancreatography (ERCP)
- 2,784 View
- 204 Download
- 2 Web of Science
- 4 Crossref

Original Articles
- Preventive effect of tacrolimus on patients with post-endoscopic retrograde cholangiopancreatography pancreatitis
- Harshavardhan Rao B., Paul K. Vincent, Priya Nair, Anoop K. Koshy, Rama P. Venu
- Clin Endosc 2022;55(5):665-673. Published online August 2, 2022
- DOI: https://doi.org/10.5946/ce.2021.265

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: In patients undergoing endoscopic retrograde cholangiopancreatography (ERCP), calcineurin activates zymogen, which results in pancreatitis. In this study, we aimed to determine the efficacy of tacrolimus, a calcineurin inhibitor, in preventing post-ERCP pancreatitis (PEP).
Methods
This was a prospective pilot study in which patients who underwent ERCP received tacrolimus (4 mg in two divided doses); this was the Tac group. A contemporaneous cohort of patients was included as a control group. All patients were followed-up for PEP. PEP was characterized by worsening abdominal pain with an acute onset, elevated pancreatic enzymes, and a duration of hospital stay of more than 48 hours. Serum tacrolimus levels were measured immediately before the procedure in the Tac group.
Results
There were no differences in the baseline characteristics between the Tac group (n=48) and the control group (n=51). Only four out of 48 patients (8.3%) had PEP in the Tac group compared to eight out of 51 patients (15.7%) who had PEP in the control group. The mean trough tacrolimus level in patients who developed PEP was significantly lower (p<0.05).
Conclusions
Oral tacrolimus at a cumulative dose of 4 mg safely prevents PEP. Further randomized controlled studies are warranted to establish the role of tacrolimus in this context. -
Citations
Citations to this article as recorded by- Acute pancreatitis: pathogenesis and emerging therapies
Saif Zaman, Fred Gorelick
Journal of Pancreatology.2024; 7(1): 10. CrossRef - Preclinical safety evaluation of calcineurin inhibitors delivered through an intraductal route to prevent post-ERCP pancreatitis demonstrates endocrine and systemic safety
Jianbo Ni, Asna Khalid, Yu-Chu Lin, Monique T. Barakat, Jing Wang, Cheng-Yu Tsai, Pasha Reza Shams Azar, Ying Ding, Judy-April Murayi, Thottala Jayaraman, Ronald Poropatich, Rita Bottino, Li Wen, Georgios I. Papachristou, Gayathri Swaminathan, Mang Yu, So
Pancreatology.2023; 23(4): 333. CrossRef - Could assessment of genetic susceptibility be an effective solution to prevent pancreatitis from occurring after endoscopic retrograde cholangiopancreatography?
Jae Min Lee
The Korean Journal of Internal Medicine.2023; 38(6): 783. CrossRef - Rectal administration of tacrolimus protects against post-ERCP pancreatitis in mice
Yu-Chu Lin, Jianbo Ni, Gayathri Swaminathan, Asna Khalid, Monique T. Barakat, Adam R. Frymoyer, Cheng-Yu Tsai, Ying Ding, Judy-April Murayi, Thottala Jayaraman, Ronald Poropatich, Rita Bottino, Li Wen, Georgios I. Papachristou, Sunil G. Sheth, Mang Yu, So
Pancreatology.2023; 23(7): 777. CrossRef - Tacrolimus for prophylaxis of post-endoscopic retrograde cholangiopancreatography pancreatitis: a potential new target of old drug?
Seok Jeong
Clinical Endoscopy.2022; 55(5): 628. CrossRef
- Acute pancreatitis: pathogenesis and emerging therapies
- 2,652 View
- 134 Download
- 5 Web of Science
- 5 Crossref

- Increased ERCP volume improves cholangiogram interpretation: a new performance measure for ERCP training?
- Shyam Vedantam, Sunil Amin, Ben Maher, Saqib Ahmad, Shanil Kadir, Saad Khalid Niaz, Mark Wright, Nadeem Tehami
- Clin Endosc 2022;55(3):426-433. Published online February 4, 2022
- DOI: https://doi.org/10.5946/ce.2021.239
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: Cholangiogram interpretation is not used as a key performance indicator (KPI) of endoscopic retrograde cholangiopancreatography (ERCP) training, and national societies recommend different minimum numbers per annum to maintain competence. This study aimed to determine the relationship between correct ERCP cholangiogram interpretation and experience.
Methods
One hundred fifty ERCPists were surveyed to appropriately interpret ERCP cholangiographic findings. There were three groups of 50 participants each: “Trainees,” “Consultants group 1” (performed >75 ERCPs per year), and “Consultants group 2” (performed >100 ERCPs per year).
Results
Trainees was inferior to Consultants groups 1 and 2 in identifying all findings except choledocholithiasis outside the intrahepatic duct on the initial or completion/occlusion cholangiogram. Consultants group 1 was inferior to Consultants group 2 in identifying Strasberg type A bile leaks (odds ratio [OR], 0.86; 95% confidence interval [CI], 0.77–0.96), Strasberg type B (OR, 0.84; 95% CI, 0.74–0.95), and Bismuth type 2 hilar strictures (OR, 0.81; 95% CI, 0.69–0.95).
Conclusions
This investigation supports the notion that cholangiogram interpretation improves with increased annual ERCP case volumes. Thus, a higher annual volume of procedures performed may improve the ability to correctly interpret particularly difficult findings. Cholangiogram interpretation, in addition to bile duct cannulation, could be considered as another KPI of ERCP training. -
Citations
Citations to this article as recorded by- UK ERCP sedation practices, patient comfort and endoscopist characteristics: National Endoscopy Database (NED) analysis on behalf of the JAG and BSG
David Beaton, Matt Rutter, Linda Sharp, Kofi W Oppong, Bidour Awadelkarim, Simon M Everett, Vikramjit Mitra
Frontline Gastroenterology.2023; 14(5): 384. CrossRef
- UK ERCP sedation practices, patient comfort and endoscopist characteristics: National Endoscopy Database (NED) analysis on behalf of the JAG and BSG
- 3,612 View
- 237 Download
- 1 Web of Science
- 1 Crossref

- Factors Predicting Difficult Biliary Cannulation during Endoscopic Retrograde Cholangiopancreatography for Common Bile Duct Stones
- Hirokazu Saito, Yoshihiro Kadono, Takashi Shono, Kentaro Kamikawa, Atsushi Urata, Jiro Nasu, Haruo Imamura, Ikuo Matsushita, Tatsuyuki Kakuma, Shuji Tada
- Clin Endosc 2022;55(2):263-269. Published online November 12, 2021
- DOI: https://doi.org/10.5946/ce.2021.153

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Difficult biliary cannulation is an important risk factor for post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis (PEP). Therefore, this study aimed to identify the factors that predict difficult cannulation for common bile duct stones (CBDS) to reduce the risk for PEP.
Methods
This multicenter retrospective study included 1,406 consecutive patients with native papillae who underwent ERCP for CBDS. Factors predicting difficult cannulation for CBDS were identified using univariate and multivariate analyses.
Results
Univariate analysis showed that six factors significantly predicted difficult cannulation: ERCP performed by non-expert endoscopists, low-volume center, absence of acute cholangitis, normal serum bilirubin, intradiverticular papilla, and type of major duodenal papilla. Multivariate analysis identified ERCP performed by non-expert endoscopists (odds ratio [OR], 2.5; p<0.001), low-volume center (OR, 1.6; p<0.001), intradiverticular papilla (OR, 1.3; p=0.007), normal serum bilirubin (OR, 1.3; p=0.038), and absence of acute cholangitis (OR, 1.3; p=0.049) as factors significantly predicting difficult cannulation for CBDS.
Conclusions
Initial cannulation by an experienced endoscopist, early rescue cannulation, or early takeover by an experienced endoscopist should be considered when performing ERCP for CBDS in the presence of factors predicting difficult cannulation. -
Citations
Citations to this article as recorded by- Advancements in Research on Challenges in Selective Biliary Cannulation during Endoscopic Retrograde Cholangiopancreatography (ERCP)
天雨 张
Journal of Clinical Personalized Medicine.2024; 03(01): 100. CrossRef - The impact of transpancreatic precut sphincterotomy on the quality of ERCP in a low-volume setting
Wei-Chih Su, Chia-Chi Wang, Tsung-Hsien Hsiao, Hung-Da Chen, Jiann-Hwa Chen
Gastrointestinal Endoscopy.2024; 99(5): 747. CrossRef - Morphology of the papilla can predict procedural safety and efficacy of ERCP—a systematic review and meta-analysis
Edina Tari, Endre Botond Gagyi, Anett Rancz, Dániel Sándor Veres, Szilárd Váncsa, Péter Jenő Hegyi, Krisztina Hagymási, Péter Hegyi, Bálint Erőss
Scientific Reports.2024;[Epub] CrossRef - En face position of the major duodenal papilla using a reopenable clip during endoscopic retrograde cholangiopancreatography
Hirokazu Saito, Akiko Ikebata, Shunpei Hashigo
Digestive Endoscopy.2023;[Epub] CrossRef - Criterios 5-5-2 de canulación biliar y complicaciones post colangiopancreatografía retrógrada endoscópica: Experiencia en un hospital de referencia, Perú
Wilmer Gustavo Quiroga Purizaca, Diego Ricardo Páucar Aguilar, Jackeline Amparo Barrientos Pérez, Isamar Benyi Gutiérrez Córdova, Renato Garrido Acedo, Daniel Andrei Vargas Blácido
Revista de Gastroenterología del Perú.2023; 43(2): e1461. CrossRef - Predictive factors of difficult biliary cannulation: An experience of a tunisian tertiary center
K. Ben Abdallah, L. Hamzaoui, M. Mahmoudi, I. Cherif, A. Ben Mohamed, M. Yakoubi, A. Khsiba, M. Medhioub, M.M. Azouz
Heliyon.2022; 8(12): e12526. CrossRef
- Advancements in Research on Challenges in Selective Biliary Cannulation during Endoscopic Retrograde Cholangiopancreatography (ERCP)
- 3,901 View
- 251 Download
- 5 Web of Science
- 6 Crossref

- Endoscopic Interventions for the Early and Remission Phases of Acute Biliary Pancreatitis: What are the More Concrete and Practical Situations for Performing Them?
- Sho Hasegawa, Shinsuke Koshita, Yoshihide Kanno, Takahisa Ogawa, Toshitaka Sakai, Hiroaki Kusunose, Kensuke Kubota, Atsushi Nakajima, Yutaka Noda, Kei Ito
- Clin Endosc 2021;54(6):888-898. Published online May 27, 2021
- DOI: https://doi.org/10.5946/ce.2020.271

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: The use of endoscopic intervention (EI) for acute biliary pancreatitis (ABP) remains controversial because the severity of biliary obstruction/cholangitis/pancreatitis is not reflected in the indications for early EI (EEI).
Methods
A total of 148 patients with ABP were included to investigate 1) the differences in the rate of worsening cholangitis/pancreatitis between the EEI group and the early conservative management (ECM) group, especially for each severity of cholangitis/pancreatitis, and 2) the diagnostic ability of imaging studies, including endoscopic ultrasound (EUS), to detect common bile duct stones (CBDSs) in the ECM group.
Results
No differences were observed in the rate of worsening cholangitis between the EEI and ECM groups, regardless of the severity of cholangitis and/or the existence of impacted CBDSs. Among patients without impacted CBDSs and moderate/severe cholangitis, worsening pancreatitis was significantly more frequent in the EEI group (18% vs. 4%, p=0.048). In patients in the ECM group, the sensitivity and specificity for detecting CBDSs were 73% and 98%, respectively, for EUS, whereas the values were 13% and 92%, respectively, for magnetic resonance cholangiopancreatography.
Conclusions
EEI should be avoided in the absence of moderate/severe cholangitis and/or impacted CBDSs because of the high rate of worsening pancreatitis. EUS can contribute to the accurate detection of residual CBDSs, for the determination of the need for elective EI.
- 3,073 View
- 103 Download

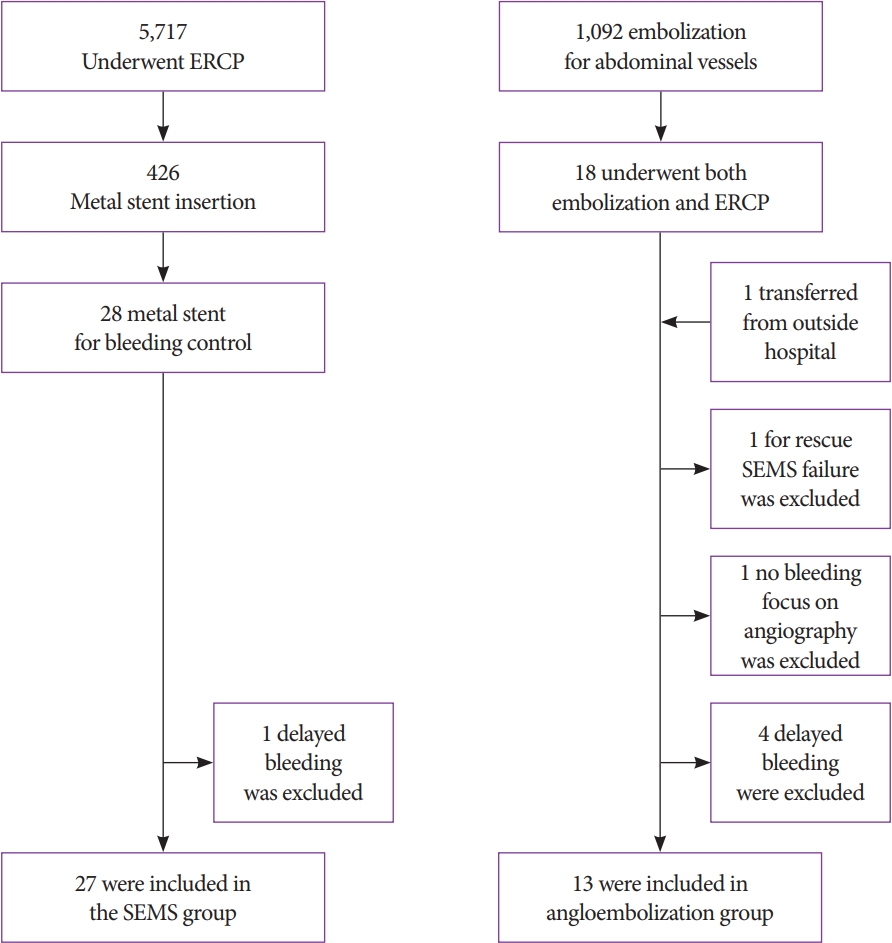
- Biliary Self-Expandable Metal Stent Could Be Recommended as a First Treatment Modality for Immediate Refractory Post-Endoscopic Retrograde Cholangiopancreatography Bleeding
- Sun Young Moon, Jun Heo, Min Kyu Jung, Chang Min Cho
- Clin Endosc 2022;55(1):128-135. Published online May 25, 2021
- DOI: https://doi.org/10.5946/ce.2021.057
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Recent reports suggest that the biliary self-expandable metallic stent (SEMS) is highly effective for maintaining hemostasis when endoscopic hemostasis fails in endoscopic retrograde cholangiopancreatography (ERCP)-related bleeding. We compared whether temporary SEMS offers better efficacy than angioembolization for refractory immediate ERCP-related bleeding.
Methods
Patients who underwent SEMS placement or underwent angioembolization for bleeding control in refractory immediate ERCP-related bleeding were included in the retrospective analysis. We evaluated the hemostasis success rate, severity of bleeding, change in hemoglobin levels, amount of transfusion, and delay to the start of hemostasis.
Results
A total of 27 patients with SEMS and 13 patients who underwent angioembolization were enrolled. More transfusions were needed in the angioembolization group (1.0±1.4 units vs. 2.5±2.0 units; p=0.034). SEMS failure was successfully rescued by angioembolization. The partially covered SEMS (n=23, 85.1%) was generally used, and the median stent-indwelling time was 4 days. The mean delay to the start of angioembolization was 95.2±142.9 (range, 9–491) min.
Conclusions
Temporary SEMS had similar results to those of angioembolization (96.3% vs. 92.3%; p=0.588). Immediate SEMS insertion is considered a bridge treatment modality for immediate refractory ERCP-related bleeding. Angioembolization still has a role as rescue therapy when SEMS does not work effectively.
- 3,430 View
- 164 Download

Review
- Technical Review of Developments in Endoscopic Ultrasound-Guided Hepaticogastrostomy
- Takeshi Ogura, Kazuhide Higuchi
- Clin Endosc 2021;54(5):651-659. Published online April 26, 2021
- DOI: https://doi.org/10.5946/ce.2021.020-KDDW
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Endoscopic ultrasound-guided biliary drainage has been developed as an alternative method for biliary drainage. EUS-guided hepaticogastrostomy (EUS-HGS) can be attempted via the trans-gastric route. These procedures are technically complex for two reasons. First, puncture of the intrahepatic bile duct via the trans-gastric route can be more difficult than that by other approaches because of the small diameter of the target site, and guidewire insertion or manipulation is challenging during EUS-HGS. Second, critical adverse events, such as stent migration into the abdominal cavity, could occur because of the greater mobility of the stomach compared to the duodenum. Therefore, endoscopists should be cautious when performing EUS-HGS. An advantage of EUS-HGS is that it can be performed in patients with complications such as duodenal bulb obstruction or surgically altered anatomy. Recent advances in technique and improvements in devices and stents for EUS-HGS have shown promise for improving the technical success rate of EUS-HGS and reducing the rate of adverse events. However, endoscopists should remain aware of the possibility of critical adverse events such as stent migration.
-
Citations
Citations to this article as recorded by- Propensity score matching analysis for clinical impact of braided-type versus laser-cut-type covered self-expandable metal stents for endoscopic ultrasound-guided hepaticogastrostomy
Mitsuki Tomita, Takeshi Ogura, Akitoshi Hakoda, Saori Ueno, Atsushi Okuda, Nobu Nishioka, Yoshitaro Yamamoto, Hiroki Nishikawa
Hepatobiliary & Pancreatic Diseases International.2024; 23(2): 181. CrossRef - Usefulness of endoscopic ultrasound‐guided transhepatic biliary drainage with a 22‐gauge fine‐needle aspiration needle and 0.018‐inch guidewire in the procedure's induction phase
Kei Yane, Masahiro Yoshida, Takayuki Imagawa, Kotaro Morita, Hideyuki Ihara, Kota Hanada, Sota Hirokawa, Yusuke Tomita, Takeyoshi Minagawa, Yutaka Okagawa, Tetsuya Sumiyoshi, Michiaki Hirayama, Hitoshi Kondo
DEN Open.2024;[Epub] CrossRef - EUS-guided hepaticogastrostomy versus EUS-guided hepaticogastrostomy with antegrade stent placement in patients with unresectable malignant distal biliary obstruction: a propensity score–matched case-control study
Hirotoshi Ishiwatari, Takeshi Ogura, Susumu Hijioka, Takuji Iwashita, Saburo Matsubara, Kazuma Ishikawa, Fumitaka Niiya, Junya Sato, Atsushi Okuda, Saori Ueno, Yoshikuni Nagashio, Yuta Maruki, Shinya Uemura, Akifumi Notsu
Gastrointestinal Endoscopy.2024;[Epub] CrossRef - Stent Deployment Without Tract Dilation in Endoscopic Ultrasound-Guided Hepaticogastrostomy Using a Novel Partially Covered Metal Stent With a Super-Slim Stent Delivery System: A Case Report
Koji Takahashi, Hiroshi Ohyama, Izumi Ohno, Naoya Kato
Cureus.2024;[Epub] CrossRef - TOKYO criteria 2024 for the assessment of clinical outcomes of endoscopic biliary drainage
Hiroyuki Isayama, Tsuyoshi Hamada, Toshio Fujisawa, Mitsuharu Fukasawa, Kazuo Hara, Atsushi Irisawa, Shigeto Ishii, Ken Ito, Takao Itoi, Yoshihide Kanno, Akio Katanuma, Hironari Kato, Hiroshi Kawakami, Hirofumi Kawamoto, Masayuki Kitano, Hirofumi Kogure,
Digestive Endoscopy.2024;[Epub] CrossRef - Efficacy of a dedicated plastic stent in endoscopic ultrasound-guided hepaticogastrostomy during the learning curve: cumulative multi-center experience
Koh Kitagawa, Akira Mitoro, Ryuki Minami, Shinsaku Nagamatsu, Takahiro Ozutsumi, Yukihisa Fujinaga, Norihisa Nishimura, Yasuhiko Sawada, Tadashi Namisaki, Takemi Akahane, Kosuke Kaji, Fumimasa Tomooka, Shohei Asada, Miki Kaneko, Hitoshi Yoshiji
Scandinavian Journal of Gastroenterology.2023; 58(3): 296. CrossRef - Removal of a small pancreatic stone in thin main pancreatic duct using an ultrafine balloon catheter (with video)
Saburo Matsubara, Keito Nakagawa, Kentaro Suda, Takeshi Otsuka, Masashi Oka, Sumiko Nagoshi
Journal of Hepato-Biliary-Pancreatic Sciences.2023;[Epub] CrossRef - Drainage of Afferent Limb Obstruction via the Trans-gastric-bile Duct Formed after Endoscopic Ultrasound-guided Hepaticogastrostomy in a Patient with Pancreatic Cancer
Masatoshi Mabuchi, Seiji Adachi, Yukari Uno, Hironori Nakamura, Makoto Shimazaki, Shinji Nishiwaki, Iwao Kumazawa, Takuji Iwashita, Masahito Shimizu
Internal Medicine.2023; 62(16): 2355. CrossRef - Clinical feasibility of endoscopic ultrasound‐guided biliary drainage for preoperative management of malignant biliary obstruction (with videos)
Shuntaro Mukai, Takao Itoi, Takayoshi Tsuchiya, Kentaro Ishii, Ryosuke Tonozuka, Yuichi Nagakawa, Shingo Kozono, Chie Takishita, Hiroaki Osakabe, Atsushi Sofuni
Journal of Hepato-Biliary-Pancreatic Sciences.2023; 30(7): 983. CrossRef - A retrospective multicenter study comparing the punctures to B2 and B3 in endoscopic ultrasound–guided hepaticogastrostomy
Masanari Sekine, Yusuke Hashimoto, Taro Shibuki, Kei Okumura, Ikuhiro Kobori, Aki Miyagaki, Yoshihiro Sasaki, Yuichi Takano, Keita Matsumoto, Hirosato Mashima
DEN Open.2023;[Epub] CrossRef - Stent‐in‐stent technique in a case of difficult removal of a EUS‐guided hepaticogastrostomy partially covered metal stent due to mucosal hyperplasia (with video)
Takeshi Ogura, Yuki Uba, Hiroki Nishikawa
Journal of Hepato-Biliary-Pancreatic Sciences.2023; 30(10): 1188. CrossRef - Loop technique for guidewire manipulation during endoscopic ultrasound‐guided hepaticogastrostomy
Haruo Miwa, Kazuya Sugimori, Yuto Matsuoka, Kazuki Endo, Ritsuko Oishi, Masaki Nishimura, Yuichiro Tozuka, Takashi Kaneko, Kazushi Numata, Shin Maeda
JGH Open.2023; 7(5): 358. CrossRef - Drainage Approach for Malignant Biliary Obstruction
Ian Eisenberg, Monica Gaidhane, Michel Kahaleh, Amy Tyberg
Journal of Clinical Gastroenterology.2023; 57(6): 546. CrossRef - Guidewire malposition outside the bile duct during endoscopic ultrasound-guided hepaticogastrostomy
Yoshimitsu Fukasawa, Mitsuharu Fukasawa, Shinichi Takano, Satoshi Kawakami, Hiroshi Hayakawa, Shota Harai, Nobuyuki Enomoto
Endoscopy.2023; 55(S 01): E894. CrossRef - Preloading guidewire method: EUS-guided hepaticogastrostomy
Hirotsugu Maruyama, Yuki Ishikawa-Kakiya, Kojiro Tanoue, Akira Higashimori, Yasuhiro Fujiwara
Arab Journal of Gastroenterology.2023; 24(3): 183. CrossRef - Guidewires in GI endoscopy
Samuel Han, Mohit Girotra, Venkata S. Akshintala, Dennis Chen, Yen-I Chen, Koushik K. Das, Allon Kahn, Girish Mishra, V. Raman Muthusamy, Jorge V. Obando, Frances U. Onyimba, Swati Pawa, Tarun Rustagi, Sonali Sakaria, Guru Trikudanathan, Ryan J. Law
iGIE.2023; 2(3): 386. CrossRef - EUS–guided transhepatic metal stent deployment technique without tract dilation using a 0.018-inch guidewire (with video)
Takeshi Ogura, Jyunichi Kawai, Kyohei Nishiguchi, Yoshitaro Yamamoto, Kazuhide Higuchi
Endoscopic Ultrasound.2023; 12(5): 431. CrossRef - The writing on the wall: self-expandable stents for endoscopic ultrasound-guided hepaticogastrostomy?
Hyung Ku Chon, Shayan Irani, Tae Hyeon Kim
Clinical Endoscopy.2023; 56(6): 741. CrossRef - Rescue technique after endoscopic ultrasound-guided hepaticogastrostomy stent dislocation
Takeshi Ogura, Taro Iwatsubo, Atsushi Okuda, Saori Ueno, Hiroki Nishikawa
Endoscopy.2023; 55(S 01): E1236. CrossRef - Endoscopic ultrasound-guided hepaticogastrostomy using a novel drill dilator
Masanori Yamada, Kazuo Hara, Shin Haba, Nobumasa Mizuno, Takamichi Kuwahara, Nozomi Okuno, Yasuhiro Kuraishi
Endoscopy.2022; 54(S 02): E856. CrossRef - Successful endoscopic treatment of huge infected biloma and hepatic abscess after endoscopic ultrasound-guided hepaticogastrostomy with brain abscess
Koji Takahashi, Hiroshi Ohyama, Hiroki Nagashima, Yotaro Iino, Yuko Kusakabe, Kohichiroh Okitsu, Izumi Ohno, Yuichi Takiguchi, Naoya Kato
Clinical Journal of Gastroenterology.2022; 15(5): 988. CrossRef - Prevention of Serious Complications during Endoscopic Ultrasound-Guided Biliary Drainage: A Case-Based Technical Review
Surinder Singh Rana, Jimil Shah, Harish Bhujade, Ujjwal Gorsi, Mandeep Kang, Rajesh Gupta
Journal of Digestive Endoscopy.2022; 13(02): 082. CrossRef - Endoscopic salvage therapy after failed biliary cannulation using advanced techniques: A concise review
Yung-Kuan Tsou, Kuang-Tse Pan, Mu Hsien Lee, Cheng-Hui Lin
World Journal of Gastroenterology.2022; 28(29): 3803. CrossRef - Usefulness of the double-guidewire technique for endoscopic procedures in the field of biliary and pancreatic diseases
Mamoru Takenaka, Masatoshi Kudo
Clinical Endoscopy.2022; 55(5): 605. CrossRef - New Stents for Endoscopic Ultrasound-Guided Procedures
Gunn Huh, Tae Jun Song
The Korean Journal of Pancreas and Biliary Tract.2021; 26(4): 248. CrossRef
- Propensity score matching analysis for clinical impact of braided-type versus laser-cut-type covered self-expandable metal stents for endoscopic ultrasound-guided hepaticogastrostomy
- 5,229 View
- 296 Download
- 21 Web of Science
- 25 Crossref

Original Article
- Outcomes of Dilation of Recalcitrant Pancreatic Strictures Using a Wire-Guided Cystotome
- Sridhar Sundaram, Dhaval Choksi, Aditya Kale, Suprabhat Giri, Biswaranjan Patra, Shobna Bhatia, Akash Shukla
- Clin Endosc 2021;54(6):903-908. Published online March 4, 2021
- DOI: https://doi.org/10.5946/ce.2020.297
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Pancreatic strictures in chronic pancreatitis are treated using endoscopic retrograde cholangiopancreatography (ERCP) with plastic stent placement. The management of recalcitrant strictures remains a challenge, with the use of a Soehendra stent retriever or a needle knife described in case reports. Here, we discuss our experience with dilation of dominant pancreatic strictures with a 6-Fr cystotome.
Methods
A retrospective review of an endoscopy database was performed to search for patients with pancreatic strictures recalcitrant to conventional methods of dilation in which a cystotome was used. Technical success was defined as the successful dilation of the stricture with plastic stent placement. Functional success was defined as substantial pain relief or resolution of pancreatic fistulae.
Results
Ten patients (mean age, 30.8 years) underwent dilation of a dominant pancreatic stricture secondary to chronic pancreatitis, with a 6-Fr cystotome. Seven patients presented with pain. Three patients had pancreatic fistulae (two had pancreatic ascites and one had a pancreaticopleural fistula). The median stricture length was 10 mm (range, 5–25 mm). The head of the pancreas was the most common location of the stricture (60%). Technical and functional success was achieved in all patients. One patient had self-limiting bleeding, whereas another patient developed mild post-ERCP pancreatitis.
Conclusions
The use of a 6-Fr cystotome (diathermy catheter) can be an alternative method for dilation of recalcitrant pancreatic strictures after the failure of conventional modalities. -
Citations
Citations to this article as recorded by- Treatment of Difficult Pancreatic Duct Strictures Using a Cystotome: A Single-Center Experience
Jonghyun Lee, Dong Uk Kim, Sung Yong Han
The Korean Journal of Pancreas and Biliary Tract.2023; 28(4): 108. CrossRef - Approach to management of pancreatic strictures: the gastroenterologist’s perspective
Vaneet Jearth, Suprabhat Giri, Sridhar Sundaram
Clinical Journal of Gastroenterology.2021; 14(6): 1587. CrossRef
- Treatment of Difficult Pancreatic Duct Strictures Using a Cystotome: A Single-Center Experience
- 3,450 View
- 87 Download
- 1 Web of Science
- 2 Crossref

Case Report
- Practical Experiences of Unsuccessful Hemostasis with Covered Self-Expandable Metal Stent Placement for Post-Endoscopic Sphincterotomy Bleeding
- Michihiro Yoshida, Tadahisa Inoue, Itaru Naitoh, Kazuki Hayashi, Yasuki Hori, Makoto Natsume, Naoki Atsuta, Hiromi Kataoka
- Clin Endosc 2022;55(1):150-155. Published online November 19, 2020
- DOI: https://doi.org/10.5946/ce.2020.217

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - We reviewed 7 patients with unsuccessful endoscopic hemostasis using covered self-expandable metal stent (CSEMS) placement for post-endoscopic sphincterotomy (ES) bleeding. ES with a medium incision was performed in 6 and with a large incision in 1 patient. All but 1 of them (86%) showed delayed bleeding, warranting second endoscopic therapies followed by CSEMS placement 1–5 days after the initial ES. Subsequent CSEMS placement did not achieve complete hemostasis in any of the patients. Lateral-side incision lines (3 or 9 o’clock) had more frequent bleeding points (71%) than oral-side incision lines (11–12 o’clock; 29%). Additional endoscopic hemostatic procedures with hemostatic forceps, hypertonic saline epinephrine, or hemoclip achieved excellent hemostasis, resulting in complete hemostasis in all patients. These experiences provide an alert: CSEMS placement is not an ultimate treatment for post-ES bleeding, despite its effectiveness. The lateral-side of the incision line, as well as the oral-most side, should be carefully examined for bleeding points, even after the CSEMS placement.
-
Citations
Citations to this article as recorded by
- 3,780 View
- 176 Download
- 2 Crossref

Original Articles
- Cholecystitis after Placement of Covered Self-Expandable Metallic Stents in Patients with Distal Malignant Biliary Obstructions
- Masafumi Watanabe, Kosuke Okuwaki, Jun Woo, Mitsuhiro Kida, Hiroshi Imaizumi, Tomohisa Iwai, Hiroshi Yamauchi, Toru Kaneko, Rikiya Hasegawa, Takahiro Kurosu, Naoki Minato, Hiroki Haradome, Wasaburo Koizumi
- Clin Endosc 2021;54(4):589-595. Published online November 17, 2020
- DOI: https://doi.org/10.5946/ce.2020.136

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Cholecystitis can occur after the placement of covered self-expandable metallic stents for distal malignant biliary obstructions. We aimed to identify risk factors for cholecystitis following covered self-expandable metallic stent placement.
Methods
We investigated risk factors related to cholecystitis following covered self-expandable metallic stent placement in 118 patients with distal malignant biliary obstructions between January 1, 2015 and April 30, 2019. Endoscopic assessments and tumor invasion to the arteries feeding the gallbladder were determined by a pancreaticobiliary endoscopist and a radiologist, respectively.
Results
The median patient age was 72 years (men, 61.0%). The flow of the contrast agent into the gallbladder and tumor involvement in the orifice of the cystic duct were observed in 35 (29.7%) and 35 (29.7%) patients, respectively. During the observation period (median, 179 days), cholecystitis occurred in 18 (15.3%) patients. Multivariate analysis revealed the flow of the contrast agent into the gallbladder (p=0.023) and tumor involvement in the orifice of the cystic duct (p=0.005) as significant independent risk factors associated with cholecystitis.
Conclusions
The flow of the contrast agent into the gallbladder and tumor involvement in the orifice of the cystic duct are potential independent risk factors for cholecystitis following the placement of covered self-expandable metallic stents. A follow-up prospective study is warranted to validate their influence. -
Citations
Citations to this article as recorded by- Adverse events of self-expandable metal stent placement for malignant distal biliary obstruction: a large multicenter study
Takashi Tamura, Takuo Yamai, Norimitsu Uza, Tomoaki Yamasaki, Atsuhiro Masuda, Fumimasa Tomooka, Hirotsugu Maruyama, Minoru Shigekawa, Takeshi Ogura, Katsutoshi Kuriyama, Masanori Asada, Hisakazu Matsumoto, Mamoru Takenaka, Koichiro Mandai, Yui Osaki, Ken
Gastrointestinal Endoscopy.2024; 99(1): 61. CrossRef - Fully covered versus partially covered self-expandable metal stents for palliation of distal malignant biliary obstruction: a systematic review and meta-analysis
Giuseppe Vanella, Chiara Coluccio, Alessandro Cucchetti, Roberto Leone, Giuseppe Dell’Anna, Paolo Giuffrida, Carmela Abbatiello, Cecilia Binda, Carlo Fabbri, Paolo Giorgio Arcidiacono
Gastrointestinal Endoscopy.2024; 99(3): 314. CrossRef - Endoscopic Ultrasound–Guided vs Endoscopic Retrograde Cholangiopancreatography–Guided Biliary Drainage as Primary Approach to Malignant Distal Biliary Obstruction: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Harishankar Gopakumar, Ritu Raj Singh, Vakya Revanur, Rajanikanth Kandula, Srinivas R. Puli
American Journal of Gastroenterology.2024;[Epub] CrossRef - Cholecystitis in patients with a fully covered self-expandable metal stent with and without externally anchored plastic stents
José Miguel Jiménez-Gutiérrez, Félix Téllez-Avila
Endoscopy.2024; 56(04): 317. CrossRef - Risk factors and treatment strategies for cholecystitis after metallic stent placement for malignant biliary obstruction: a multicenter retrospective study
Akihiro Matsumi, Hironari Kato, Taiji Ogawa, Toru Ueki, Masaki Wato, Masakuni Fujii, Tatsuya Toyokawa, Ryo Harada, Yuki Ishihara, Masahiro Takatani, Hirofumi Tsugeno, Naoko Yunoki, Takeshi Tomoda, Toshiharu Mitsuhashi, Motoyuki Otsuka
Gastrointestinal Endoscopy.2024; 100(1): 76. CrossRef - Covered versus uncovered double bare self-expandable metal stent for palliation of unresectable extrahepatic malignant biliary obstruction: a randomized controlled multicenter trial
Se Woo Park, Kyong Joo Lee, Moon Jae Chung, Jung Hyun Jo, Hee Seung Lee, Jeong Youp Park, Seung Woo Park, Si Young Song, Huapyong Kang, Eui Joo Kim, Yeon Suk Kim, Jae Hee Cho, Seungmin Bang
Gastrointestinal Endoscopy.2023; 97(1): 132. CrossRef - Risk factors for early and late cholecystitis after covered metal stent placement for distal biliary obstruction
Tatsuya Ishii, Tsuyoshi Hayashi, Hajime Yamazaki, Risa Nakamura, Kosuke Iwano, Ryo Ando, Haruka Toyonaga, Toshifumi Kin, Kuniyuki Takahashi, Akio Katanuma
Journal of Hepato-Biliary-Pancreatic Sciences.2023; 30(10): 1180. CrossRef - Efficacy and complications of inoperable malignant distal biliary obstruction treatment by metallic stents: fully covered or uncovered?
Jiangning Gu, Xiaoyi Guo, Yong Sun, Bin Fan, Haoran Li, Ting Luo, Haifeng Luo, Jiao Liu, Feng Gao, Yuan Gao, Guang Tan, Xiaoming Liu, Zhuo Yang
Gastroenterology Report.2022;[Epub] CrossRef - Endoscopic Management of Pancreatobiliary Malignancies
Dong Wook Lee, Eun Young Kim
Digestive Diseases and Sciences.2022; 67(5): 1635. CrossRef
- Adverse events of self-expandable metal stent placement for malignant distal biliary obstruction: a large multicenter study
- 5,357 View
- 151 Download
- 6 Web of Science
- 9 Crossref

- Evaluating the Revised American Society for Gastrointestinal Endoscopy Guidelines for Common Bile Duct Stone Diagnosis
- Jake S. Jacob, Michelle E. Lee, Erin Y. Chew, Aaron P. Thrift, Robert J. Sealock
- Clin Endosc 2021;54(2):269-274. Published online November 6, 2020
- DOI: https://doi.org/10.5946/ce.2020.100
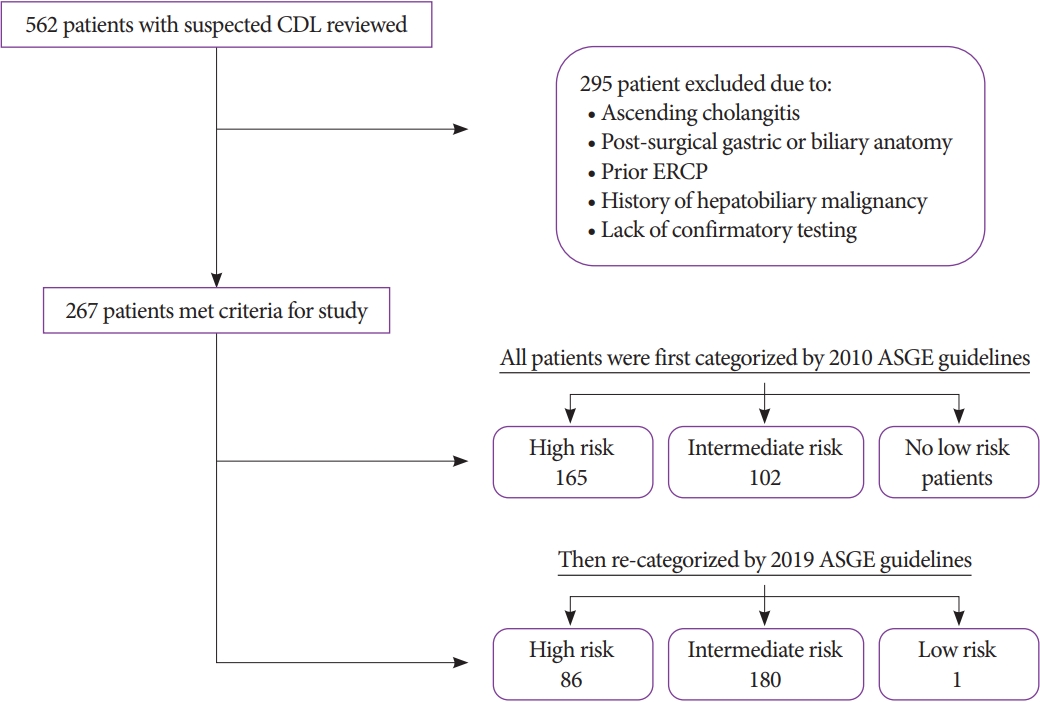
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Background
/Aims: The American Society for Gastrointestinal Endoscopy (ASGE) revised its guidelines for risk stratification of patients with suspected choledocholithiasis. This study aimed to assess the diagnostic performance of the revision and to compare it to the previous guidelines.
Methods
We conducted a retrospective cohort study of 267 patients with suspected choledocholithiasis. We identified high-risk patients according to the original and revised guidelines and examined the diagnostic accuracy of both guidelines. We measured the association between individual criteria and choledocholithiasis.
Results
Under the original guidelines, 165 (62%) patients met the criteria for high risk, of whom 79% had confirmed choledocholithiasis. The categorization had a sensitivity and specificity of 68% and 55%, respectively, for the detection of choledocholithiasis. Under the revised guidelines, 86 (32%) patients met the criteria for high risk, of whom 83% had choledocholithiasis. The revised categorization had a lower sensitivity and higher specificity of 37% and 80%, respectively. The positive predictive value of the high-risk categorization increased with the revision, reflecting a potential decrease in diagnostic endoscopic retrograde cholangiopancreatograpies (ERCPs). Stone visualized on imaging had the greatest specificity for choledocholithiasis. Gallstone pancreatitis was not associated with the risk for choledocholithiasis.
Conclusions
The 2019 revision of the ASGE guidelines decreases the utilization of ERCP as a diagnostic modality and offers an improved risk stratification tool. -
Citations
Citations to this article as recorded by- Endoscopic ultrasound avoids diagnostic ERCP among the ASGE high-risk group – Experience in an Asian population
Weng-Fai Wong, Yu-Ting Kuo, Ming-Lun Han, Hsiu-Po Wang
Journal of the Formosan Medical Association.2024; 123(3): 374. CrossRef - Rendimiento diagnóstico de la endosonografía biliopancreática en pacientes con riesgo intermedio de coledocolitiasis
Lázaro Antonio Arango Molano, Andrés Sánchez Gil, Claudia Patricia Diaz Tovar, Andrés Valencia Uribe, Christian Germán Ospina Pérez, Pedro Eduardo Cuervo Pico, Rodrigo Alberto Jiménez Gómez
Revista de Gastroenterología del Perú.2024; 44(1): 8. CrossRef - Suspected common bile duct stones: reduction of unnecessary ERCP by pre-procedural imaging and timing of ERCP
Christina J. Sperna Weiland, Evelien C. Verschoor, Alexander C. Poen, Xavier J. M. N. Smeets, Niels G. Venneman, Abha Bhalla, Ben J. M. Witteman, Hester C. Timmerhuis, Devica S. Umans, Jeanin E. van Hooft, Marco J. Bruno, P. Fockens, Robert C. Verdonk, Jo
Surgical Endoscopy.2023; 37(2): 1194. CrossRef - Low Detection Rates of Bile Duct Stones During Endoscopic Treatment for Highly Suspected Bile Duct Stones with No Imaging Evidence of Stones
Hirokazu Saito, Hajime Iwasaki, Hisashi Itoshima, Yoshihiro Kadono, Takashi Shono, Kentaro Kamikawa, Atsushi Urata, Jiro Nasu, Masayoshi Uehara, Ikuo Matsushita, Tatsuyuki Kakuma, Shuji Tada
Digestive Diseases and Sciences.2023; 68(5): 2061. CrossRef - Effect of Frailty on the Management of Suspected Choledocholithiasis
Katherine C. Bergus, Rondi B. Gelbard, Sara Scarlet, Shruthi Srinivas, Brett M. Tracy
The American Surgeon™.2023; 89(7): 3104. CrossRef - Prospective assessment of the accuracy of ASGE and ESGE guidelines for choledocholithiasis
Andy Silva-Santisteban, Ishani Shah, Madhuri Chandnani, Vaibhav Wadhwa, Leo Tsai, Abraham F. Bezuidenhout, Tyler M. Berzin, Douglas Pleskow, Mandeep Sawhney
Endoscopy International Open.2023; 11(06): E599. CrossRef - ERCP findings provide further justification for a “surgery-first” mindset in choledocholithiasis
Gloria Sanin, Gabriel Cambronero, James Patterson, Maggie Bosley, Aravindh Ganapathy, Carl Wescott, Lucas Neff
Surgical Endoscopy.2023; 37(11): 8714. CrossRef - Dynamic changes in liver function tests do not correctly reclassify patients at risk of choledocholithiasis beyond ASGE 2019 criteria
Tatiana Ramírez-Peña, Rómulo Darío Vargas-Rubio, Carlos Ernesto Lombo, Luis Miguel Rodríguez-Hortua, Oscar Mauricio Muñoz-Velandia
Therapeutic Advances in Gastrointestinal Endoscopy.2023;[Epub] CrossRef - National adherence to the ASGE-SAGES guidelines for managing suspected choledocholithiasis: An EAST multicenter study
Brett M. Tracy, Benjamin K. Poulose, Cameron W. Paterson, April E. Mendoza, Apostolos Gaitanidis, Jonathan M. Saxe, Andrew J. Young, Martin D. Zielinski, Carrie A. Sims, Rondi B. Gelbard
Journal of Trauma and Acute Care Surgery.2022; 92(2): 305. CrossRef - Accuracy of SAGES, ASGE, and ESGE criteria in predicting choledocholithiasis
Kinzang Wangchuk, Pongsakorn Srichan
Surgical Endoscopy.2022; 36(10): 7233. CrossRef - Evaluation of the American Society of Gastrointestinal Endoscopy 2019 and the European Society of Gastrointestinal Endoscopy guidelines' performances for choledocholithiasis prediction in clinically suspected patients: A retrospective cohort study
Suppadech Tunruttanakul, Borirak Chareonsil, Kotchakorn Verasmith, Jayanton Patumanond, Chatchai Mingmalairak
JGH Open.2022; 6(6): 434. CrossRef - Test Performance Characteristics of Dynamic Liver Enzyme Trends in the Prediction of Choledocholithiasis
Yang Lei, B. Lethebe, Erin Wishart, Fateh Bazerbachi, B. Elmunzer, Nirav Thosani, James Buxbaum, Yen-I Chen, Sydney Bass, Martin Cole, Christian Turbide, Darren Brenner, Steven Heitman, Rachid Mohamed, Nauzer Forbes
Journal of Clinical Medicine.2022; 11(15): 4575. CrossRef - Criterios ASGE 2010 frente a 2019 para coledocolitiasis en pacientes llevados a colangiopancreatografía retrógrada endoscópica
Ana María Lourido Gamboa, Guillermo Vallejo Vallecilla, Jesús Eduardo Díaz Realpe, Katheryn Daniela Lagos Castro, Juan David Guzmán Sandoval, Angela María Merchán Galvis
Revista colombiana de Gastroenterología.2022; 37(4): 362. CrossRef - Optimal Predictive Criteria for Common Bile Duct Stones: The Search Continues
Yun Nah Lee, Jong Ho Moon
Clinical Endoscopy.2021; 54(2): 147. CrossRef
- Endoscopic ultrasound avoids diagnostic ERCP among the ASGE high-risk group – Experience in an Asian population
- 5,514 View
- 287 Download
- 14 Web of Science
- 14 Crossref

- Novel Ablation Therapy Using Endoscopic Irreversible Electroporation in the Bile Duct: A Pilot Animal Study
- Kang Won Lee, Jae Min Lee, Hyuk Soon Choi, Eun Sun Kim, Bora Keum, Yeon Seok Seo, Yoon Tae Jeen, Soon Ho Um, Hong Sik Lee, Hoon Jai Chun, Chang Duck Kim, Chi Hyuk Oh, Hong Bae Kim
- Clin Endosc 2021;54(3):413-419. Published online October 20, 2020
- DOI: https://doi.org/10.5946/ce.2020.126

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Background
/Aims: Irreversible electroporation (IRE) is a relatively new ablation method. However, the application of IRE ablation in the treatment of biliary disease has not been attempted. A minimally invasive approach using endoscopic retrograde cholangiopancreatography (ERCP) can be a novel therapeutic modality for IRE ablation. In this study, we aimed to investigate the feasibility of endoscopic IRE for the biliary tract using an animal model.
Methods
A new catheter-type electrode was developed for endoscopic IRE ablation of the biliary tract. We performed ERCP and endoscopic IRE ablations in the normal common bile duct of Yorkshire pigs. The experimental setting of IRE was 500 V/cm (50 pulses, 100-µs length). The animals were sacrificed after 24 hr, and the ablated bile duct was examined.
Results
Well-demarcated focal color changes were observed on the mucosa of the common bile duct. The depth of change after IRE was confined to the mucosal and submucosal layers. Apoptotic changes in the bile duct were observed only around the IRE ablation area. Immunohistochemistry assay showed cell death in the bile duct along the electrode.
Conclusions
Endoscopic IRE ablation using ERCP was successfully performed in the common bile duct. It can be a potential option for the treatment of biliary tumors. -
Citations
Citations to this article as recorded by- Balloon‐assisted laser application for endoscopic treatment of biliary stricture
Seonghee Lim, Van Gia Truong, Seok Jeong, Jiho Lee, Byeong‐il Lee, Hyun Wook Kang
Lasers in Surgery and Medicine.2023; 55(10): 912. CrossRef - Biliary complications and efficacy after ablation of peribiliary tumors using irreversible electroporation (IRE) or radiofrequency ablation (RFA)
Somrach Thamtorawat, Rujira Patanawanitkul, Satit Rojwatcharapibarn, Walailak Chaiyasoot, Trongtum Tongdee, Jirawadee Yodying, Sukrit Sorotpinya
International Journal of Hyperthermia.2022; 39(1): 751. CrossRef - Large Animal Models in Pancreas and Biliary Disease
Seok Jeong, Jin-Seok Park, Don Haeng Lee
The Korean Journal of Gastroenterology.2021; 77(3): 99. CrossRef - Comparison of four endoluminal radiofrequency ablation devices and four power generators in an ex vivo bovine liver model
Stephan Rheinheimer, Anna Jacobsen, Philipp Mayer, Hans-Ulrich Kauczor, Andreas Mahnken
World Academy of Sciences Journal.2021;[Epub] CrossRef
- Balloon‐assisted laser application for endoscopic treatment of biliary stricture
- 5,068 View
- 161 Download
- 3 Web of Science
- 4 Crossref

Case Report
- A Case of Congenital Common Bile Duct Web Treated with Balloon Dilation under Endoscopic Retrograde Cholangiopancreatography in a Young Child
- Ji Sook Park, Hong Jun Kim, Ji-Hyun Seo, Hee-Shang Youn
- Clin Endosc 2021;54(2):285-288. Published online September 10, 2020
- DOI: https://doi.org/10.5946/ce.2020.167

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Web in common bile duct (CBD web) is very rare. It is usually asymptomatic and detected incidentally during surgery for other causes in adults. It can be congenital or acquired, however congenital CBD web is extremely rare. Currently, despite its invasiveness and complications, endoscopic retrograde cholangiopancreatography (ERCP) is considered as a useful diagnostic and therapeutic modality in children with hepatobiliary pancreatic diseases as in adults. Herein we report a case of congenital CBD web presenting with acute pancreatitis and choledocholithiasis in a 4-year-old girl which was diagnosed and treated using balloon dilation under ERCP. After balloon dilation of the web, a common pancreatobiliary channel was observed. To the best of our knowledge, a case of congenital CBD web with pancreatobiliary junctional abnormality treated using ERCP in a child has not been reported to date.
- 4,200 View
- 103 Download


 KSGE
KSGE


 First
First Prev
Prev



